Abstract
With the global trend of population aging becoming increasingly pronounced, the incidence of central nervous system (CNS) disorders continues to rise, posing a significant challenge to public health systems worldwide. Currently, many CNS disorders lack effective treatments, prompting researchers to investigate the therapeutic potential of natural compounds. Urolithin A (UA), a gut microbiota-derived metabolite of ellagitannins and ellagic acid, can cross the blood–brain barrier and exhibits a favorable safety profile. This review summarizes the biosynthesis, pharmacokinetic profile, and key biological effects of UA, including its promotion of mitophagy and mitochondrial homeostasis, as well as its anti-inflammatory, antioxidant, anti-senescence, and anti-apoptotic properties. We comprehensively summarize the preclinical evidence demonstrating UA’s therapeutic potential in CNS disorders, such as Alzheimer’s disease, Parkinson’s disease, and stroke. Recent clinical trials involving UA are presented, followed by a thorough analysis of the challenges associated with translating UA-based interventions into clinical practice for CNS disorders. This work aims to support the development of UA-based therapies to improve patient outcomes and address the growing global burden of CNS disorders.
1. Introduction
Central nervous system (CNS) disorders represent a significant global public health challenge. According to the World Health Organization, approximately one in five individuals worldwide is affected by a CNS condition [1]. Neurodegenerative diseases, such as Alzheimer’s disease (AD) and Parkinson’s disease (PD), exhibit a marked increase in prevalence with advancing age, a trend that aligns with the ongoing global aging population [2,3]. For instance, PD alone affects up to 3% of individuals over 65, with projections indicating a 50% rise in its prevalence by 2030 [4]. Stroke, recognized as the second leading cause of death and the foremost contributor to disability globally, continues to rise in incidence, particularly in developing countries [5,6]. Additionally, traumatic CNS injuries impact millions annually [7], while CNS tumors accounted for approximately 7.7 million disability-adjusted life years in 2016, according to the Global Burden of Disease Study [8].
Urolithin A (UA) is a natural compound produced through a multi-step metabolic process by gut microbiota, derived from dietary precursors such as ellagitannins (ETs) and ellagic acid (EA). These polyphenols are abundant in foods like pomegranates, berries (such as blackberries, raspberries, and strawberries), nuts, tropical fruits (such as Camu-Camu and jaboticaba), and tea [9,10]. Chemically, UA belongs to the dibenzo[b,d]pyran-6-one derivatives, characterized by a distinct hydroxyl substitution pattern that underpins its unique metabolic properties and biological effects [11]. Extensive preclinical research highlights UA’s diverse biological effects, including anti-inflammatory, antioxidant, anti-senescence, anti-apoptotic, and promoting mitophagy [4,9,12,13]. Randomized clinical studies further validate UA’s ability to upregulate proteins linked to mitophagy and oxidative phosphorylation (OXPHOS) in muscle tissue while reducing plasma inflammatory markers, such as C-reactive protein (CRP) [14,15]. Regarding safety, clinical trials have confirmed UA’s tolerability at doses up to 1000 mg daily, with no serious adverse effects reported in interventions lasting up to four months. Notably, UA is the first compound shown in human trials to induce mitochondrial-related gene expression without significant side effects [14,15,16]. The U.S. FDA has granted UA Generally Recognized as Safe status (GRN No. 791) as a food additive.
UA has been extensively investigated in preclinical models of various CNS disorders. This review systematically integrates preclinical evidence for UA’s therapeutic potential in CNS disorders and elucidates its biosynthesis, pharmacokinetic properties, key bioactivities, and recent clinical trials involving UA. More importantly, this review provides an in-depth analysis of the challenges encountered in the clinical translation of UA for the treatment of CNS disorders.
2. Biosynthesis and Pharmacokinetics of Urolithin A
Following ingestion of ETs-rich food, ETs are hydrolyzed to water-insoluble EA in the stomach and small intestine. Subsequently, EA undergoes stepwise metabolism by gut microbiota in the colon to produce UA, which is then absorbed into systemic circulation (Figure 1). Specifically, the process begins with EA losing a lactone ring to form pentahydroxy-urolithins (urolithin M5). Pentahydroxy-urolithins then lose one hydroxyl group to generate tetrahydroxy-urolithins (urolithin D, urolithin E, urolithin M6, and urolithin M6R), which are subsequently metabolized into trihydroxy-urolithins (urolithin C, urolithin CR, urolithin M7, and urolithin M7R). Through a dihydroxylation reaction, dihydroxy-urolithins are formed, including UA, as well as iso-urolithin A and urolithin AR. Dihydroxy-urolithins can also undergo further metabolism to become monohydroxy-urolithins (urolithin B) [4,17,18]. Enterocloster species and Gordonibacter species participate in the metabolic conversion of EA to UA in humans [11,19]. Due to differences in gut microbiota composition across populations, there is significant variation in UA production through microbial metabolism, which is influenced by factors such as age and diet [20]. Based on urolithin production patterns, three urolithin metabotypes associated with three different urolithin production profiles have been described in human populations: UM-A (producing only UA), UM-B (producing UA, iso-urolithin A and urolithin B), and UM-0 (unable to produce UA) [17]. Studies have shown that UM-0 accounts for approximately 10% in healthy Chinese populations, 6.8–25.0% in healthy Spanish populations, 26.3% in healthy Brazilian populations, and up to 60% in healthy American populations [20,21,22,23].
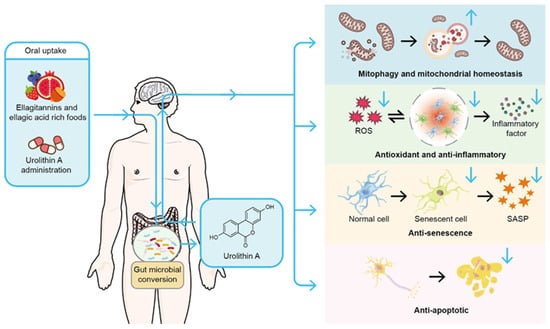
Figure 1.
Biosynthesis and biological effects of Urolithin A. Urolithin A (UA) originates from dietary ellagitannins and ellagic acid, polyphenolic compounds prevalent in pomegranates, berries (such as blackberries, raspberries, and strawberries), and nuts. These precursors undergo stepwise metabolism by gut microbiota, resulting in the production of UA. Following its formation, UA is absorbed by the intestine, enters the bloodstream, and can cross the blood–brain barrier. Alternatively, UA may be directly ingested through oral administration. Once in the body, UA exhibits a range of biological activities, including the promotion of mitophagy and maintenance of mitochondrial homeostasis, as well as anti-inflammatory, antioxidant, anti-senescence, and anti-apoptotic effects. Blue ↑: indicates activation; blue ↓: indicates inhibition.
Nevertheless, direct oral UA supplementation can overcome insufficient UA production caused by microbiota variations and other factors. A clinical study demonstrated that compared to consuming 240 mL of pomegranate juice rich in natural UA precursor compounds, intake of 500 mg UA supplement provided significantly higher plasma UA levels. Direct UA supplementation provided uniform circulating UA levels across the entire population, addressing the variations in endogenous UA synthesis levels due to individual differences in urolithin metabotypes (ClinicalTrials.gov: NCT04160312) [22].
Once absorbed in the intestine, UA exhibits significantly higher bioavailability than its precursor EA and can be excreted through urine and feces [18]. A portion of urolithin A undergoes further biotransformation in the liver, such as methylation, sulfation, and glucuronidation. Among these, sulfation and glucuronidation are the predominant metabolic pathways [24]. A clinical study showed that following direct oral UA supplementation, free UA and its two major metabolites, UA-glucuronide and UA-sulfate, can be detected in plasma, and the levels of UA-related metabolites are higher than those of free UA. Both free UA and its conjugated metabolites display similar kinetics, reaching peak plasma concentrations 6 h post-d Dosage. The half-lives of free UA and UA-glucuronide are 17–22 h, while that of UA-sulfate is 25–58 h, with no bioaccumulation (ClinicalTrials.gov: NCT02655393) [16]. Regarding tissue distribution, following oral administration of urolithin A in rats, UA was detected in the small intestine, colon, liver, prostate, kidneys, heart, and lungs [25,26]. To date, UA has been detected in various human tissues, including prostate, colon, breast, and skeletal muscle [16,17]. Furthermore, animal studies demonstrate that UA can cross the blood–brain barrier (BBB) in its free form. In rat models, brain UA concentrations reach approximately 10% of plasma levels following pomegranate juice consumption [27]. Mice were administered UA via intraperitoneal injection at a dose of 5 mg/kg. Subsequent mass spectrometry analysis detected free UA in both plasma and perfused brain samples. However, the concentration of UA-related metabolites, such as UA-sulfate, was much lower in brain samples than in plasma. UA-3-glucuronide was detected only in plasma [28].
3. Biological Effects of Urolithin A
3.1. Mitophagy and Mitochondrial Homeostasis
Mitophagy is a selective autophagy process that removes dysfunctional or superfluous mitochondria, thereby precisely regulating their quantity and quality to sustain cellular energy metabolism and homeostasis [29,30]. This mechanism involves multiple signaling pathways and molecules, including the well-characterized phosphatase and tensin homolog-induced putative kinase 1 (PINK1)/E3 ubiquitin-protein ligase parkin (Parkin) pathway. When mitochondria are damaged or dysfunctional, a drop in membrane potential stabilizes PINK1 on the outer mitochondrial membrane, recruiting and activating Parkin [31,32]. Activated Parkin ubiquitinates outer membrane proteins such as mitofusin 2 (MFN2), thereby tagging damaged mitochondria with ubiquitin chains [33]. These modifications recruit selective autophagy receptors such as p62 and optineurin (OPTN), which anchor mitochondria to autophagosomal membranes via associated protein 1 light chain 3 (LC3)-interacting domains, initiating engulfment [34,35]. Beyond the PINK/Parkin pathway, receptors like B-cell leukemia/lymphoma 2/adenovirus E1B 19 kDa interacting protein 3-like protein (BNIP3L) independently mediate mitochondrial clearance under specific conditions, such as during erythrocyte maturation, by directly binding LC3 [36]. Mitochondrial fission also facilitates mitophagy by generating fragmented mitochondria more readily targeted for removal, with dynamin-related protein 1 (DRP1)-mediated fission events cooperating with proteins like B-cell leukemia/lymphoma 2/adenovirus E1B 19kDa protein-interacting protein 3 (BNIP3) to selectively eliminate dysfunctional mitochondria [37,38]. Additionally, the inner membrane protein prohibitin 2 (PHB2) exposes its LC3-binding domain upon membrane potential loss, directly mediating autophagosomal recognition of mitochondria [39]. The entire mitophagy process is orchestrated through multilayered regulatory mechanisms involving mitochondrial dynamics, ubiquitin-proteasome system modifications, and metabolic signal integration, exemplified by reactive oxygen species (ROS). These coordinated processes collectively maintain homeostasis between cellular energy metabolism and damaged mitochondrial clearance [35,40].
Mitochondrial homeostasis relies on the interplay of biogenesis, fusion/fission, and mitophagy. Defects in mitophagy lead to the accumulation of dysfunctional mitochondria, triggering oxidative stress, calcium dysregulation, and energy deficits [41]. This pathological cascade is particularly pronounced in neurodegenerative disorders of the CNS. In AD, impaired mitophagy in the hippocampus and induced pluripotent stem cell-derived neurons contributes to amyloid-β (Aβ) accumulation and tau hyperphosphorylation. Pharmacological enhancement of mitophagy clears Aβ plaques and reverses cognitive deficits [41,42]. Similarly, in PD, abnormal α-synuclein aggregation—a hallmark feature—exhibits bidirectional regulation with mitophagy defects. Pathological α-synuclein suppresses key mitophagy molecules like PINK1, leading to the buildup of defective mitochondria, which in turn release ROS that exacerbate α-synuclein phosphorylation and aggregation [43].
Studies across diverse organisms—cells, C. elegans, mice, and humans—consistently demonstrate that UA significantly influences mitochondrial health by modulating mitophagy (Figure 1). In C. elegans, UA activates the PINK1/Parkin pathway, enhancing mitophagy, improving mitochondrial morphology, extending healthy lifespan, and boosting motor function [12]. In transgenic tau C. elegans models, UA reverses memory deficits linked to tau hyperphosphorylation by enhancing mitophagy and reducing neuroinflammatory markers [41].
In mouse disease models, UA’s role in regulating mitophagy and maintaining mitochondrial homeostasis is well validated. In AD mouse models, UA enhances microglial phagocytosis of Aβ plaques, suppresses neuroinflammation, and reduces tau hyperphosphorylation by restoring mitophagy to eliminate abnormal mitochondria [41]. In doxorubicin-induced cardiomyopathy mice, UA upregulates p62, LC3-II, PINK1, and Parkin expression, restoring impaired mitophagy, mitigating membrane potential loss and ROS accumulation, and alleviating cardiomyocyte apoptosis and mitochondrial dysfunction [44]. In Duchenne muscular dystrophy mice, UA boosts the expression of mitophagy-related proteins (PINK1, Parkin, and BNIP3), restoring muscle stem cell regeneration, improving mitochondrial respiration, and increasing survival rates [45]. Furthermore, in diabetes-associated cognitive impairment models, UA enhances PINK1/Parkin-dependent mitophagy, improving neuronal mitochondrial function and ameliorating cognitive deficits [46].
In human studies, UA’s clinical potential is increasingly evident. Randomized controlled trials in healthy middle-aged and older adults show that oral supplementation with 500–1000 mg of UA significantly improves skeletal muscle endurance and mitochondrial efficiency, reduces plasma inflammatory markers (such as C-reactive protein), and upregulates muscle proteins linked to mitophagy and oxidative phosphorylation [14,15].
These findings collectively highlight UA’s ability to regulate mitophagy and maintain mitochondrial homeostasis across species and disease models. By coordinating mitochondrial quality control networks, UA ameliorates mitochondrial dysfunction in various conditions, laying a foundation for its therapeutic application in CNS disorders.
