Obsessed with Healthy Eating: A Systematic Review of Observational Studies Assessing Orthorexia Nervosa in Patients with Diabetes Mellitus
Abstract
1. Introduction
2. Materials and Methods
2.1. Systematic Review Protocol and PIO
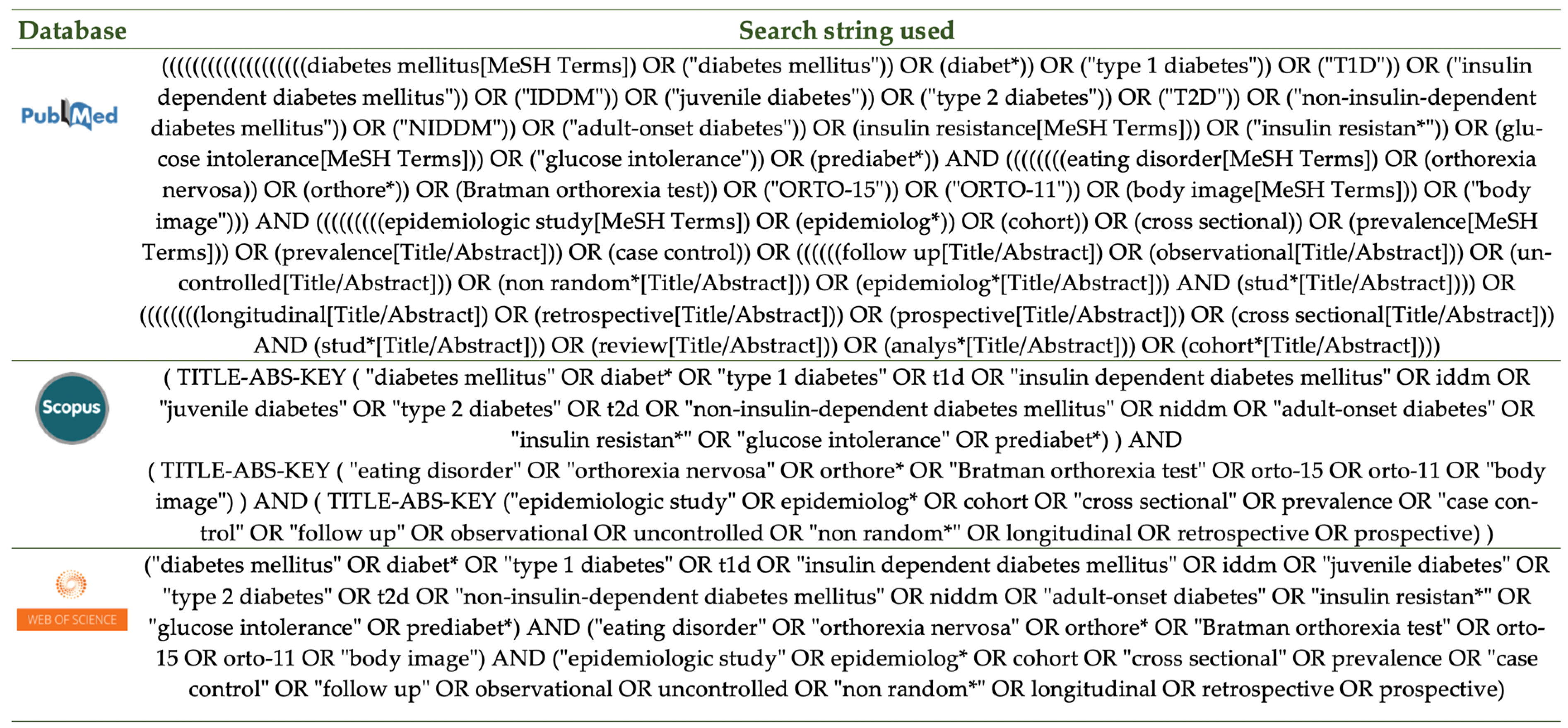
2.2. Search Strategy
2.3. Inclusion and Exclusion Criteria
2.4. Quality Assessment of the Studies
2.5. Data Extraction
2.6. Data Synthesis
3. Results
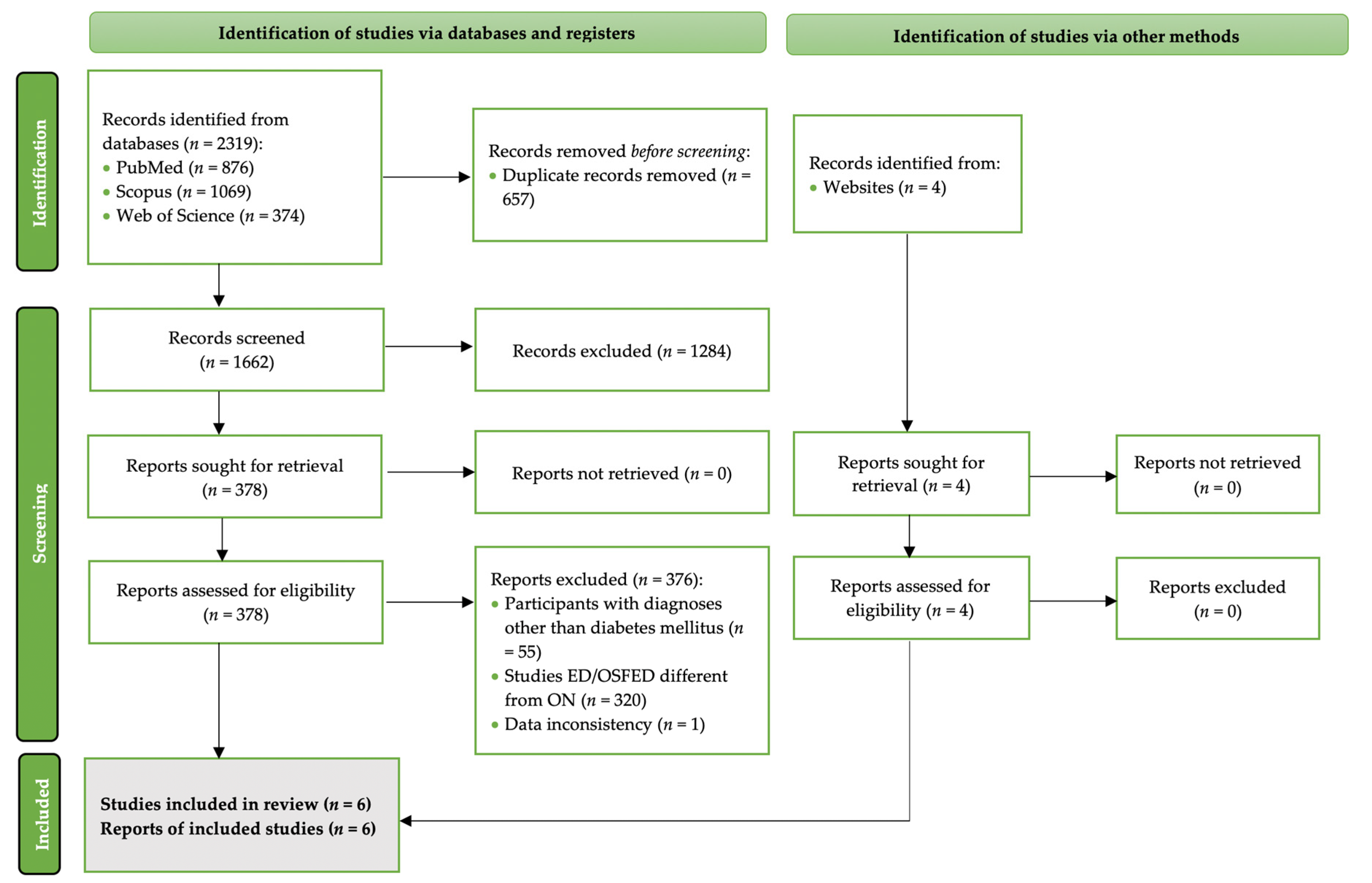
3.1. Search Results
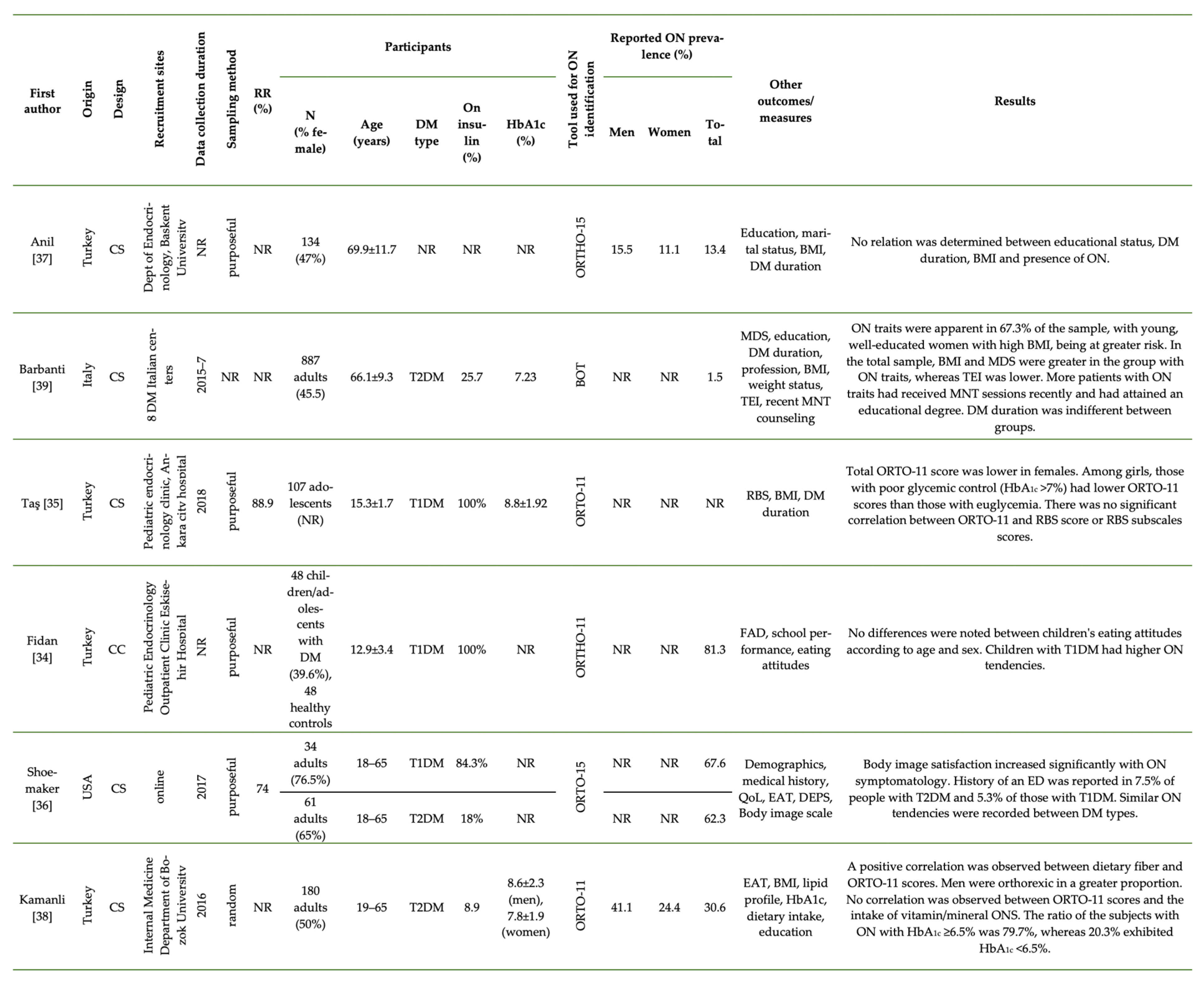
3.2. Research on ON among Patients with Prediabetes/DM
3.3. Tools Used to Identify ON Tendencies
3.4. Prevalence of ON Tendencies
3.5. Gender Differences
3.6. Body Image and Adiposity
3.7. Glycemic Control
3.8. Effect of Age
3.9. Educational Status
3.10. Dietary Intake and Supplement Use
3.11. Differences between Patients with T1DM and T2DM
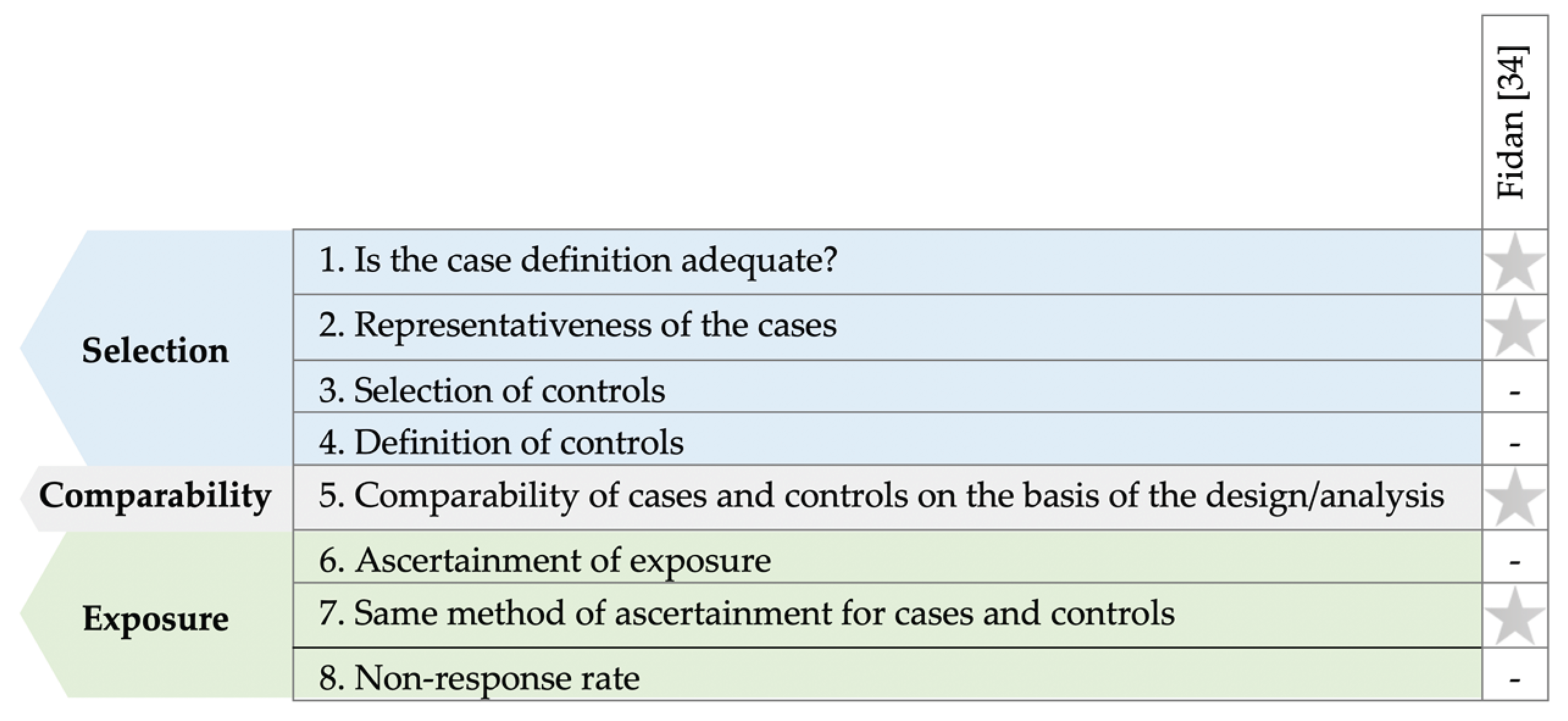
3.12. Quality of Studies
4. Discussion
4.1. Characteristics of Patients with DM and ON Tendencies
4.2. Implications for Clinical Practice
4.3. To Diagnose or Not?
4.4. Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders; American Psychiatric Association: Arlington, VA, USA, 2013; ISBN 0-89042-555-8. [Google Scholar]
- Bratman, S.; Knight, D. Health Food Junkies; Broadway Books: New York, NY, USA, 2000. [Google Scholar]
- Hanganu-Bresch, C. Orthorexia: Eating right in the context of healthism. Med. Humanit. 2020, 46, 311–322. [Google Scholar] [CrossRef] [PubMed]
- Koven, N.S.; Wabry, A. The clinical basis of orthorexia nervosa: Emerging perspectives. Neuropsychiatr. Dis. Treat. 2015, 11, 385–394. [Google Scholar] [CrossRef] [PubMed]
- Crawford, R. Healthism and the medicalization of everyday life. Int. J. Health Serv. 1980, 10, 365–388. [Google Scholar] [CrossRef] [PubMed]
- Tsirou, E.; Grammatikopoulou, M.G.; Theodoridis, X.; Gkiouras, K.; Petalidou, A.; Taousani, E.; Savvaki, D.; Tsapas, A.; Goulis, D.G. Guidelines for Medical Nutrition Therapy in Gestational Diabetes Mellitus: Systematic Review and Critical Appraisal. J. Acad. Nutr. Diet. 2019, 119, 1320–1339. [Google Scholar] [CrossRef] [PubMed]
- Katsaridis, S.; Grammatikopoulou, M.G.; Gkiouras, K.; Tzimos, C.; Papageorgiou, S.T.; Markaki, A.G.; Exiara, T.; Goulis, D.G.; Papamitsou, T. Low Reported Adherence to the 2019 American Diabetes Association Nutrition Recommendations among Patients with Type 2 Diabetes Mellitus, Indicating the Need for Improved Nutrition Education and Diet Care. Nutrients 2020, 12, 3516. [Google Scholar] [CrossRef]
- Evert, A.B.; Dennison, M.; Gardner, C.D.; Garvey, W.T.; Lau, K.H.K.; MacLeod, J.; Mitri, J.; Pereira, R.F.; Rawlings, K.; Robinson, S.; et al. Nutrition Therapy for Adults with Diabetes or Prediabetes: A Consensus Report. Diabetes Care 2019, 42, 731–754. [Google Scholar] [CrossRef]
