An Integrative Model of Self-Regulation in Type 2 Diabetes Self-Management: A Systematic Review of Individual and Family-Based Interventions
Highlights
- Self-regulation-based interventions effectively enhance self-care behaviors, knowledge, and self-efficacy among patients with type 2 diabetes.
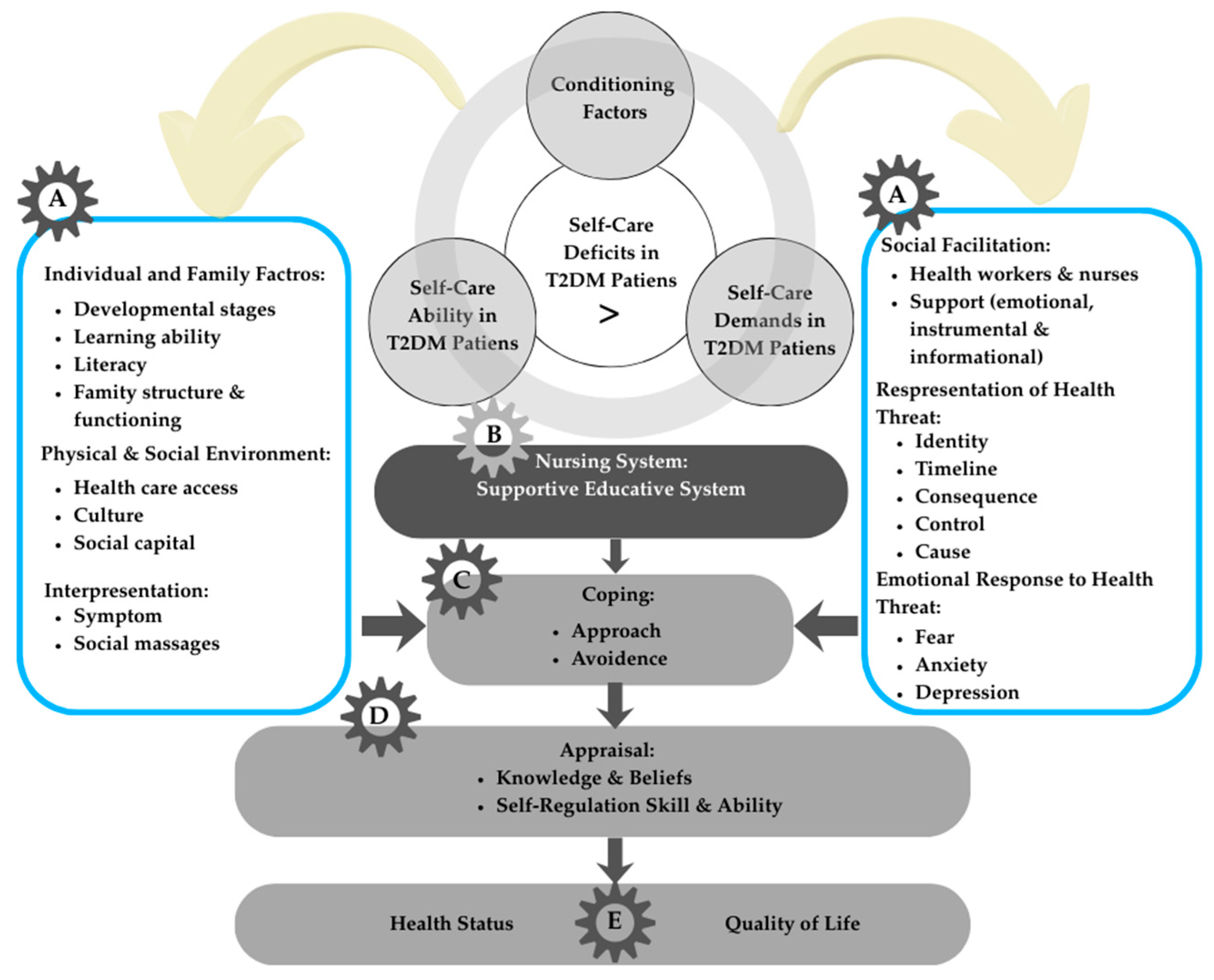
- The integrative model proposed in this systematic review explains the relationship between disease interpretation, coping strategies, and family involvement in diabetes self-management.
- The new integrative model can guide healthcare professionals in designing more comprehensive and patient-centered diabetes education programs.
- Strengthening self-regulation and family support is essential to improve glycemic control and quality of life among patients with type 2 diabetes.
Abstract
1. Introduction
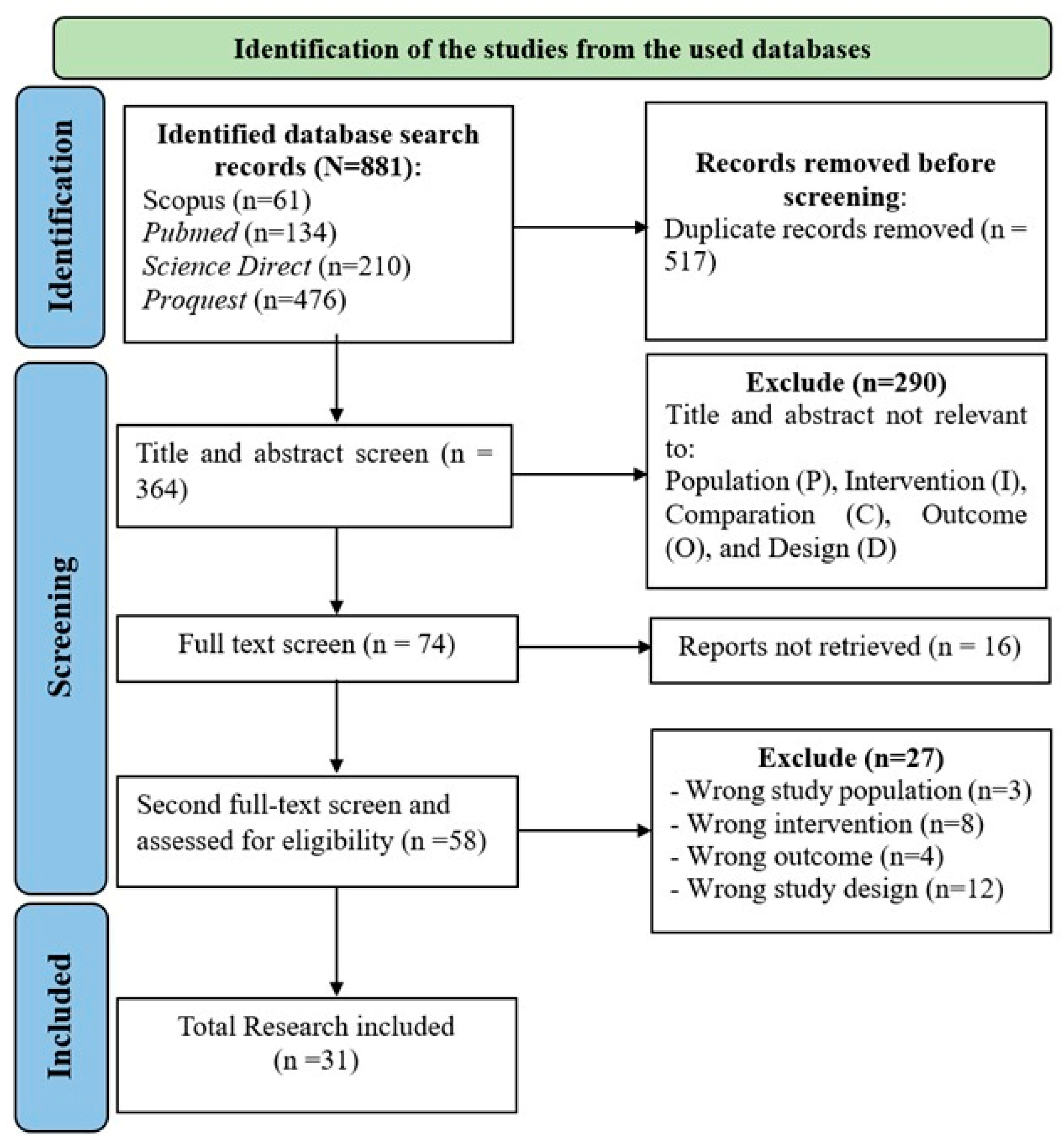
2. Materials and Methods
2.1. Eligibility Criteria
- Inclusion Criteria:
- Population (P): Adults diagnosed with type 2 diabetes mellitus (T2DM).
- Intervention (I): Interventions explicitly designed to enhance self-regulation in the management of type 2 diabetes. These included behavioral, psychosocial, or educational programs that integrated core self-regulation components such as goal-setting, self-monitoring, problem-solving, coping strategies, and appraisal of outcomes [9,26]. Educational programs that provided only didactic information or knowledge transfer, without these self-regulation components, were excluded.