3.2. Anti-Inflammatory and Antioxidant
The progression of most CNS disorders involves a complex interplay between inflammation and oxidative stress, forming a pathological network [47,48,49,50,51]. Inflammation activates microglia and astrocytes, triggering the release of pro-inflammatory cytokines and ROS. These mediators amplify local oxidative stress and impair mitochondrial function, further increasing free radical production [52]. Conversely, oxidative stress induces lipid peroxidation, DNA damage, and the release of mitochondrial DNA, which activate inflammatory signaling pathways, perpetuating a neuroinflammatory microenvironment [53,54]. This vicious cycle increases BBB permeability, promotes neuronal apoptosis, and disrupts synaptic function, ultimately accelerating CNS disease progression [47]. In AD, inflammation and oxidative stress synergistically drive Aβ accumulation and neuronal damage. Aβ buildup triggers an inflammatory response, activating microglia and exacerbating oxidative stress, which further impairs neuronal function [51]. In stroke, oxidative stress is particularly pronounced during cerebral ischemia-reperfusion injury, causing mitochondrial damage and a cytokine storm that intensifies brain tissue injury [55].
UA exhibits potent anti-inflammatory and antioxidant effects across multiple disease models, acting through diverse pathways (Figure 1). Molecular docking and dynamics simulations reveal a strong interaction between UA and human p38 mitogen-activated protein kinase (MAPK), with a binding energy of -10.1 kcal/mol, comparable to established anti-inflammatory drugs [56]. In lipopolysaccharide (LPS)-stimulated BV-2 microglia, UA suppresses the nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) signaling pathway, reducing the release of inflammatory cytokines such as interleukin 6 (IL-6), IL-1β, and tumor necrosis factor alpha (TNF-α), while also inhibiting the phosphorylation of MAPK and serine/threonine kinase 1 (Akt), thereby halting the inflammatory cascade [57,58,59]. This effect is corroborated in LPS-induced neuroinflammatory mouse models, where UA activates sirtuin 1 (SIRT1)-mediated deacetylation of NF-κB p65, suppressing glial cell activation and the production of pro-inflammatory cytokines (IL-1β, IL-6, and TNF-α), thus preventing neuronal loss and hippocampal synaptic damage [60]. In amyloid precursor protein (APP)/presenilin 1 (PS1) transgenic AD mice, UA enhances brain adenosine 5′-monophosphate-activated protein kinase (AMPK) activation, attenuating NF-κB and MAPK activity, mitigating neuroinflammation, and supporting synaptic recovery [61]. In a renal ischemia-reperfusion injury model, UA activates the p62—kelch-like ECH-associated protein 1 (Keap1)—nuclear factor erythroid 2-related factor 2 (Nrf2) pathway, boosting superoxide dismutase and catalase activity while lowering ROS levels [62]. Similarly, in acetaminophen-induced acute liver injury, UA mitigates glutathione depletion and lipid peroxidation via the Nrf2/antioxidant response element (ARE) pathway, outperforming the clinical standard N-acetylcysteine [63]. In LPS-induced acute lung injury, UA upregulates the Keap1-Nrf2/heme oxygenase 1 (HO-1) pathway to inhibit ferroptosis and reduce lipid peroxide accumulation in lung tissue [64]. A key mechanism underlying UA’s anti-inflammatory and antioxidant effects is its regulation of mitochondrial function. In an osteoarthritis mouse model, UA enhances mitophagy in articular cartilage, reducing cartilage degradation and synovial inflammation [65]. In a sleep deprivation-induced hippocampal inflammation model, UA curbs microglial activation and mitochondrial dysfunction, lowering ROS levels and preserving neuronal morphology [66]. Recent study has revealed that age-related mitochondrial DNA (mtDNA)- cyclic GMP-AMP synthase (cGAS)/stimulator of interferon genes (STING)-mediated inflammation is physiologically upregulated across different species and organs, which can be alleviated by urolithin A-induced mitophagy [28].
3.3. Anti-Senescence
Cellular senescence is an irreversible state of cell cycle arrest characterized by distinct molecular and functional changes, including the loss of proliferative capacity, altered metabolic activity, and the expression of senescence-associated secretory phenotypes (SASP) [67]. In various CNS disorders, senescent brain cells persistently release SASP factors, triggering chronic neuroinflammation and exerting toxic effects on surrounding healthy cells. This process contributes to symptoms such as memory impairment and cognitive decline [28,68,69,70,71,72,73,74,75,76]. Studies suggest that neurons, under conditions of metabolic dysregulation or inflammation, may enter a senescent state by activating signaling pathways such as p21CIP1/WAF1, while secreting SASP factors like IL-1β, IL-6, and TNF-α, which amplify the local inflammatory microenvironment [77]. In AD, senescent microglia in mouse brains enhance NF-κB signaling via H3K18 lactylation, upregulating IL-6 and IL-8 expression, thereby intensifying neuroinflammation and amyloid plaque deposition [69]. Similarly, cellular senescence contributes to PD progression through multiple mechanisms, including SASP secretion, mitochondrial dysfunction, loss of protein homeostasis, and genomic instability [72]. Our research demonstrates that senescent pericytes disrupt the BBB, exacerbating radiation brain injury (RBI) and promoting glioma cell growth and invasion [78]. In glioblastoma mouse models, radiation-induced senescent astrocytes have been shown to enhance tumor growth and invasiveness [79].
UA, a natural metabolite, exhibits anti-senescence properties across diverse disease models through multiple pathways (Figure 1). In human microglia cell line (HMC3), UA synergizes with nicotinamide riboside to modulate immunometabolism, enhancing mitochondrial respiration and reducing DNA damage-induced senescence [80]. In quinolinic acid-induced senescence of C. elegans microglia, UA restores mitophagosome formation, reducing damaged mitochondrial accumulation, alleviating senescent phenotypes, and improving overall health [81]. In skin photoaging studies, UA activates the Nrf2/ARE pathway to mitigate UVA-induced ROS accumulation and regulates the sirtuin 3 (SIRT3)/forkhead box protein O3 (FOXO3)-PINK1/Parkin network to restore mitochondrial function, thereby ameliorating senescence in human fibroblasts [82]. In a replicative senescence model of human skin fibroblasts, UA increases type I collagen expression, reduces matrix metalloproteinase 1 (MMP-1) levels, and activates Nrf2-mediated antioxidant responses, underscoring its anti-aging effects [13]. In senescent human lung fibroblasts, UA enhances circadian rhythm amplitude via SIRT1-mediated Period circadian regulator 2 (PER2) degradation, improving cellular metabolism and mitochondrial function [83]. In auditory cell senescence models, UA treatment reduces H2O2-induced p53 and p21 expression, restores mitochondrial membrane potential and ATP synthesis, and decreases the proportion of senescent cells [84]. In cultured mouse salivary gland organoids, UA activates mitophagy to reduce damaged mitochondrial buildup, mitigating radiation-induced senescence and enhancing salivary gland stem/progenitor cell function [85]. In a cartilage degeneration model, UA treatment of mechanically stressed senescent chondrocytes increases collagen type II and aggrecan expression while lowering MMP-13 and IL-6 levels [86]. In a rat model of intervertebral disc degeneration, UA suppresses TNF-α-mediated MMP-3/13 expression and alleviates oxidative stress-induced nucleus pulposus stem cell senescence via the SIRT1/peroxisome proliferator-activated receptor gamma coactivator 1-alpha (PGC-1α) pathway [87,88]. Furthermore, in corneal epithelial cells, UA inhibits ferroptosis-related marker ferroptosis-related marker acyl-CoA synthetase long-chain family member 4 (ACSL4), upregulates glutathione peroxidase 4 (GPX4), and mitigates hyperosmotic stress-induced senescence [89]. Additionally, research has demonstrated that urolithin A corrects abnormal mitochondrial accumulation in hematopoietic stem cells of aged mice, promotes mitochondrial turnover, and thereby significantly restores energy metabolism and function of hematopoietic stem cells, ultimately enabling aged mice to recover normal hematopoietic capacity [90].
These findings highlight UA’s broad anti-senescence effects across diverse tissue systems, providing a scientific foundation for its potential therapeutic application in CNS disorders linked to cellular senescence.
3.4. Anti-Apoptotic
Apoptosis, a highly conserved form of programmed cell death, involves the systematic dismantling of cellular structures through a caspase-mediated cascade. This process plays an essential role in neural development and homeostasis maintenance [91]. In CNS disorders, dysregulated apoptotic pathways are a central mechanism driving neuronal degeneration. In AD, Aβ activates caspase-6, triggering aberrant tau protein cleavage, which leads to neurofibrillary tangle formation and synaptic dysfunction [92]. Pathological tau also induces aberrant cell cycle re-entry in terminally differentiated neurons, pushing them toward apoptosis [93]. In PD, α-synuclein aggregates activate the NLR family pyrin domain containing 3 (NLRP3) inflammasome, promoting caspase-1-dependent death of dopaminergic neurons [94]. Apoptosis is similarly critical in other CNS conditions. Following spinal cord injury, neuronal and glial apoptosis exacerbates inflammation and functional deficits during secondary injury phases; inhibiting caspase-3 activity or modulating B-cell lymphoma 2 (Bcl-2) family proteins markedly reduces neuronal loss and supports recovery [95,96]. In ischemic stroke models, apoptosis not only causes direct neuronal death in the infarct core but also amplifies damage in the surrounding penumbra by releasing pro-inflammatory factors [97].
UA demonstrates potent anti-apoptotic effects across diverse disease models (Figure 1). In AD studies using APP/PS1 mice, UA reduces Aβ deposition and mitigates neuronal apoptosis by downregulating tau phosphorylation and the expression of APP-related enzymes, ultimately improving cognitive function [61]. In a controlled cortical impact model of traumatic brain injury, UA suppresses the phosphatidylinositol 3-kinase (PI3K)/Akt/mammalian target of rapamycin (mTOR) and Akt/IκB kinase (IKK)/NF-κB signaling pathways, reducing neuronal apoptosis while enhancing BBB integrity and neurological outcomes [98]. In a middle cerebral artery occlusion model, UA treatment lowers Bcl-2 expression and elevates Bcl-2 associated X protein (Bax) and caspase-3 levels in the hippocampus, attenuating neuronal damage and apoptosis [99]. Beyond CNS disorders, UA’s protective role extends to other systems. In diabetes-related studies, UA activates autophagy to inhibit pancreatic β-cell apoptosis, evidenced by reduced cleaved-caspase-3 and cleaved-caspase-1 expression, an effect reversible by the autophagy inhibitor chloroquine [100]. In a model of severe acute pancreatitis-related cardiac injury, UA restores mitochondrial membrane potential and ATP production in cardiomyocytes, balancing carnitine palmitoyltransferase1-dependent fatty acid oxidation to reduce apoptosis [101]. In intervertebral disc degeneration, UA induces mitophagy via the AMPK pathway, alleviating tert-butyl hydroperoxide (TBHP)-induced mitochondrial dysfunction and intrinsic apoptosis in nucleus pulposus cells, while delaying disc structural damage and extracellular matrix degradation in a rat puncture model [102]. In acute kidney ischemia-reperfusion injury, UA activates the p62-Keap1-Nrf2 pathway to mitigate tubular epithelial cell apoptosis, improving renal function [62]. Similarly, in acetaminophen-induced liver injury, UA activates the Nrf2/ARE pathway to suppress hepatocyte apoptosis, an effect abolished by Nrf2 gene silencing [63].
3.5. Putative Mechanisms of Urolithin A’s Biological Effects
Based on the aforementioned research findings, we summarize the potential molecular mechanisms underlying UA regulation of various biological effects in Figure 2, constructing a mechanistic network. Specifically, UA exerts a series of biological effects through activation of PINK1/Parkin, BNIP3, AMPK, SIRT1, and SIRT3, as well as inhibition of PI3K/Akt and Keap1. Activated PINK1/Parkin, BNIP3, and AMPK can directly mediate mitophagy, clearing dysfunctional mitochondria [44,45,46]. Additionally, UA can indirectly regulate the PINK1/Parkin pathway through SIRT3/FOXO3 to promote mitophagy [82]. The clearance of dysfunctional mitochondria contributes to maintaining mitochondrial homeostasis, thereby reducing mtDNA release and ROS production, diminishing activation of the cGAS/STING pathway and NF-κB pathway, and reducing cellular oxidative stress, which consequently attenuates inflammatory responses [28,57,58,59]. Mitochondrial dysfunction and oxidative stress are closely associated with cellular senescence; clearing damaged mitochondria can alleviate cellular senescence and reduce SASP production [85]. Activated AMPK can inhibit the MAPK and NF-κB pathways, reducing pro-inflammatory factor production [61]. SIRT1 activation and Keap1 expression inhibition promote transcription of downstream antioxidant stress genes through PGC-1α deacetylation and Nrf2/ARE pathway activation, respectively, thereby alleviating cellular oxidative stress [62,63,64]. Furthermore, activated SIRT1 can also inhibit the PI3K/Akt pathway, thus reducing NF-κB pathway activation [60]. Alleviation of oxidative stress and improvement of mitochondrial function can reduce the occurrence of apoptosis [101]. UA can also inhibit the PI3K/Akt pathway, thereby blocking mTOR activation-mediated inhibition of autophagy, ultimately achieving anti-apoptotic effects [98].
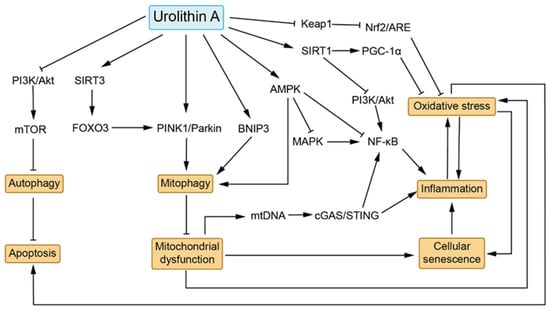
Figure 2.
