The Effect of Coffee and Caffeine Consumption on Patients with Multiple Sclerosis-Related Fatigue
Abstract
1. Introduction
2. Methods
2.1. Participants
2.2. Data Collection
2.3. Data Analysis
3. Results
3.1. Characteristics of Patients with MS
3.2. EDSS
3.3. Fatigue
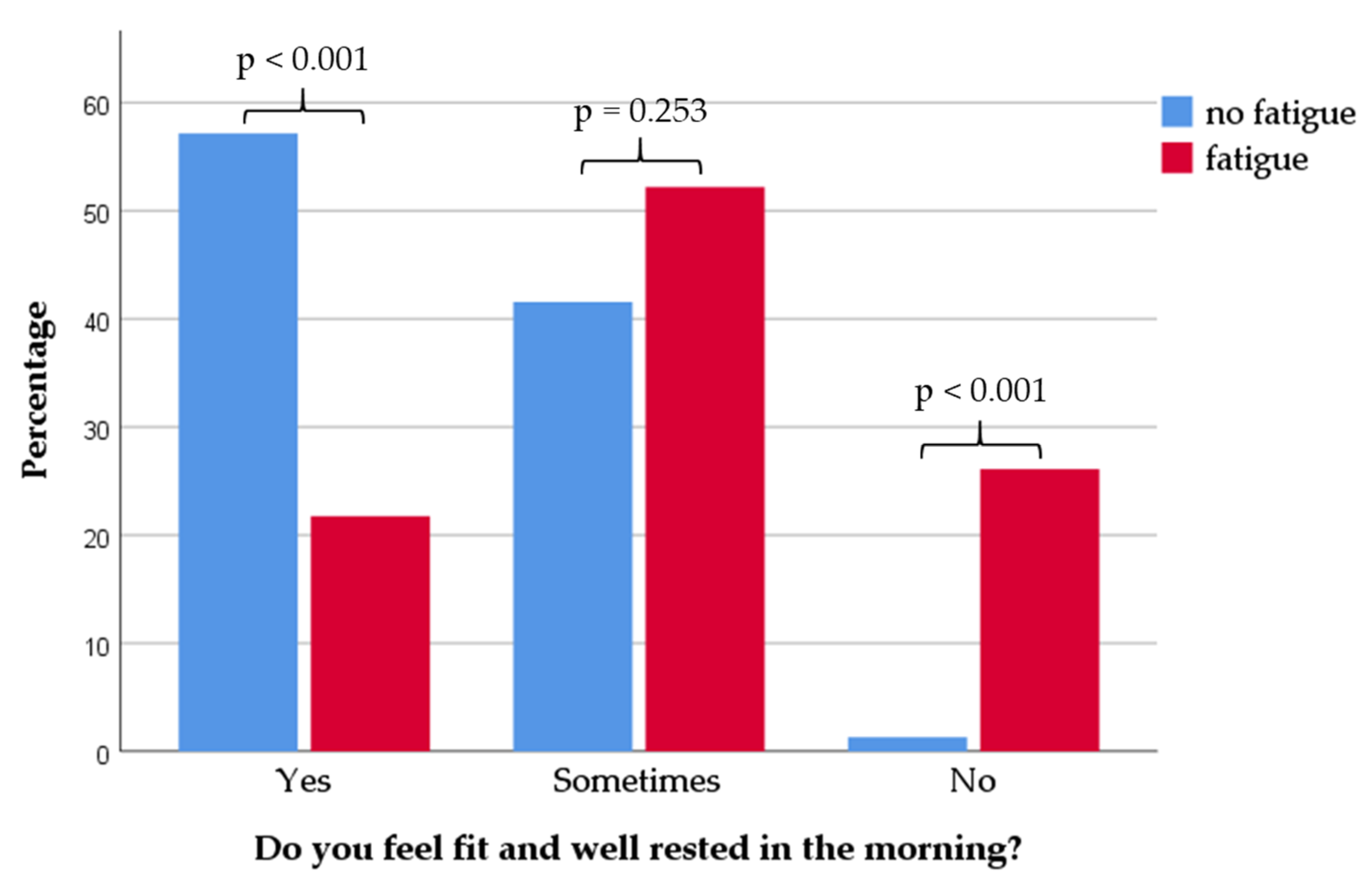
3.4. Sleep Characteristics
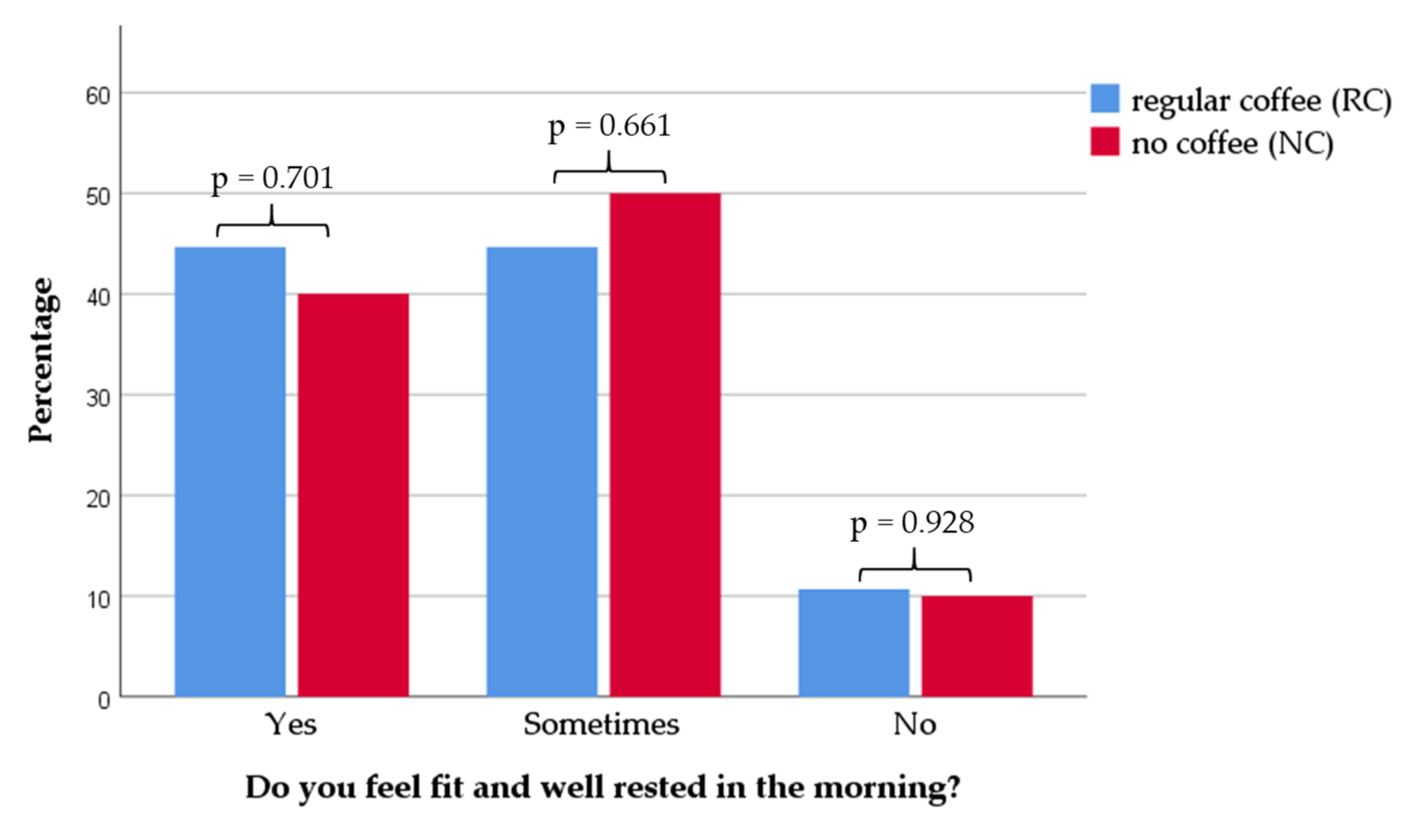
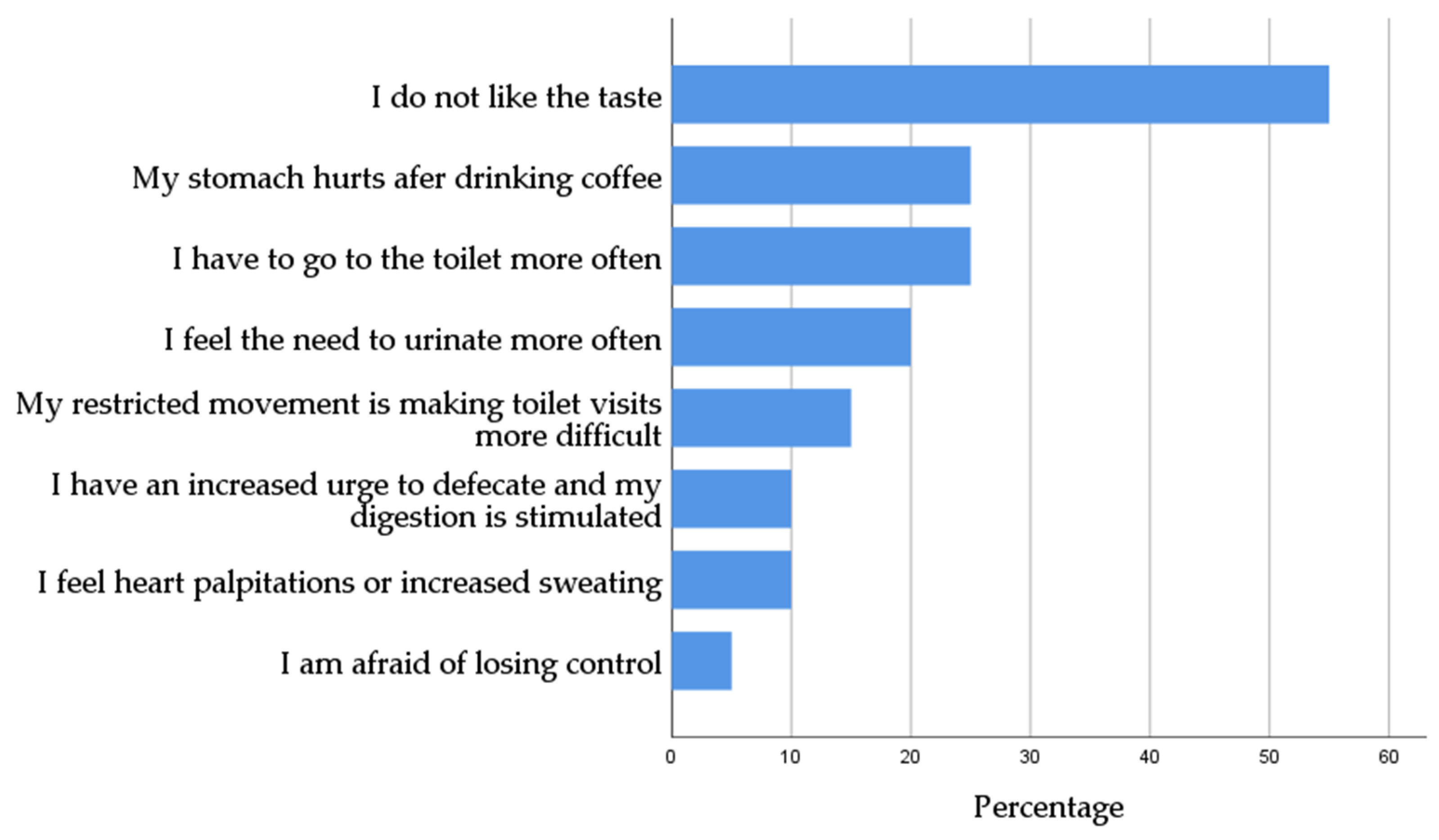
3.5. Coffee Habits
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Weissert, R. The immune pathogenesis of multiple sclerosis. J. Neuroimmune Pharm. 2013, 8, 857–866. [Google Scholar] [CrossRef] [PubMed]
- Goverman, J. Autoimmune T cell responses in the central nervous system. Nat. Rev. Immunol. 2009, 9, 393–407. [Google Scholar] [CrossRef] [PubMed]
- Lublin, F.D.; Reingold, S.C. Defining the clinical course of multiple sclerosis. Neurology 2014, 83, 278–286. [Google Scholar] [CrossRef]
- Thompson, A.J.; Banwell, B.L.; Barkhof, F.; Carroll, W.M.; Coetzee, T.; Comi, G.; Correale, J.; Fazekas, F.; Filippi, M.; Freedman, M.S.; et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 2018, 17, 162–173. [Google Scholar] [CrossRef]
- Popp, R.F.J.; Fierlbeck, A.K.; Knüttel, H.; König, N.; Rupprecht, R.; Weissert, R.; Wetter, T.C. Daytime sleepiness versus fatigue in patients with multiple sclerosis: A systematic review on the Epworth sleepiness scale as an assessment tool. Sleep Med. Rev. 2017, 32, 95–108. [Google Scholar] [CrossRef]
- Mills, R.J.; Young, C.A. A medical definition of fatigue in multiple sclerosis. QJM 2008, 101, 49–60. [Google Scholar] [CrossRef]
- Iriarte, J.; Subirá, M.L.; Castro, P. Modalities of fatigue in multiple sclerosis: Correlation with clinical and biological factors. Mult. Scler. J. 2000, 6, 124–130. [Google Scholar] [CrossRef]
- Fisk, J.D.; Pontefract, A.; Ritvo, P.G.; Archibald, C.J.; Murray, T.J. The Impact of Fatigue on Patients with Multiple Sclerosis. Can. J. Neurol. Sci. 1994, 21, 9–14. [Google Scholar] [CrossRef]
- Hadjimichael, O.; Vollmer, T.; Oleen-Burkey, M. Fatigue characteristics in multiple sclerosis: The North American Research Committee on Multiple Sclerosis (NARCOMS) survey. Health Qual. Life Outcomes 2008, 6, 100. [Google Scholar] [CrossRef]
- Koziarska, D.; Król, J.; Nocoń, D.; Kubaszewski, P.; Rzepa, T.; Nowacki, P. Prevalence and factors leading to unemployment in MS (multiple sclerosis) patients undergoing immunomodulatory treatment in Poland. PLoS ONE 2018, 13, e0194117. [Google Scholar] [CrossRef]
