Abstract
Peripheral nerves are subjected to mechanical tension during limb movements and body postures. Nerve response to tensile stress can be assessed in vivo with shear-wave elastography (SWE). Greater tensile loads can lead to greater stiffness, which can be quantified using SWE. Therefore, this study aimed to conduct a systematic review and meta-analysis to perform an overview of the effect of joint movements on nerve mechanical properties in healthy nerves. The initial search (July 2023) yielded 501 records from six databases (PubMed, Embase, Scopus, Web of Science, Cochrane, and Science Direct). A total of 16 studies were included and assessed with a modified version of the Downs and Black checklist. Our results suggest an overall tendency for stiffness increase according to a pattern of neural tensioning. The main findings from the meta-analysis showed a significant increase in nerve stiffness for the median nerve with wrist extension (SMD [95%CI]: 3.16 [1.20, 5.12]), the ulnar nerve with elbow flexion (SMD [95%CI]: 2.91 [1.88, 3.95]), the sciatic nerve with ankle dorsiflexion (SMD [95%CI]: 1.13 [0.79, 1.47]), and the tibial nerve with both hip flexion (SMD [95%CI]: 2.14 [1.76, 2.51]) and ankle dorsiflexion (SMD [95%CI]: 1.52 [1.02, 2.02]). The effect of joint movement on nerve stiffness also depends on the nerve segment, the amount of movement of the joint mobilized, and the position of other joints comprised in the entirety of the nerve length. However, due to the limited number of studies, many aspects of nerve behavior together with the effect of using different ultrasound equipment or transducers for nerve stiffness evaluation still need to be fully investigated.
1. Introduction
The evaluation of the peripheral nervous system normally includes the assessment of conduction and mechanosensitivity [1,2,3,4,5]. In a clinical context, light touch, strength, and reflexes assessment together with electrodiagnostic tests are widely adopted tools to assess neural conduction [1,2,4,5], while a variety of provocative maneuvers like the straight leg raise test or the upper limb neurodynamic test are commonly used for mechanosensitivity assessment [3,6].
Ultrasonography has been increasingly used as an additional examination in patients with suspected peripheral neuropathies [7,8,9,10]. Using conventional ultrasound, one can detect morphological changes in peripheral nerves, quantify their cross-sectional areas, and assess nerve biomechanics [7,8,9,10,11,12]. Despite being a useful technique in the diagnosis of many entrapment neuropathies [7,8,9,10], conventional gray-scale ultrasound is not able to quantify some tissues’ characteristics, such as their mechanical properties.
In the last years, shear-wave elastography (SWE) has been consolidating in the evaluation of tissues’ mechanical properties as an adjunctive technique to conventional ultrasound [13,14,15,16,17,18,19]. SWE is a non-invasive ultrasound imaging technique that uses an acoustic pulse to generate a shear wave in the tissue [13,14,15]. SWE is able to quantify the elastic properties of tissues by assessing the propagation velocity of the shear wave, which is directly related to tissue stiffness [13,14,15,17]. In an elastic, homogeneous, and isotropic medium, the shear modulus (μ) can be estimated with the equation μ = ρc2, where ρ is the density (assuming ρ = 1000 kg/m3), and c is the speed of the shear wave. Young’s modulus (E) can be approximated as three times the shear modulus: E = 3μ [20]. Consequently, SWE measurements of tissue stiffness are generally reported in m/s as shear-wave velocity (SWV) or converted into kPa as formerly described [13,15,21]. Due to its simplicity and non-invasive character, SWE has already been integrated in many medical disciplines to assess different organs [18,21,22] and musculoskeletal conditions [13,16]. More recently, its application has also been extended to the evaluation of peripheral nerves [16,23,24,25,26,27,28]. The advantage of SWE lies in its capability of recognizing changes in the mechanical properties of tissues related to injury, degeneration, compression, and tension [13,28,29,30,31]. In many neural conditions, the nerve shows an increase in its stiffness in the affected area [23,24,25,26,27,28]. Hence, SWE has been proposed as a novel diagnostic tool for carpal tunnel syndrome [23,25,26], diabetic neuropathy [23,24,25,32,33], and other peripheral neuropathies [23,25,27]. Moreover, SWE may be potentially useful for the prediction of diabetic neuropathy and for the prediction of the risk of diabetic foot ulcers in diabetic neuropathy patients [32,33,34].
However, histopathological changes due to neuropathy are not the single factor affecting nerve stiffness and SWE values [16,35]. A modification of nerve stiffness has also been described in accordance with limb positions aimed to increase or decrease mechanical tension in the nervous system [29,36,37]. Peripheral nerves are exposed to different mechanical loads during limb movements and body postures, and their mechanical response to tensile stress varies depending on nerve location, joint movement, and the position of adjacent joints [11,12,28,38,39]. An increase in nerve stiffness values may be an expression of a greater tensile load applied to a certain neural segment [29,40]. Considering this, SWE may represent a useful tool for the evaluation of in vivo neural response to movement and to define how different patterns impact nerve mechanical properties.
Therefore, this study aimed to conduct a systematic review and meta-analysis to provide an overview of the effect of joint movements on nerve mechanical properties in healthy nerves. We hypothesize that positions and movements that are thought to increase neural tension will lead to higher nerve stiffness values. This information could improve the knowledge of nerve behavior and may allow clinicians to better optimize the mechanical load applied to the neural tissue during both the evaluation and treatment of various neural conditions.
2. Materials and Methods
This study was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses [41]. The protocol was registered in the PROSPERO database with the number CRD42023451960.
2.1. Search Strategy
A systematic search was performed in six databases: PubMed, Embase, Scopus, Web of Science, Science Direct, and Cochrane Library. The search was conducted in July 2023 by introducing a combination of keywords and MeSH/Emtree terms related to SWE, peripheral nerves, and joint positioning. The Boolean operators AND and OR were used to combine the search terms. Slight adjustments were made to adapt the search process to each database. The search strategy for each database is detailed in Supplementary Materials.
2.2. Eligibility Criteria
This systematic review included studies with primary data of upper/lower extremity nerve stiffness assessed by ultrasound pulse SWE in at least two joint positions in healthy nerves, with a longitudinal or cross-sectional design, published in English, Spanish, or Italian language.
The articles were excluded if they obtained data from other types of elastography (e.g., strain elastography, magnetic resonance elastography, mechanical elastographies, etc.) or only included pathological nerves or nerves with conditions that may affect their biomechanics (e.g., surgery). Studies that did not report original data (reviews, meta-analysis, opinion articles, study protocols, etc.), case reports or case series, letters to the editor, and conference papers were also excluded.
2.3. Study Selection
Once the search was performed, duplicates were removed, and potentially relevant articles were identified from the titles and abstracts. The eligibility was determined by reading the full text and considering the inclusion and exclusion criteria proposed for this systematic review.
The systematic search, study selection, and data extraction were performed by two independent researchers (G.C. and I.A.-C.). Any doubts or disagreements were resolved by a third researcher (E.E.-d.-M.).
For each included study, the following data were extracted: author, year of publication, characteristics of the sample, number of subjects, nerve, point of measure, ultrasound system, transducer orientation, region of interest (ROI), joint position, and results obtained. If a study presented relevant data only in graphic format, the information was extracted from figures with the online tool WebPlotDigitizer [42]. In case clarification was needed, the authors of the study were contacted.