Hypothesized mechanistic network of Urolithin A. UA exerts biological activities including promotion of mitophagy, antioxidant stress, anti-inflammation, anti-senescence, and anti-apoptosis through mechanisms involving activation of PINK1/Parkin, BNIP3, AMPK, SIRT1, and SIRT3, as well as inhibition of PI3K/Akt and Keap1. Activation of PINK1/Parkin, BNIP3, and AMPK promotes mitophagy, while SIRT3/FOXO3 activation can indirectly regulate mitophagy through PINK1/Parkin pathway activation. Activated AMPK can inhibit MAPK and NF-κB pathway activity, thereby reducing inflammatory responses. SIRT1 activation and Keap1 inhibition suppress cellular oxidative stress through PGC-1α deacetylation and Nrf2/ARE pathway activation, respectively. Additionally, SIRT1 can directly inhibit the PI3K/Akt pathway, thereby suppressing NF-κB pathway activation. Mitophagy, oxidative stress, inflammation, cellular senescence, and apoptosis are closely interconnected. Mitophagy promotes clearance of dysfunctional mitochondria, reducing mtDNA release and ROS production, thereby diminishing cGAS/STING pathway and NF-κB pathway activation as well as oxidative stress. Furthermore, clearance of dysfunctional mitochondria and alleviation of oxidative stress can ameliorate cellular senescence. UA’s ameliorative effects on oxidative stress reduce the occurrence of apoptosis. UA can also promote autophagy by inhibiting PI3K/Akt/mTOR pathway activity, thereby reducing apoptosis. →: indicates activation; ┤: indicates suppression.
4. Preclinical Studies of Urolithin A in CNS Disorders
4.1. Alzheimer’s Disease
AD is a progressive neurodegenerative disorder characterized by cognitive decline and memory impairment. Affecting over 55 million people worldwide, it accounts for 60–80% of all dementia cases, with projections estimating a rise to 139 million by 2050 [103]. The etiology of AD is multifaceted: early-onset familial AD is linked to mutations in the APP, PS1, and presenilin 2 (PS2) genes, while late-onset sporadic AD is strongly associated with the apolipoprotein E4 (ApoE4) genotype and aging [2,104]. Hallmark pathological features include the accumulation of Aβ plaques and neurofibrillary tangles formed by hyperphosphorylated tau protein, both of which increase with age. The progression of AD involves diverse cellular changes, such as mitochondrial dysfunction, oxidative stress, cellular senescence, synaptic damage, and neuroinflammation mediated by microglia [69,103,105,106,107,108]. Clinically, AD manifests primarily through hippocampal and cortical dysfunction, leading to spatial disorientation, language deterioration, and, in some cases, behavioral symptoms like anxiety and social withdrawal [109,110].
UA has demonstrated multifaceted therapeutic potential across various AD models. In SH-SY5Y-APP695 cell line, UA enhances mitochondrial biogenesis by upregulating the expression of Mitochondrial Transcription Factor A (TFAM) and estrogen-related receptor (ESRR) genes, although it does not significantly affect mitophagy or overall mitochondrial function in this model [111]. Further cellular studies show that UA reduces Aβ production in APPSwe-transfected human neural stem cells, while also suppressing neuronal apoptosis through enhanced autophagic flux and SIRT1 activation [112]. In Aβ42-transgenic C. elegans, UA induces mitophagy, reduces Aβ oligomer deposition, and mitigates memory deficits [41]. In mouse models, including APP/PS1, 3xTgAD, and those injected intracerebrally with okadaic acid, long-term UA administration markedly lowers Aβ levels in the hippocampus and cortex, reduces amyloid plaque burden, and improves spatial and learning memory [41,61,105,113,114]. These effects are mediated by enhanced microglial phagocytosis of Aβ and improved autophagy-lysosome function, which facilitates the clearance of intracellular Aβ and phosphorylated tau [41,114]. In the 5xFAD model, UA modulates the small ubiquitin-like modifier 2 (SUMO2) and ADP-ribosylation factor 5 (ARF5) protein network and suppresses overactivation of the anterior basolateral amygdala to ventral CA1 (aBLA-vCA1) circuit, significantly improving social behavior [115]. Additionally, UA activates the AMPK signaling pathway to inhibit beta-site amyloid precursor protein cleaving enzyme 1 (BACE1) and APP expression, reducing Aβ production, and lowers tau phosphorylation by inhibiting dual-specificity tyrosine-phosphorylation regulated kinase 1 (ADYRK1A) kinase activity [61,113]. Across multiple AD models, UA exhibits anti-inflammatory properties by suppressing the synthesis and release of pro-inflammatory cytokines (IL-1β, IL-6, TNF-α) and reducing the activation of microglia and astrocytes, thereby alleviating AD-related symptoms [41,61,105]. Notably, combination therapy enhances UA’s efficacy; in humanized homozygous amyloid beta knockin mice modeling late-onset AD, UA combined with green tea extract (Epigallocatechin gallate) more effectively reduces brain Aβ40 and Aβ42 levels compared to UA alone [106].
Despite UA’s promising results in AD models, most studies employ short-term interventions, leaving the long-term effects of lifelong administration on disease progression unexplored.
4.2. Parkinson’s Disease
PD is a progressive neurodegenerative disorder characterized by bradykinesia, resting tremor, muscle rigidity, and impaired posture and gait. Its pathological hallmarks include the gradual loss of dopaminergic neurons in the substantia nigra and the accumulation of misfolded α-synuclein into Lewy bodies [3,116]. Genetic studies have identified mutations in genes such as synuclein alpha (SNCA) and leucine rich repeat kinase 2 (LRRK2), which impair mitochondrial function, lysosomal autophagy, or α-synuclein metabolism, directly contributing to neuronal damage. Environmental factors, such as exposure to neurotoxins, may exacerbate this process by inducing oxidative stress and neuroinflammation [116]. Disease progression involves multiple mechanisms, including the trans-neuronal spread of α-synuclein, chronic inflammation driven by aberrant microglial activation, and disrupted mitochondrial energy metabolism [3].
Research across various PD models has demonstrated the multi-target neuroprotective effects of UA. In a rotenone-induced rat model, UA were detected in the brain following pomegranate juice intake, correlating with restored dopamine release and reduced α-synuclein levels [27,117]. In mice treated with 6-hydroxydopamine, UA enhanced mitochondrial biogenesis via the SIRT1/PGC-1α signaling pathway, increasing dopaminergic neuron survival in the substantia nigra and alleviating motor deficits [118]. Similarly, in a manganese-induced PD mouse model, UA promoted mitophagy, mitigating dysfunction and improving neurobehavioral outcomes while reducing harmful microglial activation [119]. In 1-Methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP)-treated mice, UA administration elevated striatal dopamine levels and enhanced motor coordination, accompanied by suppression of NLRP3 inflammasome activation in microglia and decreased release of pro-inflammatory cytokines such as IL-1β and TNF-α [120,121]. Furthermore, studies on the cyclin-dependent kinase 5 (CDK5)—ubiquitin-specific peptidase 30 (USP30) signaling pathway revealed that UA restores mitophagy efficiency, counteracting MPTP-induced activation of the mitochondrial antiviral signaling protein (MAVS) inflammatory pathway and offering a specific therapeutic target for toxin-induced PD [121].
4.3. Diabetes-Associated Cognitive Impairment
Diabetes-associated cognitive impairment is a chronic neurological complication closely linked to diabetes, characterized by a progressive decline in cognitive functions, including memory, executive function, and processing speed. Epidemiological studies indicate that type 2 diabetes increases the risk of AD by 1.5 to 2.5 times [122]. In streptozotocin (STZ)-induced diabetic mouse models, UA mitigates cognitive deficits by regulating tissue transglutaminase 2 (TGM2)-dependent endoplasmic reticulum (ER)-mitochondria contacts and calcium homeostasis, thereby reducing Aβ production and tau phosphorylation [123]. In a model of type 2 diabetes induced by a high-fat diet combined with STZ, UA treatment significantly ameliorates cognitive dysfunction. This improvement is accompanied by reduced serum levels of metabolic endotoxemia and pro-inflammatory cytokines, as well as suppression of endoplasmic reticulum (ER) stress and excessive tau phosphorylation in hippocampal neurons [46,124,125]. Furthermore, in HT22 cells, UA inhibits ER stress-mediated apoptosis by downregulating the expression of the ATPase sarcoplasmic/endoplasmic reticulum Ca2+ Transporting 3 (Atp2a3) gene, although overexpression of Atp2a3 abolishes UA’s neuroprotective effects [125].
Beyond these cellular mechanisms, UA’s regulation of diabetes-associated cognitive impairment extends to the gut-brain axis. Studies demonstrate that UA improves systemic inflammation and gut barrier dysfunction by modulating the N-glycan biosynthesis pathway, an effect independent of gut microbiota or short-chain fatty acid metabolism [124]. These multifaceted molecular mechanisms—encompassing mitochondrial homeostasis, ER stress, and inflammatory responses—highlight UA as a promising therapeutic target for intervening in diabetes-associated cognitive impairment.
4.4. Stroke
Stroke is an acute cerebrovascular disorder caused by abnormal blood supply to the brain, primarily encompassing ischemic stroke, resulting from vessel occlusion, and hemorrhagic stroke, stemming from vessel rupture. Its onset is directly linked to cerebral ischemia and hypoxia or hematoma-induced compression of brain tissue triggered by these vascular events [5,126,127].
Preclinical studies highlight the protective potential of UA in stroke models. In mice subjected to middle cerebral artery occlusion, UA treatment significantly reduced infarct volume, improved neurological deficit scores, and ameliorated spatial memory impairments. It also suppressed neuronal apoptosis and mitigated neuroinflammation [99,128]. Mechanistic insights reveal that UA alleviates oxygen-glucose deprivation/reperfusion-induced damage in N2a cells and primary neurons, not via mitophagy, but by reducing ER stress through autophagy activation [128]. In a rat model of subarachnoid hemorrhage, UA modulated autophagy via the AMPK/mTOR pathway, decreasing cortical neuron apoptosis, enhancing BBB integrity, and reducing brain edema and neurological dysfunction [129].
4.5. Traumatic CNS Injuries
Traumatic CNS injuries arise from external mechanical forces impacting the brain or spinal cord, triggering a cascade of pathological events. These include secondary neurodegeneration following initial damage, characterized by neuronal death, uncontrolled inflammation, and blood–brain barrier disruption [50,130,131]. Such injuries often result in permanent disability or loss of motor and sensory functions, affecting millions globally each year. Notably, moderate-to-severe traumatic CNS injuries are linked to an elevated risk of neurodegenerative diseases [7].
In a C57BL/6J mouse model of traumatic brain injury, UA treatment reduced cortical neuron apoptosis, alleviated brain edema, suppressed inflammatory pathways, and improved neurological outcomes [98]. Similarly, in a mouse model of impact-induced spinal cord injury, UA enhanced motor function recovery. Further investigation revealed that UA inhibited pyroptosis following spinal cord injury by promoting autophagy [132]. In the SCI microenvironment, esterase overexpression is a pathological response. A study reported a novel silica-based integrated nanocarrier, prepared by incorporating carbamate-bridged UA into silica nanoparticles, called PEGylated UA-silicon hybrid nanoparticles (PUASi NPs). PUASi NPs can be specifically recognized and cleaved by esterase to release UA, thereby achieving targeted lesion delivery and enhancing UA’s efficacy in treating SCI via its ferroptosis-inhibiting and anti-inflammatory effects [133].
4.6. CNS Infectious Diseases
Initial research on UA in the context of CNS infectious diseases has yielded promising results. In a human neuroblastoma cell model (SK-N-SH cell line) infected with the Enterovirus 71 (EV71) virus, UA significantly inhibited viral replication, demonstrating superior antiviral effects compared to the conventional drug ribavirin. This suggests its potential for application in the treatment of aseptic meningitis [134]. In a mouse model of cerebral toxoplasmosis, UA treatment notably reduced the number and size of cysts in the brain tissue. Behavioral tests further revealed that UA-treated infected mice exhibited enhanced avoidance behavior towards felid scents, indicating an improved ability to perceive predator risks [135]. Although no studies have yet explored the use of UA in bacterial CNS infections, existing research indicates that UA exhibits substantial antimicrobial activity against various bacteria, including methicillin-resistant Staphylococcus aureus, carbapenem-resistant Acinetobacter baumannii, Campylobacter species, Shigella dysenteriae, and Vibrio cholerae [136]. A preclinical study demonstrated that oral UA significantly ameliorated Campylobacter jejuni infection in mice, with localized therapeutic effects in the gut, extending to non-gut tissues and systemic benefits [137].
Overall, while the research on UA in CNS infectious diseases is still limited, further in-depth studies are required to comprehensively assess its effects.
4.7. CNS Tumors
UA has demonstrated broad-spectrum antitumor activity in several cancer models. In studies on solid tumors, including non-small cell lung cancer, breast cancer, gastric cancer, cholangiocarcinoma, and oral squamous cell carcinoma, UA exerts its antitumor effects through mechanisms such as modulation of antitumor immunity, inhibition of epithelial-mesenchymal transition, cell cycle arrest, induction of endoplasmic reticulum stress, and suppression of the Akt/mTOR signaling pathway [138,139,140,141,142,143,144].
In the realm of CNS tumors, research on UA has primarily focused on glioblastoma (GBM), the most common and aggressive primary brain tumor with a notably low survival rate [145]. In in vitro studies using GBM cell lines, UA induced G0/G1 phase cell cycle arrest, upregulated the SIRT1/FOXO1 signaling axis, and inhibited PI3K/Akt pathway activity in a dose-dependent manner, thereby suppressing tumor cell proliferation [146]. Additionally, the aryl hydrocarbon receptor (AhR) is expressed at higher levels in glioma patients compared to healthy individuals, and UA, as a pharmacological antagonist of AhR, mitigated TNF-α-induced expression of vascular cell adhesion molecule 1 (VCAM-1) and programmed death-ligand 1 (PD-L1) in GBM cells, reversing the immune suppression [147]. In a GBM xenograft mouse model, UA administration also significantly inhibited tumor growth [146,147].
