Machine Learning Models Predicting Cardiovascular and Renal Outcomes and Mortality in Patients with Hyperkalemia
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Patient Selection, and Data Handling
2.2. Risk Factors and Outcomes
2.3. Machine Learning Algorithms
2.4. Selection of Clinical Variables
2.5. Validation
3. Results
3.1. Patient Selection and Characteristics
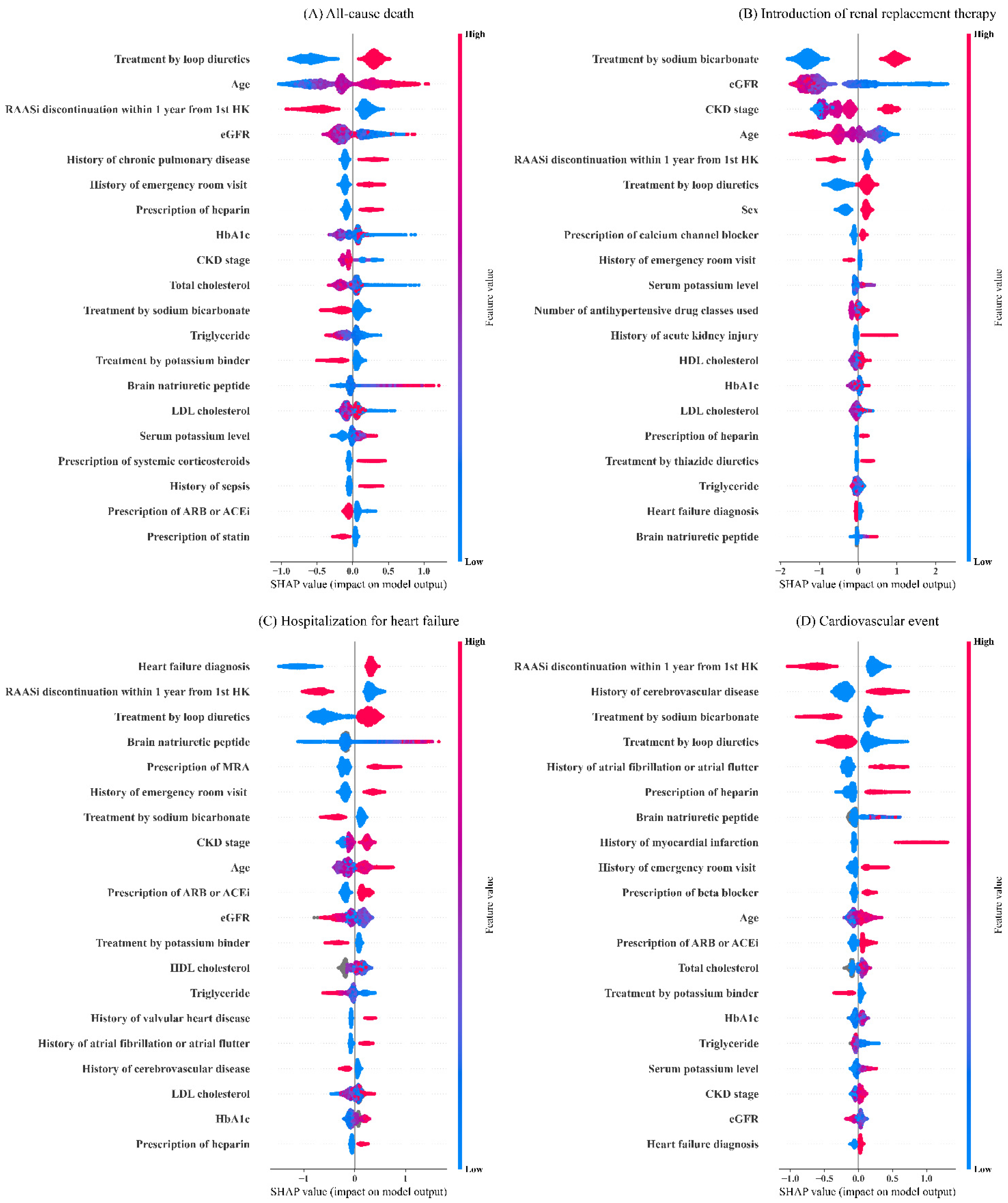
3.2. Model Derivation and Internal Validation
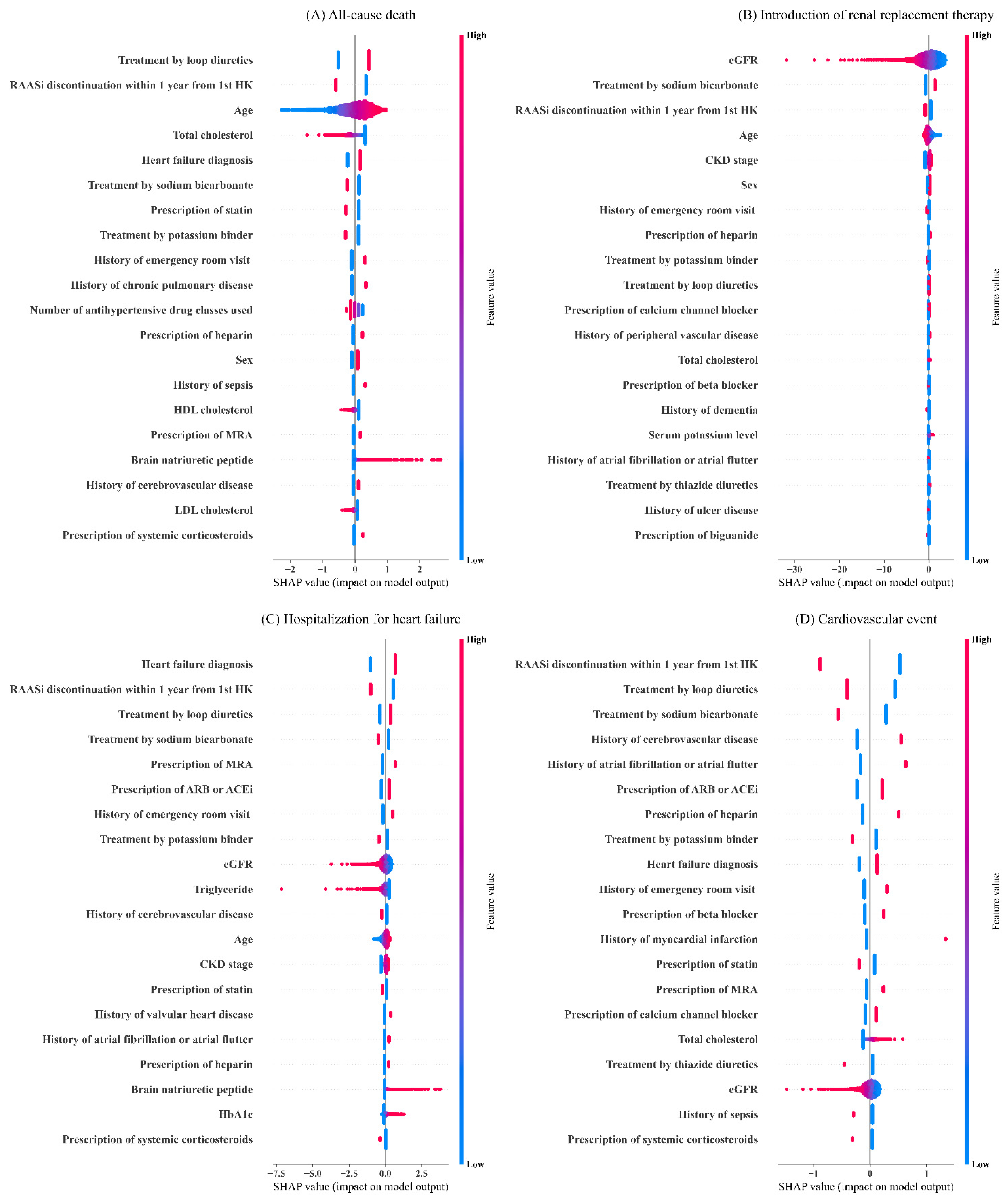
3.3. External Validation
4. Discussion
5. Strengths and Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gumz, M.L.; Rabinowitz, L.; Wingo, C.S. An Integrated View of Potassium Homeostasis. N. Engl. J. Med. 2015, 373, 60–72. [Google Scholar] [CrossRef] [PubMed]
- Palmer, B.F. Regulation of Potassium Homeostasis. Clin. J. Am. Soc. Nephrol. 2015, 10, 1050–1060. [Google Scholar] [CrossRef] [PubMed]
- Chaitman, M.; Dixit, D.; Bridgeman, M.B. Potassium-Binding Agents for the Clinical Management of Hyperkalemia. Pharm. Ther. 2016, 41, 43–50. [Google Scholar]
- Khanagavi, J.; Gupta, T.; Aronow, W.S.; Shah, T.; Garg, J.; Ahn, C.; Sule, S.; Peterson, S. Hyperkalemia among hospitalized patients and association between duration of hyperkalemia and outcomes. Arch. Med. Sci. 2014, 10, 251–257. [Google Scholar] [CrossRef]
- Palmer, B.F. Managing hyperkalemia caused by inhibitors of the renin-angiotensin-aldosterone system. N. Engl. J. Med. 2004, 351, 585–592. [Google Scholar] [CrossRef]
- Kovesdy, C.P. Updates in hyperkalemia: Outcomes and therapeutic strategies. Rev. Endocr Metab. Disord 2017, 18, 41–47. [Google Scholar] [CrossRef]
- Kovesdy, C.P. Management of hyperkalaemia in chronic kidney disease. Nat. Rev. Nephrol. 2014, 10, 653–662. [Google Scholar] [CrossRef]
- Tromp, J.; van der Meer, P. Hyperkalaemia: Aetiology, epidemiology, and clinical significance. Eur. Heart J. Suppl. 2019, 21, A6–A11. [Google Scholar] [CrossRef]
- Luo, J.; Brunelli, S.M.; Jensen, D.E.; Yang, A. Association between Serum Potassium and Outcomes in Patients with Reduced Kidney Function. Clin. J. Am. Soc. Nephrol. 2016, 11, 90–100. [Google Scholar] [CrossRef]
- Collins, A.J.; Pitt, B.; Reaven, N.; Funk, S.; McGaughey, K.; Wilson, D.; Bushinsky, D.A. Association of Serum Potassium with All-Cause Mortality in Patients with and without Heart Failure, Chronic Kidney Disease, and/or Diabetes. Am. J. Nephrol. 2017, 46, 213–221. [Google Scholar] [CrossRef]
