Abstract
An abnormal and hypertrophied upper labial frenulum (ULF) can cause diastemas, gingival recession, eruption abnormalities, and the onset of carious and periodontal problems in the upper central incisors, as well as aesthetic and functional disorders of the upper lip. The goal of this investigation is to review the evidence on the surgical techniques that are currently available for treating ULF in order to identify the best approach. PubMed, Scopus, Cochrane Library, and Embase were searched for papers that matched our topic from 13 November 2012 up to 22 November 2022 using the following Boolean keywords: “frenulum” and “surgery*”. A total of eight articles were selected for the purpose of the review. ULF can be surgically treated using either traditional scalpel surgery or laser surgery. The latter is the better option due to its intra- and post-operative benefits for both the patients and the clinicians, in terms of faster healing, fewer side effects and discomfort, and greater patient compliance. However, a higher learning curve is required for this technique, especially to calibrate the appropriate power of the laser. To date, it is not possible to identify which type of laser achieves the best clinical results for the treatment of ULF.
1. Introduction
The medial upper labial frenulum (ULF) is a thin band or fold of mucus tissue extending from the middle of the maxillary gingiva to the center of the upper lip. Its insertion height is variable. It develops from the tecto-labial bands connecting the upper lip to the tecto-labial papilla, which will originate the incisive papilla in the third to fourth month of intrauterine life [1].
The position of the frenulum remains stable from birth until the eruption of the maxillary central incisors. Atrophy and translocation of the insertion in the apical direction are correlated with the development of the permanent teeth and the growth of the alveolar process. During primary dentition, although the frenulum insertion remains stationary, fresh bone deposits heighten the alveolar ridge. The permanent central upper incisors usually erupt with a diastema. The thrust of lateral incisors and canines (11–12 years) tends to minimize the diastema and bring the incisors closer together [1,2].
The frenulum is mostly made of collagen, although it also has elastic and lax reticular fibers. The lining is distinguished by stratified compound pavimentous epithelium.
It is unknown if there is muscle tissue in the frenulum, however, it is now believed that muscle tissue is not an essential component of the frenulum [3]. Due to the lack of muscle fibers and developmental behavior, the frenulum does not appear to affect tooth emergence, gingival morphology, or the mobility of mucosal structures. At this time, an interincisal diastema is not thought to be determined by the persistence of frenulum insertion at the level of the papilla [1,4].
Different classifications for ULF have been proposed by authors, based on the place of implantation and site of insertion. Placek in 1974 classified the different forms of frenulum according to the place of implantation, distinguishing (a) mucosal attachment frenulum when the frenulum is inserted into mucosa; (b) gingival attachment frenulum, when it is inserted into adherent gingiva; (c) papillary-attached frenulum, when it inserts into the palatine papilla; and (d) penetrating papillary attachment frenulum, when the frenulum fibers pass through the interincisive papilla and insert into palatine adherent gingival [5,6].
In 1977, Popovich et al. classified the frenulum according to the site of insertion. In this case, the frenulum is divided into two primary morphotypes, thick and thin, which can be distinguished into in: high (alveolar mucosa), medium (adherent gingiva), and low (marginal gingiva) [7].
Likewise, Rui et al. proposed a classification of frenulum considering site insertion: (a) Type I: alveolar mucosa; (b) Type II: gingival insertion; (c) Type III: interdental papilla; and (d) Type IV: transpapillar [8].
Generally, the type of insertion, the width of the frenulum, the mechanical action on the gingival margin, and the difficulty in performing dental care procedures have all been regarded as criteria to identify a normal frenulum from a defective one without ever arriving at a uniformity of evaluation.
A characteristic of an abnormal frenulum, known as “pull syndrome,” is the ischemization of the palatine papilla and mesial gingival borders of the upper central incisors after traction of the top lip (Figure 1).

Figure 1.
Example of the hypertonic ULF.
Others experience the taut, fibrous, papillary, or transpapillary insertion interincisional frenulum more frequently, which has a broad triangular upper insertion known as the tecto-labial frenulum. This kind of frenulum is regarded as a genuine dysontogenic manifestation of fetal frenulum persistence after birth [5]. The surgical approaches that are currently in use are: (a) frenectomy or excision, which involves complete removal of the frenulum; (b) frenulotomy, which involves partial removal of the frenulum (Figure 2); (c) apical repositioning of the frenulum [9,10,11].
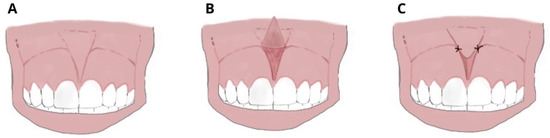
Figure 2.
Frenulotomy: (A) Hypertrophic superior median frenulum with insertion on the interincisive papilla; (B) partial thickness incision disengages frenulum and muscle fibers and does not involve the periosteum; and (C) suture and apical repositioning on the labial side.
