Etiology of Coronary Reintervention After Coronary Artery Bypass Surgery
Abstract
1. Introduction
2. Materials and Methods
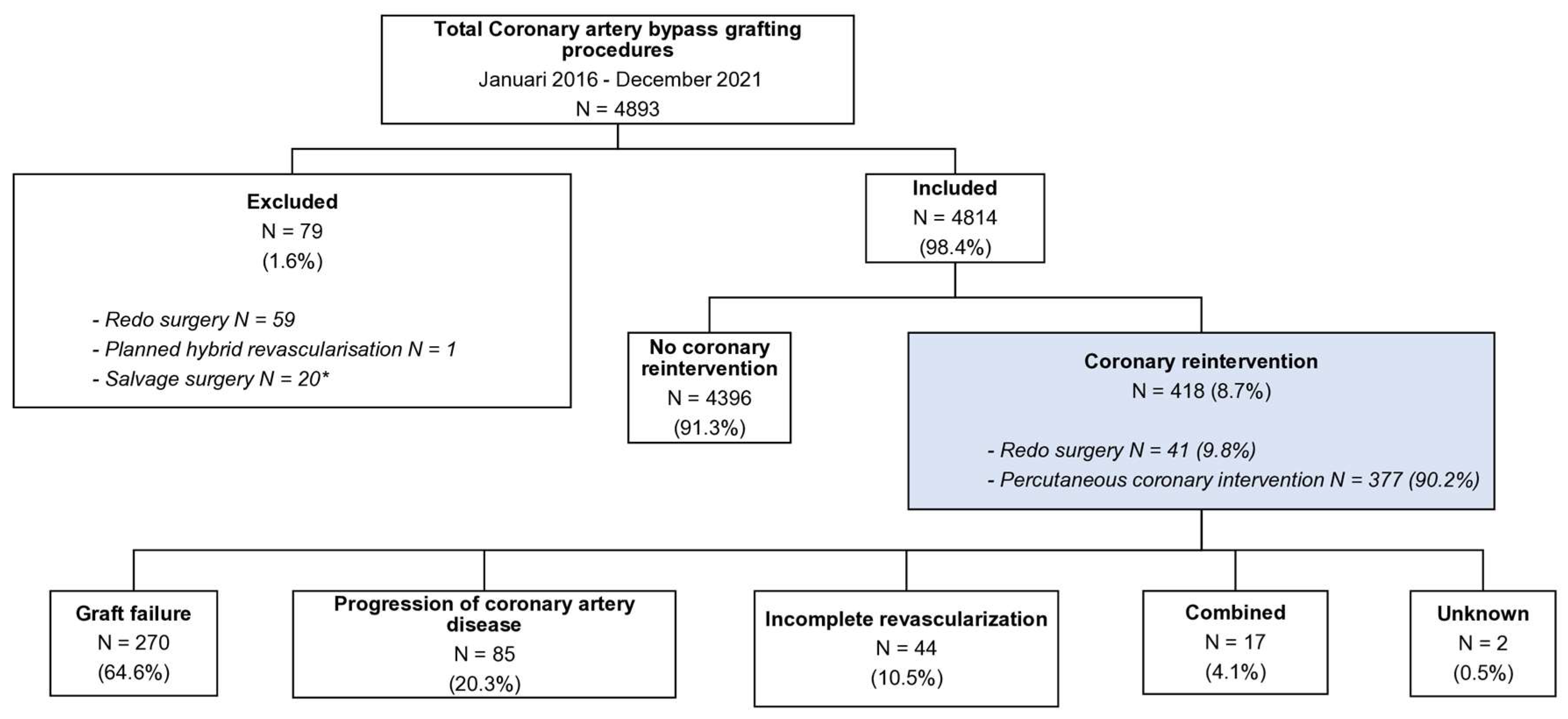
2.1. Patient Inclusion
2.2. Data Collection and Parameters
2.3. Endpoints Definitions
2.4. Identification of Etiology for Reintervention
2.5. Statistical Analysis
3. Results
3.1. Patient Demographics
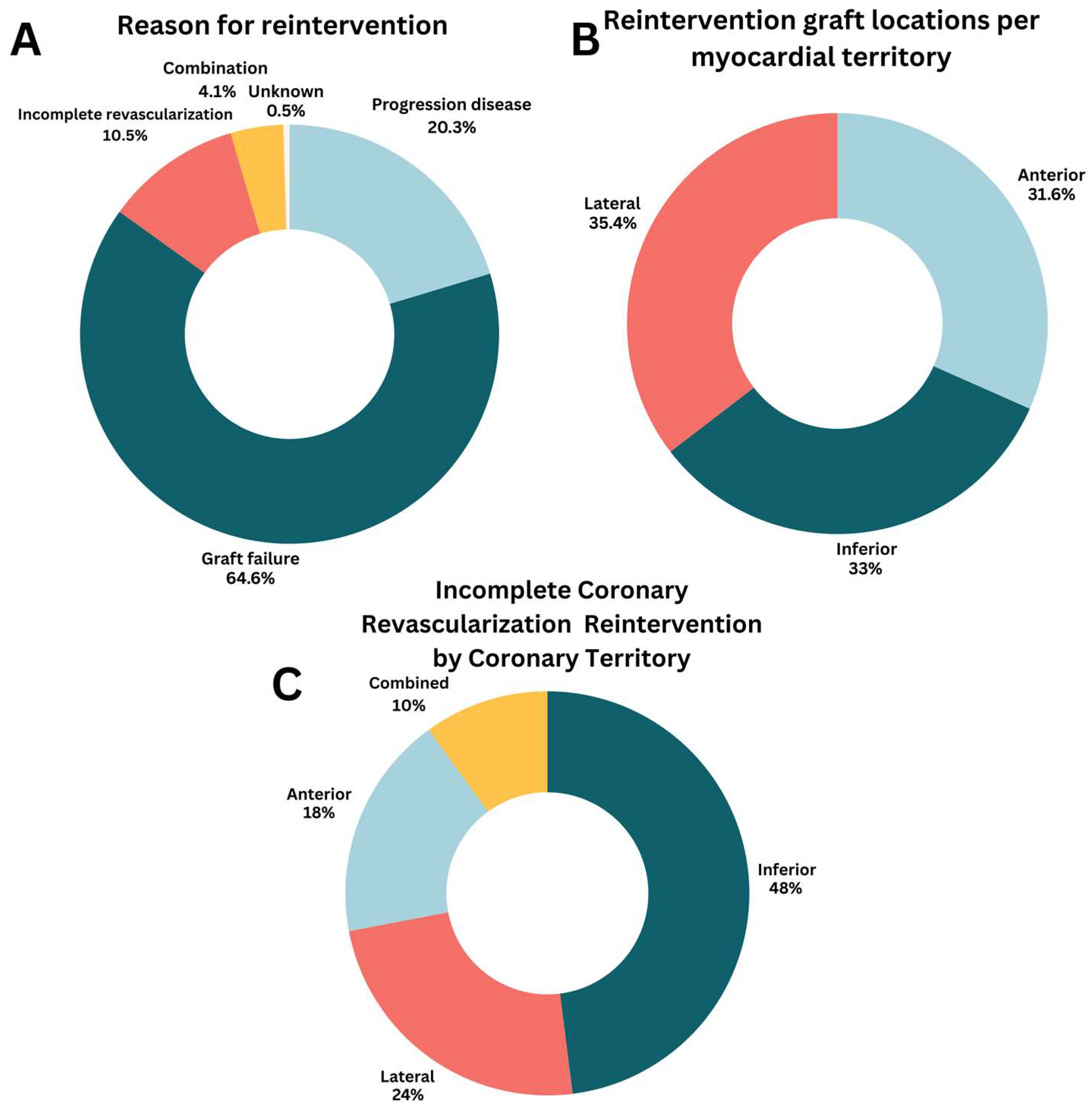
3.2. Coronary Reintervention
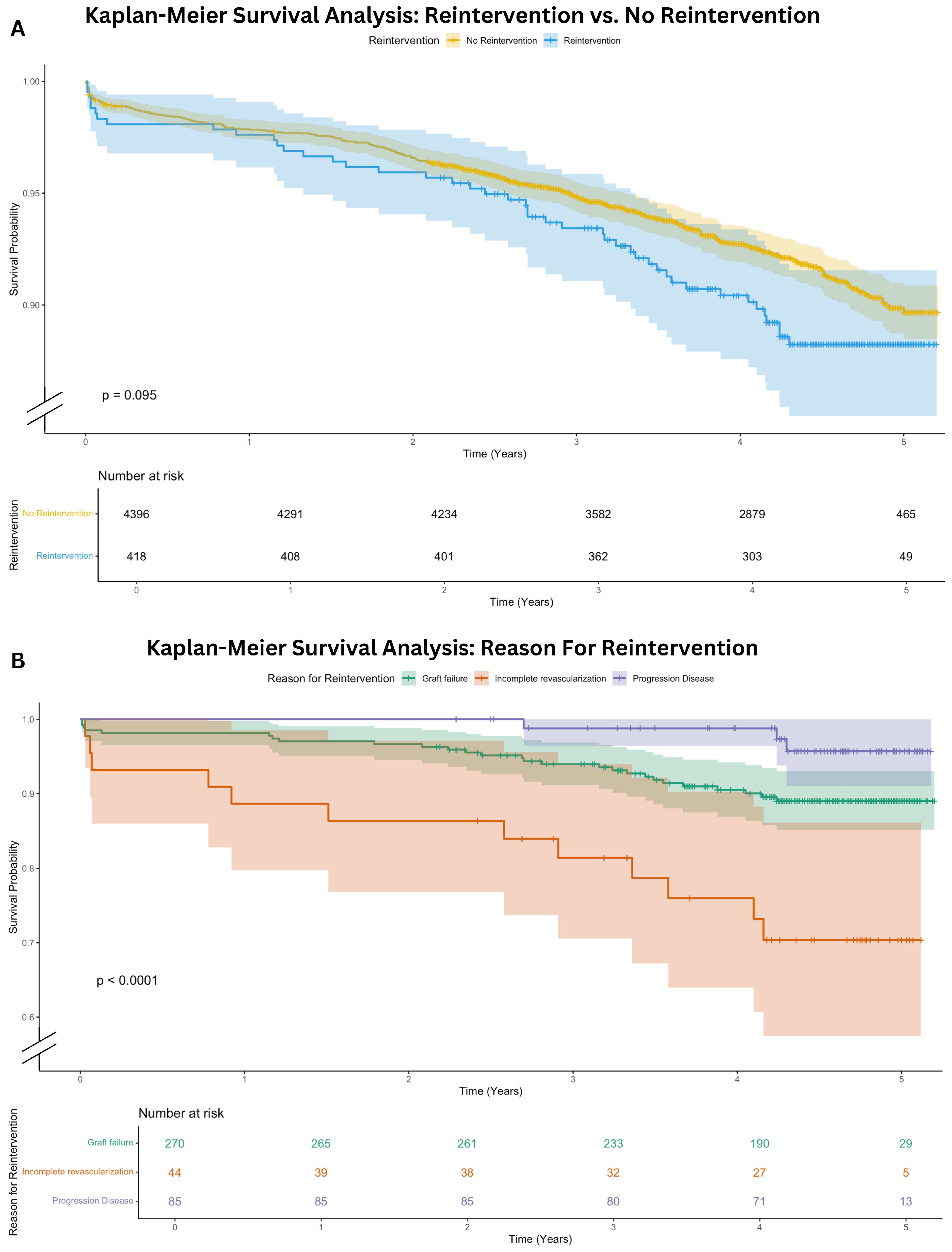
3.3. Overall Mortality
3.4. Regression Analysis
4. Discussion
4.1. Reason for Reintervention
4.2. Predictors for Coronary Reintervention
4.3. Effect of Reintervention on Mortality
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ACS | Acute coronary syndrome |
| ACE | Angiotensin Converting Enzyme |
| ARB | Angiotensin Receptor Blocker |
| CAD | Coronary artery disease |
| CABG | Coronary artery bypass grafting |
| CAG | Coronary angiogram |
| CCS | Canadian Cardiovascular Society |
| CVA | Cerebrovascular accident |
| DOAC | Direct Oral Anticoagulants |
| ECC | Extracorporeal circulation |
