Abstract
Critical illness insurance (CII) in China was introduced to protect high-cost groups from health expenditure shocks for the purpose of mutual aid. This study aimed to evaluate the impact of CII on the burden of high-cost groups in central rural China. Data were extracted from the basic medical insurance (BMI) hospitalization database of Xiantao City from January 2010 to December 2016. A total of 77,757 hospitalization records were included in our analysis. The out-of-pocket (OOP) expenses and reimbursement ratio (RR) were the two main outcome variables. Interrupted time series analysis with a segmented regression approach was adopted. Level and slope changes were reported to reflect short- and long-term effects, respectively. Results indicated that the number of high-cost inpatient visits, the average monthly hospitalization expenses, and OOP expenses per high-cost inpatient visit were increased after CII introduction. By contrast, the RR from BMI and non-reimbursable expenses ratio were decreased. The OOP expenses and RR covered by CII were higher than those uncovered. We estimated a significant level decrease in OOP expenses (p < 0.01) and rise in RR (p < 0.01), whereas the slope decreases of OOP expenses (p = 0.19) and rise of RR (p = 0.11) after the CII were non-significant. We concluded that the short-term effect of the CII policy is significant and contributes to decreasing OOP expenses and raising RR for high-cost groups, whereas the long-term effect is non-significant. These findings can be explained by increasing hospitalization expenses, many non-reimbursable expenses, low coverage for high-cost groups, and the unsustainability of the financing methods.
1. Introduction
Healthcare costs are concentrated among a small group of the most expensive patients. This group is identified as “high-need, high-cost” patients [1,2]. Previous studies have shown that the top 10%, top 5%, and top 1% high-cost patients roughly account for, respectively, 68%, 55%, and 24% of costs within a given year [3]. A few studies from the United States, European countries, Hong Kong, and Taiwan, all with different health insurance schemes and healthcare delivery systems, have presented similar findings [4,5,6,7,8]. These findings suggest that high-cost patients are a logical group to seek for cost-reduction financial support; caring for this group is an urgent priority [9].
Many insurance plans pursue this logic, and programs for “high-need, high-cost” patients have been developed [10,11]. In China, critical illness insurance (CII) is an insurance plan aimed at providing further reimbursement of high medical expenses associated with critical illness, based on the basic medical insurance (BMI) system. The initial objective of CII was to protect those “high-cost” patients from health expenditure shocks for the purpose of mutual aid and to solve the problems of illness-caused poverty. By May 2014, more than half of the rural regions in China had introduced the CII program [12]. An insured rural resident who incurs high medical costs can first receive reimbursement through BMI. Subsequently, the patients whose out-of-pocket (OOP) expenses still exceed the premium (usually the local income per capita) can obtain additional reimbursement [13]. To answer whether the CII policy is reaching its original objective, following the high-cost group is crucial.
The existing literature has mainly focused on describing and analyzing the policy design of CII [14,15,16]. Certain surveys have evaluated the effect of CII from the perspectives of financial burden [17,18] and equity [19]. These studies have targeted all beneficiaries with cross-sectional data. Research assessing the effect of CII on the high-cost group has not yet been conducted, nor has research using longitudinal data. Using the longitudinal BMI claim dataset of seven years, the present study adopted interrupted time series (ITS) analysis to evaluate the impact of CII on the burden of the high-cost group in central rural China.
2. Materials and Methods
2.1. Study Setting and the CII Policy
Xiantao City was selected as the research sample for two reasons. Geographically, the city is located in the central part of Hubei Province in China (Figure 1). In economic terms, Xiantao is representative of China in terms of per capita GDP. In 2013, the national per capita GDP was US$6995, and the per capita GDP in Xiantao was US$6854. Xiantao has a total area of 2538 km2 and had a total population of 1,563,500 at the end of 2016. The annual net income of rural residents in Xiantao was US$1005 in 2010 and US$2329 in 2016.

Figure 1.
Location of sample city.
In May 2013, the Xiantao government enacted the CII policy for the first time. Table 1 shows the details of the reimbursement system and its changes before and after the CII policy was implemented. Before the introduction of the CII policy, patients received reimbursement from BMI. The reimbursement methods differ between healthcare services in- and out-of-county. Patients seeking services in-county can apply for lower thresholds and a higher policy reimbursement ratio (PRR) for the same medical condition. In 2011, the local government abolished the deductible for seeking health services at primary hospitals in-county and raised the cap line from US$8070 to US$16,140. After the introduction of the CII policy, the local government raised the threshold of BMI. The reimbursement system includes BMI and CII, both of which share the same fund pool and reimbursement list. Expenses out of the scope of the list are non-reimbursable. The deductible of CII was US$1291, set with reference to per capita annual income. PRR was 50% for OOP payments within the range of US$1291–US$4842, 60% for payments of US$4842–US$8070, and 70% for OOP payments over US$8070.

Table 1.
Policy changes before and after the critical illness insurance (CII) policy was implemented.
For instance, if a patient’s medical expenses totaled US$19,368, assuming that all were included in the benefit package and could be reimbursed, the BMI could cover US$16,140. Before the CII policy was implemented, the reimbursement and the OOP expenses would have been US$16,140, and US$3228, respectively. After the CII policy was implemented, the OOP expenses became US$2260 (19,368 − 16,140 − (3228 − 1291) × 50%).
2.2. Data Collection
Data were extracted from the BMI hospitalization database of Xiantao City from January 2010 to December 2016, covering an observation period of seven years. High-cost visits, which were the top 10% of total hospitalization expenditures of records each year, were used in this study by referring to the criteria of previous studies [20,21]. A total of 77,757 hospitalization records were included in our analysis. During the study period 2010–2016, the total population and the aged proportion of the population grew, the male to female ratio increased, and the urbanization rate increased by 7.2% within the seven years. In general, the population structure was relatively stable.
2.3. Study Variables
To explore the changes in the quantity, structure, and expenses of high-cost inpatient visits before and after the CII policy, we accessed several key variables. The total numbers of high-cost inpatient visits were used to compare changes in quantity. The proportion of high-cost inpatients visits covered by CII was used to assess the scope of beneficiaries. Considering the differentiated reimbursement policy for medical treatment in- or out-of-county mentioned above, the proportion of high-cost inpatient visits in-county was assessed to compare the difference with out-of-county visits before and after the CII policy. The hospitalization expenses and OOP expenses of high-cost inpatient visits were also assessed. CII and BMI reimbursement ratio (RR) and non-reimbursable expenses ratio per high-cost inpatient visit were further measured.
The OOP expenses and RR were the two main outcome variables. For insured patients, part of their total medical expenses can be reimbursed by the insurance system; these expenses are called reimbursements. The remaining costs paid by such patients are called OOP expenses. In this study, the total medical expenses included all the categories of direct medical costs, typically including costs of treatment, laboratory tests, accommodation, materials, and drugs. Direct non-medical costs, such as transportation, and indirect costs, such as work loss, were not included. RR was defined as reimbursements divided by total medical expenses. With the function of reflecting the economic burden of patients and support from the reimbursement system, the OOP expenses and RR have been widely used in similar research [22,23,24,25].
Cost data inflation were adjusted with annual net income. Equivalent US$ has been reported using the average annual exchange rate.
2.4. