Dietary Potassium Intake and Risk of Diabetes: A Systematic Review and Meta-Analysis of Prospective Studies
Abstract
1. Introduction
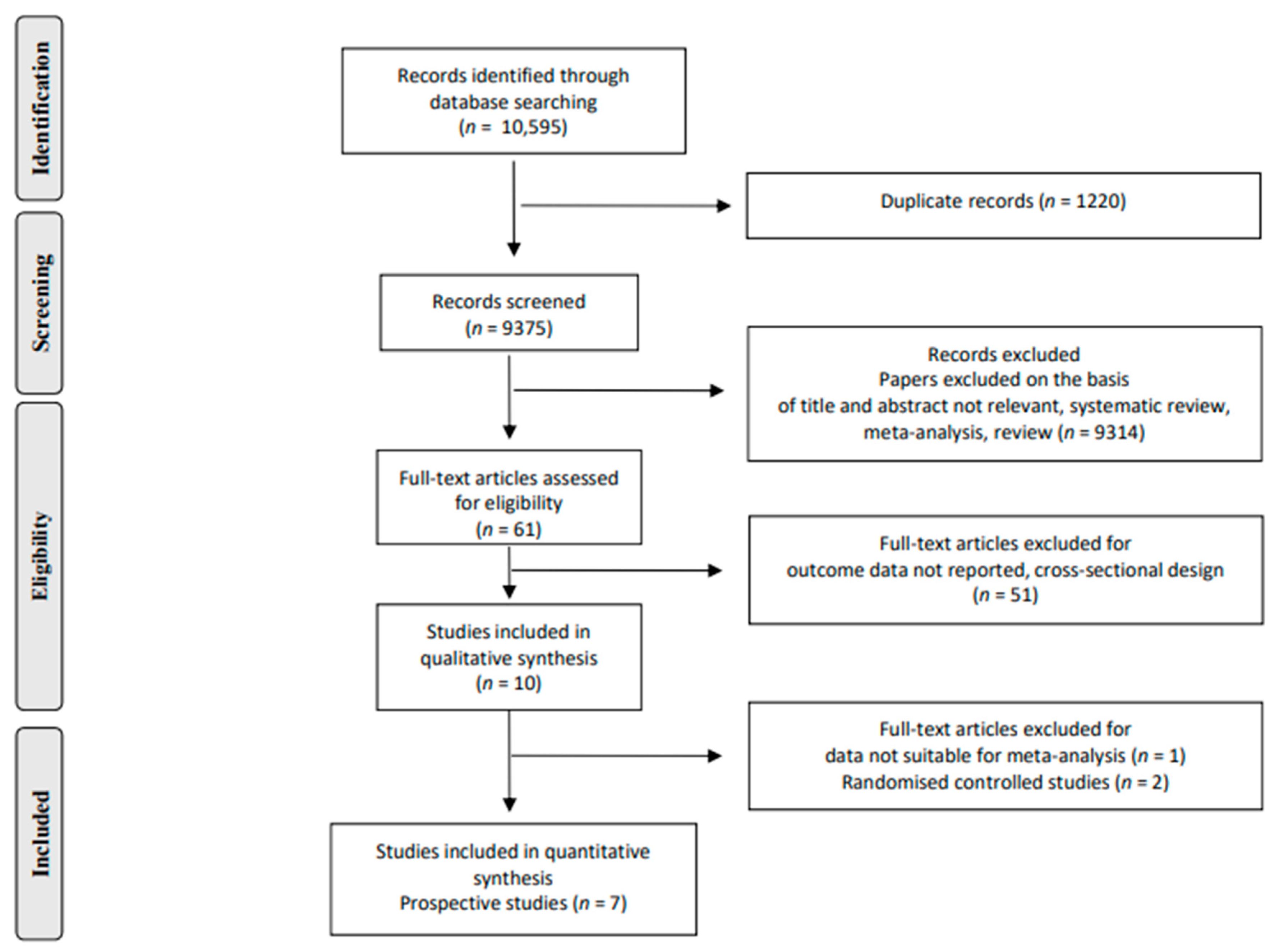
2. Materials and Methods
2.1. Data Sources and Search Strategy
2.2. Study Selection and Data Extraction
2.3. Inclusion Criteria
2.4. Risk of Bias
2.5. Grading of Evidence
2.6. Statistical Analysis
3. Results
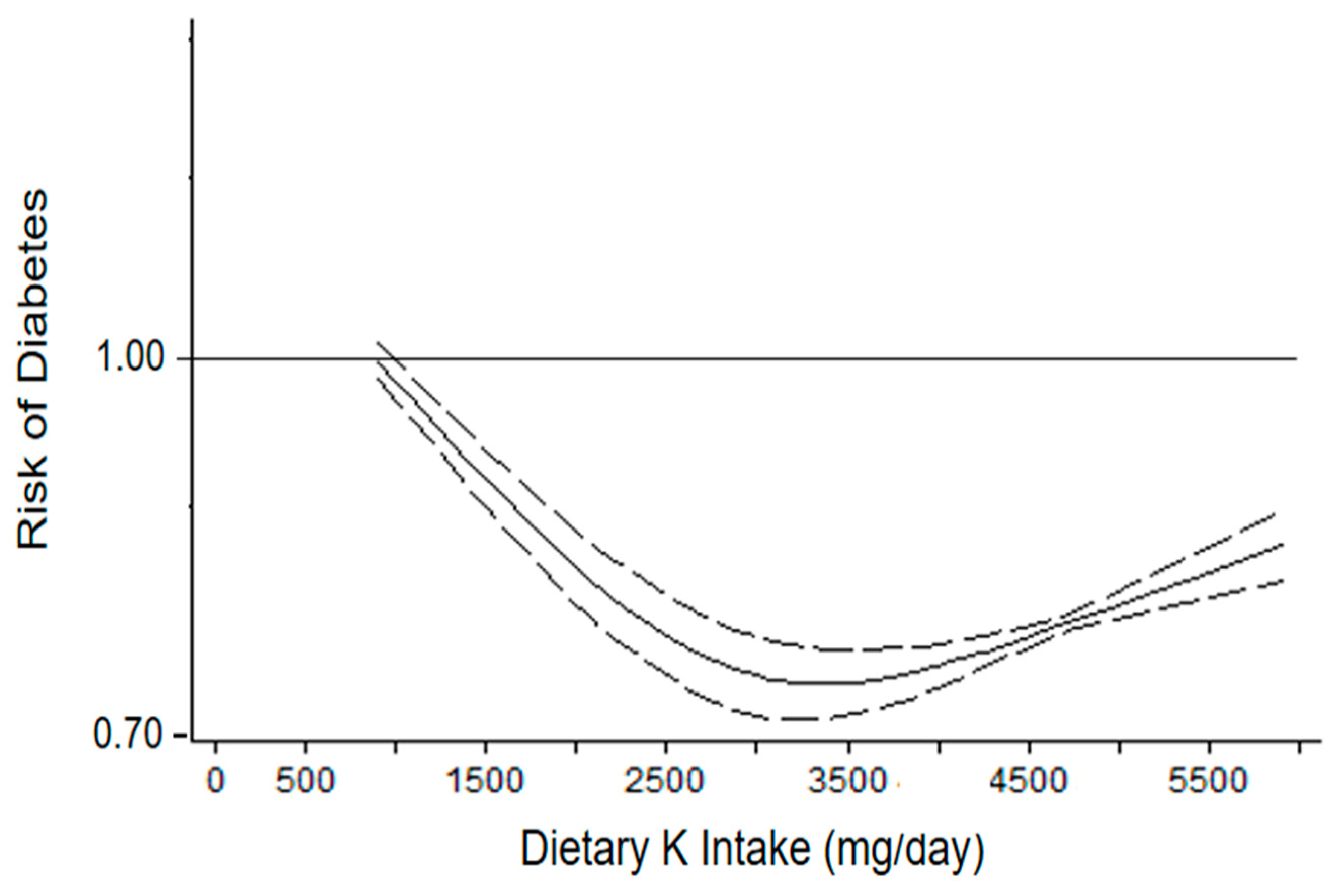
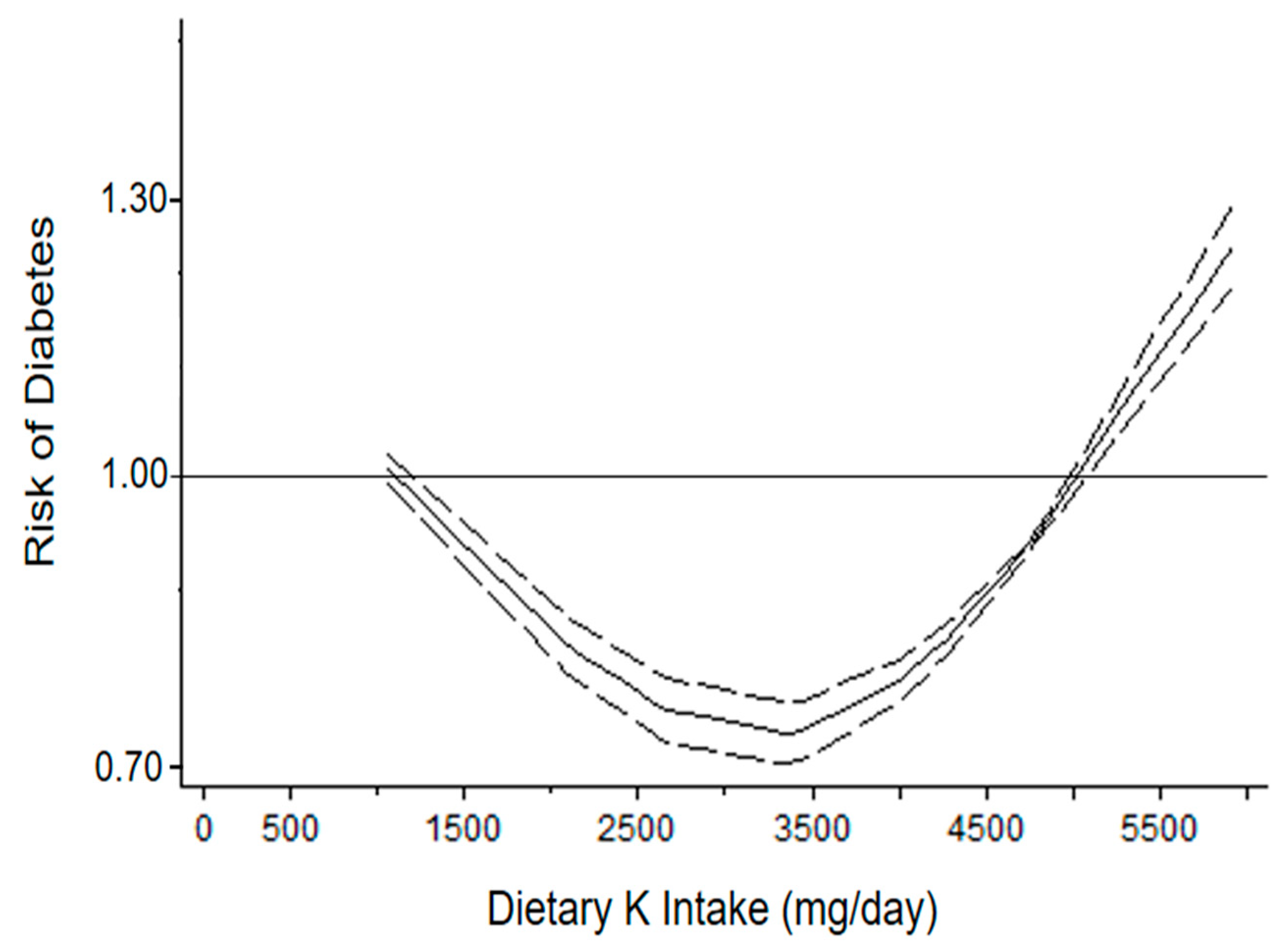
3.1. Dietary Potassium Intake and Risk of Diabetes
3.1.1. Urinary Potassium Excretion
3.1.2. Dietary Questionnaire
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Aburto, N.J.; Hanson, S.; Gutierrez, H.; Hooper, L.; Elliott, P.; Cappuccio, F.P. Effect of increased potassium intake on cardiovascular risk factors and disease: Systematic review and meta-analyses. BMJ 2013, 346, f1378. [Google Scholar] [CrossRef] [PubMed]
- D’Elia, L.; Barba, G.; Cappuccio, F.P.; Strazzullo, P. Potassium intake, stroke, and cardiovascular disease a meta-analysis of prospective studies. J. Am. Coll. Cardiol. 2011, 57, 1210–1219. [Google Scholar] [CrossRef] [PubMed]
- D’Elia, L.; Iannotta, C.; Sabino, P.; Ippolito, R. Potassium-rich diet and risk of stroke: Updated meta-analysis. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 585–587. [Google Scholar] [CrossRef] [PubMed]
