Bioactivity and Component Analysis of Water Extract of Sophora japonica against Hyperuricemia by Inhibiting Xanthine Oxidase Activity
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Extraction Process of Sophora japonica
2.3. Preparation of WESJ
2.4. UV Spectrophotometry and XOD Inhibition Activity of WESJ
2.5. Animals and Experimental Design
2.6. Biochemical Analysis
2.7. Histopathological Examinations
2.8. LC-Q-TOF-MS/MS Detection
2.8.1. LC-Q-TOF-MS/MS Analysis
2.8.2. Determination of Chemical and Serum Components of WESJ
2.9. Data Analysis
3. Results and Discussion
3.1. Development of the UV Spectrophotometry
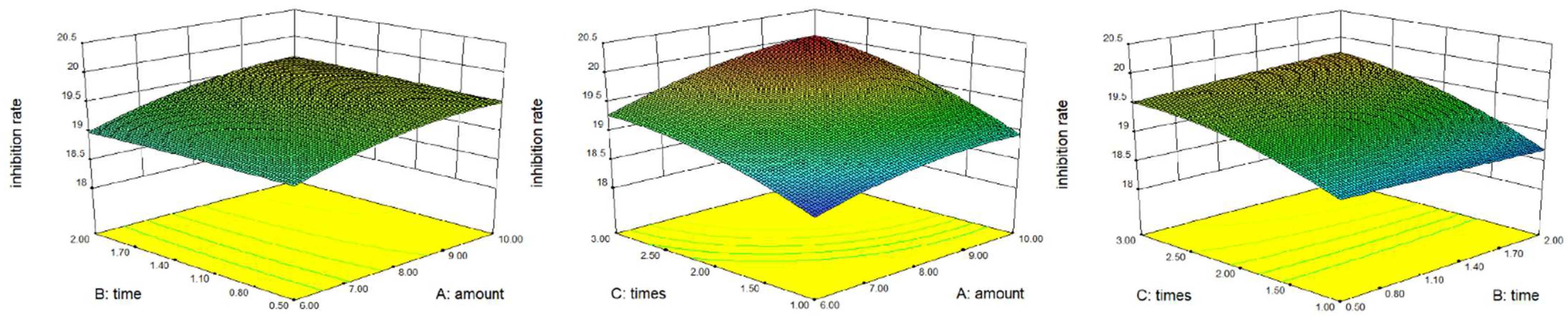
3.2. Optimization of Extraction Process
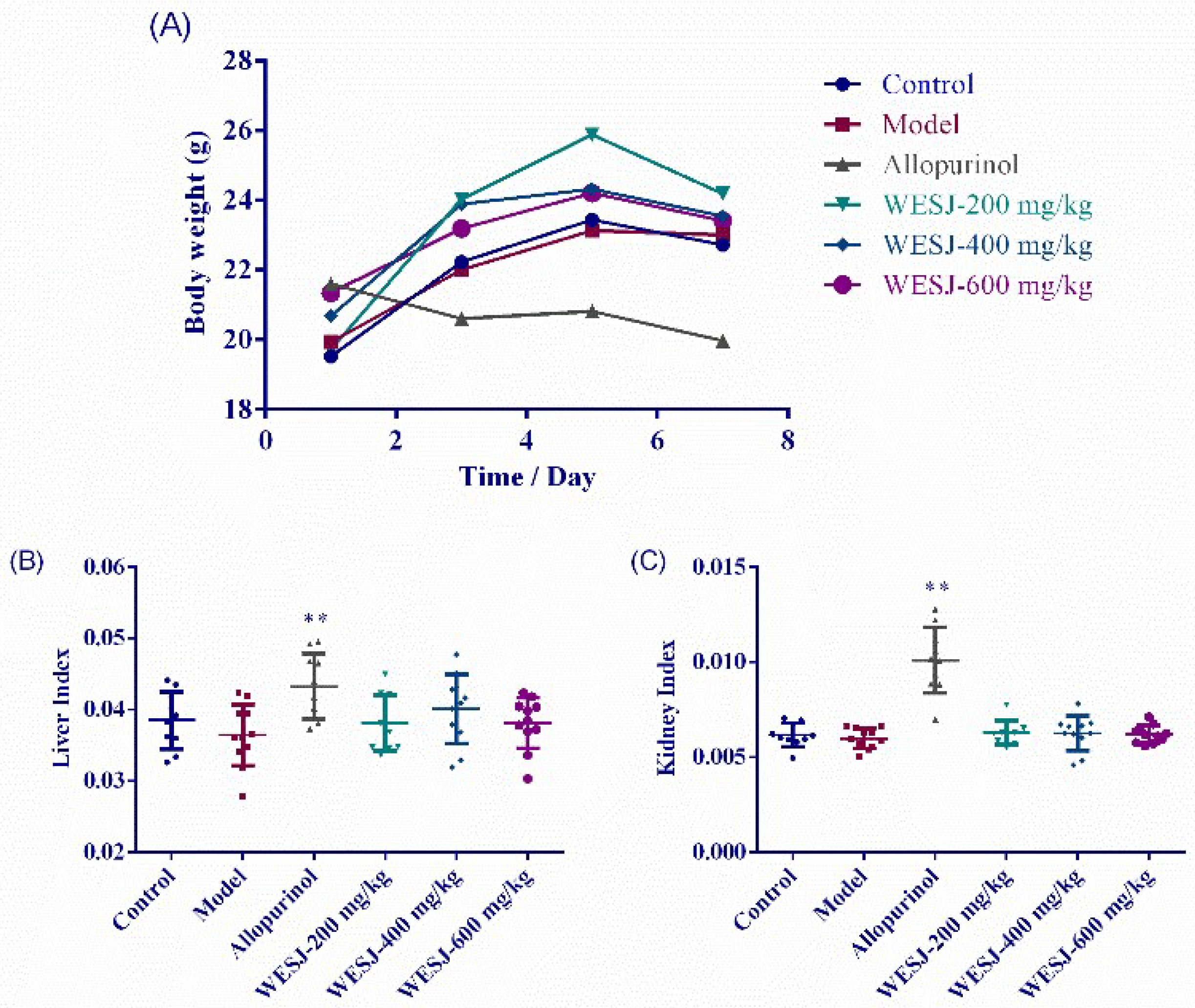
3.3. Effects of WESJ on Body Weight and Organ Index
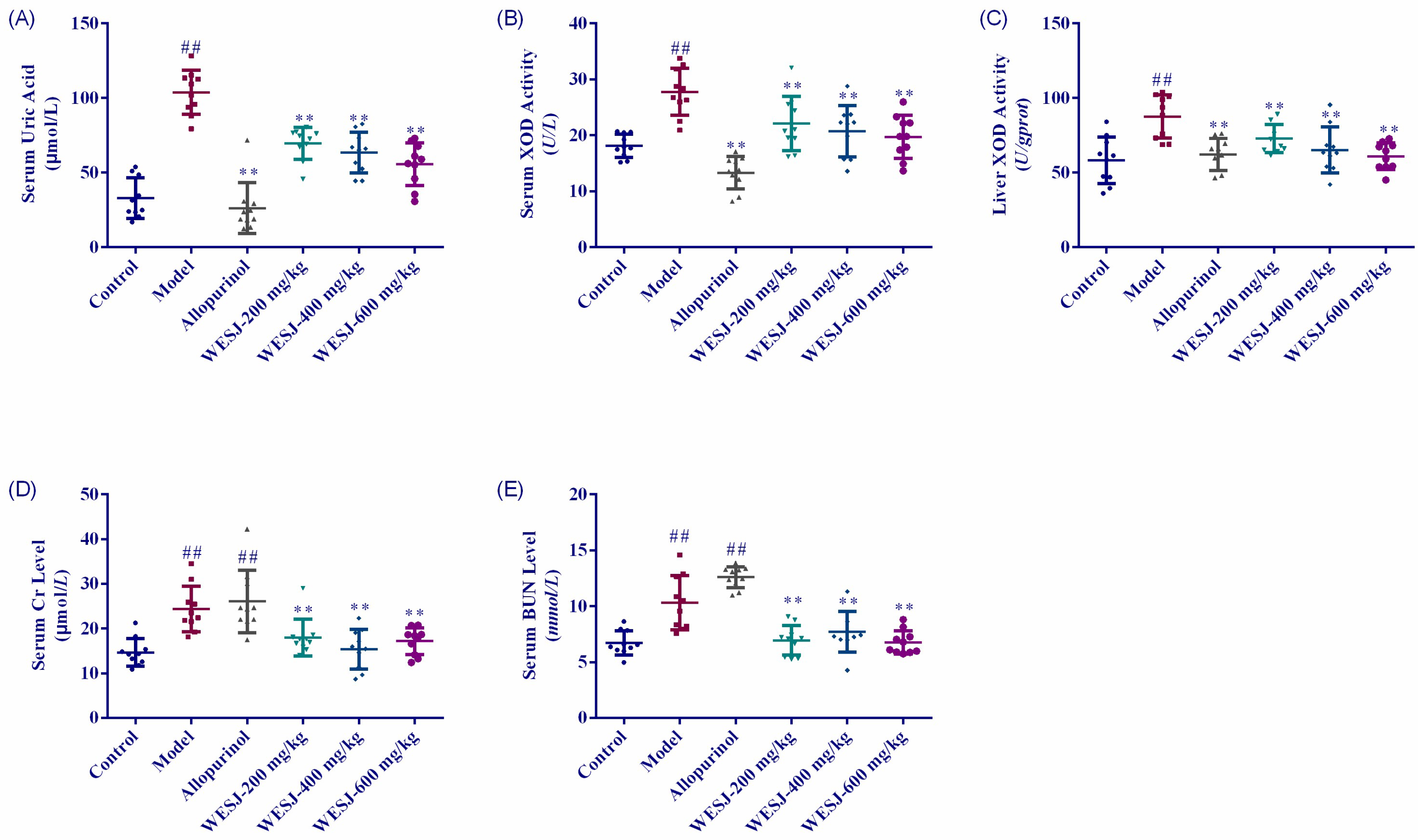
3.4. Biochemical Effects of WESJ on Hyperuricemic Mice
3.5. Effects of WESJ on Kidney Histopathology in Hyperuricemic Mice
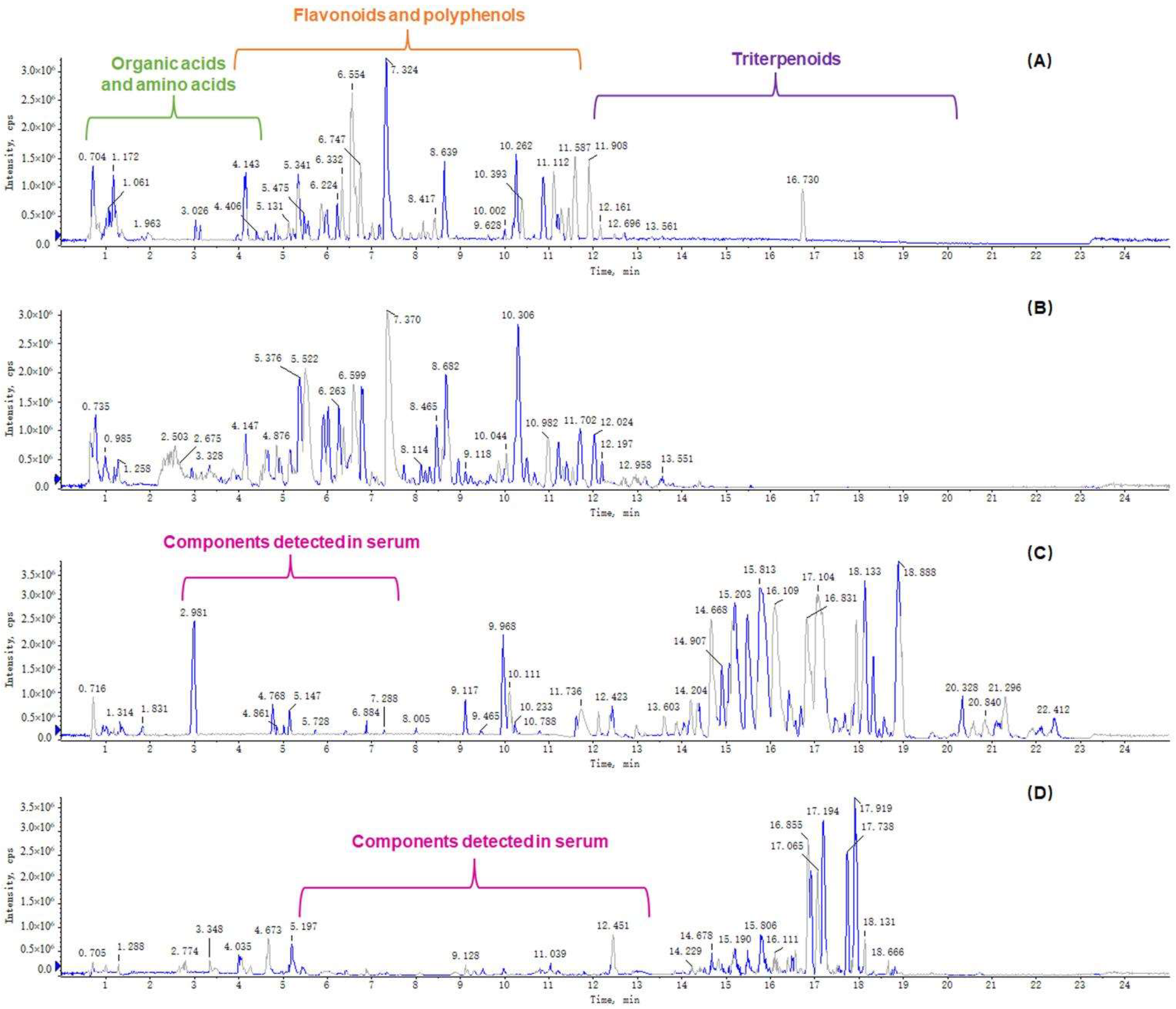
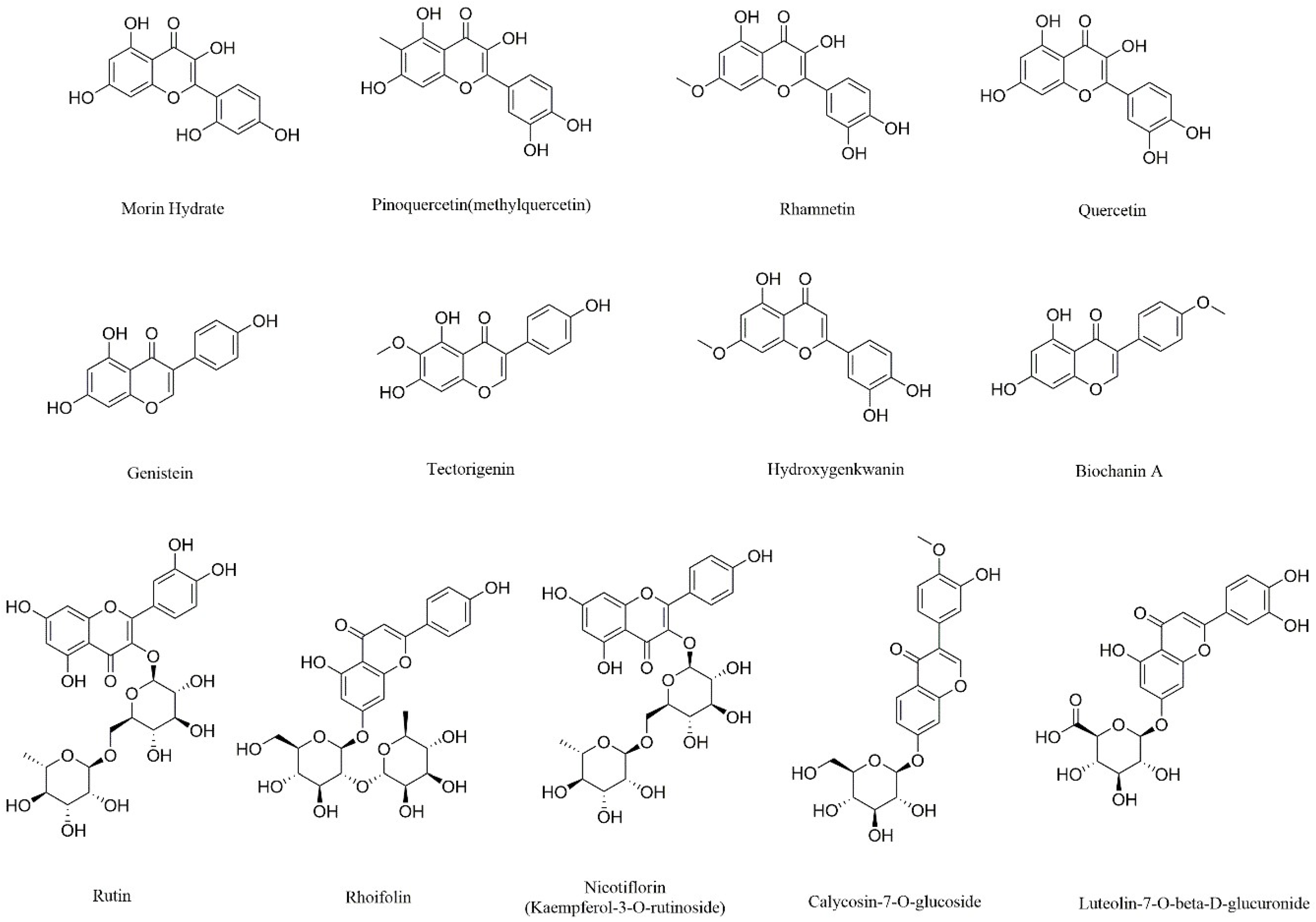
3.6. Determination of Chemical and Serum Components of WESJ
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ichida, K.; Amaya, Y.; Okamoto, K.; Nishino, T. Mutations associated with functional disorder of xanthine oxidoreductase and hereditary xanthinuria in humans. Int. J. Mol. Sci. 2012, 13, 15475–15495. [Google Scholar] [CrossRef]
