The Influence of Printing Orientation on the Properties of 3D-Printed Polymeric Provisional Dental Restorations: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Article Selection
2.2. Exposure and Outcome
2.3. Information Sources, Search Strategy, and Data Extraction
2.4. Quality Assessment of Included Studies
2.5. Quantitative Assessment
3. Results
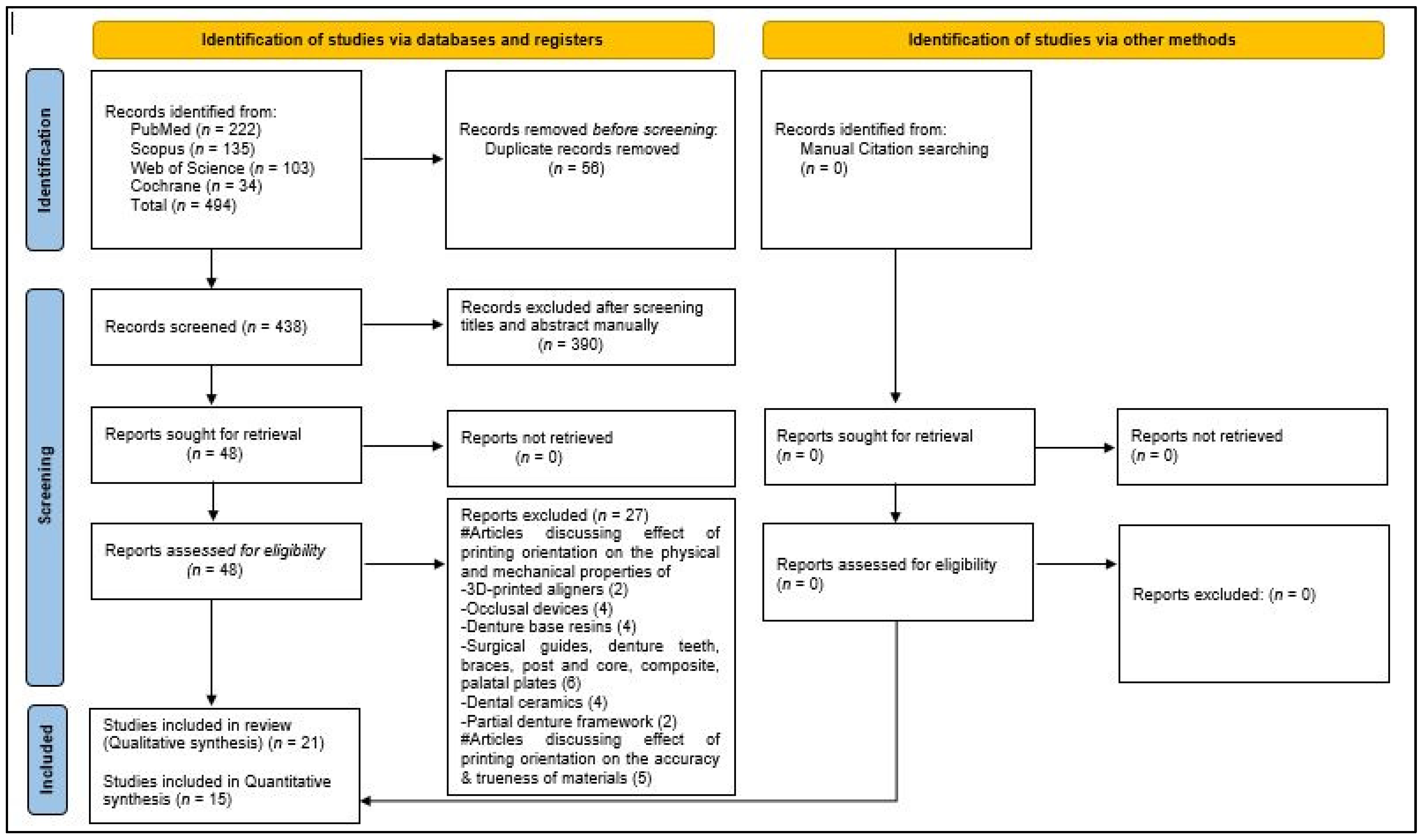
3.1. Identification and Screening
3.2. Quality Assessment of Selected Articles
3.3. The Characteristics of the Selected Studies
3.4. Assessment of Strength of Evidence
3.5. The Results of Studies Investigating the Mechanical and Physical Properties
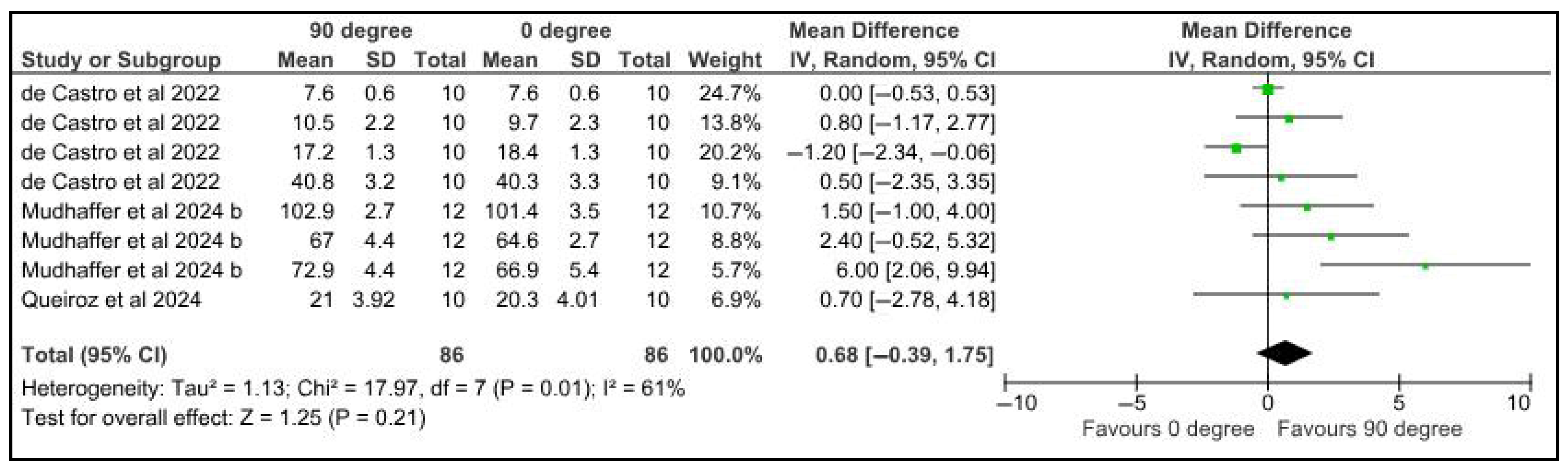
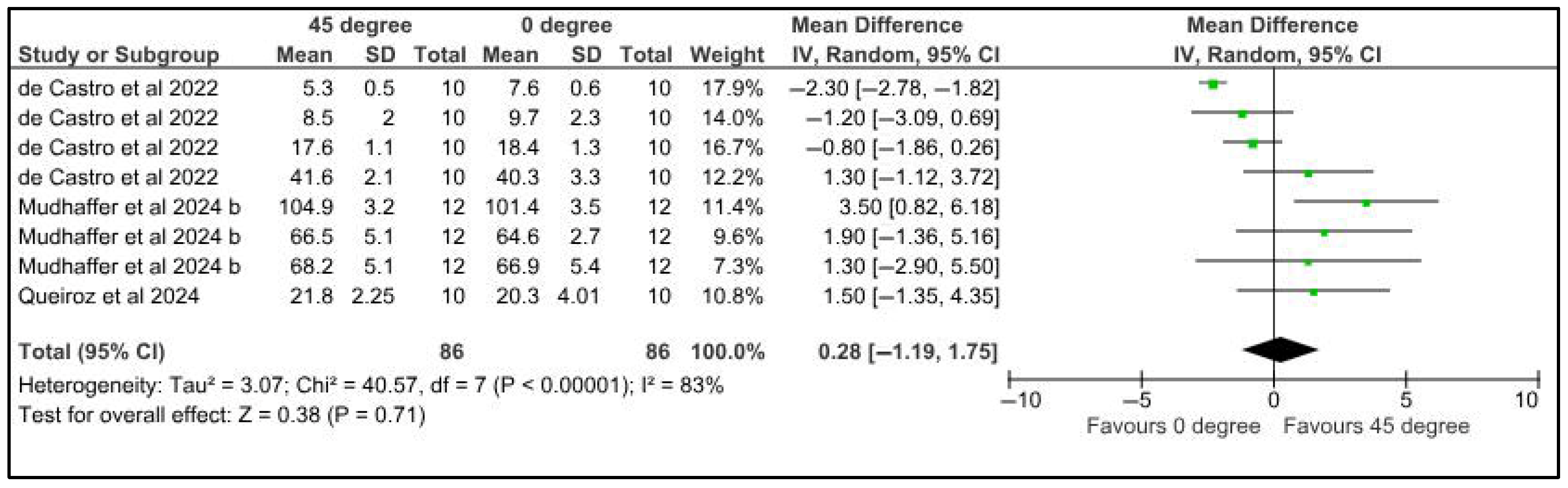
3.5.1. Microhardness
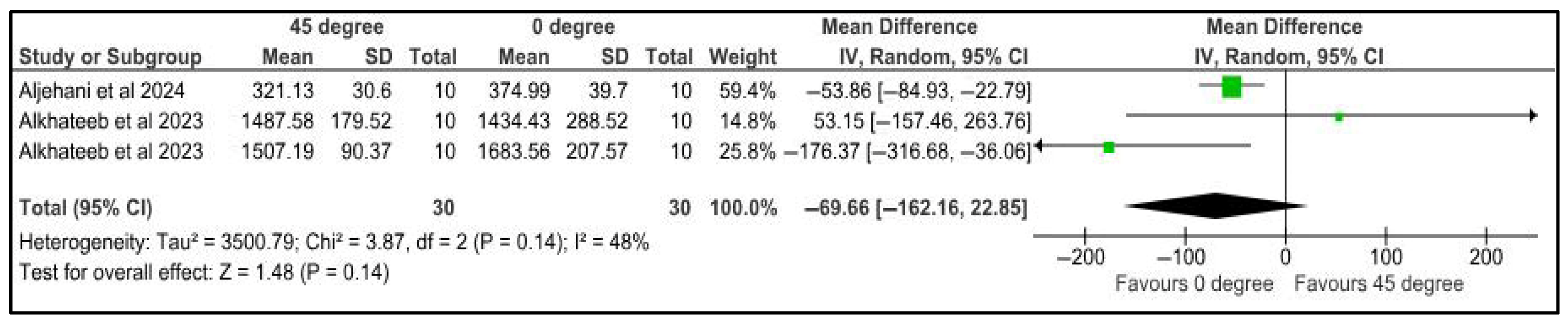
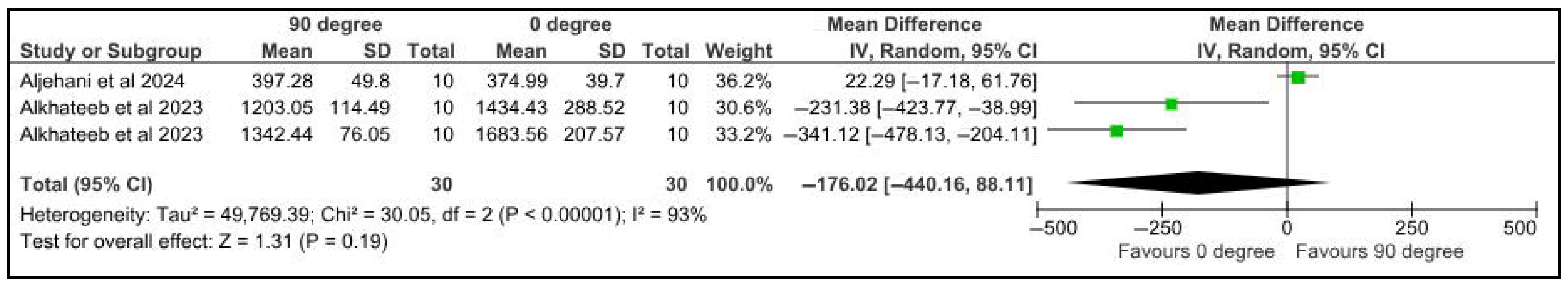
3.5.2. Fracture Resistance
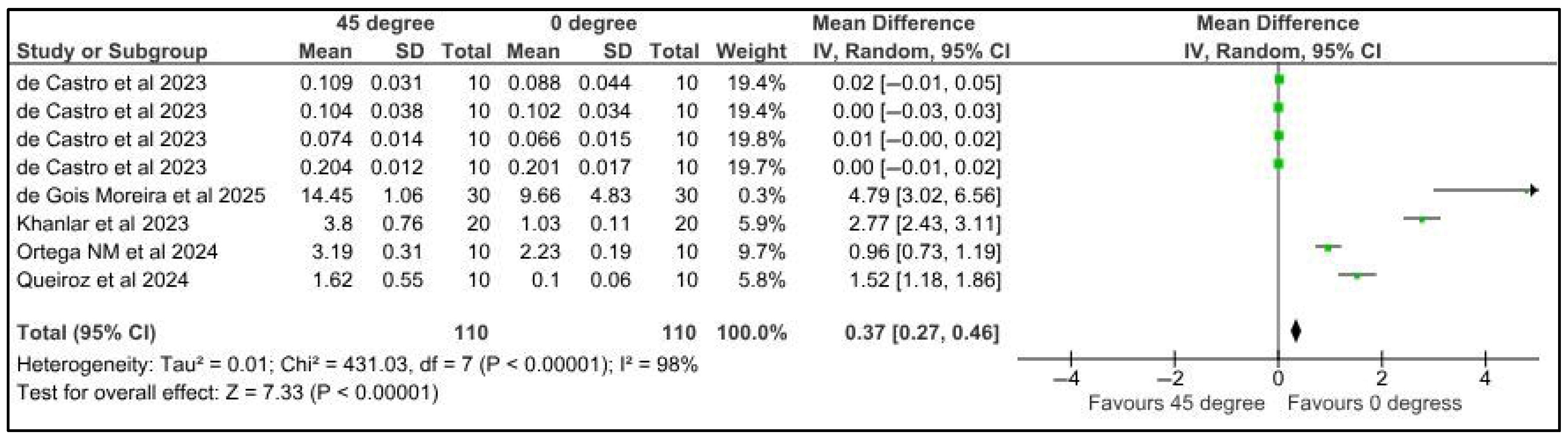
3.5.3. Surface Roughness
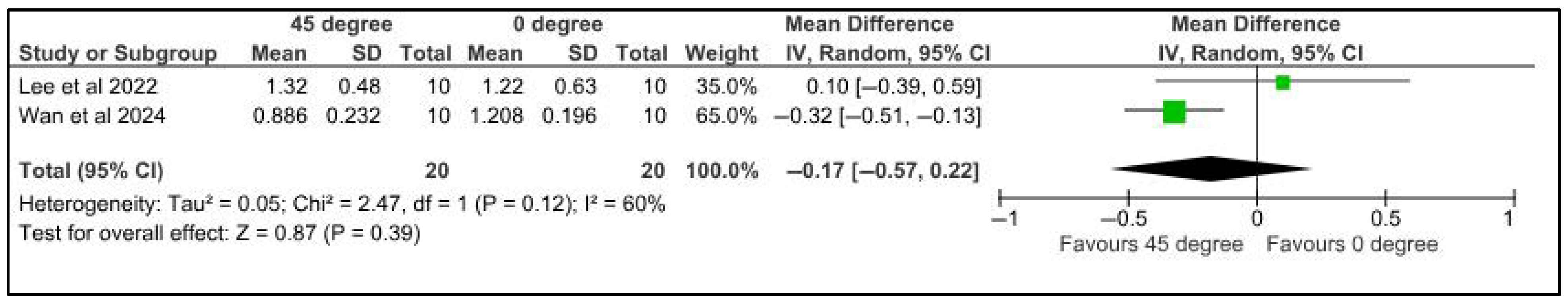
3.5.4. Wear Resistance/Wear Volume Loss
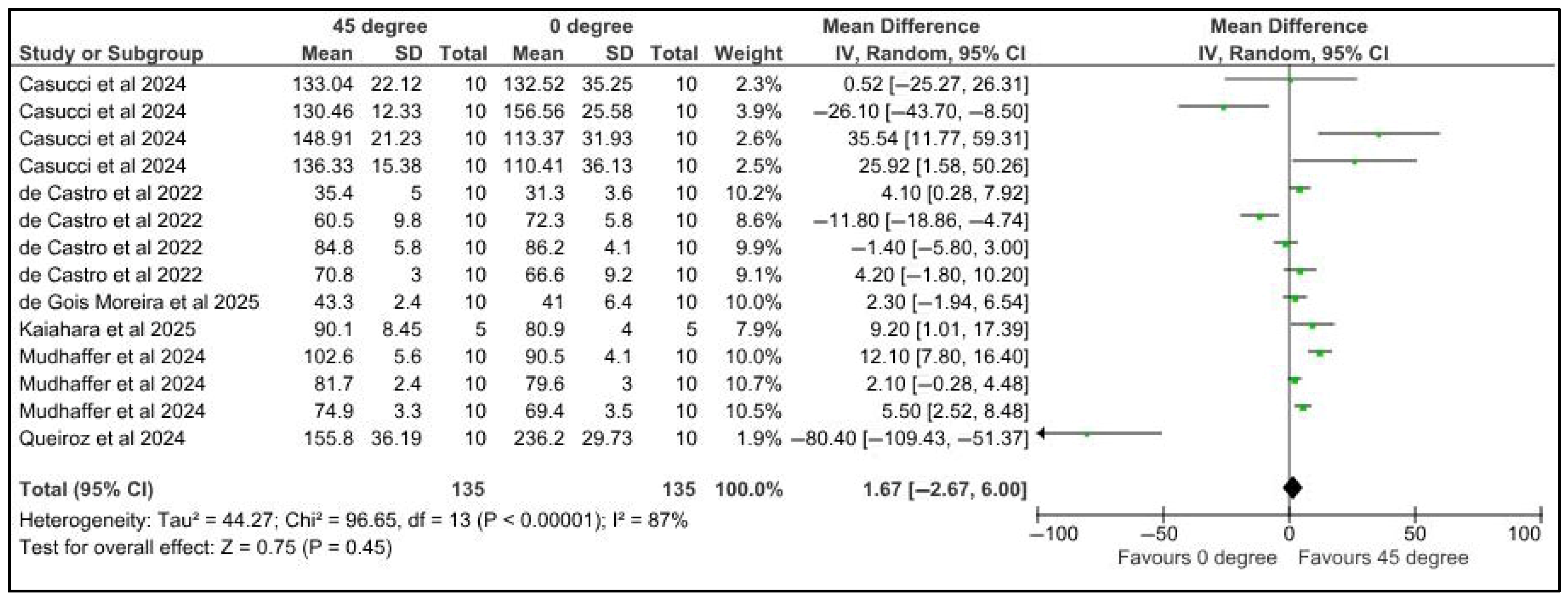
3.5.5. Flexural Strength
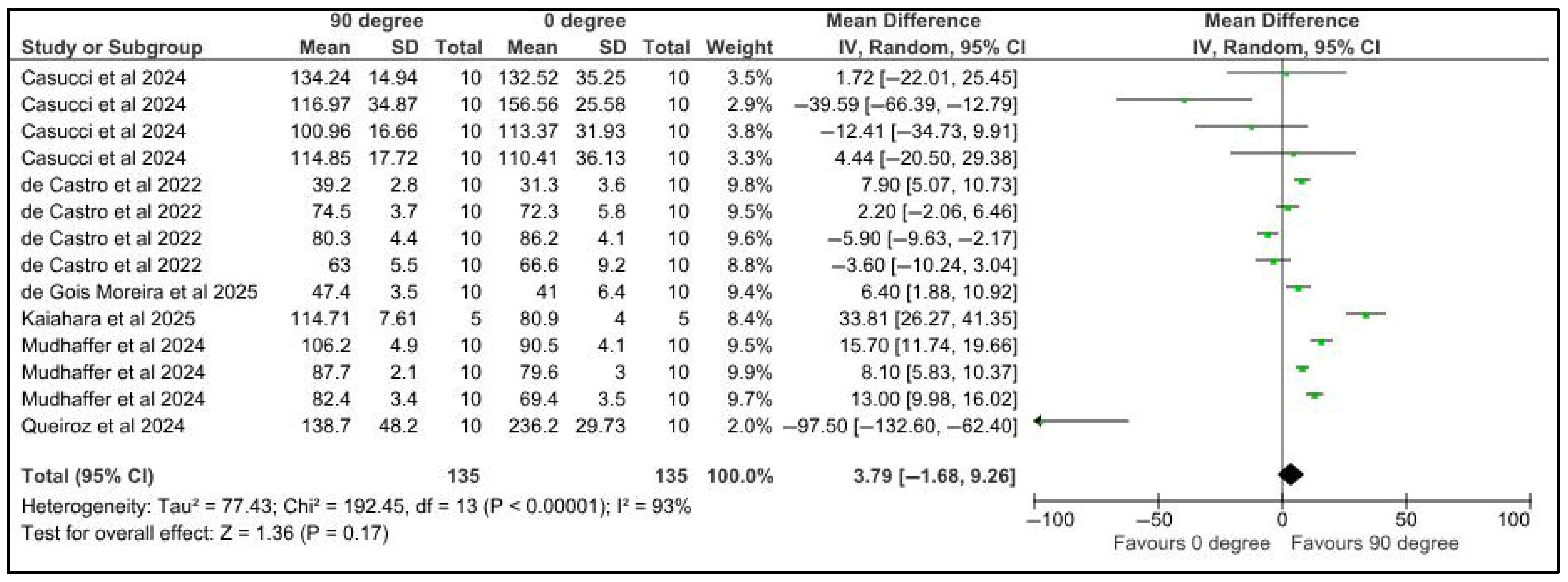
3.5.6. Color Change
3.5.7. Tensile Strength, Compressive Strength, and Elastic Modulus Results
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gratton, D.G.; Aquilino, S.A. Interim restorations. Dent. Clin. N. Am. 2004, 48, 487–497. [Google Scholar] [CrossRef]
- Wassell, R.W.; St George, G.; Ingledew, R.P.; Steele, J.G. Crowns and other extra-coronal restorations: Provisional restorations. Br. Dent. J. 2002, 192, 619–630. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lodding, D.W. Long-term esthetic provisional restorations in dentistry. Curr. Opin. Cosmet. Dent. 1997, 4, 16–21. [Google Scholar][Green Version]
- Trushkowsky, R.D. Fabrication of a fixed provisional restoration utilizing a light-curing acrylic resin. Quintessence Int. 1992, 23, 415–419. [Google Scholar][Green Version]
- Bidra, A.S.; Taylor, T.D.; Agar, J.R. Computer-aided technology for fabricating complete dentures: Systematic review of historical background, current status, and future perspectives. J. Prosthet. Dent. 2013, 109, 361–366. [Google Scholar] [CrossRef]
- Watanabe, H.; Fellows, C.; An, H. Digital Technologies for Restorative Dentistry. Dent. Clin. N. Am. 2022, 66, 567–590. [Google Scholar] [CrossRef]
- Eggmann, F.; Blatz, M.B. Recent Advances in Intraoral Scanners. J. Dent. Res. 2024, 103, 1349–1357. [Google Scholar] [CrossRef]
- Jain, S.; Sayed, M.E.; Ibraheem, W.I.; Ageeli, A.A.; Gandhi, S.; Jokhadar, H.F.; AlResayes, S.S.; Alqarni, H.; Alshehri, A.H.; Huthan, H.M.; et al. Accuracy Comparison between Robot-Assisted Dental Implant Placement and Static/Dynamic Computer-Assisted Implant Surgery: A Systematic Review and Meta-Analysis of In Vitro Studies. Medicina 2024, 60, 11. [Google Scholar] [CrossRef] [PubMed]
- Shim, J.S.; Kim, J.; Jeong, S.H.; Choi, Y.J.; Ryu, J.J. Printing accuracy, mechanical properties, surface characteristics, and microbial adhesion of 3D-printed resins with various printing orientations. J. Prosthet. Dent. 2020, 124, 468–475. [Google Scholar] [CrossRef] [PubMed]
- Beuer, F.; Schweiger, J.; Edelhoff, D. Digital dentistry: An overview of recent developments for CAD/CAM generated restorations. Br. Dent. J. 2008, 204, 505–511. [Google Scholar] [CrossRef]
- Kessler, A.; Hickel, R.; Reymus, M. 3D Printing in dentistry-state of the art. Oper. Dent. 2020, 45, 30–40. [Google Scholar] [CrossRef]
- Piedra-Cascón, W.; Krishnamurthy, V.R.; Att, W.; Revilla-León, M. 3D printing parameters, supporting structures, slicing, and post-processing procedures of vat-polymerization additive manufacturing technologies: A narrative review. J. Dent. 2021, 109, 103630. [Google Scholar] [CrossRef]
- Methani, M.M.; Cesar, P.F.; de Paula Miranda, R.B.; Susana, M.; Mutlu, O.; Marta, R.-L. Additive Manufacturing in Dentistry: Current Technologies, Clinical Applications, and Limitations. Curr. Oral Health Rep. 2020, 7, 327–334. [Google Scholar] [CrossRef]
- Siripongpreda, T.; Hoven, V.P.; Narupai, B.; Rodthongku, N. Emerging 3D printing based on polymers and nanomaterial additives: Enhancement of properties and potential applications. Eur. Polym. J. 2023, 184, 111806. [Google Scholar] [CrossRef]
- Altarazi, A.; Haider, J.; Alhotan, A.; Silikas, N.; Devlin, H. Assessing the physical and mechanical properties of 3D printed acrylic material for denture base application. Dent. Mater. 2022, 38, 1841–1854. [Google Scholar] [CrossRef]
- Goodacre, B.J.; Goodacre, C.J. Additive manufacturing for complete denture fabrication: A narrative review. J. Prosthodont. 2022, 31, 47–51. [Google Scholar] [CrossRef]
- Prpic, V.; Spehar, F.; Stajdohar, D.; Bjelica, R.; Cimic, S.; Par, M. Mechanical Properties of 3D-Printed Occlusal Splint Materials. Dent. J. 2023, 11, 199. [Google Scholar] [CrossRef] [PubMed]
- Atria, P.J.; Bordin, D.; Marti, F.; Nayak, V.V.; Conejo, J.; Benalcázar Jalkh, E.; Witek, L.; Sampaio, C.S. 3D-printed resins for provisional dental restorations: Comparison of mechanical and biological properties. J. Esthet. Restor. Dent. 2022, 34, 804–815. [Google Scholar] [CrossRef]