2.4. Quality of the Studies
Two researchers (G.C. and I.A.-C.) independently assessed the quality of the included studies. The assessment was performed with a modified version of the Downs and Black checklist [43]. This tool was previously used in systematic reviews of in vivo biomechanical properties of peripheral nerves [11,12]. Individual items were either rated as “yes” (=1) when properly described or “no/unable to determine” (=0) if not addressed in the study or if the raters could not determine it. The total quality score was reached by final consensus, with a maximum score of 17. A total score of ≤7 was considered as low quality, 8–11 as fair quality, and >11 as good quality. This modified scoring system was originally described by Fernando et al. [44] and successively adopted in other systematic reviews [11,12].
2.5. Meta-Analysis
We performed the meta-analysis when a minimum of two studies were considered comparable. Studies were considered comparable when they reported SWE values (in m/s or kPa) for similar nerve locations and similar joint movement. Standardized mean difference (SMD) was used as a measure of effect size. If standard error (SE) was reported instead of standard deviation (SD), SD was obtained using the following formula: . In case a study presented the mean and its 95% confidence interval (CI), the respective SD was calculated by dividing the width of the CI by 3.92 and then multiplying by the square root of the sample size in that group; for small sample sizes, 3.92 was substituted with a t distribution value [45]. If median, interquartile range, minimum, and maximum values were reported, mean and SD were estimated using the methods developed by Luo et al. [46] and Shi et al. [47] after checking for the absence of significant data skewness [48]. If significant skewness was detected, the data were not included in the meta-analysis [48]. When a study presented data separately for subgroups (e.g., right and left nerves, young and old participants, etc.) the following formulae were used to combine numbers into a single sample size, mean, and SD [45]:
Separate analyses were performed depending on nerve location and joint positions. In case a study reported nerve SWE values at multiple points of measure of the same nerve segment, the most similar location to the one adopted in other included studies was used for the analysis. Baseline data were analyzed in studies with a longitudinal design.
Two studies performed by the same group shared part of the sample, where the same healthy participants who represented the entirety of the sample in one study were used as control group in a second one [49,50]. To avoid introducing duplicated participants in the meta-analysis, we extracted data from healthy subjects in one study [50], and in the other, we analyzed SWV values of the unaffected leg in the patients’ group [49].
Considering the expected heterogeneity between studies, random effect models were applied, weighing each effect size by the inverse of its variance, with this being defined as the sum of the intra-study and inter-study variances. The statistical analysis comprised the calculation of the mean effect size with its 95% confidence interval as well as the calculation of the I2 to evaluate the level of heterogeneity among studies. Forest plots were constructed to represent the results. To check the robustness of the findings, sensitivity analysis was performed by removing one study at a time from each comparison with at least 3 studies. Due to the low number of studies included in each comparison, the investigation of quantitative or qualitative moderators through sub-group analysis and meta-regression was not performed, and publication bias was not assessed [45,51]. If meta-analysis for a specific comparison was not possible due to insufficient data, the results of the studies were narratively described. All meta-analyses were conducted using RevMan 5.4 software.
3. Results
3.1. Study Selection
A total of 501 records were obtained from our initial search. After the removal of duplicates, 288 studies remained. Following the screening of titles and abstracts, 260 studies were excluded. After reading 28 full-text papers, 12 were discarded for not meeting the inclusion or exclusion criteria. Finally, 16 studies were included in the current systematic review (Figure 1).
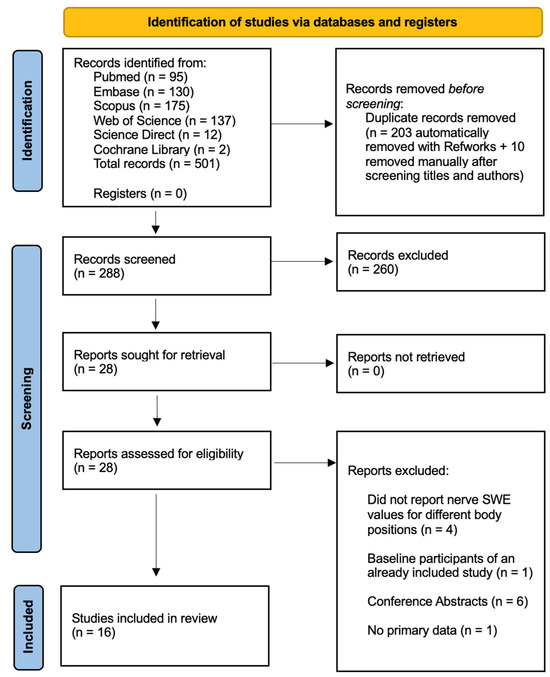
Figure 1.
PRISMA 2020 flow chart illustrating the study selection process.
3.2. Quality of the Studies
The methodological quality of the included studies is summarized in Table 1. The modified Downs and Black checklist score varied from 9 to 13. Five studies showed good quality (more than 11 points) [49,52,53,54,55], and 11 showed fair quality (8–11 points) [36,37,50,56,57,58,59,60,61,62,63]. None of the included studies scored below 9 points. The included studies mostly lacked reporting subjects’ representativeness, blinding of the assessors, and sample size calculation.

Table 1.
Modified Downs and Black checklist for quality assessment.
3.3. Characteristics of the Studies

Table 2.
Characteristics of the included studies.

Table 3.
Methodological characteristics of the included studies.
In the upper extremity, the median nerve (MN) was assessed in six studies [36,37,55,61,62,63], while the ulnar nerve (UN) was explored in three studies [37,57,60]. In the lower extremity, the sciatic nerve (SN) and the tibial nerve (TN) were evaluated in six studies [49,50,53,54,58,59] and four studies [36,52,54,56], respectively. The MN was most commonly imaged in the forearm [36,37,55,61,62], followed by the proximal elbow [36,37], and lastly at the carpal tunnel level [63]. The UN was evaluated in the elbow region in three studies [37,57,60], and one study also reported data at the forearm level [37]. The SN was assessed in the proximal thigh in all six studies [49,50,53,54,58,59], and one study also assessed it at the mid-thigh level [54]. The TN was imaged in four studies at the distal portion of the leg [36,52,54,56], and among them, one study also assessed it in the popliteal fossa and in the proximal part of the leg [54].
The most used ultrasound system was the Aixplorer Supersonic Imagine, which was employed in 10 studies [37,49,50,54,55,57,58,59,60,62]; the remaining studies used the Canon Aplio [52,56,61] and the Siemens Acuson [36,53,63]. All ultrasound systems were coupled with a lineal probe [36,37,49,50,52,53,54,55,56,57,58,59,60,61,62,63].
Fourteen studies performed nerve measurements in long axis [36,37,49,50,52,53,54,55,56,58,59,60,61,62], and two performed them in short axis [57,63]. Different regions of interest (ROIs) were used for nerve SWE assessment. In seven studies, the largest nerve area possible was used as the ROI [37,49,50,53,54,58,59]; five studies performed quantitative SWE measurements with a 2 mm ROI [55,60,61,62,63]; and three studies used multiple ROIs. Among them, two used three randomly selected ROIs [52,56], and one used four 1.5 mm ROIs along the nerve [36]; one study did not specify the characteristics of the ROI used [57]. Thirteen of the included studies reported SWE values in m/s [36,37,49,50,52,53,54,55,56,58,59,61,63], while three expressed SWE values in kPa [57,60,62].
One study [64] was excluded because its baseline was analyzed in an already included study [54].
3.4. Median Nerve
Results from the studies that analyzed the effects of joint movement/positioning on MN stiffness are summarized in Table 4.

Table 4.
Median nerve stiffness in response to joint movement.
3.4.1. Effect of Wrist Movement
The effect of wrist extension on MN SWE values was analyzed in five studies [36,55,61,62,63]. Meta-analysis showed that wrist extension significantly increased MN stiffness in its distal segment (wrist and forearm) regardless of starting from wrist flexion or wrist neutral position, with similar pooled effect sizes (SMD [95%CI]: 3.15 [1.43, 4.86], I2: 80%; SMD [95%CI]: 3.16 [1.20, 5.12], I2: 95%) (Figure 2).