4.8. Radiation Brain Injury
RBI is a severe complication that arises in brain tumor patients undergoing radiotherapy, with its pathogenesis closely related to radiation-induced damage to neurons, glial cells, and vascular structures within the CNS [78,79]. In a radiation-induced primary astrocyte model, UA activated the PINK1/Parkin-mediated mitophagy pathway, significantly reducing ROS levels in both cells and mitochondria, restoring mitochondrial morphology and function, and inhibiting the abnormal secretion of vascular endothelial growth factor (VEGF). In co-culture systems, UA treatment alleviated the disruption of endothelial cell tight junction proteins (such as zonula occludens-1 (ZO-1) and claudin) caused by radiation-exposed astrocyte-conditioned medium [148].
4.9. Multiple Sclerosis
Multiple sclerosis (MS) is an autoimmune disorder influenced by genetic and environmental factors, characterized by chronic inflammation, demyelination, and neurodegeneration in the CNS [149]. The experimental autoimmune encephalomyelitis (EAE) model, widely utilized due to its pathological similarities to MS, mimics disease progression effectively. In the MOG35-55-induced EAE mouse model, UA targets the AhR to suppress dendritic cell activation and impair antigen presentation. Additionally, UA reduces the expression of Th17 cell-related genes, such as IL-23a, IL-22, and Ccl2, thereby inhibiting Th17 cell differentiation. This action limits the infiltration of pathogenic T cells into the CNS, alleviating inflammation, demyelination, and clinical symptoms in EAE mice [150].
4.10. Amyotrophic Lateral Sclerosis
Amyotrophic lateral sclerosis (ALS) is a fatal neurodegenerative disease marked by the progressive degeneration of upper and lower motor neurons, leading to muscle weakness, paralysis, and, typically, death from respiratory failure within three years of symptom onset [151,152]. In a zebrafish ALS model with knocked-down C9orf72 and expression of glycine–proline dipeptide repeat proteins, UA has been shown to enhance motor performance [153]. Similarly, in the Cu-exposed SOD1(G93A) transgenic mouse model of ALS, UA activates mitophagy, mitigates mitochondrial dysfunction, and reduces neuroinflammation, resulting in improved gastrocnemius muscle integrity and motor function [154].
4.11. Spinal Muscular Atrophy
Spinal muscular atrophy (SMA) is an autosomal recessive disorder caused by mutations or deletions in the survival of motor neuron 1 (SMN1) gene, leading to the degeneration of spinal cord anterior horn motor neurons and progressive proximal muscle weakness and atrophy [155]. Research using muscle cells derived from SMA patients demonstrates that UA activates AMPK and enhances autophagic flux, promoting mitochondrial biogenesis and mitophagy [156].
Preclinical evidence for UA’s therapeutic application in CNS disorders is summarized below (Table 1).

Table 1.
Experimental settings and effects of UA in preclinical studies of central nervous system disorders.
5. Advances in Clinical Trials of Urolithin A
Although clinical trials targeting UA treatment for CNS disorders have not yet been initiated, multiple clinical trials have demonstrated that UA possesses favorable safety and pharmacokinetic profiles and have validated some of the biological effects observed in in preclinical studies.
Pénélope A. Andreux et al. pioneered the first double-blind, placebo-controlled randomized Phase I clinical trial to evaluate the safety and pharmacokinetic characteristics of UA in elderly subjects in 2016 (ClinicalTrials.gov: NCT02655393) [16]. This study enrolled healthy elderly male and female subjects aged 61 to 85 years. Oral UA demonstrated excellent safety in both single-dose escalation (250–2000 mg) and multiple-dose escalation (250–1000 mg daily for 28 days) cohorts. UA at all tested doses showed good bioavailability in plasma, was unaffected by food intake, and did not accumulate. Additionally, investigators assessed UA distribution in skeletal muscle, detecting UA 8 h after a single oral dose of 2000 mg, primarily in free form, with trace amounts of UA-glucuronide detected in some subjects, while UA-sulfate was undetectable. Biological effect evaluation revealed that in the multiple ascending dose study, subjects in the 500 mg and 1000 mg groups showed dose-dependent reductions in plasma acylcarnitine levels, and skeletal muscle biopsies demonstrated increased mitochondrial genome expression, suggesting UA’s potential to enhance mitochondrial health [16].
Based on UA’s safety and pharmacokinetic data, Sophia Liu et al. conducted a double-blind, placebo-controlled randomized Phase II clinical trial to evaluate UA’s effects on muscle endurance and mitochondrial health in elderly individuals (ClinicalTrials.gov: NCT03283462) [15]. This study enrolled 66 healthy elderly subjects aged 65 to 90 years who received daily oral administration of 1000 mg UA or placebo for 4 months. Results showed that compared to the placebo group, the UA group demonstrated significantly improved muscle endurance in hand and leg skeletal muscles, with significantly reduced plasma levels of mitochondrial health biomarkers (acylcarnitines, ceramides etc.) and inflammatory markers (CRP, etc.) [15]. Anurag Singh et al. conducted a randomized Phase II clinical trial investigating UA’s effects on muscle strength, exercise performance, and mitochondrial health in overweight middle-aged individuals (ClinicalTrials.gov: NCT03464500) [14]. Eighty-eight overweight middle-aged subjects aged 40 to 64 years received daily oral administration of 500 mg UA, 1000 mg UA, or placebo for 4 months. Results indicated that either dose of UA significantly improved leg muscle strength, with subjects in the 1000 mg UA group showing significantly enhanced exercise performance and aerobic endurance. The UA treatment groups exhibited reduced plasma acylcarnitine and CRP levels, with overall reductions in pro-inflammatory cytokines (IFN-γ, IL-1β, TNF-α, etc.). Molecular mechanism studies revealed that muscle RNA sequencing identified significant enrichment of mitochondrial, ribosomal translation, and muscle contraction gene sets in the 500 mg UA group, while the 1000 mg UA group showed no significantly enriched pathways. Proteomic and Western blot analyses demonstrated that UA can affect Parkin-mediated mitophagy markers in skeletal muscle and dose-dependently upregulate mitochondrial tricarboxylic acid cycle and OXPHOS protein levels [14]. Haotian Zhao et al. conducted an 8-week randomized, double-blind, placebo-controlled study on 20 male athletes with resistance training experience. Subjects received daily oral administration of 1000 mg UA, and after 8 weeks, compared to the placebo group, the UA group showed improvements in muscle strength and endurance, with significantly reduced CRP levels [157].
These studies collectively confirm UA’s clinical application potential as a natural mitochondrial health modulator. Multi-phase clinical trials have validated UA’s favorable safety profile and stable pharmacokinetic characteristics, confirming its biological effects in activating mitophagy, improving mitochondrial function, and providing anti-inflammatory benefits. Notably, different doses of UA produce varying effects [14], suggesting that dose selection requires adjustment based on specific pathophysiological requirements. Based on the discovery that UA is primarily distributed in skeletal muscle in free form and exerts mitochondrial health-promoting effects [16], combined with preclinical studies showing that UA primarily crosses the mouse BBB in free form and acts as a direct effector [28], it is speculated that UA may primarily exert its biological effects in free form. Although current research has mainly focused on UA’s effects on the motor system, the established dosing regimen and biological effect mechanisms provide important theoretical foundations and practical references for conducting clinical trials in CNS disorders.
6. Future Perspectives and Challenges
Despite extensive research on UA, considerable challenges remain regarding its potential clinical application for CNS disorders, necessitating more comprehensive investigation.
Although previous studies have demonstrated UA’s broad biological activity and complex molecular regulatory pathways, the specific molecular mechanisms underlying its effects remain incompletely understood [158]. Most preclinical studies on UA for CNS disorders have employed monotherapy without comparing efficacy to existing treatments or exploring combinatorial regimens. We propose that future preclinical research should directly compare UA with standard-of-care therapies, investigate synergistic interactions with other drugs, and leverage UA’s unique advantages in improving mitochondrial function to develop combination strategies. Similarly, current preclinical studies primarily utilize oral administration and intraperitoneal routes, with no comparative studies examining therapeutic differences among these administration methods. Furthermore, while current preclinical research demonstrates that UA can cross the BBB [28], brain concentrations reach only approximately 10% of plasma levels, significantly limiting UA’s therapeutic efficacy [27]. Future research should explore novel drug delivery systems to enhance UA brain delivery efficiency, such as nanoparticle-based carriers or prodrug strategies. For example, the previously mentioned PUASi NPs can be specifically recognized and cleaved by esterases to release UA, achieving targeted delivery to SCI injury sites and enhancing UA’s therapeutic efficacy for SCI through ferroptosis inhibition and anti-inflammatory actions [133]. Successful precedents also exist in other therapeutic areas. The integration of UA-loaded hydrogels with polycaprolactone neural guidance conduits has been achieved. This combination promotes axonal regeneration in rat models of sciatic nerve defects through sustained UA release [159]. In summary, future preclinical research should thoroughly investigate urolithin A’s pharmacological effects, toxicological data, drug delivery, and pharmacokinetic properties, providing crucial references for subsequent clinical trials.
Notably, while UA shows therapeutic potential for CNS disorders, existing evidence remains primarily limited to various cellular and animal models, with no related clinical trials conducted. Due to physiological and pathological differences between animals and humans, these disparities may substantially reduce drug efficacy in actual applications or even produce opposite effects. Therefore, conducting clinical trials of UA treatment for CNS disorders is crucial for advancing UA’s practical application. Additionally, while existing clinical trials have demonstrated UA’s favorable safety profile and pharmacokinetic characteristics and explored dose-response relationships, providing theoretical foundations and practical references for clinical trials in CNS disorders, certain limitations persist. Most of these clinical trials were short-term single-agent studies (28 days to 4 months) conducted in healthy populations, leaving gaps in data regarding potential side effects from long-term UA use or interactions with other medications. Given that CNS disorder treatments, particularly for neurodegenerative diseases, require long-term and combination therapy approaches, understanding UA’s long-term safety profile and drug interaction characteristics is essential. Moreover, current clinical trials demonstrate differential effects across various UA dosages [14], making personalized medicine approaches and reliable dosing strategies for UA clinical application worthy directions for future clinical research.
Recent studies have confirmed a close link between gut microbiota and certain CNS disorders, such as AD and PD [160,161]. An individual’s natural UA production is mainly determined by their gut microbiota [17]. Thus, it is worth exploring whether the differences in UA production, which lead to varying UA levels in humans, are causally related to these CNS disorders. Since clinical studies have shown that directly supplementing UA can resolve the differences in natural UA synthesis levels among individuals [22], understanding the relationship between UA and CNS disorders may help us better use UA to prevent certain CNS disorders.
7. Conclusions
With global aging trends intensifying, the incidence of CNS disorders continues to rise, posing a significant challenge to public health systems worldwide. Many CNS disorders, such as AD, PD, and brain tumors, currently lack effective treatments. UA, a polyphenolic metabolite derived from gut microbiota processing of dietary ETs and EA, has emerged as a promising candidate for CNS disorders treatment or adjunctive therapy due to its multi-target regulatory properties and low toxicity. This review outlines UA’s in vivo synthesis, pharmacokinetic profile, and key biological effects, including mitophagy, anti-inflammatory, antioxidant, anti-senescence, and anti-apoptosis effects. We systematically summarize preclinical evidence demonstrating UA’s therapeutic potential in CNS disorders. Furthermore, we discuss the latest clinical trials and future challenges associated with UA translation, aiming to advance UA research and application in CNS disorders, offering a promising avenue to improve patient outcomes and mitigate the global burden of these diseases.
Author Contributions
Q.Z.: Writing—review and editing, Writing—original draft, Methodology. W.Z.: Writing—review and editing, Validation. X.Y.: Writing—review and editing, Validation. X.P.: Conceptualization, Formal analysis, Supervision. G.H.: Conceptualization, Formal analysis, Supervision. All authors have read and agreed to the published version of the manuscript.
Funding
This work was funded by the National Health Council Foundation of China (grant number WKZX2023CX030002), National Natural Sciences Foundation of China (grant number 82003312 and 82404195), and Hubei Natural Science Foundation (grant number 2025AFB498).
Acknowledgments
The figure in this review was created using pictures from Servier Medical Art (https://smart.servier.com/, accessed on 21 March 2025) and SVG Repo (https://www.svgrepo.com/, accessed on 21 March 2025), licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/, accessed on 21 March 2025). We would like to thank Home for Researchers (https://www.home-for-researchers.com/, accessed on 20 March 2025) for their language polishing service.
Conflicts of Interest
There are no conflicts of interest to declare.