The types of surgical techniques that are currently available are conventional scalpel surgery and laser surgery.
1.1. Conventional Surgery
The surgical techniques are: (a) classical frenectomy/V-shaped Archer/diamond-shaped incision; (b) Z-plasty incision; (c) extension of the vestibular groove; and (d) frenectomy according to Miller’s technique.
The conventional cold-blade method has all the side effects of classical surgery, such as tissue bleeding with the need for suturing and possible bacterial overinfection of the surgical site [12,13].
Classical frenectomy/V-shaped Archer/diamond-shaped incision: devised by Archer (1961) and Kruger (1964). The cold blade procedure is the traditional technique and involves a V-shaped incision along the edges of the frenulum, removal of the coronal insertion of the frenulum with subsequent apical repositioning. The periosteal fibres are then cut horizontally and vertically, and the wound is closed with sutures. This technique involves more side effects because it produces the development of scar tissue with possible periodontal repercussions until the disappearance of the interincisive papilla (Figure 3).
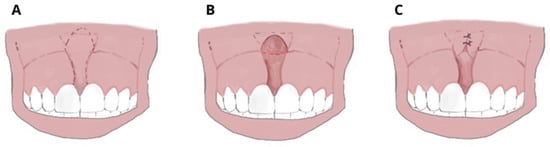
Figure 3.
Frenectomy with traditional and V-shaped surgery: (A) Transpapillary frenulum; (B) two paramedian vertical incisions are drawn parallel to the sides of the frenulum up to the retroincisive papilla, where they connect with a horizontal cut; the frenulum is raised and the periosteum is exposed; (C) the margins are sutured along the midline, not involving the adherent gingiva; and periodontal wrap and healing by second intention.
Z-plasty incision: uses a Z-shaped incision to create two triangular flaps of equal size that are then transposed and sutured. The stitches are removed 5–7 days after surgery. It has minor scar outcomes and is indicated in cases of the deep fornix, with wide, hypertrophic frenules and low insertion. It determines the partial removal of frenulum tissue that is associated with the deepening of the fornix. It may cause recurrence (Figure 4).
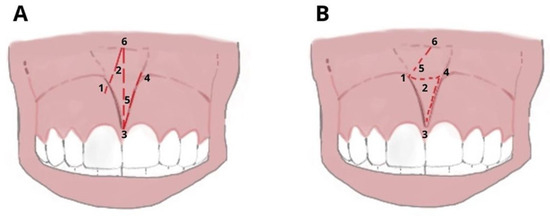
Figure 4.
Z-Plasty: (A) Vertical incision in the center of the frenulum, with releases parallel to 60° to form a Z and (B) transposition of the mucous flaps of triangular shape and suture: the orientation of the fibers that were vertical rotates and becomes horizontal. (1–6) The numbers refer to the chronology of execution of the incision.
Extension of the vestibular groove: mucosa is incised and repositioned more apically, with suturing to the periosteum and healing by second intention. It has a high relief rate.
Frenectomy according to Miller’s technique: the free gingival pedicle is placed laterally in order to reduce scar tissue formation. Although this incurs a more complex procedure for the operator, it has an aesthetic advantage and it is particularly indicated in cases of a gingival smile.
Electrosurgery: recommended in patients with coagulation problems. It also provides effective hemostasis in patients with poor compliance [14].
1.2. Laser Surgery
Nowadays, different types of lasers are commonly used in everyday practice. Each one produces a different wavelength of light, which is defined by the active medium (solid, liquid, or gas) [15].
Lasers that are actually used in oral surgery are: Potassium titanyl phosphate laser, or KTP (532 nm); diode laser (810–930 nm); neodymium-doped yttrium aluminum garnet laser, or Nd:YAG (1064 nm); erbium family lasers (2780–2940 nm), which includes the erbium-doped yttrium aluminum garnet laser, or Er:YAG; the erbium chromium yttrium scandium gallium-garnet laser, or Er,Cr:YSGG; and a carbon dioxide laser, or CO2 (10,600 nm) [15,16] (Figure 5).
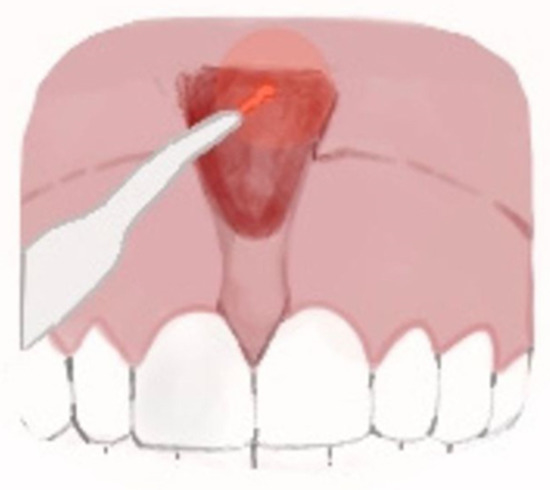
Figure 5.