- Zhou, X.; Zhang, B.; Zhao, X.; Lin, Y.; Wang, J.; Wang, X.; Hu, N.; Wang, S. Chlorogenic acid supplementation ameliorates hyperuricemia, relieves renal inflammation, and modulates intestinal homeostasis. Food Funct. 2021, 12, 5637–5649. [Google Scholar] [CrossRef]
- Hong, F.; Zheng, A.; Xu, P.; Wang, J.; Xue, T.; Dai, S.; Pan, S.; Guo, Y.; Xie, X.; Li, L.; et al. High-Protein Diet Induces Hyperuricemia in a New Animal Model for Studying Human Gout. Int. J. Mol. Sci. 2020, 21, 2147. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.Z.; Xu, X.; Zhu, J.Q.; Zhao, D.B. Association between three non-insulin-based indexes of insulin resistance and hyperuricemia. Clin. Rheumatol. 2019, 38, 3227–3233. [Google Scholar] [CrossRef]
- Shirakabe, A.; Okazaki, H.; Matsushita, M.; Shibata, Y.; Goda, H.; Uchiyama, S.; Tani, K.; Kiuchi, K.; Kobayashi, N.; Hata, N.; et al. Hyperuricemia complicated with acute kidney injury is associated with adverse outcomes in patients with severely decompensated acute heart failure. Int. J. Cardiol. Heart Vasc. 2019, 23, 100345. [Google Scholar] [CrossRef]
- Xu, D.; Lv, Q.; Wang, X.; Cui, X.; Zhao, P.; Yang, X.; Liu, X.; Yang, W.; Yang, G.; Wang, G.; et al. Hyperuricemia is associated with impaired intestinal permeability in mice. Am. J. Physiol.-Gastrointest. Liver Physiol. 2019, 317, G484–G492. [Google Scholar] [CrossRef]