References
- Moreira, R.; Nóbrega, C.; de Almeida, L.P.; Mendonça, L. Brain-targeted drug delivery—Nanovesicles directed to specific brain cells by brain-targeting ligands. J. Nanobiotechnol. 2024, 22, 260. [Google Scholar] [CrossRef] [PubMed]
- Knopman, D.S.; Amieva, H.; Petersen, R.C.; Chételat, G.; Holtzman, D.M.; Hyman, B.T.; Nixon, R.A.; Jones, D.T. Alzheimer disease. Nat. Rev. Dis. Primers 2021, 7, 33. [Google Scholar] [CrossRef]
- Bloem, B.R.; Okun, M.S.; Klein, C. Parkinson’s disease. Lancet 2021, 397, 2284–2303. [Google Scholar] [CrossRef] [PubMed]
- Wojciechowska, O.; Kujawska, M. Urolithin A in Health and Diseases: Prospects for Parkinson’s Disease Management. Antioxidants 2023, 12, 1479. [Google Scholar] [CrossRef] [PubMed]
- Campbell, B.C.V.; de Silva, D.A.; Macleod, M.R.; Coutts, S.B.; Schwamm, L.H.; Davis, S.M.; Donnan, G.A. Ischaemic stroke. Nat. Rev. Dis. Primers 2019, 5, 70. [Google Scholar] [CrossRef]
- Campbell, B.C.V.; Khatri, P. Stroke. Lancet 2020, 396, 129–142. [Google Scholar] [CrossRef]
- Brett, B.L.; Gardner, R.C.; Godbout, J.; Dams-O’Connor, K.; Keene, C.D. Traumatic Brain Injury and Risk of Neurodegenerative Disorder. Biol. Psychiatry 2022, 91, 498–507. [Google Scholar] [CrossRef]
- Patel, A.P.; Fisher, J.L.; Nichols, E.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; Abraha, H.N.; Agius, D.; Alahdab, F.; Alam, T.; et al. Global, regional, and national burden of brain and other CNS cancer, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 376–393. [Google Scholar] [CrossRef]
- D’Amico, D.; Andreux, P.A.; Valdés, P.; Singh, A.; Rinsch, C.; Auwerx, J. Impact of the Natural Compound Urolithin A on Health, Disease, and Aging. Trends Mol. Med. 2021, 27, 687–699. [Google Scholar] [CrossRef]
- Villalgordo, J.M.; Trulli, L.; García-Villalba, R.; García, V.; Althobaiti, Y.; Tomás-Barberán, F.A. Novel Regioselective Synthesis of Urolithin Glucuronides─Human Gut Microbiota Cometabolites of Ellagitannins and Ellagic Acid. J. Agric. Food. Chem. 2022, 70, 5819–5828. [Google Scholar] [CrossRef]
- Selma, M.V.; Beltran, D.; Garcia-Villalba, R.; Espin, J.C.; Tomas-Barberan, F.A. Description of urolithin production capacity from ellagic acid of two human intestinal Gordonibacter species. Food Funct. 2014, 5, 1779–1784. [Google Scholar] [CrossRef] [PubMed]
- Ryu, D.; Mouchiroud, L.; Andreux, P.A.; Katsyuba, E.; Moullan, N.; Nicolet-Dit-Félix, A.A.; Williams, E.G.; Jha, P.; Lo Sasso, G.; Huzard, D.; et al. Urolithin A induces mitophagy and prolongs lifespan in C. elegans and increases muscle function in rodents. Nat. Med. 2016, 22, 879–888. [Google Scholar] [CrossRef]
- Liu, C.; Li, X.-L.; Zhang, Z.-L.; Qiu, L.; Ding, S.-X.; Xue, J.-X.; Zhao, G.-P.; Li, J. Antiaging Effects of Urolithin A on Replicative Senescent Human Skin Fibroblasts. Rejuvenation Res. 2019, 22, 191–200. [Google Scholar] [CrossRef]
- Singh, A.; D’Amico, D.; Andreux, P.A.; Fouassier, A.M.; Blanco-Bose, W.; Evans, M.; Aebischer, P.; Auwerx, J.; Rinsch, C. Urolithin A improves muscle strength, exercise performance, and biomarkers of mitochondrial health in a randomized trial in middle-aged adults. Cell Rep. Med. 2022, 3, 100633. [Google Scholar] [CrossRef]
- Liu, S.; D’Amico, D.; Shankland, E.; Bhayana, S.; Garcia, J.M.; Aebischer, P.; Rinsch, C.; Singh, A.; Marcinek, D.J. Effect of Urolithin A Supplementation on Muscle Endurance and Mitochondrial Health in Older Adults: A Randomized Clinical Trial. JAMA Netw. Open 2022, 5, e2144279. [Google Scholar] [CrossRef]
- Andreux, P.A.; Blanco-Bose, W.; Ryu, D.; Burdet, F.; Ibberson, M.; Aebischer, P.; Auwerx, J.; Singh, A.; Rinsch, C. The mitophagy activator urolithin A is safe and induces a molecular signature of improved mitochondrial and cellular health in humans. Nat. Metab. 2019, 1, 595–603. [Google Scholar] [CrossRef]
- Iglesias-Aguirre, C.E.; García-Villalba, R.; Beltrán, D.; Frutos-Lisón, M.D.; Espín, J.C.; Tomás-Barberán, F.A.; Selma, M.V. Gut Bacteria Involved in Ellagic Acid Metabolism To Yield Human Urolithin Metabotypes Revealed. J. Agric. Food Chem. 2023, 71, 4029–4035. [Google Scholar] [CrossRef]
- Zhang, M.; Cui, S.; Mao, B.; Zhang, Q.; Zhao, J.; Zhang, H.; Tang, X.; Chen, W. Ellagic acid and intestinal microflora metabolite urolithin A: A review on its sources, metabolic distribution, health benefits, and biotransformation. Crit. Rev. Food Sci. Nutr. 2023, 63, 6900–6922. [Google Scholar] [CrossRef] [PubMed]
- Pidgeon, R.; Mitchell, S.; Shamash, M.; Suleiman, L.; Dridi, L.; Maurice, C.F.; Castagner, B. Diet-derived urolithin A is produced by a dehydroxylase encoded by human gut Enterocloster species. Nat. Commun. 2025, 16, 999. [Google Scholar] [CrossRef] [PubMed]
- Inada, K.O.P.; Tomás-Barberán, F.A.; Perrone, D.; Monteiro, M. Metabolism of ellagitannins from jabuticaba (Myrciaria jaboticaba) in normoweight, overweight and obese Brazilians: Unexpected laxative effects influence urolithins urinary excretion and metabotype distribution. J. Funct. Foods 2019, 57, 299–308. [Google Scholar] [CrossRef]
- Xian, W.; Yang, S.; Deng, Y.; Yang, Y.; Chen, C.; Li, W.; Yang, R. Distribution of Urolithins Metabotypes in Healthy Chinese Youth: Difference in Gut Microbiota and Predicted Metabolic Pathways. J. Agric. Food Chem. 2021, 69, 13055–13065. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; D’Amico, D.; Andreux, P.A.; Dunngalvin, G.; Kern, T.; Blanco-Bose, W.; Auwerx, J.; Aebischer, P.; Rinsch, C. Direct supplementation with Urolithin A overcomes limitations of dietary exposure and gut microbiome variability in healthy adults to achieve consistent levels across the population. Eur. J. Clin. Nutr. 2022, 76, 297–308. [Google Scholar] [CrossRef]
- Cortés-Martín, A.; García-Villalba, R.; González-Sarrías, A.; Romo-Vaquero, M.; Loria-Kohen, V.; Ramírez-de-Molina, A.; Tomás-Barberán, F.A.; Selma, M.V.; Espín, J.C. The gut microbiota urolithin metabotypes revisited: The human metabolism of ellagic acid is mainly determined by aging. Food Funct. 2018, 9, 4100–4106. [Google Scholar] [CrossRef] [PubMed]
- Raimundo, A.F.; Ferreira, S.; Tomás-Barberán, F.A.; Santos, C.N.; Menezes, R. Urolithins: Diet-Derived Bioavailable Metabolites to Tackle Diabetes. Nutrients 2021, 13, 4285. [Google Scholar] [CrossRef]
- Savi, M.; Bocchi, L.; Mena, P.; Dall’Asta, M.; Crozier, A.; Brighenti, F.; Stilli, D.; Del Rio, D. In vivo administration of urolithin A and B prevents the occurrence of cardiac dysfunction in streptozotocin-induced diabetic rats. Cardiovasc. Diabetol. 2017, 16, 80. [Google Scholar] [CrossRef]
- González-Sarrías, A.; Giménez-Bastida, J.A.; García-Conesa, M.T.; Gómez-Sánchez, M.B.; García-Talavera, N.V.; Gil-Izquierdo, A.; Sánchez-Alvarez, C.; Fontana-Compiano, L.O.; Morga-Egea, J.P.; Pastor-Quirante, F.A.; et al. Occurrence of urolithins, gut microbiota ellagic acid metabolites and proliferation markers expression response in the human prostate gland upon consumption of walnuts and pomegranate juice. Mol. Nutr. Food Res. 2010, 54, 311–322. [Google Scholar] [CrossRef] [PubMed]
- Kujawska, M.; Jourdes, M.; Kurpik, M.; Szulc, M.; Szaefer, H.; Chmielarz, P.; Kreiner, G.; Krajka-Kuźniak, V.; Mikołajczak, P.Ł.; Teissedre, P.-L.; et al. Neuroprotective Effects of Pomegranate Juice against Parkinson’s Disease and Presence of Ellagitannins-Derived Metabolite-Urolithin A-In the Brain. Int. J. Mol. Sci. 2019, 21, 202. [Google Scholar] [CrossRef]
- Jiménez-Loygorri, J.I.; Villarejo-Zori, B.; Viedma-Poyatos, Á.; Zapata-Muñoz, J.; Benítez-Fernández, R.; Frutos-Lisón, M.D.; Tomás-Barberán, F.A.; Espín, J.C.; Area-Gómez, E.; Gomez-Duran, A.; et al. Mitophagy curtails cytosolic mtDNA-dependent activation of cGAS/STING inflammation during aging. Nat. Commun. 2024, 15, 830. [Google Scholar] [CrossRef]
- Gustafsson, Å.B.; Dorn, G.W. Evolving and Expanding the Roles of Mitophagy as a Homeostatic and Pathogenic Process. Physiol. Rev. 2019, 99, 853–892. [Google Scholar] [CrossRef]
- Palikaras, K.; Lionaki, E.; Tavernarakis, N. Mechanisms of mitophagy in cellular homeostasis, physiology and pathology. Nat. Cell Biol. 2018, 20, 1013–1022. [Google Scholar] [CrossRef]
- Wauer, T.; Simicek, M.; Schubert, A.; Komander, D. Mechanism of phospho-ubiquitin-induced PARKIN activation. Nature 2015, 524, 370–374. [Google Scholar] [CrossRef]
- Gladkova, C.; Maslen, S.L.; Skehel, J.M.; Komander, D. Mechanism of parkin activation by PINK1. Nature 2018, 559, 410–414. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Dorn, G.W. PINK1-Phosphorylated Mitofusin 2 Is a Parkin Receptor for Culling Damaged Mitochondria. Science 2013, 340, 471–475. [Google Scholar] [CrossRef] [PubMed]
- Vargas, J.N.S.; Hamasaki, M.; Kawabata, T.; Youle, R.J.; Yoshimori, T. The mechanisms and roles of selective autophagy in mammals. Nat. Rev. Mol. Cell Biol. 2023, 24, 167–185. [Google Scholar] [CrossRef]
- Wang, S.; Long, H.; Hou, L.; Feng, B.; Ma, Z.; Wu, Y.; Zeng, Y.; Cai, J.; Zhang, D.-W.; Zhao, G. The mitophagy pathway and its implications in human diseases. Signal Transduct. Target. Ther. 2023, 8, 304. [Google Scholar] [CrossRef]
- Youle, R.J.; Narendra, D.P. Mechanisms of mitophagy. Nat. Rev. Mol. Cell Biol. 2011, 12, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Kleele, T.; Rey, T.; Winter, J.; Zaganelli, S.; Mahecic, D.; Perreten Lambert, H.; Ruberto, F.P.; Nemir, M.; Wai, T.; Pedrazzini, T.; et al. Distinct fission signatures predict mitochondrial degradation or biogenesis. Nature 2021, 593, 435–439. [Google Scholar] [CrossRef]
- Lieber, T.; Jeedigunta, S.P.; Palozzi, J.M.; Lehmann, R.; Hurd, T.R. Mitochondrial fragmentation drives selective removal of deleterious mtDNA in the germline. Nature 2019, 570, 380–384. [Google Scholar] [CrossRef]
- Wei, Y.; Chiang, W.-C.; Sumpter, R.; Mishra, P.; Levine, B. Prohibitin 2 Is an Inner Mitochondrial Membrane Mitophagy Receptor. Cell 2017, 168, 224–238.e10. [Google Scholar] [CrossRef]
- Chen, W.; Zhao, H.; Li, Y. Mitochondrial dynamics in health and disease: Mechanisms and potential targets. Signal Transduct. Target. Ther. 2023, 8, 333. [Google Scholar] [CrossRef]
- Fang, E.F.; Hou, Y.; Palikaras, K.; Adriaanse, B.A.; Kerr, J.S.; Yang, B.; Lautrup, S.; Hasan-Olive, M.M.; Caponio, D.; Dan, X.; et al. Mitophagy inhibits amyloid-β and tau pathology and reverses cognitive deficits in models of Alzheimer’s disease. Nat. Neurosci. 2019, 22, 401–412. [Google Scholar] [CrossRef]
