Highlights
- This case reveals the close connection between the infection with the HCV and the cryoglobulinemic vasculitis
- The particularity is represented by both the existence from the outset of the vasculitic disease and the current predialitic stage of the patient
Highlights
- This case reveals the close connection between the infection with the HCV and the cryoglobulinemic vasculitis
- The particularity is represented by both the existence from the outset of the vasculitic disease and the current predialitic stage of the patient
Abstract
Hepatitis C virus (HCV) represents a fundamental issue for public health, with long term evolution and the gradual appearance of several complications and associated pathologies. One of these pathologies is represented by cryoglobulinemic vasculitis, a disorder characterized by the appearance in the patient’s serum of the cryoglobulins, which typically precipitate at temperatures below normal body temperature (37 °C) and dissolve again if the serum is heated. Here, we describe the case of a patient diagnosed with HCV that, during the evolution of the hepatic disease, developed a form of cryoglobulinemic vasculitis. The connection between the vasculitis and the hepatic disorder was revealed following treatment with interferon, with the temporary remission of both pathologies and subsequent relapse at the end of the 12 months of treatment, the patient becoming a non-responder. The particularity of the case is represented by both the severity of the vasculitic disease from its onset and the deterioration of renal function up to the predialitic phase, a situation not typical of the evolution of cryoglobulinemia. Taking into account the hepatic disorder, the inevitable evolution towards cirrhosis, and the risk of developing the hepatocellular carcinoma, close monitoring is necessary.
Introduction
Patients with chronic hepatitis C virus (HCV) infection are at risk for a variety of extrahepatic manifestations (EHMs). Based on large cohort studies, up to 70% of patients develop hepatitis C virus extrahepatic manifestations [1,2]. Cryoglobulinemia represents a pathology based on the presence in the serum of immunoglobulins (Ig) that precipitate when the body temperature is lower than 37 °C, becoming soluble again when the body temperature exceeds 37 °C [3]. The presence of the cryoglobulins in the serum determines the development of a syndrome of systemic inflammation that mainly affects the kidneys and the skin.
According to the Brouet [4] classification, there are three types of cryoglobulinemias.
- Type I, or the simple form (10–15%), is characterized by the presence of a monoclonal Ig (IgM isotype) in most of cases. It is usually asymptomatic and is present within the lympho-plasmocitary proliferation (Waldenström’s macroglobulinemia, chronic lymphatic leukemia, multiple myeloma);
- Type II, or the mixed form (50–60%), is made up of a monoclonal IgM component that acts as a rheumatoid factor (RF) and as an antibody against a second component, a polyclonal IgG isotype component. Although the second type of cryoglobulinemia has been considered to be a self-existing pathology [5,6], recent studies indicate its association with HCV in a proportion of 40–100, according to the geographical area [7,8,9].
- Type III is also a mixed form, with immune complexes made up of two polyclonal Ig [10]. The diagnosis of the mixed cryoglobulinemia syndrome is based on serologic, pathologic, and clinical criteria.
Case Report
Patient A.A., 59 years old city dweller, was diagnosed in 2014 with HCV, after the performance of anti-HCV antibodies. In 2014, the patient underwent detailed investigations and renal biopsy due to the increase in liver disease symptomatology and the occurrence of systemic arterial hypertension, macroscopic hematuria, leg edemas, and Raynaud phenomena, being thus diagnosed with renal (chronic glomerulonephritis), cutaneous, and neurological cryoglobulinemic vasculitis. In 2015 she was administered a treatment with Interferon and Ribavirin for 12 months without a sustained virologic response. The patient had been diagnosed for several years with anemia by mixed and renal mechanism and iron-deficiency anaemia; for this she has been administered iron-based medicines and Neorecormon (therapeutically corrected).

Figure 1.
Livedo reticularis hyperpigmentary lesions at the level of the inferior extremities.
