Abstract
Objective: The aim of this review was to evaluate the currently available scientific evidence on the efficacy of different methods as accelerators of tooth movement during orthodontic treatment: corticotomies, piezocision, micro-osteoperforations (MOP), photobiomodulation (LLLT and LED laser) and microvibrations. Search Methods: A comprehensive search was performed in the PubMed, Google Scholar, Scopus and Medline databases in May 2024. Selection Criteria: We selected randomized controlled trials based on acceleration of tooth movement during orthodontic treatment. Articles that were not randomized controlled trials (RCTs), were not published in the last ten years or corresponded to animal trials as well as those dealing with orthognathic surgery, distraction osteogenesis, electric currents, pulsed electric fields and pharmacological approaches were excluded. Results: Twenty-three studies were included in this review. All trials show accelerated tooth movement after low-level laser application, and seven studies support the efficacy of surgically assisted orthodontic treatment with corticotomies, piezocision or MOP. No article indicates statistically significant differences between the application of microvibration during orthodontic treatment and conventional treatment. No negative effects on the periodontium, loss of dental vitality or serious root resorption were reported in any publication, except in a study carried out with MOP (with an increase in root resorption). Conclusions: There is some evidence that low-level laser therapy and surgical methods are effective techniques in accelerating tooth movement during orthodontic treatment, while the evidence is very weak for vibration.
1. Introduction
The request for orthodontic treatments and access to them has increased in recent years as well as the demand from patients to reduce the duration of the treatments. The best current evidence based on prospective studies indicates that comprehensive orthodontic treatment requires an average of two years to be completed [1], depending on factors such as the severity of malocclusion, the orthodontist’s experience and patient compliance [2]. Prolonged treatments increase the risk of the appearance of decalcification white spots, root resorption, gingival recession and reduced patient compliance [3,4,5]. Therefore, numerous techniques and materials have been suggested to accelerate orthodontic tooth movement and, thus, reduce treatment times, and we can distinguish between invasive (surgical) and non-invasive (non-surgical) techniques or methods [6]. However, do we have sufficient scientific evidence to support the effectiveness of these methods in reducing the orthodontic treatment time? This review aims to answer this question.
1.1. Orthodontic Tooth Movement Description
Applying force to the tooth results in a biological process characterized by the remodeling of the alveolar bone and the periodontal ligament, resulting in tooth displacement [7]. When we exert a force on the periodontium, it generates an aseptic inflammatory response. This inflammation alters the homeostasis and the microcirculation of the periodontal ligament, creating areas of ischemia and vasodilation and releasing biological mediators, such as cytokines, chemokines, growth factors, neurotransmitters and hormones. These molecules trigger a series of cellular responses that stimulate bone resorption by osteoclasts on the pressure side and bone formation by osteoblasts on the tension side [8].
1.2. Invasive Methods
A multitude of techniques have been proposed to shorten orthodontic treatment times, and according to the scientific evidence, invasive or surgical methods are the most effective ones at accelerating tooth movement. Among these methods, we find interventions such as alveolar corticotomies with and without a flap, micro-osteoperforations, piezocisions and dentoalveolar distraction, among others.
1.3. Non-Invasive Methods
The literature lists different non-surgical methods that have been developed in an attempt to reduce orthodontic treatment time, such as low-intensity laser therapy [9], microvibrations [10], pulsed electromagnetic fields [11], electrical currents [12] and the administration of different substances such as vitamin D, prostaglandins, parathyroid hormone and cytokines [13]. Currently, there are very few clinical trials in humans that rate the efficacy of therapies with pulsed electromagnetic fields, electric currents and pharmacological approaches; so, in this systematic review, we focus on microvibration therapy and low-level laser and LED laser photobiomodulation.
The main objective of this review is to evaluate the scientific evidence currently available on the effectiveness and, therefore, whether their application is recommended in our patients of different methods, such as accelerators of tooth movement during orthodontic treatment.