- Krupp, L.B.; LaRocca, N.; Muir-Nash, J.; Steinberg, A. The fatigue severity scale: Application to patients with multiple sclerosis ans systemic lupus erythematosus. Arch. Neurol. 1989, 46, 1121–1123. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.M.; Arnett, P.A. Factors related to employment status changes in individuals with multiple sclerosis. Mult. Scler. 2005, 11, 602–609. [Google Scholar] [CrossRef] [PubMed]
- Veauthier, C.; Paul, F. Therapie der Fatigue bei Multipler Sklerose: Ein Behandlungsalgorithmus. Nervenarzt 2016, 87, 1310–1321. [Google Scholar] [CrossRef] [PubMed]
- Krupp, L.B. Fatigue in multiple sclerosis: Definition, Pathophysiology and Treatment. CNS Drugs. 2003, 17, 225–234. [Google Scholar] [CrossRef]
- Hameleers, P. Habitual caffeine consumption and its relation to memory, attention, planning capacity and psychomotor performance across multiple age groups. Hum. Psychopharmacol. Clin. Exp. 2000, 15, 573–581. [Google Scholar] [CrossRef]
- Bonati, M.; Latini, R.; Galletti, F.; Young, J.F.; Tognoni, G.; Garattini, S. Caffeine disposition after oral doses. Clin. Pharmacol. Ther. 1982, 32, 98–106. [Google Scholar] [CrossRef]
- Marks, V.; Kelly, J.F. Absorption of caffeine from tea, coffee and coca cola. Lancet 1973, 1, 827. [Google Scholar] [CrossRef]
- Blanchard, J.; Sawers, S.J.A. The absolute bioavailability of caffeine in man. Eur. J. Clin. Pharmacol. 1983, 24, 93–98. [Google Scholar] [CrossRef]
- Fisone, G.; Borgkvist, A.; Usiello, A. Caffeine as a psychomotor stimulant: Mechanism of action. Cell. Mol. Life Sci. 2004, 61, 857–872. [Google Scholar] [CrossRef]
- Hauher, W. Adenosin: Ein Purinnukleosid mit neuromodulatorischen Wirkungen. E-Neuroforum 2002, 8, 228–334. [Google Scholar] [CrossRef]
- McLellan, T.M.; Caldwell, J.A.; Lieberman, H.R. A review of caffeine’s effects on cognitive, physical and occupational performance. Neurosci. Biobehav. Rev. 2016, 71, 294–312. [Google Scholar] [CrossRef] [PubMed]
- Nieber, K. The Impact of Coffee on Health. Planta Med. 2017, 83, 1256–1263. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, J.J.; Mestre, T.; Guedes, L.C.; Coelho, M.; Rosa, M.M.; Santos, A.T.; Barra, M.; Sampaio, C.; Rascol, O. Espresso Coffee for the Treatment of Somnolence in Parkinson’s Disease: Results of n-of-1 Trials. Front. Neurol. 2016, 7, 455. [Google Scholar] [CrossRef]
