Abstract
Temporomandibular disorders include various conditions that impact the masticatory system, affecting its structure, function, or physiology. Clinicians face a complex array of therapeutic options when treating this group of diseases, emphasizing the importance of evaluating the current evidence to guide decisions in patient care. The main objective of this article is to conduct a scoping review on the available treatment approaches to manage temporomandibular disorders (TMDs). An extensive search of the literature was performed on Scopus, Pubmed, Embase, and Web of Science. Systematic reviews published in the last 5 years were considered. Out of the 2183 publications identified, 109 studies were included in this review. Among them, 39 articles focused on the non-invasive approach, while 120 delved into the minimally invasive approach, and 15 explored the surgical approach. Non-invasive or conservative approaches like cognitive-behavioral therapy, physical therapy, and acupuncture offer effective pain management and functional improvements in TMDs. Emerging treatments offer promising alternatives for treating these disorders. Surgery should be reserved for severe cases, with conservative therapies used in conjunction with invasive procedures for optimal patient outcomes.
1. Introduction
Temporomandibular disorders (TMDs) encompass a range of diseases or disorders that impact the structure, function, or physiology of the masticatory system. TMDs primarily include disorders associated with pain, such as myalgia, myofascial pain, or arthralgia, as well as disorders related to functional or structural changes in the temporomandibular joint, such as disorders of the disc and degenerative joint conditions [1].
The prevalence of these disorders varies depending on the age group, with adults and the elderly presenting a prevalence of 31%, while children and adolescents have a prevalence that varies between 20% and 60%. Additionally, the most common disorder is disk displacement with reduction [2,3]. Based on recent epidemiological findings and scientific evidence, it has been noted that women have twice the risk of developing TMDs compared to men [4]. Gender differences have also been observed in pain tolerance and expectations; in temporal summation and somatic perception, female gender is also the most significant risk factor [5].
The etiology is multifactorial and there is no evidence of a link between genetic variants and TMDs [6]. The main factors associated with this group of disorders are third molar extraction, orthognathic surgery, catastrophizing, and bruxism [7,8,9,10]. TMDs also show a comorbid relationship with other diseases or risk factors, which increase the rate of their development, such as systemic rheumatic disease; psychosocial factors such as somatization, depression, and distress; and Parkinson’s disease [11,12,13].
The diagnosis of TMDs involves a comprehensive assessment that includes a detailed history, clinical examination, and imaging. However, the goal of TMD assessments is to identify one or more biomarkers (molecules such as prostaglandin (PG), matrix metalloproteinases (MMPs), interleukins (ILs), tumor necrosis factor (TFN), bradykinin, glutamate, neuropeptides, nerve growth factor (NFG), and serotonin; neuroimaging markers such as N-acetyl aspartate (NAA), choline (Cho), total creatine (tCr), glutamine (Gln), and myo-insitol; and biochemicals such as vitamin D and 8-hydroxydeoxyguanosine and malondialdehyde) that are involved in the manifestation of painful TMDs [14]. TMDs can manifest a variety of clinical manifestations that can only emerge through a very accurate history. They are often associated with sleep disturbances such as obstructive sleep apnea and gastroesophageal reflux; cervical musculoskeletal disorders and fibromyalgia; primary headaches; and tinnitus [15,16,17,18,19,20]. Depending on the magnitude of the TMD, the quality of life can also deteriorate [21,22].
Regarding treatment approaches for TMDs, clinicians face a complex array of therapeutic options, and recent research findings have not simplified this dilemma but rather added to the complexity. The modern management of temporomandibular disorders (TMDs) is based on a biopsychosocial model and an orthopedic approach, as they are considered as a musculoskeletal group of diseases rather than solely a dental or occlusal problem [23].
Evidence-based medicine (EBM) involves the careful and deliberate utilization of the current best evidence to guide decisions in patient care [24]. Given the multidisciplinary nature, the variety of available treatment approaches, and the emergence of new therapies for TMDs, it is imperative to synthesize the current evidence to enhance clinical practices. Therefore, the aim of this article is to provide a scoping review of the treatment strategies available to manage TMDs.
2. Materials and Methods
This scoping review was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for conducting scoping reviews (PRISMA-ScR) [25]. This scoping review was not registered.
2.1. Search Strategy
A systematic search was conducted on Scopus, PubMed, Embase, and Web of Science. The search strategy designed for each database is shown in Table 1.

Table 1.
Search strategy for Scopus, PubMed, Embase, and Web of Science.
The inclusion criteria were systematic reviews and meta-analyses with evidence-based methodologies for the assessment and evaluation of findings. Papers that made claims about the efficacy of devices, diagnostic tools, or therapeutic methods without evidence-based research were excluded.
2.2. Data Extraction and Synthesis
The review process initially involved screening the titles and abstracts. Then, the full text of the selected papers was assessed. Two different reviewers (GM, NZ) independently conducted the process and discordant evaluations were resolved through a discussion with a third researcher (AV). The final decision on inclusion or exclusion in the review was reached through consensus between all the authors. The full text of each study was retrieved and independently evaluated by two authors. After thorough discussion, the studies were categorized into the following classes: diagnosis, clinical implications, treatment, and prevention.
For each article, we extracted the following information: author, year of publication, country of the primary author’s institution, number and type of studies included in the review, treatment approaches evaluated, and conclusions.
3. Results
3.1. Literature Screening Process
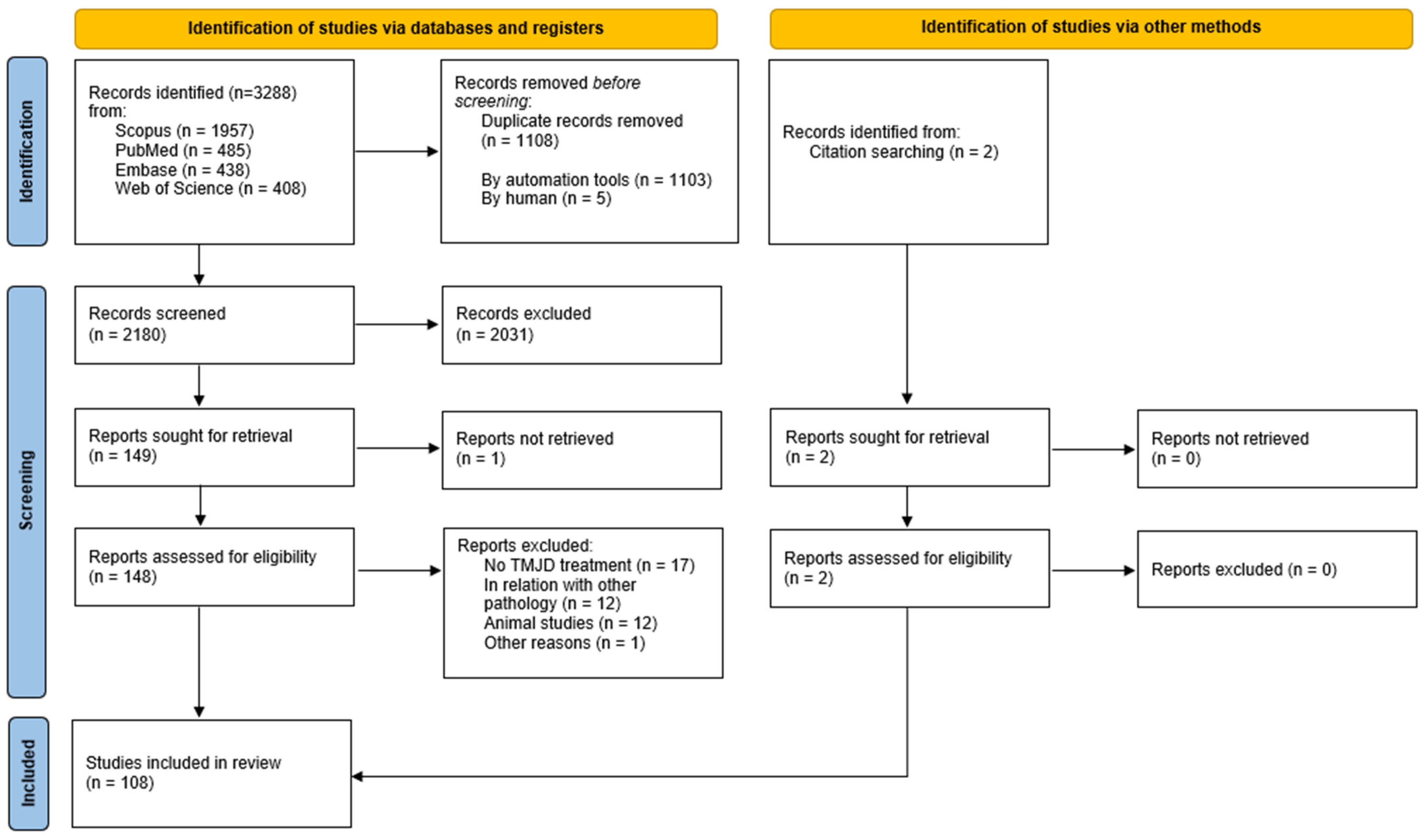
The search strategy yielded a total of 3288 publications, including 1957 from Scopus, 485 from Pubmed, 438 from Embase, and 408 from Web of Science. By removing duplicates, 1108 publications were excluded. From the remaining 2180 records, after reviewing the title and abstract, 2031 studies were excluded. Afterwards, the full text of the remaining 148 studies was thoroughly examined; one study could not be retrieved. After assessment of the full text, 42 reports were excluded. Ultimately, 106 records met the inclusion criteria. Additionally, two publications were retrieved by citation searching. The literature search and screening procedure are detailed in Figure 1.
Figure 1.
Flowchart of study selection process [26].
3.2. Description of the Selected Studies
Based on the treatment assessed, the articles were categorized into non-invasive, minimally invasive, and invasive (Table 2).

