Abstract
In this review, we summarize recent literature investigating facial-exercise-induced changes in facial soft tissue. A literature search was performed in PubMed for the terms facial exercise, rejuvenation, muscle, skin, and aging. Four studies were identified from the search and were subject to further assessment. Four studies were included in our analysis. Two of the four studies included compared the experimental (training) group to a control group. The other two studies had no control group. The participants were mainly middle-aged women. Training conditions varied; neuromuscular electrical stimulation (NMES) was used in two studies, the other two studies used an oscillatory movement device and voluntary facial isometric exercise. Two studies measured facial muscle size using ultrasonography before and after 12 weeks of NMES or 8 weeks of oscillatory movement of the face. One study assessed the changes in facial skin elasticity in a single group following 8 weeks of facial isometric exercise, while one study measured strength of labial and lingual muscles before and following 4 weeks of NMES. We found two studies that reported facial-exercise-induced increases in facial muscle size in middle-aged women. It was also reported that facial skin function may improve following facial isometric exercise. Future research is needed to clarify how these changes link with facial rejuvenation. Compared to extremity muscles, the facial muscles are small in size, their shapes are complex, and the boundaries with other tissues may be unclear. Future study is also necessary to examine the reliability of measurements of the facial muscles.
1. Introduction
The cross-sectional literature suggests that by the age of 80, approximately 20% of an individual’s total muscle mass has been lost [1]. This is characterized by a degenerative loss of muscle mass, strength, and physical function known as sarcopenia. The loss of muscle may be site specific, with the cross-sectional literature noting greater differences in the anterior thigh and abdominal regions than in the posterior sites (i.e., posterior thigh and back) in older men and women compared to a young counterpart [2,3]. This phenomenon is presumed to occur in the muscles of the face as well (i.e., some decreasing more than others). Aging may also alter other soft tissues of the body. The prevalence of obesity generally increases with age and this results in changes to both fat cell size and fat cell number [4]. Collagen also appears to undergo age-related changes with older adults having smaller collagen fibers than younger adults [5]. There also appears to be a shift in the proportion of type III collagen relative to type I collagen in older adults. These two types represent the major collagens of the skin.
Facial soft tissue is composed of a series of layers consisting of skin, subcutaneous adipose tissue, superficial musculoaponeurotic system, deep adipose tissue, and deep fascia or periosteum [6]. It is well known that sagging and wrinkles can appear on the face in older individuals. Thus, aging is expected to influence the facial soft tissues. For instance, the soft tissue thickness of the face, which is the distance between the skin and skull as described above, is affected by aging in both men and women [7,8]. Interestingly, the skin elasticity negatively correlates with age as well as sagging severity [9]. However, evidence about the age-associated change in facial muscle size is limited.
Facial expressions occur as a result of facial muscle movements. The literature suggests that when this movement is repeated, a groove is formed beneath the skin surface and fine wrinkles develop [10,11]. On the contrary, several studies have reported that a short-term facial-exercise intervention improves wrinkles and sagging of the face in middle-aged and older adults [12]. The cause of this discrepancy has not been reported. Therefore, it is unclear whether the age-related changes that occur in the soft tissue of the face in middle-aged and older adults can be favorably impacted by facial exercise/movements.
There are several methods currently used for correcting signs of facial aging. These include the injection of the botulinum toxin, chemical peeling, dermal fillers, cosmetic surgery, laser treatment, facelift, and eyelid surgery [13,14]. However, there is a growing interest in improving and/or delaying facial aging through facial exercises aimed at strengthening, moving and manipulating facial muscles. These alternative approaches are noninvasive and less expensive. A previous systematic review summarized studies regarding the influence of facial exercise on surface anthropometry, as well as perceived facial feeling and satisfaction of the treatment via questionnaire [12]. In that review, however, most of the studies were individual case (n = 1 or n = ~4) reports, and there was a lack of research investigating the effects of facial exercise on quantity and quality of each facial soft tissue component. It is necessary to search for new findings and update information on this topic. In this review, we summarize recent literature investigating facial-exercise-induced changes in profiles of facial soft tissue. Second, we discuss the reliability of ultrasound measurements for assessing the facial muscles.