- Iacoviello, L.; Bonaccio, M.; Cairella, G.; Catani, M.V.; Costanzo, S.; D’Elia, L.; Giacco, R.; Rendina, D.; Sabino, P.; Savini, I.; et al. Diet and primary prevention of stroke: Systematic review and dietary recommendations by the ad hoc Working Group of the Italian Society of Human Nutrition. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 309–334. [Google Scholar] [CrossRef]
- Rowe, J.W.; Tobin, J.D.; Rosa, R.M.; Andres, R. Effect of experimental potassium deficiency on glucose and insulin metabolism. Metabolism 1980, 29, 498–502. [Google Scholar] [CrossRef]
- Hu, G.; Jousilahti, P.; Peltonen, M.; Lindström, J.; Tuomilehto, J. Urinary sodium and potassium excretion and the risk of type 2 diabetes: A prospective study in Finland. Diabetologia 2005, 48, 1477–1483. [Google Scholar] [CrossRef]
- Chatterjee, R.; Yeh, H.C.; Shafi, T.; Selvin, E.; Anderson, C.; Pankow, J.S.; Miller, E.; Brancati, F. Serum and dietary potassium and risk of incident type 2 diabetes mellitus: The Atherosclerosis Risk in Communities (ARIC) study. Arch. Intern. Med. 2010, 170, 1745–1751. [Google Scholar] [CrossRef]
- Chatterjee, R.; Colangelo, L.A.; Yeh, H.C.; Anderson, C.A.; Daviglus, M.L.; Liu, K.; Brancati, F.L. Potassium intake and risk of incident type 2 diabetes mellitus: The Coronary Artery Risk Development in Young Adults (CARDIA) Study. Diabetologia 2012, 55, 1295–1303. [Google Scholar] [CrossRef]