| Endo-CAB | Endoscopic Coronary Artery Bypass |
| ICU | Intensive Care Unit |
| IQR | Interquartile range |
| LIMA | Left internal mammary artery |
| LVEF | Left ventricle ejection fraction |
| NHR | Netherlands Heart Registration |
| NYHA | New York Heart Association |
| PCI | Percutaneous coronary intervention |
| PSCK9 | Proprotein Convertase Subtilisin/Kexin type 9 |
| RIMA | Right internal mammary artery |
| SD | Standard deviation |
| SMD | Standard mean differences |
| SVG | Saphenous vein graft |
| TVR | Target vessel revascularization |
References
- Serruys, P.W.; Morice, M.-C.; Kappetein, A.P.; Colombo, A.; Holmes, D.R.; Mack, M.J.; Ståhle, E.; Feldman, T.E.; Van Den Brand, M.; Bass, E.J.; et al. Percutaneous Coronary Intervention versus Coronary-Artery Bypass Grafting for Severe Coronary Artery Disease. N. Engl. J. Med. 2009, 360, 961–972. [Google Scholar] [CrossRef]
- Parasca, C.A.; Head, S.J.; Milojevic, M.; Mack, M.J.; Serruys, P.W.; Morice, M.C.; Mohr, F.W.; Feldman, T.E.; Colombo, A.; Dawkins, K.D.; et al. Incidence, Characteristics, Predictors, and Outcomes of Repeat Revascularization After Percutaneous Coronary Intervention and Coronary Artery Bypass Grafting: The SYNTAX Trial at 5 Years. JACC Cardiovasc. Interv. 2016, 9, 2493–2507. [Google Scholar] [CrossRef] [PubMed]
- Mohr, F.W.; Morice, M.-C.; Kappetein, A.P.; E Feldman, T.; Ståhle, E.; Colombo, A.; Mack, M.J.; Holmes, D.R.; Morel, M.-A.; Van Dyck, N.; et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet 2013, 381, 629–638. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-J.; Ahn, J.-M.; Kim, Y.-H.; Park, D.-W.; Yun, S.-C.; Lee, J.-Y.; Kang, S.-J.; Lee, S.-W.; Lee, C.W.; Park, S.-W.; et al. Trial of Everolimus-Eluting Stents or Bypass Surgery for Coronary Disease. N. Engl. J. Med. 2015, 372, 1204–1212. [Google Scholar] [CrossRef] [PubMed]
- Inci, S.; Arslan, S.; Bakirci, E.M.; Tas, M.H.; Gundogdu, F.; Karakelleoglu, S. Predictors of reintervention after coronary artery bypass grafting. Eur. Rev. Med. Pharmacol. Sci. 2014, 18, 66–70. [Google Scholar] [PubMed]
- NHR. Nederlandse Hart Registratie. Available online: https://nhr.nl/ (accessed on 6 November 2024).