2. Evidence Acquisition
An online search using PubMed was performed with the following keywords and phrases to obtain relevant articles between January 2013 and April 2019: “facial exercise”, “rejuvenation”, “muscle”, “skin”, and “aging” (see Table 1). References from pertinent articles and the names of the authors cited were cross-referenced to locate any further relevant articles not found with the initial search. To be included, a study needed to meet the following criteria: (a) Exercise program: the study needed to perform an exercise intervention including any of the following: voluntary isometric facial muscle contractions; voluntary isotonic facial muscle contractions; or electrical-stimulated facial muscle contractions; (b) Outcome measure: the study needed to measure quantity and quality of facial soft tissue including skin, adipose tissue, skeletal muscle, and elastic component; (c) Study participants: the study needed to include apparently healthy adults aged 18 and older; (d) Language: the search was limited to original research that was written in English. Studies were excluded if the adults had any morbidities (i.e., facial paralysis and chronic stroke), as well as if studies employed an exercise program of non-facial muscles and/or combined treatment with facial surgery and injection.

Table 1.
Combinations of keywords and number of hits in PubMed.
3. Findings
Four studies [15,16,17,18] were included in our analysis, totaling 188 adults (Figure 1 and Table 2). Two of the four studies included compared the experimental group to a control group. The other two studies had no control group. The participants were mainly middle-aged women (3 studies) and the other study included a mix of young and middle-aged men and women. Training conditions varied; neuromuscular electrical stimulation (NMES) was used in two studies, the other two studies used an oscillatory movement device and voluntary facial isometric exercise.
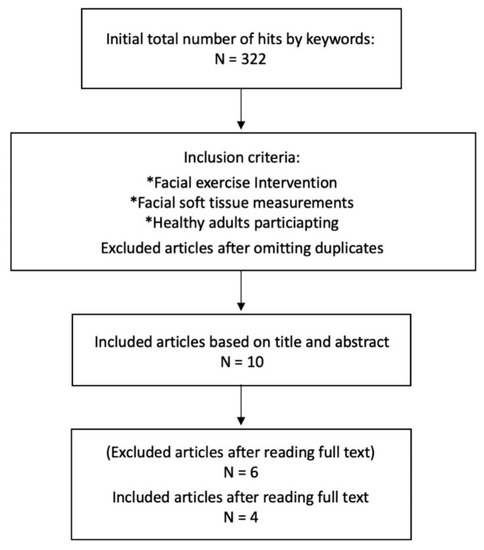
Figure 1.
Flowchart of the literature search.

Table 2.
Research results of studies included in this review.
Two studies measured facial muscle thickness (MT) and cross-sectional area (CSA) using ultrasonography before and after a 12-week NMES program [15] or 8 weeks of oscillatory movement of a face [18]. The NMES study reported a significant increase in MT of the zygomatic major muscle in the experimental group compared to the control group following the intervention [15]. The other study found a pre-post difference in facial MT or CSA of the zygomatic major, levator labii superioris, orbicularis, and digastric muscle in a group training. This study, however, did not have a control group and did not provide the test–retest reliability of their measurements [18]. One study assessed the changes in facial skin elasticity in a group performing 8 weeks of facial isometric exercise. Although the viscoelastic property was unchanged, the other facial elastic property indexes were improved when compared between pre and post values [16]. However, that study did not include a control group nor did they provide any reliability data for their measurements. Finally, the strength of labial and lingual muscles was measured using the Iowa Oral Performance Instrument (IOPI) before and following a 4-week NMES program combined with oral motor exercise. There were no significant changes in the strength measurement for either the experimental or the control group [17].