The physical examination revealed the following aspects: a moderate sclero-tegumentary pallor, with the presence of certain livedo reticularis hyperpigmentary lesions and of purpuric lesions around the bilateral leg surface, gums bleeding, sicca phenomena (xerostomia, xerophtalmia), respiratory apparatus under normal limits, arterial tension reaching 140/80 mmHg and the pulse amounting to 80 beats per minute, the abdomen sensitive to palpation in the right hypochondrium, the liver with increased consistency, macroscopic hematuria, acro-paresthesia.
The paraclinical investigation revealed the following: thrombocytes 120.000/mm3, erythrocyte sedimentation rate (ESR) 90 mm/1h, 130 mm/2h, serum urea 120 mg/dL, creatinine 3.6 mg/dL, eGFR 13 mL/min/1.73m2, proteinuria 800.0 mg/24h, the Addis test 2580 erythrocytes/min, aspartataminotranspherasis (ASAT) 70 U/L, alaninaminotranspherasis (ALAT) 59 U/L, alkaline phosphatase 67 U/L, gamma-glutamyl-transpeptidase (GGT) 162 U/L, total bilirubin 0.48 mg/dL, direct bilirubin 0.15 mg/dL, indirect bilirubin 0.33 mg/dL, cholesterol 170 mg/dL, total protein 6.4 g%, fibrinogen 458 mg/dL, C-reactive protein (CRP) 1.74 mg/L, complement factors such as C3 109.96 mg/dL (n: 90–180 mg/dL), IgA 183.96 mg/dL (n: 70–400 mg/dL), IgG 1631.6 mg/dL (n: 700–1600 mg/dL), IgM 246 mg/dL (n: 40–230 mg/dL); the electrophoresis of the seric proteins: total protein 6.4 g%, albumin/globulin 1.25, serum albumin 55.6%, alpha-1 globulin 2.2%, alpha-2 globulin 11.8%, beta-1 globulin 6.2%, beta-2 globulin 3.3%, gama globulin 20.9% with the tendency to the monoclonal band in the gama mobility area.
From the abdominal ultrasound we detected a liver with homogeneous echostructure, with several infracentimetric calcifications, hepatic left lobe reaching 6.5 cm, hepatic right lobe reaching 15.5 cm, the vena porta 8 mm, permeable, hepatopetal flow, both kidneys reduced in volume (9 cm), normal pancreas and spleen, normal values of the inferior vena cava, adenopathy reaching 1.1 cm, situated in the celiac trunk, with no peritoneal fluid.
Taking into account the long-term evolution of hepatic disease, a superior digestive endoscopy was carried out. The endoscopy revealed a stomach with diffuse hyperemia of the mucous membrane and several petechiae at the level of the gastric body and bulb with diffuse hyperemia and several petechiae, without any esophageal varicose veins, or portal hypertensive gastropathy.
For a better evaluation of the hepatic status, a real time sonoelastography (RTE) was carried out, that emphasized a tessellated structure with the predominance of the blue areas and a liver fibrosis index (LFI) of 2.18.
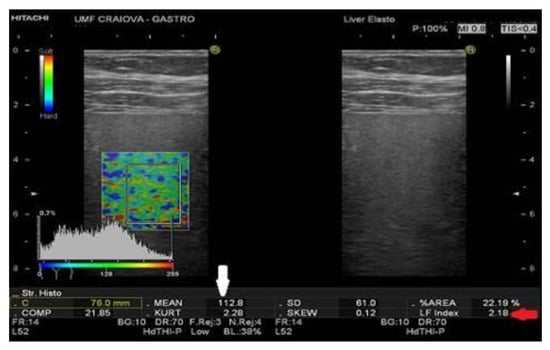
Figure 2.
RTE reveals the predominance of the blue areas and a LFI of 2.18.
Discussion
Cryoglobulinemia induces a systemic vasculitis that mainly affects the small blood vessels and, to a smaller extent the medium arteries and veins, through the gradual build-up of circulating immune complexes and the activation of the complement cascade [9]. It often coexists with the HCV infection, being cited as the main cause of type II mixed cryoglobulinemia [9]. Anti-HCV antibodies are present, together with an active viral replication, in most patients with mixed cryoglobulinemia, the cryoprecipitates containing monoclonal IgM, rheumatoid molecules that mainly act against the antigen-antibodies immune complexes [7,8,11,12].