- Xie, C.; Zhuang, X.-X.; Niu, Z.; Ai, R.; Lautrup, S.; Zheng, S.; Jiang, Y.; Han, R.; Gupta, T.S.; Cao, S.; et al. Amelioration of Alzheimer’s disease pathology by mitophagy inducers identified via machine learning and a cross-species workflow. Nat. Biomed. Eng. 2022, 6, 76–93. [Google Scholar] [CrossRef] [PubMed]
- Han, R.; Wang, Q.; Xiong, X.; Chen, X.; Tu, Z.; Li, B.; Zhang, F.; Chen, C.; Pan, M.; Xu, T.; et al. Deficiency of parkin causes neurodegeneration and accumulation of pathological α-synuclein in monkey models. J. Clin. Investig. 2024, 134, e179633. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Ma, C.; Mi, K.; Cao, X.; Tan, Y.; Yuan, H.; Ren, J.; Liang, X. Urolithin A attenuates Doxorubicin-induced cardiotoxicity by enhancing PINK1-regulated mitophagy via Ambra1. Chem. Biol. Interact. 2025, 406, 111363. [Google Scholar] [CrossRef] [PubMed]
- Luan, P.; D’Amico, D.; Andreux, P.A.; Laurila, P.-P.; Wohlwend, M.; Li, H.; Imamura de Lima, T.; Place, N.; Rinsch, C.; Zanou, N.; et al. Urolithin A improves muscle function by inducing mitophagy in muscular dystrophy. Sci. Transl. Med. 2021, 13, eabb0319. [Google Scholar] [CrossRef]
- Tang, W.; Yan, C.; He, S.; Du, M.; Cheng, B.; Deng, B.; Zhu, S.; Li, Y.; Wang, Q. Neuron-targeted overexpression of caveolin-1 alleviates diabetes-associated cognitive dysfunction via regulating mitochondrial fission-mitophagy axis. Cell Commun. Signal. 2023, 21, 357. [Google Scholar] [CrossRef]
- Shi, K.; Tian, D.-C.; Li, Z.-G.; Ducruet, A.F.; Lawton, M.T.; Shi, F.-D. Global brain inflammation in stroke. Lancet Neurol. 2019, 18, 1058–1066. [Google Scholar] [CrossRef]
- Hirsch, E.C.; Hunot, S. Neuroinflammation in Parkinson’s disease: A target for neuroprotection? Lancet Neurol. 2009, 8, 382–397. [Google Scholar] [CrossRef]
- Aisen, P.S. The potential of anti-inflammatory drugs for the treatment of Alzheimer’s disease. Lancet Neurol. 2002, 1, 279–284. [Google Scholar] [CrossRef]
- Zrzavy, T.; Schwaiger, C.; Wimmer, I.; Berger, T.; Bauer, J.; Butovsky, O.; Schwab, J.M.; Lassmann, H.; Höftberger, R. Acute and non-resolving inflammation associate with oxidative injury after human spinal cord injury. Brain 2021, 144, 144–161. [Google Scholar] [CrossRef]
- Liu, P.; Zhang, T.; Chen, Q.; Li, C.; Chu, Y.; Guo, Q.; Zhang, Y.; Zhou, W.; Chen, H.; Zhou, Z.; et al. Biomimetic Dendrimer-Peptide Conjugates for Early Multi-Target Therapy of Alzheimer’s Disease by Inflammatory Microenvironment Modulation. Adv. Mater. 2021, 33, e2100746. [Google Scholar] [CrossRef]
- Mendiola, A.S.; Ryu, J.K.; Bardehle, S.; Meyer-Franke, A.; Ang, K.K.-H.; Wilson, C.; Baeten, K.M.; Hanspers, K.; Merlini, M.; Thomas, S.; et al. Transcriptional profiling and therapeutic targeting of oxidative stress in neuroinflammation. Nat. Immunol. 2020, 21, 513–524. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.; Yong, V.W. Oxidized phospholipids as novel mediators of neurodegeneration. Trends Neurosci. 2022, 45, 419–429. [Google Scholar] [CrossRef]
- Ohsawa, I.; Ishikawa, M.; Takahashi, K.; Watanabe, M.; Nishimaki, K.; Yamagata, K.; Katsura, K.-I.; Katayama, Y.; Asoh, S.; Ohta, S. Hydrogen acts as a therapeutic antioxidant by selectively reducing cytotoxic oxygen radicals. Nat. Med. 2007, 13, 688–694. [Google Scholar] [CrossRef]
- Wang, S.; Shi, X.; Xiong, T.; Chen, Q.; Yang, Y.; Chen, W.; Zhang, K.; Nan, Y.; Huang, Q.; Ai, K. Inhibiting Mitochondrial Damage for Efficient Treatment of Cerebral Ischemia-Reperfusion Injury Through Sequential Targeting Nanomedicine of Neuronal Mitochondria in Affected Brain Tissue. Adv. Mater. 2024, 36, e2409529. [Google Scholar] [CrossRef] [PubMed]
- Massaga, C.; Paul, L.; Kwiyukwa, L.P.; Vianney, J.-M.; Chacha, M.; Raymond, J. Computational analysis of Urolithin A as a potential compound for anti-inflammatory, antioxidant, and neurodegenerative pathways. Free Radic. Biol. Med. 2025, 227, 508–520. [Google Scholar] [CrossRef]
- Xu, J.; Yuan, C.; Wang, G.; Luo, J.; Ma, H.; Xu, L.; Mu, Y.; Li, Y.; Seeram, N.P.; Huang, X.; et al. Urolithins Attenuate LPS-Induced Neuroinflammation in BV2Microglia via MAPK, Akt, and NF-κB Signaling Pathways. J. Agric. Food. Chem. 2018, 66, 571–580. [Google Scholar] [CrossRef]
- DaSilva, N.A.; Nahar, P.P.; Ma, H.; Eid, A.; Wei, Z.; Meschwitz, S.; Zawia, N.H.; Slitt, A.L.; Seeram, N.P. Pomegranate ellagitannin-gut microbial-derived metabolites, urolithins, inhibit neuroinflammation in vitro. Nutr. Neurosci. 2019, 22, 185–195. [Google Scholar] [CrossRef] [PubMed]
- Toney, A.M.; Albusharif, M.; Works, D.; Polenz, L.; Schlange, S.; Chaidez, V.; Ramer-Tait, A.E.; Chung, S. Differential Effects of Whole Red Raspberry Polyphenols and Their Gut Metabolite Urolithin A on Neuroinflammation in BV-2 Microglia. Int. J. Environ. Res. Public Health 2020, 18, 68. [Google Scholar] [CrossRef]
- Wu, Y.; Yuan, Q.; Ma, Y.; Zhou, X.; Wang, G.; Wang, S.; Li, S.; Shi, J.; Wang, D. Dietary Intervention with the Gut Microbial Metabolite Urolithin A Attenuates Lipopolysaccharide-Induced Neuroinflammation and Cognitive Deficits via the Sirt1/acetyl-NF-κB Signaling Pathway. Mol. Nutr. Food Res. 2023, 67, e2200401. [Google Scholar] [CrossRef]
- Gong, Z.; Huang, J.; Xu, B.; Ou, Z.; Zhang, L.; Lin, X.; Ye, X.; Kong, X.; Long, D.; Sun, X.; et al. Urolithin A attenuates memory impairment and neuroinflammation in APP/PS1 mice. J. Neuroinflamm. 2019, 16, 62. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Liu, M.; Zhang, Y.; Tian, M.; Chen, P.; Lan, Y.; Zhou, B. Urolithin A alleviates acute kidney injury induced by renal ischemia reperfusion through the p62-Keap1-Nrf2 signaling pathway. Phytother. Res. 2022, 36, 984–995. [Google Scholar] [CrossRef] [PubMed]
- Gao, Z.; Yi, W.; Tang, J.; Sun, Y.; Huang, J.; Lan, T.; Dai, X.; Xu, S.; Jin, Z.-G.; Wu, X. Urolithin A protects against acetaminophen-induced liver injury in mice via sustained activation of Nrf2. Int. J. Biol. Sci. 2022, 18, 2146–2162. [Google Scholar] [CrossRef] [PubMed]
- Lou, L.; Wang, M.; He, J.; Yang, S.; Meng, F.; Wang, S.; Jin, X.; Cai, J.; Cai, C. Urolithin A (UA) attenuates ferroptosis in LPS-induced acute lung injury in mice by upregulating Keap1-Nrf2/HO-1 signaling pathway. Front. Pharmacol. 2023, 14, 1067402. [Google Scholar] [CrossRef]
- D’Amico, D.; Olmer, M.; Fouassier, A.M.; Valdés, P.; Andreux, P.A.; Rinsch, C.; Lotz, M. Urolithin A improves mitochondrial health, reduces cartilage degeneration, and alleviates pain in osteoarthritis. Aging Cell 2022, 21, e13662. [Google Scholar] [CrossRef]
- Misrani, A.; Tabassum, S.; Zhang, Z.-Y.; Tan, S.-H.; Long, C. Urolithin A Prevents Sleep-deprivation-induced Neuroinflammation and Mitochondrial Dysfunction in Young and Aged Mice. Mol. Neurobiol. 2024, 61, 1448–1466. [Google Scholar] [CrossRef]
- Birch, J.; Gil, J. Senescence and the SASP: Many therapeutic avenues. Genes Dev. 2020, 34, 1565–1576. [Google Scholar] [CrossRef]
- Hou, Y.; Wei, Y.; Lautrup, S.; Yang, B.; Wang, Y.; Cordonnier, S.; Mattson, M.P.; Croteau, D.L.; Bohr, V.A. NAD+ supplementation reduces neuroinflammation and cell senescence in a transgenic mouse model of Alzheimer’s disease via cGAS-STING. Proc. Natl. Acad. Sci. USA 2021, 118, e2011226118. [Google Scholar] [CrossRef]
- Wei, L.; Yang, X.; Wang, J.; Wang, Z.; Wang, Q.; Ding, Y.; Yu, A. H3K18 lactylation of senescent microglia potentiates brain aging and Alzheimer’s disease through the NFκB signaling pathway. J. Neuroinflamm. 2023, 20, 208. [Google Scholar] [CrossRef]
- Lim, S.; Kim, T.J.; Kim, Y.-J.; Kim, C.; Ko, S.-B.; Kim, B.-S. Senolytic Therapy for Cerebral Ischemia-Reperfusion Injury. Int. J. Mol. Sci. 2021, 22, 11967. [Google Scholar] [CrossRef]
- Xu, A.; Li, R.; Ren, A.; Jian, H.; Huang, Z.; Zeng, Q.; Wang, B.; Zheng, J.; Chen, X.; Zheng, N.; et al. Regulatory coupling between long noncoding RNAs and senescence in irradiated microglia. J. Neuroinflamm. 2020, 17, 321. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Erb, M.L.; Moore, D.J. Aging, cellular senescence and Parkinson’s disease. J. Parkinsons. Dis. 2025, 15, 239–254. [Google Scholar] [CrossRef]
- Zhang, W.; Sun, H.-S.; Wang, X.; Dumont, A.S.; Liu, Q. Cellular senescence, DNA damage, and neuroinflammation in the aging brain. Trends Neurosci. 2024, 47, 461–474. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Kuca, K.; You, L.; Nepovimova, E.; Heger, Z.; Valko, M.; Adam, V.; Wu, Q.; Jomova, K. The role of cellular senescence in neurodegenerative diseases. Arch. Toxicol. 2024, 98, 2393–2408. [Google Scholar] [CrossRef] [PubMed]
- Sahu, M.R.; Rani, L.; Subba, R.; Mondal, A.C. Cellular senescence in the aging brain: A promising target for neurodegenerative diseases. Mech. Ageing Dev. 2022, 204, 111675. [Google Scholar] [CrossRef]
- Lau, V.; Ramer, L.; Tremblay, M.-È. An aging, pathology burden, and glial senescence build-up hypothesis for late onset Alzheimer’s disease. Nat. Commun. 2023, 14, 1670. [Google Scholar] [CrossRef]
- Melo Dos Santos, L.S.; Trombetta-Lima, M.; Eggen, B.; Demaria, M. Cellular senescence in brain aging and neurodegeneration. Ageing Res. Rev. 2024, 93, 102141. [Google Scholar] [CrossRef]
- Luo, N.; Zhu, W.; Li, X.; Fu, M.; Zhang, Y.; Yang, F.; Zhang, Y.; Chen, Z.; Zhang, Q.; Peng, B.; et al. Defective autophagy of pericytes enhances radiation-induced senescence promoting radiation brain injury. Neuro Oncol. 2024, 26, 2288–2304. [Google Scholar] [CrossRef]
- Fu, M.; Zhang, Y.; Peng, B.; Luo, N.; Zhang, Y.; Zhu, W.; Yang, F.; Chen, Z.; Zhang, Q.; Li, Q.; et al. All-trans retinoic acid inhibits glioblastoma progression and attenuates radiation-induced brain injury. JCI Insight 2024, 9, e179530. [Google Scholar] [CrossRef]
- Madsen, H.B.; Navarro, C.; Gasparini, E.; Park, J.-H.; Li, Z.; Croteau, D.L.; Bohr, V.A. Urolithin A and nicotinamide riboside differentially regulate innate immune defenses and metabolism in human microglial cells. Front. Aging Neurosci. 2024, 16, 1503336. [Google Scholar] [CrossRef]
- Dongol, A.; Chen, X.; Zheng, P.; Seyhan, Z.B.; Huang, X.-F. Quinolinic acid impairs mitophagy promoting microglia senescence and poor healthspan in C. elegans: A mechanism of impaired aging process. Biol. Direct 2023, 18, 86. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Yan, F.; Xu, Z.; Chen, Q.; Ren, J.; Wang, Q.; Chen, L.; Ying, J.; Liu, Z.; Zhao, J.; et al. Urolithin A protects human dermal fibroblasts from UVA-induced photoaging through NRF2 activation and mitophagy. J. Photochem. Photobiol. B 2022, 232, 112462. [Google Scholar] [CrossRef] [PubMed]
