Abstract
Self-care is a critical component of chronic disease management and is linked to better health outcomes. The Hypertension Self-Care Profile (HBP SCP) is one of the few validated instruments designed to assess not only behaviors but also self-efficacy and motivation in HBP self-care. This scoping review synthesized published research using the HBP SCP to examine its scope and utility across diverse populations. A total of 48 studies were reviewed—34 non-validation studies and 14 validation studies—spanning regions including Asia, the Middle East, and the Americas. The HBP SCP showed strong psychometric performance across multiple cultural adaptations, with Cronbach’s alpha values ranging from 0.73 to 0.99. Several correlates of HBP self-care emerged, including self-efficacy, social support, health literacy, and education. Findings also revealed that HBP self-care remains suboptimal, particularly among rural populations and low- and middle-income countries. The HBP SCP has proven to be a versatile and culturally adaptable instrument for evaluating HBP self-care behaviors, self-efficacy, and motivation. Its consistently demonstrated validity and reliability across diverse contexts, combined with its responsiveness in randomized controlled trials, affirm its value as both a clinical assessment tool and a research outcome measure in interventions aimed at improving cardiovascular health.
1. Introduction
High blood pressure (HBP) is a major risk factor that can cause serious cardiovascular health consequences such as stroke, coronary heart disease, heart failure, and kidney disease []. HBP is also associated with other debilitating outcomes including dementia []. Globally, an estimated 1.28 billion adults aged 30–79 years have HBP, defined as systolic blood pressure (BP) ≥ 140 mm Hg and/or diastolic BP ≥ 90 mm Hg []. According to a report using data from the National Health and Nutrition Examination Survey (NHANES) 2017–2020, nearly half of adults (48.1% or 119.9 million) in the United States (US) have HBP [].
Despite effective pharmacological and nonpharmacological treatment, BP control (systolic BP < 140 mm Hg and diastolic BP < 90 mm Hg) remains suboptimal; per recent research, even declining. For example, Muntner et al. [] analyzed data from NHANES 2009 to 2012, 2013 to 2016, and 2017 to 2020 and found that 52.8%, 51.3%, and 48.2% of US adults with HBP had controlled BP, in the respective periods. Data from NHANES 2017–2020 revealed that compared with non-Hispanic White adults, BP control was less likely among non-Hispanic Black, non-Hispanic Asian, and Hispanic adults (25.1% versus 16.8%, 18.4%, and 17.2%, respectively) [].
Self-care is an integral part of chronic disease management and has been linked to better health outcomes, including BP control [,,,]. Within the context of HBP, self-care areas encompass non-smoking, weight management, exercise, low-sodium and low-fat diet, decreased alcohol consumption, monitoring of BP, stress reduction, and other adherence activities such as regular physician visits and medication taking [,]. As such, existing tools addressing HBP self-care evaluate some (e.g., Hill–Bone Adherence Scale, Morisky Medication Scale, or Hypertension Self-Care Activity Level Effects) [,] or all of these areas (e.g., Hypertension Self-Care Profile [HBP SCP]) []. In particular, guided by two theoretical approaches—Orem’s Self-Care model and Motivational Interviewing—HBP SCP is one of the few validated instruments designed to measure not only behavior but also self-efficacy and motivation in terms of HBP self-care, hence allowing researchers to use one or more of the relevant scales per their study focus.
Since the original validation study was published in 2014 [], HBP SCP has been used in multiple studies with various designs and samples. A few reviews were done to include HBP SCP and other instruments addressing self-efficacy in cardiovascular disease or self-management for adults with diverse chronic conditions such as diabetes, HIV/AIDS, heart disease/HBP and arthritis [,,]. None of the published reviews specifically looked at HBP SCP, nor did they comprehensively examine the psychometrics of the instrument across the empirical studies conducted. Given the ongoing popularity and continuing use of HBP SCP, the purpose of this review was to identify published research using HBP SCP and synthesize the findings from the studies to better understand the scope and utility of HBP SCP as an instrument measuring HBP self-care behavior, motivation and self-efficacy across diverse settings, populations, and languages.
2. Materials and Methods
2.1. Design and Search
We conducted a scoping review [] to identify, select, and synthesize relevant studies using the HBP SCP. In consultation with a medical librarian, the search strategy was defined by aggregating various search terms that describe the HBP SCP instrument. The terms “High Blood Pressure Self-Care Profile”, “Hypertension Self-Care Profile”, “Self-Care Profile”, and “Hypertension Self-Care” were entered into the following databases: PubMed, Scopus, Google Scholar, Embase, CINAHL, Web of Science, and Cochrane. We conducted an initial search on 30 October 2023, and another search on 11 March 2024, to cover more recent publications, which resulted in the final search to include articles published from January 2014 to March 2024. A manual search was also performed in March 2024 to identify any additional relevant articles. This review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
2.2. Selection of Studies
Figure 1 illustrates the flow of our study selection process. We included peer-reviewed studies published in English that utilized one or more of the HBP SCP scales. Specifically, studies that validated psychometric properties, provided translation of the instrument, or utilized the HBP SCP as a study variable or outcome measurement were included. Additionally, non-English papers were included if an accompanying abstract was written in English and provided sufficient data for extraction. Excluded literature included review articles, study protocols, and studies that did not utilize the instrument. The initial search yielded 173 records, with 175 additional records from a second search, totaling 348. After removing duplicates, 165 titles and abstracts were screened for relevance. Each record was independently reviewed by two of the three authors (CB, FEM, and YT). Discrepancies were resolved by consensus among the authors. A total of 110 records were deemed ineligible for the following reasons: use of other instruments to measure HBP self-care (n = 45), did not use any instrument related to HBP self-care (n = 39), unpublished dissertations (n = 15), and non-English publications (n = 11). The remaining 55 records underwent full-text review. Of the 55 full-text articles, three were review papers [,,], two were study protocols without data [,], and two studies used some of the items on the HBP SCP to create a new instrument measuring different concepts such as dietary regulation [] or knowledge []. Ultimately, 48 studies were included in the analysis.
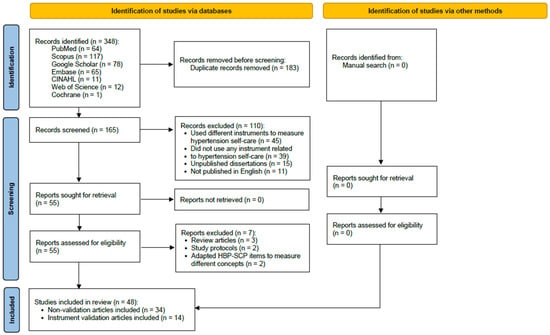
Figure 1.