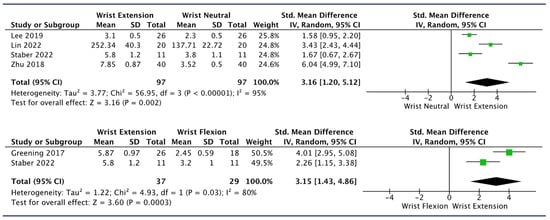
Figure 2.
Forest plots showing the impact of different wrist positions on SWE values of distal median nerve (forearm and wrist) [36,55,61,62,63].
Sensitivity analysis revealed that by removing the study of Zhu et al. [55] from the “wrist extension vs. wrist flexion” comparison, the pooled effect size decreased by 31%, and the heterogeneity decreased by 15%; however, it remained strongly in favor for wrist extension (SMD [95%CI]: 2.19 [1.07, 3.31], I2: 80%) (Table 5).

Table 5.
Summary table of sensitivity analysis performed by removing one study at a time in meta-analyses with n ≥ 3 studies.
Lin et al. [62] reported the highest MN stiffness values at the forearm level when wrist extension was combined with cervical contralateral lateral flexion starting from a shoulder abduction and elbow extension position (starting position: 137.71 ± 22.72 kPa, only wrist extension: 252.34 ± 40.30 kPa, only contralateral cervical flexion: 211.00 ± 30.49 kPa, wrist extension and contralateral cervical flexion: 297.35 ± 64.60 kPa; p < 0.001 for all movements vs. starting position). Lee et al. [63] reported that wrist extension led to higher nerve SWV values at carpal tunnel when compared to wrist at 0° regardless of the fingers’ position. However, the difference was significant only in respect to wrist at 0° with the fingers in neutral position (p < 0.001).
Additionally, one study that analyzed the effect of wrist movement on MN stiffness in the proximal elbow and in the forearm reported changes in SWV at both locations when adding wrist extension in a position of shoulder abduction and elbow flexion; however, the greatest increase in SWV was observed at the forearm level [36].
3.4.2. Effect of Finger Movement
One study assessed the effect of different finger positions on MN SWV at carpal tunnel level [55]. With the wrist in neutral position, both finger grasp and finger extension led to an increase in nerve SWV with respect to the neutral position (mean SWV ± SD (m/s): finger neutral 2.3 ± 0.5; finger grasp 2.7 ± 0.5; finger extension 2.7 ± 0.4; p < 0.05); during wrist extension, higher SWV values were observed for finger extension with respect to finger grasp and neutral positions, although the difference among these positions was not significant (mean SWV ± SD (m/s): finger neutral 2.9 ± 0.5; finger grasp 3.0 ± 0.5; finger extension 3.1 ± 0.4) [55].
3.4.3. Effect of Elbow Movement
Two studies investigated the effect of elbow movement on MN SWV in the upper arm and in the forearm, showing that performing an elbow extension from a 90° flexion angle led to a substantial increase in SWV in both locations [36,37]. Meta-analysis was not performed because data from one study [37] ended up being significantly skewed. Therefore, the SD from the median, interquartile range, and minimum and maximum values graphically reported in the study was not estimated in the present study [48].
3.4.4. Effect of Shoulder Movement
The impact of shoulder movement was investigated in one study, which reported that abducting the shoulder with the elbow and wrist flexed caused negligible changes in MN SWV in the upper arm and forearm [36].
3.4.5. Effect of Cervical Movement
One study assessed MN stiffness in response to cervical contralateral lateral flexion [62]. At the initial position of 90° of shoulder abduction and elbow extension, adding cervical contralateral lateral flexion increased nerve stiffness in the forearm from 137.71 ± 22.72 kPa to 211.00 ± 30.49 kPa with the wrist in neutral position and from 252.34 ± 40.30 kPa to 297.35 ± 64.60 with the wrist extended [62].
3.5. Ulnar Nerve
The results of the studies that investigated the UN are summarized in Table 6.

Table 6.
Ulnar nerve stiffness in response to joint movement.
Effect of Elbow Flexion
Three studies evaluated UN stiffness at different degrees of elbow flexion [37,57,60]. Meta-analysis showed a trend of progressive increase in UN stiffness in the elbow region with greater flexion angles. The largest effect sizes were observed comparing both 90° elbow flexion and end-range elbow flexion to elbow extension (SMD [95%CI]: 2.91 [1.88, 3.95], I2: 70%; SMD [95%CI]: 2.81 [0.10, 5.52], I2: 90%) (Figure 3). Sensitivity analysis was performed only for the “90° elbow flexion vs. elbow extension comparison.” After removing the study by Rugel et al. [37] from the analysis, the effect size was 16% higher and the heterogeneity decreased (SMD [95%CI]: 3.39 [2.46, 4.31], I2: 38%); after removing Wolny et al. [57], the pooled effect size decreased by 19% with no heterogeneity (SMD [95%CI]: 2.37 [1.64, 3.09], I2: 0%) (Table 5).
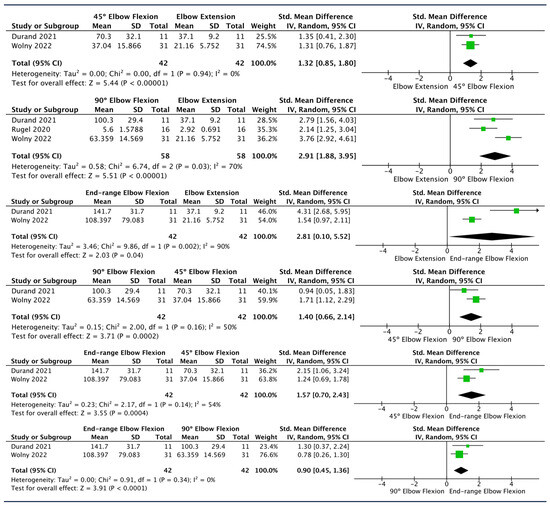
Figure 3.
Forest plots showing the impact of different elbow positions on ulnar nerve SWE values at the elbow location [37,57,60].
Additionally, one study observed a similar behavior of the UN at the forearm level, reporting an increase in SWV values with 90° elbow flexion compared to elbow extension [37].
3.6. Sciatic Nerve
SN stiffness behavior in response to joint motion is summarized in Table 7.

Table 7.
Sciatic nerve stiffness in response to joint movement.
3.6.1. Effect of Ankle Movement
Five studies measured SN SWV at different ankle angles with knee extension [49,50,53,58,59]. As these studies used different methods to express ankle angles (see Table 7), the SWV values reported at each given angle were normalized to a common scale of 0 to 100% of dorsiflexion, where 0% represented 40° of plantar flexion and 100% represented the maximum dorsiflexion. The data available for the most similar %-of-dorsiflexion angle among the mentioned studies were used to meta-analyze SN SWV in ankle dorsiflexion and ankle plantar flexion. In the comparisons of ankle dorsiflexion/plantar flexion vs. ankle in neutral position (≈0°), one study was not included due to the impossibility of estimating which percentage of the reported dorsiflexion angle corresponded to a position ≈ 0° [59].
The pooled SMDs obtained from the comparisons of ankle plantar flexion vs. neutral position and neutral position vs. ankle dorsiflexion showed a similar moderate effect size, suggesting a progressive increase in SN SWV as the ankle angle becomes greater (SMD [95%CI]: 0.44 [0.15, 0.74], I2: 0%; SMD [95%CI]: 0.56 [0.26, 0.85], I2: 0%). As expected, the greatest change in SWV was found comparing ankle plantar flexion vs. ankle dorsiflexion (SMD [95%CI]: 1.08 [0.72, 1.44], I2: 22%) (Figure 4).
