Hunger and Satiety Peptides: Is There a Pattern to Classify Patients with Prader-Willi Syndrome?
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Experimental Methods
2.3. Statistical Methods
3. Results
3.1. Fasting Study
3.2. Postprandial Study
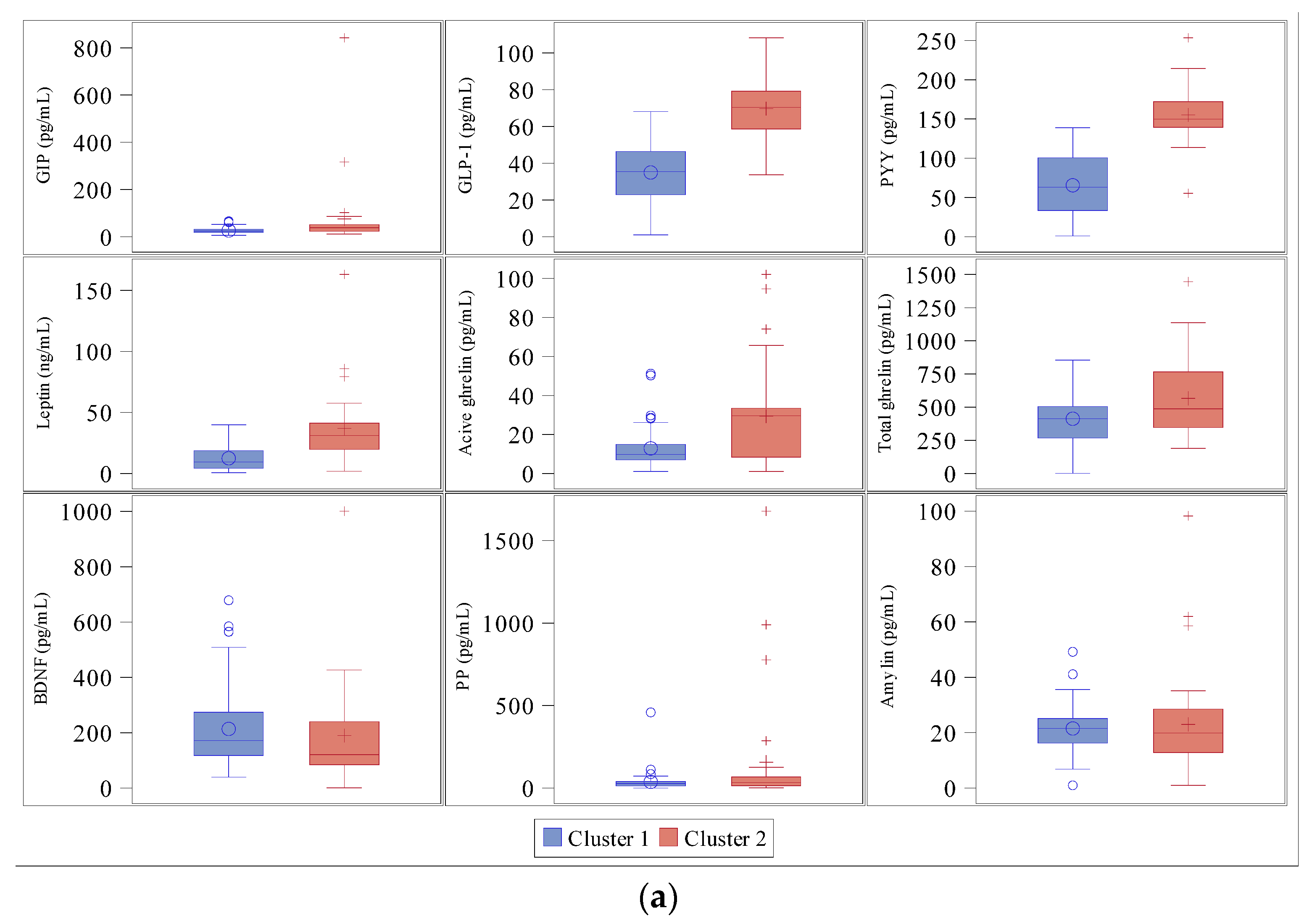
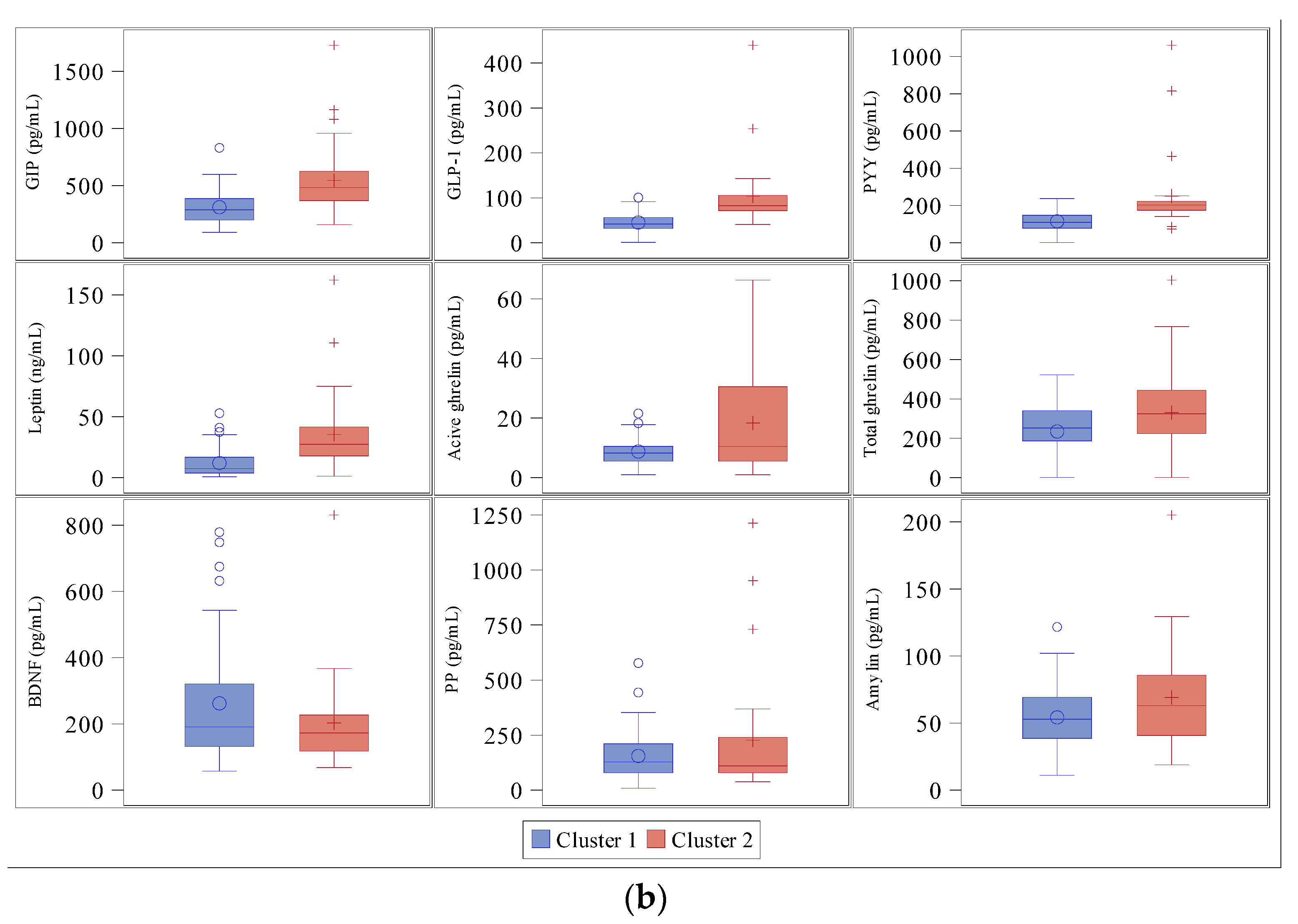
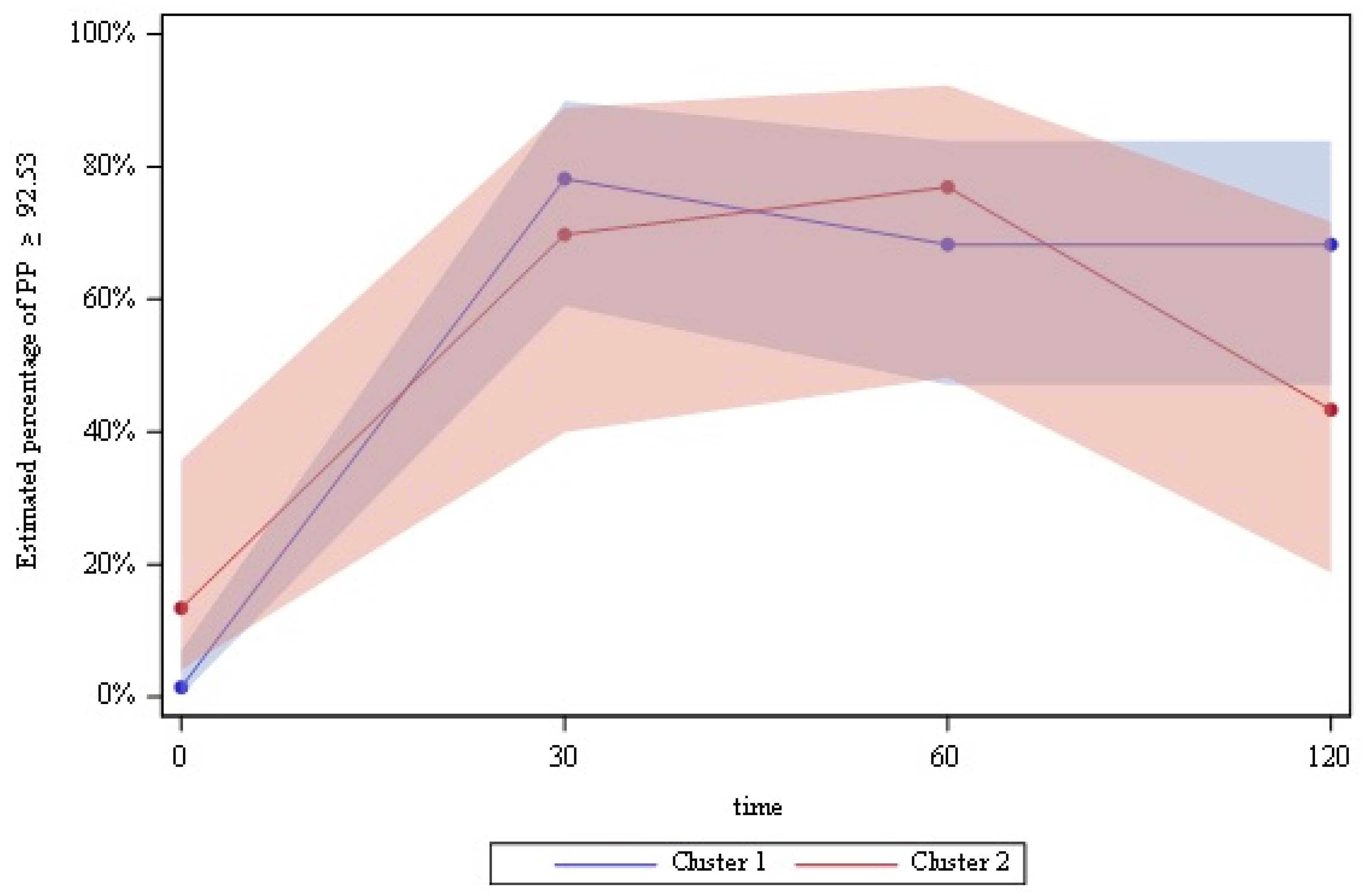
3.3. Cluster Analysis
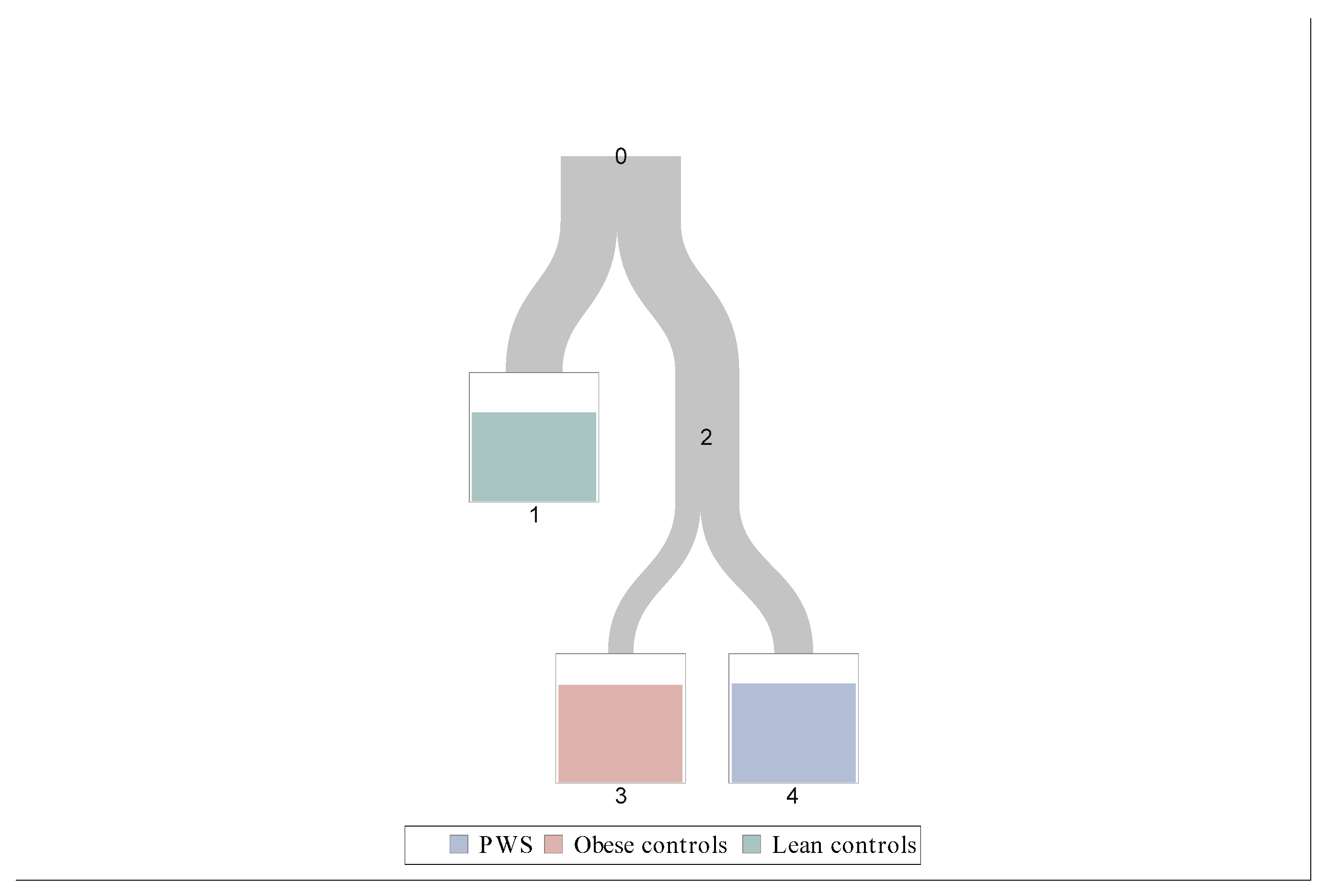
3.4. Classification Tree
- Leave 1: Leptin < 15.3 ng/mL;
- Leave 3: Leptin ≥ 15.3 ng/mL and GLP-1 < 52.5 pg/mL;
- Leave 4: Leptin ≥ 15.3 ng/mL and GLP-1 ≥ 52.5 pg/mL.
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cassidy, S.B.; Schwartz, S.; Miller, J.L.; Driscoll, D.J. Prader-Willi syndrome. Genet. Med. 2011, 14, 10–26. [Google Scholar] [CrossRef]
- Cummings, D.E.; Clement, K.; Purnell, J.Q.; Vaisse, C.; Foster, K.E.; Frayo, R.S.; Schwartz, M.W.; Basdevant, A.; Weigle, D.S. Elevated plasma ghrelin levels in Prader–Willi syndrome. Nat. Med. 2002, 8, 643–644. [Google Scholar] [CrossRef]
- Del Parigi, A.; Tschöp, M.; Heiman, M.L.; Salbe, A.D.; Vozarova, B.; Sell, S.M.; Bunt, J.C.; Tataranni, P.A. High Circulating Ghrelin: A Potential Cause for Hyperphagia and Obesity in Prader-Willi Syndrome. J. Clin. Endocrinol. Metab. 2002, 87, 5461–5464. [Google Scholar] [CrossRef] [PubMed]
- Haqq, A.M.; Farooqi, S.; O’Rahilly, S.; Stadler, D.; Rosenfeld, R.G.; Pratt, K.L.; la Franchi, S.H.; Purnell, J.Q. Serum Ghrelin Levels Are Inversely Correlated with Body Mass Index, Age, and Insulin Concentrations in Normal Children and Are Markedly Increased in Prader-Willi Syndrome. J. Clin. Endocrinol. Metab. 2003, 88, 174–178. [Google Scholar] [CrossRef]
- Kweh, F.A.; Miller, J.L.; Sulsona, C.R.; Wasserfall, C.; Atkinson, M.; Shuster, J.J.; Goldstone, A.P.; Driscoll, D.J. Hyperghrelinemia in Prader-Willi syndrome begins in early infancy long before the onset of hyperphagia. Am. J. Med. Genet. Part. A 2014, 167, 69–79. [Google Scholar] [CrossRef]