Cryoglobulinemia manifests at the systemic level, affecting the skin, the kidneys, and the nervous system, with the severity of the disease varying case by case. Treatment can act either on the viral infection, resorting in this case to the therapy with interferon, or on the symptoms, when treatment is based on corticotherapy, immunosuppressors, or plasmapheresis [12].
The primary goal of treatment is HCV eradication, which is associated with improvement of clinical symptoms, especially in patients with mixed cryoglobulinemia [13,14,15,16]. In patients with severe symptoms of mixed cryoglobulinemia, treatment with rituximab may be considered [17]. Recent studies have also tested the combination of PEG-IFN/RBV and rituximab. The clinical response may be achieved faster and SVR is not diminished in patients who receive rituximab [18,19]. Triple therapy was effective in terms of virologic response as well as clinical response, but adverse events were frequent (>80% anemia, >50% infections) [20]. Since 2015, IFN-free therapies have been an option for this group of patients, but so far data are limited. Recent data show that the INF-free combination of SOF/RBV is highly effective in inducing clinical remission in patients with cryoglobulinemia vasculitis (78% after 24 weeks of treatment) in a cohort of 18 patients [21].
Clinical remission was achieved in 50–70% of patients receiving IFN α plus RBV and was correlated with a significant reduction of viral concentrations [22]. Despite successful antiviral treatment, cryoglobulinemic vasculitis may persist in a small collective [23]. Recent data have demonstrated that rituximab is an effective and safe treatment for advanced liver disease with mixed cryoglobulinemia [24]. Thus, the combination of rituximab with PEG-IFN α and ribavirin represents a therapeutic approach for patients with severe vasculitis from mixed cryoglobulinemia and resistant to antiviral therapy alone [25].
With its recent introduction, the new interferon-free treatment consists of direct acting antivirals (DAA), although the role of rituximab remains to be observed, as non-response is unusual. The efficacy and safety of treatment with sofosbuvir in HCV-induced MC have had an SVR12 rate of 83% and has been associated with eGFR improvement as well as a reduction in proteinuria [26].
Renal impairment has been observed as an adverse event associated with the use of telaprevir and boceprevir [27]. In patients with severe renal insufficiency (eGFR < 30 mL/min), data for the use of simeprevir, ledipasvir, sofosbuvir, and other direct acting antivirals are emerging. Although the use of sofosbuvir is currently not recommended in patients with eGFR <30 mL/min, safety and efficacy of full dose sofosbuvir regimen was recently demonstrated in this population [28].
The 3D regimen, comprising of paritaprevir/ritonavir/ombitasvir + dasabuvir as well as the NS5A inhibitor daclatasvir, has been safely administered in patients with severe renal insufficiency (GFR < 30 mL/min) due to the predominant biliary elimination of these drugs [29]. The combination of grazoprevir plus elbasvir, licensed in 2016, has shown a good safety profile in patients with serious renal impairment in a dedicated trial.
A particularity of this case was the large number of signs and symptoms indicating increased activity of the autoimmune disease. The prevalence of renal involvement in the second type of cryoglobulinemia is variable, from 10 to 60% [4,6,30,31], most often occurring between the 5th and 6th decades of life, with a moderate female predominance [32,33]. These parameters describe our case, as the patient was female and 59 years old. Although the renal and systemic manifestations may appear simultaneously, most often episodes of extra-renal symptomatology with spontaneous remission are present before the installation of the renal manifestations [6,32,33]. The case described herein belongs to the classical triad described by Meltzer and Franklin: fatigability, purpura, and polyarthralgias, as noted in about one third of the cases [30,34,35]. While establishing the diagnosis, we noted a moderate affectation of the nervous system, with faint acroparesthesias. Other manifestations such as pulmonary affectation or CNS issues are generally rare and were excluded in our case. A cardiovascular investigation was carried out, and although the cryoglobulinemic vasculitis can determine the development of pericarditis, valvular pathology, myocarditis, and congestive cardiac [6,32], only a primary arterial hypertension of the second degree was found, which was therapeutically controlled.