- Comparison (C): Control groups receiving either standard care or non-self-regulation-based interventions.
- Outcomes (O): Quantitative assessment of diabetes self-care behaviors (e.g., knowledge, diet, physical activity, medication adherence, blood glucose levels monitoring, stress management, and foot care), and quality of life measured via validated questionnaires (covering physical, psychological, social, and environmental domains, including FBG and HbA1c levels).
- Study Design (S): Randomized Controlled Trials (RCTs) and quasi-experimental studies.
- Language and Timeframe: Articles published in English between 2014 and 2023.
- Exclusion Criteria:
- Non-primary research such as reviews, editorials, conference abstracts, and study protocols,
- Case reports or applied development studies,
- Qualitative studies or studies with purely descriptive designs.
2.2. Search Strategy
2.3. Study Selection
2.4. Data Extraction, Analysis, and Synthesis
2.5. Risk of Bias and Study Quality
3. Results
3.1. Study Characteristics
3.2. Risk of Bias and Study Quality
3.3. Impact of Intervention on Type 2 Diabetes Patients
3.3.1. Thematic Synthesis
3.3.2. Impact of Diabetes Self-Management Intervention
3.3.3. Impact of the Self-Regulation Training Program Intervention
3.4. Development of a New Integrative Model
3.4.1. Factors That Influence Individuals and Families with Type 2 Diabetes (Part A)
3.4.2. Nursing System (Intervention)
3.4.3. Coping and Appraisal Skills
3.4.4. Outcome (Health Status and Quality of Life)
4. Discussion
4.1. Effectiveness of DSME Intervention
4.2. Effectiveness of Self-Regulation Model Program Intervention
4.3. New Integrative Model
5. Implications for Practice
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wiebe, D.J.; Berg, C.A.; Munion, A.K.; Loyola, M.D.R.; Mello, D.; Butner, J.E.; Suchy, Y.; Marino, J.A. Executive Functioning, Daily Self-Regulation, and Diabetes Management while Transitioning into Emerging Adulthood. Ann. Behav. Med. 2023, 57, 676–686. [Google Scholar] [CrossRef]
- Pereira, E.V.; Tonin, F.S.; Carneiro, J.; Pontarolo, R.; Wiens, A. Evaluation of the application of the diabetes quality of life questionnaire in patients with diabetes mellitus. J. Arch. Endocrinol. Metab. 2020, 64, 59–65. [Google Scholar] [CrossRef]
- Goins, R.T.; Jones, J.; Schure, M.; Winchester, B.; Bradley, V. Type 2 diabetes management among older American Indians: Beliefs, attitudes, and practices. Ethn. Health 2020, 25, 1055–1071. [Google Scholar] [CrossRef]
- Castillo, R.R.; Pabón Carrasco, M.; Jiménez-Picón, N.; Ponce-Blandón, J.A. Effects of a Diabetes Self-Management Education Program on Glucose Levels and Self-Care in Type 1 Diabetes: A Pilot Randomized Controlled Trial. Int. J. Environ. Res. Public. Health 2022, 19, 16364. [Google Scholar] [CrossRef]
- Estuningsih, Y.; Rochmah, T.N.; Andriani, M.; Mahmudiono, T. Effect of self-regulated learning for improving dietary management and quality of life in patients with type-2 diabetes mellitus at Dr. Ramelan Naval Hospital, Surabaya, Indonesia. Kesmas Natl. Public Health J. 2019, 14, 51–57. [Google Scholar] [CrossRef]
- Sari, P. Regulasi Diri Dan Dukungan Sosial Dari Keluarga Pada Pasien Diabetes Melitus Tipe 2. J. Experentia 2020, 8, 122–130. [Google Scholar]
- Ryan, P.; Sawin, K.J. The Individual and Family Self-Management Theory: Background and perspectives on context, process, and outcomes. Nurs. Outlook 2009, 57, 217–225.e6. [Google Scholar] [CrossRef]
- Papachristoforou, E.; Lambadiari, V.; Maratou, E.; Makrilakis, K. Association of Glycemic Indices (Hyperglycemia, Glucose Variability, and Hypoglycemia) with Oxidative Stress and Diabetic Complications. J. Diabetes Res. 2020, 2020, 7489795. [Google Scholar] [CrossRef] [PubMed]
- Chuman, N.; Hatamochi, C. Intervention Effect Based on Self-Regulation to Promote the Continuation of Self-Care Behavior of Patients with Type-2 Diabetes Mellitus. Health J. 2021, 13, 472–481. [Google Scholar] [CrossRef]
- Iawchud, N.; Rojpaisarnkit, K.; Imami, N. The application of a self-regulation model for dietary intake and exercise to control blood sugar of type II diabetic patients. J. Hum. Behav. Soc. Environ. 2023, 34, 570–583. [Google Scholar] [CrossRef]
- Leventhal, H.; Phillips, L.A.; Burns, E. The Common-Sense Model of Self-Regulation (CSM): A dynamic framework for understanding illness self-management. J. Behav. Med. 2016, 39, 935–946. [Google Scholar] [CrossRef]
- Vohs, K.D.; Baumeister, R.F. Handbook of Self-Regulation: Research, Theory, and Applications, 2nd ed.; The Guilford Press: New York, NY, USA, 2011. [Google Scholar]
- Nursalam, N.; Fikriana, R.; Devy, S.R.; Ahsan, A. The development of self-regulation models based on belief in Patients with hypertension. Syst. Rev. Pharm. 2020, 11, 1036–1041. [Google Scholar] [CrossRef]
- Hariyono, H.; Romli, L.Y. Self Regulation Effect on Glycemic Control of Type 2 Diabetes Melitus Patients. Indian. J. Public. Health Res. Dev. 2020, 11, 1257–1262. [Google Scholar] [CrossRef]
- Eshete, A.; Getye, B.; Aynaddis, G.; Tilaye, B.; Mekonnen, E.; Taye, B.; Zeleke, D.; Deresse, T.; Kifleyohans, T.; Assefa, Y. Association between illness perception and medication adherence in patients with diabetes mellitus in North Shoa, Zone: Cross-sectional study. Front. Public Health 2023, 11, 1214725. [Google Scholar] [CrossRef]
- Tang, J.; Gao, L. Illness perceptions among patients with type 2 diabetes mellitus: A cross-sectional study. Int. J. Nurs. Pract. 2020, 26, e12801. [Google Scholar] [CrossRef] [PubMed]
- Qi, X.; Xu, J.; Chen, G.; Liu, H.; Liu, J.; Wang, J.; Zhang, X.; Hao, Y.; Wu, Q.; Jiao, M. Self-management behavior and fasting plasma glucose control in patients with type 2 diabetes mellitus over 60 years old: Multiple effects of social support on quality of life. Health Qual. Life Outcomes 2021, 19, 254. [Google Scholar] [CrossRef] [PubMed]
- Ogurtsova, K.; Guariguata, L.; Barengo, N.C.; Ruiz, P.L.D.; Sacre, J.W.; Karuranga, S.; Sun, H.; Boyko, E.J.; Magliano, D.J. IDF diabetes Atlas: Global estimates of undiagnosed diabetes in adults for 2021. Diabetes Res Clin Pract 2022, 183, 109118. [Google Scholar] [CrossRef]
- IDF. IDF Diabetes Atlas Ninth edition 2020. Lancet 2021, 266, 134–137. [Google Scholar] [CrossRef]
- John, R.; Pise, S.; Chaudhari, L.; Deshpande, P. Evaluation of quality of life in type 2 diabetes mellitus patients using quality of life instrument for indian diabetic patients: A cross-sectional study. J. Midlife Health 2019, 10, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Fassbinder, E.; Schweiger, U.; Martius, D.; Brand-de Wilde, O.; Arntz, A. Emotion regulation in schema therapy and dialectical behavior therapy. Front. Psychol. 2016, 7, 75. [Google Scholar] [CrossRef]
- Alyami, M.; Serlachius, A.; Mokhtar, I.; Broadbent, E. Longitudinal Associations Between Illness Perceptions and Glycemic Control in Type 2 Diabetes. Int. J. Behav. Med. 2022, 29, 398–407. [Google Scholar] [CrossRef] [PubMed]
- Chindankutty, N.V.; Devineni, D. Illness Perception, Coping, and Self-Care Adherence Among Adults With Type 2 Diabetes. J. Popul. Soc. Stud. 2024, 32, 687–705. [Google Scholar] [CrossRef]
- Tavakolizadeh, J.; Moghadas, M.; Ashraf, H. Effect of self-regulation training on management of type 2 diabetes. Iran. Red. Crescent Med. J. 2014, 16, e13506. [Google Scholar] [CrossRef][Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Felix, H.C.; Narcisse, M.R.; Long, C.R.; Mcelfish, P.A. Effects of a Family Diabetes Self-Management Education Intervention on the Patients’ Participating Supporters Holly. Fam. Syst. Health 2020, 38, 121–129. [Google Scholar] [CrossRef]
- Rasoul, A.M.; Jalali, R.; Abdi, A.; Salari, N.; Rahimi, M.; Mohammadi, M. The effect of self-management education through weblogs on the quality of life of diabetic patients. BMC Med. Inform. Decis. Mak. 2019, 19, 205. [Google Scholar] [CrossRef]
- Lee, S.K.; Shin, D.H.; Kim, Y.H.; Lee, K.S. Effect of diabetes education through pattern management on self-care and self-efficacy in patients with type 2 diabetes. Int. J. Environ. Res. Public. Health 2019, 16, 3323. [Google Scholar] [CrossRef]