- Choi, H.; Neogi, T.; Stamp, L.; Dalbeth, N.; Terkeltaub, R. Implications of the cardiovascular safety of febuxostat and allopurinol in patients with gout and cardiovascular morbidities (CARES) trial and associated FDA public safety alert. Arthritis Rheumatol. 2018, 70, 1702–1709. [Google Scholar] [CrossRef] [PubMed]
- Dalbeth, N.; Stamp, L. Allopurinol dosing in renal impairment: Walking the tightrope between adequate urate lowering and adverse events. Semin. Dial. 2007, 20, 391–395. [Google Scholar] [CrossRef]
- Halevy, S.; Ghislain, P.D.; Mockenhaupt, M.; Fagot, J.P.; Bouwes Bavinck, J.N.; Sidoroff, A.; Naldi, L.; Dunant, A.; Viboud, C.; Roujeau, J.C.; et al. Allopurinol is the most common cause of Stevens-Johnson syndrome and toxic epidermal necrolysis in Europe and Israel. J. Am. Acad. Dermatol. 2008, 58, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Jeannie Chao, M.; Robert Terkeltaub, M.D. A Critical Reappraisal of Allopurinol Dosing, Safety, and Efficacy for Hyperuricemia in Gout. Cryst. Arthritis 2009, 11, 135–140. [Google Scholar]
- White, W.B.; Saag, K.G.; Becker, M.A.; Borer, J.S.; Gorelick, P.B.; Whelton, A.; Hunt, B.; Castillo, M.; Gunawardhana, L.; Investigators, C. Cardiovascular Safety of Febuxostat or Allopurinol in Patients with Gout. N. Engl. J. Med. 2018, 378, 1200–1210. [Google Scholar] [CrossRef] [PubMed]
- He, X.; Bai, Y.; Zhao, Z.; Wang, X.; Fang, J.; Huang, L.; Zeng, M.; Zhang, Q.; Zhang, Y.; Zheng, X. Local and traditional uses, phytochemistry, and pharmacology of Sophora japonica L.: A review. J. Ethnopharmacol. 2016, 187, 160–182. [Google Scholar] [CrossRef] [PubMed]