Table 2.
Treatment approaches and corresponding references.
3.2.1. Study Characteristics
The countries with the highest number of reviews were China (n = 14) [47,57,59,63,70,76,77,79,104,105,112,114,122,124], followed by Brazil (n = 13) [33,44,64,90,93,106,107,111,115,123,127,129,131], and Spain (n = 9) [36,38,41,43,45,52,68,103,110]. The number of studies encompassed in these reviews ranged from 52 [34,52,125] to 3 [102], with RCTs predominating the dataset. All the characteristics of the included studies are documented in Table 3.

Table 3.
Characteristics of included systematic reviews and meta-analyses.
3.2.2. Treatment Approaches
The treatment approaches were classified into three categories: non-invasive (conservative), minimally invasive, and invasive.
Non-Invasive (Conservative) Approaches
- Cognitive–behavioral therapy (CBT) and counseling
CBT has been widely acknowledged as efficacious in the management of orofacial pain (OFP), as well as in mitigating psychological distress stemming from TMDs [27]. Counseling is also a valuable addition to traditional conservative approaches like splints or manual therapy [29]. However, a recent Cochrane review (2022) found only limited evidence that CBT has a greater capacity to diminish pain intensity compared to alternative treatments or control groups, but not at treatment completion [27].
- Physical therapy, MT, and exercises
A systematic review indicated that either a mobility or mixed approach may alleviate discomfort and enhance mobility, but with a limited impact on functional improvement [41]. MT and therapeutic exercise stand as efficacious therapeutic modalities for diminishing pain, elevating pain pressure thresholds, and augmenting both active and passive MMO in individuals afflicted with TMDs. They may be beneficial and play a role in the treatment of disc displacement without reduction [43,52]. Oral myofunctional therapy has also been effective in reducing the pain intensity compared to other conservative treatments [53]. Investigations indicated the potential utility of physiotherapy as an advantageous therapeutic avenue for individuals with TMJ dysfunction. Nonetheless, evaluating the efficacy of distinct therapeutic modalities for TMJ patients and discerning whether particular TMJ pathologies exhibit a heightened responsiveness to conservative management could furnish valuable insights into the effectiveness of conventional interventions within this patient cohort [34].
Physical therapy interventions have shown benefits for TMD patients with comorbid headaches [32].
MT has exhibited efficacy as an intervention for temporomandibular disorders in the intermediate duration, albeit with a diminishing impact observed longitudinally. Nevertheless, the integration of MT with therapeutic exercise has the potential to sustain these therapeutic outcomes over the extended term [41].
Regarding comparisons, MT has demonstrated superiority over an absence of treatment in one investigation and outperformed counseling in another. However, when MT is amalgamated with counseling, it does not exhibit statistically significant superiority over counseling in isolation. Furthermore, MT in isolation did not produce better results when contrasted with the effects of botulinum toxin. In a separate study, the combination of MT with home-based therapy proved more efficacious than home-based therapy alone. Nevertheless, due to inconclusive data and inadequate homogeneity, further research is warranted to offer more conclusive determinations [33].
Concerning cervical MT interventions, the findings indicated their superior efficacy in diminishing the pain intensity compared to placebo MT or minimal intervention, which is bolstered by moderate evidential support. Combined cervico-craniomandibular interventions yielded greater short-term reductions in pain intensity and enhanced pain-free maximum mouth opening in patients afflicted with TMDs and headaches, although the inconclusive evidence hampers drawing definitive conclusions [36]. The application of cervical-mandibular manual therapies, alongside exercise and educational components, has exhibited superior outcomes compared to exercise/education alone in individuals experiencing tinnitus attributed to a TMD [118].
In order to ascertain the optimal manual therapy methodologies for alleviating pain and enhancing maximum mouth opening in individuals with TMDs, high-caliber research employing diverse techniques across various regions and patient demographics is imperative [39].
Yet another systematic review incorporating a meta-analysis indicated that rehabilitative strategies could potentially surpass placebo and sham interventions in mitigating pain among individuals with muscle-related TMDs. Nonetheless, the scarcity of randomized controlled trials appraising conservative methodologies impedes the amalgamation of the evidence concerning distinct techniques, underscoring the necessity for circumspection in interpreting these findings [42].
- Other options
Numerous new treatment options are continuously being introduced, but only a few have sufficient supporting evidence.
Oxygen–ozone (O2O3) therapy exhibited promise in reducing TMD pain and enhancing MMO, especially when employed during arthrocentesis. Nonetheless, there is a dearth of conclusive evidence regarding its superiority compared to occlusal splints and pharmacological interventions. The studies included in this review exhibited considerable diversity in terms of comparators, application techniques, ozone concentration, treatment frequencies, and follow-up durations. Further double-blind clinical trials are imperative to consolidate our understanding before contemplating the integration of OT into clinical TMD management protocols [55]. In most studies, ozone therapy is placed in the context of a mixed approach as an adjunct to other conservative or minimally invasive treatments for TMDs [34,40,54,56].
In the systematic reviews analyzed, only one article mentions ultrasonic therapy, comparing it to acupuncture and affirming the latter technique’s greater therapeutic effects on TMDs than the former [57].
Minimally Invasive Approaches
- Arthrocentesis or intra-articular injections
It can be seen inferred that TMJ arthrocentesis enhances mandibular functionality and alleviates the pain intensity, with multiple sessions (ranging from three to five) exhibiting greater efficacy compared to a solitary session [58]. The limited data suggest that there is no notable disparity in pain or maximal mandibular aperture between single- or double-puncture techniques for arthrocentesis [61].
Intra-articular CCS or NSAID analgesic injections do not seem to provide additional advantages over lavage [57]. On the other hand, injections of hyaluronic acid (HA) administered within the joint have shown benefits in improving the functional symptoms and pain associated with TMDs [65]. Still, the evidence suggested that intra-articular pharmacological injections of corticosteroids, hyaluronic acid, and platelet-rich plasma did not produce any significant improvement in temporomandibular joint pain and functional outcomes when compared with placebo injections [78].
A systematic review incorporating a meta-analysis examining the comparative risk profiles associated with arthroscopy and arthrocentesis procedures of the TMJ determined that there is no elevated likelihood of complications with arthroscopy vis à vis arthrocentesis. Moreover, the complications observed were transient in nature [63].
Yet another systematic review evaluated the effectiveness of splint therapy in enhancing outcomes subsequent to arthrocentesis, encompassing six investigations. This review revealed no statistically notable discrepancy in pain mitigation or enhancement of the maximal mouth aperture, whether splint usage was involved or not following arthrocentesis, both at one month and six months [68]. The ideal timing for conducting arthrocentesis in TMD management was assessed in a review encompassing eight randomized controlled trials and three prospective clinical investigations. Whether performed early or late as the initial intervention, arthrocentesis exhibited enhancements in mouth opening and pain alleviation [72].
Moreover, numerous novel compounds have undergone scrutiny regarding their efficacy in managing TMJ pain and augmenting mandibular abduction. These encompass analgesic agents, dextrose coupled with lidocaine, adipose tissue, hematopoietic stem cells, and ozone. Administering arthrocentesis before the injection appears to augment the efficacy of intra-articular delivery, with bone marrow and adipose tissue showing the most promising results [85]. Among individuals diagnosed with temporomandibular joint osteoarthritis (TMJ-OA), arthrocentesis has demonstrated efficacy in significantly alleviating pain and enhancing mandibular functionality. However, additional injections of hyaluronic acid (HA), either low-molecular-weight (LMW) HA or high-molecular-weight (HMW) HA, or cortisone at the end of arthrocentesis did not lead to further improvements in clinical outcomes [97]. A systematic review comparing the treatment of TMJ-OA with HA, corticosteroids, and blood products in conjunction with arthrocentesis found that all substances efficiently alleviated pain and improved MMO [80]. For TMJ-OA, tramadol, morphine, and platelet-derived growth factor (PDGF) injections after arthrocentesis have shown positive effects in reducing pain and improving joint opening, and short-term improvements in maximal mouth opening have also been observed with hyaluronic acid injections in TMJ-OA patients [69]. In cases of recurrent TMJ luxation, intra-articular autologous blood injection combined with pericapsular tissue application, accompanied by intermaxillary fixation, stands out as the most scientifically substantiated treatment approach. Nonetheless, methodologically robust studies, encompassing adequate patient cohorts, extended follow-up periods, and comprehensive patient-reported outcome measures, are required to delineate the optimal surgical therapeutic modalities [73].
- PRP, PRF, PRGF, PDGF, and stem cell therapy
An expanding corpus of research indicates the prospective advantages of intra-articular PRP, PRF, PRGF, and PDGF injections in managing TMDs. According to the current evidence, PRP injections may provide a greater pain reduction compared to placebo injections in temporomandibular joint osteoarthritis (TMJ-OA) at both 6 months (moderate level of evidence) and 12 months (moderate level of evidence) following the injection [76]. PRP and PRF exhibited similar short-term efficacies in treating TMDs, while PRF was more advantageous in terms of long-term efficacy. Therefore, PRF was recommended for treating TMDs [75]. Moreover, in comparison to saline, PRP exhibits a prolonged duration of pain reduction and augmentation of MMO. Nevertheless, further standardized RCTs are imperative to address the discrepancies in preparation protocols and study heterogeneity across different groups [86].
PRP injections provided adjuvant efficacy to arthrocentesis or arthroscopy in pain reduction for temporomandibular joint osteoarthritis in the long term. Furthermore, PRP injections significantly reduced pain better than HA injections, saline injections, or no injections [79].
In a systematic review assessing the benefits of applying PRP or PRGF injections simultaneously or after arthrocentesis or arthroscopy, eight randomized controlled clinical trials were analyzed. The utilization of intra-articular injections of PRP and plasma rich in growth factors (PRGF) showcased noteworthy distinctions in pain alleviation across three investigations, along with enhanced mandibular function, evidenced in two studies [67].