- Krogager, M.L.; Torp-Pedersen, C.; Mortensen, R.N.; Køber, L.; Gislason, G.; Søgaard, P.; Aasbjerg, K. Short-term mortality risk of serum potassium levels in hypertension: A retrospective analysis of nationwide registry data. Eur. Heart J. 2017, 38, 104–112. [Google Scholar] [CrossRef] [PubMed]
- Kashihara, N.; Kohsaka, S.; Kanda, E.; Okami, S.; Yajima, T. Hyperkalemia in Real-World Patients under Continuous Medical Care in Japan. Kidney Int. Rep. 2019, 4, 1248–1260. [Google Scholar] [CrossRef] [PubMed]
- Kovesdy, C.P.; Matsushita, K.; Sang, Y.; Brunskill, N.J.; Carrero, J.J.; Chodick, G.; Hasegawa, T.; Heerspink, H.L.; Hirayama, A.; Landman, G.W.D.; et al. Serum potassium and adverse outcomes across the range of kidney function: A CKD Prognosis Consortium meta-analysis. Eur. Heart J. 2018, 39, 1535–1542. [Google Scholar] [CrossRef]
- Kohsaka, S.; Okami, S.; Kanda, E.; Kashihara, N.; Yajima, T. Cardiovascular and Renal Outcomes Associated with Hyperkalemia in Chronic Kidney Disease: A Hospital-Based Cohort Study. Mayo Clin. Proc. Innov. Qual. Outcomes 2021, 19, 274–285. [Google Scholar] [CrossRef]
- Fauvel, J.P.; Gueyffier, F.; Thijs, L.; Ducher, M. Combined effect of renal function and serum potassium level in sudden cardiac death in aging hypertensive subjects. Hypertens. Res. 2018, 41, 469–474. [Google Scholar] [CrossRef] [PubMed]
- Fu, E.L.; Evans, M.; Clase, C.M.; Tomlinson, L.A.; van Diepen, M.; Dekker, F.W.; Carrero, J.J. Stopping Renin-Angiotensin System Inhibitors in Patients with Advanced CKD and Risk of Adverse Outcomes: A Nationwide Study. J. Am. Soc. Nephrol. 2021, 32, 424–435. [Google Scholar] [CrossRef]
- Linde, C.; Bakhai, A.; Furuland, H.; Evans, M.; McEwan, P.; Ayoubkhani, D.; Qin, L. Real-World Associations of Renin-Angiotensin-Aldosterone System Inhibitor Dose, Hyperkalemia, and Adverse Clinical Outcomes in a Cohort of Patients with New-Onset Chronic Kidney Disease or Heart Failure in the United Kingdom. J. Am. Heart Assoc. 2019, 8, e012655. [Google Scholar] [CrossRef]