- Abd-Alla, H.I.; Souguir, D.; Radwan, M.O. Genus Sophora: A comprehensive review on secondary chemical metabolites and their biological aspects from past achievements to future perspectives. Arch. Pharm. Res. 2021, 44, 903–986. [Google Scholar] [CrossRef]
- Yang, J.; Gu, D.; Ji, Z.; Fang, C.; Xu, F.; Yang, Y. Comprehensive separation of major compositions from Sophora japonica var. violacea by counter-current chromatography using a liquid-liquid extraction strategy. Ind. Crops Prod. 2018, 124, 363–368. [Google Scholar] [CrossRef]
- Montenegro-Landivar, M.F.; Tapia-Quiros, P.; Vecino, X.; Reig, M.; Valderrama, C.; Granados, M.; Cortina, J.L.; Saurina, J. Polyphenols and their potential role to fight viral diseases: An overview. Sci. Total Environ. 2021, 801, 149719. [Google Scholar] [CrossRef]
- Chiva-Blanch, G.; Badimon, L. Effects of Polyphenol Intake on Metabolic Syndrome: Current Evidences from Human Trials. Oxidative Med. Cell. Longev. 2017, 2017, 5812401. [Google Scholar] [CrossRef]
- Hong, M.; Cheng, L.; Liu, Y.; Wu, Z.; Zhang, P.; Zhang, X. A Natural Plant Source-Tea Polyphenols, a Potential Drug for Improving Immunity and Combating Virus. Nutrients 2022, 14, 550. [Google Scholar] [CrossRef]