- Davidson, L.J.; Cleveland, J.C.; Welt, F.G.; Anwaruddin, S.; Bonow, R.O.; Firstenberg, M.S.; Gaudino, M.F.; Gersh, B.J.; Grubb, K.J.; Kirtane, A.J.; et al. A Practical Approach to Left Main Coronary Artery Disease. JACC 2022, 80, 2119–2134. [Google Scholar] [CrossRef]
- Vrints, C.; Andreotti, F.; Koskinas, K.C.; Rossello, X.; Adamo, M.; Ainslie, J.; Banning, A.P.; Budaj, A.; Buechel, R.R.; Chiariello, G.A.; et al. 2024 ESC Guidelines for the management of chronic coronary syndromes. Eur. Heart J. 2024, 45, 3415–3537. [Google Scholar] [CrossRef]
- A Byrne, R.; Rossello, X.; Coughlan, J.J.; Barbato, E.; Berry, C.; Chieffo, A.; Claeys, M.J.; Dan, G.-A.; Dweck, M.R.; Galbraith, M.; et al. 2023 ESC Guidelines for the management of acute coronary syndromes: Developed by the task force on the management of acute coronary syndromes of the European Society of Cardiology (ESC). Eur. Heart J. 2023, 44, 3720–3826. [Google Scholar] [CrossRef]
- Fitzgibbon, G.M.; Kafka, H.P.; Leach, A.J.; Keon, W.J.; Hooper, G.D.; Burton, J.R. Coronary bypass graft fate and patient outcome: Angiographic follow-up of 5065 grafts related to survival and reoperation in 1388 patients during 25 years. J. Am. Coll. Cardiol. 1996, 28, 616–626. [Google Scholar] [CrossRef]
- Faisaluddin, M.; Sattar, Y.; Manasrah, N.; Patel, N.; Taha, A.; Takla, A.; Ahmed, A.; Osama, M.; Titus, A.; Hamza, M.; et al. Cardiovascular Outcomes of Redo-coronary Artery Bypass Graft Versus Percutaneous Coronary Intervention of Index Bypass Grafts Among Acute Coronary Syndrome: Regression Matched National Cohort Study. Curr. Probl. Cardiol. 2023, 48, 101580. [Google Scholar] [CrossRef]
- Alboom, M.; Browne, A.; Sheth, T.; Zheng, Z.; Dagenais, F.; Noiseux, N.; Brtko, M.; Stevens, L.-M.; Lee, S.F.; Copland, I.; et al. Conduit selection and early graft failure in coronary artery bypass surgery: A post hoc analysis of the Cardiovascular Outcomes for People Using Anticoagulation Strategies (COMPASS) coronary artery bypass grafting study. J. Thorac. Cardiovasc. Surg. 2023, 165, 1080–1089.e1. [Google Scholar] [CrossRef]
- Ranney, D.N.; Williams, J.B.; Mulder, H.; Wojdyla, D.; Cox, M.L.; Gibson, C.M.; Mack, M.J.; Daneshmand, M.A.; Alexander, J.H.; Lopes, R.D. Comparison of Outcomes and Frequency of Graft Failure with Use of Free Versus In Situ Internal Mammary Artery Bypass Conduits (from the PREVENT IV Trial). Am. J. Cardiol. 2019, 123, 571–575. [Google Scholar] [CrossRef] [PubMed]
- Willemsen, L.M.; Janssen, P.W.; Hackeng, C.M.; Kelder, J.C.; Tijssen, J.G.; van Straten, A.H.; Soliman-Hamad, M.A.; Deneer, V.H.; Daeter, E.J.; Sonker, U.; et al. A randomized, double-blind, placebo-controlled trial investigating the effect of ticagrelor on saphenous vein graft patency in patients undergoing coronary artery bypass grafting surgery-Rationale and design of the POPular CABG trial. Am. Heart J. 2020, 220, 237–245. [Google Scholar] [CrossRef]
- Tatoulis, J.; Buxton, B.F.; Fuller, J.A. Patencies of 2127 arterial to coronary conduits over 15 years. Ann. Thorac. Surg. 2004, 77, 93–101. [Google Scholar] [CrossRef]
- Borges, J.C.; Lopes, N.; Soares, P.R.; Góis, A.F.T.; Stolf, N.A.; Oliveira, S.A.; Hueb, W.A.; Ramires, J.A.F. Five-year follow-up of angiographic disease progression after medicine, angioplasty, or surgery. J. Cardiothorac. Surg. 2010, 5, 91. [Google Scholar] [CrossRef] [PubMed]
- Jabagi, H.; Chong, A.Y.; So, D.; Glineur, D.; Rubens, F.D. Native Coronary Disease Progression Post Coronary Artery Bypass Grafting. Cardiovasc. Revascularization Med. 2020, 21, 295–302. [Google Scholar] [CrossRef]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.-M.; Capodanno, D.; et al. ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2021, 42, 3227–3337, Erratum in: Eur Heart J. 2022, 43, 4468. https://doi.org/10.1093/eurheartj/ehac458.. [Google Scholar] [CrossRef]