Based on limited evidence, the intra-articular introduction of mesenchymal stem cells into the TMJ could potentially yield significant effectiveness in diminishing joint pain and enhancing MMO in individuals with TMDs [83].
- Acupuncture
Although some reviews claim that the current evidence on acupuncture is limited regarding treatments for TMDs [87], other evidence supports exactly the opposite, stating that acupuncture promotes an improvement in TMDs and reduces pain [88]. Some authors claimed that some variants of acupuncture, such as that performed with a hot needle, have superior effects compared to traditional acupuncture, ultrasonic therapies, laser acupuncture, and drugs in the treatment of TMDs [57].
Laser acupuncture has also shown promise in relieving the signs and symptoms of TMDs when combined with traditional acupuncture and an occlusal splint [89].
- Botulinum toxin
Several reviews have examined the potential use of botulinum toxin (BTX) for various orofacial pain conditions. For instance, BTX has demonstrated effectiveness in treating refractory myofascial pain related to TMDs and bruxism [94]. However, the evidence regarding the effectiveness of BTX in managing TMDs and bruxism is currently not fully conclusive. Nevertheless, several studies meeting the inclusion criteria have reported promising findings, underscoring the need for further investigation [35,41,91].
- Drugs
Pharmacological agents commonly employed in TMD treatments encompass NSAIDs, opioids, CCS, muscle relaxants, antidepressants, anticonvulsants, and benzodiazepines [28,47,62,69,82,84,85,98,99,100,101,102]. Regarding pain management in TMDs, some evidence suggests that NSAIDs can be considered as an initial approach for alleviating joint and muscle pain in TMD patients [99,100]. Although some authors have stated that depending on the origin of the pain associated with TMDs, the pharmacological choice is different. For TMDs of muscular origin, the best results were obtained with BTX-A, granisetron, PRP, and muscle relaxants, while for TMDs of a joint nature, the most effective treatments were NSAIDs, CCS, HA, and dextrose [82].
- Laser and TENS
Multiple systematic reviews have indicated that LLLT is an effective method for pain relief and improvement of functional outcomes in patients with TMDs, including both artrogenous and myogenous conditions [104,107,111,112]. While TENS leads to decreased electrical muscle activity in the masticatory muscles, a reduced masseter muscle thickness, enhanced functionality and comfort in daily activities, and alleviated pain linked to temporomandibular disorders (TMDs), the scientific evidence supporting these effects appears to be of moderate quality [109,110]. The findings of the meta-analysis revealed that LLLT exhibited superior short-term effectiveness compared to TENS in addressing TMD pain. Enhanced outcomes can be attained with increased wavelengths. Consequently, we advocate for the utilization of LLLT with wavelengths ranging from 910 nm to 1100 nm for treating TMDs [103].
- Oral splints
Occlusal splint therapy has not been proven to provide any additional benefit in TMDs compared to standard modalities [121]. Multiple studies have shown that occlusal splinting alone or combined with other therapeutic modalities is the most effective treatment option for reducing TMD pain in the short term [29,122,123]. Some reviews have compared splinting with other therapeutic modalities and stated that therapeutic exercises have not shown a clear superiority over occlusal splints for the treatment of painful TMDs [121], and that the use of a splint therapy does not improve the effects of arthrocentesis [116]. It is worth noting that positive findings emerge when the Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) are applied, highlighting the need for standardization in diagnosing and managing TMDs [123]. Despite the treatment results of stabilization appliances, the improvements observed may be attributed to a placebo effect [116]. All types of occlusal splints, such as the anterior repositioning splint, hard stabilization splint, soft stabilization splint, mini anterior splint, and prefabricated splint, are likely to be more effective treatments for arthrogenous and myogenous temporomandibular disorders (TMDs) when compared to receiving no treatment (untreated control patients) or using non-occluding splints. Regarding patients primarily experiencing arthrogenous TMDs, limited-quality evidence suggests that the anterior repositioning splint and counseling therapy in conjunction with a hard stabilization splint are the most effective treatments for reducing pain and temporomandibular joint (TMJ) sounds. In cases of mainly myogenous TMDs, there is a very low level of evidence suggesting that mini anterior splints may offer the most effective treatment in reducing subjective pain outcomes [31].
An examination of the impacts of occlusal splints on enhancements in spinal posture among patients with TMDs implies that occlusal splints may represent a non-invasive therapeutic modality for TMD management. Nevertheless, owing to the scarcity of robust studies in this domain, additional investigations employing combined force platform stabilometry and kinematic evaluation of spinal dynamics are imperative to elucidate the influence of occlusal splints on posture [40].
In conclusion, it is important to note that while all these minimally invasive approaches show promise, further research, particularly standardized RCTs, is necessary to establish their efficacy, optimize the techniques, and determine their long-term effects.
Surgical Procedures
Among the 15 articles exploring surgical approaches, 7 examined minimally invasive surgery, while 8 focused on open surgery.
One of the latest studies suggests that arthroscopic surgery should be performed on masses confined to the superior TMJ space, while open arthroplasty is indicated in cases with extra-articular extension. A combination of both treatment methods may be necessary when the lesion extends beyond the medial sulcus of the condyle [131].
A systematic review comparing various surgical techniques, including gap arthroplasty (GA), interpositional gap arthroplasty (IGA), reconstruction arthroplasty (RA), and distraction osteogenesis (DO), revealed that IGA with autogenous materials, along with reconstruction employing autologous grafts or total joint replacement using alloplastic prosthetic implants, demonstrate comparable clinical results in the treatment of ankylosis [132].
Other systematic reviews assessing different total temporomandibular joint prosthesis systems demonstrated significant improvements in both preoperative and postoperative outcomes, with no notable differences observed between the various devices [126,127].
A systematic review comparing minimally invasive procedures with invasive surgical techniques for artrogenous TMJ management revealed lower VAS scores and higher maximum incisal opening (MIO) values after discectomies and discoplasties in the within-group comparison after discectomy [128].
However, the current scientific evidence remains unclear, and invasive surgical procedures should not be regarded as an effective primary treatment modality for arthrogenous temporomandibular disorder TMD management, notwithstanding the lower VAS scores and elevated MIO values noted post-discectomy in contrast to arthroscopy, eminectomy, and discoplasty.
Overall, while there are various surgical options available for TMJ ankylosis and other TMD conditions, it is crucial to carefully consider their use and prioritize less invasive approaches before resorting to surgery.
4. Discussion
This scoping review provides an in-depth analysis of the most recent scientific evidence regarding the therapeutic approaches for temporomandibular disorders (TMDs). Through a thorough examination of the literature, it became evident that these approaches are mainly divided into conservative or non-invasive, minimally invasive, and invasive treatments, with a wide range of specific therapeutic options available within each category.
Chronic pain remains a major concern of TMDs, and its management is a primary focus for healthcare professionals. According to some studies, such pain would appear to be related to individual psychological profiles and the pain application status [134,135]. Biological, psychological, and social factors interact with contextual and environmental stressors, generating painful TMDs and associated symptoms [136]. The existing evidence supports a positive association between work-related stress and temporomandibular disorders (TMDs), highlighting the need for primary prevention interventions [62,137]. Addressing stress in the workplace is crucial to preventing the development or worsening of TMDs. However, advancements in neuroimaging techniques have provided valuable insights into the underlying neuro-pathophysiological mechanisms involved in TMDs. These techniques, such as magnetic resonance imaging (MRI), have improved the understanding of the structural and functional alterations within the temporomandibular joint and surrounding tissues. This improved understanding helps inform treatment decisions and facilitates more targeted interventions [20].
In addition to pain management, subjective sleep quality has emerged as an important consideration in the management of TMDs. Sleep disturbances are frequently experienced by individuals with TMDs and have the potential to worsen their symptoms [15,138,139]. Addressing sleep quality through appropriate interventions, such as sleep hygiene practices or targeted treatments for sleep disorders, can have a positive impact on TMD outcomes.
In agreement with similar studies, the treatment goals for TMD encompass various aspects, including pain control, improved mandibular function, and the restoration of normal daily activities [140,141]. A multidisciplinary approach is often employed, incorporating conservative modalities such as home care regimens (e.g., self-care exercises and relaxation techniques), intraoral appliance therapy (e.g., splints or orthotics), physiotherapy, pharmacotherapy, local anesthetic trigger point injections, and complementary modalities (e.g., acupuncture or low-level laser therapy). These interventions are targeted at mitigating pain, enhancing functionality, and augmenting the overall well-being of these patients. In terms of diagnostic tools, clinical guidelines are frequently employed as initial screening aids for TMDs. These protocols help identify potential TMD cases and determine the need for further diagnostic investigations, such as imaging studies like MRI. However, there remains a lack of standardized diagnostic criteria across studies, leading to inconsistencies in TMD diagnoses. This inconsistency poses challenges when comparing findings and outcomes between different research studies.
Inherent to the design of scoping reviews, our study presents several limitations. As a result, our primary aim was to offer a comprehensive overview rather than an in-depth analysis of the information on TMD management. Furthermore, we did not conducted a risk bias assessment or meta-analysis due to the heterogeneity of the studies. Additionally, by restricting our inclusion criteria to studies published in English and from 2017 onwards, there is a potential risk of excluding significant research that was published before 2017 or in other languages. Furthermore, despite the inclusion of four databases, it may have been prudent to also include Google Scholar to mitigate any biases resulting from missing articles.
Overall, while advancements have been made in understanding and managing TMDs, there is still a need for well-conducted studies that employ established diagnostic parameters and outcome measures. This will contribute to a more comprehensive and reliable body of evidence, allowing for better comparisons and evidence-based guidelines for TMD management. The ongoing efforts to address these research gaps will help improve the care and outcomes for TMD patients in the future.