- Panda, P.K.; Yang, J.M.; Chang, Y.H.; Su, W.W. Modification of different molecular weights of chitosan by p-Coumaric acid: Preparation, characterization and effect of molecular weight on its water solubility and antioxidant property. Int. J. Biol. Macromol. 2019, 136, 661–667. [Google Scholar] [CrossRef]
- Roy, A.; Khan, A.; Ahmad, I.; Alghamdi, S.; Rajab, B.S.; Babalghith, A.O.; Alshahrani, M.Y.; Islam, S.; Islam, M.R. Flavonoids a Bioactive Compound from Medicinal Plants and Its Therapeutic Applications. Biomed. Res. Int. 2022, 2022, 5445291. [Google Scholar] [CrossRef]
- Ramesh, P.; Jagadeesan, R.; Sekaran, S.; Dhanasekaran, A.; Vimalraj, S. Flavonoids: Classification, Function, and Molecular Mechanisms Involved in Bone Remodelling. Front. Endocrinol. 2021, 12, 779638. [Google Scholar] [CrossRef]
- Awad, H.M.; Abd-Alla, H.I.; Mahmoud, K.H.; El-Toumy, S.A. In vitro anti-nitrosative, antioxidant, and cytotoxicity activities of plant flavonoids: A comparative study. Med. Chem. Res. 2014, 23, 3298–3307. [Google Scholar] [CrossRef]
- Kite, G.C.; Veitch, N.C.; Boalch, M.E.; Lewis, G.P.; Leon, C.J.; Simmonds, M.S. Flavonol tetraglycosides from fruits of Styphnolobium japonicum (Leguminosae) and the authentication of Fructus Sophorae and Flos Sophorae. Phytochemistry 2009, 70, 785–794. [Google Scholar] [CrossRef] [PubMed]
- Shi, W.; Liu, L.; Li, J.; Qu, L.; Pang, X.; Yu, H.; Zhang, Y.; Wang, T. Bioactive flavonoids from Flos Sophorae. J. Nat. Med. 2017, 71, 513–522. [Google Scholar] [CrossRef] [PubMed]