- Kuatov, R.; Takano, J.; Arie, H.; Kominami, M.; Tateishi, N.; Wakabayashi, K.-I.; Takemoto, D.; Izumo, T.; Nakao, Y.; Nakamura, W.; et al. Urolithin A Modulates PER2 Degradation via SIRT1 and Enhances the Amplitude of Circadian Clocks in Human Senescent Cells. Nutrients 2024, 17, 20. [Google Scholar] [CrossRef]
- Cho, S.I.; Jo, E.-R.; Song, H. Urolithin A attenuates auditory cell senescence by activating mitophagy. Sci. Rep. 2022, 12, 7704. [Google Scholar] [CrossRef] [PubMed]
- Cinat, D.; de Souza, A.L.; Soto-Gamez, A.; Jellema-de Bruin, A.L.; Coppes, R.P.; Barazzuol, L. Mitophagy induction improves salivary gland stem/progenitor cell function by reducing senescence after irradiation. Radiother. Oncol. 2024, 190, 110028. [Google Scholar] [CrossRef]
- He, Y.; Yocum, L.; Alexander, P.G.; Jurczak, M.J.; Lin, H. Urolithin A Protects Chondrocytes From Mechanical Overloading-Induced Injuries. Front. Pharmacol. 2021, 12, 703847. [Google Scholar] [CrossRef]
- Shi, P.-Z.; Wang, J.-W.; Wang, P.-C.; Han, B.; Lu, X.-H.; Ren, Y.; Feng, X.-M.; Cheng, X.-F.; Zhang, L. Urolithin a alleviates oxidative stress-induced senescence in nucleus pulposus-derived mesenchymal stem cells through SIRT1/PGC-1α pathway. World J. Stem Cells 2021, 13, 1928–1946. [Google Scholar] [CrossRef]
- Liu, H.; Kang, H.; Song, C.; Lei, Z.; Li, L.; Guo, J.; Xu, Y.; Guan, H.; Fang, Z.; Li, F. Urolithin A Inhibits the Catabolic Effect of TNFα on Nucleus Pulposus Cell and Alleviates Intervertebral Disc Degeneration in vivo. Front. Pharmacol. 2018, 9, 1043. [Google Scholar] [CrossRef]
- Guo, X.-X.; Chang, X.-J.; Pu, Q.; Li, A.-L.; Li, J.; Li, X.-Y. Urolithin A alleviates cell senescence by inhibiting ferroptosis and enhances corneal epithelial wound healing. Front. Med. 2024, 11, 1441196. [Google Scholar] [CrossRef]
- Girotra, M.; Chiang, Y.-H.; Charmoy, M.; Ginefra, P.; Hope, H.C.; Bataclan, C.; Yu, Y.-R.; Schyrr, F.; Franco, F.; Geiger, H.; et al. Induction of mitochondrial recycling reverts age-associated decline of the hematopoietic and immune systems. Nat. Aging 2023, 3, 1057–1066. [Google Scholar] [CrossRef]
- Nijhawan, D.; Honarpour, N.; Wang, X. Apoptosis in neural development and disease. Annu. Rev. Neurosci. 2000, 23, 73–87. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.-J.; Cao, Q.; Zhang, Y.; Su, X.-D. Activation and regulation of caspase-6 and its role in neurodegenerative diseases. Annu. Rev. Pharmacol. Toxicol. 2015, 55, 553–572. [Google Scholar] [CrossRef] [PubMed]
- Frost, B. Alzheimer’s disease and related tauopathies: Disorders of disrupted neuronal identity. Trends Neurosci. 2023, 46, 797–813. [Google Scholar] [CrossRef]
- Gordon, R.; Albornoz, E.A.; Christie, D.C.; Langley, M.R.; Kumar, V.; Mantovani, S.; Robertson, A.A.B.; Butler, M.S.; Rowe, D.B.; O’Neill, L.A.; et al. Inflammasome inhibition prevents α-synuclein pathology and dopaminergic neurodegeneration in mice. Sci. Transl. Med. 2018, 10, eaah4066. [Google Scholar] [CrossRef]
- Lou, J.; Mao, Y.; Jiang, W.; Shen, H.; Fan, Y.; Yu, Q.; Zhou, C.; Wei, Z.; Zhou, K.; Jin, M.; et al. TRIM56 Modulates YBX1 Degradation to Ameliorate ZBP1-Mediated Neuronal PANoptosis in Spinal Cord Injury. Adv. Sci. 2024, 11, e2407132. [Google Scholar] [CrossRef]
- Wu, W.; Jia, S.; Xu, H.; Gao, Z.; Wang, Z.; Lu, B.; Ai, Y.; Liu, Y.; Liu, R.; Yang, T.; et al. Supramolecular Hydrogel Microspheres of Platelet-Derived Growth Factor Mimetic Peptide Promote Recovery from Spinal Cord Injury. ACS Nano 2023, 17, 3818–3837. [Google Scholar] [CrossRef] [PubMed]
- Shi, X.; Zhang, L.; Wu, S.; Zhang, C.; Mamtilahun, M.; Li, Y.; Zhang, Z.; Zuo, C.; Cui, F.; Li, W.; et al. A simple polydopamine-based platform for engineering extracellular vesicles with brain-targeting peptide and imaging probes to improve stroke outcome. J. Extracell. Vesicles 2025, 14, e70031. [Google Scholar] [CrossRef]
- Gong, Q.-Y.; Cai, L.; Jing, Y.; Wang, W.; Yang, D.-X.; Chen, S.-W.; Tian, H.-L. Urolithin A alleviates blood-brain barrier disruption and attenuates neuronal apoptosis following traumatic brain injury in mice. Neural Regener. Res. 2022, 17, 2007–2013. [Google Scholar]
- Lin, X.-H.; Ye, X.-J.; Li, Q.-F.; Gong, Z.; Cao, X.; Li, J.-H.; Zhao, S.-T.; Sun, X.-D.; He, X.-S.; Xuan, A.-G. Urolithin A Prevents Focal Cerebral Ischemic Injury via Attenuating Apoptosis and Neuroinflammation in Mice. Neuroscience 2020, 448, 94–106. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, Y.; Halemahebai, G.; Tian, L.; Dong, H.; Aisker, G. Urolithin A, a pomegranate metabolite, protects pancreatic β cells from apoptosis by activating autophagy. J. Ethnopharmacol. 2021, 272, 113628. [Google Scholar] [CrossRef]
- Yang, Y.; Hu, Q.; Kang, H.; Li, J.; Zhao, X.; Zhu, L.; Tang, W.; Wan, M. Urolithin A protects severe acute pancreatitis-associated acute cardiac injury by regulating mitochondrial fatty acid oxidative metabolism in cardiomyocytes. MedComm 2023, 4, e459. [Google Scholar] [CrossRef]
- Lin, J.; Zhuge, J.; Zheng, X.; Wu, Y.; Zhang, Z.; Xu, T.; Meftah, Z.; Xu, H.; Wu, Y.; Tian, N.; et al. Urolithin A-induced mitophagy suppresses apoptosis and attenuates intervertebral disc degeneration via the AMPK signaling pathway. Free Radic. Biol. Med. 2020, 150, 109–119. [Google Scholar] [CrossRef]
- Alfei, S.; Zuccari, G. Ellagic Acid: A Green Multi-Target Weapon That Reduces Oxidative Stress and Inflammation to Prevent and Improve the Condition of Alzheimer’s Disease. Int. J. Mol. Sci. 2025, 26, 844. [Google Scholar] [CrossRef]
- Citron, M. Alzheimer’s disease: Strategies for disease modification. Nat. Rev. Drug Discov. 2010, 9, 387–398. [Google Scholar] [CrossRef]
- Hou, Y.; Chu, X.; Park, J.-H.; Zhu, Q.; Hussain, M.; Li, Z.; Madsen, H.B.; Yang, B.; Wei, Y.; Wang, Y.; et al. Urolithin A improves Alzheimer’s disease cognition and restores mitophagy and lysosomal functions. Alzheimers. Dement. 2024, 20, 4212–4233. [Google Scholar] [CrossRef]
- Kshirsagar, S.; Alvir, R.V.; Pradeepkiran, J.A.; Hindle, A.; Vijayan, M.; Ramasubramaniam, B.; Kumar, S.; Reddy, A.P.; Reddy, P.H. A Combination Therapy of Urolithin A+EGCG Has Stronger Protective Effects than Single Drug Urolithin A in a Humanized Amyloid Beta Knockin Mice for Late-Onset Alzheimer’s Disease. Cells 2022, 11, 2660. [Google Scholar] [CrossRef]
- Jayatunga, D.P.W.; Hone, E.; Khaira, H.; Lunelli, T.; Singh, H.; Guillemin, G.J.; Fernando, B.; Garg, M.L.; Verdile, G.; Martins, R.N. Therapeutic Potential of Mitophagy-Inducing Microflora Metabolite, Urolithin A for Alzheimer’s Disease. Nutrients 2021, 13, 3744. [Google Scholar] [CrossRef]
- Zhang, X.-W.; Zhu, X.-X.; Tang, D.-S.; Lu, J.-H. Targeting autophagy in Alzheimer’s disease: Animal models and mechanisms. Zool. Res. 2023, 44, 1132–1145. [Google Scholar] [CrossRef]
- Scheltens, P.; de Strooper, B.; Kivipelto, M.; Holstege, H.; Chételat, G.; Teunissen, C.E.; Cummings, J.; van der Flier, W.M. Alzheimer’s disease. Lancet 2021, 397, 1577–1590. [Google Scholar] [CrossRef]
- Aisen, P.S.; Cummings, J.; Jack, C.R., Jr.; Morris, J.C.; Sperling, R.; Frölich, L.; Jones, R.W.; Dowsett, S.A.; Matthews, B.R.; Raskin, J.; et al. On the path to 2025: Understanding the Alzheimer’s disease continuum. Alzheimers. Res. Ther. 2017, 9, 60. [Google Scholar] [CrossRef]
- Esselun, C.; Theyssen, E.; Eckert, G.P. Effects of Urolithin A on Mitochondrial Parameters in a Cellular Model of Early Alzheimer Disease. Int. J. Mol. Sci. 2021, 22, 8333. [Google Scholar] [CrossRef]
- Velagapudi, R.; Lepiarz, I.; El-Bakoush, A.; Katola, F.O.; Bhatia, H.; Fiebich, B.L.; Olajide, O.A. Induction of Autophagy and Activation of SIRT-1 Deacetylation Mechanisms Mediate Neuroprotection by the Pomegranate Metabolite Urolithin A in BV2 Microglia and Differentiated 3D Human Neural Progenitor Cells. Mol. Nutr. Food Res. 2019, 63, e1801237. [Google Scholar] [CrossRef]
- Tu, H.-J.; Su, C.-J.; Peng, C.-S.; Lin, T.E.; HuangFu, W.-C.; Hsu, K.-C.; Hwang, T.-L.; Pan, S.-L. Urolithin A exhibits a neuroprotective effect against Alzheimer’s disease by inhibiting DYRK1A activity. J. Food Drug Anal. 2023, 31, 358–370. [Google Scholar] [CrossRef]
- Ballesteros-Álvarez, J.; Nguyen, W.; Sivapatham, R.; Rane, A.; Andersen, J.K. Urolithin A reduces amyloid-beta load and improves cognitive deficits uncorrelated with plaque burden in a mouse model of Alzheimer’s disease. Geroscience 2023, 45, 1095–1113. [Google Scholar] [CrossRef]
- Xiong, R.; Li, B.; Yu, H.; Fan, T.; Yu, H.; Yang, Y.; Wang, J.-Z.; Pi, G.; Yang, X. Urolithin A Inhibits Anterior Basolateral Amygdala to Ventral Hippocampal CA1 Circuit to Ameliorate Amyloid-β-Impaired Social Ability. J. Alzheimers. Dis. 2024, 99, 1303–1316. [Google Scholar] [CrossRef]
- Morris, H.R.; Spillantini, M.G.; Sue, C.M.; Williams-Gray, C.H. The pathogenesis of Parkinson’s disease. Lancet 2024, 403, 293–304. [Google Scholar] [CrossRef]
- Kujawska, M.; Jourdes, M.; Witucki, Ł.; Karaźniewicz-Łada, M.; Szulc, M.; Górska, A.; Mikołajczak, P.Ł.; Teissedre, P.-L.; Jodynis-Liebert, J. Pomegranate Juice Ameliorates Dopamine Release and Behavioral Deficits in a Rat Model of Parkinson’s Disease. Brain Sci. 2021, 11, 1127. [Google Scholar] [CrossRef]
- Liu, J.; Jiang, J.; Qiu, J.; Wang, L.; Zhuo, J.; Wang, B.; Sun, D.; Yu, S.; Lou, H. Urolithin A protects dopaminergic neurons in experimental models of Parkinson’s disease by promoting mitochondrial biogenesis through the SIRT1/PGC-1α signaling pathway. Food Funct. 2022, 13, 375–385. [Google Scholar] [CrossRef]
- Lu, Y.; Gao, L.; Yang, Y.; Shi, D.; Zhang, Z.; Wang, X.; Huang, Y.; Wu, J.; Meng, J.; Li, H.; et al. Protective role of mitophagy on microglia-mediated neuroinflammatory injury through mtDNA-STING signaling in manganese-induced parkinsonism. J. Neuroinflamm. 2025, 22, 55. [Google Scholar] [CrossRef]
- Qiu, J.; Chen, Y.; Zhuo, J.; Zhang, L.; Liu, J.; Wang, B.; Sun, D.; Yu, S.; Lou, H. Urolithin A promotes mitophagy and suppresses NLRP3 inflammasome activation in lipopolysaccharide-induced BV2 microglial cells and MPTP-induced Parkinson’s disease model. Neuropharmacology 2022, 207, 108963. [Google Scholar] [CrossRef]
- Ren, Y.; Wu, X.; Bai, T.; Yang, N.; Yuan, Y.; Xu, L.; Wen, Y.; Wen, Y.; Wang, Z.; Zhou, L.; et al. CDK5-USP30 signaling pathway regulates MAVS-mediated inflammation via suppressing mitophagy in MPTP/MPP+ PD model. Ecotoxicol. Environ. Saf. 2024, 279, 116446. [Google Scholar] [CrossRef] [PubMed]