- Sabik, J.F.; Mehaffey, J.H.; Badhwar, V.; Ruel, M.; Myers, P.O.; Sandner, S.; Bakaeen, F.; Puskas, J.; Taggart, D.; Schwann, T.; et al. Multiarterial vs Single-Arterial Coronary Surgery: 10-Year Follow-up of 1 Million Patients. Ann. Thorac. Surg. 2024, 117, 780–788. [Google Scholar] [CrossRef]
- Tatoulis, J.; Buxton, B.F.; Fuller, J.A.; Meswani, M.; Theodore, S.; Powar, N.; Wynne, R. Long-term patency of 1108 radial arterial-coronary angiograms over 10 years. Ann. Thorac. Surg. 2009, 88, 23–29; discussion 29–30. [Google Scholar] [CrossRef]
- Tatoulis, J.; Buxton, B.F.; Fuller, J.A. The right internal thoracic artery: The forgotten conduit—5766 patients and 991 angiograms. Ann. Thorac. Surg. 2011, 92, 9–15; discussion 15–17. [Google Scholar] [CrossRef]
- Hayward, P.A.; Gordon, I.R.; Hare, D.L.; Matalanis, G.; Horrigan, M.L.; Rosalion, A.; Buxton, B.F. Comparable patencies of the radial artery and right internal thoracic artery or saphenous vein beyond 5 years: Results from the Radial Artery Patency and Clinical Outcomes trial. J. Thorac. Cardiovasc. Surg. 2010, 139, 60–67. [Google Scholar] [CrossRef]
- Gaudino, M.; Benedetto, U.; Fremes, S.E.; Hare, D.L.; Hayward, P.; Moat, N.; Moscarelli, M.; Di Franco, A.; Nasso, G.; Peric, M.; et al. Effect of Calcium-Channel Blocker Therapy on Radial Artery Grafts After Coronary Bypass Surgery. JACC 2019, 73, 2299–2306. [Google Scholar] [CrossRef]
- Beckman, J.A.; Creager, M.A.; Libby, P. Diabetes and AtherosclerosisEpidemiology, Pathophysiology, and Management. JAMA 2002, 287, 2570–2581. [Google Scholar] [CrossRef]
- Gaudino, M.; Di Franco, A.; Alexander, J.H.; Bakaeen, F.; Egorova, N.; Kurlansky, P.; Boening, A.; Chikwe, J.; Demetres, M.; Devereaux, P.J.; et al. Sex differences in outcomes after coronary artery bypass grafting: A pooled analysis of individual patient data. Eur. Heart J. 2021, 43, 18–28. [Google Scholar] [CrossRef]
- Kao, K.D.; Lee, S.Y.K.C.; Liu, C.Y.; Chou, N.K. Risk factors associated with longer stays in cardiovascular surgical intensive care unit after CABG. J. Formos. Med. Assoc. 2022, 121, 304–313. [Google Scholar] [CrossRef]
- Gunnarsdottir, E.L.T.; Gunnarsdottir, S.L.X.; Heimisdottir, A.A.; Heidarsdottir, S.R.; Helgadottir, S.; Gudbjartsson, T.; Sigurdsson, M.I. Incidence and predictors of prolonged intensive care unit stay after coronary artery bypass in Iceland. Laeknabladid 2020, 106, 123–129. [Google Scholar]
- Puskas, J.D.; Williams, W.H.; O’DOnnell, R.; Patterson, R.E.; Sigman, S.R.; Smith, A.S.; Baio, K.T.; Kilgo, P.D.; Guyton, R.A. Off-pump and on-pump coronary artery bypass grafting are associated with similar graft patency, myocardial ischemia, and freedom from reintervention: Long-term follow-up of a randomized trial. Ann. Thorac. Surg. 2011, 91, 1836–1842; discussion 1842–1843. [Google Scholar] [CrossRef]
- Raja, S.G.; Garg, S.; Rochon, M.; Daley, S.; Robertis, F.D.; Bahrami, T. Short-term clinical outcomes and long-term survival of minimally invasive direct coronary artery bypass grafting. Ann. Cardiothorac. Surg. 2018, 7, 62127–62627. [Google Scholar] [CrossRef] [PubMed]
- Kirmani, B.H.; Holmes, M.V.; Muir, A.D. Long-Term Survival and Freedom From Reintervention After Off-Pump Coronary Artery Bypass Grafting: A Propensity-Matched Study. Circulation 2016, 134, 1209–1220. [Google Scholar] [CrossRef] [PubMed]
- Lamy, A.; Devereaux, P.; Prabhakaran, D.; Taggart, D.P.; Hu, S.; Paolasso, E.; Straka, Z.; Piegas, L.S.; Akar, A.R.; Jain, A.R.; et al. Effects of Off-Pump and On-Pump Coronary-Artery Bypass Grafting at 1 Year. N. Engl. J. Med. 2013, 368, 1179–1188. [Google Scholar] [CrossRef] [PubMed]
- Zhao, D.F.; Edelman, J.J.; Seco, M.; Bannon, P.G.; Wilson, M.K.; Byrom, M.J.; Thourani, V.; Lamy, A.; Taggart, D.P.; Puskas, J.D.; et al. Coronary Artery Bypass Grafting with and Without Manipulation of the Ascending Aorta. JACC 2017, 69, 924–936. [Google Scholar] [CrossRef]