- Hao, G.; Liu, K.; Halbert, J.D.; Chen, H.; Wu, J.; Jing, C. Dietary sodium and potassium and risk of diabetes: A prospective study using data from the China Health and Nutrition Survey. Diabetes Metab. 2020, 46, 377–383. [Google Scholar] [CrossRef]
- Chatterjee, R.; Zelnick, L.; Mukamal, K.J.; Nettleton, J.A.; Kestenbaum, B.R.; Siscovick, D.S.; Ix, J.H.; Tracy, R.; Hoofnagle, A.N.; Svetkey, L.P.; et al. Potassium Measures and Their Associations with Glucose and Diabetes Risk: The Multi-Ethnic Study of Atherosclerosis (MESA). PLoS ONE 2016, 11, e0157252. [Google Scholar] [CrossRef]
- Chatterjee, R.; Biggs, M.L.; de Boer, I.H.; Brancati, F.L.; Svetkey, L.P.; Barzilay, J.; Djoussé, L.; Ix, J.H.; Kizer, J.R.; Siscovick, D.S.; et al. Potassium and glucose measures in older adults: The Cardiovascular Health Study. J. Gerontol. A Biol. Sci. Med. Sci. 2015, 70, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, R.; Davenport, C.A.; Svetkey, L.P.; Batch, B.C.; Lin, P.H.; Ramachandran, V.S.; Fox, E.R.; Harman, J.; Yeh, H.C.; Selvin, E.; et al. Serum potassium is a predictor of incident diabetes in African Americans with normal aldosterone: The Jackson Heart Study. Am. J. Clin. Nutr. 2017, 105, 442–449. [Google Scholar] [CrossRef] [PubMed]
- Peng, Y.; Zhong, G.C.; Mi, Q.; Li, K.; Wang, A.; Li, L.; Liu, H.; Yang, G. Potassium measurements and risk of type 2 diabetes: A dose-response meta-analysis of prospective cohort studies. Oncotarget 2017, 8, 100603–100613. [Google Scholar] [CrossRef] [PubMed]