- Saglimbene, V.M.; Wong, G.; Ruospo, M.; Almer, S.C.; Garcia-Larsen, V.; Natale, P.; Teixeira-Pinto, A.; Campbell, K.L.; Carrero, J.J.; Stenvinkel, P.; et al. Fruit and Vegetable Intake and Mortality in Adults undergoing Maintenance Hemodialysis. Clin. J. Am. Soc. Nephrol. 2019, 14, 250–260. [Google Scholar] [CrossRef]
- Kelly, J.T.; Palmer, S.C.; Wai, S.N.; Ruospo, M.; Carrero, J.J.; Campbell, K.L.; Strippoli, G.F. Healthy Dietary Patterns and Risk of Mortality and ESRD in CKD: A Meta-Analysis of Cohort Studies. Clin. J. Am. Soc. Nephrol. 2017, 12, 272–279. [Google Scholar] [CrossRef]
- Raket, L.L.; Jaskolowski, J.; Kinon, B.J.; Brasen, J.C.; Jönsson, L.; Wehnert, A.; Fusar-Poli, P. Dynamic ElecTronic hEalth reCord deTection (DETECT) of individuals at risk of a first episode of psychosis: A case-control development and validation study. Lancet Digit. Health 2020, 2, e229–e239. [Google Scholar] [CrossRef]
- Fox, K.A.A.; Lucas, J.E.; Pieper, K.S.; Bassand, J.P.; Camm, A.J.; Fitzmaurice, D.A.; Goldhaber, S.Z.; Goto, S.; Haas, S.; Hacke, W.; et al. Improved risk stratification of patients with atrial fibrillation: An integrated GARFIELD-AF tool for the prediction of mortality, stroke and bleed in patients with and without anticoagulation. BMJ Open 2017, 7, e017157. [Google Scholar] [CrossRef] [PubMed]
- Ng, A.Y. Feature selection, L1 vs. L2 regularization, and rotational invariance. In Proceedings of the Twenty-First International Conference on Machine Learning, New York, NY, USA, 4–8 July 2004; Volume 2004, p. 78. [Google Scholar]
- Chen, T.; Guestrin, C. Xgboost: A scalable tree boosting system. In Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, San Francisco, CA, USA, 13–17 August 2016; Volume 2016, pp. 785–794. [Google Scholar]
- Schmidhuber, J. Deep learning in neural networks: An overview. Neural Netw. 2015, 61, 85–117. [Google Scholar] [CrossRef] [PubMed]
- Ravizza, S.; Huschto, T.; Adamov, A.; Böhm, L.; Büsser, A.; Flöther, F.F.; Hinzmann, R.; König, H.; McAhren, S.M.; Robertson, D.H.; et al. Predicting the early risk of chronic kidney disease in patients with diabetes using real-world data. Nat. Med. 2019, 25, 57–59. [Google Scholar] [CrossRef] [PubMed]
- Makino, M.; Yoshimoto, R.; Ono, M.; Itoko, T.; Katsuki, T.; Koseki, A.; Kudo, M.; Haida, K.; Kuroda, J.; Yanagiya, R.; et al. Artificial intelligence predicts the progression of diabetic kidney disease using big data machine learning. Sci. Rep. 2019, 9, 11862. [Google Scholar] [CrossRef]
