Abstract
Bipolar disorder (BD) is a multifactorial chronic psychiatric disease highly defined by genetic, clinical, environmental and social risk factors. The present systematic review and meta-analysis aimed to examine the relationship between inflammatory and neurotrophic factors and clinical, social and environmental factors involved in the development and the characterization of BD. Web of Science, PubMed, PsycINFO, Scopus and Science Direct were searched by two independent reviewers. The systematic review was registered in PROSPERO (CRD42020180626). A total of 51 studies with 4547 patients with a diagnosis of BD were selected for systematic review. Among them, 18 articles were included for meta-analysis. The study found some evidence of associations between BDNF and/or inflammatory factors and different stressors and functional and cognitive impairment, but limitations prevented firm conclusions. The main finding of the meta-analysis was a negative correlation between circulating levels of BDNF and depression severity score (standardized mean difference = −0.22, Confidence Interval 95% = −0.38, −0.05, p = 0.01). Evidence indicates that BDNF has a role in the depressive component of BD. However, the poor consistency found for other inflammatory mediators clearly indicates that highly controlled studies are needed to identity precise biomarkers of this disorder.
Keywords:
depression; mania; bipolar disorder; BDNF; cytokines; neurotrophins; biomarker; clinical factors; systematic review; meta-analysis 1. Introduction
Bipolar affective disorder (BD) is a relatively common but serious mental illness, with a lifetime prevalence of 0.6% for bipolar disorder type I (BD-I), 0.4% for bipolar disorder type II (BD-II), 1.4% for subthreshold bipolar disorder (SBD), and 2.4% for bipolar disorder spectrum (BDS) [1]. It is one of the leading causes of disability worldwide [2], presenting high rates of psychiatric and medical morbidity and mortality [3,4,5,6], due to the co-occurrence with medical conditions (such as cardiovascular disorders, diabetes, and obesity), and psychiatric disorders (e.g., anxiety, personality disorders, attention-deficit/hyperactivity disorder (ADHD), substance use, and suicide) [7,8,9]. Furthermore, an early age of onset is associated with a more chronic, severe, and recurrent course of the disease [10]. In terms of gender, BD-I is equally distributed in men and women, whereas the BD-II affects more women, who are characterized by a predominance of depressive polarity [11].
BD is characterized by mood instability, and is manifested by the presence of at least one episode of mania or hypomania alternating with episodes of depression [12]. In addition to affective symptoms, neuropsychological and cognitive performance deficits, mainly related to memory, attention and executive tasks, are common [13,14,15]. These dysfunctions appear to be present from the onset of the disease, and in all mood states, even in euthymic patients and during remission [16,17,18,19]. Affective symptomatology and neurocognitive impairment interfere negatively in the psychosocial functioning and quality of life of the affected person [20,21,22].
This relationship between cognitive ability and emotionality in BD has been extensively studied, and there is evidence that poor cognitive ability, in terms of deficits in executive function and inhibition, negatively interferes with emotional regulation [23]. In addition to the effect of attentional and cognitive problems, it has been studied how emotional stimuli can influence the motor inhibition response. In particular, this response seems to be deficient in BD patients in whom certain emotions, such as sadness, may hinder the inhibition response [24]. Moreover, several studies have reported an association between cognitive performance and poorer psychosocial functioning [25,26,27,28] independently of the affective state. In addition, impulsivity has been the state most closely related to poorer functioning and more suicidal tendencies [29,30,31,32,33,34].
Along the same lines, an interesting recent study on the neural mechanisms involved in gaze perception suggests that the amygdala could play a role in attentional mechanisms, in addition to its well-known role in emotional processing [35]. Another mechanism that has been studied is the tryptophan (TRP)-kynurenine (KYN) metabolic pathway, whose action in the immune system seems to be related to the development of various diseases and psychiatric disorders that involve alterations in cognition and social functioning, including BD [36]. These findings could help to understand the observed alterations in cognition and social functioning in patients with BD.
On the other hand, new studies have recently been published on the identification of potential biomarkers in BD using mass spectrometry (MS)-based techniques. A systematic review and meta-analysis of selected studies showed evidence of alterations in the apolipoproteins (APOs) group, which appear to be associated with inflammatory response and cognitive decline. However, the results of the meta-analysis were inconclusive on the possible role of APOs as potential candidates for psychiatric biomarkers [37].
Knowledge of the etiology of BD is increasing. BD is known to be a highly genetic psychiatric disorder with a heritability of about 60–80% estimated from twin studies [38,39]. In addition, family history of BD and other biological variables (such as age, sex and metabolic factors) are relevant predictors of the development of the disorder [40]. Increasing evidence shows that the interaction between genetic and environmental factors, as well as the influence of epigenetic mechanisms, may play an important role in the etiopathogenesis of the disorder [41,42,43]. According to this hypothesis, neurodevelopmental pathways could be involved in the development of BD [44].
Furthermore, research on the role of neurodevelopmental factors in the onset of cognitive deficits in BD points to its conceptualization as a neurodegenerative disease [45,46,47]. In fact, this cognitive impairment has also been observed in first-degree relatives of BD patients [48], suggesting the presence of potential endophenotypes that could function as trait markers for the disorder [49,50]. Similarly, many efforts have been made so far in the search for possible biological mechanisms underlying different neurological and psychiatric disorders, such as depression, anxiety and dementia, with which BD shares some symptomatic manifestations [51].
The nature of BD is complex and is determined by multiple causes. One of the proposed mechanisms involved in the neurobiology of the disorder is neuroinflammation [52,53,54]. Numerous studies have also found differences in the levels of trophic factors of the neurotrophin family (mainly brain-derived neurotrophic factor (BDNF)) and cytokines (such as interleukins (e.g., IL-6, IL-1β, IL-2, IL-4, IL-8, IL-10, IL-18) and tumor necrosis factor alpha (TNF-α)), as well as the influence of oxidative stress mediators in BD patients compared to healthy controls [55,56]. Supporting these findings, BDNF could play an important role in the alterations in neuroinflammation, neuroplasticity and neurogenesis for BD [57]. However, no specific biomarker has yet been identified for each phase of the disorder [58].
Regarding the identification of genetic markers for BD, a candidate gene strategy has been largely unsuccessful [59]. BDNF is one of the most investigated candidate genes by studies looking at genetic (GWAS) and epigenetic (DNA methylation and EWAS) variations associated with the risk of BD [60,61]. Evidence from longitudinal analysis of methylation profiles support a role of inflammatory factors (e.g., BDNF, IL-1β) in the pathogenesis of BD [60]. However, potential confounders (underpowered sample sizes, inadequate testing correction, undetected genetic mismatch, global methylation or inconclusive results compared to other psychiatric disorders) may explain the lack of consistent findings and the difficulties in establishing BD susceptibility genes.
Furthermore, psychological and social factors must be taken into account. Indeed, a substantial body of studies indicates that there is a relationship between BD and exposure to clinical, environmental, and social risk factors [62,63,64,65] that precede and could predict the onset of BD. Exposure to environmental risk factors during prenatal and perinatal periods [66,67], childhood maltreatment or abuse [68,69,70], stressful life events [71,72,73], and alcoholism or substance abuse [74,75] are some of the factors that can be phenomenologically related to the development of BD. Interestingly, such early life stressful events could also promote a neuroinflammatory state that would eventually contribute to the onset of BD [76].
Although the existing literature demonstrates relationships between inflammatory mediators and bipolar disorder as compared to healthy controls, a systematic review of a reliable biomarker signature for bipolar disorder that could help to distinguish between different subtypes, phases (depression, mania and euthymia) and disease severities, has not been accurately performed. The aim of this study was to conduct a systematic review and meta-analysis to identify cytokines, inflammatory and neurotrophic mediators involved in the development of BD. The effort to structure and expand knowledge in this area of study has important implications for improving the knowledge of the underlying biological basis of the disorder. Thus, the clinical value of inflammatory biomarkers has to be demonstrated by highly controlled studies that follow a precise phenotyping (type, phase, severity, and comorbidities) of BD patients. The identification of accurate biomarkers could improve the objectivity of BD diagnosis and the validity of treatment in clinical trials.
2. Materials and Methods
2.1. Search Strategy
This systematic review and meta-analysis were carried out following the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [77]. The protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO CRD42020180626). An initial review was conducted to identify biomarkers involved in bipolar disorder to generate a list of search terms.
Bibliographic searches were performed in the electronic databases Web of Science, PubMed, PsycINFO, Scopus and Sciencedirect from their inception to May 2020. The database searches were complemented with manual screening of the reference list of the included studies.
Two independent searches were achieved on each database (conducted by AV-N and CG-S-L). Detailed information about the search strategy can be found in the Annex S1 of the Supplementary Materials.
The inclusion criteria applied were the following: (a) type of study: clinical trial, cohort and case-control studies; (b) age: adults subjects (patients over 18 years old); (c) diagnosis: any bipolar disorder (BD-I, BD-II, Cyclothymic Disorder and not otherwise specified BD (NOS-BD)) in any of its phases (mania, depression, mixed state or euthymia) diagnosed according to international classification systems, including clinical interviews that applied the criteria of the DSM (Diagnostic and Statistical Manual of Mental Disorders) or the ICD (International Classification of Diseases); (d) studies that include exposure to clinical, social or environmental factors; (e) studies investigating some type of inflammatory factors (biomarkers indicative of a biological state in the person, in this case the degree of brain inflammation), neurotrophic factors (or neurotrophins, a family of proteins that promote the survival, growth and differentiation of neurons; among them are nerve growth factor (NGF), the insulin-like growth factor (IGF-1), the BDNF and neurotrophin-3 (NT-3)), and cytokines (a set of IL that regulate the immune and inflammatory response) in patients with bipolar disorder; (f) language: English or Spanish only.