PRISMA 2020 flow diagram for new systematic reviews which included searches of databases and other sources []. This work is licensed under CC BY 4.0. To view a copy of this license, visit https://creativecommons.org/licenses/by/4.0/ (accessed on 5 August 2025).
2.3. Data Extraction
Preliminary data extraction was conducted and included study-specific information including author and publication year, country of origin, language, study design, study sample demographics, number and method of instrument administration, psychometrics properties and main findings. All the initial extraction and discrepancies were rectified by the first senior author (HRH). Subsequently, two authors (CB and FEM) synthesized and organized data based on whether instrument validation was a primary goal of the literature and presented this information in the tables.
3. Results
3.1. Characteristics of Studies
This review includes 48 studies that used the HBP SCP. All non-validation studies (n = 34) are summarized in Table 1 and the instrument validation studies (n = 14) in Table 2. The majority of the non-validation studies used descriptive or correlational study design (n = 18) [,,,,,,,,,,,,,,,,,] followed by clinical trials using either quasi-experimental (n = 8) [,,,,,,,] or experimental study designs (n = 6) [,,,,,]. One study [] used case-control design, and one study [] examined the psychometric properties of the Chinese version of the Dyadic Relationship Scale, using the HBP SCP to provide evidence for convergent validity. The validation studies included 14 studies that translated, adapted, or validated the HBP SCP for various cultural and linguistic contexts [,,,,,,,,,,,,,].

Table 1.
Characteristics of non-validation studies using HBP SCP and associated factors (n = 34).

Table 2.
Characteristics of validation studies of HBP SCP (n = 14).
The studies represented a diverse geographical spread: twenty-two studies were conducted in Southeast Asia (e.g., the Philippines, Vietnam, Indonesia, Singapore, Malaysia, and Thailand) [,,,,,,,,,,,,,,,,,,,,,], ten in the Middle East (Saudi Arabia, Iran, and Turkey) [,,,,,,,,,], eight in the Americas (the US and Brazil) [,,,,,,,], six in East Asia (the Republic of Korea and China) [,,,,,], and two in South Asia (Nepal and Bhutan) [,]. A total of 10,251 participants were included in these studies with sample sizes ranging from 11 to 1123. The majority of the participant samples consisted of adult patients with HBP (n = 40), but also included healthy populations (n = 3) [,,] and others with chronic conditions such as stroke (n = 2) [,], HBP with complications (n = 1) [], chronic kidney disease (n = 1) [], and peripheral neuropathy (n = 1) [].
3.2. Use of HBP SCP Scales
Most studies used one of the three scales included in the HBP SCP—behaviors, motivation, and self-efficacy. Eight studies examined all three scales of the HBP SCP in primary care or community-based clinical settings across diverse countries [,,,,,,,]. Detailed results of the non-validation studies can be found in Table S1.
3.2.1. Behavior Scale
The behavior scale was most frequently used, appearing in 23 of 34 non-validation studies [,,,,,,,,,,,,,,,,,,,,,,]. Studies employed cross-sectional designs [,,,,,,,,,,,,,,,], quasi-experimental studies [,,,], and randomized controlled trials [,,]. Most were conducted in primary care or community settings, including urban clinics [,,,] and rural health centers [,], with fewer targeting specialized populations [,,,].
AlHadlaq et al. [] found less than half of Saudi patients engaged in BP self-monitoring (37.9%) or dietary modifications (35.8%), while adherence to smoking cessation (65.2%) and physician visits (85.0%) was higher. Dorji et al. [] noted Bhutanese participants occasionally practiced lifestyle modifications, with smoking cessation scoring higher (mean = 3.3) than dietary or physical activity behaviors. Visanuyothin et al. [] reported only 13% of Thai participants demonstrated adequate HBP self-care behaviors. Buco et al. [] observed HBP self-care was significantly associated with quality of life in rural Philippines (β = 0.15, p = 0.016).
Studies identified factors influencing HBP self-care behaviors. Bahari et al. [] found family support and self-efficacy positively associated with self-care behaviors among Saudi men (β = 0.63, p < 0.05). Ho et al. [] reported health literacy significantly linked to behavior scores among Singaporean adults with HBP and chronic kidney disease (β = 0.30, p < 0.001). Lunyera et al. [] found improved perceived neighborhood health significantly impacted behavior scores among African Americans in Baltimore. Higher education and family support consistently predicted better self-care behaviors. Kim et al. [] found significant correlations between higher education and improved HBP self-care in US online participants. Salim et al. [] revealed higher education levels correlated with better adherence in Malaysian primary care patients, with education positively associated with HBP SCP scores (p < 0.001).
Interventions to improve HBP self-care behaviors showed promising results. Moon et al. [] compared smartphone app intervention with traditional logbooks in Singapore, finding no significant differences in behavior scores (p = 0.43) but higher adherence to BP monitoring among older app users. Zabler et al. [] observed significant improvements in behavior scores over six months among low-income African American patients, with scores increasing from baseline (mean = 46.73) to follow-up (mean = 54.27, p < 0.001). Zeng et al. [] demonstrated significant post-intervention improvements in rural Chinese patients (F = 17.668, p < 0.001). Visanuyothin et al. [] showed that a six-month health literacy intervention improved behavior scores in Thai urban participants (mean = 2.4 to 2.7, p < 0.001).
3.2.2. Self-Efficacy Scale
The self-efficacy scale appeared in 19 of 34 non-validation studies [,,,,,,,,,,,,,,,,,,] across primary care clinics [,,], community clinics [,], and rural settings []. Self-efficacy consistently influenced HBP self-care behaviors. Ho et al. [] and Wee et al. [] found higher self-efficacy scores associated with improved self-care behaviors, particularly medication adherence and lifestyle modifications. Zeng et al. [] demonstrated that self-efficacy improvements significantly enhanced adherence to diet, medication, and exercise in rural Chinese populations. Boulware et al. [] reported that intervention participants achieved significantly higher self-efficacy and behavior scores than usual care. Lunyera et al. [] observed better self-efficacy linked to improved medication adherence and BP monitoring among African Americans. Gardiner et al. [] found positive relationships between self-efficacy and dietary/physical activity adherence in older adults. Türkoğlu et al. [] reported significant self-efficacy increases following educational interventions. Bahari et al. [] and Pahria et al. [] found that self-efficacy mediated relationships between social support and self-care behaviors. Han et al. [] reported that culturally tailored interventions for Spanish-speaking Latinos improved self-efficacy significantly. Salim et al. [] found men had lower self-efficacy scores than women. Rasyid et al. [] reported that lower self-efficacy scores increased risk of poor HBP outcomes. Zeng et al. [] found a strong negative correlation between the HBP SCP self-efficacy scale and Dyadic Relationship Scales (r = −0.70, p < 0.001).
