Simulation Studies Provide Evidence of Aerosol Transmission of SARS-CoV-2 in a Multi-Story Building via Air Supply, Exhaust and Sanitary Pipelines
Abstract
1. Introduction
2. Materials and Methods
3. Results
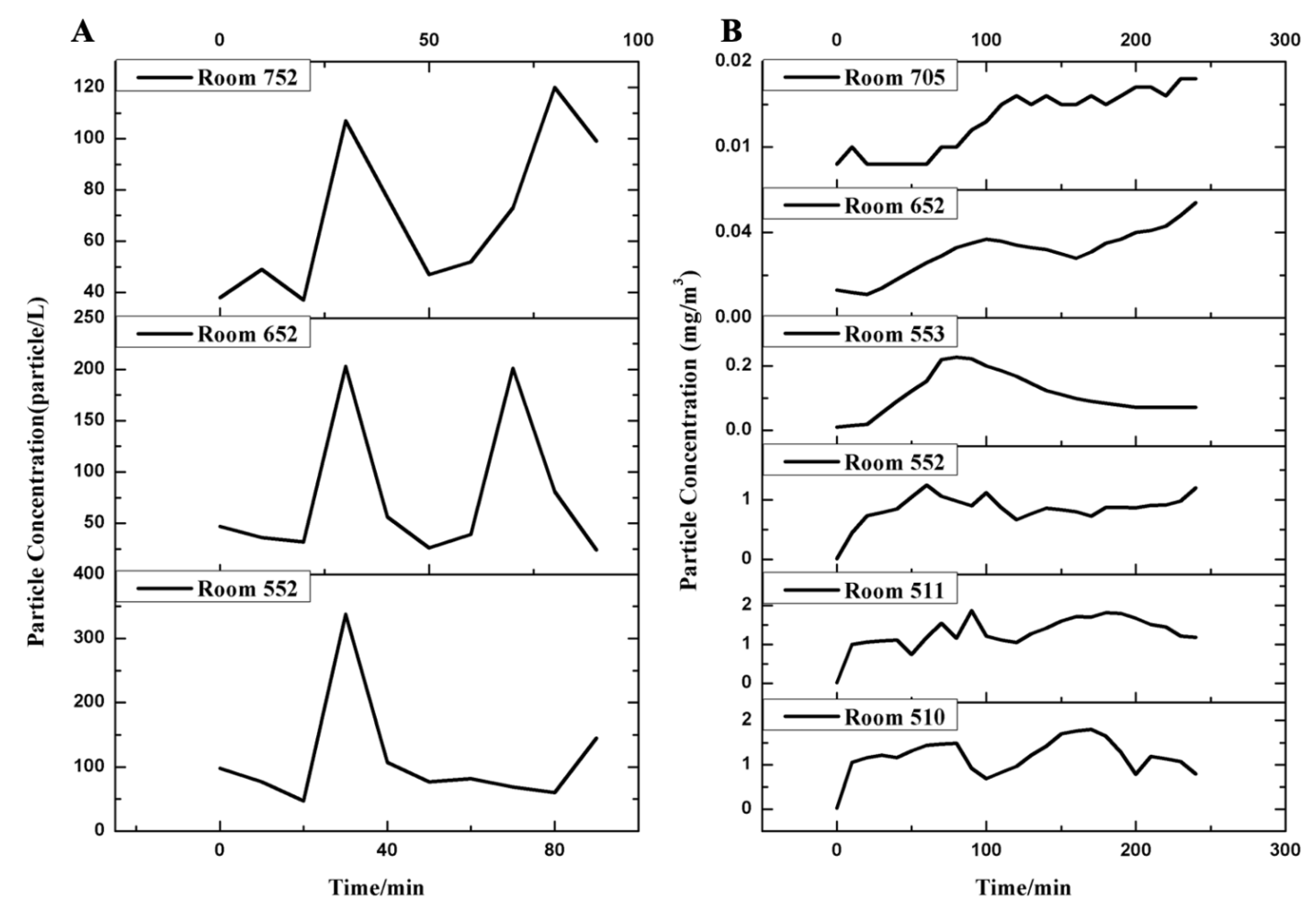
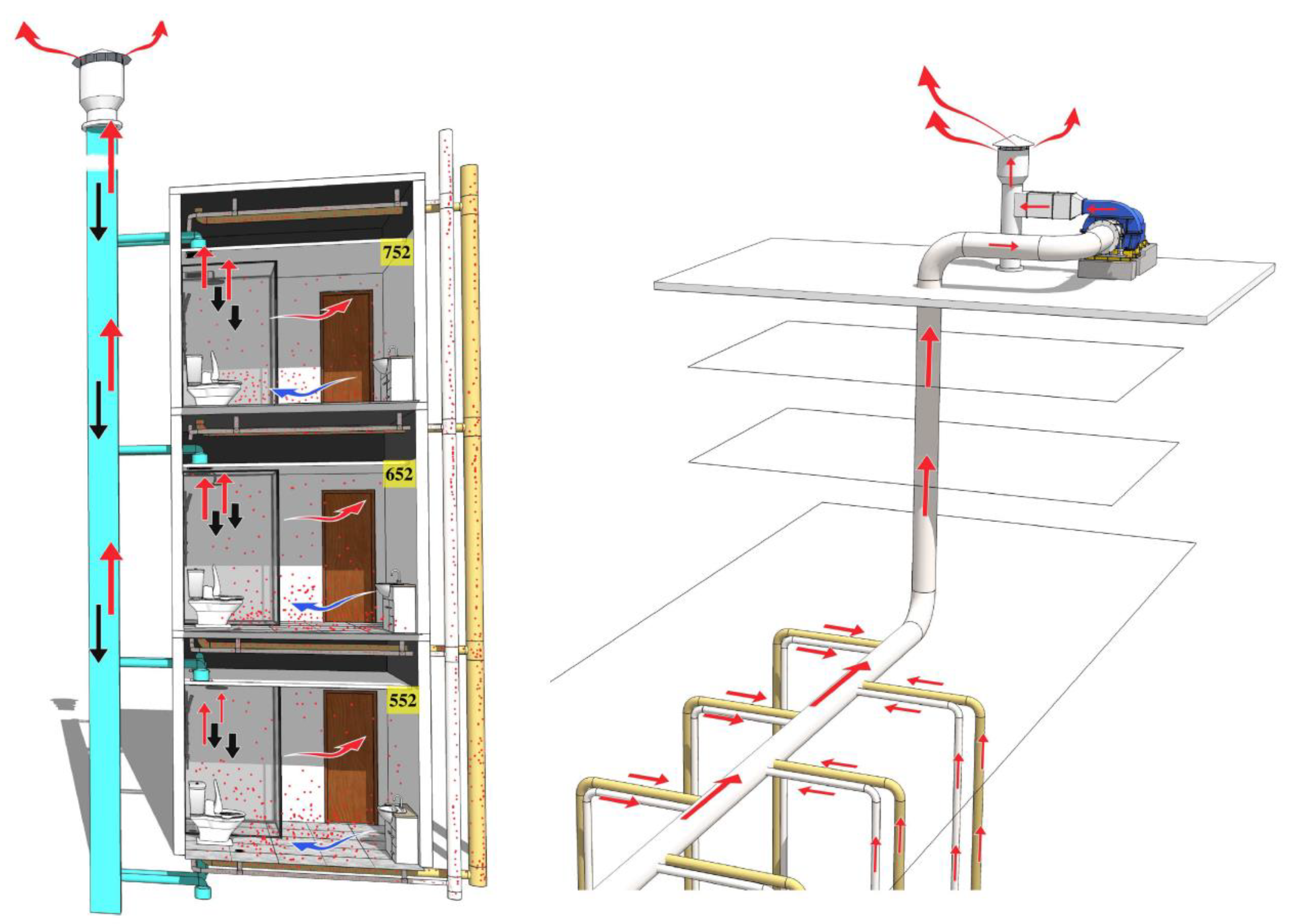
3.1. Simulated Aerosol Transmission Caused by Toilet Flushing
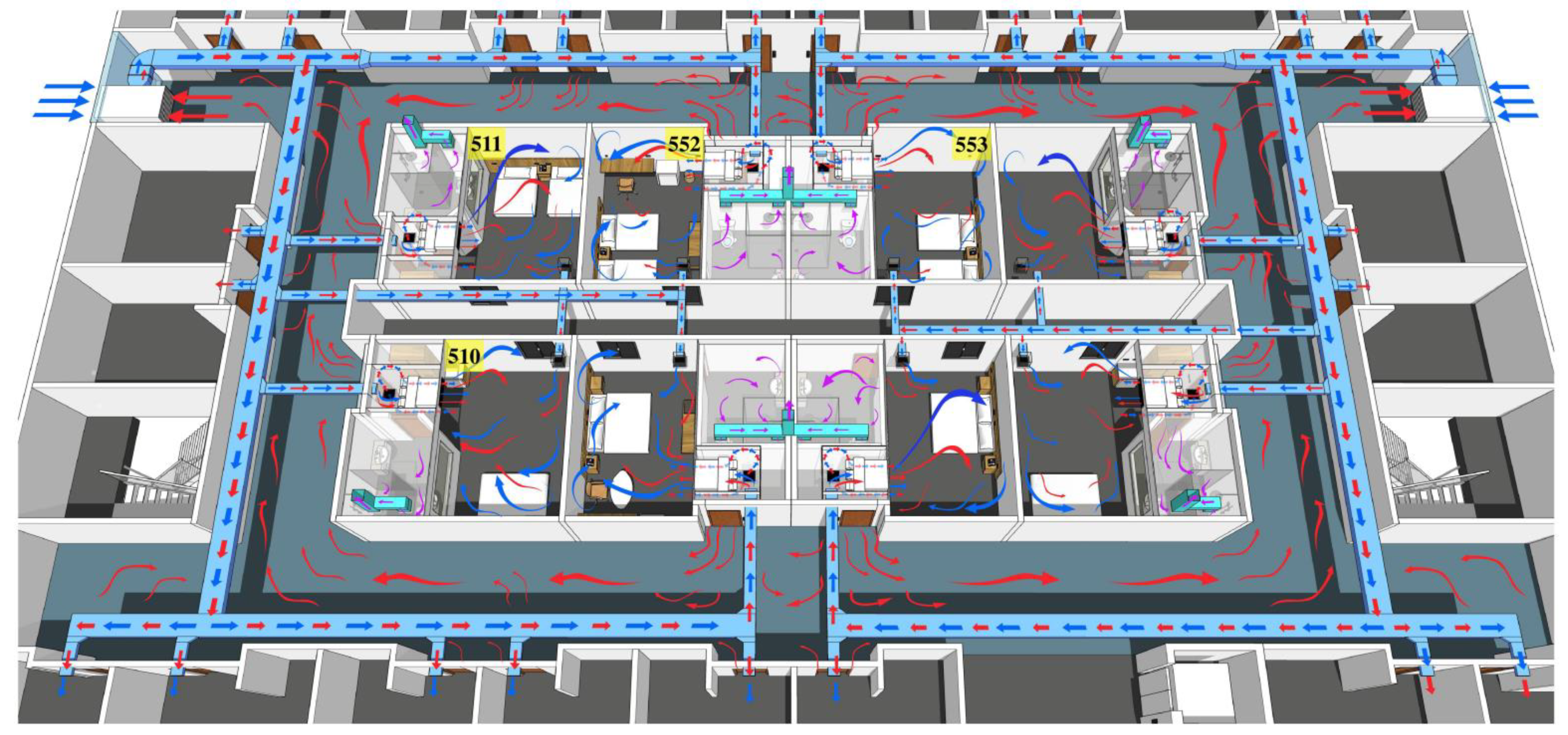
3.2. Aerosol Transmission Induced by Simulated Respiration
4. Discussion
4.1. Cross-Layer Vertical Transmission Caused by Sewage and Exhaust Pipe of the Bathroom
4.2. Same-Floor Transmission Caused by Ventilation Systems
4.3. Cross-Layer Non-Vertical Transmission Caused by the Superposition of the Exhaust System in the Bathroom and the Ventilation System in the Room
4.4. Influence Factors of Aerosol Transmission
5. Conclusions
6. Limitations
7. Sanitation Requirements for Environmental Management in Quarantine Hotels
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hung, L.S. The SARS epidemic in Hong Kong: What lessons have we learned? J. R. Soc. Med. 2003, 96, 374–378. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yu, I.T.; Li, Y.; Wong, T.W.; Tam, W.; Chan, A.T.; Lee, J.H.; Leung, D.Y.C.; Ho, T. Evidence of airborne transmission of the severe acute respiratory syndrome virus. N. Engl. J. Med. 2004, 350, 1731–1739. [Google Scholar] [CrossRef] [PubMed]