- Xie, Z.; Sun, Y.; Lam, S.; Zhao, M.; Liang, Z.; Yu, X.; Yang, D.; Xu, X. Extraction and isolation of flavonoid glycosides from Flos Sophorae Immaturus using ultrasonic-assisted extraction followed by high-speed countercurrent chromatography. J. Sep. Sci. 2014, 37, 957–965. [Google Scholar] [CrossRef]
- Biswal, A.K.; Panda, P.K.; Yang, J.M.; Misra, P.K. Isolation, process optimisation and characterisation of the protein from the de-oiled cake flour of Madhuca latifolia. IET Nanobiotechnol. 2020, 14, 654–661. [Google Scholar] [CrossRef]
- Abd-El-Aziz, N.M.; Hifnawy, M.S.; El-Ashmawy, A.A.; Lotfy, R.A.; Younis, I.Y. Application of Box-Behnken design for optimization of phenolics extraction from Leontodon hispidulus in relation to its antioxidant, anti-inflammatory and cytotoxic activities. Sci. Rep. 2022, 12, 8829. [Google Scholar] [CrossRef]
- Gong, X.; Shao, J.; Guo, S.; Pan, J.; Fan, X. Determination of inhibitory activity of Salvia miltiorrhiza extracts on xanthine oxidase with a paper-based analytical device. J. Pharm. Anal. 2021, 11, 603–610. [Google Scholar] [CrossRef]
- Rojas-Garcia, A.; Fuentes, E.; Cadiz-Gurrea, M.L.; Rodriguez, L.; Villegas-Aguilar, M.D.C.; Palomo, I.; Arraez-Roman, D.; Segura-Carretero, A. Biological Evaluation of Avocado Residues as a Potential Source of Bioactive Compounds. Antioxidants 2022, 11, 1049. [Google Scholar] [CrossRef]
- McKendrick, M.W.; Geddes, A.M. Allopurinol hypersensitivity. Br. Med. J. 1979, 1, 988. [Google Scholar] [CrossRef][Green Version]