3.2.3. Motivation Scale
The motivation scale was used less frequently, appearing in 10 of 34 non-validation studies [,,,,,,,]. Most studies were conducted in primary care or community settings [,,,], with interventions in community clinics [] and digital platforms []. AlHadlaq et al. [] reported low engagement in physical activity (12.8%) but moderate motivation for healthier cooking (60.9%) and limiting high-salt condiments (56.7%). Ho et al. [] observed significant positive association between motivation and self-care behaviors (β = 0.40, p < 0.001). Wee et al. [] identified education and family support as factors contributing to higher motivation scores. Pahria et al. [] demonstrated motivation as a significant predictor of adherence among Indonesian patients with hypertensive complications. Boulware et al. [] observed that patients in a problem-solving intervention had significantly higher motivation scores, improving self-care behaviors versus usual care (OR = 18.7, 95% CI = 4.0–87.3). Moon et al. [] found no significant differences in motivation between smartphone app and traditional logbook groups, though both experienced slight post-intervention increases.
3.3. Psychometrics of HBP SCP
Fourteen of the 48 studies included psychometric information. Most of the validation studies focused on translating and validating measurements (n = 12), while two studies involved validation using either web-based approaches [] or comparison between the Self-Care of Hypertension Inventory and HBP SCP []. Most studies employed forward and backward translation methods to ensure the tool’s adaptability to local populations (n = 11). One study [] utilized Cha’s combined translation technique [], which includes forward–backward translation, bilingual techniques, group discussions, and pretest strategies. The full measurement has been translated into various languages, including Arabic [], Persian [], Turkish [,], Chinese [], Indonesian [,], Vietnamese [], and Singaporean contexts [,,]. Some studies focused on translating and validating specific subscales. For example, the behavioral and self-efficacy scales were validated in Arabic [], the self-efficacy scale in Persian [], and the behavioral scale in Korean []. Psychometric properties from validation studies of HBP SCP are presented in Table S2.
3.3.1. Validity
HBP SCP validity was tested among adult patients across community [], public places [], senior welfare centers [], community health centers [,], primary care clinics [,,,,,], outpatient clinics [,], and in-hospital settings [,]. Approaches included content validity index, factor analyses, and concurrent/criterion validity testing.
Nine studies evaluated content validity through expert review panels, with content validity indexes ranging from 0.80 to 0.99. Upoyo et al. [] achieved CVI of 0.96 for the Indonesian version. Versiyonunun et al. [] reported mean CVI of 0.99 for behavior, 0.98 for motivation, and 0.96 for self-efficacy in the Turkish version.
Construct validity was assessed in nine studies using exploratory or confirmatory factor analysis [,,,,,,,,]. Bahari et al. [] found Arabic version factor loadings for the behavior scale (0.26–0.70) and self-efficacy scale (0.29–0.77), though three behavior items and one self-efficacy item fell below the 0.30 threshold. The Persian version identified three factors with loadings ranging from dietary (0.47–0.74), disease management (0.36–0.68), and treatment adherence (0.56–0.63), demonstrating good model fit (NNFI = 0.90, CFI = 0.91, IFI = 0.91, RMSEA = 0.082) []. The Turkish version explained 46.32% variance for behavior, 45.87% for motivation, and 48.08% for self-efficacy scales, with factor loadings of 0.62–0.78, 0.54–0.80, and 0.57–0.77, respectively []. The Chinese version identified six behavior factors, with health promotion (63.15%) and habit modification (10.01%) as primary contributors []. The Vietnamese version showed standardized factor loadings from 0.35 to 0.96 with acceptable convergent validity [].
Na et al. [] tested the concurrent validity of the Korean behavior scale, finding significant correlations with self-efficacy (r = 0.32) and HBP treatment compliance (r = 0.39). Zhao et al. [] demonstrated criterion validity by finding strong correlation (r = 0.70) between the Chinese HBP SCP and Exercise of Self-Care Agency Scale among 200 older Chinese adults.
3.3.2. Reliability
Studies with psychometric information reported reliability using Cronbach’s alpha (n = 14) [,,,,,,,,,,,,,], Guttman split-half reliability (n = 2) [,], and Spearman–Brown reliability (n = 1) []. Cronbach’s alpha values were consistently high, ranging from 0.73 to 0.99 for total scale and 0.81–0.96 for behavior, 0.88–0.95 for motivation, and 0.78–0.95 for self-efficacy subscales. Some studies reported very high values (>0.95) for total scale [,], self-efficacy [,], and behavior subscales [].
The Vietnamese version identified five behavior factors with overall Cronbach’s alpha of 0.79 and subscale values of 0.69 for advanced self-management skills, 0.82 for adverse health behaviors, 0.76 for medication adherence, 0.73 for diet-related knowledge, and 0.68 for information skills []. Split-half reliability demonstrated good internal consistency with coefficients of 0.83 for behavior, 0.94 for motivation, 0.75 for self-efficacy for the Turkish version [], and 0.91 for total scale for the Chinese version []. Spearman–Brown reliability coefficients for the Turkish version were 0.85 for behavior, 0.96 for motivation, and 0.75 for self-efficacy [].
Test–retest reliability was assessed in eight studies [,,,,,,,] with ICC values of 0.66–0.95 for behavior, 0.66–0.98 for motivation, 0.67–0.93 for self-efficacy, and 0.93 for total scale. The Malaysian version tested among Singaporean adults reported the lowest ICC values (0.66 for behavior, 0.66 for motivation, 0.68 for self-efficacy), likely due to low online response rate (43%) and lack of incentives []. Gheshlagh et al. [] reported higher test–retest reliability with ICC of 0.93 for the total scale over two weeks among 260 patients in Tehran.
4. Discussion
This review synthesized current evidence on the use of the HBP SCP and its role in evaluating HBP self-care behaviors, self-efficacy, and motivation across diverse populations, settings, and study designs. Across studies, the HBP SCP demonstrated consistent associations with BP control and self-care adherence outcomes, highlighting its sensitivity to change over time and utility in intervention research. Additionally, we found that the HBP SCP has been widely adapted into various languages, with the translated versions showing strong psychometric properties.