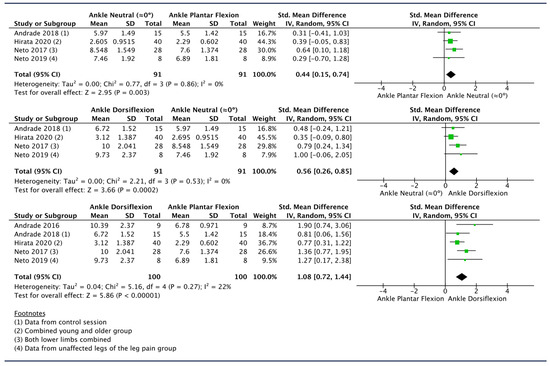
Figure 4.
Forest plots showing the impact of different ankle positions on sciatic nerve SWE values in the thigh [49,50,53,58,59].
Sensitivity analysis revealed that the largest modification of the effect size is obtained by removing the study by Hirata et al. [53] from the dorsiflexion vs. neutral and plantar flexion comparisons and the study by Neto et al. [50] from the plantar flexion vs. neutral comparison, which led to changes in the mean effect size by 30%, 17%, and 18%, respectively (Table 5).
However, the impact of ankle movement on SN stiffness may vary depending on knee position. As one study observed, at the 90° knee flexion position, ankle dorsiflexion seemed not to produce any change in SN SWV in the thigh [59].
3.6.2. Effect of Hip Movement
One study analyzed the impact of hip movement on SN stiffness at proximal and mid-thigh levels, showing that hip flexion led to a uniform average increase in SWV values by 54% from the starting position in hip extension (p < 0.0001) [54].
3.6.3. Effect of Knee Movement
SN SWV in response to progressive ankle dorsiflexion at 90° knee flexion and with full knee extension was investigated in one study [59]. According to the results of this study, SN SWV showed significantly greater values in knee extension vs. knee flexion regardless of the ankle angle (p values ranging from 0.001 to 0.002) [59].
3.7. Tibial Nerve
The studies analyzing the impact of different joint movements on TN SWE values are summarized in Table 8.

Table 8.
Tibial nerve stiffness in response to joint movement.
3.7.1. Effect of Ankle Movement
Two studies evaluated TN stiffness in response to isolated ankle movement in a 30° knee flexion position [52,56], while one study analyzed a combination of ankle dorsiflexion and knee extension [36]. Meta-analysis was performed with the data of the first two studies. Mean effect size showed a large increase in TN SWV with ankle dorsiflexion movement when compared to ankle resting position in plantar flexion (SMD [95%CI]: 1.52 [1.02, 2.02], I2: 0%) (Figure 5). A similar effect was observed when performing a combination of ankle dorsiflexion and knee extension (mean SWV ± SEM: 5.16 ± 0.21 m/s) from a starting position with 90° knee flexion and foot relaxed (mean SWV ± SEM: 3.25 ± 0.10 m/s) [36].
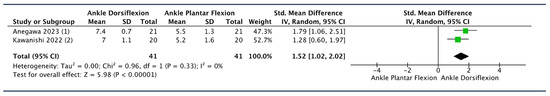
Figure 5.
Forest plot showing the impact of different ankle positions on tibial nerve SWE values in the lower leg [52,56].
3.7.2. Effect of Hip Movement
Two studies assessed the effect of hip flexion movement on TN SWV [36,54]. In both studies, the ankle was in a dorsiflexion position with the knee extended [36,54]. Pooled SMD revealed that hip flexion led to greater SWV values compared to hip extension in the distal portion of the TN (SMD [95%CI]: 2.14 [1.76, 2.51], I2: 0%) (Figure 6). Similar behavior was also observed in more proximal locations of the TN [54].
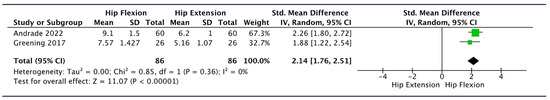
Figure 6.
Forest plots showing the impact of different hip positions on tibial nerve SWE values in the lower leg [36,54].
3.7.3. Effect of Knee Movement
The impact of knee movement on TN stiffness was reported in one study, which observed a 60% increase in TN SWV when performing knee extension in combination with ankle dorsiflexion starting from 90° knee flexion, with foot relaxed and hip neutral [36].
4. Discussion
The current systematic review and meta-analysis aimed to investigate the effects of joint movement on stiffness in healthy nerves. We hypothesized that nerve stiffness would significantly increase with movements and positions associated with more tensile load on neural structures. The results of this systematic review and meta-analysis support our initial hypothesis showing an overall tendency of stiffness increase following a pattern of neural tensioning. The effect of joint movement on nerve stiffness depends on the nerve segment, the amount of movement of the joint mobilized, and the position of other joints comprised in the entirety of the nerve length. These results are in line with previous systematic reviews that assessed nerve biomechanics [11,12].
The impact of neural-tensioning movement on nerve stiffness seems to be dependent on the amount of motion assumed by the joints involved. However, the relationship between joint angle and the increase in nerve stiffness may not always be completely linear through the entire range of motion. Some nerve segments show a gradual increase of stiffness as the joint is progressively moved [57,60], while others exhibit a different pattern, with an increase starting from a certain joint angle or that depends considerably on adjacent joint positioning [49,50,52,59,61].
Individual studies reported that a progressive increase in elbow flexion angles is associated with higher UN stiffness at the elbow [57,60]. In line with this, meta-analysis reveals significant effect sizes for higher degrees of elbow flexion when comparing 0° vs. 45°, 45° vs. 90°, and 90° vs. full flexion, suggesting that gradually increasing the elbow flexion angle could imply a further increase in UN stiffness (SMD [95%CI]: 1.32 [0.85, 1.80], I2: 0%; 1.40 [0.66, 2.14], I2: 50%; 0.90 [0.45, 1.36], I2: 0%). Surprisingly, in the analysis of elbow extension with other elbow flexion angles, the highest pooled SMD was found in the 0° vs. 90° comparison rather than in the 0° vs. full flexion comparison (SMD [95%CI]: 2.91 [1.88, 3.95], I2: 70%; SMD [95%CI]: 2.81 [0.10, 5.52], I2: 90%), as one could initially expect based on the previous findings. However, it must be considered that the width of the pooled 95% confidence interval for the SMD of the 0° vs. full flexion comparison may indicate imprecision of the estimated pooled effect size.
Wrist extension produced a significant increase in nerve stiffness in the distal segment of the MN [36,55,61,62,63] (Figure 2). Despite the presence of heterogeneity, all studies included in the analysis showed a large effect size in favor of wrist extension. Sensitivity analysis indicated that by removing the study by Zhu et al. [55], the pooled effect size reduced by 31%; nevertheless, this did not substantially change the clinical implication of the results obtained (Table 5). These findings are consistent with the increase in MN strain observed when performing similar joint movements in both cadaveric and in vivo studies [65,66]. Interestingly, the meta-analysis revealed a similar pooled effect size when comparing wrist extension to both neutral position (0°) and wrist flexion. This could indirectly suggest that the range from wrist flexion to neutral position does not seem to significantly affect nerve stiffness. Although a meta-analysis for a direct comparison was not performed due to insufficient data, the results from one study reporting a non-significant difference between these two wrist positions may support these assumptions [61]. In line with this, Silva et al. suggested that wrist movements from flexion to 0° induced less MN gliding than movements from 0° to wrist extension [11]. One possible explanation for this is that the range from wrist flexion to neutral position did not imply a sufficient level of mechanical stress to change MN stiffness, i.e., the nerve was unloaded [65]. However, care must be taken to interpret these suggestions, because wrist flexion vs. neutral was not directly meta-analyzed, and wrist flexion vs. extension was only reported in studies where participants’ elbows stayed in a flexed position (MN unloaded), and results may substantially differ if the same movements were performed in other limb positions implying more neural tension.