5. Conclusions
In conclusion, a multidisciplinary strategy is favored over singular therapies.
- Initially, non-invasive methods such as cognitive–behavioral therapy, physical therapy, and exercises should be prioritized. If these approaches are not effective, minimally invasive treatments like arthrocentesis and intra-articular injections may be considered.
- Surgery should be reserved for severe cases, with conservative therapies used in conjunction with invasive procedures for optimal patient outcomes.
- Furthermore, there is a need for standardization and higher-quality research to further advance the field. Clinicians should stay updated on the latest findings and prioritize preventive measures to reduce the chronicity of TMDs.
Author Contributions
Conceptualization, G.M. and N.Z.; methodology, G.M. and N.Z.; software, R.N. and E.M.; data curation, C.S.-F. and A.V.; writing—original draft preparation, G.M. and N.Z.; writing—review and editing, C.S.-F., A.V. and R.N.; visualization, E.M.; supervision, C.S.-F., A.V. and N.Z.; funding acquisition, E.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Acknowledgments
The authors wish to thank the Parma University Library for their assistance in elaborating the search strings and performing the searches using the cited databases.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Care Services; Board on Health Sciences Policy; Committee on Temporomandibular Disorders (TMDs): From Research Discoveries to Clinical Treatment. Temporomandibular Disorders: Priorities for Research and Care; National Academies Press: Washington, DC, USA, 2020. [Google Scholar]
- Valesan, L.F.; Da-Cas, C.D.; Réus, J.C.; Denardin, A.C.S.; Garanhani, R.R.; Bonotto, D.; Januzzi, E.; de Souza, B.D.M. Prevalence of temporomandibular joint disorders: A systematic review and meta-analysis. Clin. Oral. Investig. 2021, 25, 441–453. [Google Scholar] [CrossRef]
- Minervini, G.; Franco, R.; Marrapodi, M.M.; Fiorillo, L.; Cervino, G.; Cicciù, M. Prevalence of temporomandibular disorders in children and adolescents evaluated with Diagnostic Criteria for Temporomandibular Disorders: A systematic review with meta-analysis. J. Oral. Rehabil. 2023, 50, 522–530. [Google Scholar] [CrossRef] [PubMed]
- Bueno, C.H.; Pereira, D.D.; Pattussi, M.P.; Grossi, P.K.; Grossi, M.L. Gender differences in temporomandibular disorders in adult populational studies: A systematic review and meta-analysis. J. Rehabil. 2018, 45, 720–729. [Google Scholar] [CrossRef] [PubMed]
- Shaefer, J.R.; Khawaja, S.N.; Bavia, P.F. Sex, Gender, and Orofacial Pain. Dent. Clin. N. Am. 2018, 62, 665–682. [Google Scholar] [CrossRef]
- Scariot, R.; Corso, P.F.C.L.; Sebastiani, A.M.; Vieira, A.R. The many faces of genetic contributions to temporomandibular joint disorder: An updated review. Orthod. Craniofac. Res. 2018, 21, 186–201. [Google Scholar] [CrossRef] [PubMed]
- Damasceno, Y.S.S.; Espinosa, D.G.; Normando, D. Is the extraction of third molars a risk factor for the temporomandibular disorders? A systematic review. Clin. Oral. Investig. 2020, 24, 3325–3334. [Google Scholar] [CrossRef] [PubMed]
- Al-Moraissi, E.A.; Wolford, L.M.; Perez, D.; Laskin, D.M.; Ellis, E., 3rd. Does Orthognathic Surgery Cause or Cure Temporomandibular Disorders? A Systematic Review and Meta-Analysis. J. Oral. Maxillofac. Surg. 2017, 75, 1835–1847. [Google Scholar] [CrossRef] [PubMed]
- Häggman-Henrikson, B.; Bechara, C.; Pishdari, B.; Visscher, C.M.; Ekberg, E. Impact of Catastrophizing in Patients with Temporomandibular Disorders-A Systematic Review. J. Oral. Facial Pain Headache 2020, 34, 379–397. [Google Scholar] [CrossRef] [PubMed]
- Oliveira Reis, L.; Ribeiro, R.A.; Martins, C.C.; Devito, K.L. Association between bruxism and temporomandibular disorders in children: A systematic review and meta-analysis. Int. J. Paediatr. Dent. 2019, 29, 585–595. [Google Scholar] [CrossRef]
- Pantoja, L.L.Q.; de Toledo, I.P.; Pupo, Y.M.; Porporatti, A.L.; De Luca Canto, G.; Zwir, L.F.; Guerra, E.N.S. Prevalence of degenerative joint disease of the temporomandibular joint: A systematic review. Clin. Oral. Investig. 2019, 23, 2475–2488. [Google Scholar] [CrossRef]
- De La Torre Canales, G.; Câmara-Souza, M.B.; Muñoz Lora, V.R.M.; Guarda-Nardini, L.; Conti, P.C.R.; Rodrigues Garcia, R.M.; Del Bel Cury, A.A.; Manfredini, D. Prevalence of psychosocial impairment in temporomandibular disorder patients: A systematic review. J. Oral. Rehabil. 2018, 45, 881–889. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.Y.; Fan, H.C.; Tung, M.C.; Chang, Y.K. The association between Parkinson’s disease and temporomandibular disorder. PLoS ONE 2019, 14, e0217763. [Google Scholar] [CrossRef] [PubMed]
- Shrivastava, M.; Battaglino, R.; Ye, L. A comprehensive review on biomarkers associated with painful temporomandibular disorders. Int. J. Oral. Sci. 2021, 13, 23. [Google Scholar] [CrossRef]
- Manfredini, D.; Lobbezoo, F. Sleep bruxism and temporomandibular disorders: A scoping review of the literature. J. Dent. 2021, 111, 103711. [Google Scholar] [CrossRef]
- Manfredini, D.; Thomas, D.C.; Lobbezoo, F. Temporomandibular Disorders Within the Context of Sleep Disorders. Dent. Clin. N. Am. 2023, 67, 323–334. [Google Scholar] [CrossRef]
- de Oliveira-Souza, A.I.S.; de O Ferro, J.K.; Barros, M.M.M.B.; Oliveira, D.A. Cervical musculoskeletal disorders in patients with temporomandibular dysfunction: A systematic review and meta-analysis. J. Bodyw. Mov. Ther. 2020, 24, 84–101. [Google Scholar] [CrossRef]
- Ayouni, I.; Chebbi, R.; Hela, Z.; Dhidah, M. Comorbidity between fibromyalgia and temporomandibular disorders: A systematic review. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. 2019, 128, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Réus, J.C.; Polmann, H.; Souza, B.D.M.; Flores-Mir, C.; Gonçalves, D.A.G.; de Queiroz, L.P.; Okeson, J.; De Luca Canto, G. Association between primary headaches and temporomandibular disorders: A systematic review and meta-analysis. J. Am. Dent. Assoc. 2022, 153, 120–131.e6. [Google Scholar] [CrossRef]
- Omidvar, S.; Jafari, Z. Association Between Tinnitus and Temporomandibular Disorders: A Systematic Review and Meta-Analysis. Ann. Otol. Rhinol. Laryngol. 2019, 128, 662–675. [Google Scholar] [CrossRef]
- Bitiniene, D.; Zamaliauskiene, R.; Kubilius, R.; Leketas, M.; Gailius, T.; Smirnovaite, K. Quality of life in patients with temporomandibular disorders. A systematic review. Stomatologija 2018, 20, 3–9. [Google Scholar]
- Pigozzi, L.B.; Pereira, D.D.; Pattussi, M.P.; Moret-Tatay, C.; Irigaray, T.Q.; Weber, J.B.B.; Grossi, P.K.; Grossi, M.L. Quality of life in young and middle age adult temporomandibular disorders patients and asymptomatic subjects: A systematic review and meta-analysis. Health Qual Life Outcomes 2021, 19, 83. [Google Scholar] [CrossRef] [PubMed]
- Greene, C.S.; Manfredini, D. Treating Temporomandibular Disorders in the 21st Century: Can We Finally Eliminate the “Third Pathway”? J. Oral. Facial Pain Headache 2020, 34, 206–216. [Google Scholar] [CrossRef] [PubMed]
- Freddi, G.; Romàn-Pumar, J.L. Evidence-based medicine: What it can and cannot do. Ann. Ist. Super. Sanita 2011, 47, 22–25. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Penlington, C.; Bowes, C.; Taylor, G.; Otemade, A.A.; Waterhouse, P.; Durham, J.; Ohrbach, R. Psychological therapies for temporomandibular disorders (TMDs). Cochrane Database Syst. Rev. 2022, 8, CD013515. [Google Scholar] [CrossRef]
- Thorpe, A.R.D.S.; Haddad, Y.; Hsu, J. A systematic review and meta-analysis of randomized controlled trials comparing arthrocentesis with conservative management for painful temporomandibular joint disorder. Int. J. Oral. Maxillofac. Surg. 2023, 52, 889–896. [Google Scholar] [CrossRef] [PubMed]
- Tournavitis, A.; Sandris, E.; Theocharidou, A.; Slini, T.; Kokoti, M.; Koidis, P.; Tortopidis, D. Effectiveness of conservative therapeutic modalities for temporomandibular disorders-related pain: A systematic review. Acta Odontol. Scand. 2023, 81, 286–297. [Google Scholar] [CrossRef] [PubMed]