- Kuppens, R.J.; Diène, G.; Bakker, N.E.; Molinas, C.; Faye, S.; Nicolino, M.; Bernoux, D.; Delhanty, P.J.D.; van der Lely, A.J.; Allas, S.; et al. Elevated ratio of acylated to unacylated ghrelin in children and young adults with Prader–Willi syndrome. Endocrine 2015, 50, 633–642. [Google Scholar] [CrossRef]
- Tomita, T.; Greeley, G.; Watt, L.; Doull, V.; Chance, R. Protein Meal-Stimulated Pancreatic Polypeptide Secretion in Prader–Willi Syndrome of Adults. Pancreas 1989, 4, 395–400. [Google Scholar] [CrossRef]
- Zipf, W.B.; O’Dorisio, T.M.; Cataland, S.; Sotos, J. Blunted pancreatic polypeptide responses in children with obesity of Prader-Willi syndrome. J. Clin. Endocrinol. Metab. 1981, 52, 1264–1266. [Google Scholar] [CrossRef] [PubMed]
- Zipf, W.B.; O’Dorisio, T.M.; Cataland, S.; Dixon, K. Pancreatic Polypeptide Responses to Protein Meal Challenges in Obese but Otherwise Normal Children and Obese Children with Prader-Willi Syndrome*. J. Clin. Endocrinol. Metab. 1983, 57, 1074–1080. [Google Scholar] [CrossRef]
- Giménez-Palop, O.; Giménez-Pérez, G.; Mauricio, D.; González-Clemente, J.; Potau, N.; Berlanga, E.; Trallero, R.; Laferrere, B.; Caixas, A. A lesser postprandial suppression of plasma ghrelin in Prader?Willi syndrome is associated with low fasting and a blunted postprandial PYY response. Clin. Endocrinol. 2007, 66, 198–204. [Google Scholar] [CrossRef]
- Butler, M.G.; Bittel, U.C.; Talebizadeh, Z. Plasma peptide YY and ghrelin levels in infants and children with Prader-Willi syndrome. J. Pediatr. Endocrinol. Metab. 2004, 17, 1177–1184. [Google Scholar] [CrossRef][Green Version]
- Bizzarri, C.; E Rigamonti, A.; Luce, A.; Cappa, M.; Cella, S.G.; Berini, J.; Sartorio, A.; E Müller, E.; Salvatoni, A. Children with Prader–Willi syndrome exhibit more evident meal-induced responses in plasma ghrelin and peptide YY levels than obese and lean children. Eur. J. Endocrinol. 2010, 162, 499–505. [Google Scholar] [CrossRef][Green Version]