- Lundberg, S.M.; Lee, S.-I. A unified approach to interpreting model predictions. Adv. Neural Inf. Processing Syst. 2017, 2017, 4765–4774. [Google Scholar]
- Angraal, S.; Mortazavi, B.J.; Gupta, A.; Khera, R.; Ahmad, T.; Desai, N.R.; Jacoby, D.L.; Masoudi, F.A.; Spertus, J.A.; Krumholz, H.M. Machine Learning Prediction of Mortality and Hospitalization in Heart Failure with Preserved Ejection Fraction. JACC Heart Fail. 2020, 8, 12–21. [Google Scholar] [CrossRef]
- Akbilgic, O.; Obi, Y.; Potukuchi, P.K.; Karabayir, I.; Nguyen, D.V.; Soohoo, M.; Streja, E.; Molnar, M.Z.; Rhee, C.M.; Kalantar-Zadeh, K.; et al. Machine Learning to Identify Dialysis Patients at High Death Risk. Kidney Int. Rep. 2019, 4, 1219–1229. [Google Scholar] [CrossRef]
- Kanda, E.; Ai, M.; Kuriyama, R.; Yoshida, M.; Shiigai, T. Dietary acid intake and kidney disease progression in the elderly. Am. J. Nephrol. 2014, 39, 145–152. [Google Scholar] [CrossRef]
- Scialla, J.J.; Appel, L.J.; Astor, B.C.; Miller, E.R., 3rd; Beddhu, S.; Woodward, M.; Parekh, R.S.; Anderson, C.A.; African American Study of Kidney Disease and Hypertension Study Group. Net endogenous acid production is associated with a faster decline in GEF in African Americans. Kidney Int. 2012, 82, 106–112. [Google Scholar] [CrossRef]
- Jhee, J.H.; Kee, Y.K.; Park, J.T.; Chang, T.I.; Kang, E.W.; Yoo, T.H.; Kang, S.W.; Han, S.H. A diet rich in vegetables and fruit and incident CKD: A community-based prospective cohort study. Am. J. Kidney Dis. 2019, 74, 491–500. [Google Scholar] [CrossRef]
- Toba, K.; Hosojima, M.; Kobasawa, H.; Kuwahara, S.; Murayama, T.; Yamamoto-Kabasawa, K.; Kaseda, R.; Wada, E.; Watanabe, R.; Tanabe, N.; et al. Higher estimated net endogenous acid production with lower intake of fruits and vegetables based on a dietary survey is associated with the progression of chronic kidney disease. BMC Nephrol. 2019, 20, 421. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.W.; Park, J.T.; Yoo, T.H.; Lee, J.; Chung, W.; Lee, K.B.; Chae, D.W.; Ahn, C.; Kang, S.W.; Choi, K.H.; et al. Urinary potassium excretion and progression of CKD. Clin. J. Am. Soc. Nephrol. 2019, 14, 330–340. [Google Scholar] [CrossRef] [PubMed]