- Johns, M.W. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep 1991, 14, 540–545. [Google Scholar] [CrossRef] [PubMed]
- Kurtzke, J.F. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology 1983, 33, 1444–1452. [Google Scholar] [CrossRef] [PubMed]
- Krupp, L.B.; Coyle, P.K.; Doscher, C.; Miller, A.; Cross, A.H.; Jandorf, L.; Halper, J.; Johnson, B.; Morgante, L.; Grimson, R. Fatigue therapy in multiple sclerosis: Results of a double-blind, randomized, parallel trial of amantadine, pemoline, and placebo. Neurology 1995, 45, 1956–1961. [Google Scholar] [CrossRef]
- Patrick, E.; Christodoulou, C.; Krupp, L.B. Longitudinal correlates of fatigue in multiple sclerosis. Mult. Scler. 2009, 15, 258–261. [Google Scholar] [CrossRef]
- Čarnická, Z.; Kollár, B.; Šiarnik, P.; Krížová, L.; Klobučníková, K.; Turčáni, P. Sleep disorders in patients with multiple sclerosis. J. Clin. Sleep Med. 2015, 11, 553–557. [Google Scholar] [CrossRef]
- Bamer, A.M.; Johnson, K.L.; Amtmann, D.; Kraft, G.H. Prevalence of sleep problems in individuals with multiple sclerosis. Mult. Scler. 2008, 14, 1127–1130. [Google Scholar] [CrossRef]
- Tachibana, N.; Howard, R.S.; Hirsch, N.P.; Miller, D.H.; Moseley, I.F.; Fish, D. Sleep problems in multiple sclerosis. Eur. Neurol. 1994, 34, 320–323. [Google Scholar] [CrossRef]
- Sadeghi Bahmani, D.; Gonzenbach, R.; Motl, R.W.; Bansi, J.; Rothen, O.; Niedermoser, D.; Gerber, M.; Brand, S. Better Objective Sleep Was Associated with Better Subjective Sleep and Physical Activity; Results from an Exploratory Study under Naturalistic Conditions among Persons with Multiple Sclerosis. Int. J. Environ. Res. Public Health 2020, 17, 3522. [Google Scholar] [CrossRef] [PubMed]
- Herden, L.; Weissert, R. The Impact of Coffee and Caffeine on Multiple Sclerosis Compared to Other Neurodegenerative Diseases. Front. Nutr. 2018, 5, 133. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.Q.; Chen, Y.Y.; Wang, X.S.; Wu, S.Z.; Yang, H.M.; Xu, H.Q.; He, J.C.; Wang, X.T.; Chen, J.F.; Zheng, R.Y. Chronic caffeine treatment attenuates experimental autoimmune encephalomyelitis induced by guinea pig spinal cord homogenates in Wistar rats. Brain Res. 2010, 1309, 116–125. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Xi, N.-n.; Chen, Y.; Shang, X.-f.; Hu, Q.; Chen, J.-F.; Zheng, R.-y. Chronic caffeine treatment protects against experimental autoimmune encephalomyelitis in mice: Therapeutic window and receptor subtype mechanism. Neuropharmacology 2014, 86, 203–211. [Google Scholar] [CrossRef] [PubMed]