- Revilla-León, M.; Supaphakorn, A.; Barmak, A.B.; Rutkunas, V.; Kois, J.C. Influence of print orientation on the intaglio surface accuracy (trueness and precision) of tilting stereolithography definitive resin-ceramic crowns. J. Prosthet Dent. 2025, 133, 246–251. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.; Sayed, M.E.; Shetty, M.; Alqahtani, S.M.; Al Wadei, M.H.D.; Gupta, S.G.; Othman, A.A.A.; Alshehri, A.H.; Alqarni, H.; Mobarki, A.H.; et al. Physical and Mechanical Properties of 3D-Printed Provisional Crowns and Fixed Dental Prosthesis Resins Compared to CAD/CAM Milled and Conventional Provisional Resins: A Systematic Review and Meta-Analysis. Polymers 2022, 14, 2691. [Google Scholar] [CrossRef]
- Al Wadei, M.H.D.; Sayed, M.E.; Jain, S.; Aggarwal, A.; Alqarni, H.; Gupta, S.G.; Alqahtani, S.M.; Alahmari, N.M.; Alshehri, A.H.; Jain, M.; et al. Marginal Adaptation and Internal Fit of 3D-Printed Provisional Crowns and Fixed Dental Prosthesis Resins Compared to CAD/CAM-Milled and Conventional Provisional Resins: A Systematic Review and Meta-Analysis. Coatings 2022, 12, 1777. [Google Scholar] [CrossRef]
- Revilla-León, M.; Meyers, M.J.; Zandinejad, A.; Özcan, M. A review on chemical composition, mechanical properties, and manufacturing work flow of additively manufactured current polymers for interim dental restorations. J. Esthet. Restor. Dent. 2019, 31, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Unkovskiy, A.; Bui, P.H.; Schille, C.; Geis-Gerstorfer, J.; Huettig, F.; Spintzyk, S. Objects build orientation, positioning, and curing influence dimensional accuracy and flexural properties of stereolithographically printed resin. Dent. Mater. 2018, 34, e324–e333. [Google Scholar] [CrossRef]
- Kessler, A.; Hickel, R.; Ilie, N. In vitro investigation of the influence of printing direction on the flexural strength, flexural modulus and fractographic analysis of 3D-printed temporary materials. Dent. Mater. J. 2021, 40, 641–649. [Google Scholar] [CrossRef]
- de Castro, E.F.; Nima, G.; Rueggeberg, F.A.; Giannini, M. Effect of build orientation in accuracy, flexural modulus, flexural strength, and microhardness of 3D-Printed resins for provisional restorations. J. Mech. Behav. Biomed. Mater. 2022, 136, 105479. [Google Scholar] [CrossRef]
- Väyrynen, V.O.; Tanner, J.; Vallittu, P.K. The anisotropicity of the flexural properties of an occlusal device material processed by stereolithography. J. Prosthet. Dent. 2016, 116, 811–817. [Google Scholar] [CrossRef]
- Grzebieluch, W.; Kowalewski, P.; Grygier, D.; Rutkowska-Gorczyca, M.; Kozakiewicz, M.; Jurczyszyn, K. Printable and Machinable Dental Restorative Composites for CAD/CAM Application—Comparison of Mechanical Properties, Fractographic, Texture and Fractal Dimension Analysis. Materials 2021, 14, 4919. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Wang, L.; Dal Piva, A.M.O.; Tribst, J.P.M.; Nedeljkovic, I.; Kleverlaan, C.J.; Feilzer, A.J. Influence of surface finishing and printing layer orientation on surface roughness and flexural strength of stereolithography-manufactured dental zirconia. J. Mech. Behav. Biomed. Mater. 2023, 143, 105944. [Google Scholar] [CrossRef] [PubMed]
- Khalil, A.S.; Zaher, A.R. Effect of printing orientation and resin thickness on flexural strength of direct 3D-printed aligners. BMC Oral Health 2025, 25, 238. [Google Scholar] [CrossRef]
- Kaushik, A.; Garg, R.K.; Saini, R.S.; Bennardo, F.; Heboyan, A. Evaluating the effect of printing parameters on the performance of resin occlusal splints for a sustainable dentistry. J. Appl. Biomater. Funct. Mater. 2025, 23, 22808000251333700. [Google Scholar] [CrossRef]
- Gad, M.M.; Fouda, S.M.; Alshammary, H.; Altayyar, R.; Elakel, A.; Nassar, E.A.; Khan, S.Q.; Rahoma, A.M.; Elhagali, A.F.; Özcan, M.; et al. Influence of different printing orientations and post-polymerization time on the translucency of three-dimensional (3D) printed denture base resins. J. Prosthodont. 2024, 33, 81–92. [Google Scholar] [CrossRef]
- Dai, J.; Li, P.; Spintzyk, S.; Liu, C.; Xu, S. Influence of additive manufacturing method and build angle on the accuracy of 3D-printed palatal plates. J. Dent. 2023, 132, 104449. [Google Scholar] [CrossRef]
- Lee, E.-H.; Ahn, J.-S.; Lim, Y.-J.; Kwon, H.-B.; Kim, M.-J. Effect of layer thickness and printing orientation on the color stability and stainability of a 3D-printed resin material. J. Prosthet. Dent. 2022, 127, 784.e1–784.e7. [Google Scholar] [CrossRef]
- Alharbi, N.; Osman, R.; Wismeijer, D. Effects of build direction on the mechanical properties of 3D-printed complete coverage interim dental restorations. J. Prosthet. Dent. 2016, 115, 760–767. [Google Scholar] [CrossRef]
- Farkas, A.Z.; Galatanu, S.V.; Nagib, R. The influence of printing layer thickness and orientation on the mechanical properties of DLP 3D-printed dental resin. Polymers 2023, 15, 1113. [Google Scholar] [CrossRef] [PubMed]
- Aljehani, A.; Nabalawi, A.; Hefni, A.; Alsefri, Z.; Fakhry, O.; Al Zaibak, W.; Raffa, O. Effect of build orientation on the fracture resistance and marginal quality of 3D-printed anatomic provisional crowns: An in-vitro study. Saudi Dent. J. 2024, 36, 584–590. [Google Scholar] [CrossRef] [PubMed]