- Rodin, G.; Olmsted, M.P.; Rydall, A.C.; Maharaj, S.I.; Colton, P.A.; Jones, J.M.; Biancucci, L.A.; Daneman, D. Eating disorders in young women with type 1 diabetes mellitus. J. Psychosom. Res. 2002, 53, 943–949. [Google Scholar] [CrossRef]
- Young-Hyman, D.L.; Davis, C.L. Disordered eating behavior in individuals with diabetes: Importance of context, evaluation, and classification. Diabetes Care 2010, 33, 683–689. [Google Scholar] [CrossRef] [PubMed]
- Abbott, S.; Dindol, N.; Tahrani, A.A.; Piya, M.K. Binge eating disorder and night eating syndrome in adults with type 2 diabetes: A systematic review. J. Eat. Disord. 2018, 6, 36. [Google Scholar] [CrossRef] [PubMed]
- García-Mayor, R.V.; García-Soidán, F.J. Eating disoders in type 2 diabetic people: Brief review. Diabetes Metab. Syndr. Clin. Res. Rev. 2017, 11, 221–224. [Google Scholar] [CrossRef]
- Pursey, K.M.; Hay, P.; Bussey, K.; Trompeter, N.; Lonergan, A.; Pike, K.M.; Mond, J.; Mitchison, D. Diabetes and disordered eating behaviours in a community-based sample of Australian adolescents. J. Eat. Disord. 2020, 8, 5. [Google Scholar] [CrossRef] [PubMed]
- Powers, M.A.; Richter, S.; Ackard, D.; Gerken, S.; Meier, M.; Criego, A. Characteristics of persons with an eating disorder and type 1 diabetes and psychological comparisons with persons with an eating disorder and no diabetes. Int. J. Eat. Disord. 2012, 45, 252–256. [Google Scholar] [CrossRef] [PubMed]
- Colton, P.A.; Olmsted, M.P.; Daneman, D.; Rydall, A.C.; Rodin, G.M. Five-year prevalence and persistence of disturbed eating behavior and eating disorders in girls with type 1 diabetes. Diabetes Care 2007, 30, 2861–2862. [Google Scholar] [CrossRef]
- Affenito, S.G.; Rodriguez, N.R.; Backstrand, J.R.; Welch, G.W.; Adams, C.H. Insulin misuse by women with type 1 diabetes mellitus complicated by eating disorders does not favorably change body weight, body composition, or body fat distribution. J. Am. Diet. Assoc. 1998, 98, 686–688. [Google Scholar] [CrossRef]
- Winston, A.P. Eating Disorders and Diabetes. Curr. Diab. Rep. 2020, 20, 32. [Google Scholar] [CrossRef] [PubMed]
- Galli-Tsinopoulou, A.; Grammatikopoulou, M.G.; Stylianou, C.; Emmanouilidou, E.; Kokka, P. Diabese youngsters have 3.7 more chances in developing metabolic syndrome compared with the obese. J. Endocrinol. Investig. 2010, 33, 549–553. [Google Scholar] [CrossRef]
- Quick, V.M.; Byrd-Bredbenner, C.; Neumark-Sztainer, D. Chronic illness and disordered eating: A discussion of the literature. Adv. Nutr. 2013, 4, 277–286. [Google Scholar] [CrossRef]