- Haskell-Ramsay, C.F.; Jackson, P.A.; Forster, J.S.; Dodd, F.L.; Bowerbank, S.L.; Kennedy, D.O. The Acute Effects of Caffeinated Black Coffee on Cognition and Mood in Healthy Young and Older Adults. Nutrients 2018, 10, 1386. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, R.M.; Marshman, J.A.; Schwieder, M.; Berg, R. Caffeine content of beverages as consumed. Can. Med. Assoc. J. 1976, 114, 205–208. [Google Scholar]
- Luerding, R.; Gebel, S.; Gebel, E.M.; Schwab-Malek, S.; Weissert, R. Influence of Formal Education on Cognitive Reserve in Patients with Multiple Sclerosis. Front. Neurol. 2016, 7, 46. [Google Scholar] [CrossRef]
- Santangelo, G.; Altieri, M.; Gallo, A.; Trojano, L. Does cognitive reserve play any role in multiple sclerosis? A meta-analytic study. Mult. Scler. Relat. Disord. 2019, 30, 265–276. [Google Scholar] [CrossRef]
- Artemiadis, A.; Bakirtzis, C.; Ifantopoulou, P.; Zis, P.; Bargiotas, P.; Grigoriadis, N.; Hadjigeorgiou, G. The role of cognitive reserve in multiple sclerosis: A cross-sectional study in 526 patients. Mult. Scler. Relat. Disord. 2020, 41, 102047. [Google Scholar] [CrossRef]
- Ifantopoulou, P.; Artemiadis, A.K.; Bakirtzis, C.; Zekiou, K.; Papadopoulos, T.-S.; Diakogiannis, I.; Hadjigeorgiou, G.; Grigoriadis, N.; Orologas, A. Cognitive and brain reserve in multiple sclerosis—A cross-sectional study. Mult. Scler. Relat. Disord. 2019, 35, 128–134. [Google Scholar] [CrossRef]
- Fisniku, L.K.; Brex, P.A.; Altmann, D.R.; Miszkiel, K.A.; Benton, C.E.; Lanyon, R.; Thompson, A.J.; Miller, D.H. Disability and T2 MRI lesions: A 20-year follow-up of patients with relapse onset of multiple sclerosis. Brain 2008, 131, 808–817. [Google Scholar] [CrossRef] [PubMed]
- Luchetti, S.; Fransen, N.L.; van Eden, C.G.; Ramaglia, V.; Mason, M.; Huitinga, I. Progressive multiple sclerosis patients show substantial lesion activity that correlates with clinical disease severity and sex: A retrospective autopsy cohort analysis. Acta Neuropathol. 2018, 135, 511–528. [Google Scholar] [CrossRef] [PubMed]