2. Materials and Methods
2.1. Search Strategy
In May 2024, the authors conducted a search for studies in the PubMed, Google Scholar, Scopus and Medline databases. This search was carried out by two operators independently (P.C-G and L.A-Z). A specific combination of words and filters (Figure 1) was used to narrow down the search by focusing only on randomized clinical trials conducted in humans over the past 10 years. In addition, manual searches were performed on the reference lists of the chosen studies to identify additional potentially relevant articles.
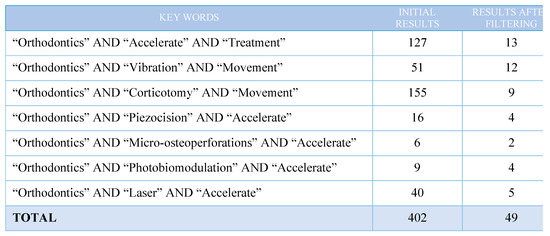
Figure 1.
Electronic literature search strategy.
2.2. Eligibility Criteria
2.2.1. Inclusion Criteria
When evaluating the inclusion of studies in the systematic review, we focused on the PICO (Population-Intervention-Comparison-Outcomes) questions:
- Population: adolescent and adult patients with Class II malocclusion requiring or not requiring the extraction of the maxillary first premolars, biprotrusive patients requiring the extraction of the four first premolars and patients with anterior lower crowding with or without requiring the extraction of the lower first premolars.
- Intervention: various surgical and non-surgical techniques used to accelerate the orthodontic tooth movement.
- Comparison: the control group is made of patients undergoing conventional orthodontic treatment (conventional brackets, self-ligating brackets or aligners) without auxiliary techniques.
- Results: rate of tooth movement in canine/incisor retraction or reduction in anterior upper and/or anterior lower crowding.
- Study Design: randomized controlled trials (RCTs).
2.2.2. Exclusion Criteria
The exclusion criteria used when selecting the studies included in this systematic review were the following:
- Studies that were conducted on animals.
- Studies that were conducted more than ten years ago.
- Studies with less than 6 participants.
- Studies other than randomized controlled trials: journal articles, systematic reviews, case reports…
- Studies referring to the acceleration of tooth movement as a result of orthognathic surgery, distraction osteogenesis procedures, electrical currents, pulsed electromagnetic fields and pharmacological approaches.
2.3. Study Selection
All titles and abstracts were independently assessed by two reviewers and selected according to the eligibility criteria. The articles were classified as included or excluded. Each reviewer (P.C-G and L.A-Z) evaluated the articles included and underwent a more detailed eligibility assessment. In cases of uncertainty, they were discussed collectively between both authors to reach a consensus.
The PRISMA (Preferred Reporting Items for Systemic Reviews and MetaAnalyses) checklist was used as a guide for the study selection flowchart of this review (Figure 2). The initial electronic search yielded 406 results, finding 24 duplicate references. A total of 353 studies were initially discarded due to the title/abstract, and subsequently, another 26 studies were discarded due to the following reasons: having been conducted more than ten years ago, being clinical trials conducted on animals or not being randomized controlled trials (RCTs); as a result, 23 clinical trials were included in this systematic review.
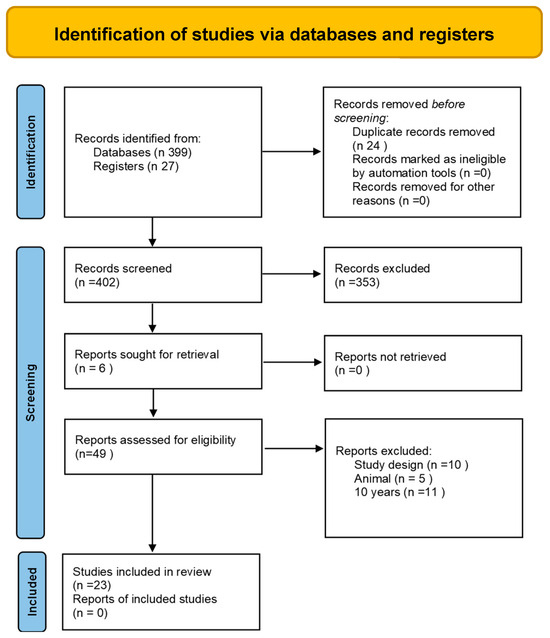
Figure 2.