The following exclusion criteria were applied: (a) narrative reviews, qualitative studies and case studies; (b) children and adolescents (under 18 years old); (c) subjects diagnosed with another mood disorder (e.g., major depressive disorder, dysthymic disorder, unspecified depressive disorder); (d) subjects diagnosed with any other psychiatric disorder; (e) subjects with a diagnosis of neurological disorder or genetic syndromes; (f) studies that not include exposure to clinical, social or environmental factors related to BD; (g) studies in which the only exposure factor was a pharmacological treatment or psychological intervention; (h) studies that have not investigated neurotrophic factors and inflammatory cytokines; (i) studies with duplicated or unoriginal data.
2.2. Study Selection
Title and abstract were screened independently by two reviewers (AV-N and CG-S-L). If the presence of the biomarkers, risk factors or study design could not be ascertained from title and abstract screening, full texts of publications selected were then reviewed by the same investigators to determine final eligibility. Team meetings were held to discuss and resolve any discrepancies and reach a consensus on all inclusion decisions with a third reviewer (JG-P). If the data needed to include the study in the meta-analysis were not available, authors were contacted up to two times (two weeks apart). If no response was received, these studies were not included in the meta-analysis but were discussed narratively.
2.3. Quantitative Analysis
A meta-analysis was performed for all factors reported on by at least three studies. Mean and standard deviation for each biomarker, separated into mood phase or subtype of bipolar, were entered into an electronic database and were analyzed with a quantitative meta-analytical approach using R 3.6.3 and Rstudio. The mean differences and 95% confidence intervals between cases and controls were calculated and displayed in forest plots. Correlations between severity scales and circulating levels of biomarkers were transformed to Fisher’s Z-score to obtain accurate weight for each study. Montgomery-Asberg Depression Rating Scale (MADRS) scores were translated to Hamilton Depression Rating Scale (HDRS) scores using the equipercentile linking method developed by Leucht and colleagues [78]. The inverse variance method and Random-effects models by Hartung-Knapp-Sidik-Jonkman were used. This method produces more robust estimates and is preferred when the number of studies is small and when there is substantial heterogeneity, because DerSimonian-Laird is prone to produce false positives under this condition [79,80]. Heterogeneity was determined by means of Q statistic tests and the I2 index. Publication bias was evaluated by use of funnel plots in each meta-analysis including ten or more studies, as is recommended for interpretation [81]. Studies included in the meta-analysis were appraised using the Risk of Bias in a Non-randomised Studies (ROBINS-I) tool [82].
3. Results
A total of 4396 studies were retrieved from the databases. Finally, 51 articles (4 of which had repeated samples with other biomarkers) that analyzed 33 inflammatory mediators were eligible for review and 18 were included in the meta-analysis (Table S2). More detailed information is shown in the PRISMA flow chart (Figure 1). Risk of bias assessment of the studies included in the meta-analysis is summarized in a traffic light plot (Figure S1) and the general risk of bias of all studies included in the meta-analysis is shown in a summary plot (Figure S2). The overall risk of bias of the studies included was between moderate and serious. Among the included studies, the most commonly reported outcomes were BDNF and mood state, BDNF and bipolar subtype, correlation between BDNF and severity of mania or depression, TNF-α, and mood state, correlation between TNF-α and severity of mania, correlation between IL-6 and severity of mania or depression. We selected these outcomes and performed 9 meta-analyses.
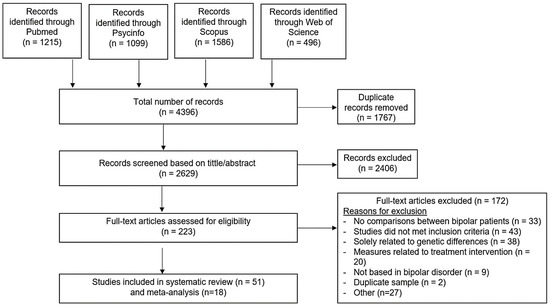
Figure 1.
PRISMA (Preferred Reporting Items for Systematic reviews and Meta-analyses) diagram. Following exclusion criteria, a total of 51 studies were selected for systematic review. Among them, 18 articles were included for meta-analysis.
The characteristics and main results of the 51 studies included in the systematic review are summarized in Table 1. The studies were conducted across several countries. The design of the studies was mostly cross-sectional, although clinical trials, post-hoc analysis of a clinical trial, longitudinal studies, retrospective and prospective studies, a historical cohort study, and a naturalistic cohort study were also included. More information on the studies can be found in the Supplementary Materials (Table S1).

Table 1.
Summary of the 51 studies analyzing 33 biomarkers in 4547 patients with a diagnosis of BD included in the systematic review and meta-analysis.
The studies comprised a total of 4547 patients with diagnoses of BD-I, BD-II and NOS-BD. Most studies used the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) or the Mini-International Neuropsychiatric Interview (MINI) to assess bipolar diagnosis, but the Structured interview of the Modified Schedule of Affective Disorder and Schizophrenia-Life Time (SADS-L) and the Schedules for Clinical Assessment in Neuropsychiatry (SCAN) were also used. Symptom severity was assessed with the Young Mania Rating Scale (YMRS) for mania or hypomania and the HDRS or the MADRS for depression. The patients were examined at different phases of the disease (euthymia, mania, depression, mixed) and in different stages of the disorder (early stage and late stage). The biomarkers evaluated were BDNF, IL-2, IL-4, IL-6, IL-8, IL-10, IL-18, IL-33, IL-1α, IL-1β, IL-1Ra, sIL-2R, sIL-6R, IL-18BP, TNF-α, IFN-γ, IGF-1, β-NGF, GDNF, VEGF, TGF-β1, TNFR1, TNFR2, TNF-R2, sTNFR60, sTNFR80, NT-3, NT-4/5, sICAM-1, sVCAM-1, sFlt-1, sSt2 and sCD40L (see Table S3 for abbreviations).
3.1. Stratifying Value of Biomarkers: Analysis of Clinical Features of BD
3.1.1. Subtypes of the Disorder
A total of 11 articles (1, 17, 21, 25, 31, 32, 39a, 39b, 40, 44a, 44b in Table 1), included in the present systematic review, evaluated the association between BD subtypes I and II and selected biomarkers, 7 studied BDNF and 9 measured inflammatory biomarkers. Only one article found differences in BDNF levels between BD-I and BD-II subtypes (40 in Table 1), in which patients with the BD-I subtype had significantly lower BDNF levels than patients with the BD-II subtype. Only one article found differences in the circulating levels of inflammatory mediators (sIL-2R and sTNF-R1), which were higher in BD-I patients than in BD-II patients (1 in Table 1). There were two more articles that compared the subtypes of BD with the SBD group (subthreshold bipolar disorder: more than 2-days but less than 4-days duration of hypomania) and found differences in the levels of inflammatory mediators (IL-1ß, IL-6, IL-8) and BDNF (45, 46 in Table 1).
In the present study, we performed a meta-analysis of BNDF between BD subtypes in three selected studies (21, 40, 45 in Table 1). These studies highlighted lower plasma BDNF levels in BDI (40 in Table 1) and SBD (45 in Table 1) patients, and in BD women with higher MADRS scores (21 in Table 1). In the meta-analysis, we found that circulating BDNF levels did not differ between BD subtypes I and II (standardized mean difference [SMD] = 0.24, 95% CI = −1.19, 0.71, p = 0.39, number of studies [k] = 3, number of participants [n] = 645) (Figure 2).
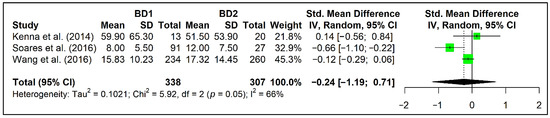
Figure 2.
Forest plot of the meta-analysis of BDNF in patients with BD1 subtype compared to those with BD2 subtype in three selected studies (21, 40, 45 in Table 1).
3.1.2. Phases of the Disorder
A total of 16 articles (1, 2, 3, 5, 8, 18, 19, 32, 33a, 33b, 34, 39a, 42, 44a, 44b, 47 in Table 1), included in the present systematic review, studied the association between biomarkers and different mood phases in BD patients, 8 of them assessed inflammatory factors, 5 assessed BDNF and other trophic factors, and 3 both biomarkers. Among the studies in which inflammatory mediators were measured, 5 of them found significant differences with respect to episode mood between depressive and (hypo)manic state (IL-4, IL-6, IL-18, IL-1β, sIL-2R, sTNF-R1, sTNF-R80) (1, 34, 33b, 39a in Table 1), 2 studies compared depressive and euthymic patients (sIL-2R, sTNF-R1, sTNF-R80) (1, 39a in Table 1), 1 study compared (hypo)manic and euthymic patients (IL-6, IL-18) (33b in Table 1), and one study compared patients with mood symptoms (depressive and (hypo)manic) and euthymic (TNF-α) (44a in Table 1). Among the studies in which BDNF and other trophic factors were evaluated, only two of them found differences in circulating BDNF levels between manic/depressed and euthymic BD patients (42 in Table 1) and between manic and depressive BD patients (47 in Table 1).
In addition, we performed a meta-analysis of BNDF between phases of the disorder from the data of five selected studies (2, 18, 32, 33a, 42 in Table 1). Most of these studies reported no differences in plasma BDNF levels between affective states (2, 18, 32, 33a in Table 1), and only one showed lower BDNF levels in depressive and manic patients compared to euthymic patients (42 in Table 1). In our meta-analysis of trophic factors between phases of the disorder, we found that circulating BDNF levels showed no difference in the depressive state compared to euthymia (SMD = −0.57, 95% CI = −3.45, 2.31, p = 0.48, k = 3, n = 313) (Figure 3a), nor in mania compared to euthymia (SMD = −0.26, 95% CI = −0.87, 0.36, p = 0.31, k = 5, n = 452) (Figure 3b). We also performed a meta-analysis of TNF-α between BD phases from three selected studies (18, 34, 44a in Table 1). Only one of them (44a in Table 1) reported increases in plasma TNF-α levels of patients with moods symptoms compared to euthymic patients. In the meta-analysis, circulating TNF-α levels show no difference in depressive patients compared to mania patients (SMD = −0.02, 95% CI = −0.69, 0.64, p = 0.91, k = 3, n = 167) (Figure 3c).