- Gathu, C.W.; Shabani, J.; Kunyiha, N.; Ratansi, R. Effect of diabetes self-management education on glycaemic control among type 2 diabetic patients at a family medicine clinic in Kenya: A randomised controlled trial. Afr. J. Prim. Health Care Fam. Med. 2018, 10, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Zheng, F.; Liu, S.; Liu, Y.; Deng, L. Effects of an outpatient diabetes self-management education on patients with type 2 diabetes in China: A randomized controlled trial. J. Diabetes Res. 2019, 2019, 1073131. [Google Scholar] [CrossRef] [PubMed]
- Moghadam, S.T.; Najafi, S.S.; Yektatalab, S. The effect of self-care education on emotional intelligence and HbA1c level in patients with type 2 diabetes mellitus: A randomized controlled clinical trial. Int. J. Community Based Nurs. Midwifery 2018, 6, 39–46. [Google Scholar]
- Abaza, H.; Marschollek, M. SMS education for the promotion of diabetes self-management in low & middle income countries: A pilot randomized controlled trial in Egypt. BMC Public Health 2017, 17, 962. [Google Scholar] [CrossRef]
- Garizábalo-Dávila, C.M.; Rodríguez-Acelas, A.L.; Mattiello, R.; Cañon-Montañez, W. Social Support Intervention for Self-Management of Type 2 Diabetes Mellitus: Study Protocol for a Randomized Controlled Trial. Open Access J. Clin. Trials 2021, 13, 37–43. [Google Scholar] [CrossRef]
- Azami, G.; Soh, K.L.; Sazlina, S.G.; Salmiah, M.S.; Aazami, S.; Mozafari, M.; Taghinejad, H. Effect of a Nurse-Led Diabetes Self-Management Education Program on Glycosylated Hemoglobin among Adults with Type 2 Diabetes. J. Diabetes Res. 2018, 2018, 4930157. [Google Scholar] [CrossRef]
- Boels, A.M.; Vos, R.C.; Dijkhorst-Oei, L.T.; Rutten, G.E.H.M. Effectiveness of diabetes self-management education and support via a smartphone application in insulin-treated patients with type 2 diabetes: Results of a randomized controlled trial (TRIGGER study). BMJ Open Diabetes Res. Care 2019, 7, e000981. [Google Scholar] [CrossRef]
- Feng, Y.; Zhao, Y.; Mao, L.; Gu, M.; Yuan, H.; Lu, J.; Zhang, Q.; Zhao, Q.; Li, X. The Effectiveness of an eHealth Family-Based Intervention Program in Patients With Uncontrolled Type 2 Diabetes Mellitus (T2DM) in the Community Via WeChat: Randomized Controlled. JMIR Mhealth Uhealth 2023, 11, e40420. [Google Scholar] [CrossRef] [PubMed]
- Kusnanto Widyanata, K.A.J.; Suprajitno Arifin, H. DM-calendar app as a diabetes self-management education on adult type 2 diabetes mellitus: A randomized controlled trial. J. Diabetes Metab. Disord. 2019, 18, 557–563. [Google Scholar] [CrossRef] [PubMed]
- Cheng, L.; Sit, J.W.H.; Choi, K.C.; Chair, S.Y.; Li, X.; Wu, Y.; Long, J.; Yang, H. The effects of an empowerment-based self-management intervention on empowerment level, psychological distress, and quality of life in patients with poorly controlled type 2 diabetes: A randomized controlled trial. Int. J. Nurs. Stud. 2019, 3, 103407. [Google Scholar] [CrossRef]
- Rondhianto; Kusnanto; Melaniani, S. The effect of diabetes self-management education, based on the health belief model, on the psychosocial outcome of type 2 diabetic patients in Indonesia. Indian. J. Public. Health Res. Dev. 2018, 9, 1718–1723. [Google Scholar] [CrossRef]
- Maslakpak, M.H.; Razmara, S.; Niazkhani, Z. Effects of Face-to-Face and Telephone-Based Family-Oriented Education on Self-Care Behavior and Patient Outcomes in Type 2 Diabetes: A Randomized Controlled Trial. J. Diabetes Res. 2017, 2017, 8404328. [Google Scholar] [CrossRef]
- Chai, S.; Yao, B.; Xu, L.; Wang, D.; Sun, J.; Yuan, N.; Ji, L. The effect of diabetes self-management education on psychological status and blood glucose in newly diagnosed patients with diabetes type 2. Patient Educ. Couns. 2018, 101, 1427–1432. [Google Scholar] [CrossRef]
- McEwen, M.M.; Pasvogel, A.; Murdaugh, C. Effects of a Family-Based Diabetes Intervention on Family Social Capital Outcomes for Mexican American Adults. Diabetes Educ. 2019, 45, 272–286. [Google Scholar] [CrossRef]
- Dobson, R.; Whittaker, R.; Jiang, Y.; Maddison, R.; Shepherd, M.; McNamara, C.; Cutfield, R.; Khanolkar, M.; Murphy, R. Effectiveness of text message based, diabetes self management support programme (SMS4BG): Two arm, parallel randomised controlled trial. BMJ 2018, 361, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Wichit, N.; Mnatzaganian, G.; Courtney, M.; Schulz, P.; Johnson, M. Randomized controlled trial of a family-oriented self-management program to improve self-efficacy, glycemic control and quality of life among Thai individuals with Type 2 diabetes. Diabetes Res. Clin. Pract. 2017, 123, 37–48. [Google Scholar] [CrossRef]
- Hailu, F.B.; Moen, A.; Hjortdahl, P. Diabetes Self-Management Education (DSME)—Effect on Knowledge, Self-Care Behavior, and Self-Efficacy Among Type 2 Diabetes Patients in Ethiopia: A Controlled Clinical Trial. Diabetes Metab. Syndr. Obes. Targets Ther. 2019, 12, 2489–2499. [Google Scholar] [CrossRef]
- Rusdiana Savira, M.; Amelia, R. The effect of diabetes self-management education on Hba1c level and fasting blood sugar in type 2 diabetes mellitus patients in primary health care in binjai city of north Sumatera, Indonesia. Open Access Maced. J. Med. Sci. 2018, 6, 715–718. [Google Scholar] [CrossRef]
- Zupa, M.F.; Lee, A.; Piette, J.D.; Trivedi, R.; Youk, A.; Heisler, M.; Rosland, A.-M. Impact of a Dyadic Intervention on Family Supporter Involvement in Helping Adults Manage Type 2 Diabetes. J. Gen Intern. Med. 2022, 37, 761–768. [Google Scholar] [CrossRef]
- Pamungkas, R.A.; Chamroonsawasdi, K. Self-management based coaching program to improve diabetes mellitus self-management practice and metabolic markers among uncontrolled type 2 diabetes mellitus in Indonesia: A quasi-experimental study. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 53–61. [Google Scholar] [CrossRef]
- Ghisi GLde, M.; Aultman, C.; Konidis, R.; Foster, E.; Tahsinul, A.; Sandison, N.; Sarin, M.; Oh, P. Effectiveness of an education intervention associated with an exercise program in improving disease-related knowledge and health behaviours among diabetes patients. Patient Educ. Couns. 2020, 103, 1790–1797. [Google Scholar] [CrossRef] [PubMed]
- Borji, M.; Otaghi, M.; Kazembeigi, S. The impact of Orem’s self-care model on the quality of life in patients with type II diabetes. Biomed. Pharmacol. J. 2017, 10, 213–220. [Google Scholar] [CrossRef]
- Hurst, C.P.; Rakkapao, N.; Hay, K. Impact of diabetes self-management, diabetes management self-efficacy and diabetes knowledge on glycemic control in people with Type 2 Diabetes (T2D): A multicenter study in Thailand. PLoS ONE 2020, 15, e0244692. [Google Scholar] [CrossRef] [PubMed]
- Bramer, W.M.; Rethlefsen, M.L.; Kleijnen, J.; Franco, O.H. Optimal database combinations for literature searches in systematic reviews: A prospective exploratory study. Syst. Rev. 2017, 6, 245. [Google Scholar] [CrossRef]
- Furlan, J.C.; Singh, J.; Hsieh, J.; Fehlings, M.G. Methodology of Systematic Reviews and Recommendations. J. Neurotrauma 2011, 28, 1335–1339. [Google Scholar] [CrossRef]
- Cumpston, M.S.; McKenzie, J.E.; Thomas, J.; Brennan, S.E. The use of ‘PICO for synthesis’ and methods for synthesis without meta-analysis: Protocol for a survey of current practice in systematic reviews of health interventions. F1000Research 2021, 9, 678. [Google Scholar] [CrossRef] [PubMed]
- Monnaatsie, M.; Biddle, S.J.H.; Khan, S.; Kolbe-Alexander, T. Physical activity and sedentary behaviour in shift and non-shift workers: A systematic review and meta-analysis. Prev. Med. Rep. 2021, 24, 101597. [Google Scholar] [CrossRef] [PubMed]
- Nooseisai, M.; Viwattanakulvanid, P.; Kumar, R.; Viriyautsahakul, N.; Muhammad Baloch, G.; Somrongthong, R. Effects of diabetes self-management education program on lowering blood glucose level, stress, and quality of life among females with type 2 diabetes mellitus in Thailand. Prim. Health Care Res. Dev. 2021, 22, e46. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, A.; Reimer, A.; Kulzer, B.; Icks, A.; Paust, R.; Roelver, K.-M.; Kaltheuner, M.; Ehrmann, D.; Krichbaum, M.; Haak, T.; et al. Measurement of psychological adjustment to diabetes with the diabetes acceptance scale. J. Diabetes Complicat. 2018, 32, 384–392. [Google Scholar] [CrossRef]