Article flowchart according to PRISMA guidelines.
2.4. Risk of Bias in Individual Studies
The risk of bias in the included trials was determined using the Cochrane collaboration tool for assessing the risk of bias in randomized trials [14], suggested in The Cochrane Handbook for Systematic Reviews of Interventions (version 5.1.0). Publications were grouped into the following categories: (A) low risk of bias if all criteria are met; (B) high risk of bias if one or more criteria are not met; and (C) uncertain risk of bias when, in one or more parameters, there are not enough data to classify them either as high or low risk.
3. Results
3.1. Data Extraction and Analysis
The data extracted from the articles selected for this review are detailed in Table 1, where the following parameters are distinguished for each study: author, origin and year of implementation, design, primary objective, characteristics of the participants (number, sex, age and malocclusion class), intervention protocol, duration and results and adverse effects (if any). After selecting the articles, a reviewer was in charge of collecting the data obtained (L.A-Z). The data were collected and organized for analysis using an Excel sheet (Microsoft, Redmond, WA, USA). The authors were arranged in alphabetical order. A third evaluator performed a thorough verification of the extracted data (L.C-M). In the case of missing data for the analysis of the results, it was decided to contact the study investigators to complete the collected data.

Table 1.
Characteristics of the articles included in the systematic review concerning patients, interventions and results.
3.2. Risk of Bias Assessment
Table 2 details the summary of the risk of bias assessment of the trials included in this systematic review, according to the Cochrane collaboration tool for systematic reviews of interventions (version 5.1.0) [14]. The “+” symbol indicates a high risk of bias, the “-” symbol indicates a low risk of bias, and the “?” indicates an unclear risk of bias.

Table 2.
Risk of bias assessment according to the Cochrane collaborative tool for systematic reviews of interventions.
3.3. Description of Interventions
3.3.1. Corticotomies
We distinguish two types of techniques in the trials: alveolar corticotomy [23] and laser-assisted flapless corticotomy [17,26]. In the first case, a flap was lifted from the mesial of the superior lateral incisor to the mesial of the second premolar, and vertical cuts were made with surgical burs in the mesial and distal canine root and the mesial of the second premolar. A horizontal cut was then made by joining the vertical cuts and the additional small perforations across the exposed alveolar surface. During the laser-assisted flapless corticotomy [5,17], vestibular gingival 1.3 mm wide perforations were performed in one trial and eight [26] in the other trial between the canine and the second premolar and then 3 mm deep perforations in the alveolar cortex, all performed with the following laser parameters: 100–200 mJ, 12 Hz, 3 W. Canine retraction began in all trials immediately after the surgical intervention by tractioning with a NiTi closed coil or elastomeric chain, using in both cases a force of 150 g.
3.3.2. Piezocision
In this technique, vertical incisions were first made in the vestibular gum with a scalpel with blade number 15: two incisions at an equal distance between the maxillary canine and the second premolar in one of the trials [17], three incisions in the mesial and the distal of the maxillary canine and the mesial of the second premolar in another trial [23], five incisions between the six anterior lower teeth in another trial [25] and, in the latter case, two incisions between the lower canines and the lateral incisors and another one between the central incisors [36]. Next, incisions were made in the alveolar cortex with a 1 to 3 mm-deep piezoelectric scalpel. Canine retraction began immediately after the surgical procedure with a NiTi coil (150 g force).