- Bao, H.; Liu, Y.; Zhang, M.; Chen, Z.; Zhang, W.; Ge, Y.; Kang, D.; Gao, F.; Shen, Y. Increased β-site APP cleaving enzyme 1-mediated insulin receptor cleavage in type 2 diabetes mellitus with cognitive impairment. Alzheimers. Dement. 2021, 17, 1097–1108. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Jung, Y.H.; Choi, G.E.; Kim, J.S.; Chae, C.W.; Lim, J.R.; Kim, S.Y.; Yoon, J.H.; Cho, J.H.; Lee, S.-J.; et al. Urolithin A suppresses high glucose-induced neuronal amyloidogenesis by modulating TGM2-dependent ER-mitochondria contacts and calcium homeostasis. Cell Death Differ. 2021, 28, 184–202. [Google Scholar] [CrossRef]
- Xiao, Y.; Li, K.; Bian, J.; Liu, H.; Zhai, X.; El-Omar, E.; Han, L.; Gong, L.; Wang, M. Urolithin A Attenuates Diabetes-Associated Cognitive Impairment by Ameliorating Intestinal Barrier Dysfunction via N-glycan Biosynthesis Pathway. Mol. Nutr. Food Res. 2022, 66, e2100863. [Google Scholar] [CrossRef]
- Xiao, Y.; Li, K.; Bian, J.; Zhang, Y.; Li, J.; Liu, H.; Ye, Y.; Han, L.; Gong, L.; Wang, M. Urolithin A Protects Neuronal Cells against Stress Damage and Apoptosis by Atp2a3 Inhibition. Mol. Nutr. Food Res. 2023, 67, e2300146. [Google Scholar] [CrossRef]
- Puy, L.; Parry-Jones, A.R.; Sandset, E.C.; Dowlatshahi, D.; Ziai, W.; Cordonnier, C. Intracerebral haemorrhage. Nat. Rev. Dis. Primers 2023, 9, 14. [Google Scholar] [CrossRef]
- Tsivgoulis, G.; Katsanos, A.H.; Sandset, E.C.; Turc, G.; Nguyen, T.N.; Bivard, A.; Fischer, U.; Khatri, P. Thrombolysis for acute ischaemic stroke: Current status and future perspectives. Lancet Neurol. 2023, 22, 418–429. [Google Scholar] [CrossRef]
- Ahsan, A.; Zheng, Y.-R.; Wu, X.-L.; Tang, W.-D.; Liu, M.-R.; Ma, S.-J.; Jiang, L.; Hu, W.-W.; Zhang, X.-N.; Chen, Z. Urolithin A-activated autophagy but not mitophagy protects against ischemic neuronal injury by inhibiting ER stress in vitro and in vivo. CNS Neurosci. Ther. 2019, 25, 976–986. [Google Scholar] [CrossRef]
- Liu, M.; Chen, Z.; Zhang, H.; Cai, Z.; Liu, T.; Zhang, M.; Wu, X.; Ai, F.; Liu, G.; Zeng, C.; et al. Urolithin A alleviates early brain injury after subarachnoid hemorrhage by regulating the AMPK/mTOR pathway-mediated autophagy. Neurochirurgie 2023, 69, 101480. [Google Scholar] [CrossRef]
- Salvador, A.F.M.; Kipnis, J. Immune response after central nervous system injury. Semin. Immunol. 2022, 59, 101629. [Google Scholar] [CrossRef]
- Maas, A.I.R.; Menon, D.K.; Manley, G.T.; Abrams, M.; Åkerlund, C.; Andelic, N.; Aries, M.; Bashford, T.; Bell, M.J.; Bodien, Y.G.; et al. Traumatic brain injury: Progress and challenges in prevention, clinical care, and research. Lancet Neurol. 2022, 21, 1004–1060. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Ying, J.; Zhu, J.; Chen, L.; Liu, R.; Jing, M.; Wang, Y.; Zhou, K.; Wu, L.; Wu, C.; et al. Urolithin A alleviates NLRP3 inflammasome activation and pyroptosis by promoting microglial mitophagy following spinal cord injury. Int. Immunopharmacol. 2025, 148, 114057. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Chang, Y.; Zhou, W.; Rao, S.; Wang, H.; Lin, R.; Hu, W.; Chen, S.; Su, G.; Li, Y.; et al. An esterase-activatable nanoprodrug mitigates severe spinal cord injury via alleviating ferroptosis and reprogramming inflammatory microenvironment. Nano Today 2024, 56, 102229. [Google Scholar] [CrossRef]
- Wang, S.; Qiao, J.; Chen, Y.; Tian, L.; Sun, X. Urolithin A inhibits enterovirus 71 replication and promotes autophagy and apoptosis of infected cells in vitro. Arch. Virol. 2022, 167, 1989–1997. [Google Scholar] [CrossRef] [PubMed]
- Tan, S.; Tong, W.H.; Vyas, A. Urolithin-A attenuates neurotoxoplasmosis and alters innate response towards predator odor. Brain Behav. Immun. Health 2020, 8, 100128. [Google Scholar] [CrossRef]
- Shetty, S.S.; Shetty, S.; Kumari, N.S. Therapeutic efficacy of gut microbiota-derived polyphenol metabolite Urolithin A. Beni-Suef Univ. J. Basic Appl. Sci. 2024, 13, 31. [Google Scholar] [CrossRef]
- Mousavi, S.; Weschka, D.; Bereswill, S.; Heimesaat, M.M. Preclinical Evaluation of Oral Urolithin-A for the Treatment of Acute Campylobacteriosis in Campylobacter jejuni Infected Microbiota-Depleted IL-10−/− Mice. Pathogens 2020, 10, 7. [Google Scholar] [CrossRef]
- Remadevi, V.; Jaikumar, V.S.; Vini, R.; Krishnendhu, B.; Azeez, J.M.; Sundaram, S.; Sreeja, S. Urolithin A, induces apoptosis and autophagy crosstalk in Oral Squamous Cell Carcinoma via mTOR/AKT/ERK1/2 pathway. Phytomedicine 2024, 130, 155721. [Google Scholar] [CrossRef]
- Zhang, Y.; Jiang, L.; Su, P.; Yu, T.; Ma, Z.; Liu, Y.; Yu, J. Urolithin A suppresses tumor progression and induces autophagy in gastric cancer via the PI3K/Akt/mTOR pathway. Drug Dev. Res. 2023, 84, 172–184. [Google Scholar] [CrossRef]
- Sahashi, H.; Kato, A.; Yoshida, M.; Hayashi, K.; Naitoh, I.; Hori, Y.; Natsume, M.; Jinno, N.; Kachi, K.; Asano, G.; et al. Urolithin A targets the AKT/WNK1 axis to induce autophagy and exert anti-tumor effects in cholangiocarcinoma. Front. Oncol. 2022, 12, 963314. [Google Scholar] [CrossRef]
- Ma, S.; Wu, Q.; Wu, W.; Tian, Y.; Zhang, J.; Chen, C.; Sheng, X.; Zhao, F.; Ding, L.; Wang, T.; et al. Urolithin A Hijacks ERK1/2-ULK1 Cascade to Improve CD8+ T Cell Fitness for Antitumor Immunity. Adv. Sci. 2024, 11, e2310065. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Cui, H.; Deng, H.; Deng, Y.; Yin, S.; Li, T.; Yuan, T. Urolithin A promotes the degradation of TMSB10 to deformation F-actin in non-small-cell lung cancer. Phytomedicine 2024, 135, 156109. [Google Scholar] [CrossRef] [PubMed]
- Denk, D.; Petrocelli, V.; Conche, C.; Drachsler, M.; Ziegler, P.K.; Braun, A.; Kress, A.; Nicolas, A.M.; Mohs, K.; Becker, C.; et al. Expansion of T memory stem cells with superior anti-tumor immunity by Urolithin A-induced mitophagy. Immunity 2022, 55, 2059–2073.e8. [Google Scholar] [CrossRef]
- Zheng, B.; Wang, Y.; Zhou, B.; Qian, F.; Liu, D.; Ye, D.; Zhou, X.; Fang, L. Urolithin A inhibits breast cancer progression via activating TFEB-mediated mitophagy in tumor macrophages. J. Adv. Res. 2025, 69, 125–138. [Google Scholar] [CrossRef]
- Friedmann-Morvinski, D.; Bushong, E.A.; Ke, E.; Soda, Y.; Marumoto, T.; Singer, O.; Ellisman, M.H.; Verma, I.M. Dedifferentiation of Neurons and Astrocytes by Oncogenes Can Induce Gliomas in Mice. Science 2012, 338, 1080–1084. [Google Scholar] [CrossRef]
- Liu, C.-L.; Zhao, D.; Li, J.-J.; Liu, S.; An, J.-J.; Wang, D.; Hu, F.-A.; Qiu, C.-Y.; Cui, M.-H. Inhibition of glioblastoma progression by Urolithin A in vitro and in vivo by regulating Sirt1-FOXO1 axis via ERK/AKT signaling pathways. Neoplasma 2022, 69, 80–94. [Google Scholar] [CrossRef]
- Shen, C.-K.; Huang, B.-R.; Charoensaensuk, V.; Yang, L.-Y.; Tsai, C.-F.; Liu, Y.-S.; Lai, S.-W.; Lu, D.-Y.; Yeh, W.-L.; Lin, C. Inhibitory Effects of Urolithins, Bioactive Gut Metabolites from Natural Polyphenols, against Glioblastoma Progression. Nutrients 2023, 15, 4854. [Google Scholar] [CrossRef] [PubMed]
- Lu, G.; Wu, J.; Zheng, Z.; Deng, Z.; Xu, X.; Li, X.; Liang, X.; Qi, W.; Zhang, S.; Qiu, Y.; et al. Urolithin A Enhances Tight Junction Protein Expression in Endothelial Cells Cultured In Vitro via Pink1-Parkin-Mediated Mitophagy in Irradiated Astrocytes. J. Mol. Neurosci. 2025, 75, 23. [Google Scholar] [CrossRef]
- Filippi, M.; Bar-Or, A.; Piehl, F.; Preziosa, P.; Solari, A.; Vukusic, S.; Rocca, M.A. Multiple sclerosis. Nat. Rev. Dis. Primers 2018, 4, 43. [Google Scholar] [CrossRef]
- Shen, P.-X.; Li, X.; Deng, S.-Y.; Zhao, L.; Zhang, Y.-Y.; Deng, X.; Han, B.; Yu, J.; Li, Y.; Wang, Z.-Z.; et al. Urolithin A ameliorates experimental autoimmune encephalomyelitis by targeting aryl hydrocarbon receptor. EBioMedicine 2021, 64, 103227. [Google Scholar] [CrossRef]
- Hardiman, O.; Al-Chalabi, A.; Chio, A.; Corr, E.M.; Logroscino, G.; Robberecht, W.; Shaw, P.J.; Simmons, Z.; van den Berg, L.H. Amyotrophic lateral sclerosis. Nat. Rev. Dis. Primers 2017, 3, 17071. [Google Scholar] [CrossRef] [PubMed]
- Hardiman, O.; van den Berg, L.H.; Kiernan, M.C. Clinical diagnosis and management of amyotrophic lateral sclerosis. Nat. Rev. Neurol. 2011, 7, 639–649. [Google Scholar] [CrossRef] [PubMed]
- de Calbiac, H.; Renault, S.; Haouy, G.; Jung, V.; Roger, K.; Zhou, Q.; Campanari, M.-L.; Chentout, L.; Demy, D.L.; Marian, A.; et al. Poly-GP accumulation due to C9orf72 loss of function induces motor neuron apoptosis through autophagy and mitophagy defects. Autophagy 2024, 20, 2164–2185. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Gao, C.; Yang, D.; Nie, L.; He, K.; Chen, C.; Li, S.; Huang, G.; Zhou, L.; Huang, X.; et al. Urolithin a Improves Motor Dysfunction Induced by Copper Exposure in SOD1G93A Transgenic Mice Via Activation of Mitophagy. Mol. Neurobiol. 2024, 62, 6922–6937. [Google Scholar] [CrossRef]
- Moultrie, F.; Chiverton, L.; Hatami, I.; Lilien, C.; Servais, L. Pushing the boundaries: Future directions in the management of spinal muscular atrophy. Trends Mol. Med. 2025, 31, 307–318. [Google Scholar] [CrossRef]
- Mikhail, A.I.; Ng, S.Y.; Xhuti, D.; Lesinski, M.A.; Chhor, J.; Deguise, M.-O.; de Repentigny, Y.; Nederveen, J.P.; Kothary, R.; Tarnopolsky, M.A.; et al. Skeletal Muscle Mitochondrial and Autophagic Dysregulation Are Modifiable in Spinal Muscular Atrophy. J. Cachexia Sarcopenia Muscle 2025, 16, e13701. [Google Scholar] [CrossRef]
- Zhao, H.; Zhu, H.; Yun, H.; Liu, J.; Song, G.; Teng, J.; Zou, D.; Lu, N.; Liu, C. Assessment of Urolithin A effects on muscle endurance, strength, inflammation, oxidative stress, and protein metabolism in male athletes with resistance training: An 8-week randomized, double-blind, placebo-controlled study. J. Int. Soc. Sports Nutr. 2024, 21, 2419388. [Google Scholar] [CrossRef]
- Tow, W.-K.; Chee, P.-Y.; Sundralingam, U.; Palanisamy, U.D. The Therapeutic Relevance of Urolithins, Intestinal Metabolites of Ellagitannin-Rich Food: A Systematic Review of In Vivo Studies. Nutrients 2022, 14, 3494. [Google Scholar] [CrossRef]
- Jin, X.-H.; Fang, J.-Q.; Wang, J.-G.; Xu, B.; Wang, X.; Liu, S.-H.; Chen, F.; Liu, J.-J. PCL NGCs integrated with urolithin-A-loaded hydrogels for nerve regeneration. J. Mater. Chem. B 2022, 10, 8771–8784. [Google Scholar] [CrossRef]
- Ji, D.; Chen, W.-Z.; Zhang, L.; Zhang, Z.-H.; Chen, L.-J. Gut microbiota, circulating cytokines and dementia: A Mendelian randomization study. J. Neuroinflamm. 2024, 21, 2. [Google Scholar] [CrossRef]
- Grabrucker, S.; Marizzoni, M.; Silajdžić, E.; Lopizzo, N.; Mombelli, E.; Nicolas, S.; Dohm-Hansen, S.; Scassellati, C.; Moretti, D.V.; Rosa, M.; et al. Microbiota from Alzheimer’s patients induce deficits in cognition and hippocampal neurogenesis. Brain 2023, 146, 4916–4934. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).