Laser frenectomy.
The fundamental distinction among them is the capacity to operate strictly on soft or hard tissues or both [17,18]. When just soft tissue surgery is required, the choice of the clinician must fall upon KTP, Diode, Nd:YAG or CO2 lasers [19,20]. Instead, the erbium family lasers (Er;Cr:YSGG or Er:YAG lasers) may be required when both soft and hard tissue surgery is necessary [20,21,22] (Figure 6).

Figure 6.
ULF laser surgery.
Several authors have highlighted the benefits of lasers over other types of traditional dental techniques, namely increased coagulation and hemostasis, which results in a dry surgical area for greater vision and a significantly diminished requirement for suturing (the erbium family lasers are an exception to this rule as they offer only a little haemostasis); decrease in bacteremia (tissue temperature changes brought on by laser surgery are efficient at reducing bacteria); accelerated healing process (laser beam can promote healing via photo-biomodulation); and reduced post-surgical pain [17,20,23,24,25].
Furthermore, the diode laser has become highly popular in dental practice given its small size, low cost and easy application for minor soft tissue surgery, for its properties of straightforward tissue incision, and its coagulation and post-surgery benefits [26,27] (Figure 7).

Figure 7.
Labial frenulum treated by laser frenectomy after healing.
Regardless of the surgical technique that is used, labial frenulums are anatomical structures with high biological memory, so surgery should include not only the removal of the frenulum, but also that of its deep periosteal insertions up to the muco-gingival line, in order to prevent a recurrence. Fibrotomy of the circular and transseptal fibers should be prolonged up to the level of the palatal bone in cases of Type IV maxillary labial frenulum with palatine insertion [9,28,29].
There are already numerous articles in the literature dealing with the lingual frenulum and its resolution, instead, although ULF is the most frequent type of frenulum and has the greatest impact on orthodontic treatments, there is little evidence about its surgical treatment. Herein, the purpose of this study is to review the surgical techniques that are currently available for the treatment of ULF, analyzing the advantages and disadvantages of each approach.
2. Materials and Methods
2.1. Protocol and Registration
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were used in this systematic review [30]. The review protocol was registered at PROSPERO under the unique number 381024.
2.2. Data Sources and Search Strategy
The qualifying criteria were developed using the PICOS (population, intervention, comparison, outcomes, and study design) framework. Pubmed, Cochrane, Scopus, and Embase databases were searched from 13 November 2012 up to 13 November 2022, using the keywords “frenulum” and “surgery”. The authors checked the titles and complete texts of any papers that might be relevant. Table 1 summarizes the search approach in detail (Table 1).

Table 1.
Database search indicator.
2.3. Inclusion and Exclusion Criteria
Articles that met the following criteria were included: (1) studies only on humans; (2) open access studies; (3) randomized trials, retrospective and observational studies; and (4) studies dealing with surgical approach of ULF and comparing the different techniques.
The exclusion criteria were: reviews, letters to the editors; animal models or dry skulls studies; and craniofacial syndromes, or cleft lip and palate.
2.4. Data Collection
The study data were selected by analyzing the study design, sample size, control group, age of intervention, type of surgery, follow-up, and outcome (Table 2).

Table 2.
Studies included characteristics [CO2: carbon dioxide laser, DB-RCT: double bind-randomized controlled trial, Er,Cr:YSGG: erbium chromium yttrium scandium gallium-garnet laser, Er:YAG: erbium-doped yttrium aluminum garnet laser KTP: potassium titanyl phosphate laser. Nd:YAG: neodymium-doped yttrium aluminum garnet laser, RCT: randomized controlled trial].
3. Results
Study Selection and Included Study Characteristics
The electronic database search identified a total of 334 studies. After duplicate removal, 274 studies underwent title and abstract screening. In total, 274 papers were not selected after the abstract screening, and 56 articles were chosen for the eligibility assessment. Subsequently, 48 papers were eliminated after the full-text evaluation: 42 off-topic, 5 wrong setting, and 1 with no outcome of interest. Finally, 8 articles were selected for the systematic review. The selection process is summarized in Figure 8.
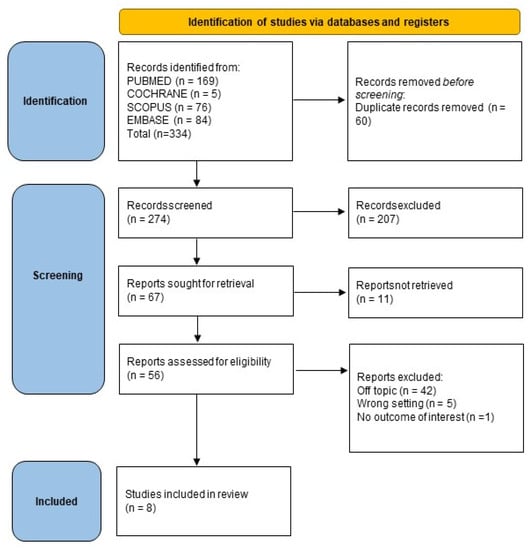
Figure 8.