The HBP SCP proved to be a versatile instrument, used successfully in cross-sectional, quasi-experimental, and RCT designs. In particular, RCTs leveraging the HBP SCP as a primary or secondary outcome measure demonstrated its responsiveness to interventions aimed at improving self-care. Studies showed significant pre- and post-intervention differences in HBP self-care behavior scores, indicating its effectiveness in detecting behavioral changes among low-income African Americans in the US [,], adults with HBP in rural China [], patients with stroke [], or housewives with HBP in Indonesia [], community-residing adults with HBP in Malaysia [], and individuals in urban communities in Thailand []. Both Boulware et al. [] and Yatim et al. [] also observed significant improvements in self-efficacy and motivation among the intervention participants. Similarly, Türkoğlu et al. [] and Zeng et al. [] found improved self-efficacy in managing HBP among adult patients with HBP in Turkey and rural China, respectively. Taken together, this highlights the value of the HBP SCP as both a clinical assessment tool and a research outcome measure in intervention trials aiming to reduce cardiovascular risk through improved HBP self-management. Future research is warranted to investigate how the HBP SCP compares to other established tools in its ability to detect differences in HBP self-care across patient subgroups and to identify individuals at risk for poor BP control due to inadequate self-care. Such investigations could help determine its relative utility and inform its broader adoption in practice.
The findings revealed that overall levels of HBP self-care remain suboptimal, particularly among rural populations and in studies conducted in low- and middle-income countries [,,,]. These studies reported low scores in key self-care areas such as medication adherence, physical activity, and dietary modifications, highlighting persistent challenges in translating knowledge into behavior. Barriers identified in these settings included limited access to healthcare resources—including medication—low health literacy, poor patient–provider communication, and a shortage of skilled providers [,,,]. These challenges underscore the need for more context-specific interventions and support systems to improve HBP self-care. Promising strategies include expanding non-communicable disease services through community pharmacies, implementing community outreach programs using mobile health interventions and community health workers, and mobilizing telehealth systems—approaches that have demonstrated effectiveness in enhancing HBP management in under-resourced populations, especially from the COVID-19 pandemic onward [,,].
The potential for digital and mobile implementation of the tool represents a significant future direction. While this scoping review focused on synthesizing published research using the tool in its various applications, integrating such a validated tool into digital or mobile health platforms presents a considerable opportunity. Integrating this validated tool into digital or mobile health platforms could allow individuals to routinely input self-care behaviors, receive real-time feedback, and access personalized educational content, fostering greater engagement and adherence. For clinicians, such digital solutions could streamline assessment, enable remote monitoring, and facilitate timely interventions. Incorporating the HBP SCP into digital and mobile health interventions offers scalable and accessible avenues for improving cardiovascular health outcomes, warranting future research into its feasibility, usability, and effectiveness.
Several key correlates of HBP self-care emerged from the studies included in this review. Specifically, greater self-efficacy [,,], stronger social support [,], and higher levels of health literacy [,] were associated with higher self-care behavior scores. As well, higher education was consistently associated with better self-care behaviors [,,,]. In contrast, comorbidities [] and low income [] were associated with lower self-care scores. Notably, Buco et al. [] found that larger family size negatively affected disease self-management among community-dwelling older adults in the Philippines. A similar pattern was observed among US-residing Korean-American older adults with HBP []: those living alone—mostly residing in senior group housing—were at least twice as likely to have controlled BP compared to those living with others. Post-survey interviews revealed that frequent social interactions in senior group housing which involved encouragement about medication taking and health information sharing contributed to better HBP management []. With growing attention to the role of social determinants in cardiovascular outcomes [], one of the studies included in the review [] revealed that better neighborhood aesthetic quality and greater healthy food availability were associated with better self-care behaviors. Further, healthy food availability attenuated the negative impact of neighborhood violence on HBP self-care among socially disadvantaged Black or African American individuals. These findings point to the critical importance of both individual psychosocial and broader social factors in shaping HBP outcomes.
This review revealed the adaptation and application of the HBP SCP across diverse cultural and linguistic contexts. Thirteen published studies reported successful translation and validation of the tool in different languages, including Arabic [], Persian [], Turkish [,], Chinese [], Indonesian [,], Korean [], Vietnamese [], and in Singaporean contexts [,,], while demonstrating cultural relevance and strong evidence of validity and reliability. Notably, validity testing was conducted in various real-world healthcare settings such as community health centers, primary care, and outpatient clinics. Construct validity was robust and supported through exploratory and confirmatory factor analyses, although cultural relevance influenced factor loadings in some contexts—such as in Saudi Arabia, where smoking-related items on the HBP SCP were affected due to the cultural and religious unacceptability of smoking in Islamic tradition []. The results highlight the need for culturally informed implementation and interpretation when applying standardized tools like the HBP SCP across global populations.
Despite offering valuable insights into the global application and utility of the HBP SCP, this review has limitations. Cultural modifications, such as omitting items related to alcohol or smoking due to sociocultural norms, were often reported but rarely followed by full re-validation, raising potential concerns about construct equivalence across versions. To address these gaps, future research should prioritize standardized cross-cultural adaptation guidelines [,], while adopting established reporting guidelines. For instance, the recommendations by Streiner and Kottner [] provide a comprehensive framework for reporting instrument development and testing, emphasizing clarity in methodology and results. Beyond linguistic translation, incorporating community-based participatory approaches can help integrate culture-specific contexts such as gender norms, literacy levels, and social support structures that may influence HBP self-care [,,]. Future adaptations may also incorporate advanced psychometric methods like item response theory and Rasch modeling [] to tailor HBP SCP to population-specific needs such as varying literacy levels while maintaining psychometric rigor. Another limitation is the possibility that some relevant studies may have been missed due to the limitations of the databases searched or variations in terminology used to describe the instrument. While a comprehensive search strategy was employed in consultation with a medical librarian, including multiple databases and manual searches, inconsistent naming conventions or indexing across studies may have limited the identification of all eligible publications.
5. Conclusions
The HBP SCP demonstrated its utility and cross-cultural adaptability, validity, and reliability, making it a suitable tool for evaluating HBP self-care behaviors, self-efficacy, and motivation across diverse populations and settings. Its demonstrated responsiveness in randomized trials affirms the value of HBP SCP as both a clinical and research tool. The successful cultural and linguistic adaptation of the HBP SCP in multiple regions further highlights its global applicability.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph22081244/s1, Table S1: Main findings of non-validation studies using HBP SCP (n = 34); Table S2: Psychometric properties result from validation studies of HBP SCP (n = 14).