- Kang, M.; Wei, J.; Yuan, J.; Guo, J.; Zhang, Y.; Hang, J.; Qu, Y.; Qian, H.; Zhuang, Y.; Chen, X.; et al. Probable Evidence of Fecal Aerosol Transmission of SARS-CoV-2 in a High-Rise Building. Ann. Intern. Med. 2020, 173, 974–980. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Li, X.; Wang, Q.; Xu, J.; Jiang, Q.; Jiang, S.; Lyu, J.; Liu, S.; Ye, L.; Yuan, J.; et al. Field Simulation of Aerosol Transmission of SARS-CoV-2 in a Special Building Layout—Guangdong Province, China, 2021. China CDC Wkly. 2021, 3, 711–715. [Google Scholar] [CrossRef]
- Ma, J.; Qi, X.; Chen, H.; Li, X.; Zhang, Z.; Wang, H.; Sun, L.; Zhang, L.; Guo, J.; Morawska, L.; et al. Coronavirus Disease 2019 Patients in Earlier Stages Exhaled Millions of Severe Acute Respiratory Syndrome Coronavirus 2 Per Hour. Clin. Infect. Dis. 2021, 72, e652–e654. [Google Scholar] [CrossRef]
- Wang, W.; Xu, Y.; Gao, R.; Lu, R.; Han, K.; Wu, G.; Tan, W. Detection of SARS-CoV-2 in Different Types of Clinical Specimens. JAMA 2020, 323, 1843–1844. [Google Scholar] [CrossRef]
- Zhang, Y.; Chen, C.; Zhu, S.; Shu, C.; Wang, D.; Song, J.; Song, Y.; Zhen, W.; Feng, Z.; Wu, G.; et al. Isolation of 2019-nCoV from a Stool Specimen of a Laboratory-Confirmed Case of the Coronavirus Disease 2019 (COVID-19). China CDC Wkly. 2020, 2, 123–124. [Google Scholar] [CrossRef]
- Guan, W.; Ni, Z.; Hu, Y.; Liang, W.; Ou, C.; He, J.; Liu, L.; Shan, H.; Lei, C.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef]
- Li, X.; Wang, Q.; Ding, P.; Cha, Y.; Mao, Y.; Ding, C.; Gu, W.; Wang, Y.; Ying, B.; Zhao, X.; et al. Risk factors and on-site simulation of environmental transmission of SARS-CoV-2 in the largest wholesale market of Beijing, China. Sci. Total Environ. 2021, 778, 146040. [Google Scholar] [CrossRef]