- Park, D.-W.; Yun, S.-C.; Lee, S.-W.; Kim, Y.-H.; Lee, C.W.; Hong, M.-K.; Kim, J.-J.; Choo, S.J.; Song, H.; Chung, C.H.; et al. Long-Term Mortality After Percutaneous Coronary Intervention with Drug-Eluting Stent Implantation Versus Coronary Artery Bypass Surgery for the Treatment of Multivessel Coronary Artery Disease. Circulation 2008, 117, 2079–2086. [Google Scholar] [CrossRef] [PubMed]
- Head, S.J.; Milojevic, M.; Daemen, J.; Ahn, J.-M.; Boersma, E.; Christiansen, E.H.; Domanski, M.J.; E Farkouh, M.; Flather, M.; Fuster, V.; et al. Mortality after coronary artery bypass grafting versus percutaneous coronary intervention with stenting for coronary artery disease: A pooled analysis of individual patient data. Lancet 2018, 391, 939–948. [Google Scholar] [CrossRef] [PubMed]
- Giustino, G.; Serruys, P.W.; Sabik, J.F.; Mehran, R.; Maehara, A.; Puskas, J.D.; Simonton, C.A.; Lembo, N.J.; Kandzari, D.E.; Morice, M.-C.; et al. Mortality After Repeat Revascularization Following PCI or CABG for Left Main Disease: The EXCEL Trial. JACC Cardiovasc. Interv. 2020, 13, 375–387. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Lunardi, M.; Hara, H.; Gao, C.; Ono, M.; Davierwala, P.M.; Holmes, D.R.; Mohr, F.W.; Curzen, N.; Burzotta, F.; et al. Impact of repeat revascularization within 5 years on 10-year mortality after percutaneous or surgical revascularization. Clin. Res. Cardiol. 2023, 112, 1302–1311. [Google Scholar] [CrossRef]
| Overall (N = 4814) | No Reintervention (N = 4396) | Reintervention (N = 418) | p-Value | |
|---|---|---|---|---|
| Sex (men) | 3961 (82.3) | 3641 (82.3) | 320 (76.6) | 0.002 |
| Age (year) | 66.5 ± 9.2 | 66.5 ± 9.2 | 65.7 ± 9.3 | 0.097 |
| Height (cm) | 173.2 ± 14.0 | 173.2 ± 14.5 | 173.4 ± 9.3 | 0.508 |
| Weight (kg) | 83.2 ± 15.1 | 83.1 ± 13.9 | 83.5 ± 13.9 | 0.601 |
| Diabetes | 0.715 | |||
| Diabetes no treatment | 22 (0.5) | 19 (0.4) | 3 (0.7) | |
| Diabetes diet | 75 (1.6) | 68 (1.5) | 7 (1.7) | |
| Diabetes oral medication | 592 (12.3) | 540 (12.3) | 52 (12.4) | |
| Diabetes insulin | 489 (10.2) | 438 (10.0) | 51 (12.2) | |
| Peripheral vascular disease | 659 (13.7) | 583 (13.3) | 76 (18.2) | 0.019 |
| Atrial fibrillation | 0.796 | |||
| Paroxysmal atrial fibrillation | 287 (93.6) | 264 (6.0) | 23 (5.5) | |
| Non-paroxysmal atrial fibrillation | 15 (0.3) | 14 (0.3) | 1 (0.2) | |
| Unstable angina | 281 (5.8) | 252 (5.7) | 29 (6.9) | 0.374 |
| Recent myocardial infarction | 1901 (39.5) | 1756 (39.9) | 145 (34.7) | <0.001 |
| Prior percutaneous coronary intervention | 1325 (27.5) | 1183 (26.9) | 142 (34.0) | 0.002 |
| Left ventricular function | 0.193 | |||
| Good (<50%) | 3694 (76.7) | 3356 (76.3) | 338 (80.7) | |
| Moderate (31–50%) | 960 (19.9) | 888 (20.2) | 72 (17.2) | |
| Poor (21–30%) | 122 (2.5) | 116 (2.6) | 6 (1.4) | |
| Very poor (<20%) | 25 (0.5) | 24 (0.5) | 1 (0.2) | |
| Chronic lung disease | 334 (6.9) | 310 (7.1) | 24 (5.7) | 0.573 |
| Pulmonary Hypertension | 55 (1.2) | 50 (1.1) | 5 (1.2) | 0.978 |
| Poor mobility | 99 (2.1) | 91 (2.1) | 8 (1.9) | 0.888 |
| Neurological dysfunction | 113 (2.3) | 102 (2.3) | 11 (2.6) | 0.817 |
| Previous cerebral vascular accident | 233 (4.8) | 212 (4.8) | 21 (5.0) | 0.949 |
| Dialysis | 21 (0.4) | 17 (0.4) | 4 (1.0) | 0.192 |
| NYHA class | 0.010 | |||
| I | 2850 (59.2) | 2624 (59.7) | 226 (54.1) | |
| II | 1707 (35.5) | 1549 (35.2) | 158 (37.8) | |
| III | 239 (5.0) | 206 (4.7) | 33 (7.9) | |
| IV | 8 (0.2) | 8 (0.2) | 0 | |
| CCS IV | 266 (5.5) | 240 (5.5) | 26 (6.2) | 0.594 |
| Extend of CAD | ||||
| Single vessel disease | 26 (6.2) | |||
| Double vessel disease | 104 (24.9) | |||
| Triple vessel disease | 288 (68.9) | |||
| Left main disease | 133 (31.8) | |||
| Level of urgency | 0.231 | |||
| Elective | 1955 (40.5) | 1784 (40.4) | 277 (66.3) | |
| Urgent | 2595 (53.7) | 2377 (53.8) | 112 (26.8) | |
| Emergency | 263 (5.4) | 234 (5.3) | 29 (6.9) | |