Author Contributions
H.-R.H. conceptualized the study and developed the methodology. H.-R.H. led the study. C.B., F.E.M., and Y.T. screened the studies and performed the analysis. H.-R.H., C.B., F.E.M., and Y.T. wrote the manuscript. H.-R.H., C.B., F.E.M., Y.T., and Y.C.-M. critically reviewed and edited the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Acknowledgments
We acknowledge the late Miyong Kim for her contributions to the development and initial validation of the Hypertension Self-Care Profile. Her dedication and expertise were essential to the success of this research, and she is greatly missed.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| BP | Blood pressure |
| CI | Confidential interval |
| CFI | Comparative fit index |
| CVI | Content validity index |
| GFI | Goodness of fit index |
| HBP | High blood pressure |
| HBP SCP | Hypertension Self-Care Profile |
| ICC | Intraclass correlation coefficient |
| IFI | Incremental fit index |
| IQR | Interquartile range |
| KMO | Kaiser–Meyer–Olkin |
| NA | Not applicable |
| NR | Not reported |
| NHANES | National Health and Nutrition Examination Survey |
| NNFI | Non-normed fit index |
| OR | Odds ratio |
| RCT | Randomized controlled trial |
| RMSEA | Root mean square error of approximation |
| SD | Standard deviation |
| TLI | Tucker–Lewis index |
| US | United States |
References
- Martin, S.S.; Aday, A.W.; Almarzooq, Z.I.; Anderson, C.A.M.; Arora, P.; Avery, C.L.; Baker-Smith, C.M.; Barone Gibbs, B.; Beaton, A.Z.; Boehme, A.K.; et al. 2024 Heart Disease and Stroke Statistics: A Report of US and Global Data from the American Heart Association. Circulation 2024, 149, e347–e913. [Google Scholar] [CrossRef]
- Raber, I.; Belanger, M.J.; Farahmand, R.; Aggarwal, R.; Chiu, N.; Al Rifai, M.; Jacobsen, A.P.; Lipsitz, L.A.; Juraschek, S.P. Orthostatic Hypotension in Hypertensive Adults: Harry Goldblatt Award for Early Career Investigators 2021. Hypertension 2022, 79, 2388–2396. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Hypertension. Available online: https://www.who.int/news-room/fact-sheets/detail/hypertension (accessed on 20 May 2025).
- Centers for Disease Control and Prevention [CDC]. Hypertension Cascade: Hypertension Prevalence, Treatment and Control Estimates Among US Adults Aged 18 Years and Older Applying the Criteria from the American College of Cardiology and American Heart Association’s 2017 Hypertension Guideline—NHANES 2017–2020. Available online: https://millionhearts.hhs.gov/data-reports/hypertension-prevalence.html (accessed on 20 May 2025).
- Muntner, P.; Miles, M.A.; Jaeger, B.C.; Hannon Iii, L.; Hardy, S.T.; Ostchega, Y.; Wozniak, G.; Schwartz, J.E. Blood Pressure Control Among US Adults, 2009 to 2012 Through 2017 to 2020. Hypertension 2022, 79, 1971–1980. [Google Scholar] [CrossRef]
- Ausili, D.; Masotto, M.; Dall’Ora, C.; Salvini, L.; Di Mauro, S. A literature review on self-care of chronic illness: Definition, assessment and related outcomes. Prof. Inferm. 2014, 67, 180–189. [Google Scholar] [PubMed]
- Cano, F.; Alves, E.; João, A.; Oliveira, H.; Pinho, L.G.; Fonseca, C. A rapid literature review on the health-related outcomes of long-term person-centered care models in adults with chronic illness. Front. Public Health 2023, 11, 1213816. [Google Scholar] [CrossRef] [PubMed]
- Maharjan, S.R.S.; Davenport, A. The effects of supported shared-care and hemodialysis self-care on patient psychological well-being, interdialytic weight gain, and blood pressure control. Hemodial. Int. 2020, 24, 29–35. [Google Scholar] [CrossRef]
- Avegno, K.S.; Roberson, K.B.; Onsomu, E.O.; Edwards, M.F.; Dean, E.L.; Bertoni, A.G. Evaluating a Telephone and Home Blood Pressure Monitoring Intervention to Improve Blood Pressure Control and Self-Care Behaviors in Adults with Low-Socioeconomic Status. Int. J. Environ. Res. Public Health 2023, 20, 5287. [Google Scholar] [CrossRef]
- Riegel, B.; Moser, D.K.; Buck, H.G.; Dickson, V.V.; Dunbar, S.B.; Lee, C.S.; Lennie, T.A.; Lindenfeld, J.; Mitchell, J.E.; Treat-Jacobson, D.J.; et al. Self-Care for the Prevention and Management of Cardiovascular Disease and Stroke: A Scientific Statement for Healthcare Professionals from the American Heart Association. J. Am. Heart Assoc. 2017, 6, e006997. [Google Scholar] [CrossRef]
- Han, H.R.; Lee, H.; Commodore-Mensah, Y.; Kim, M. Development and validation of the Hypertension Self-care Profile: A practical tool to measure hypertension self-care. J. Cardiovasc. Nurs. 2014, 29, E11–E20. [Google Scholar] [CrossRef]
- Warren-Findlow, J.; Basalik, D.W.; Dulin, M.; Tapp, H.; Kuhn, L. Preliminary validation of the Hypertension Self-Care Activity Level Effects (H-SCALE) and clinical blood pressure among patients with hypertension. J. Clin. Hypertens. 2013, 15, 637–643. [Google Scholar] [CrossRef]
- Han, H.R.; Song, H.J.; Nguyen, T.; Kim, M.T. Measuring self-care in patients with hypertension: A systematic review of literature. J. Cardiovasc. Nurs. 2014, 29, 55–67. [Google Scholar] [CrossRef]
- Turan Kavradim, S.; Yangöz, Ş.T.; Canli Ozer, Z.; Boz, I. Instruments to assess self-efficacy among people with cardiovascular disease: A COSMIN systematic review. Int. J. Clin. Pract. 2020, 74, e13606. [Google Scholar] [CrossRef] [PubMed]
- Lua, A.Y.H.; Hong, L.; Bong, S.H.S.; Yeo, J.L.S.; Tsang, M.L.P.; Ong, K.Z.; Wong, S.S.W.; Tan, N.C. A narrative review of the evaluation and selection of instruments which assess self-efficacy amongst patients with essential hypertension. Proc. Singap. Healthc. 2016, 25, 98–104. [Google Scholar] [CrossRef]