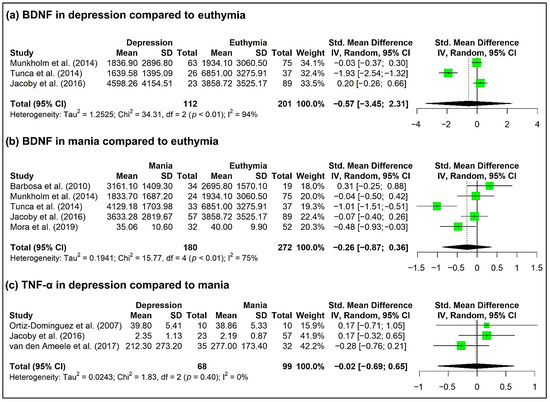
Figure 3.
Forest plot of the meta-analysis of BDNF in (a) depression compared to euthymia from the data of three selected studies (18, 33a, 42 in Table 1), (b) mania compared to euthymia (b) from the data of five selected studies (2, 18, 32, 33a, 42 in Table 1), and (c) TNF-α in depression compared to mania from the data of three selected studies (18, 34, 44a in Table 1).
3.1.3. Severity of Mood Symptoms
A total of 30 articles (1, 2, 3, 5, 7, 8, 11, 12, 13, 17, 19, 21, 22, 23, 25, 26, 27, 28, 30b, 33a, 33b, 35, 38, 39a, 40, 42, 43, 44a, 44b, 46 in Table 1) studied the relationship between symptom severity and the biomarkers included in the present systematic review. Among them, 24 reports assessed the severity of manic symptoms and 26 reports assessed the severity of depressive symptoms. In terms of biomarkers, 14 studies measured inflammatory mediators, 14 measured BDNF and/or other trophic factors, and 2 measured both biomarkers. Seven studies reported an association between circulating levels (11, 26, 27, 42 in Table 1) of BDNF and another trophic factor (NGF) (3) and severity of manic symptoms, as well as between trophic factors (BDNF, GDNF) and the severity of depressive symptoms (12, 21, 42 in Table 1). On the other hand, several studies reported an association between inflammatory mediators (sVCAM-1, TNF-α, IL-2, IL-6, sIL-6R, sTNF-R1, TGF-ß1) and severity of manic symptoms in 6 studies (1, 13, 8, 23, 35, 46 in Table 1) (inflammatory mediator with growth properties), as well as between inflammatory mediators (sTNFR60, sTNFR80, sVCAM-1, IL-6, IL-1ß, TNF-α, sIL-6R, sIL-2R, sTNF-R1, TNF-R1, TGF-ß1) and severity of depressive symptoms in 9 studies (1, 8, 13, 19, 23, 28, 35, 44a, 46 in Table 1). Another study found higher GDNF levels in manic and depressed BD patients when compared to euthymic patients (38 in Table 1).
Among the above studies, 5 of them evaluated the global disease severity (12, 17, 19, 35, 42 in Table 1) in which inflammatory mediators, BDNF and GDNF were evaluated, and 4 of them found a connection between plasma biomarker levels (sVCAM-1, TNF-α, BDNF) and disease severity (12, 19, 35, 42 in Table 1).
In the present study, we performed a meta-analysis between BNDF and severity of mood symptoms from the data of seven selected studies (11, 12, 21, 22, 26, 40, 42 in Table 1). These studies reported contradictory results; plasma BDNF levels positively correlated with YMRS scores among BD manic patients (11 in Table 1), and negatively correlated with YMRS, HDRS and/or CGI scores in BD patients (12, 42 in Table 1), with MADRS scores in BD women patients (21 in Table 1) and with HDRS and CGI scores among the BD depressed group (12 in Table 1), and no correlation was observed between BDNF and YMRS scores (22, 40 in Table 1). Similarly, no correlation between TNF-α and mania severity score (CGI, MADRS, HDRS, YMRS and/or PANSS) were reported in the three studies selected. Meta-analysis indicated that circulating BDNF levels showed a significant negative correlation with the severity of depression (SMD = −0.24, 95% CI = −0.37, −0.10, p = 0.01, k = 5, n = 271) (Figure 4a).
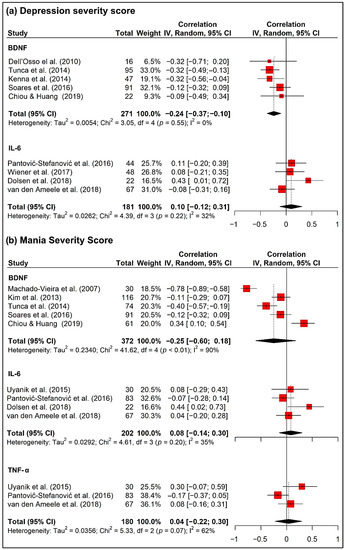
Figure 4.
Forest plot of correlations between inflammatory factors (BDNF, IL-6 and TNF-α) and (a) depression severity score (HDRS or MADRS) from the data of selected studies (11, 12, 13, 21, 30b, 35, 40, 42, 44a in Table 1) and (b) mania severity score (YMRS) from the data of selected studies (11, 13, 22, 26, 35, 40, 42, 43, 44a in Table 1).
We also performed a meta-analysis between IL-6 and severity of mood symptoms from five selected studies (13, 30, 35, 43, 44b in Table 1). Only one of these studies reported a positive correlation between plasma IL-6 levels and severity of depressive symptoms in BD patients (13 in Table 1). The remaining studies reported that plasma IL-6 levels did not correlate with MADRS, YMRS, CGI, HDRS and/or PANSS scores in BD patients (30b, 35, 43, 44b in Table 1). In the meta-analysis, no correlation between depression severity and IL-6 was found (SMD = 0.10, 95% CI = −0.12, 0.31, p = 0.38, k = 4, n = 181) (Figure 4a).
Severity of mania did not correlate with BDNF (SMD = −0.25, 95% CI = −0.60, 0.18, p = 0.25, k = 4, n = 372), IL-6 (SMD = 0.08, 95% CI = −0.14, 0.30, p = 0.48, k = 4, n = 202), nor TNF-α (SMD = 0.04, 95% CI = −0.22, 0.30, p = 0.76, k = 3, n = 180) (Figure 4b).
3.1.4. Factors Related to Clinical Staging of the Disorder
The length of illness was assessed in 17 (1, 2, 3, 5, 8, 9, 17, 19, 25, 31, 32, 33a, 39a, 40, 44a, 44b, 46 in Table 1) of the articles included in the systematic review, 8 of them evaluated inflammatory mediators, 6 reports analyzed BDNF and other trophic factors and 3 of them evaluated both biomarkers. Length of illness was associated with inflammatory mediators (IL-6, sIL-6R, sIL-2R, sTNF-R1, TNF-α) in 4 studies (1, 32, 44b, 46 in Table 1), and with BDNF and other trophic factors (NT3, NT4/5, NGF) in 3 other studies (3, 25, 33a in Table 1). In one study, although correlation between BDNF and overall disease duration was not observed (2 in Table 1), significant differences were found when the groups were segregated into more than 10 years and less than 10 years of disease duration.
Age at onset was assessed in five articles (31,35,39a,42,44a in Table 1). Two of them found an association between age of onset and inflammatory (sVCAM-1) and trophic (GDNF) factors (35, 42 in Table 1). No relationship was found between biomarkers and the number of hospitalizations in any study (3, 44a, 44b in Table 1). No interaction was also found between BDNF levels and chronicity and time [7]. Levels of sVCAM-1 correlated negatively with the bipolarity index (BPx) in the acute and remission phases (35 in Table 1). Another inflammatory mediator (TNF-α) was associated with the duration of untreated BD only in one study (35 in Table 1). Among the 3 studies (15, 19, 41 in Table 1), in which they classify BD patients into early or late stage, all measured inflammatory mediators, 2 of them evaluated BDNF and the other analyzed additional trophic factors. These three studies found significant differences in circulating levels of inflammatory mediators (IL-6, IL-10, IL-1RA, TNF-α) when comparing early- and late-stage patient groups, but not when analyzing circulating levels of trophic factors.
3.1.5. Number of Previous Episodes, Duration of Episodes and Polarity
Regarding the number of previous episodes, the results are heterogeneous. Some studies evaluated the number of lifetime mood episodes, but no association with biomarkers was found (39a, 44b in Table 1). Only one article associated the number of depressive episodes with inflammatory factors (IL-6) (37 in Table 1), but not with BDNF (31 in Table 1) or with the presence of previous episodes of depression (4 in Table 1). In one study, a longer duration of mood episodes (mixed, manic, depressive, euthymic) was associated with inflammatory mediators (IL-6, IL-18) in comparison with episodes of less than one-week duration (33b in Table 1). However, no association was found between mood duration and BDNF or other trophic factors (GDNF) (42 in Table 1). Another study found an association between the duration of current mood state and inflammatory and trophic factors (TNF-α, BDNF, VEGF and sFlt-1) (44a in Table 1), but this result was not confirmed (44b in Table 1). The duration of depressive episodes was associated with inflammatory mediators (TNF-α) in only one study (35 in Table 1).