- Luo, L.S.; Wang, Y.; Dai, L.J.; He, F.X.; Zhang, J.L.; Zhou, Q. Triterpenoid acids from medicinal mushroom Inonotus obliquus (Chaga) alleviate hyperuricemia and inflammation in hyperuricemic mice: Possible inhibitory effects on xanthine oxidase activity. J. Food Biochem. 2022, 46, e13932. [Google Scholar] [CrossRef]
- Deng, L.; Qiu, S.; Wang, C.; Bian, H.; Wang, L.; Li, Y.; Wu, B.; Liu, M. Effects of the blood urea nitrogen to creatinine ratio on haemorrhagic transformation in AIS patients with diabetes mellitus. BMC Neurol. 2019, 19, 63. [Google Scholar] [CrossRef] [PubMed]
- Forcet, C.; Stein, E.; Pays, L.; Corset, V.; Llambi, F.; Tessier-Lavigne, M.; Mehlen, P. Netrin-1-mediated axon outgrowth requires deleted in colorectal cancer-dependent MAPK activation. Nature 2002, 417, 443–447. [Google Scholar] [CrossRef] [PubMed]
- Matsue, Y.; van der Meer, P.; Damman, K.; Metra, M.; O’Connor, C.M.; Ponikowski, P.; Teerlink, J.R.; Cotter, G.; Davison, B.; Cleland, J.G.; et al. Blood urea nitrogen-to-creatinine ratio in the general population and in patients with acute heart failure. Heart 2017, 103, 407–413. [Google Scholar] [CrossRef] [PubMed]
- Ok, F.; Erdogan, O.; Durmus, E.; Carkci, S.; Canik, A. Predictive values of blood urea nitrogen/creatinine ratio and other routine blood parameters on disease severity and survival of COVID-19 patients. J. Med. Virol. 2021, 93, 786–793. [Google Scholar] [CrossRef]