Literature search preferred reporting items for systematic reviews and meta-analyses (PRISMA) flow diagram.
4. Discussion
The presence of an abnormal and hypertrophied interdental ULF could cause diastemas, gingival recession, eruption abnormalities, and the onset of carious and periodontal problems of the upper central incisors, as well as aesthetic and functional disorders of the upper lip [8,33]. The surgical approach to solving the problem involves the use of a conventional scalpel [31,36,37], electrosurgery, or the use of different types of high-intensity laser devices [8,31,32,33,34,35,36,37]. Although electrosurgery is a well-known surgical technique for ULF [14], in this review only studies about traditional surgery and laser surgery have passed the screening phase. The surgical techniques that are used have always been studied and compared, and although no study emphasizes which technique is the most effective, the literature is unanimous that conventional surgery unless combined with a Z-plasty is contraindicated in the presence of a short lip and fornix, as the scarring outcome would worsen the initial clinical situation [32,38].
In the case of conventional scalpel surgery, suturing is always necessary; the electric scalpel has great hemostatic capabilities, but it causes cicatricial outcomes and often postoperative pain; the laser irradiation, on the other hand, under the correct parameters does not penetrate deeply into the tissues, but draws precise, non-bleeding surgical margins, consequently improving the visibility of the surgical site and the comfort and compliance of the patient [8,39].
Studies comparing traditional surgical techniques vs. diode laser surgery highlight the superiority of the laser surgery technique in terms of hemostasis, surgical time, pain, edema, post-surgical inflammation, and wound healing time [35,36,37].
In a clinical retrospective study, Komori et al. analyzed the use of CO2 laser with a wavelength of 10.6 μm on six pediatric patients, of which two presented Type II frenulum and four presented Type III frenulum according to Rui’s classification. Suturing was necessary for only one patient out of the six that were treated, as the high-frequency laser irradiation demonstrates excellent hemostatic activity, as well as precise resection and vaporization of the soft tissues of the oral cavity. None of the patients complained of postoperative problems such as pain, difficulty in chewing, hemorrhage, and recurrence with fiber reattachment. The surgical time is short and the technique is simpler than traditional surgery [8,40,41,42,43].
Ling et al. compared the conventional surgical approach with a frenectomy procedure that uses two successive pulses of the Er:YAG and Nd:YAG lasers. The authors demonstrate that the laser surgery technique is more comfortable and less painful for the patient both intra-operatively and post-operatively, and chair time is reduced as there is no need to suture and then remove the suture, so there is an increase in patient cooperation. The patient does not even need to take antibiotic therapy due to the laser irradiation’s ability to sterilize and hemostasis the area. On the other hand, the conventional surgical technique may result in longer healing times if the patient does not observe strict oral hygiene leading to plaque accumulation on the sutures, but it has the advantage of having a shorter learning curve for the operator and being less expensive [31,44].
In a prospective study of 50 patients, Pie-Sanchez et al. compared the efficiency of two types of laser devices: CO2 and Er,Cr:YSGG concluding that the CO2 laser allows the operator to perform surgery in a shorter time and with a bloodless surgical field, but the Er,Cr:YSGG laser gives faster wound healing [32,45,46].
The versatility of the laser surgery technique was illustrated in Rozo’s case study. The 16-year-old patient received frenolectomy and anterior gingivoplasty in the same procedure, the first for functional reasons, and the second for artistic ones. Laser intervention may be utilized for two treatments at once, cutting down on visits and discomfort for patients [35].
Sfasciotti et. al. analyzed frenectomy treatment in pediatric patients that were at risk of developing gingival recessions aggravated by the presence of the frenulum. The study compared diode vs. CO2 laser appliances and concluded that the former is a better performer in terms of pain management and wound healing speed, but the latter gives better bleeding control [33,47,47,48,49].
In their work, Onur et al. analyzed pain perception and wound healing time in patients that were treated with Er,Cr: YSGG vs. diode laser surgery, with no statistically significant differences between the two groups with regards to safety and efficiency [3,34,50].
When employing lasers, caution must be taken to calibrate the appropriate power and to safeguard the operator’s and patient’s eyes using a particular equipment. Excessive power can cause damage to the bone surface [8,32]. Diode, Nd: YAG, and CO2 lasers in particular overheat nearby tissues, and any fiber interaction with the periosteum must be avoided since this might result in localized, reversible tissue necrosis and pain for the patient [32,36].
The main limitation of this study is that although studies examined analyze the same clinical parameters, they use different classifications and compare one type of laser with the traditional surgical technique or only two types of laser appliances with each other. As a result, it is impossible to make an exact comparison between the traditional surgical technique and the different types of laser techniques.
5. Conclusions
Diastemas, gingival recession, eruption abnormalities, carious and periodontal lesions of the upper central incisors, as well as aesthetic and functional lip disorders, can all be caused by an abnormal median ULF.