No associations were found between any biomarker and rapid cycling bipolar patients or atypical depression (20, 39a in Table 1). Furthermore, no differences in circulating levels of inflammatory mediators (sTNF-R1, sIL-6R) were found between patients with subsyndromal BD and without subsyndromal symptoms (9 in Table 1). Similarly, no differences in mean levels of sICAM-1, sVCAM-1, IL-6 and TNF-α were observed when comparing patients in an acute phase and patients in a remission phase of the bipolar disorder (35 in Table 1). Regarding polarity, BD patients with manic polarity had significantly lower levels of sVCAM-1 than BD patients with depressive polarity (35 in Table 1). No differences were found in terms of acute episode polarity and levels of sICAM-1, IL-6 or TNF-α (35 in Table 1).
3.1.6. Cognition and Functionality
Four articles evaluated general cognitive abilities in BD patients, including cognitive and executive functioning, 1 with inflammatory mediators, 1 with BDNF and 2 with both types of factors. Among these reports, significant associations were found between cognitive abilities and inflammatory mediators (IL-1RA, sCD4DL, TNF-α) (4, 16 in Table 1) and BDNF (24, 32 in Table 1). On the other hand, two studies evaluated the degree of functionality. In one, functional impairment was associated with inflammatory mediators (IL-6, IL-10) (30b in Table 1), and in the other was reported a significant interaction between psychosocial functioning and time on BDNF levels (7 in Table 1). In one study, BDNF was not associated with quality of life (24 in Table 1). Finally, a positive correlation between BDNF levels and Global Assessment of Functioning (GAF) scores was found in one study (42 in Table 1), but not when the trophic factor GDNF was analyzed.
3.1.7. Other Clinical Parameters and Comorbidity
Nine articles evaluated age in BD patients, which was associated with inflammatory mediators (IL-6, IL-8, IL-18, IL-18BP, TNF-α, sTNFR1, sTNFR2) in 3 of these studies (10, 17, 44b in Table 1). Only two of these articles included sex as a study variable, but it was not correlated with any biomarker (17,28 in Table 1).
Only one article found an association between the number of previous psychotic episodes and inflammatory mediators (sVCAM-1) (35), and others did not find any association between biomarkers and lifetime features of psychosis (4, 17, 44a, 44b in Table 1). The presence of psychotic symptoms was not associated with inflammatory mediators or BDNF in any study (19, 25, 39a, 44a, 44b in Table 1).
Psychiatric comorbidities were generally not associated with inflammatory mediators or BDNF (2, 3, 4 in Table 1), with the exception of one study (46 in Table 1) that found a relationship with TGF-ß1. Melancholia was associated with inflammatory mediators (sTNFR80, IL-1α) in the two selected studied (39a, 39b in Table 1). Comorbid anxiety symptoms were associated with inflammatory mediators (IL-6, IL-10, TNF-α) in one study (14 in Table 1), but another study found no association between comorbid anxiety syndrome and inflammatory mediators (17 in Table 1). Post-traumatic stress disorder was not associated with the biomarkers assessed (20). The history of suicide attempts was not associated with BDNF (20 in Table 1), nor was suicidal ideation with inflammatory factors (39a in Table 1). ADHD was not associated with the biomarkers evaluated (17 in Table 1). Tobacco use, substance abuse or dependence, and alcohol abuse or dependence, were not associated with any biomarker in the studies evaluated (3, 4, 17, 20, 25, 28 in Table 1).
Childhood abuse and neglect and childhood trauma were associated with BDNF in the two studies that assessed this biomarker (6, 20 in Table 1), but in two other studies inflammatory factors were not related to these variables (28, 36 in Table 1). No association was found between resilience and BDNF (29 in Table 1). An inflammatory factor (sVCAM-1) was associated with family history of BD in one study (35 in Table 1).
Chronotype was associated with an inflammatory biomarker (IL-6) in one study (30a in Table 1). As for sleep disorders, they were associated with the inflammatory factor IL-6 in one study (13 in Table 1). Dietary intake was associated with inflammatory factors (sTNFR1, sTNFR2) in one study (10 in Table 1), and weight cycling was associated with inflammatory factors (IL-6) in another (37 in Table 1). Two studies included BMI, but no correlations with inflammatory factors were found (17, 28 in Table 1).
4. Discussion
This systematic review and a series of exploratory meta-analyses represent an effort to synthesize reliable evidence on the association of inflammatory and trophic factors with subtypes, phases and severity of the disorder, in addition to factors related to clinical staying, episodes, duration, polarity, among other clinical parameters and comorbidities related to BD. We were able to include 51 studies, comprising 4547 patients with BD. The main finding of this systematic review and meta-analysis is the negative correlation found between BDNF levels and severity of depressive symptoms in BD patients. This evidence suggests that BDNF may be an eventual biomarker for BD.
This result is consistent with one of the most replicated findings in the literature, the decreased peripheral levels of BDNF and its association with depressive symptoms [83,84]. Besides, a positive correlation has recently been found between severity of manic symptoms and BDNF levels in BD patients [85]. Moreover, other studies find lower BDNF levels in BD patients in manic and depressive phases compared to controls [86], but these differences were not significant across affective states in general [87]. Although evidence suggests that BDNF has an important role in the psychopathology and progression of BD [88], there are inconsistent findings due to a number of confounding factors in uncontrolled studies that highlight the need for specificity as a biomarker in the diagnosis of BD. BDNF plays an increasingly important role as a biomarker not only in affective disorders, but also in cognitive impairment, such as that associated with alcohol abuse. It will be important to identify whether the decrease in BDNF observed in BD could be associated with present or ulterior cognitive impairment in BD [89].
The present review and meta-analysis do not show consistent associations between the inflammatory biomarkers studied and the main psychiatric and clinical variables of the disorder. Persistent pathogens likely support a role of an altered immune system in the etiology of mood disorders [90]. In particular cases such as TNF-α, the previously proposed association with BD is not supported by the present meta-analysis, and this finding is supported by recent studies with monoclonal antibodies against this cytokine that showed no effects in the prefrontal neurochemistry of patients with BD [91]. In a systematic review and exploratory meta-analyses in which levels of neurotrophic, inflammatory and oxidative stress biomarkers were analyzed in combination as a function of an affective state (euthymia, mania, depression), no biomarkers were found that could be individually discriminative of each mood phase, with the combination of hsCRP/IL-6, sTNFR1 with BDNF/TNF-α being significant [58]. However, later studies suggest that elevated levels of CRP and TNF-α in manic, depressive, and mixed episodes would point to these substances as biomarkers of mood episode, whereas elevated IL-6 levels during euthymic could refer to a euthymic role as a trait biomarker in BD [92].
Overall, heterogeneity and inconsistency in previous studies are supporting the search for new potential targets with a clinical value in BD. Several additional inflammatory factors, such as specific chemokines (MCP-1, fractalkine), glial factors (GFAP, S100B), or lipid-derived mediators such as endocannabinoids, and neurodegeneration-related molecules such as neurofilament light chain, neurogranin and β-amyloid peptide isoforms (Aβ42, Aβ40, Aβ38) and their fragments could be promising biomarkers in patients with BD in relation to prospective clinical outcomes, such as those of neuronal injury, cognitive deficits and risk of dementia [93]. Recent studies have also evaluated non-coding RNA expression, sexual hormones, oxidative stress (uric acid, bilirubin, albumin) and metabolic biomarkers (metabolic syndrome, overweight/obesity, thyroid and liver function) in predicting BD and suicidality in individuals with bipolar disorder [94,95,96,97,98]. In addition, big data of cerebral blood flow and structural and functional connectivity using magnetic resonance imaging are becoming useful tools for actual practice in psychiatry [99,100]. By gathering all this information and using multivariable logistic regression, it could be possible to construct a model to predict BD.
Other results, such as the correlation between the biomarkers and bipolar subtypes, stage of disease, severity of manic symptoms and global severity of illness, were heterogeneous and should be analyzed with caution. Some studies found an association between biomarkers and other clinical variables included in the study, such as stressful life events, childhood trauma, cognitive abilities and functionality, but further studies are needed to confirm the relationship between inflammatory and neurotrophic factors and these variables. In general, more studies are necessary to understand precisely the neurobiology of BD and their interactions with stress and clinical factors. This improvement will presumably translate to more sophisticated treatments.
Taken together, although biomarkers and clinical, social and environmental factors have been shown to play an important role in understanding the etiopathology and development of bipolar disorder, these variables are not clinically replicable [101]. The clinical value of BDNF and other inflammatory biomarkers has yet to be demonstrated by highly controlled studies that follow a precise phenotyping (type, phase, severity, and comorbidities) of BD patients. Moreover, other promising biomarkers related to mitochondrial dysfunction, oxidative stress, metalloproteinases, HPA axis function, autoimmunity and urinary metabolites, among others, need to be studied [102,103].
Strengths and Limitations
This comprehensive systematic review includes a series of exploratory meta-analyses of neurotrophic and inflammatory factors in bipolar disorder. The results for each biomarker have been separated by clinical and social factors, attempting to provide information on the physiological changes that occur with the illness, and reducing the risk of type 2 error. The use of random effects models adds further validity to the results.
However, this review has several limitations and the results should be interpreted with caution. First, most of the studies were cross-sectional, and changes in trophic/inflammatory biomarkers throughout the development of BD in an individual patient cannot be described. Most of the studies reviewed were observational and at significant risk of bias and confounding, so causality cannot be established. Individual characteristics varied greatly between studies. Many studies included small samples and the aims between them were different. Some factors influencing biomarker levels, such as body mass index, physical activity, drug use, or blood pressure, were not addressed in many studies [104,105]. Some studies measured several cytokines, but the results were not reported due to a lack of sensitivity in assays that detected valid levels. Dilution and storage of blood samples and measurement factors in plasma or serum may also influence the variability and reproducibility of biomarker levels [106,107,108]. The influence of medication is not analyzed in most studies, while others include drug-naïve patients. The inclusion of patients followed different criteria for defining bipolar disorder (i.e., 2 days of hypomania vs. 4 days) and the variation in YMRS and depression scale scores for defining mood phase probably contributed to the heterogeneity of the results. Several clinical variables were assessed from clinical interviews only, which may compromise the reliability and validity of the results. Because of the need to separate results by clinical and social factors, a significant number of meta-analyses were performed, which increases the risk of type 1 error. The decision to perform the meta-analysis with only three studies is arbitrary, but we have taken this decision to increase our statistical power by reducing the standard error of the weighted average effect size. The purpose of our review was exploratory, so multiple testing was not corrected for, and the results should be considered with caution. In addition, it is likely that some meta-analyses were underpowered as a result of a small sample size and the small number of studies included. To determine the validity and precision of a potential biomarker, future methodologically consistent and repeatable studies are needed to allow homogeneity and comparability of results.