Regarding the SN, the meta-analysis revealed a progressive increase in stiffness at the thigh level with ankle dorsiflexion movement in a position of knee extension. Significant pooled SMD values were observed for ankle dorsiflexion and ankle neutral position (≈0°) when compared to ankle plantar flexion (SMD [95%CI]: 1.08 [0.72, 1.44], I2: 22%; SMD [95%CI]: 0.44 [0.15, 0.74], I2: 0%) as well as for ankle dorsiflexion compared to neutral position (SMD [95%CI]: 0.56 [0.26, 0.85], I2: 0%) (Figure 4). As expected, the ankle dorsiflexion vs. ankle plantar flexion comparison presented a larger effect size. These results seem to indicate a linear increase in SN stiffness related to the amount of ankle dorsiflexion movement. However, several included studies also reported non-significant changes in SN in the range from 40° ankle plantar flexion to 40% of maximum ankle dorsiflexion, being 50% of ankle dorsiflexion, the starting point from which the SN starts to build up more tension, while lower ankle dorsiflexion angles are likely to keep the nerve unloaded [49,50,59]. In the present meta-analysis, the extracted mean (± SD) SWE values for ankle neutral position were ≥50% of subjects’ maximum ankle dorsiflexion, consequently the first phase of ankle dorsiflexion movement, when the nerve is unloaded, was obviated in the analysis and thus not reported quantitatively in this review.
The TN showed a similar pattern, with nerve SWV increasing with ankle dorsiflexion (SMD [95%CI]: 1.52 [1.02, 2.02], I2: 0%) (Figure 5). However, similarly to the MN [61] and SN [49,50,59], the TN exhibited an initial phase of unloading during ankle movement. One study found that the TN SWV increase was only significant beyond a certain point of the plantar flexion-dorsiflexion range of motion (75% of maximum dorsiflexion), as the initial phase of the range of motion did not significantly affect nerve stiffness [52]. As the TN is located closer to the mobilized than the SN, the threshold from which the TN starts building tension (75%) may be expected in a smaller dorsiflexion angle position compared to the SN (50%). This may be due to the different limb positioning. The TN was measured with 30° knee flexion and 90° hip flexion [52], while the SN was measured with knee and hip extension [49,50,59]. The angle of knee and hip flexion may have supposed less tensile load on the TN than the angle of knee and hip extension did for the SN; therefore, if this is the case, more ankle dorsiflexion might be required to produce the same neural tension. A study on cadavers investigated the effect on TN strain of ankle dorsiflexion in different combinations of hip and knee positions and reported no significant differences in the final position when performing ankle dorsiflexion in a hip flexion-knee flexion position or a hip extension-knee extension position; however, the initial strain was different between the two positions, which may indicate that TN may experiment with a different pattern of tensile load depending on limb positioning (initial strain: −3.6% for hip flexion-knee flexion; −1.3% for hip extension-knee extension; expressed as % of change from the reference position) [67]. Regardless, further investigations are needed to fully understand cumulative nerve tensioning produced by the position of the joints that it crosses.
Limb positioning and its effect on neural tension and stiffness may also vary depending on the nerve segment considered.
MN seems to exhibit a greater increase in SWV in the proximal elbow (89.3%) than in the forearm (64.0%) during elbow extension [37], while wrist extension is more likely to produce a larger increase in SWV in the forearm (127%) than in the proximal elbow (40%) [36]. A similar pattern of change was observed for the UN, with a 91.1% increase in SWV at the proximal elbow and a 37.4% increase at the forearm when the elbow was flexed [37]. These findings for the MN and UN may indicate that changing the position of the limb could lead to changes in stiffness that vary along the nerve path. The large difference in stiffness increase between the forearm and the upper arm in these positions could reflect more tension in the nerve segment closer to the moving joint.
On the other hand, one study reported the effect of hip flexion on different portions of the sciatic/tibial nerve and observed a homogeneous average 54% increase in SWV along the SN and TN [54]. However, it must be considered that in this study, SN and TN were not fully unloaded due to the knee extension and ankle (0°) angles, so a partial pre-tensioned status of the nerve could have influenced its pattern of stiffness modification during hip flexion. In line with this, a previous cadaveric study reported a greater increase in TN strain at the ankle during the first phase of the straight leg raise test, when the first movement was ankle dorsiflexion compared to hip flexion [68].
The main strength of this systematic review lies in its synthesis of in vivo nerve biomechanics from both qualitative and quantitative perspectives. The direction of the effect is consistent among the included studies, showing an increase in nerve stiffness in response to tension-increasing movements. The exclusive inclusion of studies that used SWE, which is considered less operator-dependent than other types of elastographies such as strain elastography [30], may have contributed to the consistency of the observed effect and represent another point of strength.
Beside this, several limitations need to be considered. First, the limited number of studies included in the meta-analyses did not allow a proper investigation of moderator variables such as age, the position of adjacent joints, the ultrasound system used, or the transducer position; thus, the heterogeneity reported for various comparisons could not be fully explained. Despite the presence of heterogeneity for some comparisons, sensitivity analysis indicated robustness of the results, showing that no individual study had a significant impact on the entire analysis or produced substantial changes that might affect the clinical interpretation of the results. Furthermore, the methodological quality of the included studies was assessed with a modified version of the Downs and Black checklist. Although this scale was adopted in previous similar reviews [11,12], its clinometric properties have not yet been studied. Nevertheless, it was adopted because other quality assessment tools seem to be less adequate than this modified checklist.
Another relevant aspect to take into account is that under mechanical tension, nerve SWV exhibits higher values, which is assumed to imply an increase in its stiffness [29]. However, the actual amount of neural tension cannot be non-invasively quantified nor isolated from the effects of other forces acting upon the nerve, and thus resultant nerve stiffness may also be influenced by interactions of the nerve with its surrounding tissues. Lastly, this systematic review focused exclusively on describing and analyzing healthy nerve behavior. Nerves under pathological conditions may present different mechanical properties in response to joint movement [57,61]; therefore, our findings must be interpreted in this context and cannot be generalized to pathological nerves. Future systematic reviews may investigate how different types of movements may affect nerve stiffness in different pathologies.
5. Conclusions
Peripheral nerves are exposed to different mechanical loads during limb movements, and their mechanical response to tensile stress is variable. Shear-wave elastography may represent a useful tool for the evaluation of in vivo neural response to movement and to define how different patterns impact nerve mechanical properties. Taking this into account, the present systematic review and meta-analysis aimed to investigate the effects of joint movement on nerve stiffness.
Our findings suggest an overall tendency for stiffness increase following a pattern of neural tensioning, where greater stiffness values were observed for movement and positions associated with more tensile load on neural structures. The effect of joint movement on nerve stiffness is complex and depends on the nerve segment, the amount of movement of the joint mobilized, and the position of other joints comprised in the entirety of the nerve length. However, due to the limited number of studies, many aspects of the nerve behavior, such as the cumulative effect produced by the position of many joints, together with the effect of using different ultrasound equipment and transducers for nerve stiffness evaluation, still need to be fully investigated.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/diagnostics14030343/s1, File S1: PRISMA 2020 Checklist. File S2: The search strategy.