- National Academies of Sciences, Engineering, and Medicine. Dietary Reference Intakes for Sodium and Potassium; The National Academies Press: Washington, DC, USA, 2019. [Google Scholar] [CrossRef]
- Conen, K.; Scanni, R.; Gombert, M.T.; Hulter, H.N.; Krapf, R. Effects of potassium citrate or potassium chloride in patients with combined glucose intolerance: A placebo-controlled pilot study. J. Diabetes Complicat. 2016, 30, 1158–1161. [Google Scholar] [CrossRef]
- Chatterjee, R.; Slentz, C.; Davenport, C.A.; Johnson, J.; Lin, P.H.; Muehlbauer, M.; D’Alessio, D.; Svetkey, L.P.; Edelman, D. Effects of potassium supplements on glucose metabolism in African Americans with prediabetes: A pilot trial. Am. J. Clin. Nutr. 2017, 106, 1431–1438. [Google Scholar] [CrossRef]
- Saeedi, P.; Petersohn, I.; Salpea, P.; Malanda, B.; Karuranga, S.; Unwin, N.; Colagiuri, S.; Guariguata, L.; Motala, A.A.; Ogurtsova, K.; et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res. Clin. Pract. 2019, 157, 107843. [Google Scholar] [CrossRef]
- D’Elia, L.; Brajović, M.; Klisic, A.; Breda, J.; Jewell, J.; Cadjenović, V.; Cappuccio, F.P. Sodium and Potassium Intake, Knowledge Attitudes and Behaviour Towards Salt Consumption Amongst Adults in Podgorica, Montenegro. Nutrients 2019, 11, 160. [Google Scholar] [CrossRef]