In our case, the patient is a C virus carrier, with active replication for several years, being subjected to several investigations for the evaluation of hepatic function. The prognosis of the hepatic disease is based on the degree of fibrosis, a proper, complete, and early evaluation being essential. Although the hepatic biopsy remains the “gold standard,” a series of noninvasive techniques concerned with the evaluation of the degree of fibrosis, including RTE, have recently been recently. This contemporary and noninvasive method enables evaluation of the differences of hardness between affected and healthy tissues, with applicability that varies from the differentiation of malign tumors from benign ones via the evaluation of the degree of elasticity specific to a tumoral tissue, up to the evaluation of the degree of hepatic fibrosis [36].
The close relation between the infection with HCV and the cryoglobulinemia is demonstrated after treatment with Interferon for 12 months in 2015 when an increase in the seric values of RF-IgM, viremy, and creatinine were noticed, with an amelioration of the renal function, reaching a eGFR of 13 mL/min/1.73m2 before the initiation of the treatment, a rate of 22 mL/min/1.73m2, at the end of the 12 months; the cutaneous symptomatology entered remission. The patient was, however, a non-responder to the therapy with interferon, which led to another remission at the end of the treatment, with the recurrence the vasculitic symptomatology and the increase in the values of the nitrogen retention.
The status of being a non-responder exposed the patient to both the progressive deterioration of the hepatic function, with the gradual installation of cirrhosis and its complications, and the development of a hepatocellular carcinoma, which led to the use of periodical RTE, as this technique can be applied in either case. By the LFI, the degree of hepatic fibrosis and potential tumorous formations can be determined.
Conclusions
This case study reveals the close connection between the infection with the HCV and the cryoglobulinemic vasculitis with cutaneous, renal, and neurologic injury, its particularity being represented by both the existence from the outset of the vasculitic disease of a large number of signs and symptoms specific to vasculitis, and the current predialitic stage of the patient, due to the deterioration of the renal function during the last years. This pattern is not characteristic of type II cryoglobulinemia, which in most cases does not progress towards dialysis, although the affected area is moderate since the establishment of the diagnosis [6,35,36].
Taking into account the failure of the therapy with interferon and the progressive accentuation of all the complications, close monitoring of the clinical and paraclinical state is necessary at periodic time intervals.
Acknowledgments
All authors participated equally in this work.
Conflicts of Interest
The authors report no conflict of interests regarding this study.
References