- Goldstone, A.P.; Patterson, M.; Kalingag, N.; Ghatei, M.A.; Brynes, A.E.; Bloom, S.R.; Grossman, A.B.; Korbonits, M. Fasting and Postprandial Hyperghrelinemia in Prader-Willi Syndrome Is Partially Explained by Hypoinsulinemia, and Is Not Due to Peptide YY3–36Deficiency or Seen in Hypothalamic Obesity Due to Craniopharyngioma. J. Clin. Endocrinol. Metab. 2005, 90, 2681–2690. [Google Scholar] [CrossRef] [PubMed]
- Irizarry, K.A.; Bain, J.; Butler, M.G.; Ilkayeva, O.; Muehlbauer, M.; Haqq, A.M.; Freemark, M. Metabolic profiling in Prader-Willi syndrome and nonsyndromic obesity: Sex differences and the role of growth hormone. Clin. Endocrinol. 2015, 83, 797–805. [Google Scholar] [CrossRef]
- Haqq, A.M.; Muehlbauer, M.; Svetkey, L.P.; Newgard, C.B.; Purnell, J.Q.; Grambow, S.C.; Freemark, M.S. Altered distribution of adiponectin isoforms in children with Prader-Willi syndrome (PWS): Association with insulin sensitivity and circulating satiety peptide hormones. Clin. Endocrinol. 2007, 67, 944–951. [Google Scholar] [CrossRef] [PubMed]
- Haqq, A.M.; Muehlbauer, M.J.; Newgard, C.B.; Grambow, S.; Freemark, M. The Metabolic Phenotype of Prader-Willi Syndrome (PWS) in Childhood: Heightened Insulin Sensitivity Relative to Body Mass Index. J. Clin. Endocrinol. Metab. 2011, 96, E225–E232. [Google Scholar] [CrossRef]
- Goldstone, A.P.; Thomas, E.; Brynes, A.E.; Castroman, G.; Edwards, R.; Ghatei, M.A.; Frost, G.; Holland, A.J.; Grossman, A.B.; Korbonits, M.; et al. Elevated Fasting Plasma Ghrelin in Prader-Willi Syndrome Adults Is Not Solely Explained by Their Reduced Visceral Adiposity and Insulin Resistance. J. Clin. Endocrinol. Metab. 2004, 89, 1718–1726. [Google Scholar] [CrossRef] [PubMed]
- Purtell, L.; Sze, L.; Loughnan, G.; Smith, E.; Herzog, H.; Sainsbury, A.; Steinbeck, K.; Campbell, L.V.; Viardot, A. In adults with Prader–Willi syndrome, elevated ghrelin levels are more consistent with hyperphagia than high PYY and GLP-1 levels. Neuropeptides 2011, 45, 301–307. [Google Scholar] [CrossRef] [PubMed]