- Tate, A.E.; Liu, S.; Zhang, R.; Yilmaz, Z.; Larsen, J.T.; Petersen, L.V.; Bulik, C.M.; Svensson, A.-M.; Gudbjörnsdottir, S.; Larsson, H.; et al. Association and Familial Coaggregation of Type 1 Diabetes and Eating Disorders: A Register-Based Cohort Study in Denmark and Sweden. Diabetes Care 2021, 44, 1143–1150. [Google Scholar] [CrossRef] [PubMed]
- Baechle, C.; Castillo, K.; Straßburger, K.; Stahl-Pehe, A.; Meissner, T.; Holl, R.W.; Giani, G.; Rosenbauer, J. Is disordered eating behavior more prevalent in adolescents with early-onset type 1 diabetes than in their representative peers? Int. J. Eat. Disord. 2014, 47, 342–352. [Google Scholar] [CrossRef]
- Calcaterra, V.; Mazzoni, C.; Ballardini, D.; Tomba, E.; Zuccotti, G.V.; Mameli, C.; De Giuseppe, R.; Cena, H. Disturbed Eating Behaviors in Youth with Type 1 Diabetes: An Exploratory Study about Challenges in Diagnosis. Diagnostics 2020, 10, 1044. [Google Scholar] [CrossRef] [PubMed]
- Tokatly Latzer, I.; Rachmiel, M.; Zuckerman Levin, N.; Mazor-Aronovitch, K.; Landau, Z.; Ben-David, R.F.; GrafBar-El, C.; Gruber, N.; Levek, N.; Weiss, B.; et al. Increased prevalence of disordered eating in the dual diagnosis of type 1 diabetes mellitus and celiac disease. Pediatr. Diabetes 2018, 19, 749–755. [Google Scholar] [CrossRef] [PubMed]
- Atik Altınok, Y.; Özgür, S.; Meseri, R.; Özen, S.; Darcan, Ş.; Gökşen, D. Reliability and validity of the diabetes eating problem survey in Turkish children and adolescents with type 1 diabetes mellitus. JCRPE J. Clin. Res. Pediatr. Endocrinol. 2017, 9, 323–328. [Google Scholar] [CrossRef]
- Trace, S.E.; Baker, J.H.; Peñas-Lledó, E.; Bulik, C.M. The Genetics of Eating Disorders. Annu. Rev. Clin. Psychol. 2013, 9, 589–620. [Google Scholar] [CrossRef]
- Hübel, C.; Abdulkadir, M.; Herle, M.; Loos, R.J.F.; Breen, G.; Bulik, C.M.; Micali, N. One size does not fit all. Genomics differentiates among anorexia nervosa, bulimia nervosa, and binge-eating disorder. Int. J. Eat. Disord. 2021, 54, 785–793. [Google Scholar] [CrossRef] [PubMed]
- Duncan, L.; Yilmaz, Z.; Gaspar, H.; Walters, R.; Goldstein, J.; Anttila, V.; Bulik-Sullivan, B.; Ripke, S.; Thornton, L.; Hinney, A.; et al. Significant locus and metabolic genetic correlations revealed in genome-wide association study of anorexia nervosa. Am. J. Psychiatry 2017, 174, 850–858. [Google Scholar] [CrossRef]
- Watson, H.J.; Yilmaz, Z.; Thornton, L.M.; Hübel, C.; Coleman, J.R.; Gaspar, H.A.; Bryois, J.; Hinney, A.; Leppä, V.M.; Mattheisen, M.; et al. Genome-wide Association Study Identifies Eight Risk Loci and Implicates Metabo-Psychiatric Origins for Anorexia Nervosa. Nat. Genet. 2019, 51, 1214. [Google Scholar] [CrossRef] [PubMed]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Cooke, A.; Smith, D.; Booth, A. Beyond PICO: The SPIDER tool for qualitative evidence synthesis. Qual. Health Res. 2012, 22, 1435–1443. [Google Scholar] [CrossRef] [PubMed]