- Araki, S.; Haneda, M.; Koya, D.; Kondo, K.; Tanaka, S.; Arima, H.; Kume, S.; Nakazawa, J.; Chin-Kanasaki, M.; Ugi, S.; et al. Urinary potassium excretion and renal and cardiovascular complications in patients with type 2 diabetes and normal renal function. Clin. J. Am. Soc. Nephrol. 2015, 10, 2152–2158. [Google Scholar] [CrossRef] [PubMed]
- Ikizler, T.A.; Burrowes, J.D.; Byham-Gray, L.D.; Campbell, K.L.; Carrero, J.J.; Chan, W.; Fouque, D.; Friedman, A.N.; Ghaddar, S.; Goldstein-Fuchs, D.J.; et al. Kdoqi Clinical Practice Guideline for Nutrition in Ckd: 2020 Update. Am. J. Kidney Dis. 2020, 76, S1–S107. [Google Scholar] [CrossRef]
- Kholghi, M.; Sitbon, L.; Zuccon, G.; Nguyen, A. Active learning: A step towards automating medical concept extraction. J. Am. Med. Inform. Assoc. 2016, 23, 289–296. [Google Scholar] [CrossRef]
- Lv, X.; Guan, Y.; Deng, B. Transfer learning based clinical concept extraction on data from multiple sources. J. Biomed. Inform. 2014, 52, 55–64. [Google Scholar] [CrossRef]



| Derivation Set (N = 8752) | Internal Validation Set (N = 4990) | External Validation Set (N = 86,279) | |
|---|---|---|---|
| Age (years) | |||
| mean ± SD | 75.7 ± 12.4 | 74.9 ± 12.8 | 74.9±13.1 |
| Gender, male, n (%) | 4717 (53.9) | 2697 (54.1) | 46,976 (54.4) |
| Follow up time (days) | |||
| mean ± SD | 755.2 ± 641.6 | 805.3 ± 743.4 | 664.2 ± 443.3 |
| Serum potassium value (mmol/L) | |||
| mean ± SD | 5.4 ± 0.4 | 5.5 ± 0.5 | 5.7 ± 2.2 |
| Serum potassium value group, n (%) | |||
| ≥5.1 and <5.5 mmol/L | 6326 (72.3) | 3347 (67.1) | 55,984 (64.9) |
| ≥5.5 and <6.0 mmol/L | 1727 (19.7) | 1094 (21.9) | 18,443 (21.4) |
| ≥6.0 and <6.5 mmol/L | 434 (5.0) | 328 (6.6) | 5656 (6.6) |
| ≥6.5 and <7.0 mmol/L | 145 (1.7) | 123 (2.5) | 2492 (2.9) |
| ≥7.0 mmol/L | 120 (1.4) | 98 (2.0) | 3704 (4.3) |
| CKD, n (%) | 6854 (78.3) | 4033 (80.8) | 56,224 (65.2) |
| Stage 1 | 27 (0.4) | 11 (0.3) | 654 (1.2) |
| Stage 2 | 165 (2.4) | 80 (2.0) | 3771 (6.7) |
| Stage 3a | 1215 (17.7) | 628 (15.6) | 8607 (15.3) |
| Stage 3b | 1944 (28.4) | 1073 (26.6) | 12,863 (22.9) |
| Stage 4 | 2212 (32.3) | 1215 (30.1) | 14,570 (25.9) |
| Stage 5 | 1,291 (18.8) | 1025 (25.4) | 15,759 (28.0) |
| HF, n (%) | 5206 (59.5) | 2628 (52.7) | 38,955 (45.2) |
| Diabetes, n (%) | 4954 (56.6) | 2478 (49.7) | 31,073 (36.0) |
| Hypertension, n (%) | 7247 (82.8) | 3605 (72.2) | 31,956 (37.0) |