- Shinoda, K.; Matsushita, T.; Nakamura, Y.; Masaki, K.; Sakai, S.; Nomiyama, H.; Togao, O.; Hiwatashi, A.; Niino, M.; Isobe, N.; et al. Contribution of cortical lesions to cognitive impairment in Japanese patients with multiple sclerosis. Sci. Rep. 2020, 10, 5228. [Google Scholar] [CrossRef] [PubMed]
- Bakshi, R.; Miletich, R.S.; Henschel, K.; Shaikh, Z.A.; Janardhan, V.; Wasay, M.; Stengel, L.M.; Ekes, R.; Kinkel, P.R. Fatigue in multiple sclerosis: Cross-sectional correlation with brain MRI findings in 71 patients. Neurology 1999, 53, 1151–1153. [Google Scholar] [CrossRef] [PubMed]
- Niepel, G.; Tench, C.R.; Morgan, P.S.; Evangelou, N.; Auer, D.P.; Constantinescu, C.S. Deep gray matter and fatigue in MS: A T1 relaxation time study. J. Neurol. 2006, 253, 896–902. [Google Scholar] [CrossRef]
- Chen, M.H.; Wylie, G.R.; Sandroff, B.M.; Dacosta-Aguayo, R.; DeLuca, J.; Genova, H.M. Neural mechanisms underlying state mental fatigue in multiple sclerosis: A pilot study. J. Neurol. 2020, 267, 2372–2382. [Google Scholar] [CrossRef]
- Möller, F.; Poettgen, J.; Broemel, F.; Neuhaus, A.; Daumer, M.; Heesen, C. HAGIL (Hamburg Vigil Study): A randomized placebo-controlled double-blind study with modafinil for treatment of fatigue in patients with multiple sclerosis. Mult. Scler. 2011, 17, 1002–1009. [Google Scholar] [CrossRef]
- Stankoff, B.; Waubant, E.; Confavreux, C.; Edan, G.; Debouverie, M.; Rumbach, L.; Moreau, T.; Pelletier, J.; Lubetzki, C.; Clanet, M. Modafinil for fatigue in MS: A randomized placebo-controlled double-blind study. Neurology 2005, 64, 1139–1143. [Google Scholar] [CrossRef] [PubMed]
- Lange, R.; Volkmer, M.; Heesen, C.; Liepert, J. Modafinil effects in multiple sclerosis patients with fatigue. J. Neurol. 2009, 256, 645–650. [Google Scholar] [CrossRef]
- Asano, M.; Finlayson, M.L. Meta-analysis of three different types of fatigue management interventions for people with multiple sclerosis: Exercise, education, and medication. Mult. Scler. Int. 2014, 2014, 798285. [Google Scholar] [CrossRef]
- Steimer, J.; Weissert, R. Effects of Sport Climbing on Multiple Sclerosis. Front. Physiol. 2017, 8, 1021. [Google Scholar] [CrossRef] [PubMed]
| All (n = 124) | Fatigue (n = 46) | No Fatigue (n = 78) | p-Value | ||
|---|---|---|---|---|---|
| Age (y) | |||||
| Median (r) | 46 (18–80) | 49 (20–80) | 45 (18–64) | 0.116 | |
| Sex | |||||