- Qian, H.; Tang, C.; Yan, G. Predictive value of blood urea nitrogen/creatinine ratio in the long-term prognosis of patients with acute myocardial infarction complicated with acute heart failure. Medicine 2019, 98, e14845. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiang, S.; Song, D.; Zhao, H.; Wang, F.; Su, X.; Zhang, X.; Zhao, X. Bioactivity and Component Analysis of Water Extract of Sophora japonica against Hyperuricemia by Inhibiting Xanthine Oxidase Activity. Foods 2022, 11, 3772. https://doi.org/10.3390/foods11233772
Jiang S, Song D, Zhao H, Wang F, Su X, Zhang X, Zhao X. Bioactivity and Component Analysis of Water Extract of Sophora japonica against Hyperuricemia by Inhibiting Xanthine Oxidase Activity. Foods. 2022; 11(23):3772. https://doi.org/10.3390/foods11233772
Chicago/Turabian StyleJiang, Shunyi, Danni Song, Honghui Zhao, Fuqi Wang, Xin Su, Xinyang Zhang, and Xu Zhao. 2022. "Bioactivity and Component Analysis of Water Extract of Sophora japonica against Hyperuricemia by Inhibiting Xanthine Oxidase Activity" Foods 11, no. 23: 3772. https://doi.org/10.3390/foods11233772
APA StyleJiang, S., Song, D., Zhao, H., Wang, F., Su, X., Zhang, X., & Zhao, X. (2022). Bioactivity and Component Analysis of Water Extract of Sophora japonica against Hyperuricemia by Inhibiting Xanthine Oxidase Activity. Foods, 11(23), 3772. https://doi.org/10.3390/foods11233772