- Downes, M.J.; Brennan, M.L.; Williams, H.C.; Dean, R.S. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ Open 2016, 6, e011458. [Google Scholar] [CrossRef]
- Wells, G.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality If Nonrandomized Studies in Meta-Analyses; University of Ottawa: Ottawa, ON, Canada, 2009; Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 25 October 2021).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Fidan, T.; Orbak, Z.; Karabag, K.; Kocak, K. Orthorexia Nervosa and Family Functionality in Children and Adolescents with Type 1 Diabetes Mellitus. J. Med. Orig. Artic. 2017, 1, 1–6. [Google Scholar] [CrossRef][Green Version]
- Taş, D.; Mengen, E.; Kocaay, P.; Uçaktürk, S.A. The Effects of Risk Behaviors and Orthorexic Behavior on Glycemic Control in Adolescents with Type 1 Diabetes. J. Clin. Res. Pediatr. Endocrinol. 2020, 12, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Shoemaker, C.J. Orthorexia Nervosa Prevalence in US Adults with Type 1 and Type 2 Diabetes. Ph.D. Thesis, University of Minnesota, Minneapolis, MN, USA, 2020. [Google Scholar]
- Anil, C.; Aritici, G.; Ari, H.; Tutuncu, N.B. Prevalence of orthorexia in diabetic patients. Endocr. Abstr. 2015, 37, EP327. [Google Scholar] [CrossRef]
- Kamanli, B. TİP 2 Diyabetli Bireylerde Beslenme Durumu ve Sağlıklı Beslenme Takıntısı Arasındaki İlişkinin Değerlendirilmesi; Sağlık Bilimleri Enstitüsü, İstanbul Üniversitesi: İstanbul, Turkey, 2017. [Google Scholar]
- Barbanti, F.A.; Trento, M.; Bruno, G.; Bonadonna, R.; Croci, M.; D’Eusebio, C.; Dei Cas, A.; Invitti, C.; Merlo, F.; Pontiroli, A.E.; et al. Prevalence of orthorexic traits in type 2 diabetes mellitus: At the crossroads between nutritional counseling and eating disorders. Acta Diabetol. 2020, 57, 1117–1119. [Google Scholar] [CrossRef] [PubMed]
- Donini, L.M.; Marsili, D.; Graziani, M.P.; Imbriale, M.; Cannella, C. Orthorexia nervosa: Validation of a diagnosis questionnaire. Eat. Weight Disord. 2005, 10, e28–e32. [Google Scholar] [CrossRef]
- Niedzielski, A.; Kaźmierczak-Wojtaś, N. Prevalence of orthorexia nervosa and its diagnostic tools—A literature review. Int. J. Environ. Res. Public Health 2021, 18, 5488. [Google Scholar] [CrossRef]
- Cena, H.; Barthels, F.; Cuzzolaro, M.; Bratman, S.; Brytek-Matera, A.; Dunn, T.; Varga, M.; Missbach, B.; Donini, L.M. Definition and Diagnostic Criteria for Orthorexia Nervosa: A Narrative Review of the Literature. Eat. Weight Disord. 2019, 24, 209–246. [Google Scholar] [CrossRef] [PubMed]