- Rigamonti, A.E.; Bini, S.; Grugni, G.; Agosti, F.; De Col, A.; Mallone, M.; Cella, S.G.; Sartorio, A. Unexpectedly increased anorexigenic postprandial responses of PYY and GLP-1 to fast ice cream consumption in adult patients with Prader-Willi syndrome. Clin. Endocrinol. 2014, 81, 542–550. [Google Scholar] [CrossRef]
- Lee, H.J.; Choe, Y.H.; Lee, J.H.; Sohn, Y.B.; Kim, S.J.; Park, S.W.; Son, J.S.; Kim, S.W.; Jin, D.-K. Delayed Response of Amylin Levels after an Oral Glucose Challenge in Children with Prader-Willi Syndrome. Yonsei Med. J. 2011, 52, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Han, J.C.; Muehlbauer, M.J.; Cui, H.N.; Newgard, C.B.; Haqq, A.M. Lower Brain-Derived Neurotrophic Factor in Patients with Prader-Willi Syndrome Compared to Obese and Lean Control Subjects. J. Clin. Endocrinol. Metab. 2010, 95, 3532–3536. [Google Scholar] [CrossRef] [PubMed]
- Bueno, M.; Esteba-Castillo, S.; Novell, R.; Giménez-Palop, O.; Coronas, R.; Gabau, E.; Corripio, R.; Baena, N.; Viñas-Jornet, M.; Guitart, M.; et al. Lack of Postprandial Peak in Brain-Derived Neurotrophic Factor in Adults with Prader-Willi Syndrome. PLoS ONE 2016, 11, e0163468. [Google Scholar] [CrossRef]
- Cummings, D.E.; Purnell, J.Q.; Frayo, R.S.; Schmidova, K.; Wisse, B.E.; Weigle, D.S. A Preprandial Rise in Plasma Ghrelin Levels Suggests a Role in Meal Initiation in Humans. Diabetes 2001, 50, 1714–1719. [Google Scholar] [CrossRef] [PubMed]
- Feigerlová, E.; Diene, G.; Conte-Auriol, F.; Molinas, C.; Gennero, I.; Salles, J.-P.; Arnaud, C.; Tauber, M. Hyperghrelinemia Precedes Obesity in Prader-Willi Syndrome. J. Clin. Endocrinol. Metab. 2008, 93, 2800–2805. [Google Scholar] [CrossRef]
- De Waele, K.; Ishkanian, S.L.; Bogarin, R.; A Miranda, C.; A Ghatei, M.; Bloom, S.R.; Pacaud, D.; Chanoine, J.-P. Long-acting octreotide treatment causes a sustained decrease in ghrelin concentrations but does not affect weight, behaviour and appetite in subjects with Prader–Willi syndrome. Eur. J. Endocrinol. 