- Cacoub, P.; Renou, C.; Rosenthal, E.; Cohen, P.; Loury, I.; Loustaud-Ratti, V.; Yamamoto, A.M.; Camproux, A.C.; Hausfater, P.; Musset, L.; Veyssier, P.; Raguin, G.; Piette, J.C. Extrahepatic manifestations associated with hepatitis C virus infection. A prospective multicenter study of 321 patients. Groupe d’ Etude et de Recherche en Medicine Interne et Maladies Infectieuses sur le Virus de VHepatite C. Medicine 2000, 79, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Cacoub, P.; Poynard, T.; Ghillani, P.; Charlotte, F.; Olivi, M.; Piette, J.C.; Opolon, P. Extrahepatic manifestations of chronic hepatitis C. MULTIVIRC group. Multidepartment Virus C. Athritis Rheum. 1999, 42, 2204–2212. [Google Scholar] [CrossRef] [PubMed]
- Kallemuchikkal, U.; Gorevic, P.D. Evaluation of cryoglobulins. Arch Pathol Lab Med. 1999, 123, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Brouet, J.C.; Clauvel, J.P.; Danon, F.; Klein, M.; Seligmann, M. Biologic and clinical significance of cryoglobulins. A report of 86 cases. Am J Med. 1974, 57, 775–788. [Google Scholar] [PubMed]
- Cordonnier, D.; Martin, H.; Groslambert, P.; Micouin, C.; Chenais, F.; Stoebner, P. Mixed IgG-IgM cryoglobulinemia with glomerulo-nephritis. Immunochemical, fluorescent and ultrastructural study of kidney and in vitro cryoprecipitate. Am J Med. 1975, 59, 867–872. [Google Scholar] [PubMed]
- Cordonnier, D.; Vialtel, P.; Renversez, J.C.; Chenais, F.; Favre, M.; Tournoud, A.; Barioz, C.; Bayle, F.; Dechelette, E.; Denis, M.C.; Couderc, P. Renal diseases in 18 patients with mixed type II IgM-IgG cryoglobulinemia: Monoclonal lymphoid infiltration (2 cases) and membrano-proliferative glomerulonephritis (14 cases). Adv Nephrol Necker Hosp. 1983, 12, 177–204. [Google Scholar] [PubMed]
- Agnello, V.; Chung, R.T.; Kaplan, L.M. A role for hepatitis C virus infection in type II cryglobulinemia. N Engl J Med. 1992, 327, 1490–1495. [Google Scholar] [CrossRef] [PubMed]
- Misiani, R.; Bellavita, P.; Fenili, D.; Borelli, G.; Marchesi, D.; Massaza, M.; Vendramin, G.; Commoti, B.; Tanzi, E.; Scudellr, G.; et al. Hepatitis C virus infection in patients with essential mixed cryoglobulinemia. Ann Intern Med. 1992, 117, 573–577. [Google Scholar] [PubMed]
- Sansonno, D.; Dammacco, F. Hepatitis C virus, cryoglobulinaemia, and vasculitis: Immune complex relations. Lanced Infect Dis. 2005, 5, 227–236. [Google Scholar] [CrossRef] [PubMed]
- De Re, V.; Pavan, A.; Sansonno, S.; Sansonno, D.; Racanelli, V. Clonal CD27+ CD19+ B cell expansion through inhibition of FC gammaIIR in HCV(+) cryoglobulinemic patients. Ann N Y Acad Sci. 2009, 1173, 326–333. [Google Scholar] [CrossRef] [PubMed]
- Justin Burbano, C.; Rojas, M.; Vásquez, G.; Castaño, D. Microparticles That Form Immune Complexes as Modulatory Structures in Autoimmune Responses. Mediators Inflamm. 2015, 2015, 267590. [Google Scholar] [CrossRef] [PubMed]
- Sadoun, D.; Resche-Rigon, M.; Thibault, V.; Piette, J.C.; Cacoub, P. Antiviral therapy for hepatitis C virus-associated mixed cryoglobulinemia vasculitis: A long term followup study. Arthritis Rheum. 2006, 54, 3696–3706. [Google Scholar] [CrossRef] [PubMed]
- Cresta, P.; Musset, L.; Cacoub, P.; Frangeul, L.; Vitour, D.; Poynard, T.; Opolon, P.; Nguyen, D.T.; Golliot, F.; Piette, J.C.; Huraux, J.M.; Lunel, F. Response to interferon alpha treatment and disappearance of cryoglobulinaemia in patients infected by hepatitis C virus. Gut. 1999, 45, 122–128. [Google Scholar] [CrossRef] [PubMed]
- Pischke, S.; Schott, P.; Hartmann, H.; Ramadori, G. Hepatitis C virus-associated mixed cryoglo-bulinemia. Clinical manifestations, histopathological changes, mechanisms of cryoprecipitation and options of treatment. Histol Histopathol. 2001, 16, 1275–1285. [Google Scholar] [PubMed]