3.3.3. Micro-Osteoperforations (MOP)
In six of the trials, three perforations were made vertically on the vestibular surface [16,20,28,34,35,37], and in the other trial, three perforations were made on the oral surface with three others made on the palate [21]. The perforations were made with a mini-screw, diameter 1.2 mm [21], 1.5 mm [16] or 1.8 mm [20], in the center of the area between the canine distal and the mesial of the second maxillary premolar. The depth of these perforations varied between 2 and 5 mm [34,35]. Canine traction was performed with NiTi closed coils of 150 g force and started after MOP were performed or using a closed coil spring to the micro-screw (TAD) [32,37].
3.3.4. Photobiomodulation
In this section, we distinguish five trials with low-level laser therapy (LLLT) and one trial with low-level laser with light-emitting diode (LED). Trials with LLLT employ a continuous-wave aluminum–gallium–arsenide (AlGaAs) semiconductor laser device, with a wavelength of 658 nm [29], 830 nm [19] and 940 nm [24,31,33] and energy of 2.29 J/cm2/point [29], 2.25 J/cm2/point [19], 2.5 J/cm2 [24], 7.5 J/cm2/point [33] and 8 J/cm2/point [31]. The laser was applied at various points around the teeth that were intended to be moved for a period of 3 to 10 s for each point until the canine alignment or retraction phase was completed, depending on the trial in question. The trial with an LED laser used the Biolux OrthoPulse® device, with a continuous wavelength of 850 nm and energy of 0.065 J/cm2, for five minutes per day per dental arch for six months [18].
3.3.5. Microvibration
The AcceleDent® device (OrthoAccel Technologies, Inc., Bellaire, TX, USA), which exerts a vibrational force of 0.25 N with a frequency of 30 Hz, was used in all the trials. It was used 20 min a day for 10 weeks in the trials in which the patients had conventional orthodontics (conventional brackets) [15,22,30] or until six aligner changes were completed in the trial with patients treated with Invisalign® [27], with the aligner being changed every 7 days.
3.4. Effects of Interventions
3.4.1. Corticotomies
No increase in the canine retraction rate was observed in the trial where patients underwent an alveolar corticotomy, as it was similar to that experienced in the control group. For laser-assisted flapless corticotomy, the time needed for canine retraction was reduced by 25% in one of the trials [17] and was 1.6 times faster in the other trial [26] compared to patients undergoing only conventional orthodontic treatment. No periodontal damage or loss of dental vitality was reported, and only one of the trials [26] mentions that patients experienced a mild degree of pain and secondary discomfort after the surgical procedure.
3.4.2. Piezocision
In two of the trials with patients undergoing piezocision, there was no increase in the rate of mandibular crowding alignment or the rate of maxillary canine retraction [23,36] compared to the control side or group. In another trial [17], the canine retraction rate was 2 times faster in the first month and 1.5 times faster in the second month compared to the control group, so the duration of canine retraction was reduced by 25% on the side exposed to piezocision. This increase in canine retraction was greater if it was combined with laser therapy [31]. No damage or side effects were reported after the performance of the piezocision in any of the articles.
3.4.3. Micro-Osteoperforations
Regarding this surgical technique, in three trials, no differences were found in the canine retraction rate between the side/group that underwent MOP and the control side/group [16,20,32]. However, in other studies [21,37], an increase in the rate of tooth movement was obtained on the sides subjected to MOP concerning the control sides, with canine retraction being greater in the group that underwent MOP both in a vestibular and a palatal position and not only in a vestibular (three per side). According to the different authors, this increase occurred mainly in the first 4 weeks [34] or 16 weeks [35]. A swelling sensation on the first day and mild to moderate pain that went away within a week were described as side effects.
3.4.4. Photobiomodulation
All trials describe an increase in the rate of orthodontic tooth movement in the anterior maxillary alignment and the canine retraction with both the use of LLLT and LED laser [24,29,31,33]. No differences were found between patients treated with conventional brackets and self-ligating brackets [29]. One of the trials reported that pain during the orthodontic treatment was lower on the side irradiated by laser [33], and no loss of dental vitality or periodontal damage was observed in any of the studies.