2008, 159, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Tan, T.M.-M.; Vanderpump, M.; Khoo, B.; Patterson, M.; Ghatei, M.A.; Goldstone, A.P. Somatostatin Infusion Lowers Plasma Ghrelin without Reducing Appetite in Adults with Prader-Willi Syndrome. J. Clin. Endocrinol. Metab. 2004, 89, 4162–4165. [Google Scholar] [CrossRef]
- Allas, S.; Caixàs, A.; Poitou, C.; Coupaye, M.; Thuilleaux, D.; Lorenzini, F.; Diene, G.; Crinò, A.; Illouz, F.; Grugni, G.; et al. AZP-531, an unacylated ghrelin analog, improves food-related behavior in patients with Prader-Willi syndrome: A randomized placebo-controlled trial. PLoS ONE 2018, 13, e0190849. [Google Scholar] [CrossRef]
- Tauber, M.; Diene, G. Prader–Willi syndrome: Hormone therapies. Genet. Med. 2021, 181, 351–367. [Google Scholar] [CrossRef]
- Batterham, R.; Le Roux, C.; Cohen, M.A.; Park, A.J.; Ellis, S.M.; Patterson, M.; Frost, G.S.; Ghatei, M.A.; Bloom, S.R. Pancreatic Polypeptide Reduces Appetite and Food Intake in Humans. J. Clin. Endocrinol. Metab. 2003, 88, 3989–3992. [Google Scholar] [CrossRef]
- Berntson, G.G.; Zipf, W.B.; O’Dorisio, T.; Hoffman, J.A.; Chance, R.E. Pancreatic polypeptide infusions reduce food intake in Prader-Willi syndrome. Peptides 1993, 14, 497–503. [Google Scholar] [CrossRef]
- Perez-Tilve, D.; Matías, L.C.G.; Alvarez-Crespo, M.; Leiras, R.; Tovar, S.; Diéguez, C.; Mallo, F. Exendin-4 Potently Decreases Ghrelin Levels in Fasting Rats. Diabetes 2006, 56, 143–151. [Google Scholar] [CrossRef]
- Senda, M.; Ogawa, S.; Nako, K.; Okamura, M.; Sakamoto, T.; Ito, S. The glucagon-like peptide-1 analog liraglutide suppresses ghrelin and controls diabetes in a patient with Prader-Willi syndrome. Endocr. J. 2012, 59, 889–894. [Google Scholar] [CrossRef]
- Lin, D.; Wang, Q.; Ran, H.; Liu, K.; Wang, Y.; Wang, J.; Liu, Y.; Chen, R.; Sun, Y.; Liu, R.; et al. Abnormal Response to the Anorexic Effect of GHS-R Inhibitors and Exenatide in Male Snord116 Deletion Mouse Model for Prader-Willi Syndrome. Endocrinology 2014, 155, 2355–2362. [Google Scholar] [CrossRef][Green Version]