- D’Elia, L.; Obreja, G.; Ciobanu, A.; Breda, J.; Jewell, J.; Cappuccio, F.P. Sodium, Potassium and Iodine Intake, in A National Adult Population Sample of the Republic of Moldova. Nutrients 2019, 11, 2896. [Google Scholar] [CrossRef]
- Al-Mawali, A.; D’Elia, L.; Jayapal, S.K.; Morsi, M.; Al-Shekaili, W.N.; Pinto, A.D.; Al-Kharusi, H.; Al-Balushi, Z.; Idikula, J.; Al-Harrasi, A.; et al. National survey to estimate sodium and potassium intake and knowledge attitudes and behaviours towards salt consumption of adults in the Sultanate of Oman. BMJ Open 2020, 10, e037012. [Google Scholar] [CrossRef]
- Donfrancesco, C.; Lo Noce, C.; Russo, O.; Buttari, B.; Profumo, E.; Minutoli, D.; Di Lonardo, A.; Iacone, R.; Vespasiano, F.; Vannucchi, S.; et al. Trend in potassium intake and Na/K ratio in the Italian adult population between the 2008 and 2018 CUORE project surveys. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 814–826. [Google Scholar] [CrossRef]
- Cogswell, M.E.; Zhang, Z.; Carriquiry, A.L.; Gunn, J.P.; Kuklina, E.V.; Saydah, S.H.; Yang, Q.; Moshfegh, A.J. Sodium and potassium intakes among US adults: NHANES 2003–2008. Am. J. Clin. Nutr. 2012, 96, 647–657. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Tammy, C.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; Chou, R.; Glanville, J.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 1 June 2022).