3.4.5. Microvibration
Regarding this technique, none of the trials found statistically significant differences in the rate of space closure or tooth alignment among patients who used the vibrating device and those who underwent conventional orthodontic treatment alone. There were also no differences in the perception of pain associated with the orthodontic treatment, and no adverse effects were described [15,22,27,30].
4. Discussion
In terms of surgical methods, nine of the fourteen studies show favorable results in both canine retraction rate and tooth alignment rate. MOP appear to be effective according to one of the trials, obtaining a better effect when the number of perforations made was increased, although some authors consider that this effect occurs in the first weeks after MOP [21,28,34,35,37]. Piezocision and laser-assisted flapless corticotomy are less invasive techniques than traditional alveolar corticotomy, resulting in less discomfort and inconveniences for the patient [17,23,25,26,31,36]. In addition, they can be used in patients with thin biotypes as they do not damage soft tissues and promote their healing [38], another advantage over traditional corticotomies. However, it is important to keep in mind that (1) the effect of any surgical procedure on the overall duration of the treatment is limited by the indication for the procedure, the timing of the surgery and the skill of the practitioner and that (2) the number of appointments and chair time required to complete treatment may not decrease due to the recommended shorter intervals between check-ups. Therefore, it would be interesting to assess whether any reduction in the duration of the orthodontic treatment would exceed the additional cost of the surgery [39].
On the other hand, regarding non-surgical methods, we have found no evidence that the use of a supplemental vibrating device accelerates tooth movement during the treatment with conventional orthodontics or aligners [15,22,27,30]. However, the effect of low-level laser therapy and LED laser therapy appears to be promising, and the results obtained are generally consistent [18,19,24,29,31,33]. In addition, a reduction in secondary pain to orthodontic treatment was found in one of the articles [33], which could be another advantage associated with the use of this type of therapy. In contrast, it is necessary to know how much radiation could be accumulated, so investigators must be careful with the doses administered in order not to exceed the biostimulating dose range or to reach the inhibition range [40]. The use of a laser in clinical practice may be interesting in those patients who do not mind having appointments several times and at short intervals and prefer not to undergo surgical procedures [6]. Still, it is difficult to establish a standard clinical protocol, as there was not enough evidence to determine either the ideal laser configuration, the utilization frequency or the time between sessions.
To conclude, it is obvious that the number of long-term, quality studies investigating interventions to accelerate orthodontic tooth movement is very small. In most cases, only a portion of the therapy is evaluated, and so, the effects during the entire treatment are not fully evaluated. The side effects are mentioned only in some trials, and the procedures are not evaluated in terms of cost/benefit. On the other hand, perhaps we can increase the number of studies analyzed by increasing the publication time in the search so that we can obtain a larger sample for analysis and comparison of results, as well as including, in the same analysis, studies that analyze both acceleration and inhibition of movement. Therefore, long-term studies would be necessary to analyze qualitatively and quantitatively the pros and cons of each intervention, thus being able to assess which one would be the best choice for each individual patient.
5. Conclusions
- Although the contemporary literature describes numerous methods to accelerate orthodontic tooth movement, in most cases, there is no scientific evidence behind their efficacy, so their success cannot be guaranteed by applying such techniques in daily clinical practice.
- There is some evidence about surgical techniques and photobiomodulation (LLLT and LED laser) being effective in accelerating tooth movement, at least in the short-term. On the contrary, we have not found any evidence to support the effectiveness of the use of microvibration therapy during orthodontic treatment.
- The requirement for further research in the field of orthodontic tooth movement acceleration is evident, with well-designed studies paying attention to optimal application protocols, overall treatment time, potential side effects and cost–benefit analysis based on the specific characteristics of each technique.