| Dyslipidemia, n (%) | 3039 (34.7) | 1391 (27.9) | 17,194 (19.9) |
| Comorbidity, n (%) | |||
| Myocardial infarction | 382 (4.4) | 268 (5.4) | 5,322 (6.2) |
| Peripheral vascular disease | 1648 (18.8) | 798 (16.0) | 9,844 (11.4) |
| Cerebrovascular disease | 2,567 (29.3) | 1255 (25.2) | 13,455 (15.6) |
| Chronic pulmonary disease | 1821 (20.8) | 829 (16.6) | 8,620 (10.0) |
| Moderate to severe disease | 130 (1.5) | 68 (1.4) | 868 (1.0) |
| Atrial flutter or atrial fibrillation | 1846 (21.1) | 900 (18.0) | 9,827 (11.4) |
| Valvular heart disease | 1347 (15.4) | 623 (12.5) | 8,594 (10.0) |
| Acute kidney injury | 385 (4.4) | 309 (6.2) | 3,271 (3.8) |
| Sepsis | 1161 (13.3) | 537 (10.8) | 7,178 (8.3) |
| Gastrointestinal bleeding | 320 (3.7) | 178 (3.6) | 3,330 (3.9) |
| Peripheral oedema | 343 (3.9) | 150 (3.0) | 926 (1.1) |
| eGFR value (mL/min/1.73 m2) | |||
| mean ± SD | 35.3 ± 22.0 | 32.9 ± 21.7 | 37.7 ± 26.6 |
| RAASi treatment, n (%) | 5075 (58.0) | 2485 (49.8) | 30,445 (35.3) |
| Angiotensin converting enzyme inhibitors | 1,041 (11.9) | 555 (11.1) | 7,629 (8.8) |
| Angiotensin receptor blockers | 3653 (41.7) | 1755 (35.2) | 21,475 (24.9) |
| MRA | 1,820 (20.8) | 881 (17.7) | 9,003 (10.4) |
| Hyperkalemia treatment, n (%) | |||
| Thiazide diuretics | 264 (3.0) | 122 (2.4) | 3,472 (4.0) |
| Loop diuretics | 2186 (25.0) | 1251 (25.1) | 26,134 (30.3) |
| Calcium gluconate | 181 (2.1) | 151 (3.0) | 2,587 (3.0) |
| Sodium bicarbonate | 658 (7.5) | 402 (8.1) | 1,086 (1.3) |
| Potassium binder (SPS/CPS) | 607 (6.9) | 404 (8.1) | 4,388 (5.1) |
| Glucose injection and insulin | 181 (2.1) | 133 (2.7) | 972 (1.1) |
| Outcome | ML Algorithm | AUROC | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|---|---|
| Cut-off = 0.5 | ||||||
| All-cause death | XGB | 0.823 | 0.244 | 0.966 | 0.594 | 0.863 |
| LR | 0.809 | 0.224 | 0.964 | 0.556 | 0.860 | |
| NN | 0.741 | 0.285 | 0.935 | 0.470 | 0.866 | |
| Introduction of RRT | XGB | 0.957 | 0.903 | 0.893 | 0.594 | 0.981 |
| LR | 0.947 | 0.612 | 0.967 | 0.761 | 0.935 | |
| NN | 0.923 | 0.584 | 0.966 | 0.750 | 0.930 | |
| Hospitalization for HF | XGB | 0.863 | 0.403 | 0.967 | 0.680 | 0.903 |
| LR | 0.838 | 0.330 | 0.967 | 0.632 | 0.892 | |
| NN | 0.839 | 0.438 | 0.948 | 0.594 | 0.907 | |
| Cardiovascular events | XGB | 0.809 | 0.107 | 0.998 | 0.810 | 0.920 |