- Zignego, A.L.; Ferri, C.; Pileri, S.A.; Caini, P.; Bianchi, F.B. Italian Association of the Study of Liver Commission on Extrahepatic Manifestations of HCV infection. Extrahepatic manifestations of Hepatitis C Virus infection: A general overview and guidelines for a clinical approach. Dig Liver Dis. 2007, 39, 2–17. [Google Scholar] [CrossRef] [PubMed]
- Maasoumy Sollima, S.; Milazzo, L.; Antinori, S.; Galli, M. Direct-Acting Antivirals and Mixed Cryoglobulinemia Vasculitis: Long-Term Outcome of Patients Achieving HCV Eradication. Am J Gastroenterol. 2017, 112, 1753–1754. [Google Scholar] [CrossRef] [PubMed]
- Cacoub, P.; Delluc, A.; Saadoun, D.; Landau, D.A.; Sene, D. Anti-CD20 monoclonal antibody (rituximab) treatment for cryoglobulinemic vasculitis where do we stand? Ann Rheum Dis. 2008, 67, 283–287. [Google Scholar] [CrossRef] [PubMed]
- Dammacco, F.; Tucci, F.A.; Lauletta, G.; Gatti, P.; De Re, V.; Conteduca, V.; Sansonno, S.; Russi, S.; Mariggiò, M.A.; Chironna, M.; Sansonno, D. Pegylated interferon-alpha, ribavirin, and rituximab combined therapy of hepatitis C virus-related mixed cryoglobulinemia: A long-term study. Blood 2010, 116, 343–353. [Google Scholar] [CrossRef] [PubMed]
- Saadoun, D.; Resche Rigon, M.; Sene, D.; Terrier, B.; Karras, A.; Perard, L.; Schoindre, Y.; Coppéré, B.; Blanc, F.; Musset, L.; Piette, J.C.; Rosenzwajg, M.; Cacoub, P. Rituximab plus Peg-interferon-alpha/ribavirin compared with Peg-interferon-alpha/ribavirin in hepatitis C-related mixed cryoglobulinemia. Blood 2010, 116, 326–334. [Google Scholar] [CrossRef] [PubMed]
- Saadoun, D.; Thibault, V.; Pialoux, G.; Elkrief, L.; Mallet, M.; Musset, L.; Bazin Kara, D.; Cazorla, C.; Pol, S.; Cacoub, P. All oral therapy (Sofosbuvir-Ribavirin) combination in severe HCV-mixed cryoglobulinemia vasculitis, the vascuvaldic study. J Hepatol. 2015, 62, S640. [Google Scholar] [CrossRef]
- Saadoun, D.; Resche Rigon, M.; Pol, S.; Thibault, V.; Blanc, F.; Pialoux, G.; Karras, A.; Bazin-Kara, D.; Cazorla, C.; Vittecoq, D.; Musset, L.; Peltier, J.; Decaux, O.; Ziza, J.M.; Lambotte, O.; Cacoub, P. PegIFN/ribavirin/protease inhibitor combination in severe hepatitis C virus-associated mixed cryoglobulinemia vasculitis. J Hepatol. 2015, 62, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Calleja, J.L.; Albillos, A.; Moreno-Otero, R.; Rossi, I.; Cacho, G.; Domper, F.; Yebra, M.; Escartín, P. Sustained response to interferon-alpha or to interferon-alpha plus ribavirin in hepatitis C virus-associated symptomatic mixed cryoglobulinaemia. Aliment Pharmacol Ther. 1999, 13, 1179–1186. [Google Scholar] [CrossRef] [PubMed]
- Levine, J.W.; Gota, C.; Fessier, B.J.; Calabrese, L.H.; Cooper, S.M. Persistent cryoglobulinemie vasculitis following successful treatment of hepatitis C virus. J Rheumatol. 2005, 32, 1164–1167. [Google Scholar] [PubMed]
- Petrarca, A.; Rigacci, L.; Caini, P.; Colagrande, S.; Romagnoli, P.; Vizzutti, F.; Arena, U.; Giannini, C.; Monti, M.; Montalto, P.; Matucci-Cerinic, M.; Bosi, A.; Laffi, G.; Zignego, A.L. Safety and efficacy of rituximab in patients with hepatitis C virus-related mixed cryoglobulinemia and severe liver disease. Blood 2010, 116, 335–342. [Google Scholar] [CrossRef] [PubMed]