- Schünemann, H.; Brożek, J.; Guyatt, G.; Oxman, A. GRADE Handbook. Handbook for Grading the Quality of Evidence and the Strength of Recommendations Using the GRADE Approach. 2013. Available online: https://gdt.gradepro.org/app/handbook/handbook.html (accessed on 15 June 2022).
- Orsini, N.; Li, R.; Wolk, A.; Khudyakov, P.; Spiegelman, D. Meta-analysis for linear and nonlinear dose-response relations: Examples, an evaluation of approximations, and software. Am. J. Epidemiol. 2012, 175, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Colditz, G.A.; Manson, J.E.; Stampfer, M.J.; Rosner, B.; Willett, W.C.; Speizer, F.E. Diet and risk of clinical diabetes in women. Am. J. Clin. Nutr. 1992, 55, 1018–1023. [Google Scholar] [CrossRef]
- Hayes, D.P. Nutritional hormesis. Eur. J. Clin. Nutr. 2007, 61, 147–159. [Google Scholar] [CrossRef]
- Filippini, T.; Naska, A.; Kasdagli, M.I.; Torres, D.; Lopes, C.; Carvalho, C.; Moreira, P.; Malavolti, M.; Orsini, N.; Whelton, P.K.; et al. Potassium Intake and Blood Pressure: A Dose-Response Meta-Analysis of Randomized Controlled Trials. J. Am. Heart Assoc. 2020, 9, e015719. [Google Scholar] [CrossRef]
- World Health Organization. Guideline: Potassium Intake for Adults and Children; WHO: Geneva, Switzerland, 2012. [Google Scholar]
- Gumz, M.L.; Rabinowitz, L.; Wingo, C.S. An Integrated View of Potassium Homeostasis. N. Engl. J. Med. 2015, 373, 60–72. [Google Scholar] [CrossRef] [PubMed]
- Norbiato, G.; Bevilacqua, M.; Meroni, R.; Raggi, U.; Dagani, R.; Scorza, D.; Frigeni, G.; Vago, T. Effects of potassium supplementation on insulin binding and insulin action in human obesity: Protein-modified fast and refeeding. Eur. J. Clin. Investig. 1984, 14, 414–419. [Google Scholar] [CrossRef] [PubMed]
- Helderman, J.H.; Elahi, D.; Andersen, D.K.; Raizes, G.S.; Tobin, J.D.; Shocken, D.; Andres, R. Prevention of the glucose intolerance of thiazide diuretics by maintenance of body potassium. Diabetes 1983, 32, 106–111. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J. Hypertens 2018, 36, 1953–2041. [Google Scholar] [CrossRef]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E., Jr.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American college of cardiology/American heart association task force on clinical practice guidelines. J. Am. Coll. Cardiol. 2018, 71, e127–e248. [Google Scholar] [PubMed]
- EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies); Turck, D.; Bresson, J.-L.; Burlingame, B.; Dean, T.; Fairweather-Tait, S.; Heinonen, M.; Hirsch-Ernst, K.I.; Mangelsdorf, I.; McArdle, H.; et al. Scientific opinion on dietary reference values for potassium. EFSA J. 2016, 14, 4592. [Google Scholar] [CrossRef]
- D’Elia, L.; La Fata, E.; Galletti, F.; Scalfi, L.; Strazzullo, P. Coffee consumption and risk of hypertension: A dose-response meta-analysis of prospective studies. Eur. J. Nutr. 2019, 58, 271–280. [Google Scholar] [CrossRef] [PubMed]
- D’Elia, L.; Dinu, M.; Sofi, F.; Volpe, M.; Strazzullo, P.; SINU Working Group, Endorsed by SIPREC. 100% Fruit juice intake and cardiovascular risk: A systematic review and meta-analysis of prospective and randomised controlled studies. Eur. J. Nutr. 2021, 60, 2449–2467. [Google Scholar] [CrossRef]