- Nasiry Khanlar, L.; Revilla-León, M.; Barmak, A.B.; Ikeda, M.; Alsandi, Q.; Tagami, J.; Zandinejad, A. Surface roughness and shear bond strength to composite resin of additively manufactured interim restorative material with different printing orientations. J. Prosthet. Dent. 2023, 129, 788–795. [Google Scholar] [CrossRef] [PubMed]
- Mudhaffer, S.; Haider, J.; Satterthwaite, J.; Silikas, N. Effects of print orientation and artificial aging on the flexural strength and flexural modulus of 3D printed restorative resin materials. J. Prosthet. Dent. 2025, 133, 1345–1357. [Google Scholar] [CrossRef]
- Mudhaffer, S.; Althagafi, R.; Haider, J.; Satterthwaite, J.; Silikas, N. Effects of printing orientation and artificial ageing on martens hardness and indentation modulus of 3D printed restorative resin materials. Dent. Mater. 2024, 40, 1003–1014. [Google Scholar] [CrossRef]
- de Castro, E.F.; Nima, G.; Rueggeberg, F.A.; Araújo-Neto, V.G.; Faraoni, J.J.; Palma-Dibb, R.G.; Giannini, M. Effect of build orientation in gloss, roughness and color of 3D-printed resins for provisional indirect restorations. Dent. Mater. 2023, 39, e1–e11. [Google Scholar] [CrossRef]
- Espinar, C.; Pérez, M.M.; Pulgar, R.; Leon-Cecilla, A.; López-López, M.T.; Della Bona, A. Influence of printing orientation on mechanical properties of aged 3D-printed restorative resins. Dent. Mater. 2024, 40, 756–763. [Google Scholar] [CrossRef]
- Alkhateeb, R.I.; Algaoud, H.S.; Aldamanhori, R.B.; Alshubaili, R.R.; Alalawi, H.; Gad, M.M. Fracture Load of 3D-Printed Interim Three-Unit Fixed Dental Prostheses: Impact of Printing Orientation and Post-Curing Time. Polymers 2023, 15, 1737. [Google Scholar] [CrossRef]
- Queiroz, N.V.; Martins, A.S.; Antunes, A.N.G.; Barros, V.M. Effect of the Printing Angle on Flexural Strength, Microhardness, and Surface Roughness of Three-Dimensionally Printed Resin for Provisional Restorations. Pesqui. Bras. Em Odontopediatria E Clin. Integr. 2024, 25, e230050. [Google Scholar]
- Espinar, C.; Bona, A.D.; Pérez, M.M.; Tejada-Casado, M.; Pulgar, R. The influence of printing angle on color and translucency of 3D printed resins for dental restorations. Dent. Mater. 2023, 39, 410–417. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Son, K.; Lee, D.-H.; Kim, S.-Y.; Lee, K.-B. Comparison of Wear of Interim Crowns in Accordance with the Build Angle of Digital Light Processing 3D Printing: A Preliminary In Vivo Study. Bioengineering 2022, 9, 417. [Google Scholar] [CrossRef]
- Wan, Q.; Lee, J.H.; Daher, R.; Karasan, D.; Myagmar, G.; Sailer, I. Wear Resistance of Additively Manufactured Resin with Different Printing Parameters and Postpolymerization Conditions. Int. J. Prosthodont. 2024, 37, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Derban, P.; Negrea, R.; Rominu, M.; Marsavina, L. Influence of the Printing Angle and Load Direction on Flexure Strength in 3D Printed Materials for Provisional Dental Restorations. Materials 2021, 14, 3376. [Google Scholar] [CrossRef]
- Casucci, A.; Verniani, G.; Sami Haichal, W.; Manfredini, D.; Ferrari, M.; Ferrari Cagidiaco, E. Influence of Printing Angulation on the Flexural Strength of 3D Printed Resins: An In Vitro Study. Appl. Sci. 2024, 14, 10067. [Google Scholar] [CrossRef]
- de Gois Moreira, F.G.; Bezerra, M.G.P.G.; de Miranda, L.M.; da Silva, S.E.G.; de Andrade Dantas, E.L.; de Sousa, F.B.; Özcan, M.; Souza, R.O.A.E. Influence of build angle, printing layer thickness and aging on the flexural strength, precision, roughness and porosity analysis of a printed resin for provisional restorations. Odontology 2025, 113, 1165–1179. [Google Scholar] [CrossRef] [PubMed]
- Kaiahara, F.H.; Pizi, E.C.G.; Straioto, F.G.; Galvani, L.D.; Kuga, M.C.; Arrué, T.A.; Junior, A.R.; Só, M.V.R.; Pereira, J.R.; Vidotti, H. Influence of Printing Orientation on the Mechanical Properties of Provisional Polymeric Materials Produced by 3D Printing. Polymers 2025, 17, 265. [Google Scholar] [CrossRef]
- Ortega, N.M.; Revilla-León, M.; Ortega, R.; Gómez-Polo, C.; Barmak, A.B.; Gómez-Polo, M. Comparison of surface roughness of additively manufactured implant-supported interim crowns fabricated with different print orientations. J. Prosthodont. 2024, 33, 141–148. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Alharbi, N.; Osman, R. Does Build Angle Have an Influence on the Surface Roughness of Anterior 3D-Printed Restorations? An In Vitro Study Int. J. Prosthodont. 2021, 34, 505–510. [Google Scholar] [CrossRef]
- Faggion, C.M. Guidelines for reporting pre-clinical in vitro studies on dental materials. J. Evid. Based Dent. Pract. 2012, 12, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Krithikadatta, J.; Datta, M.; Gopikrishna, V. CRIS guidelines (checklist for reporting in-vitro studies): A concept note on the need for standardized guidelines for improving quality and transparency in reporting in-vitro studies in experimental dental research. J. Conserv. Dent. 2014, 17, 301–304. [Google Scholar] [CrossRef]
- RevMan. (RevMan) The Cochrane Collaboration, Version 541; Cochrane: London, UK, 2020.