- Salehi, P.; Hsu, I.; Azen, C.G.; Mittelman, S.D.; Geffner, M.E.; Jeandron, D. Effects of exenatide on weight and appetite in overweight adolescents and young adults with Prader-Willi syndrome. Pediatr. Obes. 2016, 12, 221–228. [Google Scholar] [CrossRef]
- Sze, L.; Purtell, L.; Jenkins, A.; Loughnan, G.; Smith, E.; Herzog, H.; Sainsbury, A.; Steinbeck, K.; Campbell, L.V.; Viardot, A. Effects of a Single Dose of Exenatide on Appetite, Gut Hormones, and Glucose Homeostasis in Adults with Prader-Willi Syndrome. J. Clin. Endocrinol. Metab. 2011, 96, E1314–E1319. [Google Scholar] [CrossRef]
- Miller, J.L.; Tamura, R.; Butler, M.G.; Kimonis, V.; Sulsona, C.; Gold, J.-A.; Driscoll, D.J. Oxytocin treatment in children with Prader-Willi syndrome: A double-blind, placebo-controlled, crossover study. Am. J. Med. Genet. Part. A 2017, 173, 1243–1250. [Google Scholar] [CrossRef] [PubMed]
- Hollander, E.; Levine, K.G.; Ferretti, C.J.; Freeman, K.; Doernberg, E.; Desilva, N.; Taylor, B.P. Intranasal oxytocin versus placebo for hyperphagia and repetitive behaviors in children with Prader-Willi Syndrome: A randomized controlled pilot trial. J. Psychiatr. Res. 2020, 137, 643–651. [Google Scholar] [CrossRef]
- Damen, L.; Grootjen, L.N.; Juriaans, A.F.; Donze, S.H.; Huisman, T.M.; Visser, J.A.; Delhanty, P.J.; Hokken-Koelega, A.C. Oxytocin in young children with Prader-Willi syndrome: Results of a randomized, double-blind, placebo-controlled, crossover trial investigating 3 months of oxytocin. Clin. Endocrinol. 2020, 94, 774–785. [Google Scholar] [CrossRef]
- Everitt, B.S.; Landau, S.; Leese, M.; Stahl, D. Cluster Analysis, 5th ed.; John Wiley & Sons: London, UK, 2011; pp. 71–100. [Google Scholar]
- Zhang, H.; Singer, B.H. Recursive Partitioning and Applications. Springer Sci. Bus. Media 2010. [Google Scholar] [CrossRef]