- Hsieh, M.H.; Chen, Y.C.; Ho, C.H.; Lin, C.Y. Validation of Diabetes Knowledge Questionnaire (DKQ) in the Taiwanese Population—Concurrent Validity with Diabetes-Specific Quality of Life Questionnaire Module. Diabetes, Metab. Syndr. Obes. Targets Ther. 2022, 15, 2391–2403. [Google Scholar] [CrossRef]
- Toobert, D.J.; Hampson, S.E.; Glasgow, R.E. The Summary of Diabetes Self-Care. Diabetes Care J. 2000, 23, 943–950. [Google Scholar] [CrossRef]
- Dempsey, P.C.; Dunstan, D.W.; Larsen, R.N.; Lambert, G.W.; Kingwell, B.A.; Owen, N. Prolonged uninterrupted sitting increases fatigue in type 2 diabetes. Diabetes Res. Clin. Pract. 2018, 135, 128–133. [Google Scholar] [CrossRef]
- Jokelainen, J.; Timonen, M.; Keinänen-Kiukaanniemi, S.; Härkönen, P.; Jurvelin, H.; Suija, K. Validation of the Zung self-rating depression scale (SDS) in older adults. Scand. J. Prim. Health Care 2019, 37, 353–357. [Google Scholar] [CrossRef]
- WHO. WHO Quality of Life-BREF (WHOQOL-BREF) 2014. Available online: https://www.sralab.org/rehabilitation-measures/who-quality-life-bref-whoqol-bref (accessed on 1 May 2024).
- Bujang, M.A.; Adnan, T.H.; Mohd Hatta, N.K.B.; Ismail, M.; Lim, C.J. A Revised Version of Diabetes Quality of Life Instrument Maintaining Domains for Satisfaction, Impact, and Worry. J. Diabetes Res. 2018, 2018, 5804687. [Google Scholar] [CrossRef]
- Pham, T.B.; Nguyen, T.T.; Truong, H.T.; Trinh, C.H.; Du, H.N.T.; Ngo, T.T.; Nguyen, L.H. Effects of Diabetic Complications on Health-Related Quality of Life Impairment in Vietnamese Patients with Type 2 Diabetes. J. Diabetes Res. 2020, 2020, 4360804. [Google Scholar] [CrossRef]
- Fiqri, A.M.; Sjattar, E.L.; Irwan, A.M. Cognitive Behavioral Therapy for self-care behaviors with type 2 diabetes mellitus patients: A systematic review. Diabetes Metab. Syndr. Clin. Res. Rev. 2022, 16, 102538. [Google Scholar] [CrossRef]
- Alligood, M.R. Nursing Theory Utilization & Application, 5th ed.; Mosby Elsevier: Amsterdam, The Netherlands, 2014. [Google Scholar]
- Ogden, J. Health Psychology, 4th ed.; Open University Press: London, UK, 2007. [Google Scholar]
- Fadli, F.; Uly, N.; Safruddin, S.; Darmawan, S.; Batupadang, M. Analysis of self-regulation model to improvement of self-care capability in type 2 Diabetes Mellitus patients. Multidiscip. Sci. J. 2023, 6, 2024082. [Google Scholar] [CrossRef]
- Alaslawi, H.; Berrou, I.; Hamid AAl Alhuwail, D.; Aslanpour, Z. Diabetes Self-management Apps: Systematic Review of Adoption Determinants and Future Research Agenda. JMIR Diabetes 2022, 7, e28153. [Google Scholar] [CrossRef]
- Salari, R.; Niakan Kalhori, S.R.; GhaziSaeedi, M.; Jeddi, M.; Nazari, M.; Fatehi, F. Mobile-based and cloud-based system for self-management of people with type 2 diabetes: Development and usability evaluation. J. Med. Internet Res. 2021, 23, e18167. [Google Scholar] [CrossRef]
- Li, W.-W.; Tong, J. Family-Based, Culturally Responsive Intervention for Chinese Americans With Diabetes: Lessons Learned From a Literature Review to Inform Study Design and Implementation. Asian/Pac. Isl. Nurs. J. 2023, 7, e48746. [Google Scholar] [CrossRef] [PubMed]
- Motamed-Jahromi, M.; Kaveh, M.H.; Vitale, E. Mindfulness and self-regulation intervention for improved self-neglect and self-regulation in diabetic older adults. Sci. Rep. 2024, 14, 13857. [Google Scholar] [CrossRef]
- Syabariyah, S.; Putri, P.; Wardani, K.; Aisyah, P.S.; Hisan, U.K. Mobile health applications for self-regulation of glucose levels in type 2 diabetes mellitus patients: A systematic review. Fam. Med. Prim. Care Rev. 2024, 26, 123–136. [Google Scholar] [CrossRef]
- Ward, J.E.F. Self-Regulation Theory and Self-Monitoring of Blood Glucose Behavior in Type 2 Diabetes Mellitus; University of Louisville: Louisville, KY, USA, 2014. [Google Scholar] [CrossRef]
- Sukartini, T.; Nursalam, N.; Pradipta, R.O.; Ubudiyah, M. Potential Methods to Improve Self-Management in Those with Type 2 Diabetes: A Narrative Review. Int. J. Endocrinol. Metab. 2023, 21, e119698. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Sun, J.; Bian, H.; Wang, X.; Zhang, C.; Dong, K.; Shen, C.; Liu, T. The relationship between hope level and self-management behaviors in Chinese patients with type 2 diabetes mellitus: A chain-mediated role of social support and disease perception. BMC Psychol. 2024, 12, 446. [Google Scholar] [CrossRef]
- Shaban, M.M.; Sharaa, H.M.; Amer, F.G.M.; Shaban, M. Effect of digital based nursing intervention on knowledge of self-care behaviors and self-efficacy of adult clients with diabetes. BMC Nurs. 2024, 23, 130. [Google Scholar] [CrossRef]
- Abedini, M.; Bijari, B.; Miri, Z.; Shakhs, F.; Abbasi, A. The quality of life of the patients with diabetes type 2 using EQ-5D-5 L in Birjand. Health and Quality of Life Outcomes. Health Qual. Life Outcomes 2020, 18, 18. [Google Scholar] [CrossRef]
- Kumah, E.; Otchere, G.; Ankomah, S.E.; Fusheini, A.; Kokuro, C.; Aduo-Adjei, K.; Amankwah, J.A. Diabetes self-management education interventions in the WHO African Region: A scoping review. PLoS ONE 2021, 16, e0256123. [Google Scholar] [CrossRef] [PubMed]
- Sofiani, Y.; Kamil, A.R.; Rayasari, F. The relationship between illness perceptions, self-management, and quality of life in adult with type 2 diabetes mellitus. J. Keperawatan Padjadjaran 2022, 10, 187–195. [Google Scholar] [CrossRef]
- Gurmu, Y.; Dechasa, A. Effect of patient centered diabetes self care management education among adult diabetes patients in Ambo town, Ethiopia: An interventional study. Int. J. Afr. Nurs. Sci. 2023, 19, 100606. [Google Scholar] [CrossRef]
- Tamiru, S.; Dugassa, M.; Amsalu, B.; Bidira, K.; Bacha, L.; Tsegaye, D. Effects of Nurse-Led diabetes Self-Management education on Self-Care knowledge and Self-Care behavior among adult patients with type 2 diabetes mellitus attending diabetes follow up clinic: A Quasi-Experimental study design. Int. J. Afr. Nurs. Sci. 2023, 18, 100548. [Google Scholar] [CrossRef]
- Alyami, M.; Serlachius, A.; O’Donovan, C.E.; Werf Bvan der Broadbent, E. A systematic review of illness perception interventions in type 2 diabetes: Effects on glycaemic control and illness perceptions. Diabet Med. 2021, 38, e14495. [Google Scholar] [CrossRef]
- Emery, K.A.; Robins, J.; Salyer, J.; Thurby-Hay, L. Self and Family Management in Type 2 Diabetes: Influencing Factors and Outcomes. Nurs. Sci. Q. 2019, 32, 189–197. [Google Scholar] [CrossRef]
- Mohamed, A.; Staite, E.; Ismail, K.; Winkley, K. A systematic review of diabetes self-management education interventions for people with type 2 diabetes mellitus in the Asian Western Pacific (AWP) region. Nurs. Open 2019, 6, 1424–1437. [Google Scholar] [CrossRef]
- Izquierdo, V.; Pazos-Couselo, M.; González-Rodríguez, M.; Rodríguez-González, R. Educational programs in type 2 diabetes designed for community-dwelling older adults: A systematic review. Geriatr. Nurs. 2022, 46, 157–165. [Google Scholar] [CrossRef]
- Mannucci, E.; Giaccari, A.; Gallo, M.; Bonifazi, A.; Belén, Á.D.P.; Masini, M.L.; Trento, M.; Monami, M. Self-management in patients with type 2 diabetes: Group-based versus individual education. A systematic review with meta-analysis of randomized trails. Nutr. Metab. Cardiovasc. Dis. 2022, 32, 330–336. [Google Scholar] [CrossRef]
- Holton, S.; Rasmussen, B.; Turner, J.; Steele, C.; Ariarajah, D.; Hamblin, S.; Crowe, S.; Schutte, S.; Wynter, K.; Hussain, I.M. Nurse, midwife and patient perspectives and experiences of diabetes management in an acute inpatient setting: A mixed-methods study. BMC Nurs. 2022, 21, 249. [Google Scholar] [CrossRef]
- Kim, S.H.; Kim, Y.; Choi, S.; Jeon, B. Evaluation of nurse-led social media intervention for diabetes self-management: A mixed-method study. J. Nurs. Sch. 2022, 54, 569–577. [Google Scholar] [CrossRef]