Author Contributions
Conceptualization, L.C.-M. and P.C.-G.; methodology, H.B.-S. and M.A.-L.; software, I.D.; validation, L.C.-M.; formal analysis, C.C.-P.; investigation, P.C.-G. and L.A.-Z.; resources, M.A.-L.; data curation, C.C.-P. and H.B.-S.; writing—original draft preparation, L.C.-M.; writing—review and editing, L.A.-Z. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
The original contributions presented in this study are included in the article; further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Tsichlaki, A.; Chin, S.Y.; Pandis, N.; Fleming, P.S. How long does treatment with fixed orthodontic appliances last? A systematic review. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 308–318. [Google Scholar] [CrossRef] [PubMed]
- Mavreas, D.; Athanasiou, A.E. Factors affecting the duration of orthodontic treatment: A systematic review. Eur. J. Orthod. 2008, 30, 386–395. [Google Scholar] [CrossRef] [PubMed]
- Bishara, S.E.; Ostby, A.W. White spot lesions: Formation, prevention, and treatment. Semin. Orthod. 2008, 14, 174–182. [Google Scholar] [CrossRef]
- Segal, G.R.; Schiffman, P.H.; Tuncay, O.C. Meta analysis of the treatment-related factors of external apical root resorption. Orthod. Craniofac Res. 2004, 7, 71–78. [Google Scholar] [CrossRef]
- Royko, A.; Denes, Z.; Razouk, G. The relationship between the length of orthodontic treatment and patient compliance. Fogorvosi Szle. 1999, 92, 79–86. [Google Scholar]
- Gkantidis, N.; Mistakidis, I.; Kouskoura, T.; Pandis, N. Effectiveness of non-conventional methods for accelerated orthodontic tooth movement: A systematic review and meta-analysis. J. Dent. 2014, 42, 1300–1319. [Google Scholar] [CrossRef]
- Huang, H.; Williams, R.C.; Kyrkanides, S. Accelerated orthodontic tooth movement: Molecular mechanisms. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 620–632. [Google Scholar] [CrossRef]
- Krishnan, V.; Davidovitch, Z. On a path to unfolding the biological mechanisms of orthodontic tooth movement. J. Dent. Res. 2009, 88, 597–608. [Google Scholar] [CrossRef]
- Doshi-Mehta, G.; Bhad-Patil, W.A. Efficacy of low-intensity laser therapy in reducing treatment time and orthodontic pain: A clinical investigation. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 289–297. [Google Scholar] [CrossRef]
- Woodhouse, N.R.; DiBiase, A.T.; Johnson, N.; Slipper, C.; Grant, J.; Alsaleh, M.; Donaldson, A.N.A.; Cobourne, M.T. Supplemental vibrational force during orthodontic alignment: A randomized trial. J. Dent. Res. 2015, 94, 682–689. [Google Scholar] [CrossRef]
- Showkatbakhsh, R.; Jamilian, A.; Showkatbakhsh, M. The effect of pulsed electromagnetic fields on the acceleration of tooth movement. World J. Orthod. 2010, 11, 52–56. [Google Scholar]
- Kim, D.H.; Park, Y.G.; Kang, S.G. The effects of electrical current from a microelectrical device on tooth movement. Korean J. Orthod. 2008, 38, 337–345. [Google Scholar] [CrossRef]
- Bartzela, T.; Türp, J.C.; Motschall, E.; Maltha, J.C. Medication effects on the rate of orthodontic tooth movement: A systematic literature review. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 16–26. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.; Altman, D.; Gøtzsche, P.; Jüni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C.; et al. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. Br. Med. J. 2011, 343, 5928. [Google Scholar] [CrossRef] [PubMed]