| Salvage | 0 | 0 | 0 | |
| EuroSCORE II | 1.30 [0.88–2.10] | 1.31 [0.88–2.10] | 1.23 [0.85–1.91] | 0.478 |
| Preoperative hemoglobin (mmol/L) | 8.8 [8.2–9.3] | 8.8 [8.2–9.4] | 8.7 [8.1–9.3] | 0.102 |
| Preoperative hematocrit | 0.43 [0.40–0.45] | 0.43 [0.40–0.45] | 0.42 [0.40–0.45] | 0.126 |
| Preoperative creatinine (mL/min/1.72 m2) | 86 [76–100] | 86 [76–100] | 86 [74–98] | 0.764 |
| Overall (N = 4814) | No Reintervention (N = 4396) | Reintervention (N = 418) | p-Value | |
|---|---|---|---|---|
| Graft conduit | <0.001 | |||
| Single arterial | 251 (5.2) | 214 (4.9) | 37 (8.9) | |
| Single arterial + SVG | 4022 (85.5) | 3699 (84.1) | 323 (77.3) | |
| Multi arterial + SVG | 53 (1.1) | 44 (1.0) | 9 (2.2) | |
| Total arterial | 388 (8.1) | 349 (7.9) | 39 (9.3) | |
| Total venous | 100 (2.1) | 90 (2.1) | 10 (2.4) | |
| Number of distal anastomoses | 3.3 ± 1.0 | 3.3 ± 1.0 | 3.1 ± 1.1 | <0.001 |
| Number of arterial grafts | 1.3 ± 0.75 | 1.3 ± 0.7 | 1.3 ± 0.8 | 0.426 |
| Number of venous grafts | 2.0 ± 1.16 | 2.0 ± 1.2 | 1.8 ± 1.2 | 0.752 |
| Off-pump | 1107 (23.0) | 983 (22.4) | 124 (29.7) | 0.001 |
| Blood transfusion | ||||
| Red blood cells | 1060 (22.0) | 952 (21.6) | 108 (25.8) | 0.056 |
| Blood plasm | 173 (3.4) | 156 (3.5) | 17 (4.1) | 0.205 |
| Thrombocytes | 366 (7.6) | 334 (7.6) | 32 (7.7) | 0.239 |
| Hospital stay (Days) | 5.0 [4.0–6.0] | 5.0 [4.0–6.0] | 5.0 [4.0–7.0] | <0.001 |
| Readmission ICU | 100 (2.1) | 80 (1.8) | 20 (4.8) | <0.001 |
| Ventilation > 24 h | 90 (1.9) | 73 (1.7) | 17 (4.1) | 0.001 |
| Mortality | ||||
| In hospital | 32 (0.7) | 28 (0.6) | 4 (1.0) | 0.650 |
| Overall | 394 (8.2) | 349 (7.9) | 45 (10.8) | 0.095 |
| Reintervention Group (N = 418) | |
|---|---|
| Antihyperlipidemic medicines | |
| Statins | 327 (78.2) |
| Ezetimibe | 10 (2.4) |
| PSCK9 inhibitor | 3 (0.7) |
| Fibrate | 1 (0.4) |
| Combination medications | 32 (7.7) |
| Unknown/Hospital Death | 14 (3.3) |
| Anticoagulation | |
| Acetylsalicylic acid | 173 (41.4) |
| P2Y12 inhibitor | 11 (2.6) |
| Dual antiplatelet therapy | 137 (32.8) |
| DOAC | 4 (1.0) |
| Vitamin K antagonists | 1 (0.2) |
| Dual therapy * | 31 (14.6) |
| Triple therapy ** | 16 (3.8) |
| None | 2 (0.5) |
| Unknown/Hospital Death | 14 (3.3) |
| ACE-inhibitors/ARB | |
| Yes | 250 (59.8) |
| No | 154 (36.8) |
| Unknown/Hospital Death | 14 (3.3) |
| Beta-blockers | |
| Yes | 378 (90.4) |
| No | 26 (6.2) |
| Unknown/Hospital Death | 14 (3.3) |
| Calcium channel blockers | |
| Yes | 101 (24.2) |
| No | 303 (72.5) |
| Unknown/Hospital Death | 14 (3.3) |
| Diuretics | |
| Yes | 321 (76.8) |
| No | 82 (19.6) |
| Unknown/Hospital Death | 14 (3.3) |
| Reintervention Group (N = 418) | |
|---|---|
| Reintervention type | |
| Coronary artery bypass grafting | 40 (9.6) |
| Percutaneous coronary intervention | 378 (90.4) |
| Reason intervention | |
| Progression disease | 85 (20.3) |
| Graft failure | 270 (64.6) |
| Incomplete revascularization | 44 (10.5) |
| Combined | 17 (4.1) |
| Unknown | 2 (0.5) |
| Graft failure conduit (total used grafts) | (as percentage of total used grafts) |
| Left internal mammary artery (n = 4692) | 111 (2.4) |
| Right internal mammary artery (n = 246) | 8 (3.3) |
| Radial artery (n = 214) | 13 (6.1) |
| Venous (n = 4175) | 182 (4.4) |
| Unknown | 2 (0.5) |
| Univariable Analysis | Multivariable Analysis | |||||
|---|---|---|---|---|---|---|
| Variable | Hazard Ratio | 95% CI | p-Value | Hazard Ratio | 95% CI | p-Value |
| Female gender | 1.46 | 1.16–1.84 | 0.001 | 0.88 | 0.50–1.55 | 0.664 |
| Age (year) | 1.01 | 1.00–1.03 | 0.011 | 1.02 | 0.99–1.05 | 0.165 |
| Height (cm) | 0.98 | 0.97–0.99 | 0.001 | 1.02 | 0.99–1.05 | 0.151 |
| Weight (kg) | 0.99 | 0.98–1.00 | 0.001 | 0.98 | 0.97–1.00 | 0.044 |
| Diabetes | 1.01 | 1.00–1.02 | 0.076 | 1.02 | 1.00–1.04 | 0.011 |
| No treatment | ||||||
| Diet | ||||||
| Oral medication | ||||||
