Abstract
Appendiceal mucinous tumors are rare, with variable malignant potential, and they are usually found incidentally. Clinical symptoms are nonspecific. Rarely, appendiceal mucinous neoplasm causes bowel obstruction and makes diagnosis more difficult. We present a case of an 84-year-old female who came to our emergency department having had abdominal fullness and constipation for 5 days. Ileus, due to an affected adhesion band, was diagnosed initially, and symptoms improved gradually under conservative treatment. However, 3 months later she presented to the emergency department again with abdominal pain and distension; small bowel obstruction due to adhesion was again diagnosed. Recurrent bowel obstruction prompted emergent surgery. Operative findings showed a whitish appendiceal tumor adhering to and directly invading the adjacent ileum, with a segment of herniated small bowel wedged in between, causing the obstruction. Upon reviewing the initial computed tomography scan, the dilated tubular structure of appendiceal tumor was misrecognized as small bowel loop; there was no surrounding inflammatory sign, leading to diagnosis difficulty. Instead of a common cause of bowel obstruction, such as adhesion band, this case revealed bowel obstruction can be caused by the direct invasion of an appendiceal tumor. Awareness of this condition with careful image evaluation of small bowel obstruction is essential for diagnosis.
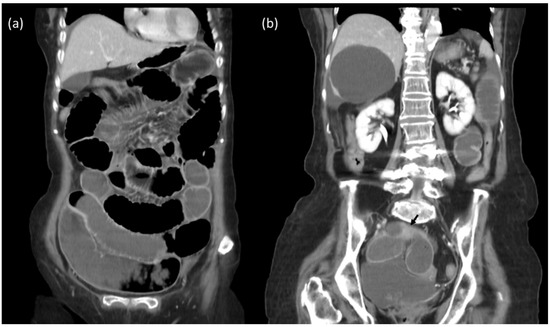
Figure 1.
The 84-year-old female presented to emergency department having had abdominal fullness and constipation for 5 days. Initial KUB radiograph shows distended small bowels. Contrast-enhanced computed tomography of abdomen–pelvis: (a,b) Distended small bowel loops, with transition zone at ileum (black arrow). Mechanical obstruction due to adhesion was diagnosed.
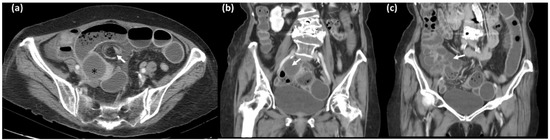
Figure 2.
Three months later she presented to the emergency department again with abdominal pain and distension, they repeated the contrast-enhanced computed tomography of abdomen–pelvis: (a) Dilated small bowel loops, with whirl sign (arrow), which may indicate bowel volvulus or closed loop obstruction. A cystic structure adjacent to transition zone was found (*) suspected to be the enlarged appendix. (arrows in coronal image (b,c)) [1,2].
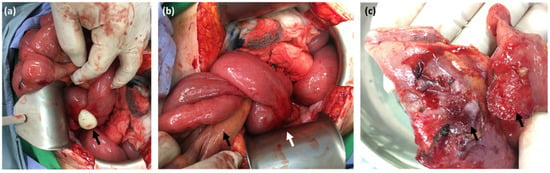
Figure 3.
Operative findings: (a) Appendiceal mucocele (arrow). (b) Tumor caused small bowel adhesion (white arrow) and internal herniation (black arrow). (c) Tumor capsule adhered to serosa of ileum (arrows). Bowel obstruction caused by appendiceal tumor was rarely reported [3,4,5,6,7].
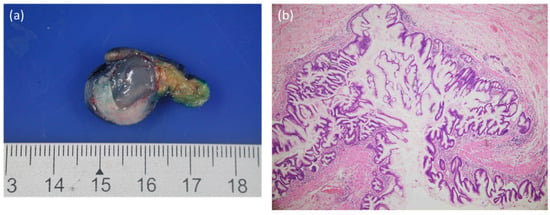
Figure 4.