- Eghtedari, M.; Goodarzi—Khoigani, M.; Shahshahani, M.S.; Javadzade, H.; Abazari, P. Is Web-Based Program Effective on Self-Care Behaviors and Glycated Hemoglobin in Patients with Type 2 Diabetes: A Randomized Controlled Trial. Iran. J. Nurs. Midwifery Res. 2023, 28, 723–729. [Google Scholar] [CrossRef]
- Jiang, X.; Jiang, H.; Li, M.; Lu, Y.; Liu, K.; Sun, X. The Mediating Role of Self-Efficacy in Shaping Self-Management Behaviors Among Adults With Type 2 Diabetes. Worldviews Evid.-Based Nurs. 2019, 16, 151–160. [Google Scholar] [CrossRef]
- Jiang, X.; Wang, J.; Lu, Y.; Jiang, H.; Li, M. Self-efficacy-focused education in persons with diabetes: A systematic review and meta-analysis. Psychol. Res. Behav. Manag. 2019, 12, 67–79. [Google Scholar] [CrossRef]
| Component | Characteristics | (n = 31) | Percentage (%) |
|---|---|---|---|
| Study Design | RCT | 17 | 54.8 |
| Non-RCT | 14 | 45.2 | |
| Intervention Type | Self-regulation training | 4 | 12.9 |
| Diabetes Self-Management Education (DSME) | 13 | 41.9 | |
| Self-Care Education | 5 | 16.1 | |
| SMS Self-Care Education | 5 | 16.1 | |
| Social Support Intervention | 3 | 9.7 | |
| Self-care Model | 1 | 3.2 | |
| Results | Self-Care Behavior | 4 | 12.9 |
| Control blood sugar | 1 | 3.2 | |
| Glycemic Control | 4 | 12.9 | |
| Knowledge, Self-Care Behavior, and Self-Efficacy | 6 | 19.4 | |
| HbA1c Level and Fasting Blood Sugar | 5 | 16.1 | |
| Emotional Intelligence and HbA1c level | 3 | 9.7 | |
| Quality of life | 1 | 3.2 | |
| Blood glucose level, stress, and quality of life | 7 | 22.6 |
| Studies Include Randomized Control Trials (RCT) (n = 17) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | Author | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 | Total Score | Category |
| 1 | Gathu et al., 2018 [29] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 13/13 | 100.0% (Good) |
| 2 | Zheng et al., 2019 [30] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 13/13 | 100.0% (Good) |
| 3 | Moghadam et al., 2018 [31] | Y | Y | Y | N | Y | Y | Y | N | Y | Y | Y | Y | Y | 11/13 | 84.6% (Good) |
| 4 | Abaza and Marschollek, 2017 [32] | N | N | Y | N | Y | N | Y | Y | Y | Y | Y | Y | Y | 9/13 | 69.0% (Enough) |
| 5 | Felix et al., 2020 [26] | Y | Y | Y | N | N | Y | Y | Y | Y | Y | Y | N | Y | 10/13 | 76.9% (Good) |
| 6 | Garizábalo-Dávila et al., 2021 [33] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 13/13 | 100.0% (Good) |
| 7 | Azami et al., 2018 [34] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 13/13 | 100.0% (Good) |
| 8 | Boels et al., 2019 [35] | N | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 11/13 | 84.6% (Good) |
| 9 | Feng et al., 2023 [36] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 13/13 | 100.0% (Good) |
| 10 | Kusnanto et al., 2019 [37] | Y | Y | N | N | N | N | Y | Y | Y | Y | Y | N | N | 7/13 | 53.8% (Enough) |
| 11 | Cheng et al., 2019 [38] | Y | Y | N | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 10/13 | 76.9% (Good) |
| 12 | Rondhianto et al., 2018 [39] | Y | Y | N | N | N | N | Y | Y | Y | Y | Y | N | N | 7/13 | 53.8% (Enough) |
| 13 | Maslakpak et al., 2017 [40] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 13/13 | 100.0% (Good) |
| 14 | Chai et al., 2018 [41] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 13/13 | 100.0% (Good) |
| 15 | McEwen et al., 2019 [42] | Y | Y | Y | N | Y | Y | Y | Y | N | Y | Y | Y | Y | 11/13 | 84.6% (Good) |
| 16 | Dobson et al., 2018 [43] | Y | Y | Y | N | N | N | Y | Y | Y | Y | Y | Y | Y | 10/13 | 76.9% (Good) |
| 17 | Wichit et al., 2017 [44] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 13/13 | 100.0% (Good) |
| Studies Include Non-Randomized Control Trial (Non-RCT) (n = 14) | ||||||||||||||||
| No. | Author | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Total Score | Category | ||||
| 18 | Chuman and Hatamochi, 2021 [9] | Y | Y | Y | Y | Y | Y | Y | Y | Y | - | - | - | - | 9/9 | 100.0% (Good) |
| 19 | Iawchud et al., 2023 [10] | Y | Y | Y | Y | Y | Y | Y | Y | Y | - | - | - | - | 9/9 | 100.0% (Good) |
| 20 | Hariyono and Romli, 2020 [14] | Y | Y | Y | Y | Y | N | Y | Y | Y | - | - | - | - | 8/9 | 88.8% (Good) |
| 21 | Hailu et al., 2019 [45] | Y | Y | Y | Y | Y | Y | Y | Y | Y | - | - | - | - | 9/9 | 100.0% (Good) |
| 22 | Rusdiana et al., 2018 [46] | Y | Y | Y | N | Y | N | Y | Y | Y | - | - | - | - | 7/9 | 77.8% (Good) |
| 23 | Tavakolizadeh et al., 2014 [24] | Y | Y | Y | Y | Y | N | Y | Y | Y | - | - | - | - | 8/9 | 88.8% (Good) |
| 24 | Zupa et al., 2021 [47] | Y | Y | Y | Y | Y | Y | Y | Y | Y | - | - | - | - | 9/9 | 100.0% (Good) |
| 25 | Rasoul et al., 2019 [27] | Y | Y | Y | Y | Y | Y | Y | Y | Y | - | - | - | - | 9/9 | 100.0% (Good) |
| 26 | Lee et al., 2019 [28] | Y | Y | Y | Y | Y | Y | Y | Y | Y | - | - | - | - | 9/9 | 100.0% (Good) |
| 27 | Nooseisai et al., 2021 [56] | Y | Y | Y | Y | Y | Y | Y | Y | Y | - | - | - | - | 8/9 | 88.8% (Good) |
| 28 | Pamungkas et al., 2020 [48] | Y | Y | Y | Y | Y | Y | Y | Y | Y | - | - | - | - | 9/9 | 100% (Good) |
| 29 | Hailu et al., 2019 [45] | Y | Y | Y | Y | Y | Y | Y | Y | Y | - | - | - | - | 9/9 | 100.0% (Good) |
| 30 | Ghisi et al., 2020 [49] | Y | Y | Y | Y | Y | N | Y | Y | Y | - | - | - | - | 8/9 | 88.8% (Good) |
| 31 | Borji et al., 2017 [50] | Y | Y | Y | Y | Y | Y | Y | Y | Y | - | - | - | - | 9/9 | 100.0% (Good) |
| Initial Codes | Categories | Themes |
|---|---|---|
| Increased diabetes knowledge; improved illness understanding | Knowledge acquisition | Theme 1: Education strengthens cognitive foundations for self-regulation |
| Improved diet, exercise, medication adherence, and self-monitoring | Behavioral change | Theme 2: Structured self-management strategies enhance behavior modification |
| Increased confidence, motivation, and perceived control | Self-efficacy | Theme 3: Self-efficacy acts as a central mediator in self-regulation processes |
| Family reminders, shared diet preparation, and emotional support | Family support | Theme 4: Family engagement facilitates sustained self-management |
| Nurse-led education; digital tools (apps, SMS); video-based modules | Health system facilitation | Theme 5: Multi-modal delivery improves accessibility and continuity |
| Reduced HbA1c; improved glycemic control | Clinical outcomes and quality of life | Theme 6: Self-regulation interventions yield measurable metabolic improvements |
| Coping strategies, reduced distress, enhanced emotional regulation | Coping and emotional processes | Theme 7: Emotional adaptation supports long-term maintenance of self-care behaviors |
| No. | Author, Year | Country | Design | Sample Size (n) Age Mean ± SD (Min − Max) | Participants and Setting | Intervention Type | Instrument | Outcome | Result | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention Group | Control Group | Intervention Group | Control Group | ||||||||
| 1 | Chuman and Hatamochi, 2021 [9] | Japan | Quasi-Experiment | n = 19 age = 59.8 ± 6.14 | n = 10 age = 64.3 ± 3.95 | 29 people living with type 2 diabetes were divided into two groups | Self-regulation training was delivered over 3 weeks, consisting of: 6 structured sessions (2 sessions per week); 60–90 min per session; Session components included (diabetes education, cognitive behavioral self-monitoring, and behavioral practice); no formal follow-up was reported | Standard care program for people living with type 2 diabetes | Diabetes self-management behavior scale; Cognitive Behavioral Self-Monitoring Scale: Chronic disease self-efficacy scale | Knowledge, Self-Care Behavior, and Self-Efficacy | Self-regulation training improved knowledge and self-management behaviors compared to the control group. |
| 2 | Iawchud et al., 2023 [10] | Thailand | Quasi-Experiment | n = 30 age = 59.5 ± 7.29 | n = 30 age = 58.5 ± 6.91 | Thirty people living with type 2 diabetes were divided into two groups with ages 35–65 years and fasting blood glucose values 126–182 mg/dL. | Self-regulation theory–based program delivered over 3 weeks, consisting of structured face-to-face educational and behavioral practice sessions. | Standard care program for patients | Diabetes self-management behavior scale | Diabetes self-management; Blood glucose control | The intervention enhanced diabetes self-management behaviors and improved glycemic control. |