- Xu, D.; Zhang, Z.; Wang, Q.; Li, X. Targeted Prevention and Control of Key Links in Airports to Mitigate Public Health Risks. China CDC Wkly. 2021, 3, 859–862. [Google Scholar] [CrossRef]
- Johnson, D.; Lynch, R.; Marshall, C.; Mead, K.; Hirst, D. Aerosol Generation by Modern Flush Toilets. Aerosol. Sci. Technol. 2013, 47, 1047–1057. [Google Scholar] [CrossRef] [PubMed]
- Lou, M.; Liu, S.; Gu, C.; Hu, H.; Tang, Z.; Zhang, Y.; Xu, C.; Li, F. The bioaerosols emitted from toilet and wastewater treatment plant: A literature review. Environ. Sci. Pollut. Res. Int. 2021, 28, 2509–2521. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.Y.; Wang, J.X.; Chen, X. Can a toilet promote virus transmission? From a fluid dynamics perspective. Phys. Fluids 2020, 32, 065107. [Google Scholar] [CrossRef] [PubMed]
- Elsamadony, M.; Fujii, M.; Miura, T.; Watanabe, T. Possible transmission of viruses from contaminated human feces and sewage: Implications for SARS-CoV-2. Sci. Total Environ. 2021, 755, 142575. [Google Scholar] [CrossRef] [PubMed]
- Jones, D.L.; Baluja, M.Q.; Graham, D.W.; Corbishley, A.; Mcdonald, J.E.; Malham, S.K.; Hillary, L.S.; Connor, T.R.; Gaze, W.H.; Moura, I.B.; et al. Shedding of SARS-CoV-2 in feces and urine and its potential role in person-to-person transmission and the environment-based spread of COVID-19. Sci. Total Environ. 2020, 749, 141364. [Google Scholar] [CrossRef] [PubMed]
- Qian, H.; Zheng, X. Ventilation control for airborne transmission of human exhaled bio-aerosols in buildings. J. Thorac. Dis. 2018, 10, S2295–S2304. [Google Scholar] [CrossRef] [PubMed]