4. Discussion
Our findings suggest that a relatively short-term (8–12 weeks) intervention which consists of performing facial muscle contractions by NMES [15] or an oscillatory movement device [18] may produce increases in facial muscle size in middle-aged women (Table 2). Regarding these training effects, previous authors have speculated that the exercise-induced increase in the zygomatic major muscle size may be linked to the shortening of the resting length of the muscle, resulting in improvements in facial tone, firmness and lift. However, there is no direct evidence to support these claims. Compared to the extremity muscles, the facial muscle contains smaller muscle fascicles composed of loosely packed muscle fibers with substantial amounts of intervening connective tissue [19]. At present, it is unknown whether the exercise-induced increase in facial muscle size relates to muscle hypertrophy or if it simply reflects a change in the resting length.
Of the studies included in this review, only two provided test–retest reliability on the measurement of facial MT/CSA. However, these studies reported only intra-rater correlation coefficients (ICC) (Table 3) [20,21]. Of note, there are large variations in the ICC values among the facial muscles and the zygomatic major muscle was 0.71. Compared to the results of extremity and trunk muscles [22,23], the ICC values of facial muscles were relatively low. While ICC is a relative measure of reliability, a measure of absolute reliability (i.e., standard error of measurement and minimal difference) [24] of the facial muscle size has not been previously evaluated. Future research is needed to clarify the absolute reliability of facial MT/CSA by ultrasound; particularly when an intervention does not include a time matched non-exercise control group.

Table 3.
Intra-rater reliability of ultrasound measurements of facial muscle thickness.
One study has reported that isometric exercise of the face was effective for improving the elasticity of facial skin [16]. However, the mechanism by which facial exercise causes the improvement of facial skin elasticity is not clear. The superficial musculoaponeurotic system is sandwiched between subcutaneous and deep adipose tissue compartments in a series of facial soft tissue layers. One hypothesis might be that contracting the facial musculature simultaneously stretches the facial skin. Outside of few facial muscles (e.g., mentalis) [25] and a rare case (i.e., dimple by zygomatic major) [26], the majority of facial muscles are not in direct contact with the skin. Moreover, when the muscle is inserted into the skin, the stretching of the skin due to muscle contraction is limited. That is, the skin may not be greatly stretched by the contraction of the facial muscles. However, it should be noted that during isometric exercise, the participants were using their fingers to fix the facial skin as an aid to muscle contraction [16]. Therefore, the skin stretching effect by the fingers which fixed the skin should also be considered. Given that this has only been reported in a single study, it is necessary to conduct additional research in order to better understand the potential mechanisms. Similarly, it is unknown at present whether the facial muscle contractions affect the quantity and quality of the connective tissue and adipose tissue of the face.
As mentioned above, NMES training has been reported to increase facial muscle size [15]. When discussing changes in muscle size, changes in muscle strength are also traditionally measured. However, we have recently proposed that training-induced changes in limb-muscle strength may not necessarily be driven by exercise-induced increases in muscle size [27]. In other words, changes in muscle size do not appear necessary, sufficient, or contributory for changes in muscle strength [27]. Thus, muscle strength of the face may not change as facial muscle size changes and vice versa. One study in this review focused on the effect of NMES combined with oral motor exercise on the strength of labial and lingual muscles [17]. However, the strength was not improved following four weeks of the intervention [17]. In that study, the intensity of NMES stimulation was adjusted according to the participant’s response and then applied to the maximum level each participant could tolerate. The lack of change relative to a control group highlights the potential inability of participants to tolerate high stimulation intensities with muscles of the face, which may ultimately limit their ability to adapt following this form of exercise. This suggests a need for the development of effective voluntary facial-exercise programs.
5. Future Tasks
Although there are many options for facial-exercise protocols (i.e., several devices and masks for facial exercise or several types of voluntary facial exercise and movements), this review included only four studies investigating the effect of facial exercise on the soft tissue of the face and only three types of training conditions for facial muscles. The different types of facial training (i.e., NMES or types of voluntary facial exercise) may elicit different effects on specific facial soft tissue. Moving forward, it is important to work towards determining which exercise protocol is most effective for producing changes in muscle size and strength. At present, there is no established method to assess muscle strength and performance of the facial muscles. It is of importance to develop a standard protocol which is both valid and repeatable. This is also true of the measurement of muscle size. Interpreting the exercise-induced changes in the context of the reliability of the measurement will be an important consideration moving forward; particularly, when there is no time-matched non-exercise control group. In terms of safety and cost, ultrasound is considered to be effective for measuring facial soft tissue.