| 3 | Hariyono and Romli, 2020 [14] | Indonesia | Quasi-Experiment | n = 30 age = 20–55 years | There is no control group | 30 people living with type 2 diabetes, ages 35–65 years | Self-regulation treatment was conducted over 3 weeks, consisting of 1 session per week, each lasting 90 min. The program included diabetes education, guidance on self-monitoring, behavioral regulation strategies, and goal-setting activities to improve glycemic control. | No control group | Glycemic Control in Type 2 Diabetes Patients | Control blood sugar | The self-regulation program improved glycemic control in patients with type 2 diabetes. |
| 4 | Hailu et al., 2019 [45] | Ethiopia | Quasi-Experiment | n = 116 age = 35–75 years | n = 104 age = 35–75 years | 220 type 2 diabetes patients meet the criteria with age > 30 years who use insulin therapy | Diabetes Self-Management Education (DSME) is delivered over 3 weeks, consisting of 3 structured sessions (one per week), each lasting 60 min. The DSME program covered diabetes knowledge, diet management, physical activity, blood glucose monitoring, and foot care. Each session included follow-up reinforcement to support participants’ self-care behaviors. | Standard care program for type 2 diabetes patients | DKS, Summary of Diabetes Self-Care Activity (SDSCA), Stanford Self-Management Resource Center (SMRC) | Diabetes Knowledge, Self-Care Behavior, Diabetes Self-Efficacy | The DSME intervention improved knowledge and several self-care behaviors (diet, exercise, glucose monitoring, and foot care), although it did not significantly improve self-efficacy. |
| 5 | Gathu et al., 2018 [29] | Kenya | Randomized Controlled Trial (RCT) | n = 55 age = 50.2 ± 9.93 | n = 41 age = 47.5 ± 9.54 | 96 people living with type 2 diabetes who meet the criteria with age 16–65 years and have HbA1c ≥ 8% | DSME delivered over 6 months, consisting of three 1 h sessions held every six weeks. Sessions included diabetes education, review and reinforcement of key messages, and distribution of self-care materials. Follow-up support was provided through telephone reminders and access to a hotline for consultation. | Following the standard care program in people living with type 2 diabetes | HbA1c from laboratory results; Blood pressure was measured using a calibrated digital tensiometer | HbA1c, blood pressure, body mass index (BMI) | The DSME intervention did not produce significant improvements in glycemic control or other clinical outcomes, suggesting that additional factors such as motivation, attitudes, social support, and self-care behaviors may need to be addressed. |
| 6 | Rusdiana et al., 2018 [46] | Indonesia | Quasi-Experiment | n = 80 age = 45–75 years | There is no control group | 80 type 2 diabetes patients with age criteria > 40 years | DSME delivered over 8 weeks, consisting of weekly 2 h sessions. The program provided structured diabetes education covering diet, physical activity, blood glucose monitoring, and medication adherence. | There is no control group. | Glycosylated hemoglobin test with Alere Afinion as 100 Analyzer; Fasting blood glucose with a portable measuring device (Gluco DR) | HbA1c and fasting blood glucose | The DSME intervention improved glycemic control, as indicated by reductions in HbA1c and fasting blood glucose levels. |
| 7 | Zheng et al., 2019 [30] | China | Randomized Controlled Trial (RCT) | n = 30 age = 52 52 ± 10 46 | n = 30 age = 51 92 ± 12.30 | Sixty people living with type 2 diabetes who meet the criteria, age > 40, have HbA1c ≥ 65% and fasting blood glucose ≥ 7.0 mmol/L. | DSME delivered over 3 months, consisting of 2 sessions, each lasting 45 min. The program focused on improving self-care behaviors (diet control, physical activity, medication adherence, blood glucose monitoring, and foot care) through structured diabetes education. | Regular education program for 3 months | The SDSCA scale, emotional response of PAID score, and Glycemic control | SDSCA, PAID, blood glucose, and HbA1c | The 2-session DSME program improved self-care behaviors across multiple domains and enhanced glycemic control over 3 months |
| 8 | Tavakolizadeh et al., 2014 [24] | Iran | Quasi-Experiment | n = 30 age = 54.53 ± 9.06 | n = 30 age = 58.93 ± 11.12 | Sixty people living with type 2 diabetes meet the criteria with a minimum of suffering from diabetes type 4 for 4 years and age > 50 years. | Self-regulation training was delivered over 1 month, consisting of 10 sessions, each lasting 65 min. The program included education, behavioral practice, and skill development in self-regulation to improve dietary behavior, physical activity, and glycemic control. | Standard care | The SDSCA scale: Self-regulation questionnaire | Diabetes Self-Management and Blood Glucose | Self-regulation training improved blood sugar control and enhanced key self-care behaviors compared to the control group. |
| 9 | Moghadam et al., 2018 [31] | Iran | Randomized Controlled Trial (RCT) | n = 21 age = 48.57 ± 7.89 | n = 21 age = 45.42 ± 7.71 | Forty-two people living with type 2 diabetes who meet the criteria are between 18 and 60 years old. | Video-based self-care education delivered over eight consecutive weeks, consisting of weekly 90 min sessions. The program focused on diabetes knowledge, glycemic control, stress management, and the enhancement of emotional intelligence. | Following the standard program in the clinic and using leaflets | Bar-On Model of Emotional-Social Intelligence (ESI); Glycemic control | Emotional response and HbA1c | Self-care education improved glycemic control and enhanced emotional intelligence, supporting better stress management in patients with type 2 diabetes. |
| 10 | Abaza and Marschollek, 2017 [32] | Egypt | Randomized Controlled Trial (RCT) | n = 34 age = 51.77 ± 9.68 | n = 39 age = 51.24 ± 8.66 | 73 people living with type 2 diabetes who are actively treated at the clinic. | Short Message Service (SMS) based education program for 12 weeks (diet control, physical activity, medication adherence, blood glucose monitoring, and foot care) | Leaflet distribution | Diabetes Self-Care Inventory (SCI); HbA1c levels; blood glucose levels. | Self-Care Behavior, HbA1c levels, and blood glucose, | SMS-based education improved glycemic control and strengthened self-care management among patients with type 2 diabetes |
| 11 | Felix et al., 2020 [26] | Egypt | Randomized Controlled Trial (RCT) | n = 94 age = 34.60 ± 13.20 | n = 44 age = 33.20 ± 9.30 | 138 people living with type 2 diabetes and their families. | A culturally tailored DSME program delivered through eight 75 min classes over eight weeks, conducted in participants’ homes. The sessions included didactic diabetes education, food and anatomical models, storytelling, question–and–answer discussions, and culturally specific examples. Data collection occurred at baseline and 9 weeks post-intervention. | Standard education | The SDSCA scale: Glycemic control | Self-care (Diet pattern, physical activity) and A1c | Family-based DSME improved A1c levels and supported healthier dietary and physical activity behaviors, highlighting the essential role of family involvement in diabetes management. |
| 12 | Garizábalo-Dávila et al., 2021 [33] | Colombia | Randomized Controlled Trial (RCT) | n = 47 age = 34.60 ± 13.20 | n = 47 age = 33.20 ± 9.30 | 94 people living with type 2 diabetes who are adults and actively receiving treatment at the Barranquilla health center. | Social support–based intervention delivered over 4 weeks, consisting of 40 min sessions. The program focused on enhancing social support to improve diabetes self-management, self-care abilities, and quality of life. | Standard care | The SDSCA scale | Diabetes Self-Management | Social-support–based interventions significantly improved diabetes self-management, enabling patients with type 2 diabetes to enhance their self-care abilities and overall quality of life. |