- Correia, G.; Rodrigues, L.; Gameiro, D.S.M.; Goncalves, T. Airborne route and bad use of ventilation systems as non-negligible factors in SARS-CoV-2 transmission. Med. Hypotheses 2020, 141, 109781. [Google Scholar] [CrossRef] [PubMed]
- Pease, L.F.; Wang, N.; Salsbury, T.I.; Underhill, R.M.; Flaherty, J.E.; Vlachokostas, A.; Kulkarni, G.; James, D.P. Investigation of potential aerosol transmission and infectivity of SARS-CoV-2 through central ventilation systems. Build. Environ. 2021, 197, 107633. [Google Scholar] [CrossRef]
- Wang, Q.; Li, Y.; Lung, D.C.; Chan, P.T.; Dung, C.H.; Jia, W.; Miao, T.; Huang, J.; Chen, W.; Wang, Z.; et al. Aerosol transmission of SARS-CoV-2 due to the chimney effect in two high-rise housing drainage stacks. J. Hazard. Mater. 2022, 421, 126799. [Google Scholar] [CrossRef]
- Chirico, F.; Sacco, A.; Bragazzi, N.L.; Magnavita, N. Can Air-Conditioning Systems Contribute to the Spread of SARS/MERS/COVID-19 Infection? Insights from a Rapid Review of the Literature. Int. J. Environ. Res. Public Health 2020, 17, 6052. [Google Scholar] [CrossRef]
- Zhao, Y.; Richardson, B.; Takle, E.; Chai, L.; Schmitt, D.; Xin, H. Airborne transmission may have played a role in the spread of 2015 highly pathogenic avian influenza outbreaks in the United States. Sci. Rep. 2019, 9, 11755. [Google Scholar] [CrossRef] [PubMed]
- Nissen, K.; Krambrich, J.; Akaberi, D.; Hoffman, T.; Ling, J.; Lundkvist, A.; Svensson, L.; Salaneck, E. Long-distance airborne dispersal of SARS-CoV-2 in COVID-19 wards. Sci. Rep. 2020, 10, 19589. [Google Scholar] [CrossRef] [PubMed]