| Female (%) | 79 (63.7) | 29 (63.0) | 50 (64.1) | 0.906 | |
| Male (%) | 45 (36.3) | 17 (37.0) | 28 (35.9) | ||
| Diagnosis | |||||
| RRMS (%) | 85 (68.5) | 29 (63.0) | 56 (71.8) | 0.177 | |
| PPMS (%) | 12 (9.7) | 8 (17.4) | 4 (5.1) | ||
| SPMS (%) | 14 (11.3) | 6 (13.0) | 8 (10.3) | ||
| Initial diagnosis (%) | 6 (4.8) | 2 (4.3) | 5 (6.4) | ||
| Unspecified (%) | 7 (5.6) | 1 (2.2) | 5 (6.4) | ||
| Duration of disease | |||||
| Mean (y) ± SD | 10.45 ± 9.3 | 11.28 ± 9.4 | 10.15 ± 9.6 | 0.532 | |
| EDSS (n = 120) | |||||
| Median (r) | 2.5 (0–8.5) | 2.0 (0–8.5) | 3.0 (0–8.5) | 0.003 | |
| Working status | |||||
| Working (%) | 81 (65.3) | 20 (43.5) | 61 (78.2) | <0.001 | |
| Not Working (%) | 43 (34.7) | 26 (56.5) | 17 (21.8) | ||
| Coffee consumption (cups/day) | |||||
| 0 cups (%) | 14 (11.3) | 7 (15.2) | 7 (9.0) | 0.606 | |
| <2 cups (%) | 48 (38.7) | 15 (32.6) | 33 (42.3) | ||
| 2 to 4 cups (%) | 48 (38.7) | 19 (41.3) | 29 (37.2) | ||
| >4 cups (%) | 14 (11.3) | 5 (10.9) | 9 (11.5) | ||
| Frequency, n (%) | Mean Age (y) | Duration of Disease (y) | ||
|---|---|---|---|---|
| Groups (n/%) | EDSS = 0 | 37 (29.8) | 34.8 ± 10.2 | 5.9 ± 6.1 |
| EDSS < 4 | 54 (43.6) | 44.7 ± 11.6 | 9.1 ±7.7 | |
| EDSS ≥ 4 | 33 (26.6) | 53.4 ± 11.5 | 17.4 ± 11.1 | |
| Total | 124 (100.0) | 44.1 ± 13.1 | 10.6 ± 9.5 | |
| No Fatigue (n = 78) | Fatigue (n = 46) | |||||
|---|---|---|---|---|---|---|
| “I need the coffee to start the day fitter in the morning” | ||||||
| Yes | 36 (46.2%) | 22 (47.8%) | ||||
| No | 42 (53.8%) | 24 (52.2%) | ||||
| “I am taking deliberate breaks“ | ||||||
| Yes | 37 (47.4%) | 19 (41.3%) | ||||
| No | 41 (52.6%) | 27 (58.7%) | ||||
| “I feel more active, so I get a little more exercise in my day” | ||||||
| Yes | 22 (28.2%) | 9 (19.6%) | ||||
| No | 56 (71.8%) | 37 (80.4%) | ||||
| “I have more strength to assert myself in difficult situations and feel more competent in everyday life as well” | ||||||
| Yes | 4 (5.1%) | 4 (8.7%) | ||||
| No | 74 (94.9%) | 42 (91.3%) | ||||
| “I can concentrate better and thus fulfill my tasks” | ||||||
| Yes | 13 (16.7%) | 11 (23.9%) | ||||
| No | 65 (83.3%) | 35 (76.1%) | ||||
| “I can lengthen my attention span and listen more attentively to conversations” | ||||||
| Yes | 10 (12.8%) | 7 (15.2%) | ||||
| No | 68 (87.2%) | 39 (84.8%) | ||||
| “I drink coffee from the “custom” of going out for coffee with someone, e.g., to get to know someone or meet a friend again” | ||||||