5. Conclusions
The present study shed light on the evidence supporting inflammatory and neurotrophic factors as reliable biomarkers that can characterize clinical features for BD. At the moment, the mixed and contradictory evidence regarding the association of inflammatory and neurotrophic factors with clinical features suggest that highly controlled studies with wide sample sizes need to be conducted. Probably, heterogeneous and small samples, selection bias, different methodologies and bias in the measurement of outcomes, lack of control regarding confounders and bias in the selection of the reported results could explain the mixed evidence found in this review. The meta-analysis clearly indicates that BDNF has a role in the depressive component of BD and more studies need to be conducted to establish the clinical value of this biomarker. The systematic review suggests a possible association between stressors, functional and cognitive impairment, and BDNF and/or inflammatory factors but the small number of studies do not permit to establish solid conclusions. Moreover, the poor consistency of promising inflammatory mediators such as IL-6 and TNF-α indicates the need for homogeneous studies that help identify additional biomarkers of this disorder.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/biomedicines10061368/s1, Table S1: Additional information on the 51 selected studies; Table S2: Summary of the number of studies included in the systematic review and meta-analysis; Table S3: Abbreviations of inflammatory and trophic factors; Annex 1: Details of the search strategy conducted in the present systematic review; Figure S1: Traffic light plot of the domain-level judgments for risk-of-bias assessment; Figure S2: Traffic light plot of the domain-level judgments for risk-of-bias assessment.
Author Contributions
Conception and design: F.M.-C., A.B., F.R.d.F., J.S. and J.G.-P. Data acquisition: A.V.-N. and C.G.-S.-L. Data analysis and interpretation: A.V.-N., C.G.-S.-L., J.S. and J.G.-P. Draft writing: A.V.-N., C.G.-S.-L., J.S. and J.G.-P. Review and editing: F.M.-C., A.B. and F.R.d.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Atención Primaria, Cronicidad y Promoción de la Salud: Red de Investigación en Atención Primaria de Adicciones (RIAPAd), Instituto de Salud Carlos III (ISCIII), Ministerio de Ciencia e Innovación and European Regional Development Funds-European Union (ERDF-EU), grant number RD21/0009/0003; ISCIII, ERDF-EU, grant number PI19/01577; Ministerio de Sanidad, Delegación de Gobierno para el Plan Nacional sobre Drogas, grant numbers PND 2019/040; and Consejería de Salud y Familia, Junta de Andalucía, grant numbers RIC-0111-2019. AV-N (CM19/00025) and CG-S-L (CM19/00240) hold “Rio Hortega” research contracts from the National System of Health, ISCIII, ERDF-EU. FM-C and JG-P has received funding from the Andalusia Government in the grants for human resources reinforcement in the research activity (Acción A de intensificación 2019 and Acción B de refuerzos de larga duración 2014). The funding sources had no further role in study design; in the collection, analysis and interpretation of data; in writing of the report; and in the decision to submit the paper for publication. Funding for open access charge: Universidad de Málaga/CBUA.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Merikangas, K.R.; Jin, R.; He, J.-P.; Kessler, R.C.; Lee, S.; Sampson, N.A.; Viana, M.C.; Andrade, L.H.; Hu, C.; Karam, E.G.; et al. Prevalence and Correlates of Bipolar Spectrum Disorder in the World Mental Health Survey Initiative. Arch. Gen. Psychiatry 2011, 68, 241–251. [Google Scholar] [CrossRef] [PubMed]
- Alonso, J.; Petukhova, M.; Vilagut, G.; Chatterji, S.; Heeringa, S.; Üstün, T.B.; Alhamzawi, A.O.; Viana, M.C.; Angermeyer, M.; Bromet, E.; et al. Days out of Role Due to Common Physical and Mental Conditions: Results from the WHO World Mental Health Surveys. Mol. Psychiatry 2011, 16, 1234–1246. [Google Scholar] [CrossRef] [PubMed]
- Merikangas, K.R.; Akiskal, H.S.; Angst, J.; Greenberg, P.E.; Hirschfeld, R.M.A.; Petukhova, M.; Kessler, R.C. Lifetime and 12-Month Prevalence of Bipolar Spectrum Disorder in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 2007, 64, 543–552. [Google Scholar] [CrossRef] [PubMed]
- McIntyre, R.S.; Konarski, J.Z.; Yatham, L.N. Comorbidity in Bipolar Disorder: A Framework for Rational Treatment Selection. Hum. Psychopharmacol. 2004, 19, 369–386. [Google Scholar] [CrossRef]
- Staudt Hansen, P.; Frahm Laursen, M.; Grøntved, S.; Puggard Vogt Straszek, S.; Licht, R.W.; Nielsen, R.E. Increasing Mortality Gap for Patients Diagnosed with Bipolar Disorder-A Nationwide Study with 20 Years of Follow-Up. Bipolar Disord. 2019, 21, 270–275. [Google Scholar] [CrossRef]
- Osby, U.; Brandt, L.; Correia, N.; Ekbom, A.; Sparén, P. Excess Mortality in Bipolar and Unipolar Disorder in Sweden. Arch. Gen. Psychiatry 2001, 58, 844–850. [Google Scholar] [CrossRef]
- Gonda, X.; Pompili, M.; Serafini, G.; Montebovi, F.; Campi, S.; Dome, P.; Duleba, T.; Girardi, P.; Rihmer, Z. Suicidal Behavior in Bipolar Disorder: Epidemiology, Characteristics and Major Risk Factors. J. Affect. Disord. 2012, 143, 16–26. [Google Scholar] [CrossRef]
- McIntyre, R.S.; Berk, M.; Brietzke, E.; Goldstein, B.I.; López-Jaramillo, C.; Kessing, L.V.; Malhi, G.S.; Nierenberg, A.A.; Rosenblat, J.D.; Majeed, A.; et al. Bipolar Disorders. Lancet Lond. Engl. 2020, 396, 1841–1856. [Google Scholar] [CrossRef]
- Pompili, M.; Gonda, X.; Serafini, G.; Innamorati, M.; Sher, L.; Amore, M.; Rihmer, Z.; Girardi, P. Epidemiology of Suicide in Bipolar Disorders: A Systematic Review of the Literature. Bipolar Disord. 2013, 15, 457–490. [Google Scholar] [CrossRef]
- Perlis, R.H.; Dennehy, E.B.; Miklowitz, D.J.; Delbello, M.P.; Ostacher, M.; Calabrese, J.R.; Ametrano, R.M.; Wisniewski, S.R.; Bowden, C.L.; Thase, M.E.; et al. Retrospective Age at Onset of Bipolar Disorder and Outcome during Two-Year Follow-up: Results from the STEP-BD Study. Bipolar Disord. 2009, 11, 391–400. [Google Scholar] [CrossRef]
- Nivoli, A.M.A.; Pacchiarotti, I.; Rosa, A.R.; Popovic, D.; Murru, A.; Valenti, M.; Bonnin, C.M.; Grande, I.; Sanchez-Moreno, J.; Vieta, E.; et al. Gender Differences in a Cohort Study of 604 Bipolar Patients: The Role of Predominant Polarity. J. Affect. Disord. 2011, 133, 443–449. [Google Scholar] [CrossRef] [PubMed]
- Phillips, M.L.; Kupfer, D.J. Bipolar Disorder Diagnosis: Challenges and Future Directions. Lancet Lond. Engl. 2013, 381, 1663–1671. [Google Scholar] [CrossRef]
- Bortolato, B.; Miskowiak, K.W.; Köhler, C.A.; Vieta, E.; Carvalho, A.F. Cognitive Dysfunction in Bipolar Disorder and Schizophrenia: A Systematic Review of Meta-Analyses. Neuropsychiatr. Dis. Treat. 2015, 11, 3111–3125. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Aran, A.; Vieta, E.; Torrent, C.; Sanchez-Moreno, J.; Goikolea, J.M.; Salamero, M.; Malhi, G.S.; Gonzalez-Pinto, A.; Daban, C.; Alvarez-Grandi, S.; et al. Functional Outcome in Bipolar Disorder: The Role of Clinical and Cognitive Factors. Bipolar Disord. 2007, 9, 103–113. [Google Scholar] [CrossRef]
- Martinez-Aran, A.; Vieta, E. Cognition as a Target in Schizophrenia, Bipolar Disorder and Depression. Eur. Neuropsychopharmacol. J. Eur. Coll. Neuropsychopharmacol. 2015, 25, 151–157. [Google Scholar] [CrossRef]
- Torres, I.J.; Boudreau, V.G.; Yatham, L.N. Neuropsychological Functioning in Euthymic Bipolar Disorder: A Meta-Analysis. Acta Psychiatr. Scand. Suppl. 2007, 116, 17–26. [Google Scholar] [CrossRef]