| Prospective Studies | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| First Author, Year (Ref) | Country | Population [Ethnicity] | Participants (n)/Cases (n) | Gender [M/F] (%) | Follow-Up (Year) | Age (Year) (Range) | BMI (kg/m2) | Dietary Assessment Tool | Dietary Potassium Intake (mg/day) | Outcome (Type of Assessment) |
| Hu, 2005 [6] | Finland | General population | 1935/129 | 48/52 | 18.1 | 49.7 (35–64) | 27 | 24 h urinary potassium excretion | 4120 * | Fasting blood glucose > 126 mg/dL Non-fasting glucose > 200 mg/dL |
| Chatterjee, 2010 [7] | US | ARIC [African American 22%] | 12,209/1475 | 44/56 | 9 | 54 (45–65) | 27 | Validated FFQ | 2655 | Fasting blood glucose ≥ 126 mg/dL Non-fasting glucose ≥ 200 mg/dL Clinician-diagnosed diabetes Use of antidiabetic medications |
| Chatterjee, 2012 [8] | US | CARDIA [African American 50%] | 4754/373 | 45/55 | 20 | 25 (18–30) | 24.5 | Validated FFQ | 3661 | Fasting blood glucose ≥ 126 mg/dL Non fasting glucose ≥ 200 mg/dL HbA1c ≥ 6.5% Use of antidiabetic medication |
| [African American 55%] | 1066/99 | 43/57 | 15 | 30 (18–30) | 26.9 | 24 h urinary potassium excretion | 2788 * | |||
| Chatterjee, 2015 [11] | US | CHS | 4111/375 | 41/59 | 12.1 | 72.9 (≥65) | 26.3 | Validated FFQ | 3191 | Fasting blood glucose ≥ 126 mg/dL Non-fasting glucose ≥ 200 mg/dL Use of antidiabetic medications |
| Chatterjee, 2016 [10] | US | MESA [42% Caucasian/white, 24.8% African American, 20.5% Hispanic, 12.5% Asian] | 5415/1281 | 46/54 | 8 | 61.8 (45–84) | 28 | Validated FFQ | 2555 | Fasting blood glucose ≥ 126 mg/dL Use of antidiabetic medications |
| Chatterjee, 2016 [12] | US | Jackson Heart Study [African American] | 2157/398 | 37/63 | 8 | 52.4 (21–95) | 31.1 | Validated FFQ | 2542 | Fasting blood glucose ≥ 126 mg/dL HbA1c ≥ 6.5% Use of antidiabetic medications |
| Hao, 2020 [9] | China | CHNS | 5867/611 | 46/54 | 4.7 | 48.1 (18–93) | ** | 3 consecutive 24 h recalls | 1791 | Fasting glucose levels ≥ 126 mg/dL HbA1c ≥ 6.5% Use of antidiabetic medications |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
D’Elia, L.; Masulli, M.; Cappuccio, F.P.; Zarrella, A.F.; Strazzullo, P.; Galletti, F. Dietary Potassium Intake and Risk of Diabetes: A Systematic Review and Meta-Analysis of Prospective Studies. Nutrients 2022, 14, 4785. https://doi.org/10.3390/nu14224785
D’Elia L, Masulli M, Cappuccio FP, Zarrella AF, Strazzullo P, Galletti F. Dietary Potassium Intake and Risk of Diabetes: A Systematic Review and Meta-Analysis of Prospective Studies. Nutrients. 2022; 14(22):4785. https://doi.org/10.3390/nu14224785
Chicago/Turabian StyleD’Elia, Lanfranco, Maria Masulli, Francesco P. Cappuccio, Aquilino F. Zarrella, Pasquale Strazzullo, and Ferruccio Galletti. 2022. "Dietary Potassium Intake and Risk of Diabetes: A Systematic Review and Meta-Analysis of Prospective Studies" Nutrients 14, no. 22: 4785. https://doi.org/10.3390/nu14224785
APA StyleD’Elia, L., Masulli, M., Cappuccio, F. P., Zarrella, A. F., Strazzullo, P., & Galletti, F. (2022). Dietary Potassium Intake and Risk of Diabetes: A Systematic Review and Meta-Analysis of Prospective Studies. Nutrients, 14(22), 4785. https://doi.org/10.3390/nu14224785








