In 2002, the Working Group for Echocardiography of the Swiss Society of Cardiology Awards, with the support of Menarini Switzerland, created a prize to promote echocardiography and support young cardiologists in Switzerland. It is awarded each year to the first author of the best abstracts presented at the annual scientific meeting of the SSC, after assessment and grading by an independent scientific committee.
This year in Basel, on June 6–8 2006, the Menarini Prize was awarded to:
- ‒
- 1st Prize: Dr. P. Luthi, Zurich
- ‒
- 2nd Prize: Dr. C. Jansen, Basel
- ‒
- 3rd Prize: Dr. Haran Burri, Genève
The three laureates were invited to present their work as an abstract in Kardiovaskuläre Medizin.
Systolic and Diastolic Function in Former Professional Cyclists After Long-Term Deconditioning of More than 30 Years
- P. Luthia, M. Zuberb, M. Rittere, E. N. Oechslind, R. Jennia, B. Seifertf, S. Baldesbergera, C. Attenhofer Jostc
- a Cardiovascular Center, University Hospital, Zurich
- b Doctor’s practice, Othmarsingen
- c Klinik im Park, Zurich
- d University Health Network, Toronto General Hospital, Toronto, Canada
- e Herzzentrum Hirslanden, Zurich
- f Division of Biostatistic, University, Zurich
Background: In professional cyclists (PC), typical echocardiographic changes include reversible dilatation of atria and left ventricle, and eccentric left ventricular hypertrophy but no change in diastolic function. Data on long-term outcome are limited.
Methods: Of all 134 former Swiss PC who participated at least once in the professional bicycle race Tour de Suisse in 1955–1975, 62 could be recruited for a prospective case control study. The PC were screened with a clinical exam, history, echocardiographic exam, and measurement of proBNP levels (normal <227 pg/mL). The control group consisted of 62 golfers matched for age, gender and hypertension. One bicycle year was defined as riding 1000 km on the bicycle per year in the past.
Results: The time interval since the last bicycle race as a professional was 38 (15–49) years. The average age at exam was equal in controls and PC (66 ± 6 vs 66 ± 7; p = 0.73). There was no difference in Body Mass Index, or cardiac medication. The percentage of patients still undergoing >4 h of endurance training per week was identical (p = 0.72). The number of bicycle years was significantly higher in PCs with 311 (60–975) compared to 2.5 (0–120) in controls (p < 0.0001). Left ventricular muscle mass tended to be higher in PC (p = 0.07), indicating eccentric left ventricular hypertrophy. PC had significantly larger left ventricles and atria (p < 0.002), and tended to have a larger right ventricular area (p = 0.14). Longitudinal contraction of both ventricles, measured as systolic velocities of mitral and tricuspid annulus but not as annular motion in the M-Mode echocardiography were lower in PC (p ≤ 0.04). Also, there were signs of diastolic dysfunction with lower annular E’, A’ velocities and larger atria in PC. ProBNP levels were 61.5 (12–2585) in PC and 58.5 (13–341) in controls (p = 0.21). Atrial size and left ventricular Muscle Mass Index correlated with the number of bike years in PC.
Conclusions: Among former PC, complete reversibility of exercise induced cardiac changes must be questioned as significant differences in systolic and diastolic function can be found between former PCs and controls in the long time follow-up. Therefore, endurance level training at an extremely high level may have a persisting impact on cardiac remodelling and function.
Children Are More Prone to Pulmonary Hypertension at High Altitude
- C. Jansena, A. Linkaa, S. Kriemlerb, M. Kohlerc, T. Schürmanna, M. Zehnderb, K. E. Blochc, H. P. Brunner-La Roccaa
- a Cardiology, University Hospital, Basel
- b Division of Physiology, University, Zurich
- c Division of Pneumology, University Hospital, Zurich
Background: It has become increasingly popular for families to spend vacation in high mountain areas. The question of high altitude tolerance of children, however, has been poorly studied. It has been shown in adults that up to 10% of the population may be susceptible to high altitude pulmonary oedema (HAPE). These individuals show more severe pulmonary hypertension when exposed to high altitude. Thus, the severity of hypoxia-induced pulmonary hypertension is an indicator of HAPE susceptibility. The response of pulmonary artery pressure to high-altitude induced hypoxia in children is completely unknown. Furthermore, it is unknown if the individual response is hereditary.