- Torres, I.J.; DeFreitas, V.G.; DeFreitas, C.M.; Kauer-Sant’Anna, M.; Bond, D.J.; Honer, W.G.; Lam, R.W.; Yatham, L.N. Neurocognitive Functioning in Patients with Bipolar I Disorder Recently Recovered from a First Manic Episode. J. Clin. Psychiatry 2010, 71, 1234–1242. [Google Scholar] [CrossRef]
- Lee, R.S.C.; Hermens, D.F.; Scott, J.; Redoblado-Hodge, M.A.; Naismith, S.L.; Lagopoulos, J.; Griffiths, K.R.; Porter, M.A.; Hickie, I.B. A Meta-Analysis of Neuropsychological Functioning in First-Episode Bipolar Disorders. J. Psychiatr. Res. 2014, 57, 1–11. [Google Scholar] [CrossRef]
- Martino, D.J.; Samamé, C.; Ibañez, A.; Strejilevich, S.A. Neurocognitive Functioning in the Premorbid Stage and in the First Episode of Bipolar Disorder: A Systematic Review. Psychiatry Res. 2015, 226, 23–30. [Google Scholar] [CrossRef]
- Grande, I.; Goikolea, J.M.; de Dios, C.; González-Pinto, A.; Montes, J.M.; Saiz-Ruiz, J.; Prieto, E.; Vieta, E.; PREBIS group. Occupational Disability in Bipolar Disorder: Analysis of Predictors of Being on Severe Disablement Benefit (PREBIS Study Data). Acta Psychiatr. Scand. 2013, 127, 403–411. [Google Scholar] [CrossRef]
- Hirschfeld, R.M.A.; Lewis, L.; Vornik, L.A. Perceptions and Impact of Bipolar Disorder: How Far Have We Really Come? Results of the National Depressive and Manic-Depressive Association 2000 Survey of Individuals with Bipolar Disorder. J. Clin. Psychiatry 2003, 64, 161–174. [Google Scholar] [CrossRef] [PubMed]
- Solé, B.; Jiménez, E.; Torrent, C.; Reinares, M.; Bonnin, C.D.M.; Torres, I.; Varo, C.; Grande, I.; Valls, E.; Salagre, E.; et al. Cognitive Impairment in Bipolar Disorder: Treatment and Prevention Strategies. Int. J. Neuropsychopharmacol. 2017, 20, 670–680. [Google Scholar] [CrossRef]
- Lima, I.M.M.; Peckham, A.D.; Johnson, S.L. Cognitive Deficits in Bipolar Disorders: Implications for Emotion. Clin. Psychol. Rev. 2018, 59, 126–136. [Google Scholar] [CrossRef]
- Battaglia, S.; Serio, G.; Scarpazza, C.; D’Ausilio, A.; Borgomaneri, S. Frozen in (e)Motion: How Reactive Motor Inhibition Is Influenced by the Emotional Content of Stimuli in Healthy and Psychiatric Populations. Behav. Res. Ther. 2021, 146, 103963. [Google Scholar] [CrossRef]
- Baune, B.T.; Malhi, G.S. A Review on the Impact of Cognitive Dysfunction on Social, Occupational, and General Functional Outcomes in Bipolar Disorder. Bipolar Disord. 2015, 17 (Suppl. S2), 41–55. [Google Scholar] [CrossRef]
- Depp, C.A.; Mausbach, B.T.; Harmell, A.L.; Savla, G.N.; Bowie, C.R.; Harvey, P.D.; Patterson, T.L. Meta-Analysis of the Association between Cognitive Abilities and Everyday Functioning in Bipolar Disorder. Bipolar Disord. 2012, 14, 217–226. [Google Scholar] [CrossRef]
- Mackala, S.A.; Torres, I.J.; Kozicky, J.; Michalak, E.E.; Yatham, L.N. Cognitive Performance and Quality of Life Early in the Course of Bipolar Disorder. J. Affect. Disord. 2014, 168, 119–124. [Google Scholar] [CrossRef]
- Mora, E.; Portella, M.J.; Forcada, I.; Vieta, E.; Mur, M. Persistence of Cognitive Impairment and Its Negative Impact on Psychosocial Functioning in Lithium-Treated, Euthymic Bipolar Patients: A 6-Year Follow-up Study. Psychol. Med. 2013, 43, 1187–1196. [Google Scholar] [CrossRef]
- Johnson, S.L.; Carver, C.S. Emotion-Relevant Impulsivity Predicts Sustained Anger and Aggression after Remission in Bipolar I Disorder. J. Affect. Disord. 2016, 189, 169–175. [Google Scholar] [CrossRef]
- Johnson, S.L.; Carver, C.S.; Tharp, J.A. Suicidality in Bipolar Disorder: The Role of Emotion-Triggered Impulsivity. Suicide Life. Threat. Behav. 2017, 47, 177–192. [Google Scholar] [CrossRef]
- Miller, J.N.; Black, D.W. Bipolar Disorder and Suicide: A Review. Curr. Psychiatry Rep. 2020, 22, 6. [Google Scholar] [CrossRef]
- Ramírez-Martín, A.; Ramos-Martín, J.; Mayoral-Cleries, F.; Moreno-Küstner, B.; Guzman-Parra, J. Impulsivity, Decision-Making and Risk-Taking Behaviour in Bipolar Disorder: A Systematic Review and Meta-Analysis. Psychol. Med. 2020, 50, 2141–2153. [Google Scholar] [CrossRef]
- Zakowicz, P.; Skibińska, M.; Wasicka-Przewoźna, K.; Skulimowski, B.; Waśniewski, F.; Chorzepa, A.; Różański, M.; Twarowska-Hauser, J.; Pawlak, J. Impulsivity as a Risk Factor for Suicide in Bipolar Disorder. Front. Psychiatry 2021, 12, 706933. [Google Scholar] [CrossRef]
- Gvion, Y.; Levi-Belz, Y.; Hadlaczky, G.; Apter, A. On the Role of Impulsivity and Decision-Making in Suicidal Behavior. World J. Psychiatry 2015, 5, 255–259. [Google Scholar] [CrossRef]
- Battaglia, S.; Fabius, J.H.; Moravkova, K.; Fracasso, A.; Borgomaneri, S. The Neurobiological Correlates of Gaze Perception in Healthy Individuals and Neurologic Patients. Biomedicines 2022, 10, 627. [Google Scholar] [CrossRef]
- Tanaka, M.; Tóth, F.; Polyák, H.; Szabó, Á.; Mándi, Y.; Vécsei, L. Immune Influencers in Action: Metabolites and Enzymes of the Tryptophan-Kynurenine Metabolic Pathway. Biomedicines 2021, 9, 734. [Google Scholar] [CrossRef]
- Rodrigues, J.E.; Martinho, A.; Santos, V.; Santa, C.; Madeira, N.; Martins, M.J.; Pato, C.N.; Macedo, A.; Manadas, B. Systematic Review and Meta-Analysis on MS-Based Proteomics Applied to Human Peripheral Fluids to Assess Potential Biomarkers of Bipolar Disorder. Int. J. Mol. Sci. 2022, 23, 5460. [Google Scholar] [CrossRef]
- Fabbri, C. The Role of Genetics in Bipolar Disorder. Curr. Top. Behav. Neurosci. 2021, 48, 41–60. [Google Scholar] [CrossRef]
- Johansson, V.; Kuja-Halkola, R.; Cannon, T.D.; Hultman, C.M.; Hedman, A.M. A Population-Based Heritability Estimate of Bipolar Disorder—In a Swedish Twin Sample. Psychiatry Res. 2019, 278, 180–187. [Google Scholar] [CrossRef]
- Craddock, N.; Jones, I. Genetics of Bipolar Disorder. J. Med. Genet. 1999, 36, 585–594. [Google Scholar] [CrossRef]
- Craddock, N.; Sklar, P. Genetics of Bipolar Disorder. Lancet Lond. Engl. 2013, 381, 1654–1662. [Google Scholar] [CrossRef]
- Grande, I.; Berk, M.; Birmaher, B.; Vieta, E. Bipolar Disorder. Lancet Lond. Engl. 2016, 387, 1561–1572. [Google Scholar] [CrossRef]
- Kendler, K.S. Reflections on the Relationship between Psychiatric Genetics and Psychiatric Nosology. Am. J. Psychiatry 2006, 163, 1138–1146. [Google Scholar] [CrossRef]
- Sanches, M.; Keshavan, M.S.; Brambilla, P.; Soares, J.C. Neurodevelopmental Basis of Bipolar Disorder: A Critical Appraisal. Prog. Neuropsychopharmacol. Biol. Psychiatry 2008, 32, 1617–1627. [Google Scholar] [CrossRef]
- Bora, E. Developmental Trajectory of Cognitive Impairment in Bipolar Disorder: Comparison with Schizophrenia. Eur. Neuropsychopharmacol. J. Eur. Coll. Neuropsychopharmacol. 2015, 25, 158–168. [Google Scholar] [CrossRef]
- Joseph, M.F.; Frazier, T.W.; Youngstrom, E.A.; Soares, J.C. A Quantitative and Qualitative Review of Neurocognitive Performance in Pediatric Bipolar Disorder. J. Child Adolesc. Psychopharmacol. 2008, 18, 595–605. [Google Scholar] [CrossRef]
- Post, R.M.; Fleming, J.; Kapczinski, F. Neurobiological Correlates of Illness Progression in the Recurrent Affective Disorders. J. Psychiatr. Res. 2012, 46, 561–573. [Google Scholar] [CrossRef]
- Arts, B.; Jabben, N.; Krabbendam, L.; van Os, J. Meta-Analyses of Cognitive Functioning in Euthymic Bipolar Patients and Their First-Degree Relatives. Psychol. Med. 2008, 38, 771–785. [Google Scholar] [CrossRef]
- Balanzá-Martínez, V.; Rubio, C.; Selva-Vera, G.; Martinez-Aran, A.; Sánchez-Moreno, J.; Salazar-Fraile, J.; Vieta, E.; Tabarés-Seisdedos, R. Neurocognitive Endophenotypes (Endophenocognitypes) from Studies of Relatives of Bipolar Disorder Subjects: A Systematic Review. Neurosci. Biobehav. Rev. 2008, 32, 1426–1438. [Google Scholar] [CrossRef]