6. Summary
It has been reported that facial exercise may improve wrinkles and sagging of the face, however, the mechanism has not previously been elucidated. In this review, we found that two studies reported facial-exercise-induced increases in facial MT/CSA in middle-aged women. It was also reported that facial skin function may improve following facial isometric exercise. However, it is unclear how these changes link with facial rejuvenation. In addition, compared to muscles in the extremity and trunk, the facial muscles are small in size, their shapes are complex, and the boundaries with other tissues may be unclear. Therefore, it is necessary to examine the absolute reliability of ultrasound measurements of the facial muscles.
Author Contributions
T.A. and J.P.L. designed the study. T.A. performed the review of literature and wrote the manuscript. J.P.L. reviewed and critically revised the manuscript. All authors approved the final version of the manuscript.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
Conflicts of Interest
The authors declared no conflicts of interests with respect to the research, authorship, and publication of this article.
References
- Janssen, I.; Heymsfield, S.B.; Wang, Z.M.; Ross, R. Skeletal muscle mass and distribution in 468 men and women aged 18–88 yr. J. Appl. Physiol. 2000, 89, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Abe, T.; Loenneke, J.P.; Thiebaud, R.S.; Fukunaga, T. Age-related site-specific muscle wasting of upper and lower extremities and trunk in Japanese men and women. Age 2014, 36, 813–821. [Google Scholar] [CrossRef] [PubMed]
- Loenneke, J.P.; Thiebaud, R.S.; Abe, T. Estimating site-specific muscle loss: A valuable tool for early sarcopenia detection? Rejuvenation Res. 2014, 17, 496–498. [Google Scholar] [CrossRef] [PubMed]
- Smith, U.; Kahn, B.B. Adipose tissue regulates insulin sensitivity: Role of adipogenesis, de novo lipogenesis and novel lipids. J. Intern. Med. 2016, 280, 465–475. [Google Scholar] [CrossRef] [PubMed]
- Lovell, C.R.; Smolenski, K.A.; Duance, V.C.; Light, N.D.; Young, S.; Dyson, M. Type I and III collagen content and fibre distribution in normal human skin during ageing. Br. J. Dermatol. 1987, 117, 419–428. [Google Scholar] [CrossRef] [PubMed]
- Kruglikov, I.; Trujillo, O.; Kristen, Q.; Isac, K.; Zorko, J.; Fam, M.; Okonkwo, K.; Mian, A.; Thanh, H.; Koban, K.; et al. The facial adipose tissue: A revision. Facial Plast. Surg. 2016, 32, 671–682. [Google Scholar] [CrossRef]
- Sahni, D.; Sanjeev; Singh, G.; Jit, I.; Singh, P. Facial soft tissue thickness in northwest Indian adults. Forensic Sci. Int. 2008, 176, 137–146. [Google Scholar] [CrossRef]
- Drgacova, A.; Dupej, J.; Veleminska, J. Facial soft tissue thickness in the present Czech population. Forensic Sci. Int. 2016, 260, 106.e1–106.e7. [Google Scholar] [CrossRef]
- Ezure, T.; Amano, S. Influence of subcutaneous adipose tissue mass on dermal elasticity and sagging severity in lower cheek. Skin Res. Technol. 2010, 16, 332–338. [Google Scholar] [CrossRef]
- Calleja-Agius, J.; Brincat, M.; Borg, M. Skin connective tissue and ageing. Best Pract. Res. Clin. Obstet. Gynaecol. 2013, 27, 727–740. [Google Scholar] [CrossRef]