- Rogoza, R.; Donini, L.M. Introducing ORTO-R: A revision of ORTO-15: Based on the re-assessment of original data. Eat. Weight Disord. 2020, 26, 887–895. [Google Scholar] [CrossRef]
- Rogowska, A.M.; Kwaśnicka, A.; Ochnik, D. Development and Validation of the Test of Orthorexia Nervosa (TON-17). J. Clin. Med. 2021, 10, 1637. [Google Scholar] [CrossRef] [PubMed]
- Oberle, C.D.; De Nadai, A.S.; Madrid, A.L. Orthorexia Nervosa Inventory (ONI): Development and validation of a new measure of orthorexic symptomatology. Eat. Weight Disord. 2020, 26, 609–622. [Google Scholar] [CrossRef] [PubMed]
- Bauer, S.M.; Fusté, A.; Andrés, A.; Saldaña, C. The Barcelona Orthorexia Scale (BOS): Development process using the Delphi method. Eat. Weight Disord. 2018, 24, 247–255. [Google Scholar] [CrossRef]
- Barthels, F.; Meyer, F.; Pietrowsky, R. Düesseldorf orthorexia scale–construction and evaluation of a questionnaire measuring orthorexic eating behavior. Z. Klin. Psychol. Psychother 2015, 44, 97–105. [Google Scholar] [CrossRef]
- Gleaves, D.H.; Graham, E.C.; Ambwani, S. Measuring “orthorexia”: Development of the Eating Habits Questionnaire. Int. J. Educ. Psychol. Assess. 2013, 12, 1–18. [Google Scholar]
- Barrada, J.R.; Roncero, M. Bidimensional Structure of the Orthorexia: Development and Initial Validation of a New Instrument. Anal. Psicol. 2018, 34, 282–290. [Google Scholar] [CrossRef]
- Dunn, T.M.; Bratman, S. On orthorexia nervosa: A review of the literature and proposed diagnostic criteria. Eat. Behav. 2016, 21, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Missbach, B.; Hinterbuchinger, B.; Dreiseitl, V.; Zellhofer, S.; Kurz, C.; König, J. When Eating Right, Is Measured Wrong! A Validation and Critical Examination of the ORTO-15 Questionnaire in German. PLoS ONE 2015, 10, e0135772. [Google Scholar] [CrossRef] [PubMed]
- Valente, M.; Brenner, R.; Cesuroglu, T.; Bunders-Aelen, J.; Syurina, E.V. ‘‘And it snowballed from there’’: The development of orthorexia nervosa from the perspective of people who self-diagnose. Appetite 2020, 155, 104840. [Google Scholar] [CrossRef]
- Pinhas-Hamiel, O.; Hamiel, U.; Levy-Shraga, Y. Eating disorders in adolescents with type 1 diabetes: Challenges in diagnosis and treatment. World J. Diabetes 2015, 6, 517. [Google Scholar] [CrossRef]
- Nicolau, J.; Simó, R.; Sanchís, P.; Ayala, L.; Fortuny, R.; Zubillaga, I.; Masmiquel, L. Eating disorders are frequent among type 2 diabetic patients and are associated with worse metabolic and psychological outcomes: Results from a cross-sectional study in primary and secondary care settings. Acta Diabetol. 2015, 52, 1037–1044. [Google Scholar] [CrossRef] [PubMed]