- Abd ElMotaleb, M.A.; El-Beialy, A.R.; El-Sharaby, F.A.; ElDakroury, A.E.; Eid, A.A. Effectiveness of low frequency vibration on the rate of canine retraction: A randomized controlled clinical trial. Sci. Rep. 2024, 14, 7952. [Google Scholar] [CrossRef]
- Alkebsi, A.; Al-Maaitah, E.; Al-Shorman, H.; Alhaija, E.A. Three-dimensional assessment of the effect of micro-osteoperforations on the rate of tooth movement during canine retraction in adults with class II malocclusion: A randomized controlled clinical trial. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 771–785. [Google Scholar] [CrossRef]
- Alfawal, A.M.H.; Hajeer, M.Y.; Ajaj, M.A.; Hamadah, O.; Brad, B. Evaluation of piezocision and laser-assisted flapless corticotomy in the acceleration of canine retraction: A randomized controlled trial. Head. Face Med. 2018, 14, 4. [Google Scholar] [CrossRef]
- Al-Okla, N.; Bader, D.M.; Makki, L. Effect of photobiomodulation on maxillary decrowding and root resorption: A randomized clinical trial. APOS Trends Orthod. 2019, 8, 200–203. [Google Scholar]
- AlSayed Hasan, M.M.A.; Sultan, K.; Hamadah, O. Low-level laser therapy effectiveness in accelerating orthodontic tooth movement: A randomized controlled clinical trial. Angle Orthod. 2017, 87, 499–504. [Google Scholar] [CrossRef]
- Aboalnaga, A.A.; Salah Fayed, M.M.; El-Ashmawi, N.A.; Soliman, S.A. Effect of micro-osteoperforation on the rate of canine retraction: A split-mouth randomized controlled trial. Prog. Orthod. 2019, 20, 21. [Google Scholar] [CrossRef]
- Babanouri, N.; Ajami, S.; Saleh, P. Effect of mini-screw-facilitated micro-osteoperforation on the rate of orthodontic tooth movement: A single-center, split-mouth, randomized, controlled trial. Prog. Orthod. 2020, 21, 7. [Google Scholar] [CrossRef] [PubMed]
- DiBiase, A.T.; Woodhouse, N.R.; Papageorgiou, S.N.; Johnson, N.; Slipper, C.; Grant, J.; Alsaleh, M.; Khaja, Y.; Cobourne, M.T. Effects of supplemental vibrational force on space closure, treatment duration, and occlusal outcome: A multicenter randomized clinical trial. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 469–480. [Google Scholar] [CrossRef] [PubMed]
- da Matta Cid Pinto Fernandes, L.S.; Figueiredo, D.S.F.; Oliveira, D.D.; Houara, R.G.; Rody, W.J., Jr.; Gribel, B.F.; Soares, R.V. The effects of corticotomy and piezocision in orthodontic canine retraction: A randomized controlled clinical trial. Prog. Orthod. 2021, 22, 37. [Google Scholar] [CrossRef] [PubMed]
- Ghaffar, Y.K.A.; El Sharaby, F.A.; Negm, I.M. Effect of low-level laser therapy on the time needed for leveling and alignment of mandibular anterior crowding. Angle Orthod. 2022, 92, 478–486. [Google Scholar] [CrossRef] [PubMed]
- Gibreal, O.; Hajeer, M.Y.; Brad, B. Efficacy of piezocision-based flapless corticotomy in the orthodontic correction of severely crowded lower anterior teeth: A randomized controlled trial. Eur. J. Orthod. 2018, 41, 188–195. [Google Scholar] [CrossRef]
- Jaber, S.T.; Al-Sabbagh, R.; Hajeer, M.Y. Evaluation of the efficacy of laser-assisted fapless corticotomy in accelerating canine retraction: A split-mouth randomized controlled clinical trial. J. Oral. Maxillofac. Surg. 2022, 26, 81–89. [Google Scholar] [CrossRef]
- Katchooi, M.; Tai, S.; Cohanim, B.; Spiekerman, C.; Huang, G.; Bayirli, B. Effect of supplemental vibration on orthodontic treatment with aligners: A randomized trial. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 336–346. [Google Scholar] [CrossRef]
- Kumar, P.; Rampurawala, A.H.; Patil, A.S. Effect of micro-osteoperforations (MOPs) on the rate of en masse orthodontic tooth retraction. J. Orofac. Orthop. 2024, 85, 189–198. [Google Scholar] [CrossRef]