| 13 | Zupa et al., 2021 [47] | United States | Quasi-Experiment | n = 123 age = 62.0 ± 12.0 | n = 116 age = 64.0 ± 16.0 | 239 people living with type 2 diabetes who meet the criteria with age > 50 years and HbA1c values > 8%. | Family-supported self-care education was delivered over 123 days, comprising six structured sessions lasting 90 min each. The program emphasized family involvement to enhance self-efficacy and diabetes self-management. Outcomes were assessed at baseline and 12 months post-intervention. | Standard services | Problem Areas in Diabetes Scale (PAID-5); Adapted Stanford Chronic Disease Self-Efficacy Scale | Knowledge, Self-Care Behavior, and Self-Efficacy | These results showed that patients’ support for intervention programs, including family involvement, can improve self-efficacy and self-management. |
| 14 | Azami et al., 2018 [34] | Iran | Randomized Controlled Trial (RCT) | n = 71 age = 55.09 ± 10.16 | n = 71 age = 53.49 ± 10.98 | 142 people living with type 2 diabetes with age > 18 years and no disease complications. | Nurse-assisted DSME delivered over 4 weeks, consisting of four 10 min educational videos (one per week). The videos, produced in Persian, provided general information on diabetes self-management, complication prevention, physical activity and foot care, healthy eating, and healthy living with diabetes. The videos were accompanied by nurse-led coaching and verbal encouragement. | Standard care | DSMQ; WHOQOL-BREF; Centre for Epidemiology Studies Short Depression Scale (CES-D) | Blood glucose level, stress, and quality of life | The nurse-assisted DSME program improved long-term glycemic control and blood glucose levels, while also enhancing emotional responses and quality of life among patients with type 2 diabetes. |
| 15 | Rasoul et al., 2019 [27] | Iran | Quasi-Experiment | n = 49 age = 44.63 ± 5.29 | n = 49 age = 55.26 ± 4.42 | 98 type 2 diabetes patients with age > 18 years, who have had diabetes for >5 years, and who can use the web. | Weblog-based self-management education delivered over 20 weeks (5 months). Educational content was posted three times per week, with each educational session lasting 90 min. In addition, the program included 20 exercise-related sessions combining aerobic activity and general physical activity, conducted four times per week for 45 min each. | Following the standard program from the clinic | Diabetes Quality of Life (DQOL) | Quality of life | Web-based self-management education improved quality of life in the intervention group, demonstrating the effectiveness of digital platforms in supporting diabetes self-care. |
| 16 | Boels et al., 2019 [35] | Netherlands | Randomized Controlled Trial (RCT) | n = 114 age = 40–70 years | n = 114 age = 40–70 years | 228 people living with type 2 diabetes aged 40–70 years, receiving insulin therapy for >3 months and HbA1c > 7%. | SMS-based diabetes education in which participants selected their preferred frequency (2–6 messages per week), educational topics (two or three optional topics in addition to mandatory hypoglycemia content), and program duration (6 or 9 months). The intervention delivered tailored educational messages through a smartphone-based system to support glycemic control and self-management behaviors. | Standard care | Summary of Diabetes Self-Care Activities Measure (SDSCA); Quality of life questionnaire (EQ-5D-5 L) | Blood glucose level and quality of life | SMS-based education delivered over 3–6 months effectively improved blood glucose control and enhanced quality of life, highlighting the value of mobile health tools in supporting diabetes management. |
| 17 | Lee et al., 2019 [28] | Korea | Quasi-Experiment | n = 30 age = 53.77 ± 9.22 | n = 30 age = 53.60 ± 9.04 | 60 people living with type 2 diabetes aged 18–70 years, HbA1c > 8%, and suffering from diabetes > 6 months. | Personalized lifestyle education delivered through 60 min sessions, including individualized exercise planning (≥150 min, ≥3 times/week) and dietary regimen guidance. Patients received PM education supported by CGMS results and a diabetes education booklet. A telephone follow-up session was provided two weeks later. | Standard program delivery | Cognitive Behavioral Self-Monitoring Scale; American Association of Diabetes Educators | Self-care behavior, self-efficacy, and HbA1c | Enhanced diabetes-management education improved self-care behaviors, increased self-efficacy, and reduced HbA1c compared with basic diabetes education. |
| 18 | Nooseisai et al., 2021 [56] | Thailand | Quasi-Experiment | n = 39 age = 58.9 ± 5.15 | n = 38 age = 58.82 ± 4.32 | 77 female people living with type 2 diabetes aged 50–60 years and HbA1c > 7%. | DSME delivered 3 days per week for 4 months, focusing on diabetes education, stress reduction, and self-care skill development. | Standard care | WHOQOL-BREF; Stress Test-20 (SPST—20) | Blood glucose level, stress, and quality of life | DSME lowered blood glucose levels, reduced stress, and improved quality of life among adult women with type 2 diabetes. |
| 19 | Hurst et al., 2020 [51] | Thailand | Quasi-Experiment | n = 367 age = 5.16 ± 10.94 | There is no control group | Type 2 diabetes patients who are actively taking medication with an age of >20 years. | DSME delivered over 3 weeks, consisting of two sessions per week, each lasting 60–90 min. The program focused on improving diabetes self-management skills, self-efficacy, glycemic control, and patient knowledge. | There is no control group. | Diabetes self-management (SDSCA), Diabetes management self-efficacy (DMSE), Diabetes knowledge (DK) | Diabetes self-management, self-efficacy, knowledge, and glycemic control | The results showed that the diabetes self-management program intervention improved glycemic control, care management, self-efficacy, and knowledge. |
| 20 | Pamungkas et al., 2020 [48] | Indonesia | Quasi-Experiment | n = 30 age = 56.5 ± 7.6 | n = 30 age = 54.2 ± 9.20 | 60 people living with type 2 diabetes aged 35–59 years and HbA1c > 6.5%. | Self-management-based coaching program delivered over 12 weeks, with three sessions per week, each session lasting 60 min, including individual follow-up calls once a week to reinforce learning and monitor progress. | Routine program at the Health Center | Socio-demographic and Health Information (SDHI); DSMQ | Diabetes self-management and HbA1c | Coaching based on diabetes self-management principles improved self-management practices and reduced glycemic levels, demonstrating its feasibility and effectiveness for patients with type 2 diabetes. |
| 21 | Feng et al., 2023 [36] | China | Randomized Controlled Trial (RCT) | n = 113 age = 65.7 ± 6.7 | n = 112 age = 65.4 ± 7.5 | 225 type 2 diabetes patients aged 18–79 years, HbA1c > 7%, and living with family | Family-based health education eHealth program delivered over 3 months, with two sessions per week, each session lasting 60 min, including weekly follow-up via messaging or phone calls to reinforce learning and monitor family support. | Standard care | Summary of Diabetes Self-Care Activities Scale; Diabetes Family Behavior Checklist | Diabetes Self-Care Activities, Family Support, and HbA1c | Family-based eHealth interventions improved self-care activities, strengthened family support, and reduced HbA1c levels, indicating suitability for use in community health center services. |
| 22 | Kusnanto et al., 2019 [37] | Indonesia | Randomized Controlled Trial (RCT) | n = 15 age = 36–65 years | n = 15 age = 36–65 year | 30 people living with type 2 diabetes aged 36–65 years, HbA1c > 7%, have been treated for >3 months, and can operate an Android phone | DSME program based on the diabetes calendar application, 6 times a day for 33-month evaluations | Given leaflet media | Summary of Diabetes Self-Care Activities Measure (SDSCA); Diabetes management self-efficacy scale (DMSES) | Self-efficacy, blood glucose, and HbA1c | The results showed differences between the intervention and control groups in self-efficacy, metabolic control, and lipid control among patients with type 2 diabetes. |