- Considine, R.V.; Sinha, M.K.; Heiman, M.L.; Kriauciunas, A.; Stephens, T.W.; Nyce, M.R.; Ohannesian, J.P.; Marco, C.C.; McKee, L.J.; Bauer, T.L.; et al. Serum Immunoreactive-Leptin Concentrations in Normal-Weight and Obese Humans. N. Engl. J. Med. 1996, 334, 292–295. [Google Scholar] [CrossRef] [PubMed]
- Irizarry, K.A.; Mager, D.R.; Triador, L.; Muehlbauer, M.J.; Haqq, A.M.; Freemark, M. Hormonal and metabolic effects of carbohydrate restriction in children with Prader-Willi syndrome. Clin. Endocrinol. 2019, 90, 553–561. [Google Scholar] [CrossRef]
- Hirsch, H.J.; Gross-Tsur, V.; Sabag, Y.; Nice, S.; Genstil, L.; Benarroch, F.; Constantini, N. Myokine levels after resistance exercise in young adults with Prader–Willi syndrome (PWS). Am. J. Med. Genet. Part. A 2019, 182, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Talebizadeh, Z.; Butler, M.G. Insulin resistance and obesity-related factors in Prader-Willi syndrome: Comparison with obese subjects. Clin. Genet. 2004, 67, 230–239. [Google Scholar] [CrossRef] [PubMed]


| PWS (n = 30) | Obese Controls (n = 30) | Lean Controls (n = 30) | |
|---|---|---|---|
| Sex (M/F) | 15/15 | 15/15 | 15/15 |
| Age (year) | 27.5 ± 8.02 | 28.4 ± 7.13 | 27.9 ± 7.77 |
| BMI (kg/m2) | 32.4 ± 8.14 | 33.7 ± 6.88 | 22.1 ± 2.05 *$ |
| Body fat (%) | 37.0 ± 8.39 | 35.7 ± 9.70 | 20.3 ± 7.23 *$ |
| Waist (cm) | 105.0 ± 18.3 | 105.3 ± 15.1 | 78.3 ± 7.43 *$ |
| Glucose (mg/dL) | 94.1 ± 22.0 | 98.2 ± 32.1 | 86.7 ± 6.64 $ |
| Insulin (μU/mL) | 333.7 ± 218.5 | 493.2 ± 213.7 * | 304.8 ± 134.7 $ |
| HOMA-IR | 1.69 ± 0.84 | 2.94 ± 1.57 * | 1.69 ± 0.77 $ |
| PWS | Obese Controls | Lean Controls | |
|---|---|---|---|
| BDNF (pg/mL) | 113.7 (75.6–237.7) | 187.6 (119.3–303.0) | 158.2 (118.0–275.8) |
| Leptin (ng/mL) | 35.3 (20.8–42.9) | 18.5 (12.8–25.4) * | 4.4 (2.7–9.2) *$ |
| Total ghrelin (pg/mL) | 572.4 (379.8–812.5) | 279.0 (199.4–396.2) * | 477.2 (350.7–633.6) $ |
| Active ghrelin (pg/mL) | 29.0 (1.0–35.8) | 9.5 (5.5–15.0) | 12.3 (8.6–16.0) |
| PYY (pg/mL) | 149.2 (134.2–176.6) | 101.3 (72.0–134.3) * | 34.6 (1.0–67.7) *$ |