- Lalnunpuii, H.; Batra, P.; Sharma, K.; Srivastava, A.; Raghavan, S. Comparison of rate of orthodontic tooth movement in adolescent patients undergoing treatment by first bicuspid extraction and en-mass retraction, associated with low level laser therapy in passive self-ligating and conventional brackets: A randomized controlled trial. Int. Orthod. 2020, 18, 412–423. [Google Scholar]
- Miles, P.; Fisher, E. Assessment of the changes in arch perimeter and irregularity in the mandibular arch during initial alignment with the AcceleDent Aura appliance vs. no appliance in adolescents: A single-blind randomized clinical trial. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 928–936. [Google Scholar] [CrossRef]
- Moradinejad, M.; Chaharmahali, R.; Shamohammadi, M.; Mir, M.; Rakhshan, V. Low-level laser therapy, piezocision, or their combination vs. conventional treatment for orthodontic tooth movement: A hierarchical 6-arm split-mouth randomized clinical trial. J. Orofac. Orthop. 2024, 85, 110–122. [Google Scholar] [CrossRef] [PubMed]
- Mordente, C.M.; Oliveira, D.D.; Palomo, J.M.; Cardoso, P.A.; Assis, M.A.L.; Zenóbio, E.G.; Souki, B.Q.; Soares, R.V. The effect of micro-osteoperforations on the rate of maxillary incisors’ retraction in orthodontic space closure: A randomized controlled clinical trial. Prog. Orthod. 2024, 25, 6. [Google Scholar] [CrossRef] [PubMed]
- Qamruddin, I.; Husein, A.; Alam, M.K.; Mahroof, V.; Fida, M.; Khamis, M.F. Effects of lowlevel laser irradiation on the rate of orthodontic tooth movement and associated pain with self-ligating brackets. Am. J. Orthod. Dentofac. Orthop. 2017, 152, 622–630. [Google Scholar] [CrossRef] [PubMed]
- Raghav, P.; Khera, A.K.; Preeti, P.; Jain, S.; Mohan, S.; Tiwari, A. Effect of micro-osteoperforations on the rate of orthodontic tooth movement and expression of biomarkers: A randomized controlled clinical trial. Dent. Press. J. Orthod. 2022, 27, e2219403. [Google Scholar] [CrossRef]
- Sivarajan, S.; Doss, J.G.; Papageorgiou, S.N.; Cobourne, M.T.; Wey, M.C. Mini-implant supported canine retraction with micro-osteoperforation: A split-mouth randomized clinical trial. Angle Orthod. 2019, 89, 183–189. [Google Scholar] [CrossRef]
- Uribe, F.; Davoody, L.; Mehr, R. Efficiency of piezotome-corticision assisted orthodontics in alleviating mandibular anterior crowding-a randomized clinical trial. Eur. J. Orthod. 2017, 39, 595–600. [Google Scholar] [CrossRef]
- Venkatachalapathy, S.; Natarajan, R.; Maheswari, R.U.; Rajakumar, P.; Rangarajan, S.; Patil, D.; Manickavasagam, V. Effect of Frequency of Micro-osteoperforation on Miniscrewsupported Canine Retraction: A Single-centered, Split-mouth Randomized Controlled Trial. J. Contemp. Dent. Pract. 2022, 23, 781–787. [Google Scholar] [CrossRef]
- Vercellotti, T.; Podesta, A. Orthodontic microsurgery: A new surgically guided technique for dental movement. Int. J. Periodontics Restor. Dent. 2007, 27, 324–331. [Google Scholar]
- Hoogeveen, E.J.; Jansma, J.; Ren, Y. Surgically facilitated orthodontic treatment: A systematic review. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 51–64. [Google Scholar] [CrossRef]
- Carvalho-Lobato, P.; Garcia, V.J.; Tallón-Walton, V.; Ustrell-Torrent, J.M.; ManzanaresCéspedes, M.C.; Kasem, K. Tooth movement in orthodontic treatment with low-level laser therapy: A systematic review of human and animal studies. Photomed. Laser Surg. 2014, 32, 302–309. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).