Author Contributions
Conceptualization, G.C.; methodology, G.C., I.A.-C. and E.E.-d.-M.; formal analysis, G.C., I.A.-C. and E.E.-d.-M.; investigation, G.C. and J.P.-R.; resources, J.P.-R., A.M.-C. and P.P.-A.; data curation, G.C. and A.M.-C.; writing—original draft preparation, G.C., E.E.-d.-M., M.M.-U. and J.P.-R.; writing—review and editing, A.M.-C., I.A.-C., M.M.-U. and P.P.-A.; supervision, E.B.-G. and E.E.-d.-M.; project administration G.C., E.B.-G. and E.E.-d.-M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Bono, C.M.; Ghiselli, G.; Gilbert, T.J.; Kreiner, D.S.; Reitman, C.; Summers, J.T.; Baisden, J.L.; Easa, J.; Fernand, R.; Lamer, T.; et al. An Evidence-Based Clinical Guideline for the Diagnosis and Treatment of Cervical Radiculopathy from Degenerative Disorders. Spine J. 2011, 11, 64–72. [Google Scholar] [CrossRef]
- American Association of Electrodiagnostic Medicine. Guidelines in Electrodiagnostic Medicine. Muscle Nerve 1992, 15, 229–253. [Google Scholar] [CrossRef] [PubMed]
- Koulidis, K.; Veremis, Y.; Anderson, C.; Heneghan, N.R. Diagnostic Accuracy of Upper Limb Neurodynamic Tests for the Assessment of Peripheral Neuropathic Pain: A Systematic Review. Musculoskelet. Sci. Pract. 2019, 40, 21–33. [Google Scholar] [CrossRef] [PubMed]
- Veves, A.; Backonja, M.; Malik, R.A. Painful Diabetic Neuropathy: Epidemiology, Natural History, Early Diagnosis, and Treatment Options. Pain Med. 2008, 9, 660–674. [Google Scholar] [CrossRef] [PubMed]
- Erickson, M.; Lawrence, M.; Jansen, C.W.S.; Coker, D.; Amadio, P.; Cleary, C. Hand Pain and Sensory Deficits: Carpal Tunnel Syndrome. J. Orthop. Sports Phys. Ther. 2019, 49, CPG1–CPG85. [Google Scholar] [CrossRef] [PubMed]
- Nee, R.J.; Coppieters, M.W.; Boyd, B.S. Reliability of the Straight Leg Raise Test for Suspected Lumbar Radicular Pain: A Systematic Review with Meta-Analysis. Musculoskelet. Sci. Pract. 2022, 59, 102529. [Google Scholar] [CrossRef] [PubMed]
- Haj-Mirzaian, A.; Hafezi-Nejad, N.; del Grande, F.; Endo, Y.; Nwawka, O.K.; Miller, T.T.; Carrino, J.A. Optimal Choice of Ultrasound-Based Measurements for the Diagnosis of Ulnar Neuropathy at the Elbow: A Meta-Analysis of 1961 Examinations. Am. J. Roentgenol. 2020, 215, 1171–1183. [Google Scholar] [CrossRef] [PubMed]
- Torres-Costoso, A.; Martínez-Vizcaíno, V.; Álvarez-Bueno, C.; Ferri-Morales, A.; Cavero-Redondo, I. Accuracy of Ultrasonography for the Diagnosis of Carpal Tunnel Syndrome: A Systematic Review and Meta-Analysis. Arch. Phys. Med. Rehabil. 2018, 99, 758–765.e10. [Google Scholar] [CrossRef] [PubMed]
- Roomizadeh, P.; Eftekharsadat, B.; Abedini, A.; Ranjbar-Kiyakalayeh, S.; Yousefi, N.; Ebadi, S.; Babaei-Ghazani, A. Ultrasonographic Assessment of Carpal Tunnel Syndrome Severity: A Systematic Review and Meta-Analysis. Am. J. Phys. Med. Rehabil. 2019, 98, 373–381. [Google Scholar] [CrossRef]
- Fowler, J.R.; Gaughan, J.P.; Ilyas, A.M. The Sensitivity and Specificity of Ultrasound for the Diagnosis of Carpal Tunnel Syndrome: A Meta-Analysis. Clin. Orthop. Relat. Res. 2011, 469, 1089–1094. [Google Scholar] [CrossRef]
- Silva, A.; Manso, A.; Andrade, R.; Domingues, V.; Brandão, M.P.; Silva, A.G. Quantitative in Vivo Longitudinal Nerve Excursion and Strain in Response to Joint Movement: A Systematic Literature Review. Clin. Biomech. 2014, 29, 839–847. [Google Scholar] [CrossRef]
- Szikszay, T.; Hall, T.; Von Piekartz, H. In Vivo Effects of Limb Movement on Nerve Stretch, Strain, and Tension: A Systematic Review. J. Back Musculoskelet. Rehabil. 2017, 30, 1171–1186. [Google Scholar] [CrossRef]
- Taljanovic, M.S.; Gimber, L.H.; Becker, G.W.; Latt, L.D.; Klauser, A.S.; Melville, D.M.; Gao, L.; Witte, R.S. Shear-Wave Elastography: Basic Physics and Musculoskeletal Applications. Radiographics 2017, 37, 855–870. [Google Scholar] [CrossRef]
- Nightingale, K. Acoustic Radiation Force Impulse (ARFI) Imaging: A Review. Curr. Med. Imaging Rev. 2011, 7, 328–339. [Google Scholar] [CrossRef]
- Blank, J.; Blomquist, M.; Arant, L.; Cone, S.; Roth, J. Characterizing Musculoskeletal Tissue Mechanics Based on Shear Wave Propagation: A Systematic Review of Current Methods and Reported Measurements. Ann. Biomed. Eng. 2022, 50, 751–768. [Google Scholar] [CrossRef]
- Cipriano, K.J.; Wickstrom, J.; Glicksman, M.; Hirth, L.; Farrell, M.; Livinski, A.A.; Esfahani, S.A.; Maldonado, R.J.; Astrow, J.; Berrigan, W.A.; et al. A Scoping Review of Methods Used in Musculoskeletal Soft Tissue and Nerve Shear Wave Elastography Studies. Clin. Neurophysiol. 2022, 140, 181–195. [Google Scholar] [CrossRef]
- Eby, S.F.; Song, P.; Chen, S.; Chen, Q.; Greenleaf, J.F.; An, K.N. Validation of Shear Wave Elastography in Skeletal Muscle. J. Biomech. 2013, 46, 2381–2387. [Google Scholar] [CrossRef]
- Sebag, F.; Vaillant-Lombard, J.; Berbis, J.; Griset, V.; Henry, J.F.; Petit, P.; Oliver, C. Shear Wave Elastography: A New Ultrasound Imaging Mode for the Differential Diagnosis of Benign and Malignant Thyroid Nodules. J. Clin. Endocrinol. Metab. 2010, 95, 5281–5288. [Google Scholar] [CrossRef] [PubMed]
- Ashir, A.; Jerban, S.; Barrère, V.; Wu, Y.; Shah, S.B.; Andre, M.P.; Chang, E.Y. Skeletal Muscle Assessment Using Quantitative Ultrasound: A Narrative Review. Sensors 2023, 23, 4763. [Google Scholar] [CrossRef] [PubMed]
- Bercoff, J.; Tanter, M.; Fink, M. Supersonic Shear Imaging: A New Technique for Soft Tissue Elasticity Mapping. IEEE Trans. Ultrason. Ferroelectr. Freq. Control 2004, 51, 396–409. [Google Scholar] [CrossRef] [PubMed]
- Youk, J.H.; Son, E.J.; Park, A.Y.; Kim, J.-A. Shear-Wave Elastography for Breast Masses: Local Shear Wave Speed (m/s) versus Young Modulus (KPa). Ultrasonography 2013, 33, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Deffieux, T.; Gennisson, J.L.; Bousquet, L.; Corouge, M.; Cosconea, S.; Amroun, D.; Tripon, S.; Terris, B.; Mallet, V.; Sogni, P.; et al. Investigating Liver Stiffness and Viscosity for Fibrosis, Steatosis and Activity Staging Using Shear Wave Elastography. J. Hepatol. 2015, 62, 317–324. [Google Scholar] [CrossRef] [PubMed]