| 23 | Ghisi et al., 2020 [49] | Canada | Quasi-Experiment | n = 84 age = 59.8 ± 311.39 | There is no control group | 84 type 2 diabetes patients with a maximum age of 65 years, who are actively treated at the clinic | 24-week DSME program with one supervised class/week (1.5 h: 30 min education + 1 h exercise) and home exercise 6 days/week, delivered by an interdisciplinary team. | There is no Diabetes control group. | Diabetes Education Questionnaire (DATE-Q); Exercise self-efficacy (ESE) | DSME and self-efficacy | The education program increased diabetes management knowledge and enhanced self-efficacy, demonstrating effectiveness in strengthening self-management skills during the 24-week intervention. |
| 24 | Cheng et al., 2019 [38] | China | Randomized Controlled Trial (RCT) | n = 121 age = 56.13 ± 10.72 | n = 121 age = 53.91 ± 13.01 | 242 type 2 diabetes patients aged >18 years, HbA1c > 6.5%, can be contacted by landline and have good cognitive | 6-week empowerment-based program with one weekly session, including one intake session, two small group discussions, and four phone-based individual consultations, using a written curriculum. | Given standard education only once every 2 weeks | Diabetes Distress Scale (DDS); Diabetes Dependent Quality of Life (ADDQoL) Audit | Emotional response and quality of life | Empowerment-based interventions improved quality of life and reduced diabetes-related stress, indicating their potential for broader, longer-term application across patient age groups. |
| 25 | Borji et al., 2017 [50] | Iran | Quasi-Experiment | n = 40 age = 44.30 ± 9.80 | n = 40 age = 43.80 ± 11.93 | 80 type 2 diabetes patients who have been diagnosed for >1 year, with ages 18–65 years. | Education program based on the Orem Self-care Model in 6 sessions, with a duration of 90 min each session and an evaluation time of 12 weeks. | Standard care | QOL survey (SF-36) | Quality of life | The Orem self-care model improved quality of life over 12 weeks, supporting its use as an effective approach to enhance self-care and quality of life in patients with type 2 diabetes. |
| 26 | Rondhianto et al., 2018 [39] | Indonesia | Randomized Controlled Trial (RCT) | n = 60 age = 57.50 ± 6.83 | n = 60 age = 57.70 ± 5.65 | 120 type 2 diabetes patients who have been diagnosed >6 months with ages 40–65 years. | Health belief model-based DSME program in 6 sessions, with 120 min each session and 6 weeks of evaluation | Daily care is as usual at the Health Center | Diabetes management self-efficacy scale (DMSES); Diabetes distress scale (DDS); Summary of diabetes self-care activities (SDSCA); Diabetes quality of life scale (DQOL) | Self-efficacy, self-care behavior, and diabetes distress, and quality of life | HBM-based educational interventions improved self-efficacy, strengthened self-care behaviors, enhanced quality of life, and reduced diabetes distress, supporting their use as an effective DSME approach for patients with type 2 diabetes. |
| 27 | Maslakpak et al., 2017 [40] | Iran | Randomized Controlled Trial (RCT) | n = 30 age = 49.46 ± 4.76 | n = 30 age = 50.60 ± 3.74 | 60 patients with type 2 diabetes, ages 18–55 years, with no psychiatric disorders. | Family-oriented face-to-face and telephone-based education program twice a week, with 30 min each session and 3 months of evaluation | Standard care | Summary of diabetes self-care activities (SDSCA) | Self-Care Behavior and HbA1c | Family-oriented education delivered through face-to-face and telephone-based programs was highly effective in improving self-care behaviors and enhancing glycemic control among patients with type 2 diabetes. |
| 28 | Chai et al., 2018 [41] | China | Randomized Controlled Trial (RCT) | n = 63 age = 55.00 ± 7 0.0 | n = 55 age = 53.00 ± 9.00 | 118 people living with type 2 diabetes with ages > 18 years and no psychological diseases. | DSME program once a week for 120 min and 6 months of evaluation | Standard care with 5–10 min of education | SAS; SDS | Emotional response and blood glucose levels | Self-management education significantly improved psychological status and reduced depression, anxiety, and blood glucose levels. |
| 29 | McEwen et al., 2019 [42] | United States | Randomized Controlled Trial (RCT) | n = 83 age = 53.64 ± 9.60 | n = 74 age = 53.41 ± 8.40 | 157 type 2 diabetes patients diagnosed >1 year, with ages 35–74 years, HbA1c 8%, and at least one family member participated | Family-based diabetes intervention once a week for 120 min and 12 weeks of evaluation | Standard care with education every 3 weeks | Family Efficacy for Diabetes Scale (FSE) | Self-Efficacy for Health Behaviors | Family-based intervention improved self-efficacy, particularly physical activity, and strengthened family support in managing type 2 diabetes. Thus, involving family members is essential to enhance diabetes self-management. |
| 30 | Dobson et al., 2018 [43] | New Zealand | Randomized Controlled Trial (RCT) | n = 177 age = 47.0 ± 15.0 | n = 177 age = 47.0 ± 15.0 | 354 type 2 diabetes patients with ages > 16 years and HbA1c > 8% | Text message-based diabetes self-management support program with follow-up phone interview at 9 months; HbA1c measured at baseline, 3, 6, and 9 months. | Standard care | Stanford self- Efficacy for diabetes scale (SEDM); summary of diabetes self-care activities (SDSCA; two item diabetes distress scale (DDS2); Health-related quality of life | Self-efficacy, diabetes self-care behaviors, diabetes distress, and quality of life | A text-message–based diabetes self-management program improved self-efficacy, HbA1c, and self-management behaviors, thereby reducing stress and enhancing quality of life in patients with type 2 diabetes. |
| 31 | Wichit et al., 2017 [44] | Thailand | Randomized Controlled Trial (RCT) | n = 70 age = 61.3 ± 11.6 | n = 70 age = 55.5 ± 10.5 | 140 people living with type 2 diabetes, ages > 35 years, fasting blood glucose > 140 mg/dL, and living with family | 3-group education sessions delivered at baseline, Week 5, and Week 9, 2 h per session (1 h interactive learning + 1 h discussion), for groups of 8–12 patient–family dyads, facilitated by a registered nurse; included a Diabetes Information Workbook. | Standard care | Diabetes Self-Care Activities Scale (SDSCA); Diabetes Management Self-Efficacy Scale (DMSES); Physical Component Summary (PCS) | Self-efficacy, quality of life, and glycemic control | Family-oriented self-management intervention programs improved self-efficacy among patients with type 2 diabetes and reduced HbA1c, thereby improving quality of life. Therefore, in conducting DSME, the family should be included in the self-management of type 2 diabetes patients. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fadli, F.; Nursalam, N.; Sjattar, E.L.; Uly, N. An Integrative Model of Self-Regulation in Type 2 Diabetes Self-Management: A Systematic Review of Individual and Family-Based Interventions. Healthcare 2025, 13, 3230. https://doi.org/10.3390/healthcare13243230
Fadli F, Nursalam N, Sjattar EL, Uly N. An Integrative Model of Self-Regulation in Type 2 Diabetes Self-Management: A Systematic Review of Individual and Family-Based Interventions. Healthcare. 2025; 13(24):3230. https://doi.org/10.3390/healthcare13243230
Chicago/Turabian StyleFadli, Fadli, Nursalam Nursalam, Elly Lilianty Sjattar, and Nilawati Uly. 2025. "An Integrative Model of Self-Regulation in Type 2 Diabetes Self-Management: A Systematic Review of Individual and Family-Based Interventions" Healthcare 13, no. 24: 3230. https://doi.org/10.3390/healthcare13243230
APA StyleFadli, F., Nursalam, N., Sjattar, E. L., & Uly, N. (2025). An Integrative Model of Self-Regulation in Type 2 Diabetes Self-Management: A Systematic Review of Individual and Family-Based Interventions. Healthcare, 13(24), 3230. https://doi.org/10.3390/healthcare13243230