This systematic review includes studies that examine the surgical techniques that are available for treatment, including traditional surgery and laser surgery.
Although traditional scalpel surgery has a shorter learning curve and lower costs, it has several drawbacks, including longer operating times, bleeding, decreased visibility of the surgical field, the need for tissue suturing, longer healing times, and the risk of plaque build-up on the sutures. In contrast, the laser surgery approach allows for treatment with significant reductions in intra-operative and post-operative discomfort for both the operator and the patient. It enables clean, bleed-free margins that improve surgical site visibility and do not require suturing. Based on the examination of the chosen articles, it appears that the laser surgery technique appears to be better in terms of haemostasis, surgical time, pain, edema, post-surgical inflammation, and healing time when compared with conventional surgery.
Despite this, it has not been possible to determine which type of laser source has the best clinical results. Consistent randomized controlled trials are necessary to compare the benefits and drawbacks of the various surgical laser devices currently available.
Author Contributions
Conceptualization, A.M.I., A.D.I., G.M., I.F., F.V., D.A., B.R., A.N. and N.D.L.; methodology, S.B., E.d.R., F.V., G.L., I.F. and A.N.; software, F.V., F.I., G.L. and G.D.; validation, A.N., F.L., I.R.B., A.S., D.D.V., D.A., N.D.L., F.I. and G.D.; formal analysis, A.D.I., I.F., S.B., S.S., G.M.T., B.R., D.D.V., F.I. and G.D.; resources, A.D.I., A.M.I., G.M., A.P., N.D.L., A.N., F.V., D.A., G.L. and P.A.; data curation, G.M., A.M., S.B., I.R.B., F.L., F.I., F.V. and G.D.; writing—original draft preparation, A.D.I., A.M.I., E.d.R., S.B., B.R., I.F., D.D.V., S.S., A.N., F.I., G.D. and P.A.; writing—review and editing, D.A., A.N., G.L., N.D.L., S.B., I.R.B. and M.C.F.; visualization, I.F., G.L., N.D.L., B.R., F.L., D.A., A.N. and P.A.; supervision, A.S., A.D.I., A.M.I., I.F., A.P., G.M., D.D.V., F.I., G.D. and M.C.F.; project administration, B.R., G.M.T., F.L., F.I., G.D. and M.C.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No applicable.
Acknowledgments
We would like to thank Antonio Scarano and Ioana Roxana Bordea for their collaboration in this work.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| CO2 | Carbon dioxide laser |
| Er,Cr:YSGG | Erbium chromium yttrium scandium gallium-garnet laser |
| Er:YAG | Erbium-doped yttrium aluminum garnet laser |
| KTP | Potassium titanyl phosphate laser |
| Nd:YAG | Neodymium-doped yttrium aluminum garnet laser |
| ULF | Upper labial frenulum |
References
- Miotti, A.; Frezza, F.; Favero, G.; Cecchetto, A. Histologic characteristics of the upper labial frenum in individuals with middle interincisor diastema. Mondo Odontostomatol. 1979, 21, 22–25. [Google Scholar] [PubMed]
- Cantore, S.; Ballini, A.; Farronato, D.; Malcangi, G.; Dipalma, G.; Assandri, F.; Garagiola, U.; Inchingolo, F.; De Vito, D.; Cirulli, N. Evaluation of an Oral Appliance in Patients with Mild to Moderate Obstructive Sleep Apnea Syndrome Intolerant to Continuous Positive Airway Pressure Use: Preliminary Results. Int. J. Immunopathol. Pharm. 2016, 29, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Scarano, A.; Lorusso, F.; Inchingolo, F.; Postiglione, F.; Petrini, M. The Effects of Erbium-Doped Yttrium Aluminum Garnet Laser (Er: YAG) Irradiation on Sandblasted and Acid-Etched (SLA) Titanium, an In Vitro Study. Materials 2020, 13, 4174. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.D.; Patano, A.; Coloccia, G.; Ceci, S.; Inchingolo, A.M.; Marinelli, G.; Malcangi, G.; Montenegro, V.; Laudadio, C.; Palmieri, G.; et al. Genetic Pattern, Orthodontic and Surgical Management of Multiple Supplementary Impacted Teeth in a Rare, Cleidocranial Dysplasia Patient: A Case Report. Medicina 2021, 57, 1350. [Google Scholar] [CrossRef]