| Yes | 29 (37.2%) | 13 (28.3%) | ||||
| No | 49 (62.8%) | 33 (71.7%) | ||||
| “It stimulates my digestion and I notice that I have to go to the toilet more often and more regularly” | ||||||
| Yes | 22 (28.2%) | 11 (23.9%) | ||||
| No | 56 (71.8%) | 35 (76.1%) | ||||
| “I feel my heart beating faster or I’m shaking or sweating afterwards” | ||||||
| Yes | 3 (3.8%) | 4 (8.7%) | ||||
| No | 75 (96.2%) | 42 (91.3%) | ||||
| “I get heartburn or stomachache” | ||||||
| Yes | 3 (3.8%) | 1 (2.2%) | ||||
| No | 75 (96.2%) | 45 (97.8%) | ||||
| “I feel no effect” | ||||||
| Yes | 21 (26.9%) | 11 (23.9%) | ||||
| No | 57 (73.1%) | 35 (76.1%) | ||||
| All | Problem | No Problem | p-Value | |
|---|---|---|---|---|
| Problems with falling asleep | n = 124 | n = 34 | n = 90 | |
| Lay awake (h) | 0.5 ± 0.94 | 1.86 ± 0.93 | 0.4 ± 0.17 | <0.001 |
| Coffee consumption (mean in cups) | 2.67 ± 2.08 | 2.98 ± 2.13 | 2.55 ± 2.06 | 0.316 |
| ESS (median + range) | 7 (0–18) | 8.5 (0–18) | 6 (0–18) | 0.013 |
| Problems with sleeping through the night | n = 124 | n = 66 | n = 58 | |
| Frequency of waking up (median + range) | 1 (0–4) | 2 (0–4) | 0 (0–1) | <0.001 |
| Regular coffee consumption (%) | 83.9 | 80.3 | 87.9 | 0.249 |
| Coffee consumption (mean in cups) | 2.67 ± 2.08 | 3.02 ± 2.33 | 2.28 ± 1.69 | 0.051 |
| Time of Coffee Consumption | n | % |
|---|---|---|
| In the morning (until 12 p.m.) | 24 | 19.4 |
| In the afternoon (12 p.m. to 6 p.m.) | 5 | 4 |
| In the evening (after 6 p.m.) | 0 | 0 |
| In the morning and afternoon (until 6 p.m.) | 70 | 56.5 |
| In the morning and evening (until 12 p.m. and after 6 p.m.) | 1 | 0.8 |
| Whole day (in the morning, afternoon, and evening) | 9 | 7.3 |
| Never | 15 | 12.0 |
| EDSS = 0 (n = 37) | EDSS < 4 (n = 54) | EDSS ≥ 4 (n = 33) | p-Value | ||
|---|---|---|---|---|---|
| “I need the coffee to start the day fitter in the morning” | |||||
| Yes | 12 (32.4) | 31(57.4%) | 15 (45.5%) | 0.079 | |
| No | 25 (67.6%) | 23 (42.6%) | 18 (54.5%) | ||
| “I am taking deliberate breaks” | |||||
| Yes | 18 (48.6%) | 29 (53.7%) | 9 (27.3%) | 0.049 | |
| No | 19 (51.4%) | 25 (46.3%) | 24 (72.7%) | ||
| “I feel more active, so I get a little more exercise in my day.” | |||||
| Yes | 6 (16.2%) | 13 (24.1%) | 12 (36.4%) | 0.151 | |
| No | 31 (83.8%) | 41 (75.9%) | 21 (63.6%) | ||