- Zakrzewski, J.; Zakrzewska, K.; Pluta, K.; Nowak, O.; Miłoszewska-Paluch, A. Ultrasound Elastography in the Evaluation of Peripheral Neuropathies: A Systematic Review of the Literature. Pol. J. Radiol. 2019, 84, 581–591. [Google Scholar] [CrossRef] [PubMed]
- Dong, B.; Lyu, G.; Yang, X.; Wang, H.; Chen, Y. Shear Wave Elastography as a Quantitative Biomarker of Diabetic Peripheral Neuropathy: A Systematic Review and Meta-Analysis. Front. Public Health 2022, 10, 915883. [Google Scholar] [CrossRef] [PubMed]
- Wee, T.C.; Simon, N.G. Ultrasound Elastography for the Evaluation of Peripheral Nerves: A Systematic Review. Muscle Nerve 2019, 60, 501–512. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.P.; Chen, I.J.; Chang, K.V.; Wu, W.T.; Özçakar, L. Utility of Ultrasound Elastography in Evaluation of Carpal Tunnel Syndrome: A Systematic Review and Meta-Analysis. Ultrasound Med. Biol. 2019, 45, 2855–2865. [Google Scholar] [CrossRef] [PubMed]
- Dąbrowska-Thing, A.; Zakrzewski, J.; Nowak, O.; Nitek, Ż. Ultrasound Elastography as a Potential Method to Evaluate Entrapment Neuropathies in Elite Athletes: A Mini-Review. Pol. J. Radiol. 2019, 84, e625–e629. [Google Scholar] [CrossRef]
- Rossetto, G.; Lopomo, N.F.; Shaikh, S.Z. Longitudinal Movements and Stiffness of Lower Extremity Nerves Measured by Ultrasonography and Ultrasound Elastography in Symptomatic and Asymptomatic Populations: A Systematic Review with Meta-Analysis. Ultrasound Med. Biol. 2023, 49, 1913–1929. [Google Scholar] [CrossRef]
- Schrier, V.J.M.M.; Lin, J.; Gregory, A.; Thoreson, A.R.; Alizad, A.; Amadio, P.C.; Fatemi, M. Shear Wave Elastography of the Median Nerve: A Mechanical Study. Muscle Nerve 2020, 61, 826–833. [Google Scholar] [CrossRef]
- Prado-Costa, R.; Rebelo, J.; Monteiro-Barroso, J.; Preto, A.S. Ultrasound Elastography: Compression Elastography and Shear-Wave Elastography in the Assessment of Tendon Injury. Insights Imaging 2018, 9, 791–814. [Google Scholar] [CrossRef]
- Creze, M.; Nordez, A.; Soubeyrand, M.; Rocher, L.; Maître, X.; Bellin, M.F. Shear Wave Sonoelastography of Skeletal Muscle: Basic Principles, Biomechanical Concepts, Clinical Applications, and Future Perspectives. Skelet. Radiol. 2018, 47, 457–471. [Google Scholar] [CrossRef]
- Wang, C.; Wang, H.; Zhou, Y.; Zhang, S.; Huang, M. Evaluation of the Clinical Value of Shear Wave Elastography for Early Detection and Diagnosis of Diabetic Peripheral Neuropathy: A Controlled Preliminary Prospective Clinical Study. BMC Musculoskelet. Disord. 2022, 23, 1120. [Google Scholar] [CrossRef]
- Chen, R.; Wang, X.L.; Xue, W.L.; Sun, J.W.; Dong, X.Y.; Jiang, Z.P.; Wu, H.; Ma, R.; Zhou, X.L. Application Value of Conventional Ultrasound and Real-Time Shear Wave Elastography in Patients with Type 2 Diabetic Polyneuropathy. Eur. J. Radiol. 2020, 126, 108965. [Google Scholar] [CrossRef]
- Chen, S.P.; Ye, T.T.; Hong, J.; Zhu, H. Evaluation of Sciatic Nerve Stiffness Using Shear Wave Elastography in Patients with Unilateral Diabetic Foot Ulcers. Diagnostics 2023, 13, 547. [Google Scholar] [CrossRef]
- Ruby, L.; Mutschler, T.; Martini, K.; Klingmüller, V.; Frauenfelder, T.; Rominger, M.B.; Sanabria, S.J. Which Confounders Have the Largest Impact in Shear Wave Elastography of Muscle and How Can They Be Minimized? An Elasticity Phantom, Ex Vivo Porcine Muscle and Volunteer Study Using a Commercially Available System. Ultrasound Med. Biol. 2019, 45, 2591–2611. [Google Scholar] [CrossRef] [PubMed]
- Greening, J.; Dilley, A. Posture-Induced Changes in Peripheral Nerve Stiffness Measured by Ultrasound Shear-Wave Elastography. Muscle Nerve 2017, 55, 213–222. [Google Scholar] [CrossRef] [PubMed]
- Rugel, C.L.; Franz, C.K.; Lee, S.S.M. Influence of Limb Position on Assessment of Nerve Mechanical Properties by Using Shear Wave Ultrasound Elastography. Muscle Nerve 2020, 61, 616–622. [Google Scholar] [CrossRef]
- Ellis, R.; Blyth, R.; Arnold, N.; Miner-Williams, W. Is There a Relationship between Impaired Median Nerve Excursion and Carpal Tunnel Syndrome? A Systematic Review. J. Hand Ther. 2017, 30, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Boyd, B.S.; Dilley, A. Altered Tibial Nerve Biomechanics in Patients with Diabetes Mellitus. Muscle Nerve 2014, 50, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Hug, F.; Tucker, K.; Gennisson, J.L.; Tanter, M.; Nordez, A. Elastography for Muscle Biomechanics: Toward the Estimation of Individual Muscle Force. Exerc. Sport Sci. Rev. 2015, 43, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Drevon, D.; Fursa, S.R.; Malcolm, A.L. Intercoder Reliability and Validity of WebPlotDigitizer in Extracting Graphed Data. Behav. Modif. 2017, 41, 323–339. [Google Scholar] [CrossRef]
- Downs, S.H.; Black, N. The Feasibility of Creating a Checklist for the Assessment of the Methodological Quality Both of Randomised and Non-Randomised Studies of Health Care Interventions. J. Epidemiol. Community Health 1998, 52, 377–384. [Google Scholar] [CrossRef]
- Fernando, M.; Crowther, R.; Lazzarini, P.; Sangla, K.; Cunningham, M.; Buttner, P.; Golledge, J. Biomechanical Characteristics of Peripheral Diabetic Neuropathy: A Systematic Review and Meta-Analysis of Findings from the Gait Cycle, Muscle Activity and Dynamic Barefoot Plantar Pressure. Clin. Biomech. 2013, 28, 831–845. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions; Version 6.3 (Updated February 2022); Wiley: Hoboken, NJ, USA, 2022. [Google Scholar]