- Horve, P.F.; Dietz, L.G.; Fretz, M.; Constant, D.A.; Wilkes, A.; Townes, J.M.; Martindale, R.G.; Messer, W.B.; Van Den Wymelenberg, K.G. Identification of SARS-CoV-2 RNA in healthcare heating, ventilation, and air conditioning units. Indoor Air 2021, 31, 1826–1832. [Google Scholar] [CrossRef]
- Bazant, M.Z.; Bush, J. A guideline to limit indoor airborne transmission of COVID-19. Proc. Natl. Acad. Sci. USA 2021, 118, e2018995118. [Google Scholar] [CrossRef] [PubMed]
- Frumkin, H. COVID-19, the Built Environment, and Health. Environ. Health Perspect. 2021, 129, 075001. [Google Scholar] [CrossRef] [PubMed]
| Sample Location | Scenario 1/h | |||||||||||
| Room 552 | Room 652 | Room 752 | ||||||||||
| 0 | 0.5 | 1 | 1.5 | 0 | 0.5 | 1 | 1.5 | 0 | 0.5 | 1 | 1.5 | |
| floor drain, toilet lid and seat ring |  |  |  |  |  |  | ||||||
| Exhaust fan of bathroom |  |  |  |  |  |  |  | |||||
| air supply outlets of fresh air system and the air conditioning |  |  |  |  | ||||||||
| air sample (filter member) |  |  |  | |||||||||
| air sample (liquid) |  |  |  | |||||||||
| exhaust outlet of the roof |  | |||||||||||
| sewage pipe riser vent on the roof |  | |||||||||||
| Sample Location | Scenario 2/h | |||||||||||
| Room 553 | Room 652 | Room 705 | ||||||||||
| 1 | 2 | 3 | 4 | 1 | 2 | 3 | 4 | 1 | 2 | 3 | 4 | |
| air supply outlet of the air conditioning |  |  |  |  |  |  |  |  |  | |||
| table, door, bed |  |  |  |  |  |  |  | |||||
| air supply outlets of fresh air system |  |  |  |  |  |  |  |  | ||||
| air sample (filter member) |  |  |  |  |  |  | ||||||
| air sample (liquid) |  |  |  |  |  |  | ||||||
| exhaust outlet of the roof |  | |||||||||||