- Depa, J.; Barrada, J.R.; Roncero, M. Are the Motives for Food Choices Different in Orthorexia Nervosa and Healthy Orthorexia? Nutrients 2019, 11, 697. [Google Scholar] [CrossRef]
- Gramaglia, C.; Brytek-Matera, A.; Rogoza, R.; Zeppegno, P. Orthorexia and anorexia nervosa: Two distinct phenomena? A cross-cultural comparison of orthorexic behaviours in clinical and non-clinical samples. BMC Psychiatry 2017, 17, 75. [Google Scholar] [CrossRef]
- Striegel-Moore, R.H.; Rosselli, F.; Perrin, N.; DeBar, L.; Wilson, G.T.; May, A.; Kraemer, H.C. Gender difference in the prevalence of eating disorder symptoms. Int. J. Eat. Disord. 2009, 42, 471–474. [Google Scholar] [CrossRef]
- Vamado, P.J.; Williamson, D.A.; Bentz, B.G.; Ryan, D.H.; Rhodes, S.K.; O’Neil, P.M.; Sebastian, S.B.; Barker, S.E. Prevalence of binge eating disorder in obese adults seeking weight loss treatment. Eat. Weight Disord. 1997, 2, 117–124. [Google Scholar] [CrossRef]
- Hughes, E.K.; Kerr, J.A.; Patton, G.C.; Sawyer, S.M.; Wake, M.; Le Grange, D.; Azzopardi, P. Eating disorder symptoms across the weight spectrum in Australian adolescents. Int. J. Eat. Disord. 2019, 52, 885–894. [Google Scholar] [CrossRef]
- Young, V.; Eiser, C.; Johnson, B.; Brierley, S.; Epton, T.; Elliott, J.; Heller, S. Eating problems in adolescents with Type 1 diabetes: A systematic review with meta-analysis. Diabet. Med. 2013, 30, 189–198. [Google Scholar] [CrossRef]
- Mannucci, E.; Rotella, F.; Ricca, V.; Moretti, S.; Placidi, G.F.; Rotella, C.M. Eating disorders in patients with Type 1 diabetes: A meta-analysis. J. Endocrinol. Investig. 2014, 28, 417–419. [Google Scholar] [CrossRef] [PubMed]
- Troncone, A.; Cascella, C.; Chianese, A.; Zanfardino, A.; Piscopo, A.; Borriello, A.; Casaburo, F.; del Giudice, E.M.; Iafusco, D. Body Image Problems and Disordered Eating Behaviors in Italian Adolescents With and Without Type 1 Diabetes: An Examination With a Gender-Specific Body Image Measure. Front. Psychol. 2020, 11, 2547. [Google Scholar] [CrossRef]
- Araia, E.; Hendrieckx, C.; Skinner, T.; Pouwer, F.; Speight, J.; King, R.M. Gender differences in disordered eating behaviors and body dissatisfaction among adolescents with type 1 diabetes: Results from diabetes MILES youth-Australia. Int. J. Eat. Disord. 2017, 50, 1183–1193. [Google Scholar] [CrossRef]
- Troncone, A.; Chianese, A.; Zanfardino, A.; Cascella, C.; Piscopo, A.; Borriello, A.; Rollato, S.; Casaburo, F.; Testa, V.; Iafusco, D. Disordered eating behaviors in youths with type 1 diabetes during COVID-19 lockdown: An exploratory study. J. Eat. Disord. 2020, 8, 76. [Google Scholar] [CrossRef]