- Kelemen, K.; König, J.; Czumbel, M.; Szabó, B.; Hegyi, P.; Gerber, G.; Borbély, J.; Mikulás, K.; Schmidt, P.; Hermann, P. Additional splint therapy has no superiority in myogenic temporomandibular disorders: A systematic review and meta-analysis of randomized controlled trials. J. Prosthodont. Res. 2024, 68, 12–19. [Google Scholar] [CrossRef]
- Al-Moraissi, E.A.; Farea, R.; Qasem, K.A.; Al-Wadeai, M.S.; Al-Sabahi, M.E.; Al-Iryani, G.M. Effectiveness of occlusal splint therapy in the management of temporomandibular disorders: Network meta-analysis of randomized controlled trials. Int. J. Oral. Maxillofac. Surg. 2020, 49, 1042–1056. [Google Scholar] [CrossRef]
- van der Meer, H.A.; Calixtre, L.B.; Engelbert, R.H.H.; Visscher, C.M.; Nijhuis-van der Sanden, M.W.; Speksnijder, C.M. Effects of physical therapy for temporomandibular disorders on headache pain intensity: A systematic review. Musculoskelet. Sci. Pract. 2020, 50, 102277. [Google Scholar] [CrossRef] [PubMed]
- de Melo, L.A.; de Medeiros, A.K.B.; Campos, M.D.F.T.P.; de Resende, C.M.B.M.; Barbosa, G.A.S.; de Almeida, E.O. Manual Therapy in the Treatment of Myofascial Pain Related to Temporomandibular Disorders: A Systematic Review. J. Oral. Facial Pain Headache 2020, 34, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Al-Moraissi, E.A.; Conti, P.C.R.; Alyahya, A.; Alkebsi, K.; Elsharkawy, A.; Christidis, N. The hierarchy of different treatments for myogenous temporomandibular disorders: A systematic review and network meta-analysis of randomized clinical trials. Oral. Maxillofac. Surg. 2022, 26, 519–533. [Google Scholar] [CrossRef] [PubMed]
- Patel, J.; Cardoso, J.A.; Mehta, S. A systematic review of botulinum toxin in the management of patients with temporomandibular disorders and bruxism. Br. Dent. J. 2019, 226, 667–672. [Google Scholar] [CrossRef] [PubMed]
- La Touche, R.; Martínez García, S.; Serrano García, B.; Proy Acosta, A.; Adraos Juárez, D.; Fernández Pérez, J.J.; Angulo-Diaz-Parreno, S.; Cuenca-Martinez, F.; Paris-Alemany, A.; Suso-Marti, L. Effect of Manual Therapy and Therapeutic Exercise Applied to the Cervical Region on Pain and Pressure Pain Sensitivity in Patients with Temporomandibular Disorders: A Systematic Review and Meta-analysis. Pain. Med. 2020, 21, 2373–2384. [Google Scholar] [CrossRef] [PubMed]
- Lee, N.W.; Lee, S.H.; Kim, K.W.; Ha, I.H.; Cho, J.H.; Lee, Y.J. Effectiveness of Chuna (or Tuina) Manual Therapy for Temporomandibular Disorder: A Systematic Review. Altern. Ther. Health Med. 2023, 29, 258–268. [Google Scholar] [PubMed]
- Menéndez-Torre, Á.; Pintado-Zugasti, A.M.; Zaldivar, J.N.C.; García-Bermejo, P.; Gómez-Costa, D.; Molina-Álvarez, M.; Arribas-Romano, A.; Fernández-Carnero, J. Effectiveness of deep dry needling versus manual therapy in the treatment of myofascial temporomandibular disorders: A systematic review and network meta-analysis. Chiropr. Man. Ther. 2023, 31, 46. [Google Scholar] [CrossRef]
- Asquini, G.; Pitance, L.; Michelotti, A.; Falla, D. Effectiveness of manual therapy applied to craniomandibular structures in temporomandibular disorders: A systematic review. J. Oral. Rehabil. 2022, 49, 442–455. [Google Scholar] [CrossRef]
- Ferrillo, M.; Nucci, L.; Giudice, A.; Calafiore, D.; Marotta, N.; Minervini, G.; D’Apuzzo, F.; Ammendolia, A.; Perillo, L.; de Sire, A. Efficacy of conservative approaches on pain relief in patients with temporomandibular joint disorders: A systematic review with network meta-analysis. Cranio 2022, 1–17. [Google Scholar] [CrossRef]
- Herrera-Valencia, A.; Ruiz-Muñoz, M.; Martin-Martin, J.; Cuesta-Vargas, A.; González-Sánchez, M. Efficacy of manual therapy in temporomandibular joint disorders and its medium-and long-term effects on pain and maximum mouth opening: A systematic review and meta-analysis. J. Clin. Med. 2020, 9, 3404. [Google Scholar] [CrossRef]
- Ferrillo, M.; Ammendolia, A.; Paduano, S.; Calafiore, D.; Marotta, N.; Migliario, M.; Fortunato, L.; Giudice, A.; Michelotti, A.; de Sire, A. Efficacy of rehabilitation on reducing pain in muscle-related temporomandibular disorders: A systematic review and meta-analysis of randomized controlled trials. J. Back. Musculoskelet. Rehabil. 2022, 35, 921–936. [Google Scholar] [CrossRef] [PubMed]
- La Touche, R.; Boo-Mallo, T.; Zarzosa-Rodríguez, J.; Paris-Alemany, A.; Cuenca-Martínez, F.; Suso-Martí, L. Manual therapy and exercise in temporomandibular joint disc displacement without reduction. A systematic review. Cranio 2022, 40, 440–450. [Google Scholar] [CrossRef] [PubMed]
- Liberato, F.M.; da Silva, T.V.; Santuzzi, C.H.; de Oliveira, N.F.F.; Nascimento, L.R. Manual Therapy Applied to the Cervial Joint Reduces Pain and Improves Jaw Function in Individuals with Temporomandibular Disorders: A Systematic Review on Manual Therapy for Orofacial Disorders. J. Oral. Facial Pain Headache 2023, 37, 101–111. [Google Scholar] [CrossRef]
- González-Sánchez, B.; García Monterey, P.; Ramírez-Durán, M.D.V.; Garrido-Ardila, E.M.; Rodríguez-Mansilla, J.; Jiménez-Palomares, M. Temporomandibular Joint Dysfunctions: A Systematic Review of Treatment Approaches. J. Clin. Med. 2023, 12, 4156. [Google Scholar] [CrossRef] [PubMed]
- Lam, A.C.; Liddle, L.J.; MacLellan, C.L. The Effect of Upper Cervical Mobilization/Manipulation on Temporomandibular Joint Pain, Maximal Mouth Opening, and Pressure Pain Thresholds: A Systematic Review and Meta-Analysis. Arch. Rehabil. Res. Clin. Transl. 2023, 5, 100242. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Luo, M.; Ma, J.; Tian, Y.; Han, X.; Bai, D. The treatment modalities of masticatory muscle pain a network meta-analysis. Medicine 2019, 98, e17934. [Google Scholar] [CrossRef] [PubMed]
- Al-Moraissi, E.A.; Almaweri, A.A.; Al-Tairi, N.H.; Alkhutari, A.S.; Grillo, R.; Christidis, N. Treatments for painful temporomandibular disc displacement with reduction: A network meta-analysis of randomized clinical trials. Int. J. Oral. Maxillofac. Surg. 2024, 53, 45–56. [Google Scholar] [CrossRef]
- Dinsdale, A.; Costin, B.; Dharamdasani, S.; Page, R.; Purs, N.; Treleaven, J. What conservative interventions improve bite function in those with temporomandibular disorders? A systematic review using self-reported and physical measures. J. Oral. Rehabil. 2022, 49, 456–475. [Google Scholar] [CrossRef]
- Argueta-Figueroa, L.; Flores-Mejía, L.A.; Ávila-Curiel, B.X.; Flores-Ferreyra, B.I.; Torres-Rosas, R. Nonpharmacological Interventions for Pain in Patients with Temporomandibular Joint Disorders: A Systematic Review. Eur. J. Dent. 2022, 16, 500–513. [Google Scholar] [CrossRef]
- Al-Moraissi, E.A.; Wolford, L.M.; Ellis, E., 3rd; Neff, A. The hierarchy of different treatments for arthrogenous temporomandibular disorders: A network meta-analysis of randomized clinical trials. J. Craniomaxillofac. Surg. 2020, 48, 9–23. [Google Scholar] [CrossRef]
- Idáñez-Robles, A.M.; Obrero-Gaitán, E.; Lomas-Vega, R.; Osuna-Pérez, M.C.; Cortés-Pérez, I.; Zagalaz-Anula, N. Exercise therapy improves pain and mouth opening in temporomandibular disorders: A systematic review with meta-analysis. Clin. Rehabil. 2023, 37, 443–461. [Google Scholar] [CrossRef] [PubMed]
- Melis, M.; Di Giosia, M.; Zawawi, K.H. Oral myofunctional therapy for the treatment of temporomandibular disorders: A systematic review. Cranio 2022, 40, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Ávila-Curiel, B.X.; Gómez-Aguirre, J.N.; Gijón-Soriano, A.L.; Acevedo-Mascarúa, A.E.; Argueta-Figueroa, L.; Torres-Rosas, R. Complementary interventions for pain in patients with temporomandibular joint disorders: A systematic review. Int. J. Acupunct. 2020, 14, 151–159. [Google Scholar] [CrossRef]
- Torres-Rosas, R.; Marcela Castro-Gutiérrez, M.E.; Flores-Mejía, L.A.; Torres-Rosas, E.U.; Nieto-García, R.M.; Argueta-Figueroa, L. Ozone for the treatment of temporomandibular joint disorders: A systematic review and meta-analysis. Med. Gas. Res. 2023, 13, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Chęciński, M.; Chęcińska, K.; Nowak, Z.; Sikora, M.; Chlubek, D. Treatment of Mandibular Hypomobility by Injections into the Temporomandibular Joints: A Systematic Review of the Substances Used. J. Clin. Med. 2022, 11, 2305. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.F.; Gao, Z.; Liu, Z.N.; Yang, M.; Zhang, S.; Tan, T.P. Effects of Warm Needle Acupuncture on Temporomandibular Joint Disorders: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Evid. Based Complement. Altern. Med. 2021, 2021, 6868625. [Google Scholar] [CrossRef] [PubMed]