The microscopic examination of appendiceal tumor revealed low-grade appendiceal mucinous neoplasm, which was adherent to the adjacent small bowel. (a) Low-grade appendiceal neoplasm with a dilated lumen filled with mucus. (b) Low-grade mucinous appendiceal neoplasm lined by filiform mucinous epithelium. The mucinous epithelium displayed no obvious nuclear pleomorphism [8,9].
Author Contributions
Conceptualization, W.-T.L., W.T.L.; data curation, W.-T.L., Y.-H.W., W.-Y.C., W.T.L.; writing—original draft preparation, W.-T.L.; writing—review and editing, W.T.L.; supervision, W.T.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This retrospective study was approved by the Joint Institutional Review Board of Taipei Medical University (TMU-JIRB) (Approval No. N202205050; Approved date: 20 May, 2022). The study was conducted according to the guidelines of the Declaration of Helsinki.
Informed Consent Statement
Written informed consent was waived due to the retrospective nature of this work.
Data Availability Statement
All data are available within the article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Leonards, L.M.; Pahwa, A.; Patel, M.K.; Petersen, J.; Nguyen, M.J.; Jude, C.M. Neoplasms of the Appendix: Pictorial Review with Clinical and Pathologic Correlation. Radiographics 2017, 37, 1059–1083. [Google Scholar] [CrossRef] [PubMed]
- Karande, G.Y.; Chua, W.M.; Yiin, R.S.Z.; Wong, K.M.; Hedgire, S.; Tan, J.T. Spectrum of computed tomography manifestations of appendiceal neoplasms: Acute appendicitis and beyond. Singap. Med. J. 2019, 60, 173–182. [Google Scholar] [CrossRef]
- Kawai, K.; Murata, K.; Kagawa, Y.; Naito, A.; Takase, K.; Mori, R.; Nose, Y.; Sakamoto, T.; Murakami, K.; Katsura, Y.; et al. A Case of Strangulating Intestinal Obstruction Caused by Coiling of Low-Grade Appendiceal Mucinous Neoplasm to Terminal Ileum. Gan Kagaku Ryoho 2019, 46, 291–293. [Google Scholar]
- Komo, T.; Kohashi, T.; Hihara, J.; Oishi, K.; Yoshimitsu, M.; Kanou, M.; Nakashima, A.; Aoki, Y.; Miguchi, M.; Kaneko, M.; et al. Intestinal obstruction caused by low-grade appendiceal mucinous neoplasm: A case report and review of the literature. Int. J. Surg. Case Rep. 2018, 51, 37–40. [Google Scholar] [CrossRef] [PubMed]
- Takei, R.; Kanamoto, K.; Tamaru, Y.; Nojima, K.; Mitta, K.; Zaimoku, R.; Kanamoto, A.; Terakawa, H.; Higashi, Y.; Tsukioka, Y.; et al. A Case of Strangulation Ileus Due to a Low-Grade Appendiceal Mucinous Neoplasm. Am. J. Case Rep. 2020, 21, e922405. [Google Scholar] [CrossRef] [PubMed]
- Houlzé-Laroye, C.; Eveno, C. Low-grade appendiceal mucinous neoplasms with bowel obstruction. Pleura Peritoneum 2019, 4, e20190020. [Google Scholar] [CrossRef] [PubMed]
- Nakamatsu, D.; Nishida, T.; Yamamoto, M.; Matsubara, T.; Hayashi, S. Colon intussusceptions caused by a low-grade appendiceal mucinous neoplasm. Indian J. Gastroenterol. 2018, 37, 475–476. [Google Scholar] [CrossRef] [PubMed]
- Shaib, W.L.; Assi, R.; Shamseddine, A.; Alese, O.B.; Staley, C., 3rd; Memis, B.; Adsay, V.; Bekaii-Saab, T.; El-Rayes, B.F. Appendiceal Mucinous Neoplasms: Diagnosis and Management. Oncologist 2017, 22, 1107–1116. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Zhou, J.; Dong, M.; Yang, L. Management and prognosis of low-grade appendiceal mucinous neoplasms: A clinicopathologic analysis of 50 cases. Eur. J. Surg. Oncol. 2018, 44, 1640–1645. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).