- Mirko, P.; Miroslav, S.; Lubor, M. Significance of the Labial Frenum Attachment in Periodontal Disease in Man. Part I. Classification and Epidemiology of the Labial Frenum Attachment. J. Periodontol. 1974, 45, 891–894. [Google Scholar] [CrossRef]
- Kramer, P.F.; de Amorim, L.M.; de Moura Alves, N.; Ruschel, H.C.; Bervian, J.; Feldens, C.A. Maxillary Labial Frenum in Preschool Children: Variations, Anomalies and Associated Factors. J. Clin. Pediatr. Dent. 2022, 46, 51–57. [Google Scholar] [CrossRef]
- Popovich, F.; Thompson, G.W.; Main, P.A. The Maxillary Interincisal Diastema and Its Relationship to the Superior Labial Frenum and Intermaxillary Suture. Angle Orthod. 1977, 47, 265–271. [Google Scholar] [CrossRef]
- Komori, S.; Matsumoto, K.; Matsuo, K.; Suzuki, H.; Komori, T. Clinical Study of Laser Treatment for Frenectomy of Pediatric Patients. Int. J. Clin. Pediatr. Dent. 2017, 10, 272–277. [Google Scholar] [CrossRef]
- Delli, K.; Livas, C.; Sculean, A.; Katsaros, C.; Bornstein, M.M. Facts and Myths Regarding the Maxillary Midline Frenum and Its Treatment: A Systematic Review of the Literature. Quintessence Int. 2013, 44, 177–187. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.D.; Malcangi, G.; Inchingolo, A.M.; Piras, F.; Settanni, V.; Garofoli, G.; Palmieri, G.; Ceci, S.; Patano, A.; De Leonardis, N.; et al. Benefits and Implications of Resveratrol Supplementation on Microbiota Modulations: A Systematic Review of the Literature. Int. J. Mol. Sci. 2022, 23, 4027. [Google Scholar] [CrossRef]
- Ceratti, C.; Maspero, C.; Consonni, D.; Caprioglio, A.; Connelly, S.T.; Inchingolo, F.; Tartaglia, G.M. Cone-Beam Computed Tomographic Assessment of the Mandibular Condylar Volume in Different Skeletal Patterns: A Retrospective Study in Adult Patients. Bioengineering 2022, 9, 102. [Google Scholar] [CrossRef]
- Devishree; Gujjari, S.K.; Shubhashini, P.V. Frenectomy: A Review with the Reports of Surgical Techniques. J. Clin. Diagn. Res. 2012, 6, 1587–1592. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Ceci, S.; Limongelli, L.; Corriero, A.; Curatoli, L.; Azzollini, D.; Mezzapesa, P.P.; Marinelli, G.; Malcangi, G.; Coloccia, G.; et al. Cavernous Sinus Involvement and Near Miss Mediastinitis Following Mandibular Tooth Infection Treated during the COVID-19 Pandemic: Clinical Diagnosis and Treatment. Case Rep. Dent. 2022, 2022, 8650099. [Google Scholar] [CrossRef]
- Miller, P.D. The Frenectomy Combined with a Laterally Positioned Pedicle Graft. Functional and Esthetic Considerations. J. Periodontol. 1985, 56, 102–106. [Google Scholar] [CrossRef]
- Protásio, A.C.R.; Galvão, E.L.; Falci, S.G.M. Laser Techniques or Scalpel Incision for Labial Frenectomy: A Meta-Analysis. J. Maxillofac. Oral Surg. 2019, 18, 490–499. [Google Scholar] [CrossRef]
- Aoki, A.; Sasaki, K.M.; Watanabe, H.; Ishikawa, I. Lasers in Nonsurgical Periodontal Therapy. Periodontol. 2000 2004, 36, 59–97. [Google Scholar] [CrossRef]
- Tachmatzidis, T.; Dabarakis, N. Technology of Lasers and Their Applications in Oral Surgery: Literature Review. Balk. J. Dent. Med. 2016, 20, 131–137. [Google Scholar] [CrossRef]
- Iodice, G.; Nanda, R.; Drago, S.; Repetto, L.; Tonoli, G.; Silvestrini-Biavati, A.; Migliorati, M. Accuracy of Direct Insertion of TADs in the Anterior Palate with Respect to a 3D-Assisted Digital Insertion Virtual Planning. Orthod. Craniofac. Res. 2022, 25, 192–198. [Google Scholar] [CrossRef]
- Capodiferro, S.; Tempesta, A.; Limongelli, L.; Barile, G.; Di Venere, D.; Corsalini, M. Minimally Invasive (Flapless) Crown Lengthening by Erbium:YAG Laser in Aesthetic Zone. F1000Research 2020, 9, 1185. [Google Scholar] [CrossRef]
- Parker, S. Verifiable CPD Paper: Laser-Tissue Interaction. Br. Dent. J. 2007, 202, 73–81. [Google Scholar] [CrossRef]