| LR | 0.798 | 0.095 | 0.996 | 0.700 | 0.919 | |
| NN | 0.783 | 0.286 | 0.982 | 0.603 | 0.934 | |
| Best cut-off | ||||||
| All-cause death | XGB | 0.823 | 0.819 | 0.677 | 0.339 | 0.949 |
| LR | 0.809 | 0.802 | 0.676 | 0.334 | 0.944 | |
| NN | 0.741 | 0.670 | 0.690 | 0.304 | 0.912 | |
| Introduction of RRT | XGB | 0.957 | 0.899 | 0.903 | 0.616 | 0.981 |
| LR | 0.947 | 0.914 | 0.867 | 0.544 | 0.983 | |
| NN | 0.923 | 0.866 | 0.862 | 0.522 | 0.974 | |
| Hospitalization for HF | XGB | 0.863 | 0.751 | 0.813 | 0.411 | 0.949 |
| LR | 0.838 | 0.743 | 0.797 | 0.389 | 0.947 | |
| NN | 0.839 | 0.708 | 0.830 | 0.420 | 0.942 | |
| Cardiovascular events | XGB | 0.809 | 0.639 | 0.869 | 0.320 | 0.961 |
| LR | 0.798 | 0.637 | 0.858 | 0.302 | 0.961 | |
| NN | 0.783 | 0.746 | 0.689 | 0.189 | 0.965 |
| Outcome | AUROC | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|---|
| All-cause death | 0.747 | 0.757 | 0.613 | 0.209 | 0.949 |
| Introduction of RRT | 0.888 | 0.555 | 0.916 | 0.285 | 0.971 |
| Hospitalization for HF | 0.673 | 0.445 | 0.767 | 0.183 | 0.922 |
| Cardiovascular events | 0.585 | 0.326 | 0.771 | 0.141 | 0.909 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kanda, E.; Okami, S.; Kohsaka, S.; Okada, M.; Ma, X.; Kimura, T.; Shirakawa, K.; Yajima, T. Machine Learning Models Predicting Cardiovascular and Renal Outcomes and Mortality in Patients with Hyperkalemia. Nutrients 2022, 14, 4614. https://doi.org/10.3390/nu14214614
Kanda E, Okami S, Kohsaka S, Okada M, Ma X, Kimura T, Shirakawa K, Yajima T. Machine Learning Models Predicting Cardiovascular and Renal Outcomes and Mortality in Patients with Hyperkalemia. Nutrients. 2022; 14(21):4614. https://doi.org/10.3390/nu14214614
Chicago/Turabian StyleKanda, Eiichiro, Suguru Okami, Shun Kohsaka, Masafumi Okada, Xiaojun Ma, Takeshi Kimura, Koichi Shirakawa, and Toshitaka Yajima. 2022. "Machine Learning Models Predicting Cardiovascular and Renal Outcomes and Mortality in Patients with Hyperkalemia" Nutrients 14, no. 21: 4614. https://doi.org/10.3390/nu14214614
APA StyleKanda, E., Okami, S., Kohsaka, S., Okada, M., Ma, X., Kimura, T., Shirakawa, K., & Yajima, T. (2022). Machine Learning Models Predicting Cardiovascular and Renal Outcomes and Mortality in Patients with Hyperkalemia. Nutrients, 14(21), 4614. https://doi.org/10.3390/nu14214614