- McCarty, M.C.; Chen, S.J.; English, J.D.; Kasper, F. Effect of print orientation and duration of ultraviolet curing on the dimensional accuracy of a 3-dimensionally printed orthodontic clear aligner design. Am. J. Orthod. Dentofacial. Orthop. 2020, 158, 889–897. [Google Scholar] [CrossRef] [PubMed]
- Revilla-León, M.; Cascos-Sánchez, R.; Zeitler, J.M.; Barmak, A.B.; Kois, J.C.; Gómez-Polo, M. Influence of print orientation and wet-dry storage time on the intaglio accuracy of additively manufactured occlusal devices. J. Prosthet. Dent. 2024, 131, 1226–1234. [Google Scholar] [CrossRef]
- Janjić, K.; Valentova, A.; Arellano, S.; Unterhuber, A.; Krause, A.; Oberoi, G.; Unger, E.; Tabrizi, H.A.S.; Schedle, A. The impact of print orientation and graphene nanoplatelets on biaxial flexural strength and cytotoxicity of a 3D printable resin for occlusal splints. Dent. Mater. 2024, 40, 1742–1752. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Araújo, S.R.; Sampaio-Fernandes, M.A.; de Freitas, B.N.; Simionato, A.A.; Figueiral, M.H.; Macedo, A.P. Accuracy of occlusal splints printed in different orientations by liquid crystal display technology: An in vitro study. J. Dent. 2025, 152, 105461. [Google Scholar] [CrossRef]
- Aarts, J.M.; Choi, J.J.E.; Metcalfe, S.; Bennani, V. Influence of build angulation on the mechanical properties of a direct-metal laser-sintered cobalt-chromium used for removable partial denture frameworks. J. Prosthet. Dent. 2021, 126, 224–230. [Google Scholar] [CrossRef]
- Li, P.; Fernandez, P.K.; Spintzyk, S.; Schmidt, F.; Yassine, J.; Beuer, F.; Unkovskiy, A. Effects of layer thickness and build angle on the microbial adhesion of denture base polymers manufactured by digital light processing. J. Prosthodont. Res. 2023, 67, 562–567. [Google Scholar] [CrossRef]
- Alharethi, N.A. Evaluation of the Influence of Build Orientation on the Surface Roughness and Flexural Strength of 3D-Printed Denture Base Resin and Its Comparison with CAD-CAM Milled Denture Base Resin. Eur. J. Dent. 2024, 18, 321–328. [Google Scholar] [CrossRef]
- Turanoglu, O.F.; Cevlik, E.T.; Vural, C. Investigation of adhesion status of Candida species to the surface of resin materials produced at different angles with additive manufacturing. BMC Oral Health 2024, 24, 738. [Google Scholar] [CrossRef]
- Sone, K.P.; Takahashi, H.; Iwaki, M.; Namano, S.; Komagamine, Y.; Minakuchi, S.; Kanazawa, M. Effect of build orientation on the wear resistance and hardness of denture teeth fabricated using digital light processing: An in vitro study. J Prosthodont. Res. 2025, 69, 267–274. [Google Scholar] [CrossRef]
- Çokakoğlu, S.; Karaokutan, I.; Buyuk, S.K. Effects of orientation and post processing on the bonding of 3-dimensional printed brackets to printable permanent crown resin. Am. J. Orthod. Dentofac. Orthop. 2025, 167, 362–370. [Google Scholar] [CrossRef] [PubMed]
- Kalyoncuoğlu, Ü.T.; Ayyıldız, S.; Odabasi Tezer, E. The impact of print orientation on the fracture resistance and failure patterns of additively manufactured cobalt-chromium post and cores. J. Prosthodont. 2023, 32, 714–720. [Google Scholar] [CrossRef] [PubMed]
- Sukindar, N.A.; Azhar, M.A.M.; Shaharuddin, S.I.S.; Kamaruddin, S.; Azhar, A.Z.A.; Choong, Y.C.; Adesta, E.Y.T. A review study on the effect of printing parameters of fused deposition modelling (fdm) metal polymer composite parts on mechanical properties and surface roughness. Malays. J. Microsc. 2022, 18, 281–297. [Google Scholar]
- Alghauli, M.A.; Almuzaini, S.; Aljohani, R.; Alqutaibi, A.Y. Influence of 3D printing orientations on physico-mechanical properties and accuracy of additively manufactured dental ceramics. J. Prosthodont. Res. 2025, 69, 181–202. [Google Scholar] [CrossRef]
- Cameron, A.B.; Choi, J.J.E.; Ip, A.; Lyons, N.; Yaparathna, N.; Dehaghani, A.E.; Feih, S. Assessment of the trueness of additively manufactured mol3% zirconia crowns at different printing orientations with an industrial and desktop 3D printer compared to subtractive manufacturing. J. Dent. 2024, 144, 104942. [Google Scholar] [CrossRef]
- Mou, Z.; Zhong, J.; Wang, F.; Alhotan, A.; Zhu, P.; Li, P.; Huang, J. Zirconia crowns manufactured using digital light processing: Effects of build angle and layer thickness on the accuracy. J. Dent. 2024, 151, 105359. [Google Scholar] [CrossRef]
- Hussein, M.O.; Hussein, L.A. Trueness of 3D printed partial denture frameworks: Build orientations and support structure density parameters. J. Adv. Prosthodont. 2022, 14, 150–161. [Google Scholar] [CrossRef] [PubMed]
- Hai, P.N.; Son, T.M.; Anh, N.V.; Ngoc, T.N.; Tra, N.T. Effect of Horizontal Resolution of Printer on Trueness of 3D-Printed Provisional Crown: An In Vitro Study. Eur. J. Gen. Dent. 2023, 12, 34–41. [Google Scholar] [CrossRef]
- Cameron, A.B.; Evans, J.L.; Abuzar, M.A.; Tadakamadla, S.K.; Love, R.M. Trueness assessment of additively manufactured maxillary complete denture bases produced at different orientations. J. Prosthet. Dent. 2024, 131, 129–135. [Google Scholar] [CrossRef]
- Alharbi, N.; Osman, R.B.; Wismeijer, D. Factors influencing the dimensional accuracy of 3D-printed full-coverage dental restorations using stereolithography technology. Int. J. Prosthodont. 2016, 29, 503–510. [Google Scholar] [CrossRef] [PubMed]
- Chaiamornsup, P.; Katheng, A.; Ha, R.; Tsuchida, Y.; Kanazawa, M.; Uo, M.; Minakuchi, S.; Suzuki, T.; Takahashi, H. Effects of build orientation and bar addition on accuracy of complete denture base fabricated with digital light projection: An in vitro study. J. Prosthodont. Res. 2023, 67, 641–646. [Google Scholar] [CrossRef] [PubMed]
- Osman, R.B.; Alharbi, N.; Wismeijer, D. Build Angle: Does It Influence the Accuracy of 3D-Printed Dental Restorations Using Digital Light-Processing Technology? Int. J. Prosthodont. 2017, 30, 182–188. [Google Scholar] [CrossRef]
- Granholm, A.; Alhazzani, W.; Møller, M.H. Use of the GRADE approach in systematic reviews and guidelines. Br. J. Anaesth. 2019, 123, 554–559. [Google Scholar] [CrossRef]
- Ferracane, J.L. Hygroscopic and hydrolytic effects in dental polymer networks. Dent. Mater. 2006, 22, 211–222. [Google Scholar] [CrossRef]
- Yap, A.; Chandra, S.; Chungo, S.; Lim, C. Changes in flexural properties of composite restoratives after aging in water. Oper. Dent. 2002, 27, 468–474. [Google Scholar]
- Turksayar, A.A.D.; Donmez, M.B.; Olcay, E.O.; Demirel, M.; Demir, E. Effect of printing orientation on the fracture strength of additively manufactured 3-unit interim fixed dental prostheses after aging. J. Dent. 2022, 124, 104155. [Google Scholar] [CrossRef]
- Reymus, M.; Fabritius, R.; Keßler, A.; Hickel, R.; Edelhoff, D.; Stawarczyk, B. Fracture load of 3D-printed fixed dental prostheses compared with milled and conventionally fabricated ones: The impact of resin material, build direction, post-curing, and artificial aging—An in vitro study. Clin. Oral Investig. 2019, 24, 701–710. [Google Scholar] [CrossRef]
- Alaqeel, S.M.; Ramakrishnaiah, R.; Basavaraju, R.M.; Kotha, S.B.; Durgesh, B.H.; Vallittu, P.K. Effect of 3D printing direction and water storage on nano-mechanical properties of 3D printed and auto-polymerized polymer with special emphasis on printing layer interface. Mater. Express. 2019, 9, 351–357. [Google Scholar] [CrossRef]
- Štaffová, M.; Ondreáš, F.; Svatík, J.; Zbončák, M.; Jančář, J.; Lepcio, P. 3D printing and post-curing optimization of photopolymerized structures: Basic concepts and effective tools for improved thermomechanical properties. Polym. Test. 2022, 108, 107499. [Google Scholar] [CrossRef]
- Ikejima, I.; Nomoto, R.; McCabe, J.F. Shear punch strength and flexural strength of model composites with varying filler volume fraction, particle size and silanation. Dent. Mater. 2003, 19, 206–211. [Google Scholar] [CrossRef]
- Gajewski, V.E.; Pfeifer, C.S.; Fróes-Salgado, N.R.; Boaro, L.C.; Braga, R.R. Monomers used in resin composites: Degree of conversion, mechanical properties and water sorption/solubility. Braz. Dent. J. 2012, 23, 508–514. [Google Scholar] [CrossRef]
- Kowalska, A.; Sokolowski, J.; Bociong, K. The photoinitiators used in resin based dental composite—A review and future perspectives. Polymers 2021, 13, 470. [Google Scholar] [CrossRef]
- Park, S.M.; Park, J.M.; Kim, S.K.; Heo, S.J.; Koak, J.Y. Comparison of Flexural Strength of Three-Dimensional Printed Three-Unit Provisional Fixed Dental Prostheses according to Build Directions. J. Korean Dent. Sci. 2019, 12, 13–19. [Google Scholar]