- Guarda-Nardini, L.; De Almeida, A.M.; Manfredini, D. Arthrocentesis of the Temporomandibular Joint: Systematic Review and Clinical Implications of Research Findings. J. Oral Facial Pain Headache 2021, 35, 17–29. [Google Scholar] [CrossRef]
- Hu, Y.; Liu, S.; Fang, F. Arthrocentesis vs. conservative therapy for the management of TMJ disorders: A systematic review and meta-analysis. J. Stomatol. Oral. Maxillofac. Surg. 2023, 124, 101283. [Google Scholar] [CrossRef]
- Tang, Y.; van Bakelen, N.; Gareb, B.; Spijkervet, F. Arthroscopy versus arthrocentesis and versus conservative treatments for temporomandibular joint disorders: A systematic review with meta-analysis and trial sequential analysis. Int. J. Oral. Maxillofac. Surg. 2024, 53, 503–520. [Google Scholar] [CrossRef]
- Nagori, S.A.; Bansal, A.; Jose, A.; Roychoudhury, A. Comparison of outcomes with the single-puncture and double-puncture techniques of arthrocentesis of the temporomandibular joint: An updated systematic review and meta-analysis. J. Oral. Rehabil. 2021, 48, 1056–1065. [Google Scholar] [CrossRef]
- Li, J.; Zhang, Z.; Han, N. Diverse therapies for disc displacement of temporomandibular joint: A systematic review and network meta-analysis. Br. J. Oral. Maxillofac. Surg. 2022, 60, 1012–1022. [Google Scholar] [CrossRef]
- Nogueira, E.F.C.; Lemos, C.A.A.; Vasconcellos, R.J.H.; Moraes, S.L.D.; Vasconcelos, B.C.E.; Pellizzer, E.P. Does arthroscopy cause more complications than arthrocentesis in patients with internal temporomandibular joint disorders? Systematic review and meta-analysis. Br. J. Oral. Maxillofac. Surg. 2021, 59, 1166–1173. [Google Scholar] [CrossRef] [PubMed]
- Nemeth, A.; Gurgel, B.V.; Lowenstein, A.; Juliasse, L.; Siroma, R.S.; Zhu, Z.; Shibli, J.A.; Mourão, C.F. Does Liquid/Injectable Platelet-Rich Fibrin Help in the Arthrocentesis Treatment of Temporomandibular Joint Disorder Compared to Other Infusion Options? A Systematic Review of Randomized Clinical Trials. Bioengineering 2024, 11, 247. [Google Scholar] [CrossRef] [PubMed]
- Goker, F.; Russillo, A.; Taschieri, S.; Giannì, A.B.; Mortellaro, C.; Colletti, L.; Manfredi, B.; Rovati, M.; Biagi, R.; Del Fabbroet, M. Evaluation of Arthrocentesis with hyaluronic acid injections for management of temporomandibular disorders: A systematic review and case series. J. Biol. Regul. Homeost. Agents 2021, 35, 21–35. [Google Scholar] [CrossRef] [PubMed]
- Ulmner, M.; Bjørnland, T.; Rosén, A.; Berge, T.I.; Olsen-Bergem, H.; Lund, B. Evidence for minimally invasive treatment-A systematic review on surgical management of disc displacement. J. Oral. Rehabil. 2024, 5, 1061–1080. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez, I.Q.; Sábado-Bundó, H.; Gay-Escoda, C. Intraarticular injections of platelet rich plasma and plasma rich in growth factors with arthrocenthesis or arthroscopy in the treatment of temporomandibular joint disorders: A systematic review. J. Stomatol. Oral. Maxillofac. Surg. 2022, 123, e327–e335. [Google Scholar] [CrossRef]
- Nagori, S.A.; Jose, A.; Roy Chowdhury, S.K.; Roychoudhury, A. Is splint therapy required after arthrocentesis to improve outcome in the management of temporomandibular joint disorders? A systematic review and meta-analysis. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. 2019, 127, 97–105. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Wu, J.S.; Tang, Y.L.; Tang, Y.J.; Fei, W.; Liang, X.H. Multiple Treatment Meta-Analysis of Intra-Articular Injection for Temporomandibular Osteoarthritis. J. Oral. Maxillofac. Surg. 2020, 78, 373.e1–373.e18. [Google Scholar] [CrossRef] [PubMed]
- Haddad, C.; Zoghbi, A.; El Skaff, E.; Touma, J. Platelet-rich plasma injections for the treatment of temporomandibular joint disorders: A systematic review. J. Oral. Rehabil. 2023, 50, 1330–1339. [Google Scholar] [CrossRef]
- Siewert-Gutowska, M.; Pokrowiecki, R.; Kamiński, A.; Zawadzki, P.; Stopa, Z. State of the Art in Temporomandibular Joint Arthrocentesis—A Systematic Review. J. Clin. Med. 2023, 12, 4439. [Google Scholar] [CrossRef]
- Li, D.T.S.; Wong, N.S.M.; Li, S.K.Y.; McGrath, C.P.; Leung, Y.Y. Timing of arthrocentesis in the management of temporomandibular disorders: An integrative review and meta-analysis. Int. J. Oral. Maxillofac. Surg. 2021, 50, 1078–1088. [Google Scholar] [CrossRef] [PubMed]
- Abrahamsson, H.; Eriksson, L.; Abrahamsson, P.; Häggman-Henrikson, B. Treatment of temporomandibular joint luxation: A systematic literature review. Clin. Oral. Investig. 2020, 24, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Agostini, F.; Ferrillo, M.; Bernetti, A.; Finamore, N.; Mangone, M.; Giudice, A.; Paoloni, M.; de Sire, A. Hyaluronic acid injections for pain relief and functional improvement in patients with temporomandibular disorders: An umbrella review of systematic reviews. J. Oral. Rehabil. 2023, 50, 1518–1534. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Ren, H.; Zhao, S.; Li, Q.; Li, C.; Bao, G.; Kang, H. Comparative effectiveness of hyaluronic acid, platelet-rich plasma, and platelet-rich fibrin in treating temporomandibular disorders: A systematic review and network meta-analysis. Head Face Med. 2023, 19, 39. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Wu, C.; Sun, H.; Zhou, Q. Effect of Platelet-Rich Plasma Injections on Pain Reduction in Patients with Temporomandibular Joint Osteoarthrosis: A Meta-Analysis of Randomized Controlled Trials. J. Oral. Facial Pain Headache 2020, 34, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Quezada, D.L.; López, C.L.; Montini, F.C.; Skarmeta, N.P. Effectiveness of intra-articular infiltration of platelet concentrates for the treatment of painful joint disorders in the temporomandibular joint: A systematic review. Med. Oral. Patol. Oral. Cir. Bucal 2024, 29, 25658. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Zhao, K.; Ye, G.; Yao, X.; Yu, M.; Ouyang, H. Effectiveness of Intra-Articular Injections of Sodium Hyaluronate, Corticosteroids, Platelet-Rich Plasma on Temporomandibular Joint Osteoarthritis: A Systematic Review and Network Meta-Analysis of Randomized Controlled Trials. J. Evid. Based Dent. Pract. 2022, 22, 101720. [Google Scholar] [CrossRef] [PubMed]
- Chung, P.Y.; Lin, M.T.; Chang, H.P. Effectiveness of platelet-rich plasma injection in patients with temporomandibular joint osteoarthritis: A systematic review and meta-analysis of randomized controlled trials. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. 2019, 127, 106–116. [Google Scholar] [CrossRef] [PubMed]
- Liapaki, A.; Thamm, J.R.; Ha, S.; Monteiro, J.L.G.C.; McCain, J.P.; Troulis, M.J.; Guastaldi, F.P.S. Is there a difference in treatment effect of different intra-articular drugs for temporomandibular joint osteoarthritis? A systematic review of randomized controlled trials. Int. J. Oral. Maxillofac. Surg. 2021, 50, 1233–1243. [Google Scholar] [CrossRef]
- Derwich, M.; Mitus-Kenig, M.; Pawlowska, E. Mechanisms of Action and Efficacy of Hyaluronic Acid, Corticosteroids and Platelet-Rich Plasma in the Treatment of Temporomandibular Joint Osteoarthritis-A Systematic Review. Int. J. Mol. Sci. 2021, 22, 7405. [Google Scholar] [CrossRef]
- Christidis, N.; Al-Moraissi, E.A.; Barjandi, G.; Svedenlöf, J.; Jasim, H.; Christidis, M.; Collin, M. Pharmacological Treatments of Temporomandibular Disorders: A Systematic Review Including a Network Meta-Analysis. Drugs 2024, 84, 59–81. [Google Scholar] [CrossRef]
- Chęciński, M.; Chęcińska, K.; Turosz, N.; Kamińska, M.; Nowak, Z.; Sikora, M.; Chlubek, D. Autologous Stem Cells Transplants in the Treatment of Temporomandibular Joints Disorders: A Systematic Review and Meta-Analysis of Clinical Trials. Cells 2022, 11, 2709. [Google Scholar] [CrossRef]