- Bora, E.; Yucel, M.; Pantelis, C. Cognitive Endophenotypes of Bipolar Disorder: A Meta-Analysis of Neuropsychological Deficits in Euthymic Patients and Their First-Degree Relatives. J. Affect. Disord. 2009, 113, 1–20. [Google Scholar] [CrossRef]
- Tanaka, M.; Vécsei, L. Editorial of Special Issue “Crosstalk between Depression, Anxiety, and Dementia: Comorbidity in Behavioral Neurology and Neuropsychiatry”. Biomedicines 2021, 9, 517. [Google Scholar] [CrossRef]
- Goldstein, B.I.; Kemp, D.E.; Soczynska, J.K.; McIntyre, R.S. Inflammation and the Phenomenology, Pathophysiology, Comorbidity, and Treatment of Bipolar Disorder: A Systematic Review of the Literature. J. Clin. Psychiatry 2009, 70, 1078–1090. [Google Scholar] [CrossRef]
- Rosenblat, J.D.; Cha, D.S.; Mansur, R.B.; McIntyre, R.S. Inflamed Moods: A Review of the Interactions between Inflammation and Mood Disorders. Prog. Neuropsychopharmacol. Biol. Psychiatry 2014, 53, 23–34. [Google Scholar] [CrossRef]
- Rosenblat, J.D.; McIntyre, R.S. Bipolar Disorder and Inflammation. Psychiatr. Clin. N. Am. 2016, 39, 125–137. [Google Scholar] [CrossRef]
- Munkholm, K.; Braüner, J.V.; Kessing, L.V.; Vinberg, M. Cytokines in Bipolar Disorder vs. Healthy Control Subjects: A Systematic Review and Meta-Analysis. J. Psychiatr. Res. 2013, 47, 1119–1133. [Google Scholar] [CrossRef]
- Sayana, P.; Colpo, G.D.; Simões, L.R.; Giridharan, V.V.; Teixeira, A.L.; Quevedo, J.; Barichello, T. A Systematic Review of Evidence for the Role of Inflammatory Biomarkers in Bipolar Patients. J. Psychiatr. Res. 2017, 92, 160–182. [Google Scholar] [CrossRef]
- Grande, I.; Fries, G.R.; Kunz, M.; Kapczinski, F. The Role of BDNF as a Mediator of Neuroplasticity in Bipolar Disorder. Psychiatry Investig. 2010, 7, 243–250. [Google Scholar] [CrossRef]
- Rowland, T.; Perry, B.I.; Upthegrove, R.; Barnes, N.; Chatterjee, J.; Gallacher, D.; Marwaha, S. Neurotrophins, Cytokines, Oxidative Stress Mediators and Mood State in Bipolar Disorder: Systematic Review and Meta-Analyses. Br. J. Psychiatry 2018, 213, 514–525. [Google Scholar] [CrossRef]
- Gordovez, F.J.A.; McMahon, F.J. The Genetics of Bipolar Disorder. Mol. Psychiatry 2020, 25, 544–559. [Google Scholar] [CrossRef]
- Duffy, A.; Goodday, S.M.; Keown-Stoneman, C.; Scotti, M.; Maitra, M.; Nagy, C.; Horrocks, J.; Turecki, G. Epigenetic Markers in Inflammation-Related Genes Associated with Mood Disorder: A Cross-Sectional and Longitudinal Study in High-Risk Offspring of Bipolar Parents. Int. J. Bipolar Disord. 2019, 7, 17. [Google Scholar] [CrossRef]
- Alameda, L.; Trotta, G.; Quigley, H.; Rodriguez, V.; Gadelrab, R.; Dwir, D.; Dempster, E.; Wong, C.C.Y.; Forti, M.D. Can Epigenetics Shine a Light on the Biological Pathways Underlying Major Mental Disorders? Psychol. Med. 2022, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Marangoni, C.; Hernandez, M.; Faedda, G.L. The Role of Environmental Exposures as Risk Factors for Bipolar Disorder: A Systematic Review of Longitudinal Studies. J. Affect. Disord. 2016, 193, 165–174. [Google Scholar] [CrossRef] [PubMed]
- Marangoni, C.; Faedda, G.L.; Baldessarini, R.J. Clinical and Environmental Risk Factors for Bipolar Disorder: Review of Prospective Studies. Harv. Rev. Psychiatry 2018, 26, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Aldinger, F.; Schulze, T.G. Environmental Factors, Life Events, and Trauma in the Course of Bipolar Disorder. Psychiatry Clin. Neurosci. 2017, 71, 6–17. [Google Scholar] [CrossRef]
- Bortolato, B.; Köhler, C.A.; Evangelou, E.; León-Caballero, J.; Solmi, M.; Stubbs, B.; Belbasis, L.; Pacchiarotti, I.; Kessing, L.V.; Berk, M.; et al. Systematic Assessment of Environmental Risk Factors for Bipolar Disorder: An Umbrella Review of Systematic Reviews and Meta-Analyses. Bipolar Disord. 2017, 19, 84–96. [Google Scholar] [CrossRef]
- Barichello, T.; Badawy, M.; Pitcher, M.R.; Saigal, P.; Generoso, J.S.; Goularte, J.A.; Simões, L.R.; Quevedo, J.; Carvalho, A.F. Exposure to Perinatal Infections and Bipolar Disorder: A Systematic Review. Curr. Mol. Med. 2016, 16, 106–118. [Google Scholar] [CrossRef]
- Pugliese, V.; Bruni, A.; Carbone, E.A.; Calabrò, G.; Cerminara, G.; Sampogna, G.; Luciano, M.; Steardo, L.; Fiorillo, A.; Garcia, C.S.; et al. Maternal Stress, Prenatal Medical Illnesses and Obstetric Complications: Risk Factors for Schizophrenia Spectrum Disorder, Bipolar Disorder and Major Depressive Disorder. Psychiatry Res. 2019, 271, 23–30. [Google Scholar] [CrossRef]
- Garno, J.L.; Goldberg, J.F.; Ramirez, P.M.; Ritzler, B.A. Impact of Childhood Abuse on the Clinical Course of Bipolar Disorder. Br. J. Psychiatry J. Ment. Sci. 2005, 186, 121–125. [Google Scholar] [CrossRef]
- Agnew-Blais, J.; Danese, A. Childhood Maltreatment and Unfavourable Clinical Outcomes in Bipolar Disorder: A Systematic Review and Meta-Analysis. Lancet Psychiatry 2016, 3, 342–349. [Google Scholar] [CrossRef]
- Palmier-Claus, J.E.; Berry, K.; Bucci, S.; Mansell, W.; Varese, F. Relationship between Childhood Adversity and Bipolar Affective Disorder: Systematic Review and Meta-Analysis. Br. J. Psychiatry J. Ment. Sci. 2016, 209, 454–459. [Google Scholar] [CrossRef]
- Gershon, A.; Johnson, S.L.; Miller, I. Chronic Stressors and Trauma: Prospective Influences on the Course of Bipolar Disorder. Psychol. Med. 2013, 43, 2583–2592. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Koenders, M.A.; Giltay, E.J.; Spijker, A.T.; Hoencamp, E.; Spinhoven, P.; Elzinga, B.M. Stressful Life Events in Bipolar I and II Disorder: Cause or Consequence of Mood Symptoms? J. Affect. Disord. 2014, 161, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Simhandl, C.; Radua, J.; König, B.; Amann, B.L. The Prevalence and Effect of Life Events in 222 Bipolar I and II Patients: A Prospective, Naturalistic 4 Year Follow-up Study. J. Affect. Disord. 2015, 170, 166–171. [Google Scholar] [CrossRef]
- Schepis, T.S.; Hakes, J.K. Non-Medical Prescription Use Increases the Risk for the Onset and Recurrence of Psychopathology: Results from the National Epidemiological Survey on Alcohol and Related Conditions. Addict. Abingdon Engl. 2011, 106, 2146–2155. [Google Scholar] [CrossRef] [PubMed]
- Feingold, D.; Weiser, M.; Rehm, J.; Lev-Ran, S. The Association between Cannabis Use and Mood Disorders: A Longitudinal Study. J. Affect. Disord. 2015, 172, 211–218. [Google Scholar] [CrossRef] [PubMed]
- Miller, S.; Hallmayer, J.; Wang, P.W.; Hill, S.J.; Johnson, S.L.; Ketter, T.A. Brain-Derived Neurotrophic Factor Val66met Genotype and Early Life Stress Effects upon Bipolar Course. J. Psychiatr. Res. 2013, 47, 252–258. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 Statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef]
- Leucht, S.; Fennema, H.; Engel, R.R.; Kaspers-Janssen, M.; Szegedi, A. Translating the HAM-D into the MADRS and Vice Versa with Equipercentile Linking. J. Affect. Disord. 2018, 226, 326–331. [Google Scholar] [CrossRef]
- IntHout, J.; Ioannidis, J.P.A.; Borm, G.F. The Hartung-Knapp-Sidik-Jonkman Method for Random Effects Meta-Analysis Is Straightforward and Considerably Outperforms the Standard DerSimonian-Laird Method. BMC Med. Res. Methodol. 2014, 14, 25. [Google Scholar] [CrossRef]