- Revilla-León, M.; Jordan, D.; Methani, M.M.; Piedra-Cascón, W.; Özcan, M.; Zandinejad, A. Influence of printing angulation on the surface roughness of additive manufactured clear silicone indices: An in vitro study. J. Prosthet. Dent. 2021, 125, 462–468. [Google Scholar] [CrossRef] [PubMed]
- Loflin, W.A.; English, J.D.; Borders, C.; Harris, L.M.; Moon, A.; Holland, J.N.; Kasper, F.K. Effect of print layer height on the assessment of 3D-printed models. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 283–289. [Google Scholar] [CrossRef] [PubMed]
- Tahayeri, A.; Morgan, M.; Fugolin, A.P.; Bompolaki, D.; Athirasala, A.; Pfeifer, C.S.; Ferracane, J.L.; Bertassoni, L.E. 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent. Mater. 2018, 34, 192–200. [Google Scholar] [CrossRef]
- Deville, S.; Meille, S.; Seuba, J. A meta-analysis of the mechanical properties of ice-templated ceramics and metals. Sci. Technol. Adv. Mater. 2015, 16, 043501. [Google Scholar] [CrossRef] [PubMed]


| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Research articles in the English language | Research articles in a language other than English. |
| Human clinical studies; in vitro studies | Animal studies. |
| Studies comparing the influence of printing orientation on the physical and mechanical properties of 3D-printed polymeric provisional dental restorations | Editorials, case reports, theses, incomplete trials, reports, commentaries, review papers, conference papers, unpublished abstracts. |
| Studies comparing the influence of printing orientation on the marginal or internal fit of 3D-printed provisional dental restorations. | |
| Studies comparing the influence of printing orientation on the other properties of 3D-printed provisional dental restorations. | |
| Studies comparing the effect of printing orientation on materials other than provisional dental resins (for example, ceramics or metallic alloys). | |
| Studies comparing the effect of printing orientation on various properties of 3D-printed resins used for the fabrication of denture bases, dies, models, or orthodontic aligners. | |
| Studies comparing properties of materials under trial. |
| Author and Year | Studied Characteristics | Reviewed Property | Sample Size (n) | Details of the Assessed Materials | Primary Composition | Printing Orientation | Form and Size of Tested Specimens | Layer Thickness |
Printer Type/Brand/ Tradename |
|---|---|---|---|---|---|---|---|---|---|
| Alharbi et al., 2016 [34], Netherlands | Compressive strength | MP | n = 40 (20/orientation) | Temporis (DWS) | Hybrid composite resin | (a) 0° (b) 90° | Cylinder (height: 5.04–4.97 mm, diameter: 3.07 mm) | 50 μm | DW028D three-dimensional printer |
| Derban et al., 2021 [47], Romania | Flexure Strength | MP | n = 60 (30 material) (10 orientation) | (A) DETAX Freeprint Temp (Detax Gmbh & Co., Ettlingen, Germany); (B) NEXTDENT C & B MFH (Vertex Dental B.V., Soesterberg, The Netherlands) | (A) Methylmethacrylates; (B) Micro filled hybrid methacrylic oligomers | (a) 0° (b) 45° (c) 90° | Parallelepiped shaped (25 mm × 2 mm × 2 mm) | 50 μm | SheraPrint D30 printer (Shera Material Technology Gmbh, Lemforde, Germany) |
| Alharbi et al., 2021 [53], Saudi Arabia | Surface roughness | MP | n = 45 (9/orientation) | Temporis A2 (DWS systems) | Hybrid composite resin | (a) 90 (b) 120 (c) 135 (d) 150 (e) 180 | Anatomical crown maxillary central incisor | 50 µm | 028DWS SLA printer (DWS systems) |
| Lee at al., 2022 [45], Korea | Wear volume | MP | n = 20 (5 patients) (1 orientation and 1 conventional resin) | (A) Conventional self-cure resin: Unifast III (GC Corporation, Seoul, Republic of Korea)); (B) 3D-printed resin: RAYDENT C&B (Ray Co., Ltd., Hwaseong-si, Republic of Korea) | (A) Methylmethacrylate resin; (B) hybrid composite resin | (a) 0° (b) 45° (c) 90° | Crown (Molar) | 50 μm | MEG-PRINTER 3D II (Megagen, Daegu, Republic of Korea) |
| de Castro et al., 2022 [25], Brazil | Flexural strength; flexural modulus; microhardness | MP | For FS and FM n = 1430 (30 materials, 10 orientation, and 10 milled) | (A) Cosmos Temp SLA (Yller, Pelotas, RS, Brazil) (B) Cosmos Temp DLP (Yller, Pelotas, RS, Brazil) (C) PriZma Bioprov (Makertech, Tatuí, SP, Brazil) (D) NAnolab 3D (Wilcos do Brasil, Petr´ opolis, RJ, Brazil) | (A) and (B): Oligomers, monomers (C) acrylic monomers and oligomers; (D) nanohybrid resin | (a) 0° (b) 45° (c) 90° | FS: Bar (25 × 2 × 2 mm) microhardness analyses: disk (15 mm in diameter and 2.5 mm thick) | 50 μm | (A) FormLabs 2 (FormLabs, Somerville, MA, USA) (B) P30 (Straumann Basel, Switzerland) (C) Flash Forge Hunter (Zhejiang Flashforge 3D technology Co., Jinhua City, ZJ, China) (D) W3D (Wilcos do Brasil, Petr´opolis, RJ, Brazil) |
| Lee et al., 2022 [33], South Korea | Color stability; roughness | PP MP | n = 180 (90 layer thickness) (30 orientation) | C&B 5.0 Hybrid; ARUM | Urethane Dimethacrylate | (a) 0° (b) 45° (c) 90° | Disk-shaped (15 × 3 mm) | 25 μm 100 μm | ASIGA MAX UV (ASIGA NSW, Australia) |
| de Castro et al., 2023 [40], Brazil | Roughness; color | MP PP | For FS and FM n = 130 (30 materials, 10 orientation, and 10 milled) | (A) Cosmos Temp SLA (Yller, Pelotas, RS, Brazil); (B) Cosmos Temp DLP (Yller, Pelotas, RS, Brazil); (C) PriZma Bioprov (Makertech, Tatuí, SP, Brazil); (D) NAnolab 3D (Wilcos do Brasil, Petr´ opolis, RJ, Brazil); (E) Vita CAD-Temp (Vita Zahnfabrik, Bad Säckingen, Germany) (Control) | (A) and (B): Formlabs Temporary CB; (C) acrylic monomers and oligomers; (D) nanohybrid resin; (E) PMMA | (a) 0° (b) 45° (c) 90° | Disks (15 mm in diameter, 2.5 mm in thickness) | 50 μm | (A) FormLabs 2 (FormLabs, Somerville, MA, USA) (B) P30 (Straumann Basel, Switzerland) (C) Flash Forge Hunter (Zhejiang Flashforge 3D technology Co., Jinhua City, ZJ, China)) (D) W3D (Wilcos do Brasil, Petr´opolis, RJ, Brazil) |
| Farkas et al., 2023 [35], Romania | Tensile strength; compression strength | MP | For tensile strength: n = 24 Layer thickness 100 μm: n = 12 50 μm: n = 12 (4 orientation) For compression test n = 12 (layer thickness 100 μm) (4 orientation) | NextDent C&B MFH (3D Systems, Rock Hill, SC, USA) (ND) | Micro filled hybrid methacrylic oligomers | (a) 0° (b) 45° (c) 90° | For tensile strength: Bar (NM) For compression test: Cylinder (NM) | For tensile strength: 100 μm and 50 μm; For compression test: 50 μm | ANYCUBIC Photon Mono X |
| Alkhateeb et al. [42], 2023, Saudi Arabia | Fracture load | MP | n = 300 (150 resin, n = 10 orientation, 10 post-curing time) | (A) NextDent, C&B (NextDent, Soesterberg, The Netherlands) (CB); (B) ASIGA Asiga DentaTOOTH (ASIGA, Erfurt, Germany) | (A) Micro filled hybrid methacrylic oligomers; (B) Methacrylate-based microhybrid composite resin | (a) 0° (b) 45° (c) 90° | Three-unit interim FDP | 50 μm | NextDent 5100 DLP (3D Systems, Rock Hill, SC, USA) ASIGA MAX LED-based DLP (Asiga, Alexandria, Australia) |
| Espinar et al., 2023 [44], Spain | Color stability | PP | n = 24 (3 orientation) | (A) Detax Freeprint Temp (DETAX GmbH, Ettlingen, Germany); (B) Formlabs Temporary CB (Formlabs Inc., Somerville, MA, USA); (C) Formlabs Permanent Crown (Formlabs Inc., Somerville, MA, USA); (D) GCT- GC TempPrint, (GC Corporation, Tokyo, Japan) | (A) Methylmethacrylates; (B) Formlabs Temporary CB; (C) Ceramic-filled resin; (D) UDMA | (a) 0° (b) 90° | Square-shaped specimens (10 mm × 10 mm × 1.2 mm) | 50 µm | Asiga Max UV1 (Asiga, Alexandria, Australia) |
| Espinar et al., 2024 [41], Spain | Flexural strength; elastic modulus | MP MP | n = 160 (40 material, 20 orientation) | (A) Detax Freeprint Temp (DETAX GmbH, Ettlingen, Germany); (B) Formlabs Temporary CB (Formlabs Inc., Somerville, MA, USA); (C) Formlabs Permanent Crown (Formlabs Inc., Somerville, MA, USA); (D) GCT- GC (TempPrint, (GC Corporation, Tokyo, Japan) | (A) Methylmethacrylates; (B) Formlabs Temporary CB; (C) Ceramic-filled resin; (D) UDMA | (a) 0° (b) 90° | Bar-shaped specimens (25 mm × 2 mm × 2 mm) | 50 µm | Asiga Max UV1 (Asiga, Alexandria, Australia) |
| Queiroz et al., 2024 [43], Brazil | Flexural strength; microhardness; surface roughness | MP | n = 30 (10 orientation) | AA Temp, PrintaX, (Odonto Mega import, Odonto Mega import, Ribeirão Preto, SP, Brazil) | N/M | (a) 0° (b) 45° (c) 90° | Bar (4 × 2 × 10 mm) | 50 μm | Mikra Resin 3D Printer (Zhangzhou Echo Technology Co., Ltd., Zhangzhou, China) |