| “I have more strength to assert myself in difficult situations and feel more competent in everyday life as well” | |||||
| Yes | 2 (5.4%) | 3 (5.6%) | 3 (9.1%) | 0.771 | |
| No | 35 (94.6%) | 51 (94.4%) | 30 (90.0%) | ||
| “I can concentrate better and thus fulfill my tasks” | |||||
| Yes | 2 (5.4%) | 18 (33.3%) | 4 (12.1%) | 0.002 | |
| No | 35 (94.6%) | 36 (66.7%) | 29 (87.9%) | ||
| “I can lengthen my attention span and listen more attentive in conversations” | |||||
| Yes | 3 (8.1%) | 13 (24.1%) | 1 (3.0%) | 0.011 | |
| No | 34 (91.9%) | 41 (75.9%) | 32 (97.0%) | ||
| “I drink coffee from the ‘custom’ of going out for coffee with someone, e.g., to get to know someone or meet a friend again” | |||||
| Yes | 12 (32.4%) | 18 (33.3%) | 12 (36.4%) | 0.936 | |
| No | 25 (67.6%) | 36 (66.7%) | 21 (63.6%) | ||
| “It stimulates my digestion and I notice that I have to go to the toilet more often and more regularly” | |||||
| Yes | 7 (18.9%) | 19 (35.2%) | 7 (21.2%) | 0.162 | |
| No | 30 (81.1%) | 35 (64.8%) | 26 (78.8%) | ||
| “I feel my heart beating faster or I’m shaking or sweating afterwards” | |||||
| Yes | 3 (8.1%) | 3 (5.6%) | 1 (3.0%) | 0.671 | |
| No | 34 (91.9%) | 51 (94.4%) | 32 (97.0%) | ||
| “I get heartburn or stomachache” | |||||
| Yes | 3 (8.1%) | 0(0.0%) | 1 (3.0%) | 0,101 | |
| No | 34 (91.9%) | 54 (100.0%) | 32 (97.0%) | ||
| “I feel no effect” | |||||
| Yes | 8 (21.6%) | 14 (25.9%) | 10 (30.3%) | 0.661 | |
| No | 29 (78.4%) | 40 (74.1%) | 23 (69.7%) | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Herden, L.; Weissert, R. The Effect of Coffee and Caffeine Consumption on Patients with Multiple Sclerosis-Related Fatigue. Nutrients 2020, 12, 2262. https://doi.org/10.3390/nu12082262
Herden L, Weissert R. The Effect of Coffee and Caffeine Consumption on Patients with Multiple Sclerosis-Related Fatigue. Nutrients. 2020; 12(8):2262. https://doi.org/10.3390/nu12082262
Chicago/Turabian StyleHerden, Lena, and Robert Weissert. 2020. "The Effect of Coffee and Caffeine Consumption on Patients with Multiple Sclerosis-Related Fatigue" Nutrients 12, no. 8: 2262. https://doi.org/10.3390/nu12082262
APA StyleHerden, L., & Weissert, R. (2020). The Effect of Coffee and Caffeine Consumption on Patients with Multiple Sclerosis-Related Fatigue. Nutrients, 12(8), 2262. https://doi.org/10.3390/nu12082262