- Malcangi, G.; Inchingolo, A.D.; Patano, A.; Coloccia, G.; Ceci, S.; Garibaldi, M.; Inchingolo, A.M.; Piras, F.; Cardarelli, F.; Settanni, V.; et al. Impacted Central Incisors in the Upper Jaw in an Adolescent Patient: Orthodontic-Surgical Treatment—A Case Report. Appl. Sci. 2022, 12, 2657. [Google Scholar] [CrossRef]
- Cirulli, N.; Inchingolo, A.D.; Patano, A.; Ceci, S.; Marinelli, G.; Malcangi, G.; Coloccia, G.; Montenegro, V.; Di Pede, C.; Ciocia, A.M.; et al. Innovative Application of Diathermy in Orthodontics: A Case Report. Int. J. Environ. Res. Public Health 2022, 19, 7448. [Google Scholar] [CrossRef]
- Ishikawa, I.; Aoki, A.; Takasaki, A.A. Potential Applications of Erbium:YAG Laser in Periodontics. J. Periodontal. Res. 2004, 39, 275–285. [Google Scholar] [CrossRef]
- Russell, A.D. Lethal Effects of Heat on Bacterial Physiology and Structure. Sci. Prog. 2003, 86, 115–137. [Google Scholar] [CrossRef]
- Haytac, M.C.; Ozcelik, O. Evaluation of Patient Perceptions after Frenectomy Operations: A Comparison of Carbon Dioxide Laser and Scalpel Techniques. J. Periodontol. 2006, 77, 1815–1819. [Google Scholar] [CrossRef]
- Azma, E.; Safavi, N. Diode Laser Application in Soft Tissue Oral Surgery. J. Lasers Med. Sci. 2013, 4, 206–211. [Google Scholar]
- Ortega-Concepción, D.; Cano-Durán, J.A.; Peña-Cardelles, J.-F.; Paredes-Rodríguez, V.-M.; González-Serrano, J.; López-Quiles, J. The Application of Diode Laser in the Treatment of Oral Soft Tissues Lesions. A Literature Review. J. Clin. Exp. Dent. 2017, 9, e925–e928. [Google Scholar] [CrossRef]
- Maspero, C.; Abate, A.; Inchingolo, F.; Dolci, C.; Cagetti, M.G.; Tartaglia, G.M. Incidental Finding in Pre-Orthodontic Treatment Radiographs of an Aural Foreign Body: A Case Report. Children 2022, 9, 421. [Google Scholar] [CrossRef]
- Pasciuti, E.; Coloccia, G.; Inchingolo, A.D.; Patano, A.; Ceci, S.; Bordea, I.R.; Cardarelli, F.; Di Venere, D.; Inchingolo, F.; Dipalma, G. Deep Bite Treatment with Aligners: A New Protocol. Appl. Sci. 2022, 12, 6709. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Healthcare Interventions: Explanation and Elaboration. BMJ 2009, 339, e1–e34. [Google Scholar] [CrossRef]
- Xie, L.; Wang, P.; Ding, Y.; Zhang, L. Comparative Frenectomy with Conventional Scalpel and Dual-Waved Laser in Labial Frenulum. World Jnl. Ped. Surg. 2022, 5, e000363. [Google Scholar] [CrossRef]
- Pie-Sanchez, J.; Espana-Tost, A.; Arnabat-Dominguez, J.; Gay-Escoda, C. Comparative Study of Upper Lip Frenectomy with the CO2 Laser versus the Er, Cr:YSGG Laser. Med. Oral 2012, 17, e228–e232. [Google Scholar] [CrossRef]
- Sfasciotti, G.L.; Zara, F.; Vozza, I.; Carocci, V.; Ierardo, G.; Polimeni, A. Diode versus CO2 Laser Therapy in the Treatment of High Labial Frenulum Attachment: A Pilot Randomized, Double-Blinded Clinical Trial. Int. J. Environ. Res. Public Health 2020, 17, 7708. [Google Scholar] [CrossRef]
- Onur, S.G. Evaluation of Pain Perception and Wound Healing After Laser-Assisted Frenectomy in Pediatric Patients: A Retrospective Comparative Study. Photobiomodulation Photomed. Laser Surg. 2021, 39, 204–210. [Google Scholar] [CrossRef]
- Pulido Rozo, M.A.; Tirado Amador, L.R.; Madrid Troconis, C.C. Gingivoplastia y frenillectomía labial con láser de alta intensidad: Presentación de caso. Rev. Clín. Periodoncia Implantol. Rehabil. Oral 2015, 8, 157–162. [Google Scholar] [CrossRef]
- Júnior, R.M.; Gueiros, L.A.; Silva, I.H.; de Albuquerque Carvalho, A.; Leão, J.C. Labial Frenectomy with Nd:YAG Laser and Conventional Surgery: A Comparative Study. Lasers Med. Sci. 2015, 30, 851–856. [Google Scholar] [CrossRef]
- De SPinheiroa, A.F.; Furtadoa, G.S.; Sanderb, H.H.; Serraa, L.L.; Lagoa, A.D. Duas propostas cirúrgicas para frenectomia labial—Convencional e a laser de alta potência. Rev. Port. Estomatol. Med. Dent. Cir. Maxilofac. 2018, 59, 125–130. [Google Scholar] [CrossRef]