- Packer, T.L.; Fracini, A.; Audulv, Å.; Alizadeh, N.; van Gaal, B.G.I.; Warner, G.; Kephart, G. What we know about the purpose, theoretical foundation, scope and dimensionality of existing self-management measurement tools: A scoping review. Patient Educ. Couns. 2018, 101, 579–595. [Google Scholar] [CrossRef] [PubMed]
- Pujiastuti, T.; Aljaberi, M.A.; Sansuwito, T. Effectiveness of Android-based Hypertension Self-Care Education to Improve Blood Pressure Control among Hypertensive Patients at Yogyakarta: Study Protocol. Malays. J. Med. Health Sci. 2023, 19, 354–359. [Google Scholar] [CrossRef]
- Ephraim, P.L.; Hill-Briggs, F.; Roter, D.L.; Bone, L.R.; Wolff, J.L.; Lewis-Boyer, L.; Levine, D.M.; Aboumatar, H.J.; Cooper, L.A.; Fitzpatrick, S.J.; et al. Improving urban African Americans’ blood pressure control through multi-level interventions in the Achieving Blood Pressure Control Together (ACT) study: A randomized clinical trial. Contemp. Clin. Trials 2014, 38, 370–382. [Google Scholar] [CrossRef]
- Fikriana, R.; Nursalam, N.; Devy, S.; Ahsan, A.; Afik, A. The Effect of Coping Strategy on Dietary Regulation in Patient with Hypertension. Int. J. Psychosoc. Rehabil. 2020, 24, 7781–7787. [Google Scholar]
- Thomas, J. A proposed intervention to improve knowledge of self-management of hypertension for Kenneth Young and C4 community mental health center staff in Cook County, Illinois. J. Public. Health Med. 2022, 30, 121–134. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Acharya, R.; Chaudhary, A.; Pandey, J.; Pandey, C. Self-care management and its associated factors among patient with hypertension in Nepal. J. Chitwan Med. Coll. 2022, 12, 91–96. [Google Scholar] [CrossRef]
- AlHadlaq, R.K.; Swarelzahab, M.M.; AlSaad, S.Z.; AlHadlaq, A.K.; Almasari, S.M.; Alsuwayt, S.S.; Alomari, N.A. Factors affecting self-management of hypertensive patients attending family medicine clinics in Riyadh, Saudi Arabia. J. Fam. Med. Prim. Care 2019, 8, 4003–4009. [Google Scholar] [CrossRef] [PubMed]
- Bahari, G.; Scafide, K.; Krall, J.; Mallinson, R.K.; Weinstein, A.A. Mediating role of self-efficacy in the relationship between family social support and hypertension self-care behaviours: A cross-sectional study of Saudi men with hypertension. Int. J. Nurs. Pract. 2019, 25, e12785. [Google Scholar] [CrossRef]
- Buco, C.E.A.M.; Buenviaje, K.A.C.; Bulan, R.B.C.; Cabana, R.J.L.; Cabuhat, M.K.S.; Bongar, M.V.V.; Macindo, J.R.B. Developing and testing a model of quality of life among chronically-ill, community-dwelling older adults: A structural equation model. Arch. Gerontol. Geriatr. 2018, 78, 261–268. [Google Scholar] [CrossRef] [PubMed]
- Darvishpour, A.; Mansour-Ghanaei, R.; Mansouri, F. The relationship between health literacy, self-efficacy, and self-care behaviors in older adults with hypertension in the north of Iran. HLRP Health Lit. Res. Pract. 2022, 6, e262–e269. [Google Scholar] [CrossRef]
- Dorji, N.; Samartkit, N. Factors influencing lifestyle modification among persons with hypertension in Punakha, Bhutan. Bangk. Med. J. 2021, 17, 1–8. [Google Scholar] [CrossRef]
- Ea, E.E.; Colbert, A.; Turk, M.; Dickson, V.V. Self-care among Filipinos in the United States who have hypertension. Appl. Nurs. Res. 2018, 39, 71–76. [Google Scholar] [CrossRef]
- Ho, H.-K.; Koh, E.Y.-L.; Abdullah, A.; Tan, N.-C. Health literacy and self-care among patients with chronic kidney disease in a primary care setting. Singap. Med. J. 2024, 66, 307. [Google Scholar] [CrossRef]
- Jung, S.Y.; Moon, K.J. Factors affecting self-care among community-dwelling hypertensive older adults: A cross-sectional study. Nurs. Open. 2023, 10, 3892–3905. [Google Scholar] [CrossRef]
- Kim, M.T.; Murry, N.; Hecht, J.; Hutson, T.; Nnaka, T.; Ewere, T.; Heitkemper, E.; Hebert, E.T.; Radhakrishnan, K.; Stuifbergen, A. Patterns and correlates of physical symptoms among people with peripheral neuropathy. J. Neurol. Disord. 2022, 10, 523. [Google Scholar]
- Lunyera, J.; Davenport, C.A.; Ephraim, P.; Mohottige, D.; Bhavsar, N.A.; Clark-Cutaia, M.N.; Cabacungan, A.; DePasquale, N.; Peskoe, S.; Boulware, L.E. Association of Perceived Neighborhood Health With Hypertension Self-care. JAMA Netw. Open 2023, 6, e2255626. [Google Scholar] [CrossRef]
- Nazeri, N.S.; Mohamad, N.; Redzuan, M.; Mulud, Z.A. Social Support and Self-care Practice Among Patients With Hypertension in a Teaching Hospital. Malays. J. Med. Health Sci. 2022, 18, 281. [Google Scholar]
- Nursalam, N.; Fikriana, R.; Devy, S.R.; Ahsan, A. The development of self-regulation models based on belief in patients with hypertension. Syst. Rev. Pharm. 2020, 11, 1036–1041. [Google Scholar]
- Pahria, T.; Nugroho, C.; Yani, D.I. Factors influencing self-care behaviors in hypertension patients with complications. Vasc. Health Risk Manag. 2022, 18, 463–471. [Google Scholar] [CrossRef]
- Salim, H.; Lee, P.Y.; Sazlina, S.G.; Ching, S.M.; Mawardi, M.; Shamsuddin, N.H.; Ali, H.; Adibah, H.I.; Tan, N.C. The self-care profiles and its determinants among adults with hypertension in primary health care clinics in Selangor, Malaysia. PLoS ONE 2019, 14, e0224649. [Google Scholar] [CrossRef] [PubMed]
- Tan, P.P.S.; Sandhu, R.S.; Zain, S.M.; Hall, D.; Tan, N.C.; Lim, H.M.; Daud, F.; Pung, Y.-F. Health motivations and perceived barriers are determinants of self-care behaviour for the prevention of hypertension in a Malaysian community. PLoS ONE 2022, 17, e0278761. [Google Scholar] [CrossRef]
- Visanuyothin, S.; Plianbangchang, S.; Somrongthong, R. Appearance and potential predictors of poorly controlled hypertension at the primary care level in an urban community. J. Multidiscip. Healthc. 2018, 11, 131–138. [Google Scholar] [CrossRef]