- Lemperle, G.; Holmes, R.E.; Cohen, S.R.; Lemperle, S.M. A classification of facial wrinkles. Plast. Reconstr. Surg. 2001, 108, 1735–1750. [Google Scholar] [CrossRef]
- Van Borsel, J.; De Vos, M.C.; Bastiaansen, K.; Welvaert, J.; Lambert, J. The effectiveness of facial exercise for facial rejuvenation: A systematic review. Aesthet. Surg. J. 2014, 34, 22–27. [Google Scholar] [CrossRef]
- Litner, J.A.; Rotenberg, B.W.; Dennis, M.; Adamson, P.A. Impact of cosmetic facial surgery on satisfaction with appearance and quality of life. Arch. Facial Plast. Surg. 2008, 10, 79–83. [Google Scholar] [CrossRef]
- Small, R. Aesthetic procedures in office practice. Am. Fam. Physician 2009, 80, 1231–1237. [Google Scholar]
- Kavanagh, S.; Newell, J.; Hennessy, M.; Sadick, N. Use of a neuromuscular electrical stimulation device for facial muscle toning: A randomized, controlled trial. J. Cosmet. Dermatol. 2012, 11, 261–266. [Google Scholar] [CrossRef]
- Kim, K.; Jeon, S.; Kim, J.K.; Hwang, J.S. Effects of Kyunghee Facial Resistance Program (KFRP) on mechanical and elastic properties of skin. J. Dermatol. Treat. 2016, 27, 191–196. [Google Scholar] [CrossRef]
- Safi, M.F.; Wright-Harp, W.; Lucker, J.R.; Payne, J.C. Effect of surface neuromuscular electrical stimulation on labial and lingual muscles in healthy volunteers. Int. J. Rehabil. Res. 2017, 40, 119–126. [Google Scholar] [CrossRef]
- Hwang, U.; Kwon, O.; Jung, S.; Ahn, S.; Gwak, G. Effect of a facial muscle exercise device on facial rejuvenation. Aesthet. Surg. J. 2018, 38, 463–476. [Google Scholar] [CrossRef]
- Goodmurphy, C.W.; Ovalle, W.K. Morphological study of two human facial muscles: Orbicularis oculi and corrugator supercilia. Clin. Anat. 1999, 12, 1–11. [Google Scholar] [CrossRef]
- Volk, G.F.; Wystub, N.; Pohlmann, M.; Finkensieper, M.; Chalmers, H.J.; Guntinas-Lichius, O. Quantitative ultrasonography of facial muscles. Muscle Nerve 2013, 47, 878–883. [Google Scholar] [CrossRef]
- Alfen, N.V.; Gilhuis, H.J.; Keijzers, J.P.; Pillen, S.; Van Dijk, J.P. Quantitative facial muscle ultrasound: Feasibility and reproducibility. Muscle Nerve 2013, 48, 375–380. [Google Scholar] [CrossRef]
- Abe, T.; Loenneke, J.P.; Thiebaud, R.S.; Loftin, M. Morphological and functional relationships with ultrasound measured muscle thickness of the upper extremity and trunk. Ultrasound 2014, 22, 229–235. [Google Scholar] [CrossRef]
- Abe, T.; Loenneke, J.P.; Thiebaud, R.S. Morphological and functional relationships with ultrasound measured muscle thickness of the lower extremity: A brief review. Ultrasound 2015, 23, 166–173. [Google Scholar] [CrossRef]
- Weir, J.P. Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J. Strength Cond. Res. 2005, 19, 231–240. [Google Scholar]
- Hansen, J.T. Netter’s Clinical Anatomy, 3rd ed.; Elsevier: Philadelphia, PA, USA, 2014; pp. 436–437. [Google Scholar]
- Pessa, J.E.; Zadoo, V.P.; Garza, P.A.; Adrian, E.K., Jr.; Dewitt, A.I.; Garza, J.R. Double or bifid zygomaticus major muscle: Anatomy, incidence, and clinical correlation. Clin. Anat. 1998, 11, 310–313. [Google Scholar] [CrossRef]
- Loenneke, J.P.; Dankel, S.J.; Bell, Z.W.; Buckner, S.L.; Mattocks, K.T.; Jessee, M.B.; Abe, T. Is muscle growth a mechanism for increasing strength? Med. Hypotheses 2019, 125, 51–56. [Google Scholar] [CrossRef]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).