| Mudhaffer et al., 2025 [38], United Kingdom | Flexural strength; flexural modulus | MP | n = 540 (180 material) (60 orientation) | (A) Nextdent CB MFH (3D systems, Netherlands) (ND) (B) Dima CB temp (Kulzer GmbH, Germany) (DT) (C) GC temp print (GC dental, Japan) (GC) | (A) Microfilled Hybrid Methacrylic oligomers; (B) Esterification products of isopropylidiphenol; (C) UDMA | (a) 0° (b) 45° (c) 90° | Bar (2 × 2 × 25 mm) | 50 μm | ASIGA MAX UV; (ASIGA, NSW, Australia) |
| Casucci et al., 2024 [48], Italy | Flexural strength | MP | n = 120 (30 material) (10 orientation) | (A) Varseo smile teeth (VS) (Bego GmbH & Co., Bremen, Germany) (B) V-print C&B temp (VP) (Voco GmbH, Cuxhaven, Germany) (C) Bego Triniq (BT) (Bego GmbH & Co., Bremen, Germany) (D) Sprintray Crown (SC) (SprintRay, CA, USA) | (A) Isopropylidenediphenol; (B)UDMA Bis-EMA TEGDMA; (C) methylprop-2enoic acid, alpha-oxo-methyl ester; (D) methylbenzoateformate | (a) 0° (b) 45° (c) 90° | Bar (25 × 2 × 2 mm) | 50 μm | ASIGA MAX UV; (ASIGA, NSW, Australia) |
| Wan et al., 2024 [46], South Korea | Wear resistance | MP | n = 60 (10 orientation; 10 layer thickness) | C&B MFH (NextDent (3D systems, The Netherlands) | Methacrylic oligomers | (a) 0° (b) 45° (c) 90 | Rectangular specimens (15 × 10 × 10 mm) | 50 µm 100 µm | MAX UV, (Asiga, NSW, Australia) |
| Ortega NM et al., 2024 [51], Spain | Surface roughness | MP | n = 30 (10/orientation) | GC Temp PRINT (GC Corporation, Tokyo, Japan) | UDMA | (a) 0° (b) 45° (c) 90 | Anatomical crown maxillary right premolar | 50 µm | Asiga MAX UV (Asiga, NSW, Australia) |
| Aljehani et al., 2024 [36], Saudi Arabia | Fracture resistance | MP | n = 40 (10 orientation and 10 milled) | (A) Freeprint temp (Detax, Ettlingen, Germany); (B) Milled (control group): Coratemp, (White Peaks, Germany) | (A) Methylmethacrylates; (B) polymethyl methacrylate | (a) 0° (b) 45° (c) 90° | Fully contoured anatomical crown (central incisor) | 50 μm | Asiga Max, (Asiga, NSW, Australia) |
| Khanlar et al., 2023 [37], United States | Surface roughness | MP | n = 80 (20 orientation and 20 conventional) | (A) E-Dent C&B MHF (EnvisionTEC Inc, GmbH, Gladbeck, Germany); (B) Protemp 4 (3M ESPE) | (A) Microfilled hybrid material; (B) Bis-acryl resin | (a) 0° (b) 45° (c) 90° | Disk-shaped specimens (20 × 10 mm) | NM | Envisiontec VIDA HD; (EnvisionTEC GmbH, Gladbeck, Germany) |
| Mudhaffer et al., 2024 [39], United Kingdom | Martens hardness | MP | 3D-rinted n = 108 (36 material) (12 orientation); Milled (n = 24) (12 material) | 3D-Printed: (A) Nextdent CB MFH, 3D systems, The Netherlands (ND); (B) Dima CB temp, Kulzer, Germany (DT); (C) GC temp print, GC dental, Japan (GC) Milled; (D) LAVA ultimate, 3 M ESPE, USA; (E) Telio CAD, Ivoclar vivadent AG | (A) Microfilled Hybrid Methacrylic oligomers; (B) Esterification products of isopropylidiphenol; (C) UDMA; (D) BisGMA, UDMA; (E) PMMA | (a) 0° (b) 45° (c) 90° | Disks 20 mm (diameter) × 2.3 mm (height) | 50 μm | ASIGA MAX UV; (ASIGA, NSW, Australia) |
| de Gois Moreira et al., 2025 [49], Brazil | Flexural strength Roughness | MP | For Flexural strength: n = 450 (150 layer thickness) (30 orientation); For roughness n = 2 groups | Cosmos Tempo (Yller Biometeriais SA, Pelotas, Brazil) | Oligomers; monomers | (a) 0° (b) 30° (c) 45° (d) 60° (e) 90° | Bars (26 mm × 2.2 mm × 2.2 mm) | 25 μm 50 μm 100 μm | Forms 2, Formslab |
| Kaiahara et al., 2025 [50], Brazil | Flexural strength | MP | n = 15 (5/orientation) (n = 5; control group) | COSMOS TEMP, A1, (Yller Biomaterials, Pelotas, Brazil); Milled resin: Duralay color 81(Reliance Dental MFG Co, IL, USA) | Methacrylates PMMA | (a) 0° (b) 45° (c) 90 | Bar-shaped specimen | 50 µm | BASIC PRINTER X (3DBasic, Marília, Sao Paulo, Brazil) |
| Author and Year | Alkhateeb et al., 2023 [42] | Aljehani et al., 2024 [36] |
|---|---|---|
| Maximum Fracture Force (N) (Printing angle: 0°) | Fracture Load: (A) NextDent, C&B: Post-curing time: 0 min: 610.06 ± 208.95; 30 min: 980.72 ± 298.70; 60 min: 1259.64 ± 205.80; 90 min: 1476.99 ± 71.47; 120 min: 1683.56 ± 207.57 (B) ASIGA resin: Post-curing time: 0 min: 794.83 ± 68.52; 30 min: 1013.31 ± 140.13; 60 min: 1067.35 ± 75.42; 90 min: 1267.00 ± 240.58; 120 min: 1434.43 ± 288.52 | Fracture resistance: 374.99 ± 39.7 |
| Maximum Fracture Force (N) (Printing angle: 45°) | Fracture Load: (A) NextDent, C&B: Post-curing time: 0 min: 532.83 ± 109.21; 30 min: 1307.32 ± 88.89; 60 min: 1438.88 ± 209.60; 90 min: 1437.02 ± 230.00; 120 min: 1507.19 ± 90.37 (B) ASIGA resin: Post-curing time: 0 min: 626.32 ± 96.41; 30 min: 1113.47 ± 61.84; 60 min: 1102.81 ± 148.05; 90 min: 1327.30 ± 161.96; 120 min: 1487.58 ± 179.52 | Fracture resistance: 321.13 ± 30.6 |
| Maximum Fracture Force (N) (Printing angle: 90°) | Fracture Load: (A) NextDent, C&B: Post-curing time: 0 min: 503.29 ± 196.37; 30 min: 1168.46 ± 172.91; 60 min: 1207.51 ± 151.98; 90 min: 1237.17 ± 98.03; 120 min: 1342.44 ± 76.05 (B) ASIGA resin: Post-curing time: 0 min: 602.03 ± 82.76; 30 min: 1041.01 ± 145.87; 60 min: 1076.02 ± 89.74; 90 min: 1124.87 ± 121.59; 120 min: 1203.05 ± 114.49 | Fracture resistance: 397.28 ± 49.8 |
| Maximum Fracture Force (N) for Milled/conventional specimens (N) | N/A | Fracture resistance: Milled: 1157.16 ± 75.0 |
| Exposure Agent/Aging Procedure | Thermal cycling for 5000 cycles | No |
| Testing Machine | Universal testing machine | Universal testing machine |
| Conclusions &/or Recommendations | For all respective curing times, Fracture Load: 45° > 0° > 90° Post-curing time has a positive effect on fracture load. Fracture load according to curing time: 120 min > 90 min > 60 min > 30 min > 0 min | Fracture resistance: Milled > 3D printed 3D printed: 90° > 0° > 45° |
| Author and Year | de Castro et al., 2023 [40] | Lee et al., 2022 [33] | Espinar et al., 2023 [44] |
|---|---|---|---|
| Immersion media/surface treatment | Toothbrushing wear | Distilled water, coffee solution, and red wine | - |
| Immersion/exposure duration/aging | 10,000 cycles | 30 days | - |
| Mean alteration in color of conventional/milled specimens | 2.063 | - | - |
| Mean alteration in color of specimens printed at 0° | (A) Cosmos Temp SLA: 3.14 ##; (B) Cosmos Temp DLP: 10.01 ## (C) PriZma Bioprov:3.61 ##; (D) NAnolab 3D:8.41 ## | ΔE00 25 μm: DW: 3.954 ± 0.107; CS: 4.434 ± 0.057; RW: 8.050 ± 0.557 100 μm: DW: 4.259 ± 0.126: CS: 2.243 ± 0.158: RW: 7.078 ± 0.324 | ΔE00 DFT showed the greatest color differences between 0° and 90° printing orientation |
| Mean alteration in color of specimens printed at 45° | (A) Cosmos Temp SLA: 3.58 ##; (B) Cosmos Temp DLP:9.46 ## (C) PriZma Bioprov:3.74 ##; (D) NAnolab 3D:8.63 ## | ΔE00 25 μm: DW: 4.058 ± 0.136; CS: 5.384 ± 0.412 RW: 8.732 ± 0.369 100 μm: DW: 3.781 ± 0.132; CS: 4.669 ± 0.093 RW: 9.038 ± 0.152 | - |
| Mean alteration in color of specimens printed at 90° | (A) Cosmos Temp SLA: 3.07 ##; (B) Cosmos Temp DLP:9.68 ## (C) PriZma Bioprov:3.55 ##; (D) NAnolab 3D:7.58 ## | ΔE00 25 μm: DW: 3.297 ± 0.041; CS: 5.697 ± 0.156 RW: 9.431 ± 0.238 100 μm: DW: 3.457 ± 0.060; CS: 5.428 ± 0.189 RW: 9.197 ± 0.247 | ΔE00 DFT showed the greatest color differences between 0° and 90° printing orientation |
| Device used | Spectrophotometer (VITA Easyshade® V, Vita Zahnfabrik) | Spectrophotometer (CM 700d; Konica Minolta) | Spectroradiometer (PR 670—Photo Research) |
| Authors’ suggestions/conclusions | No influence of printing orientation on the change in color | Printing orientation affects the color stability ΔE00: 90° > 45° > 0° | Building orientation influences the visual color and translucency. ΔE00 varies with the type of 3D-printed resin. |
| Author and Year | Farkas et al., 2023 [35] |
|---|---|
| Mean tensile strength for specimens printed at 0° (MPa) | Layer thickness: 100 μm: 56.81; 50 μm: 58.53 |
| Mean tensile strength for specimens printed at 45° (MPa) | Layer thickness: 100 μm: 51.52: 50 μm: 53.69 |
| Mean tensile strength for specimens printed at 90° (MPa) | Layer thickness: 100 μm: 49.59; 50 μm: 58.01 |
| Exposure agent/aging procedure | No |
| Testing machine | Universal testing machine |
| Conclusions and/or suggestions | TS is influenced by print orientation and print layer thickness. TS at 50 μm: 0° > 90° > 45°; TS at 100 μm: 0° > 45° > 90°; TS: 50 μm > 100 μm |
| Author and Year | Farkas et al., 2023 [35] | Alharbi et al., 2016 [34] |
|---|---|---|
| Mean compressive strength for specimens printed at 0° (Mpa) | Yield stress: 85.90; Max. stress: 146.64 | 257.7 ± 41.1 |