- López, J.P.; Orjuela, M.P.; González, L.V.; Peraza-Labrador, A.J.; Díaz-Baez, D. Comparison of the Clinical Effectiveness of Intra-Articular Injection with Different Substances After TMJ Arthroscopy: A Systematic Review and Meta-Analysis. J. Maxillofac. Oral. Surg. 2024, 23, 261–270. [Google Scholar] [CrossRef]
- Chęciński, M.; Chęcińska, K.; Rąpalska, I.; Turosz, N.; Chlubek, D.; Sikora, M. Autologous Blood Injections in Temporomandibular Hypermobility: A Systematic Review. J. Clin. Med. 2023, 12, 5590. [Google Scholar] [CrossRef]
- Al-Hamed, F.S.; Hijazi, A.; Gao, Q.; Badran, Z.; Tamimi, F. Platelet Concentrate Treatments for Temporomandibular Disorders: A Systematic Review and Meta-analysis. JDR Clin. Trans. Res. 2021, 6, 174–183. [Google Scholar] [CrossRef]
- Di Francesco, F.; Minervini, G.; Siurkel, Y.; Cicciù, M.; Lanza, A. Efficacy of acupuncture and laser acupuncture in temporomandibular disorders: A systematic review and meta-analysis of randomized controlled trials. BMC Oral. Health 2024, 24, 174. [Google Scholar] [CrossRef]
- Park, E.Y.; Cho, J.H.; Lee, S.H.; Kim, K.W.; Ha, I.H.; Lee, Y.J. Is acupuncture an effective treatment for temporomandibular disorder?: A systematic review and meta-analysis of randomized controlled trials. Medicine 2023, 102, e34950. [Google Scholar] [CrossRef]
- Peixoto, K.O.; Abrantes, P.S.; De Carvalho, I.H.G.; De Almeida, E.O.; Barbosa, G.A.S. Temporomandibular disorders and the use of traditional and laser acupuncture: A systematic review. Cranio 2023, 41, 501–507. [Google Scholar] [CrossRef]
- Mohamad, N.; de Oliveira-Souza, A.I.S.; de Castro-Carletti, E.M.; Müggenborg, F.; Dennett, L.; McNeely, M.L.; Armijo-Olivo, S. The effectiveness of different types of acupuncture to reduce symptoms and disability for patients with orofacial pain. A systematic review and meta-analysis. Disabil. Rehabil. 2024, 1–17. [Google Scholar] [CrossRef]
- Thambar, S.; Kulkarni, S.; Armstrong, S.; Nikolarakos, D. Botulinum toxin in the management of temporomandibular disorders: A systematic review. Br. J. Oral. Maxillofac. Surg. 2020, 58, 508–519. [Google Scholar] [CrossRef] [PubMed]
- Machado, D.; Martimbianco, A.L.C.; Bussadori, S.K.; Pacheco, R.L.; Riera, R.; Santos, E.M. Botulinum Toxin Type A for Painful Temporomandibular Disorders: Systematic Review and Meta-Analysis. J. Pain 2020, 21, 281–293. [Google Scholar] [CrossRef] [PubMed]
- Li, K.; Tan, K.; Yacovelli, A.; Bi, W.G. Effect of botulinum toxin type A on muscular temporomandibular disorder: A systematic review and meta-analysis of randomized controlled trials. J. Oral. Rehabil. 2024, 51, 886–897. [Google Scholar] [CrossRef] [PubMed]
- Ramos-Herrada, R.M.; Arriola-Guillén, L.E.; Atoche-Socola, K.J.; Bellini-Pereira, S.A.; Castillo, A.A.D. Effects of botulinum toxin in patients with myofascial pain related to temporomandibular joint disorders: A systematic review. Dent. Med. Probl. 2022, 59, 271–280. [Google Scholar] [CrossRef] [PubMed]
- El-Kahky, A.M.; Hamdy, T.A.H.; El-Tantawy, M.E.S.A.; Askoura, A.M. Meta Analytical Study of the Role of Intramuscular Botulinum A Toxin Injection in the Treatment of Temporomandibular Joint (TMJ) Disorders. Egypt J. Ear Nose Throat Allied Sci. 2022, 23, 1–18. [Google Scholar] [CrossRef]
- Saini, R.S.; Almoyad, M.A.A.; Binduhayyim, R.I.H.; Quadri, S.A.; Gurumurthy, V.; Bavabeedu, S.S.; Kuruniyan, M.S.; Naseef, P.P.; Mosaddad, S.A.; Heboyan, A. The effectiveness of botulinum toxin for record temporomandibular disorders: A systematic review and meta-analysis. PLoS ONE 2024, 19, e0300157. [Google Scholar] [CrossRef] [PubMed]
- Derwich, M.; Górski, B.; Amm, E.; Pawłowska, E. Oral Glucosamine in the Treatment of Temporomandibular Joint Osteoarthritis: A Systematic Review. Int. J. Mol. Sci. 2023, 24, 4925. [Google Scholar] [CrossRef] [PubMed]
- Minervini, G.; Franco, R.; Crimi, S.; Di Blasio, M.; D’Amico, C.; Ronsivalle, V.; Cervino, G.; Bianchi, A.; Cicciu, M. Pharmacological therapy in the management of temporomandibular disorders and orofacial pain: A systematic review and meta-analysis. BMC Oral. Health 2024, 24, 78. [Google Scholar] [CrossRef]
- Kulkarni, S.; Thambar, S.; Arora, H. Evaluating the effectiveness of non-steroidal anti-inflammatory drugs (nsaids)for relief of pain associated with temporomandibular joint disorders: A systematic review. Int. J. Oral. Maxillofac. Surg. 2019, 48, 285. [Google Scholar] [CrossRef] [PubMed]
- Montinaro, F.; Nucci, L.; d’Apuzzo, F.; Perillo, L.; Chiarenza, M.C.; Grassia, V. Oral nonsteroidal anti-inflammatory drugs as treatment of joint and muscle pain in temporomandibular disorders: A systematic review. Cranio 2022, 1–10. [Google Scholar] [CrossRef]
- Srinivasulu, Y.; Wahab, A.; Senthil Murugan, P. Comparison of efficacy of amitryptyline and duloxetine sodium in reduction of pain in temporomandibular joint disorder (Tmd) patients-a systematic review. Int. J. Pharm. Res. 2020, 12, 2315–2325. [Google Scholar] [CrossRef]
- Ruiz-Romero, V.; Toledano-Serrabona, J.; Gay-Escoda, C. Efficacy of the use of chondroitin sulphate and glucosamine for the treatment of temporomandibular joint dysfunction: A systematic review and meta-analysis. Cranio 2022, 1–10. [Google Scholar] [CrossRef]
- Ren, H.; Liu, J.; Liu, Y.; Yu, C.; Bao, G.; Kang, H. Comparative effectiveness of low-level laser therapy with different wavelengths and transcutaneous electric nerve stimulation in the treatment of pain caused by temporomandibular disorders: A systematic review and network meta-analysis. J. Oral. Rehabil. 2022, 49, 138–149. [Google Scholar] [CrossRef]
- Jing, G.; Zhao, Y.; Dong, F.; Zhang, P.; Ren, H.; Liu, J.; Liu, Y.; Yu, C.; Hu, J.; Bao, G.; et al. Effects of different energy density low-level laser therapies for temporomandibular joint disorders patients: A systematic review and network meta-analysis of parallel randomized controlled trials. Lasers Med. Sci. 2021, 36, 1101–1108. [Google Scholar] [CrossRef]
- Máximo, C.F.G.P.; Coêlho, J.F.; Benevides, S.D.; Alves, G.Â.D.S. Effects of low-level laser photobiomodulation on the masticatory function and mandibular movements in adults with temporomandibular disorder: A systematic review with meta-analysis. Codas 2022, 34, e20210138. [Google Scholar] [CrossRef]
- da Silva Mira, P.C.; Biagini, A.C.S.C.F.; Gomes, M.G.; Galo, R.; Corona, S.A.M.; Borsatto, M.C. Laser acupuncture to reduce temporomandibular disorder (TMD) symptoms: Systematic review and meta-analysis. Lasers Med. Sci. 2024, 39, 66. [Google Scholar] [CrossRef]
- Ahmad, S.A.; Hasan, S.; Saeed, S.; Khan, A.; Khan, M. Low-level laser therapy in temporomandibular joint disorders: A systematic review. J. Med. Life 2021, 14, 148–164. [Google Scholar] [CrossRef]
- Fertout, A.; Manière-Ezvan, A.; Lupi, L.; Ehrmann, E. Management of temporomandibular disorders with transcutaneous electrical nerve stimulation: A systematic review. Cranio 2022, 40, 217–228. [Google Scholar] [CrossRef]
- Serrano-Muñoz, D.; Beltran-Alacreu, H.; Martín-Caro Álvarez, D.; Fernández-Pérez, J.J.; Aceituno-Gómez, J.; Arroyo-Fernández, R.; Avendaño-Coy, J. Effectiveness of Different Electrical Stimulation Modalities for Pain and Masticatory Function in Temporomandibular Disorders: A Systematic Review and Meta-Analysis. J. Pain. 2023, 24, 946–956. [Google Scholar] [CrossRef]
- de Castro-Carletti, E.M.; Müggenborg, F.; Dennett, L.; de Oliveira-Souza, A.I.S.; Mohamad, N.; Pertille, A.; Rodrigues-Bigaton, D.; Armijo-Olivo, S. Effectiveness of electrotherapy for the treatment of orofacial pain: A systematic review and meta-analysis. Clin. Rehabil. 2023, 37, 891–926. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Zhu, J.; Zheng, B.; Liu, J.; Wu, Z. Effectiveness of low-level gallium aluminium arsenide laser therapy for temporomandibular disorder with myofascial pain A systemic review and meta-analysis. Medicine 2021, 100, e28015. [Google Scholar] [CrossRef] [PubMed]
- Zwiri, A.; Alrawashdeh, M.A.; Khan, M.; Ahmad, W.M.A.W.; Kassim, N.K.; Ahmed Asif, J.; Phaik, K.S.; Husein, A.; Ab-Ghani, Z. Effectiveness of the Laser Application in Temporomandibular Joint Disorder: A Systematic Review of 1172 Patients. Pain Res. Manag. 2020, 2020, 5971032. [Google Scholar] [CrossRef]