- Luo, D.; Wan, X.; Liu, J.; Tong, T. Optimally Estimating the Sample Mean from the Sample Size, Median, Mid-Range, and/or Mid-Quartile Range. Stat. Methods Med. Res. 2018, 27, 1785–1805. [Google Scholar] [CrossRef]
- Shi, J.; Luo, D.; Weng, H.; Zeng, X.T.; Lin, L.; Chu, H.; Tong, T. Optimally Estimating the Sample Standard Deviation from the Five-Number Summary. Res. Synth. Methods 2020, 11, 641–654. [Google Scholar] [CrossRef]
- Shi, J.; Luo, D.; Wan, X.; Liu, Y.; Liu, J.; Bian, Z.; Tong, T. Detecting the Skewness of Data from the Five-Number Summary and Its Application in Meta-Analysis. Stat. Methods Med. Res. 2023, 32, 09622802231172043. [Google Scholar] [CrossRef] [PubMed]
- Neto, T.; Freitas, S.R.; Andrade, R.J.; Vaz, J.R.; Mendes, B.; Firmino, T.; Bruno, P.M.; Nordez, A.; Oliveira, R. Noninvasive Measurement of Sciatic Nerve Stiffness in Patients with Chronic Low Back Related Leg Pain Using Shear Wave Elastography. J. Ultrasound Med. 2019, 38, 157–164. [Google Scholar] [CrossRef]
- Neto, T.; Freitas, S.R.; Andrade, R.J.; Gomes, J.; Vaz, J.; Mendes, B.; Firmino, T.; Nordez, A.; Oliveira, R. Sciatic Nerve Stiffness Is Not Changed immediately after a Slump Neurodynamics Technique. Muscles Ligaments Tendons J. 2017, 7, 583–589. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Sutton, A.J.; Ioannidis, J.P.A.; Terrin, N.; Jones, D.R.; Lau, J.; Carpenter, J.; Rücker, G.; Harbord, R.M.; Schmid, C.H.; et al. Recommendations for Examining and Interpreting Funnel Plot Asymmetry in Meta-Analyses of Randomised Controlled Trials. BMJ Online 2011, 343, d4002. [Google Scholar] [CrossRef] [PubMed]
- Kawanishi, K.; Nariyama, Y.; Anegawa, K.; Tsutsumi, M.; Kudo, S. Changes in Tibial Nerve Stiffness during Ankle Dorsiflexion According to In-Vivo Analysis with Shear Wave Elastography. Medicine 2022, 101, e29840. [Google Scholar] [CrossRef]
- Hirata, K.; Yamadera, R.; Akagi, R. Associations between Range of Motion and Tissue Stiffness in Young and Older People. Med. Sci. Sports Exerc. 2020, 52, 2179–2188. [Google Scholar] [CrossRef]
- Andrade, R.J.; Freitas, S.R.; Hug, F.; Coppieters, M.W.; Sierra-Silvestre, E.; Nordez, A. Spatial Variation in Mechanical Properties along the Sciatic and Tibial Nerves: An Ultrasound Shear Wave Elastography Study. J. Biomech. 2022, 136, 111075. [Google Scholar] [CrossRef]
- Zhu, B.; Yan, F.; He, Y.; Wang, L.; Xiang, X.; Tang, Y.; Yang, Y.; Qiu, L. Evaluation of the Healthy Median Nerve Elasticity: Feasibility and Reliability of Shear Wave Elastography. Medicine 2018, 97, e12956. [Google Scholar] [CrossRef]
- Anegawa, K.; Kawanishi, K.; Nakamura, M.; Izumi, M.; Tsutsumi, M.; Kudo, S. Tibial Nerve Dynamics during Ankle Dorsiflexion: The Relationship between Stiffness and Excursion of the Tibial Nerve. J. Biomech. 2023, 155, 111646. [Google Scholar] [CrossRef]
- Wolny, T.; Fernández-de-las-Peñas, C.; Granek, A.; Linek, P. Changes in Ultrasound Measurements of the Ulnar Nerve at Different Elbow Joint Positions in Patients with Cubital Tunnel Syndrome. Sensors 2022, 22, 8354. [Google Scholar] [CrossRef]
- Andrade, R.J.; Freitas, S.R.; Hug, F.; Le Sant, G.; Lacourpaille, L.; Gross, R.; McNair, P.; Nordez, A. The Potential Role of Sciatic Nerve Stiffness in the Limitation of Maximal Ankle Range of Motion. Sci. Rep. 2018, 8, 14532. [Google Scholar] [CrossRef]
- Andrade, R.J.; Nordez, A.; Hug, F.; Ates, F.; Coppieters, M.W.; Pezarat-Correia, P.; Freitas, S.R. Non-Invasive Assessment of Sciatic Nerve Stiffness during Human Ankle Motion Using Ultrasound Shear Wave Elastography. J. Biomech. 2016, 49, 326–331. [Google Scholar] [CrossRef] [PubMed]
- Durand, S.; Raffoul, W.; Christen, T.; Pedrazzi, N. Post-Operative Assessment of Ulnar Nerve Tension Using Shear-Wave Elastography. Neurol. Int. 2021, 13, 469–476. [Google Scholar] [CrossRef] [PubMed]
- Staber, D.; Oppold, J.; Grimm, A.; Schuhmann, M.U.; Romano, A.; Marquetand, J.; Kleiser, B. Shear-Wave-Elastography in Neurofibromatosis Type I. Diagnostics 2022, 12, 360. [Google Scholar] [CrossRef] [PubMed]
- Lin, M.; Chen, Y.; Deng, W.; Liang, H.; Yu, S.; Zhang, Z.; Liu, C. Quantifying the Elasticity Properties of the Median Nerve during the Upper Limb Neurodynamic Test 1. Appl. Bionics Biomech. 2022, 2022, 3300835. [Google Scholar] [CrossRef]
- Lee, S.; Kwak, J.; Lee, S.; Cho, H.; Oh, E.; Park, J.W. Quantitative Stiffness of the Median Nerve, Flexor Tendons, and Flexor Retinaculum in the Carpal Tunnel Measured with Acoustic Radiation Force Impulse Elastography in Various Wrist and Finger Positions. Medicine 2019, 98, e17066. [Google Scholar] [CrossRef]
- Andrade, R.J.; Freitas, S.R.; Hug, X.F.; Sant, G.L.; Lacourpaille, L.; Gross, R.; Quillard, J.-B.; Mcnair, P.J.; Nordez, A. Chronic Effects of Muscle and Nerve-Directed Stretching on Tissue Mechanics. J. Appl. Physiol. 2020, 129, 1011–1023. [Google Scholar] [CrossRef]
- Dilley, A.; Lynn, B.; Greening, J.; DeLeon, N. Quantitative in Vivo Studies of Median Nerve Sliding in Response to Wrist, Elbow, Shoulder and Neck Movements. Clin. Biomech. 2003, 18, 899–907. [Google Scholar] [CrossRef] [PubMed]
- Topp, K.S.; Boyd, B.S. Structure and Biomechanics of Peripheral Nerves: Nerve Responses to Physical Stresses and Implications for Physical Therapist Practice Perspective. Phys. Ther. 2006, 86, 92–109. [Google Scholar] [CrossRef] [PubMed]
- Alshami, A.M.; Babri, A.S.; Souvlis, T.; Coppieters, M.W. Strain in the Tibial and Plantar Nerves with Foot and Ankle Movements and the Influence of Adjacent Joint Positions. J. Appl. Biomech. 2008, 24, 368–376. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Boyd, B.S.; Topp, K.S.; Coppieters, M.W. Impact of Movement Sequencing on Sciatic and Tibial Nerve Strain and Excursion during the Straight Leg Raise Test in Embalmed Cadavers. J. Orthop. Sports Phys. Ther. 2013, 43, 398–403. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).