- Hartung, J.; Knapp, G. On Tests of the Overall Treatment Effect in Meta-Analysis with Normally Distributed Responses. Stat. Med. 2001, 20, 1771–1782. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Sutton, A.J.; Ioannidis, J.P.A.; Terrin, N.; Jones, D.R.; Lau, J.; Carpenter, J.; Rücker, G.; Harbord, R.M.; Schmid, C.H.; et al. Recommendations for Examining and Interpreting Funnel Plot Asymmetry in Meta-Analyses of Randomised Controlled Trials. BMJ 2011, 343, d4002. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A Tool for Assessing Risk of Bias in Non-Randomised Studies of Interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed]
- Arosio, B.; Guerini, F.R.; Voshaar, R.C.O.; Aprahamian, I. Blood Brain-Derived Neurotrophic Factor (BDNF) and Major Depression: Do We Have a Translational Perspective? Front. Behav. Neurosci. 2021, 15, 626906. [Google Scholar] [CrossRef]
- Fernandes, B.S.; Berk, M.; Turck, C.W.; Steiner, J.; Gonçalves, C.-A. Decreased Peripheral Brain-Derived Neurotrophic Factor Levels Are a Biomarker of Disease Activity in Major Psychiatric Disorders: A Comparative Meta-Analysis. Mol. Psychiatry 2014, 19, 750–751. [Google Scholar] [CrossRef]
- Chiou, Y.-J.; Huang, T.-L. Brain-Derived Neurotrophic Factor (BDNF) and Bipolar Disorder. Psychiatry Res. 2019, 274, 395–399. [Google Scholar] [CrossRef]
- Fernandes, B.S.; Molendijk, M.L.; Köhler, C.A.; Soares, J.C.; Leite, C.M.G.S.; Machado-Vieira, R.; Ribeiro, T.L.; Silva, J.C.; Sales, P.M.G.; Quevedo, J.; et al. Peripheral Brain-Derived Neurotrophic Factor (BDNF) as a Biomarker in Bipolar Disorder: A Meta-Analysis of 52 Studies. BMC Med. 2015, 13, 289. [Google Scholar] [CrossRef]
- Munkholm, K.; Vinberg, M.; Kessing, L.V. Peripheral Blood Brain-Derived Neurotrophic Factor in Bipolar Disorder: A Comprehensive Systematic Review and Meta-Analysis. Mol. Psychiatry 2016, 21, 216–228. [Google Scholar] [CrossRef]
- Fernandes, B.S.; Gama, C.S.; Ceresér, K.M.; Yatham, L.N.; Fries, G.R.; Colpo, G.; de Lucena, D.; Kunz, M.; Gomes, F.A.; Kapczinski, F. Brain-Derived Neurotrophic Factor as a State-Marker of Mood Episodes in Bipolar Disorders: A Systematic Review and Meta-Regression Analysis. J. Psychiatr. Res. 2011, 45, 995–1004. [Google Scholar] [CrossRef]
- Silva-Peña, D.; García-Marchena, N.; Alén, F.; Araos, P.; Rivera, P.; Vargas, A.; García-Fernández, M.I.; Martín-Velasco, A.I.; Villanúa, M.Á.; Castilla-Ortega, E.; et al. Alcohol-Induced Cognitive Deficits Are Associated with Decreased Circulating Levels of the Neurotrophin BDNF in Humans and Rats. Addict. Biol. 2019, 24, 1019–1033. [Google Scholar] [CrossRef]
- Simanek, A.M.; Parry, A.; Dowd, J.B. Differences in the Association between Persistent Pathogens and Mood Disorders among Young- to Middle-Aged Women and Men in the U.S. Brain Behav. Immun. 2018, 68, 56–65. [Google Scholar] [CrossRef]
- Mansur, R.B.; Subramaniapillai, M.; Lee, Y.; Pan, Z.; Carmona, N.E.; Shekotikhina, M.; Iacobucci, M.; Rodrigues, N.; Nasri, F.; Rosenblat, J.D.; et al. Effects of Infliximab on Brain Neurochemistry of Adults with Bipolar Depression. J. Affect. Disord. 2021, 281, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Solmi, M.; Suresh Sharma, M.; Osimo, E.F.; Fornaro, M.; Bortolato, B.; Croatto, G.; Miola, A.; Vieta, E.; Pariante, C.M.; Smith, L.; et al. Peripheral Levels of C-Reactive Protein, Tumor Necrosis Factor-α, Interleukin-6, and Interleukin-1β across the Mood Spectrum in Bipolar Disorder: A Meta-Analysis of Mean Differences and Variability. Brain Behav. Immun. 2021, 97, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Knorr, U.; Simonsen, A.H.; Jensen, C.S.; Zetterberg, H.; Blennow, K.; Akhøj, M.; Forman, J.; Hasselbalch, S.G.; Kessing, L.V. Alzheimer’s Disease Related Biomarkers in Bipolar Disorder—A Longitudinal One-Year Case-Control Study. J. Affect. Disord. 2022, 297, 623–633. [Google Scholar] [CrossRef] [PubMed]
- Maloum, Z.; Taheri, M.; Ghafouri-Fard, S.; Shirvani-Farsani, Z. Significant Reduction of Long Non-Coding RNAs Expression in Bipolar Disorder. BMC Psychiatry 2022, 22, 256. [Google Scholar] [CrossRef] [PubMed]
- Steinacker, P.; Al Shweiki, M.R.; Oeckl, P.; Graf, H.; Ludolph, A.C.; Schönfeldt-Lecuona, C.; Otto, M. Glial Fibrillary Acidic Protein as Blood Biomarker for Differential Diagnosis and Severity of Major Depressive Disorder. J. Psychiatr. Res. 2021, 144, 54–58. [Google Scholar] [CrossRef]
- Isgren, A.; Sellgren, C.; Ekman, C.-J.; Holmén-Larsson, J.; Blennow, K.; Zetterberg, H.; Jakobsson, J.; Landén, M. Markers of Neuroinflammation and Neuronal Injury in Bipolar Disorder: Relation to Prospective Clinical Outcomes. Brain Behav. Immun. 2017, 65, 195–201. [Google Scholar] [CrossRef]
- Niu, Z.; Wu, X.; Zhu, Y.; Yang, L.; Shi, Y.; Wang, Y.; Qiu, H.; Gu, W.; Wu, Y.; Long, X.; et al. Early Diagnosis of Bipolar Disorder Coming Soon: Application of an Oxidative Stress Injury Biomarker (BIOS) Model. Neurosci. Bull. 2022. [Google Scholar] [CrossRef]
- Stenzel, C.; Dalkner, N.; Unterrainer, H.-F.; Birner, A.; Bengesser, S.A.; Fellendorf, F.T.; Fink, A.; Fleischmann, E.; Lenger, M.; Maget, A.; et al. Effects of Metabolic Syndrome and Obesity on Suicidality in Individuals with Bipolar Disorder. J. Affect. Disord. 2022, 311, 1–7. [Google Scholar] [CrossRef]
- Wei, Y.; Womer, F.Y.; Sun, K.; Zhu, Y.; Sun, D.; Duan, J.; Zhang, R.; Wei, S.; Jiang, X.; Zhang, Y.; et al. Applying Dimensional Psychopathology: Transdiagnostic Prediction of Executive Cognition Using Brain Connectivity and Inflammatory Biomarkers. Psychol. Med. 2022, 1–11. [Google Scholar] [CrossRef]
- Cattarinussi, G.; Kubera, K.M.; Hirjak, D.; Wolf, R.C.; Sambataro, F. Neural Correlates of the Risk for Schizophrenia and Bipolar Disorder: A Meta-Analysis of Structural and Functional Neuroimaging Studies. Biol. Psychiatry, 2022; S0006-3223(22)01068-X, in press. [Google Scholar] [CrossRef]
- Sagar, R.; Pattanayak, R.D. Potential Biomarkers for Bipolar Disorder: Where Do We Stand? Indian J. Med. Res. 2017, 145, 7–16. [Google Scholar] [CrossRef]
- Scola, G.; Andreazza, A.C. Current State of Biomarkers in Bipolar Disorder. Curr. Psychiatry Rep. 2014, 16, 514. [Google Scholar] [CrossRef] [PubMed]
- Sigitova, E.; Fišar, Z.; Hroudová, J.; Cikánková, T.; Raboch, J. Biological Hypotheses and Biomarkers of Bipolar Disorder. Psychiatry Clin. Neurosci. 2017, 71, 77–103. [Google Scholar] [CrossRef] [PubMed]
- Figueiredo, C.; Antunes, B.M.; Giacon, T.R.; Vanderlei, L.C.M.; Campos, E.Z.; Peres, F.P.; Clark, N.W.; Panissa, V.L.G.; Lira, F.S. Influence of Acute and Chronic High-Intensity Intermittent Aerobic Plus Strength Exercise on BDNF, Lipid and Autonomic Parameters. J. Sports Sci. Med. 2019, 18, 359–368. [Google Scholar]
- Haack, M.; Hinze-Selch, D.; Fenzel, T.; Kraus, T.; Kühn, M.; Schuld, A.; Pollmächer, T. Plasma Levels of Cytokines and Soluble Cytokine Receptors in Psychiatric Patients upon Hospital Admission: Effects of Confounding Factors and Diagnosis. J. Psychiatr. Res. 1999, 33, 407–418. [Google Scholar] [CrossRef]
- Rosenberg-Hasson, Y.; Hansmann, L.; Liedtke, M.; Herschmann, I.; Maecker, H.T. Effects of Serum and Plasma Matrices on Multiplex Immunoassays. Immunol. Res. 2014, 58, 224–233. [Google Scholar] [CrossRef] [PubMed]
- Vincent, F.B.; Nim, H.T.; Lee, J.P.W.; Morand, E.F.; Harris, J. Effect of Storage Duration on Cytokine Stability in Human Serum and Plasma. Cytokine 2019, 113, 453–457. [Google Scholar] [CrossRef]
- Gejl, A.K.; Enevold, C.; Bugge, A.; Andersen, M.S.; Nielsen, C.H.; Andersen, L.B. Associations between Serum and Plasma Brain-Derived Neurotrophic Factor and Influence of Storage Time and Centrifugation Strategy. Sci. Rep. 2019, 9, 9655. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).