- Zhang, Y.; Qian, Y.; Huo, K.; Liu, J.; Huang, X.; Bao, J. Efficacy of laser therapy for temporomandibular disorders: A systematic review and meta-analysis. Complement. Ther. Med. 2023, 74, 102945. [Google Scholar] [CrossRef]
- de França, A.M.P.; Gonçalves Borges, A.; Boff Daitx, R.; Ferrer, R.M.; Baptista Dohnert, M.; Durigan, J.L.Q. Photobiomodulation in temporomandibular dysfunction: A systematic review. Muscles Ligaments Tendons J. 2021, 11, 463–474. [Google Scholar] [CrossRef]
- Farshidfar, N.; Farzinnia, G.; Samiraninezhad, N.; Assar, S.; Firoozi, P.; Rezazadeh, F.; Hakimiha, N. The Effect of Photobiomodulation on Temporomandibular Pain and Functions in Patients With Temporomandibular Disorders: An Updated Systematic Review of the Current Randomized Controlled Trials. J. Lasers Med. Sci. 2023, 14, e24. [Google Scholar] [CrossRef]
- Alkhutari, A.S.; Alyahya, A.; Rodrigues Conti, P.C.; Christidis, N.; Al-Moraissi, E.A. Is the therapeutic effect of occlusal stabilization appliances more than just placebo effect in the management of painful temporomandibular disorders? A network meta-analysis of randomized clinical trials. J. Prosthet. Dent. 2021, 126, 24–32. [Google Scholar] [CrossRef]
- Muresanu, S.A.; Hedesiu, M.; Dinu, C.; Roman, R.; Almasan, O. Digital occlusal splints for temporomandibular joint disorders: A systematic review. Rom. J. Stomatol. 2022, 68, 97–105. [Google Scholar] [CrossRef]
- Michiels, S.; Nieste, E.; Van de Heyning, P.; Braem, M.; Visscher, C.; Topsakal, V.; Gilles, A.; Jacquemin, L.; De Hertogh, W. Does conservative temporomandibular therapy affect tinnitus complaints? A systematic review. J. Orofac. Pain. 2019, 33, 308–317. [Google Scholar] [CrossRef]
- Hidalgo Ordoñez, S.; Mora Rojas, M.; Velásquez Ron, B. Effect of occlusal splints on temporomandibular dysfunctions: Systematic review. Av. Odontoestomatol. 2021, 37, 67–77. [Google Scholar] [CrossRef]
- Maheshwari, K.; Srinivasan, R.; Singh, B.P.; Tiwari, B.; Kirubakaran, R. Effectiveness of anterior repositioning splint versus other occlusal splints in the management of temporomandibular joint disc displacement with reduction: A meta-analysis. J. Indian. Prosthodont. Soc. 2024, 24, 15–24. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Xu, L.; Wu, D.; Yu, C.; Fan, S.; Cai, B. Effectiveness of exercise therapy versus occlusal splint therapy for the treatment of painful temporomandibular disorders: A systematic review and meta-analysis. Ann. Palliat. Med. 2021, 10, 6122–6132. [Google Scholar] [CrossRef] [PubMed]
- Honnef, L.R.; Pauletto, P.; Conti Réus, J.; Massignan, C.; Souza, B.D.M.D.; Michelotti, A.; Flores-Mir, C.; De Luca Canto, G. Effects of stabilization splints on the signs and symptoms of temporomandibular disorders of muscular origin: A systematic review. Cranio 2022, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.H.; He, K.X.; Lin, C.J.; Liu, X.D.; Wu, L.; Chen, J.; Rausch-Fan, X. Efficacy of occlusal splints in the treatment of temporomandibular disorders: A systematic review of randomized controlled trials. Acta Odontol. Scand. 2020, 78, 580–589. [Google Scholar] [CrossRef]
- Fouda, A.A.H. No evidence on the effectiveness of oral splints for the management of temporomandibular joint dysfunction pain in both short and long-term follow-up systematic reviews and meta-analysis studies. J. Korean Assoc. Oral. Maxillofac. Surg. 2020, 46, 87–98. [Google Scholar] [CrossRef] [PubMed]
- Riley, P.; Glenny, A.M.; Worthington, H.V.; Jacobsen, E.; Robertson, C.; Durham, J.; Davies, S.; Petersen, H.; Boyers, D. Oral splints for patients with temporomandibular disorders or bruxism: A systematic review and economic evaluation. Health Technol. Assess. 2020, 24, 1–224. [Google Scholar] [CrossRef] [PubMed]
- Lima, F.G.G.P.; Rios, L.G.C.; Paranhos, L.R.; Vieira, W.A.; Zanetta-Barbosa, D. Survival of temporomandibular total joint replacement: A systematic review and meta-analysis. J. Oral. Rehabil. 2024, 51, 775–784. [Google Scholar] [CrossRef]
- Yaseen, M.; Abdulqader, D.; Audi, K.; Ng, M.; Audi, S.; Vaderhobli, R.M. Temporomandibular Total Joint Replacement Implant Devices: A Systematic Review of Their Outcomes. J. Long-Term Eff. Med. Implants 2021, 31, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Rodhen, R.M.; de Holanda, T.A.; Barbon, F.J.; de Oliveira da Rosa, W.L.; Boscato, N. Invasive surgical procedures for the management of internal derangement of the temporomandibular joint: A systematic review and meta-analysis regarding the effects on pain and jaw mobility. Clin. Oral. Investig. 2022, 26, 3429–3446. [Google Scholar] [CrossRef] [PubMed]
- López, J.P.; Orjuela, M.P.; Díaz-Baez, D.; González, L.V. Comparison of the TMJ arthroscopy discopexy techniques: A systematic review and meta-analysis. J. Craniomaxillofac. Surg. 2024, 52, 558–564. [Google Scholar] [CrossRef] [PubMed]
- Marlière, D.A.A.; Vicentin Calori, M.J.A.; Medeiros, Y.D.L.; Santiago, R.C.; Strujak, G.; Asprino, L. Clinical outcomes of the discopexy using suture anchors for repositioning disc displacement in temporomandibular joints: Systematic review and meta-analysis. J. Craniomaxillofac. Surg. 2023, 51, 475–484. [Google Scholar] [CrossRef]
- Gonzalez, L.V.; López, J.P.; Orjuela, M.P.; Mejía, M.; Gallo-Orjuela, D.M.; Granizo López, R.M. Diagnosis and management of temporomandibular joint synovial chondromatosis: A systematic review. J. CranioMaxillofac. Surg. 2023, 51, 551–559. [Google Scholar] [CrossRef]
- Mittal, N.; Goyal, M.; Sardana, D.; Dua, J.S. Outcomes of surgical management of TMJ ankylosis: A systematic review and meta-analysis. J. CranioMaxillofac. Surg. 2019, 47, 1120–1133. [Google Scholar] [CrossRef] [PubMed]
- Askar, H.; Aronovich, S.; Christensen, B.J.; McCain, J.; Hakim, M. Is Arthroscopic Disk Repositioning Equally Efficacious to Open Disk Repositioning? A Systematic Review. J. Oral. Maxillofac. Surg. 2021, 79, 2030–2041.e2. [Google Scholar] [CrossRef] [PubMed]
- Slade, G.D.; Fillingim, R.B.; Sanders, A.E.; Bair, E.; Greenspan, J.D.; Ohrbach, R.; Dubner, R.; Diatchenko, L.; Smith, S.B.; Knott, C.; et al. Summary of findings from the OPPERA prospective cohort study of incidence of first-onset temporomandibular disorder: Implications and future directions. J. Pain. 2013, 14 (Suppl. S12), T116–T124. [Google Scholar] [CrossRef] [PubMed]
- Maixner, W.; Diatchenko, L.; Dubner, R.; Fillingim, R.B.; Greenspan, J.D.; Knott, C.; Ohrbach, R.; Weir, B.; Slade, G.D. Orofacial pain prospective evaluation and risk assessment study—The OPPERA study. J. Pain. 2011, 12 (Suppl. S11), T4–T11.e2. [Google Scholar] [CrossRef] [PubMed]
- Suvinen, T.I.; Reade, P.C.; Kemppainen, P.; Könönen, M.; Dworkin, S.F. Review of aetiological concepts of temporomandibular pain disorders: Towards a biopsychosocial model for integration of physical disorder factors with psychological and psychosocial illness impact factors. Eur. J. Pain 2005, 9, 613–633. [Google Scholar] [CrossRef]
- Aranha, R.L.B.; Martins, R.C.; de Aguilar, D.R.; Moreno-Drada, J.A.; Sohn, W.; Martins, C.C.; de Abreu, M.H.N.G. Association between Stress at Work and Temporomandibular Disorders: A Systematic Review. Biomed. Res. Int. 2021, 2021, 2055513. [Google Scholar] [CrossRef] [PubMed]
- Dreweck, F.D.S.; Soares, S.; Duarte, J.; Conti, P.C.R.; De Luca Canto, G.; Luís Porporatti, A. Association between painful temporomandibular disorders and sleep quality: A systematic review. J. Oral. Rehabil. 2020, 47, 1041–1051. [Google Scholar] [CrossRef] [PubMed]
- Roithmann, C.C.; Silva, C.A.G.D.; Pattussi, M.P.; Grossi, M.L. Subjective sleep quality and temporomandibular disorders: Systematic literature review and meta-analysis. J. Oral. Rehabil. 2021, 48, 1380–1394. [Google Scholar] [CrossRef]
- Kapos, F.P.; Exposto, F.G.; Oyarzo, J.F.; Durham, J. Temporomandibular disorders: A review of current concepts in aetiology, diagnosis and management. Oral. Surg. 2020, 13, 321–334. [Google Scholar] [CrossRef]
- Chan, N.H.Y.; Ip, C.K.; Li, D.T.S.; Leung, Y.Y. Diagnosis and Treatment of Myogenous Temporomandibular Disorders: A Clinical Update. Diagnostics 2022, 12, 2914. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).