| PP (pg/mL) | 29.9 (9.5–55.3) | 23.5 (12.5–38.3) | 31.8 (23.7–61.2) |
| GLP-1 (pg/mL) | 68.5 (55.8–77.0) | 38.1 (33.7–53.3) * | 32.5 (19.3–49.6) * |
| GIP (pg/mL) | 30.2 (21.1–47.4) | 27.5 (18.5–35.6) | 24.8 (19.6–32.7) |
| Amylin (pg/mL) | 19.9 (7.8–28.5) | 22.4 (15.6–27.1) | 20.9 (16.2–24.2) |
| Classification Tree Leaves | PWS | Obese Controls | Lean Controls |
|---|---|---|---|
| Leave 1 | 2 (4.9%) | 10 (24.4%) | 29 (70.7%) |
| Leave 3 | 3 (16.7%) | 14 (77.8%) | 1 (5.6%) |
| Leave 4 | 22 (77.8%) | 6 (21.4%) | 0 (0%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bueno, M.; Boixadera-Planas, E.; Blanco-Hinojo, L.; Esteba-Castillo, S.; Giménez-Palop, O.; Torrents-Rodas, D.; Pujol, J.; Corripio, R.; Deus, J.; Caixàs, A. Hunger and Satiety Peptides: Is There a Pattern to Classify Patients with Prader-Willi Syndrome? J. Clin. Med. 2021, 10, 5170. https://doi.org/10.3390/jcm10215170
Bueno M, Boixadera-Planas E, Blanco-Hinojo L, Esteba-Castillo S, Giménez-Palop O, Torrents-Rodas D, Pujol J, Corripio R, Deus J, Caixàs A. Hunger and Satiety Peptides: Is There a Pattern to Classify Patients with Prader-Willi Syndrome? Journal of Clinical Medicine. 2021; 10(21):5170. https://doi.org/10.3390/jcm10215170
Chicago/Turabian StyleBueno, Marta, Ester Boixadera-Planas, Laura Blanco-Hinojo, Susanna Esteba-Castillo, Olga Giménez-Palop, David Torrents-Rodas, Jesús Pujol, Raquel Corripio, Joan Deus, and Assumpta Caixàs. 2021. "Hunger and Satiety Peptides: Is There a Pattern to Classify Patients with Prader-Willi Syndrome?" Journal of Clinical Medicine 10, no. 21: 5170. https://doi.org/10.3390/jcm10215170
APA StyleBueno, M., Boixadera-Planas, E., Blanco-Hinojo, L., Esteba-Castillo, S., Giménez-Palop, O., Torrents-Rodas, D., Pujol, J., Corripio, R., Deus, J., & Caixàs, A. (2021). Hunger and Satiety Peptides: Is There a Pattern to Classify Patients with Prader-Willi Syndrome? Journal of Clinical Medicine, 10(21), 5170. https://doi.org/10.3390/jcm10215170