Aim: To test the response of pulmonary artery pressure to high altitude in prepubertal children (age 10 to 12 years) in comparison to their fathers (age 30 to 50 years).
Methods: Twenty children (4 girls and 16 boys; age 11 ± 1 year) and their fathers (age 44 ± 4 year) were included in this study. Within 3 weeks prior to ascent, echocardiography (Toshiba Aplio) was performed at rest at low altitude (Zurich-Irchel 500 m). Subjects travelled within two hours from low altitude to Jungfraujoch (JFJ; 3450 m), where examinations were done 3 to 4 h after arrival (day 1), the following afternoon (day 2), and the second morning after arrival before descent (day 3). Systolic pulmonary artery pressure was estimated from pressure gradient of tricuspid regurgitation (dp TR), diastolic pressure from pressure gradient of pulmonary insufficiency at end-diastole (dp PI), and pulmonary vascular resistance (PVR) by dividing the velocity of tricuspid regurgitation by time-velocity integral of the right-ventricular outflow tract.
Results: Pulmonary artery pressure increased significantly more in children on the first day (p < 0.001), returning to the level of the adults on day 3 (Figure 1). Interestingly, the increase of dp TR from low to high altitude of each child correlated significantly with the corresponding increase in his/her father (r = 0.57, p < 0.01). Also, dp PI (5.4 ± 3.2 vs 1.6 ± 2.8 mmHg) and PVR (0.5 ± 0.3 vs 0.3 ± 0.3 WU) increased significantly more in children (p < 0.05), confirming the findings of dpTR.
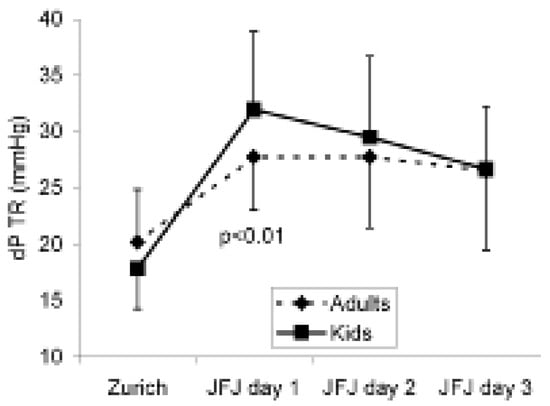
Figure 1.
Conclusion: Prepubertal children develop more severe pulmonary hypertension when exposed to high altitude than their parental counterparts. This might make them more susceptible to HAPE. The individual response of pulmonary pressure to high altitude seems to be hereditary.
Left Atrial Remodelling After Pulmonary Vein Isolation for Atrial Fibrillation: Evidence from Real-Time 3D Echocardiography
- H. Burri, H. Müller, S. Noble, H. Sunthorn, P. Sigaud, P.-F. Keller, P. Gentil, R. Lerch, D. Shah
- Service de Cardiologie, Hôpitaux Universitaires de Genève, Genève
Background: Pulmonary vein isolation by catheter radiofrequency ablation has been shown to effectively treat atrial fibrillation (AF). However the effect of this therapy on remodelling of the left atrium (LA) has not been well studied.
Methods: We included 51 patients (age 59 ± 8 years, 41 males) referred to our centre for radiofrequency ablation of paroxysmal (n = 37) or persistent (n = 14) AF who had undergone pulmonary vein isolation. LA volumes were measured using real-time full-volume 3D echocardiography at baseline and after 6.7 ± 2.3 months’ follow-up. Data on AF recurrences were also collected.
Results: As compared to baseline, LA volumes were significantly reduced at follow-up (59 ± 23 cc vs 50 ± 16 cc, p < 0.001). Patients with persistent AF had larger LA at baseline that those with paroxysmal AF (71 ± 19 cc vs 54 ± 22 cc, p = 0.012), and a trend in greater reduction in LA volumes at follow-up (–15 ± 14 cc vs –6 ± 15 cc, p = 0.064), although both groups showed significant reduction in LA volumes (p < 0.008 for both). There were no significant differences in reduction in LA volumes between patients with AF recurrence at follow-up (n = 10) and those in whom the arrhythmia was cured (n = 41).
Conclusions: 3D echocardiography shows evidence of LA remodelling with reduction in volumes in patients with paroxysmal and persistent AF. Remodelling takes place despite recurrence of AF, possibly due to a reduction in arrhythmia burden, or to scarring following the ablation lesions.

© 2006 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.