- Coscia, M.F.; Monno, R.; Ballini, A.; Mirgaldi, R.; Dipalma, G.; Pettini, F.; Cristallo, V.; Inchingolo, F.; Foti, C.; de Vito, D. Human Papilloma Virus (HPV) Genotypes Prevalence in a Region of South Italy (Apulia). Ann. Ist. Super Sanita 2015, 51, 248–251. [Google Scholar] [CrossRef]
- Saucedo, C.L.; Courtois, E.C.; Wade, Z.S.; Kelley, M.N.; Kheradbin, N.; Barrett, D.W.; Gonzalez-Lima, F. Transcranial Laser Stimulation: Mitochondrial and Cerebrovascular Effects in Younger and Older Healthy Adults. Brain Stimul. 2021, 14, 440–449. [Google Scholar] [CrossRef]
- Farronato, M.; Maspero, C.; Abate, A.; Grippaudo, C.; Connelly, S.T.; Tartaglia, G.M. 3D Cephalometry on Reduced FOV CBCT: Skeletal Class Assessment through AF-BF on Frankfurt Plane-Validity and Reliability through Comparison with 2D Measurements. Eur. Radiol. 2020, 30, 6295–6302. [Google Scholar] [CrossRef]
- Tartaglia, G.M.; Mapelli, A.; Maspero, C.; Santaniello, T.; Serafin, M.; Farronato, M.; Caprioglio, A. Direct 3D Printing of Clear Orthodontic Aligners: Current State and Future Possibilities. Materials 2021, 14, 1799. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Inchingolo, A.M.; Bordea, I.R.; Malcangi, G.; Xhajanka, E.; Scarano, A.; Lorusso, F.; Farronato, M.; Tartaglia, G.M.; Isacco, C.G.; et al. SARS-CoV-2 Disease through Viral Genomic and Receptor Implications: An Overview of Diagnostic and Immunology Breakthroughs. Microorganisms 2021, 9, 793. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, F.; Hazballa, D.; Inchingolo, A.D.; Malcangi, G.; Marinelli, G.; Mancini, A.; Maggiore, M.E.; Bordea, I.R.; Scarano, A.; Farronato, M.; et al. Innovative Concepts and Recent Breakthrough for Engineered Graft and Constructs for Bone Regeneration: A Literature Systematic Review. Materials 2022, 15, 1120. [Google Scholar] [CrossRef]
- Maspero, C.; Cappella, A.; Dolci, C.; Cagetti, M.G.; Inchingolo, F.; Sforza, C. Is Orthodontic Treatment with Microperforations Worth It? A Scoping Review. Children 2022, 9, 208. [Google Scholar] [CrossRef]
- Contaldo, M.; Itro, A.; Lajolo, C.; Gioco, G.; Inchingolo, F.; Serpico, R. Overview on Osteoporosis, Periodontitis and Oral Dysbiosis: The Emerging Role of Oral Microbiota. Appl. Sci. 2020, 10, 6000. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Ferrara, I.; Viapiano, F.; Netti, A.; Campanelli, M.; Buongiorno, S.; Latini, G.; Carpentiere, V.; Ciocia, A.M.; Ceci, S.; et al. Rapid Maxillary Expansion on the Adolescent Patient: Systematic Review and Case Report. Children 2022, 9, 1046. [Google Scholar] [CrossRef] [PubMed]
- Coloccia, G.; Inchingolo, A.D.; Inchingolo, A.M.; Malcangi, G.; Montenegro, V.; Patano, A.; Marinelli, G.; Laudadio, C.; Limongelli, L.; Di Venere, D.; et al. Effectiveness of Dental and Maxillary Transverse Changes in Tooth-Borne, Bone-Borne, and Hybrid Palatal Expansion through Cone-Beam Tomography: A Systematic Review of the Literature. Medicina 2021, 57, 288. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Pezzolla, C.; Patano, A.; Ceci, S.; Ciocia, A.M.; Marinelli, G.; Malcangi, G.; Montenegro, V.; Cardarelli, F.; Piras, F.; et al. Experimental Analysis of the Use of Cranial Electromyography in Athletes and Clinical Implications. Int. J. Environ. Res. Public Health 2022, 19, 7975. [Google Scholar] [CrossRef]
- Rapone, B.; Ferrara, E.; Santacroce, L.; Cesarano, F.; Arazzi, M.; Di Liberato, L.; Scacco, S.; Grassi, R.; Grassi, F.R.; Gnoni, A.; et al. Periodontal Microbiological Status Influences the Occurrence of Cyclosporine-A and Tacrolimus-Induced Gingival Overgrowth. Antibiotics 2019, 8, 124. [Google Scholar] [CrossRef]
- Lorusso, F.; Inchingolo, F.; Dipalma, G.; Postiglione, F.; Fulle, S.; Scarano, A. Synthetic Scaffold/Dental Pulp Stem Cell (DPSC) Tissue Engineering Constructs for Bone Defect Treatment: An Animal Studies Literature Review. Int. J. Mol. Sci. 2020, 21, 9765. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).