- Bratman, S. Orthorexia vs. theories of healthy eating. Eat. Weight Disord. 2017, 22, 381–385. [Google Scholar] [CrossRef]
- Moroze, R.M.; Dunn, T.M.; Craig Holland, J.; Yager, J.; Weintraub, P. Microthinking About Micronutrients: A Case of Transition From Obsessions About Healthy Eating to Near-Fatal “Orthorexia Nervosa” and Proposed Diagnostic Criteria. Psychosomatics 2015, 56, 397–403. [Google Scholar] [CrossRef]
- Park, S.W.; Kim, J.Y.; Go, G.J.; Jeon, E.S.; Pyo, H.J.; Kwon, Y.J. Orthorexia nervosa with hyponatremia, subcutaneous emphysema, pneumomediastinum, pneumothorax, and pancytopenia. Electrolyte Blood Press. 2011, 9, 32–37. [Google Scholar] [CrossRef]
- Mitrofanova, E.; Mulrooney, H.; Petróczi, A. Assessing psychological and nutritional impact of suspected orthorexia nervosa: A cross-sectional pilot study. J. Hum. Nutr. Diet. 2000, 34, 42–53. [Google Scholar] [CrossRef]
- Hanachi, M.; Dicembre, M.; Rives-Lange, C.; Ropers, J.; Bemer, P.; Zazzo, J.-F.; Poupon, J.; Dauvergne, A.; Melchior, J.-C. Micronutrients Deficiencies in 374 Severely Malnourished Anorexia Nervosa Inpatients. Nutrients 2019, 11, 792. [Google Scholar] [CrossRef]
- Tarı Selçuk, K.; Çevik, C. Use of dietary supplements among nursing students in Turkey in the last 12 months and its relation with orthorexia nervosa. Perspect. Psychiatr. Care 2020, 56, 885–893. [Google Scholar] [CrossRef]
- Oberle, C.D.; Klare, D.L.; Patyk, K.C. Health beliefs, behaviors, and symptoms associated with orthorexia nervosa. Eat. Weight Disord. 2019, 24, 495–506. [Google Scholar] [CrossRef]
- Larrañaga, A.; Docet, M.F.; García-Mayor, R.V. Disordered eating behaviors in type 1 diabetic patients. World J. Diabetes 2011, 2, 189–195. [Google Scholar] [CrossRef]
- Nieto-Martínez, R.; González-Rivas, J.P.; Medina-Inojosa, J.R.; Florez, H. Are Eating Disorders Risk Factors for Type 2 Diabetes? A Systematic Review and Meta-analysis. Curr. Diab. Rep. 2017, 17, 138. [Google Scholar] [CrossRef]
- Hendrieckx, C.; Halliday, J.; Beeney, L.; Speight, J. Diabetes and Emotional Health: A Practical Guide for Healthcare Professionals Supporting Adults with Type 1 and Type 2 Diabetes, 2nd ed.; Diabetes UK: London, UK, 2019. [Google Scholar]
- Vist, G.E.; Reinar, L.M.; Straumann, G.H.; Wisting, L. Treatment of Persons who Suffer from Both an Eating Disorder and Diabetes; Knowledge Centre for the Health Services at The Norwegian Institute of Public Health (NIPH): Oslo, Norway, 2015; ISBN 9788281219700. [Google Scholar]
- Zickgraf, H.F. Treatment of pathologic healthy eating (orthorexia nervosa). In Advanced Casebook of Obsessive-Compulsive and Related Disorders: Conceptualizations and Treatment; Storch, E.A., McKay, D., Abramowitz , J.S., Eds.; Elsevier Academic Press: London, UK, 2020; pp. 21–40. ISBN 9780128165638. [Google Scholar]