- Saadoun, D.; Resche-Rigon, M.; Sene, D.; Perard, L.; Piette, J.C.; Cacoub, P. Rituximab combined with Peg-Interferon-Ribavirin in refractory HCV-associated cryoglobulinemia vasculitis. Ann Rheum Dis. 2008, 67, 1431–1436. [Google Scholar] [CrossRef] [PubMed]
- Sise, M.E.; Bloom, A.K.; Wisocky, J.; Lin, M.V.; Gustafson, J.L.; Lundquist, A.L.; Steele, D.; Thiim, M.; Williams, W.W.; Hashemi, N.; Kim, A.Y.; Thadhani, R.; Chung, R.T. Treatment of Hepatitis C Virus-Associated Mixed Cryoglobulinemia with Direct-Acting Antiviral Agents. Hepatology 2016, 63, 408–417. [Google Scholar] [CrossRef] [PubMed]
- Loustaud-Ratti, V.; Carrier, P.; Vong, C.; Essig, M. Renal impairment is frequent in chronic hepatitis C patients under triple therapy with telaprevir or boceprevir. Hepatology 2014, 59, 2426. [Google Scholar] [CrossRef]
- Hundemer, G.L.; Sise, M.E.; Wisocky, J.; Ufere, N.; Friedman, L.S.; Corey, K.E.; Chung, R.T. Use of sofosbuvir-based direct-acting antiviral therapy for hepatitis C viral infection in patient; with severe renal insufficiency. Infect Dis (Lond). 2015, 47, 924–929. [Google Scholar] [CrossRef] [PubMed]
- Fabrizi, F.; Messa, P. Therapy of hepatitis C by direct-acting anti-virals: The end of HCV in dialysis population? Expert Rev Clin Pharmacol. 2015, 8, 785–793. [Google Scholar] [CrossRef] [PubMed]
- Monti, G.; Saccardo, F.; Pioltelli, P.; Rinaldi, G. The natural history of cryoglobulinemia: Symptoms at onset and during follow-up. A report by the Italian Group for the Study of Cryoglobulinemias (GISC). Clin Exp Rheumatol. 1995, 13, S129–33. [Google Scholar] [PubMed]
- Bryce, A.H.; Kile, R.A.; Dispenzieri, A.; Gertz, M.A. Natural history and therapy of 66 patients with mixed cryoglobulinemia. Am J Hematol. 2006, 81, 511–518. [Google Scholar] [CrossRef] [PubMed]
- Tarantino, A.; Campise, M.; Banfi, G.; Confalonieri, R.; Bucci, A.; Montoli, A.; Colasanti, G.; Damilano, I.; D’Amico, G.; Minetti, L.; et al. Long-term predictors of survival in essential mixed cryoglobulinemic glomerulonephritis. Kidney Int. 1995, 47, 618–623. [Google Scholar] [PubMed]
- D’Amico, G. Renal involvement in hepatitis C infection: Cryoglobulinemic glomerulo nephritis. Kidney Int. 1998, 54, 650–671. [Google Scholar] [CrossRef] [PubMed]
- Iovănescu, V.F.; Constantinescu, A.F.; Streba, C.T.; Zaharie, S.I.; Vere, C.C.; Mandache, E.; Penescu, M.N.; Mota, E. Clinical and pathological considerations on renal diseases in patients with chronic viral hepatitis. Rom J Morphol Embryol. 2016, 57, 401–406. [Google Scholar] [PubMed]
- Meltzer, M.; Franklin, E.C. Cryoglobulinemia-a study of twenty-nine patients. IgG and IgM cryoglobulins and factors affecting cryoprecibitability. Am J Med. 1996, 40, 828–836. [Google Scholar] [PubMed]
- Sandulescu, L.; Padureanu, V.; Dumitrescu, C.; Braia, N.; Streba, C.T.; Gheonea, D.I.; Cazacu, S.; Ciurea, T.; Rogoveanu, I.; Saftoiu, A. A pilot study of real time elastography in the differentiation of focal liver lesions. Curr Health Sci J. 2012, 38, 32–35. [Google Scholar] [PubMed]
© 2018 by the author. 2018 Daniel C. Caragea, Larisa Săndulescu, Vlad Pădureanu, Mircea C. Forțofoiu, Costin Streba, Lidia Boldeanu, Mihail V. Boldeanu, Mircea Popescu-Drigă, Marius E. Ciurea, Maria Forțofoiu, Ion Rogoveanu, Tudorel Ciurea and Cristin C. Vere.