| Mean compressive strength for specimens printed at 45° (Mpa) | Yield stress: 98.45; Max. stress: 228.28 | - |
| Mean compressive strength for specimens printed at 90° (Mpa) | Yield stress: 110.06; Max. stress: 238.26 | 297.7 ± 34.4 |
| Exposure agent/aging procedure | No | - |
| Testing machine | Universal testing machine | Universal testing machine |
| Conclusions and/or recommendations | CS influenced by print orientation: CS: 90° > 45° > 0° | CS influenced by print orientation: CS: 90° > 0° |
| Author and Year | Queiroz et al., 2024 [43] | de Castro et al., 2022 [25] | Mudhaffer et al., 2024 [39] |
|---|---|---|---|
| Mean microhardness for specimens printed at 0° (Kgf/mm2/KHN/HV/MPa) | VH (HV): 20.30 ± 4.01 | Knoop Hardness: Cosmos Temp—SLA: 7.6 ± 0.6 Cosmos Temp—DLP: 9.7 ± 2.3 PriZma BioProv: 18.4 ± 1.3 Nanolab 3D: 40.3 ± 3.3 | Martens hardness (A) ND: DW:101.4 ± 3.5; AS: 101.9 ± 4.3 (B) DT: DW: 64.6 ± 2.7; AS: 60.8 ± 5.8 (C) GC: DW: 66.9 ± 5.4; AS: 66.6 ± 5.4 |
| Mean microhardness for specimens printed at 45° (Kgf/mm2/KHN/HV/MPa) | VH (HV): 21.80 ± 2.25 | Knoop Hardness: Cosmos Temp—SLA: 5.3 ± 0.5 Cosmos Temp—DLP: 8.5 ± 2.0 PriZma BioProv: 18.4 17.6 ± 1.1 Nanolab 3D: 41.6 ± 2.1 | Martens hardness (A) ND: DW: 104.9 ± 3.2; AS: 102.4 ± 3.7 (B) DT: DW: 66.5 ± 5.1; AS: 64.4 ± 3.3 (C) GC: DW: 68.2 ± 3.5; AS: 65.3 ± 6.5 |
| Mean microhardness for specimens printed at 90° (Kgf/mm2/KHN/HV/MPa) | VH (HV): 21.00 ± 3.92 | Knoop Hardness: Cosmos Temp—SLA: 7.6 ± 0.6 Cosmos Temp—DLP: 10.5 ± 2.2 PriZma BioProv: 17.2 ± 1.3 Nanolab 3D: 40.8 ± 3.2 | Martens hardness (A) ND:DW: 102.9 ± 2.7; AS: 101.2 ± 4.8 (B) DT: DW: 67.0 ± 4.4; AS: 66.7 ± 3.0 (C) GC: DW: 72.9 ± 4.4; AS: 72.5 ± 2.9 |
| Mean microhardness for specimens fabricated by milling/conventional technique (in MPa) | - | Knoop Hardness: Vita Temp CAD (Control): 28.4 ± 1.8 | (D) LAVA ultimate: DW:584.4 ± 14.8; AS: 579.7 ± 9.4 (E) Telio CAD: DW: 119 ± 13.3; AS: 104 ± 12.0 |
| Surface treatment/exposure agent/aging procedure | No | Immersion for 1 year in distilled water | Immersion in distilled water and artificial saliva for 90 days |
| Surface treatment/exposure agent/aging procedure | HMV-G series (Shimadzu Corp.) | Future-Tech FM Corp. | Zwick Martens Hardness Instrument (Z2.5, ZwickRoell Ltd.) |
| Authors’ recommendations/conclusions | MH: 45° > 90° > 0° | KH: Cosmos Temp-SLA: 0° = 90° > 45° Cosmos Temp-DLP: 90° > 0° > 45° PriZma BioProv: 0° > 45° > 90° Nanolab 3D: 45° > 90° > 0° Milled > 3D Printed | MH: ND: 45° > 90° > 0° DT: 90° > 45° > 0° GC: 90° > 45° > 0° Milled > 3D Printed |
| Author and Year | SR Without Aging/Wear | SR After Aging/Wear | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Specimens Printed at 0° (Ra/Sa in μm) | Specimens Printed at 30° (Ra/Sa in μm) | Specimens Printed at 45° (Ra/Sa in μm) | Specimens Printed at 60° (Ra/Sa in μm) | Specimens Printed at 90° (Ra/Sa in μm) | Milled/ Conventional Specimens (Ra/Sa in μm) | Specimens Printed at 0° (Ra in μm) | Specimens Printed at 45° (Ra in μm) | Specimens Printed at 90° (Ra in μm) | Milled/ Conventional Specimens (Ra/Sa in μm) | |
| Queiroz et al., 2024 [43] | Ra: 0.10 ± 0.06 | - | Ra: 1.62 ± 0.55 | - | Ra: 0.97 ± 0.22 | NA | NA | NA | NA | |
| Khanlar et al., 2023 [37] | Sa: 1.03 ± 0.11 | - | Sa: 3.80 ± 0.76 | - | Sa: 2.34 ± 0.62 | Sa: 2.93 ± 0.90 | NA | NA | NA | |
| de Gois Moreira et al., 2025 [49] | Sa: 25 μm: 9.58 ± 3.50 50 μm: 9.66 ± 4.83 100 μm: 16.85 ± 0.64 | Sa: 25 μm: 28.25 ± 2.62 50 μm: 10.0 ± 4.67 100 μm: 13.65 ± 3.61 | Sa: 25 μm: 13.73 ± 1.75 50 μm: 14.45 ± 1.06 100 μm: 9.17 ± 0.48 | Sa: 25 μm: 9.5 ± 3.50 50 μm: 11.47 ± 2.81 100 μm: 15.69 ± 4.89 | Sa: 25 μm: 8.97 ± 3.39 50 μm: 8.41 ± 2.82 100 μm: 8.81 ± 3.51 | NA | NA | NA | NA | |
| de Castro et al., 2023 [40] | Sa: (A) Cosmos Temp SLA: 0.088 ± 0.044 (B) Cosmos Temp DLP: 0.102 ± 0.034 (C) PriZma Bioprov: 0.066 ± 0.015 (D) Nanolab 3D: 0.201 ± 0.017 | - | Sa: (A) Cosmos Temp SLA: 0.109 ± 0.031 (B) Cosmos Temp DLP: 0.104 ± 0.038 (C) PriZma Bioprov: 0.074 ± 0.014 (D) Nanolab 3D: 0.204 ± 0.012 | - | Sa: (A) Cosmos Temp SLA: 0.110 ± 0.044 (B) Cosmos Temp DLP: 0.116 ± 0.047 (C) PriZma Bioprov: 0.067 ± 0.009 (D) Nanolab 3D: 0.202 ± 0.014 | Sa: 0.050 ± 0.005 | Toothbrushing wear: Sa: (A) Cosmos Temp SLA: 0.310 ± 0.041 (B) Cosmos Temp DLP: 0.284 ± 0.052 (C) PriZma Bioprov: 0.252.4 ± 0.064 (D) Nanolab 3D: 0.288 ± 0.015 | Toothbrushing wear: Sa: (A) Cosmos Temp SLA: 0.329 ± 0.076 (B) Cosmos Temp DLP: 0.288 ± 0.043 (C) PriZma Bioprov: 0.268 ± 0.088 (D) Nanolab 3D: 0.281.9 ± 0.014 | Toothbrushing wear: Sa: (A) Cosmos Temp SLA: 0.306 ± 0.039 (B) Cosmos Temp DLP: 0.308.9 ± 0.029 (C) PriZma Bioprov: 0.229.0 ± 0.049 (D) Nanolab 3D: 0.278.2 ± 0.013 | Toothbrushing wear: Sa: 0.541.5 ± 0.656 |
| Ortega NM et al., 2024 [51] | Ra: 2.23 ± 0.19 | - | Ra: 3.19 ± 0.31 | - | Ra: 1.20 ± 0.36 | - | - | - | - | - |
| Alharbi et al., 2021 [53] | Surface roughness prepolishing (Ra) (a) 90: 9.423 ± 0.954; (b) 120: 2.474 ± 0.994; (c) 135: 1.926 ± 0.531; (d) 150: 2.523 ± 0.447; (e) 180: 0.787 ± 0.166 | - | Surface roughness after polishing (Ra) (a) 90: 0.083 ± 0.032; (b) 120: 0.190 ± 0.108 (c) 135: 0.201 ± 0.056; (d) 150: 0.187 ± 0.132 (e) 180: 0.191 ± 0.099 | - | ||||||
| Author and Year | External Condition Inducing Change in SR | Testing Device | Authors’ Suggestions/Conclusions |
|---|---|---|---|
| Queiroz et al., 2024 [43] | NA | Contact profilometer (Rugosimeter model TR210, Time Group Inc.) | SR: 0° > 90° > 45° |
| Khanlar et al., 2023 [37] | NA | 3D laser scanning confocal microscope (CLSM) (KEYENCE VK-X 150/160; KEYENCE | Surface roughness: significantly influenced by printing orientation SR: 45° > 90° > 0° |
| de Gois Moreira et al., 2025 [49] | NA | 3D optical profilometer (Taylor Hobson-AMETEK) | Maximum SR displayed by e 30°/25 μm group At 50 μm printing layer thickness: SR: 45° > 60° > 30° > 0° > 90 ° |
| de Castro et al., 2023 [40] | Toothbrushing | Laser confocal microscope (OLS5000, Olympus) | No influence of printing orientation on SR. SR: (A) Cosmos Temp SLA: 90° > 45° > 0° (B) Cosmos Temp DLP: 90° > 45° > 0° (C) PriZma Bioprov: 45° > 90° > 0° (D) Nanolab 3D: 45° > 90° > 0° |
| Ortega NM et al., 2024 [51] | - | Optical 3D measurement system (InfiniteFocusG5 plus) | Print orientation parameter significantly impacted the surface roughness. Ra: 45° > 0° > 90° |
| Alharbi et al., 2021 [53] | - | Contact stylus profilometer (Talysurf i60, Metek) | Surface roughness (Ra): Pre polishing: 90° > 150° > 120° > 135° > 180° After polishing: 135° > 180° > 120° > 150° > 90° |
| Author and Year | Lee et al., 2022 [45] | Wan et al., 2024 [46] |
|---|---|---|
| Mean volume loss (mm3)/RMS (µm) for conventional self-cure resin | Mean wear volume loss: 0.70 ± 0.15 RMS values: 11.88 ± 2.69 | - |
| Mean volume loss (mm3)/RMS (µm) for specimens printed at 0° | Mean wear volume loss: 1.22 ± 0.63 RMS values: 12.14 ± 2.38 | Mean wear volume loss (mm3): 50 μm: 1.208 ± 0.196; 100 μm: 1.010 ± 0.159 |
| Mean volume loss (mm3)/RMS (µm) for specimens printed at 45° | Mean wear volume loss: 1.32 ± 0.48 RMS values: 13.78 ± 1.29 | Mean wear volume loss (mm3): 50 μm: 0.886 ± 0.232; 100 μm: 0.854 ± 0.164 |
| Mean volume loss (mm3)/RMS (µm) for specimens printed at 90° | Mean wear volume loss: 1.74 ± 0.41 RMS values: 16.46 ± 2.39 | Mean wear volume loss (mm3): 50 μm: 1.063 ± 0.268; 100 μm: 1.136 ± 0.265 |
| Duration of use/test | 1 Week | 60,000 cycles (equivalent to 3 months of clinical use) |
| Parameters of the chewing simulator | NA | Chewing simulator (vertical movement: 5 mm; horizontal movement: 2 mm) Vertical load: 5 KG; 0.8 Hz repetitive motion |
| Measuring device | Superimposition of scanned crowns | Superimposition of scanned specimens using a 3D metrology software (version 2018.1.2, 3D Systems). |
| Authors’ suggestions/conclusions | Wear volume loss and RMS: 90° > 45° > 0° > Conventional WR of 3D printed: 0° > 45° > 90° WR: Conv. Self-cure > 3D printed | Mean wear volume loss (mm3): 50 μm: 0° > 90° > 45°: 100 μm: 90° > 0° > 45° |
| Author and Year | Mean Maximum Force at Fracture for Specimens Printed at 0° (in MPa) | Mean Maximum Force at Fracture for Specimens Printed at 30° (in MPa) | Mean Maximum Force at Fracture for Specimens Printed at 45° (in MPa) | Mean Maximum Force at Fracture for Specimens Printed at 60° (in MPa) | Mean Maximum Force at Fracture for Specimens Printed at 90° (in MPa) |
|---|---|---|---|---|---|