- Wee, S.Y.; Salim, H.; Mawardi, M.; Koh, Y.L.E.; Ali, H.; Shariff Ghazali, S.; Lee, P.Y.; Ching, S.M.; Shamsuddin, N.H.; Tan, N.C. Comparing and determining factors associated with hypertension self-care profiles of patients in two multi-ethnic Asian countries: Cross-sectional studies between two study populations. BMJ Open 2021, 11, e044192. [Google Scholar] [CrossRef]
- Gardiner, P.; McGonigal, L.; Villa, A.; Kovell, L.C.; Rohela, P.; Cauley, A.; Rinker, D.; Olendzki, B. Our whole lives for hypertension and cardiac risk factors—Combining a teaching kitchen group visit with a web-based platform: Feasibility trial. JMIR Form. Res. 2022, 6, e29227. [Google Scholar] [CrossRef]
- Han, H.-R.; Delva, S.; Greeno, R.V.; Negoita, S.; Cajita, M.; Will, W. A health literacy-focused intervention for Latinos with hypertension. HLRP Health Lit. Res. Pract. 2018, 2, e21–e25. [Google Scholar] [CrossRef]
- Lee, H.-Y.; Lee, K.S. Withdrawal of antihypertensive medication in young to middle-aged adults: A prospective, single-group, intervention study. Clin. Hypertens. 2023, 29, 1. [Google Scholar] [CrossRef]
- Rasdiyanah, R.; Wiarsih, W.; Sukihananto, S. Health education using booklet and diary media on the self-efficacy of housewives with hypertension. J. Pendidik. Keperawatan Indones. 2020, 6, 14–25. [Google Scholar] [CrossRef]
- Türkoğlu, N.; Kılıc, D. Comparison of the effects of web-based and face-to-face training on the self-efficacy and health literacy of patients with hypertension: A quasi-experimental trial. Eskişehir Türk Dünyası Uygul. Ve Araştırma Merk. Halk Sağlığı Derg. 2022, 7, 15–25. [Google Scholar] [CrossRef]
- Lynch, E.B.; Tangney, C.; Ruppar, T.; Zimmermann, L.; Williams, J.; Jenkins, L.; Epting, S.; Avery, E.; Olinger, T.; Berumen, T.; et al. Heart 2 Heart: Pilot Study of a Church-Based Community Health Worker Intervention for African Americans with Hypertension. Prev. Sci. 2024, 25, 22–33. [Google Scholar] [CrossRef] [PubMed]
- Yatim, H.M.; Wong, Y.Y.; Lim, S.H.; Hassali, M.A.; Hong, Y.H.; Dali, A.F.; Neoh, C.F. Evaluation of a group-based hypertension self-management education programme among hypertensive community dwellers. Eur. J. Integr. Med. 2018, 24, 79–84. [Google Scholar] [CrossRef]
- Visanuyothin, S.; Manwong, M.; Thongnopakun, S. Community-Based Health Literacy Program on Uncontrolled Hypertension in Urban Area, Thailand. J. Public Hlth. Dev. 2020, 18, 74–88. [Google Scholar]
- Boulware, L.E.; Ephraim, P.L.; Hill-Briggs, F.; Roter, D.L.; Bone, L.R.; Wolff, J.L.; Lewis-Boyer, L.; Levine, D.M.; Greer, R.C.; Crews, D.C. Hypertension self-management in socially disadvantaged African Americans: The Achieving Blood Pressure Control Together (ACT) randomized comparative effectiveness trial. J. Gen. Intern. Med. 2020, 35, 142–152. [Google Scholar] [CrossRef] [PubMed]
- Moon, E.W.; Tan, N.C.; Allen, J.C.; Jafar, T.H. The use of wireless, smartphone app–assisted home blood pressure monitoring among hypertensive patients in Singapore: Pilot randomized controlled trial. JMIR mHealth uHealth 2019, 7, e13153. [Google Scholar] [CrossRef]
- Rasyid, A.; Pemila, U.; Aisah, S.; Harris, S.; Wiyarta, E.; Fisher, M. Exploring the self-efficacy and self-care-based stroke care model for risk factor modification in mild-to-moderate stroke patients. Front. Neurol. 2023, 14, 1177083. [Google Scholar] [CrossRef]
- Talebi, F.; Jesmi, A.A.; Rakhshani, M.H.; Tajabadi, A. Effects of telenursing on the management of self-care behaviors in patients with chronic hypertension. J. Res. Health 2023, 13, 273–280. [Google Scholar] [CrossRef]
- Zabler, B.; Tsai, P.Y.; Fendrich, M.; Cho, Y.; Taani, M.H.; Schiffman, R. Effect of a nurse case management intervention for hypertension self-management in low-income African Americans. Contemp. Clin. Trials 2018, 71, 199–204. [Google Scholar] [CrossRef]
- Zeng, D.; Yang, C.; Chien, W.T. Effects of a family dyadic partnership program for people with hypertension in a rural community: A pilot randomised controlled trial. Aust. J. Rural. Health 2021, 29, 435–448. [Google Scholar] [CrossRef] [PubMed]
- Rasyid, A.; Pemila, U.; Aisah, S.; Harris, S.; Wiyarta, E.; Fisher, M. Self-efficacy and self-care as risk factors for ischemic stroke: Development and validation of a nomogram. J. Clin. Med. 2023, 12, 5665. [Google Scholar] [CrossRef]
- Zeng, D.; Yang, C.; Chien, W.T. Testing the psychometric properties of a Chinese version of Dyadic Relationship Scale for families of people with hypertension in China. BMC Psychol. 2022, 10, 34. [Google Scholar] [CrossRef]
- Bahari, G.; Scafide, K.; Weinstein, A.A.; Krall, J.; Han, H.R. Assessment of Hypertension Self-Care Behaviors and Self-Efficacy Among Men in Saudi Arabia. J. Nurs. Meas. 2020, 28, 283–302. [Google Scholar] [CrossRef] [PubMed]
- Barati, F.; Sadeghmoghadam, L.; Sajjadi, M.; Nazari, S.; Bahri, N. Validation of the Persian version of self-care tools for hypertension among older adults. Med. Glas. 2019, 16, 156–161. [Google Scholar] [CrossRef]
- Gheshlagh, R.G.; Parizad, N.; Ghalenoee, M.; Dalvand, S.; Baghi, V.; Najafi, F.; Ebadi, A. Psychometric features of the persian version of self-efficacy tool for patients with hypertension. Int. Cardiovasc. Res. J. 2018, 12, 50–56. [Google Scholar]
- Kes, D.; Gökdoğan, F. Reliability and validity of a Turkish version of the hypertension self-care profile. J. Vasc. Nurs. 2020, 38, 149–155. [Google Scholar] [CrossRef]
- Koh, Y.L.E.; Lua, Y.H.A.; Hong, L.; Bong, H.S.S.; Yeo, L.S.J.; Tsang, L.P.M.; Ong, K.Z.; Wong, S.W.S.; Tan, N.C. Using a Web-Based Approach to Assess Test-Retest Reliability of the “Hypertension Self-Care Profile” Tool in an Asian Population: A Validation Study. Medicine 2016, 95, e2955. [Google Scholar] [CrossRef]