- Cuzzolaro, M.; Donini, L.M. Orthorexia nervosa by proxy? Eat. Weight Disord. 2016, 21, 549–551. [Google Scholar] [CrossRef]
- Ryman, F.V.M.; Cesuroglu, T.; Bood, Z.M.; Syurina, E.V. Orthorexia Nervosa: Disorder or Not? Opinions of Dutch Health Professionals. Front. Psychol. 2019, 10, 555. [Google Scholar] [CrossRef]

| Population | Patients with prediabetes or diabetes mellitus (T1DM/T2DM) |
| Issue | Orthorexia nervosa |
| Outcomes | Symptoms, glycemic control. |
| Sample | Patients with Prediabetes or DM (T1DM/T2DM) of Any Age |
|---|---|
| Phenomenon of Interest | ON measures, tendencies, prevalence and correlates |
| Design | Original published research (any design, with emphasis on cross-sectional studies), including grey literature |
| Evaluation | Characteristics, views, experiences, prevalence |
| Research type | Quantitative and mixed methods peer-reviewed studies; grey literature including third-sector and government reports and briefings, educational theses, conference proceedings |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grammatikopoulou, M.G.; Gkiouras, K.; Polychronidou, G.; Kaparounaki, C.; Gkouskou, K.K.; Magkos, F.; Donini, L.M.; Eliopoulos, A.G.; Goulis, D.G. Obsessed with Healthy Eating: A Systematic Review of Observational Studies Assessing Orthorexia Nervosa in Patients with Diabetes Mellitus. Nutrients 2021, 13, 3823. https://doi.org/10.3390/nu13113823
Grammatikopoulou MG, Gkiouras K, Polychronidou G, Kaparounaki C, Gkouskou KK, Magkos F, Donini LM, Eliopoulos AG, Goulis DG. Obsessed with Healthy Eating: A Systematic Review of Observational Studies Assessing Orthorexia Nervosa in Patients with Diabetes Mellitus. Nutrients. 2021; 13(11):3823. https://doi.org/10.3390/nu13113823
Chicago/Turabian StyleGrammatikopoulou, Maria G., Konstantinos Gkiouras, Georgia Polychronidou, Chrysi Kaparounaki, Kalliopi K. Gkouskou, Faidon Magkos, Lorenzo Maria Donini, Aristides G. Eliopoulos, and Dimitrios G. Goulis. 2021. "Obsessed with Healthy Eating: A Systematic Review of Observational Studies Assessing Orthorexia Nervosa in Patients with Diabetes Mellitus" Nutrients 13, no. 11: 3823. https://doi.org/10.3390/nu13113823
APA StyleGrammatikopoulou, M. G., Gkiouras, K., Polychronidou, G., Kaparounaki, C., Gkouskou, K. K., Magkos, F., Donini, L. M., Eliopoulos, A. G., & Goulis, D. G. (2021). Obsessed with Healthy Eating: A Systematic Review of Observational Studies Assessing Orthorexia Nervosa in Patients with Diabetes Mellitus. Nutrients, 13(11), 3823. https://doi.org/10.3390/nu13113823