| Derban et al., 2021 [47] | Loading direction: Perpendicular NextDent: 117.24; Detax: 100.76 | - | Loading direction: Perpendicular NextDent: 106.35; Detax: 85.05 | - | Loading direction: Perpendicular NextDent: 117.84; Detax: 113.98 |
| Queiroz et al., 2024 [43] | 236.20 ± 29.73 | - | 155.80 ± 36.19 | - | 138.70 ± 48.20 |
| Mudhaffer et al., 2025 [38] | (A) ND: (1) DW: (i) 24 h: 90.5 ± 4.1; (ii) 1 m: 81.8 ± 3.6; (iii) 3 m: 87.6 ± 4.8 (2) AS: (i) 24 h: 87.7 ± 2.7 (ii) 1 m: 72.9 ± 1.4; (iii) 3 m: 81.2 ± 3.5 (B) DT: (1) DW: (i) 24 h: 79.6 ± 3.0 (ii) 1 m: 78.3 ± 8.6; (iii) 3 m: 79.4 ± 5.7 (2) AS: (i) 24 h: 80.4 ± 2.2 (ii) 1 m: 79.5 ± 2.2; (iii) 3 m: 78.1 ± 7.0 (C) GC: (1) DW: (i) 24 h: 69.4 ± 3.5 (ii) 1 m: 82.6 ± 3.3; (iii) 3 m: 88.8 ± 7.2 (2) AS: (i) 24 h: 74.4 ± 4.0 (ii) 1 m: 78.7 ± 8.3; (iii) 3 m: 87.4 ± 8.6 | - | (A) ND: (1) DW: (i) 24 h: 102.6 ± 5.6 (ii) 1 m: 83.6 ± 1.5; (iii) 3 m: 89.6 ± 1.7 (2) AS: (i) 24 h: 94.3 ± 2.1 (ii) 1 m: 77.5 ± 1.2; (iii) 3 m: 86.6 ± 3.81 (B) DT: (1) DW: (i) 24 h: 81.7 ± 2.4 (ii) 1 m: 87.5 ± 10.0; (iii) 3 m: 92.1 ± 3.8 (2) AS: (i) 24 h: 80.0 ± 4.2 (ii) 1 m: 79.2 ± 3.2; (iii) 3 m: 87.7 ± 3.2 (C) GC: (1) DW: (i) 24 h: 74.9 ± 3.3 (ii) 1 m: 76.8 ± 4.9: (iii) 3 m: 79.7 ± 5.6 (2) AS: (i) 24 h: 85.4 ± 5.5 (ii) 1 m: 75.4 ± 3.3: (iii) 3 m: 76.9 ± 9.5 | - | (A) ND: (1) DW: (i) 24 h: 106.2 ± 4.9 (ii) 1 m: 83.2 ± 1.5; (iii) 3 m: 89.9 ± 1.9 (2) AS: (i) 24 h: 95.5 ± 3.2 (ii) 1 m: 79.9 ± 1.4; (iii) 3 m: 91.3 ± 2.1 (B) DT: (1) DW: (i) 24 h: 87.7 ± 2.1 (ii) 1 m: 102.0 ± 1.2; (iii) 3 m: 93.4 ± 6.9 (2) AS: (i) 24 h: 86.8 ± 1.1 (ii) 1 m: 86.6 ± 3.4; (iii) 3 m: 93.3 ± 1.7 (C) GC: (1) DW: (i) 24 h: 82.4 ± 3.4 (ii) 1 m: 90.3 ± 3.8; (iii) 3 m: 89.7 ± 5.8 (2) AS: (i) 24 h: 85.2 ± 3.8 (ii) 1 m: 82.9 ± 4.3; (iii) 3 m: 89.2 ± 6.9 |
| Casucci et al., 2024 [48] | (A) VS: 132.52 ± 35.25 (B) VP: 156.56 ± 25.58 (C) BT: 113.37 ± 31.93 (D) SC: 110.41 ± 36.13 | - | (A) VS: 133.04 ± 22.12 (B) VP: 130.46 ± 12.33 (C) BT: 148.91 ± 21.23 (D) SC: 136.33 ± 15.38 | - | (A) VS: 134.24 ± 14.94 (B) VP: 116.97 ± 34.87 (C) BT: 100.96 ± 16.66 (D) SC: 114.85 ± 17.72 |
| de Gois Moreira et al., 2025 [49] | Without thermocycling 25 μm: 48.6 ± 6.6; 50 μm: 41.0 ± 6.4 100 μm: 39.4 ± 5.4 With thermocycling 25 μm: 45.8 ± 3.1; 50 μm: 34.3 ± 5.8 100 μm: 39.0 ± 4.4 | Without thermocycling 25 μm: 51.0 ± 4.5; 50 μm: 44.0 ± 2.3 100 μm: 34.8 ± 4.5 With thermocycling 25 μm: 54.5 ± 6.4; 50 μm: 40.5 ± 38 100 μm: 36.0 ± 5.0 | Without thermocycling 25 μm: 41.0 ± 3.9; 50 μm: 43.3 ± 2.4 100 μm: 43.4 ± 4.0 With thermocycling 25 μm: 57.7 ± 3.1; 50 μm: 41.3 ± 4.7 100 μm: 33.6 ± 4.6 N | Without thermocycling 25 μm: 50.3 ± 3.0; 50 μm: 42.8 ± 4.6 100 μm: 38.7 ± 3.1 With thermocycling 25 μm: 47.6 ± 4.8; 50 μm: 37.9 ± 3.0 100 μm: 37.1 ± 3.4 | Without thermocycling 25 μm: 46.2 ± 4.9; 50 μm: 47.4 ± 3.5 100 μm: 37.7 ± 3.4 With thermocycling 25 μm: 63.0 ± 4.5; 50 μm: 53.6 ± 5.1 100 μm: 47.7 ± 3.7 |
| de Castro et al., 2022 [25] | Without aging Cosmos Temp-SLA: 31.3 ± 3.6 Cosmos Temp-DLP: 72.3 ± 5.8 PriZma BioProv: 86.2 ± 4.1 Nanolab 3D: 66.6 ± 9.2 After 1-year aging Cosmos Temp-SLA: 71.0 ± 10.1 Cosmos Temp-DLP: 41.3 ± 4.9 PriZma BioProv: 89.3 ± 3.4 Nanolab 3D: 41.2 ± 1.6 | - | Without aging Cosmos Temp-SLA: 35.4 ± 5 Cosmos Temp-DLP: 60.5 ± 9.8 PriZma BioProv: 84.8 ± 5.8 Nanolab 3D: 70.8 ± 3.0 After 1-year aging Cosmos Temp-SLA: 90.7 ± 12.2 Cosmos Temp-DLP: 40.9 ± 6.1 PriZma BioProv: 91.8 ± 6.6 Nanolab 3D: 39.7 ± 10.3 | - | Without aging Cosmos Temp-SLA: 39.2 ± 2.8 Cosmos Temp-DLP: 74.5 ± 3.7 PriZma BioProv: 80.3 ± 4.4 Nanolab 3D: 63.0 ± 5.5 After 1-year aging Cosmos Temp-SLA: 109.3 ± 13.9 Cosmos Temp-DLP: 35.6 ± 3.7 PriZma BioProv: 86.1 ± 8.1 Nanolab 3D: 39.4 ± 4.1 |
| Espinar et al., 2024 [41] | (A) Detax Freeprint Temp: 98.81 ± 13.54 (B) Formlabs Temporary CB: 127.83 ± 20.35 (C) Formlabs Permanent Crown: 142.62 ± 12.98 (D) GCT-GC: 94.28 ± 11.03 | - | - | - | (A) Detax Freeprint Temp: 111.36 ± 14.80 (B) Formlabs Temporary CB: 129.29 ± 23.02 (C) Formlabs Permanent Crown: 120.73 ± 18.07 (D) GCT-GC: 91.68 ± 11.78 |
| Kaiahara et al., 2025 [50] | 80.90 ± 4.0 | - | 90.10 ± 8.45 | - | 114.71 ± 7.61 |
| Author and Year | Mean/Median of Maximum Force at Fracture for Specimens Fabricated by Milling/Conventional Technique (in MPa) | Exposure Agent/Aging Method | Testing Machine | Authors’ Recommendations/ Conclusions |
|---|---|---|---|---|
| Derban et al., 2021 [47] | - | NM | Universal testing machine | FS: For both NextDent and Detax: 90° > 0° > 45° NextDent > Detax |
| Queiroz et al., 2024 [43] | - | No | Universal testing machine | FS: 0° > 45° > 90° |
| Mudhaffer et al., 2025 [38] | - | DW and AS (24 h, 1 m, 3 m) | Universal testing machine | FS is significantly influenced by printing orientation. FS: 90° > 45° > 0° Effect of aging is minimal and varies with each material. All materials met the minimum FS requirement of 80 MPa when printed at 90°. |
| Casucci et al., 2024 [48] | - | DW (24 h) | Universal testing machine | FS is significantly influenced by printing orientation, with different materials displaying varied results. FS: (A) VS: 90° > 45° > 0° (B) VP: 0° > 45° > 90° (C) BT: 45° > 0° > 90° (D) SC: 45° > 90° > 0° |
| de Gois Moreira et al., 2025 [49] | - | Thermocycling (10,000 cycles) | Universal testing machine | FS is best for specimens printed at a print layer thickness of 25 μm combined with build angles of 90° and 45°. |
| de Castro et al., 2022 [25] | Vita Temp (Control) (Milled): 94.8 ± 3.3 After 1-year aging: 83.7 ± 8.2 | 1 year water storage | Universal testing machine | After 1-year water storage, Cosmos-SLA printed at 90° showed the highest FS. FS varied with material and printing orientation. FS After 1-year aging Cosmos Temp-SLA: 90° > 45° > 0° Cosmos Temp-DLP: 0° > 45° > 90° PriZma BioProv: 45° > 0° > 90° Nanolab 3D: 0° > 45° > 90° |
| Espinar et al., 2024 [41] | - | - | Universal testing machine | Printing orientation did not influence flexural strength. (A) Detax Freeprint Temp: 90° > 0° (B) Formlabs Temporary CB: 90° > 0° (C) GCT-GC: 0° > 90° |
| Kaiahara et al., 2025 [50] | 78.13 ± 7.94 | - | Universal testing machine | Printing orientation significantly influences flexural strength. FS: 90° > 45° > 0° FS: 3D printed > Milled |
| Author and Year | Espinar et al., 2024 [41] |
|---|---|
| Mean Elastic Modulus of specimens printed at 0° (MPa) | (A) Detax Freeprint Temp: 2552.55 ± 155.84 (B) Formlabs Temporary CB: 4426.70 ± 512.76 (C) Formlabs Permanent Crown: 4262 ± 442.49 (D) GCT-GC: 2898.73 ± 267.65F |
| Mean Elastic Modulus of specimens printed at 90° (MPa) | (A) Detax Freeprint Temp: 2750.00 ± 140.31 (B) Formlabs Temporary CB: 6639.50 ± 231.74 (C) Formlabs Permanent Crown: 4349.20 ± 230.93 (D) GCT-GC: 2887.67 ± 176.63 |
| Testing Machine | Universal testing machine |
| Authors’ Recommendations/Conclusions | Printing orientation did not influence elastic modulus. (A) Detax Freeprint Temp: 90° > 0° (B) Formlabs Temporary CB: 90° > 0° (C) GCT-GC: 0° > 90° |
| Outcome | Effect of Different Printing Orientations on the Mechanical Properties of 3D-Printed Provisional Fixed Dental Prosthesis [25,34,39,41,42,43,45,46,47,48,49,50,51,53] | Effect of Different Printing Orientations on the Physical Properties of 3D-Printed Provisional Fixed Dental Prosthesis [33,40,44] |
|---|---|---|
| Inconsistency | NP | NP |
| Indirectness | NP | NP |
| Imprecision | NP | NP |
| Risk of Bias | P | P |
| Publication Bias | NP | NP |
| Strength of Evidence |  |  |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alqarawi, F.K. The Influence of Printing Orientation on the Properties of 3D-Printed Polymeric Provisional Dental Restorations: A Systematic Review and Meta-Analysis. J. Funct. Biomater. 2025, 16, 278. https://doi.org/10.3390/jfb16080278
Alqarawi FK. The Influence of Printing Orientation on the Properties of 3D-Printed Polymeric Provisional Dental Restorations: A Systematic Review and Meta-Analysis. Journal of Functional Biomaterials. 2025; 16(8):278. https://doi.org/10.3390/jfb16080278
Chicago/Turabian StyleAlqarawi, Firas K. 2025. "The Influence of Printing Orientation on the Properties of 3D-Printed Polymeric Provisional Dental Restorations: A Systematic Review and Meta-Analysis" Journal of Functional Biomaterials 16, no. 8: 278. https://doi.org/10.3390/jfb16080278
APA StyleAlqarawi, F. K. (2025). The Influence of Printing Orientation on the Properties of 3D-Printed Polymeric Provisional Dental Restorations: A Systematic Review and Meta-Analysis. Journal of Functional Biomaterials, 16(8), 278. https://doi.org/10.3390/jfb16080278