- Ma, Y.; Cheng, H.Y.; Sit, J.W.H.; Chien, W.T. Psychometric Evaluation of the Chinese Version of Hypertension Self-care Profile. J. Cardiovasc. Nurs. 2021, 36, 420–429. [Google Scholar] [CrossRef]
- Na, A.; Jun, Y.; Song, Y. Psychometric Properties of the Hypertension Self-Care Behavior Scale for Elders with Hypertension in Korea. J. Korean Acad. Fundam. Nurs. 2017, 24, 1–8. [Google Scholar] [CrossRef]
- Ngoh, S.H.A.; Lim, H.W.L.; Koh, Y.L.E.; Tan, N.C. Test-retest reliability of the Mandarin versions of the Hypertension Self-Care Profile instrument. Medicine 2017, 96, e8568. [Google Scholar] [CrossRef]
- Salami, S.; Soon Siew, C.; Said, F.M.; Wilandika, A. Psychometric Properties of The Indonesian Version of Hypertension Self Care Profile. Malays. J. Med. Health Sci. 2023, 19, 231–236. [Google Scholar] [CrossRef]
- Seow, K.C.; Mohamed Yusoff, D.; Koh, Y.L.E.; Tan, N.C. What is the test-retest reliability of the Malay version of the Hypertension Self-Care Profile self efficacy assessment tool? A validation study in primary care. BMJ Open 2017, 7, e016152. [Google Scholar] [CrossRef]
- Upoyo, A.S.; Taufik, A.; Anam, A.; Nuriya, N.; Saryono, S.; Setyopranoto, I.; Pangastuti, H.S. Translation and Validation of the Indonesian Version of the Hypertension Self-care Profile. Open Access Maced. J. Med. Sci. 2021, 9, 980–984. [Google Scholar] [CrossRef]
- Van Truong, P.; Lin, M.Y.; Chiu, H.Y.; Hou, W.H.; Tsai, P.S. Psychometric Properties and Factorial Structure of Vietnamese Version of the Hypertension Self-care Profile Behavior Scale. J. Cardiovasc. Nurs. 2021, 36, 446–453. [Google Scholar] [CrossRef]
- Versiyonunun, H.Ö.B.P.T. Psychometric Properties of the Turkish Version of Hypertension Self-Care Profile. Turk. J. Cardiovasc. Nurs. 2023, 14, 95–102. [Google Scholar] [CrossRef]
- Zhao, Q.; Guo, Y.; Gu, L.; Yang, L. Comparison of two instruments for hypertension self-care assessments among older adults from China. Nurs. Open 2023, 10, 1672–1683. [Google Scholar] [CrossRef]
- Cha, E.S.; Kim, K.H.; Erlen, J.A. Translation of scales in cross-cultural research: Issues and techniques. J. Adv. Nurs. 2007, 58, 386–395. [Google Scholar] [CrossRef]
- Mbah, T.B.; Lema, B.S.; Rikam, A.B.; Baning, J.M.B.; Ngon, S.B.; Kilama, G.M.; Ngon, D.G.; Ngon, O.; Ebango, F.P.T.; Ebango, S.A.S.; et al. A Call to Action: Insights into Hypertension Prevalence and Management in an Urban Sub-Saharan African Population. Niger. Med. J. 2025, 66, 290–302. [Google Scholar] [CrossRef]
- Wulandari, W.; Zakiyah, N.; Rahayu, C.; Puspitasari, I.M.; Suwantika, A.A. Health-related quality of life in hypertensive patients with chronic kidney disease in low and middle-income countries. BMC Nephrol. 2025, 26, 34. [Google Scholar] [CrossRef]
- Adhikari, R.; Shah, R.; Khanal, V. Older people’s challenges accessing health services in central Nepal: A qualitative study using the domain of access framework. BMC Health Serv. Res. 2024, 24, 1273. [Google Scholar] [CrossRef]
- Elnaem, M.H.; Mosaad, M.; Abdelaziz, D.H.; Mansour, N.O.; Usman, A.; Elrggal, M.E.; Cheema, E. Disparities in Prevalence and Barriers to Hypertension Control: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 14571. [Google Scholar] [CrossRef]
- Ayob, R.; Vally, M.; Khan, R.; Orchard, A. Disparities in patients’ understanding of cardiovascular disease management. Cardiovasc. J. Afr. 2024, 35, 50–56. [Google Scholar] [CrossRef]
- Gentilini, A.; Kasonde, L.; Babar, Z.U. Expanding access to NCD services via community retail pharmacies in LMICs: A systematic review of the literature. J. Pharm. Policy Pract. 2025, 18, 2462450. [Google Scholar] [CrossRef]
- Han, H.R.; Song, Y.; Song, H.J.; Kim, M.T. Influence of living arrangements on the management and control of hypertension: A mixed-methods study of Korean American elderly. J. Immigr. Minor. Health 2013, 15, 944–952. [Google Scholar] [CrossRef] [PubMed]
- Powell-Wiley, T.M.; Baumer, Y.; Baah, F.O.; Baez, A.S.; Farmer, N.; Mahlobo, C.T.; Pita, M.A.; Potharaju, K.A.; Tamura, K.; Wallen, G.R. Social Determinants of Cardiovascular Disease. Circ. Res. 2022, 130, 782–799. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHOQOL Translation Methodology. Available online: https://cdn.who.int/media/docs/default-source/publishing-policies/whoqol-100-guidelines/translation-methodology.pdf?sfvrsn=74cdb8f5_2 (accessed on 20 May 2025).
- Kim, M.T.; Han, H.R. Cultural considerations in research instrumentation development. In Instruments for Clinical Health Care Research, 3rd ed.; Frank-Stromborg, M., Olsen, S., Eds.; Jones & Bartlett Pub.: Sudbury, MA, USA, 2004; pp. 73–80. [Google Scholar]
- Streiner, D.L.; Kottner, J. Recommendations for reporting the results of studies of instrument and scale development and testing. J. Adv. Nurs. 2014, 70, 1970–1979. [Google Scholar] [CrossRef] [PubMed]
- Warnecke, R.B.; Johnson, T.P.; Chávez, N.; Sudman, S.; O’Rourke, D.P.; Lacey, L.; Horm, J. Improving question wording in surveys of culturally diverse populations. Ann. Epidemiol. 1997, 7, 334–342. [Google Scholar] [CrossRef]
- Stewart, A.L.; Nápoles-Springer, A. Health-related quality-of-life assessments in diverse population groups in the United States. Med. Care 2000, 38 (Suppl. 9), II102–II124. [Google Scholar] [CrossRef]
- Nguyen, T.H.; Paasche-Orlow, M.K.; Kim, M.T.; Han, H.R.; Chan, K.S. Modern Measurement Approaches to Health Literacy Scale Development and Refinement: Overview, Current Uses, and Next Steps. J. Health Commun. 2015, 20 (Suppl. 2), 112–115. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).