| Insulin | ||||||
| Peripheral vascular disease | 1.15 | 0.90–1.48 | 0.259 | |||
| Atrial fibrillation | 1.03 | 0.99–1.07 | 0.132 | |||
| Paroxysmal | ||||||
| Non-paroxysmal | ||||||
| Unstable angina | 1.16 | 0.80–1.70 | 0.429 | |||
| Recent myocardial infarction | 1.13 | 0.93–1.39 | 0.222 | |||
| Prior percutaneous coronary intervention | 0.90 | 0.73–1.10 | 0.290 | |||
| Left ventricular function | ||||||
| Good (<50%) | 1.50 | 0.21–10.69 | 0.686 | |||
| Moderate (31–50%) | 2.01 | 0.28–14.45 | 0.490 | |||
| Poor (21–30%) | 1.11 | 0.13–9.22 | 0.925 | |||
| Very poor (<20%) | 6.29 | 0.39–101.35 | 0.195 | |||
| Chronic lung disease | 1.26 | 0.83–1.91 | 0.270 | |||
| Pulmonary Hypertension | 1.05 | 0.99–1.11 | 0.130 | |||
| Poor mobility | 1.87 | 0.93–3.78 | 0.080 | 2.79 | 0.21–37.65 | 0.440 |
| Neurological dysfunction | 1.88 | 1.03–3.43 | 0.040 | 1.48 | 0.70–3.12 | 0.300 |
| Previous cerebral vascular accident | ||||||
| Dialysis | 0.98 | 0.36–2.62 | 0.965 | |||
| NYHA class | 1.05 | 0.91–1.22 | 0.510 | |||
| I | ||||||
| II | ||||||
| III | ||||||
| IV | ||||||
| CCS IV | 1.35 | 0.91–2.01 | 0.140 | |||
| Level of urgency | 1.01 | 0.99–1.03 | 0.191 | |||
| Elective | ||||||
| Urgent | ||||||
| Emergency | ||||||
| Salvage | ||||||
| Euroscore II | 1.05 | 1.01–1.09 | 0.015 | 0.94 | 0.77–1.14 | 0.517 |
| Preoperative hemoglobin (mmol/L) | 0.90 | 0.81–1.01 | 0.062 | 1.00 | 0.79–1.26 | 0.985 |
| Preoperative hematocrit | 0.56 | 0.33–0.96 | 0.035 | 0.64 | 0.32–1.28 | 0.208 |
| Preoperative creatinine (mL/min/1.72 m2) | 1.00 | 0.99–1.00 | 0.641 | |||
| ECC use | 1.00 | 0.99–1.01 | 0.665 | |||
| Graft conduit | ||||||
| Single arterial | 1.79 | 1.28–2.52 | <0.001 | 2.26 | 1.31–3.91 | 0.003 |
| Single arterial + SVG | 0.97 | 0.77–1.22 | 0.793 | |||
| Multi arterial + SVG | 1.03 | 0.53–2.00 | 0.928 | |||
| Total Arterial | 0.75 | 0.54–1.05 | 0.090 | 1.48 | 0.70–3.12 | 0.300 |
| Total Venous | 0.82 | 0.44–1.53 | 0.527 | |||
| Number of distal anastomoses | 1.03 | 0.93–1.13 | 0.588 | |||
| Arterial grafts | 1.00 | 0.88–1.13 | 0.960 | |||
| Venous grafts | 1.02 | 0.94–1.11 | 0.613 | |||
| Blood transfusion | ||||||
| Red blood cells | 1.50 | 1.21–1.87 | <0.001 | 1.11 | 0.71–1.74 | 0.642 |
| Blood plasm | 1.81 | 1.09–2.99 | 0.022 | 1.42 | 0.73–2.77 | 0.303 |
| Thrombocytes | 1.09 | 0.74–1.62 | 0.651 | |||
| Mortality | ||||||
| In hospital | 19.15 | 6.78–54.12 | <0.001 | 1.02 | 0.98–1.06 | 0.260 |
| Overall | 2.09 | 1.53–2.87 | <0.001 | 1.50 | 0.77–2.95 | 0.237 |
| Hospital stay (Days) | 1.01 | 1.00–1.03 | 0.026 | 1.02 | 0.98–1.06 | 0.260 |
| Readmission ICU | 1.88 | 1.19–2.95 | 0.006 | 0.74 | 0.32–1.69 | 0.472 |
| Ventilation > 24 h | 3.02 | 1.85–4.93 | <0.001 | 4.61 | 1.85–11.51 | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Achbar, I.; Görtzen, D.Q.F.N.; ter Woorst, J.F.J.; Teeuwen, K.; Tonino, P.A.L.; Akca, F. Etiology of Coronary Reintervention After Coronary Artery Bypass Surgery. J. Cardiovasc. Dev. Dis. 2026, 13, 20. https://doi.org/10.3390/jcdd13010020
Achbar I, Görtzen DQFN, ter Woorst JFJ, Teeuwen K, Tonino PAL, Akca F. Etiology of Coronary Reintervention After Coronary Artery Bypass Surgery. Journal of Cardiovascular Development and Disease. 2026; 13(1):20. https://doi.org/10.3390/jcdd13010020
Chicago/Turabian StyleAchbar, Ikram, De Qing F. N. Görtzen, Joost F. J. ter Woorst, Koen Teeuwen, Pim A. L. Tonino, and Ferdi Akca. 2026. "Etiology of Coronary Reintervention After Coronary Artery Bypass Surgery" Journal of Cardiovascular Development and Disease 13, no. 1: 20. https://doi.org/10.3390/jcdd13010020
APA StyleAchbar, I., Görtzen, D. Q. F. N., ter Woorst, J. F. J., Teeuwen, K., Tonino, P. A. L., & Akca, F. (2026). Etiology of Coronary Reintervention After Coronary Artery Bypass Surgery. Journal of Cardiovascular Development and Disease, 13(1), 20. https://doi.org/10.3390/jcdd13010020