| sewage pipe riser vent on the roof |  | |||||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Z.; Li, X.; Wang, Q.; Zhao, X.; Xu, J.; Jiang, Q.; Jiang, S.; Lyu, J.; Liu, S.; Ye, L.; et al. Simulation Studies Provide Evidence of Aerosol Transmission of SARS-CoV-2 in a Multi-Story Building via Air Supply, Exhaust and Sanitary Pipelines. Int. J. Environ. Res. Public Health 2022, 19, 1532. https://doi.org/10.3390/ijerph19031532
Zhang Z, Li X, Wang Q, Zhao X, Xu J, Jiang Q, Jiang S, Lyu J, Liu S, Ye L, et al. Simulation Studies Provide Evidence of Aerosol Transmission of SARS-CoV-2 in a Multi-Story Building via Air Supply, Exhaust and Sanitary Pipelines. International Journal of Environmental Research and Public Health. 2022; 19(3):1532. https://doi.org/10.3390/ijerph19031532
Chicago/Turabian StyleZhang, Zhuona, Xia Li, Qin Wang, Xiaoning Zhao, Jin Xu, Qinqin Jiang, Sili Jiang, Jiayun Lyu, Shiqiang Liu, Ling Ye, and et al. 2022. "Simulation Studies Provide Evidence of Aerosol Transmission of SARS-CoV-2 in a Multi-Story Building via Air Supply, Exhaust and Sanitary Pipelines" International Journal of Environmental Research and Public Health 19, no. 3: 1532. https://doi.org/10.3390/ijerph19031532
APA StyleZhang, Z., Li, X., Wang, Q., Zhao, X., Xu, J., Jiang, Q., Jiang, S., Lyu, J., Liu, S., Ye, L., Yuan, J., Feng, W., Xie, J., Chen, Q., Zou, H., & Xu, D. (2022). Simulation Studies Provide Evidence of Aerosol Transmission of SARS-CoV-2 in a Multi-Story Building via Air Supply, Exhaust and Sanitary Pipelines. International Journal of Environmental Research and Public Health, 19(3), 1532. https://doi.org/10.3390/ijerph19031532





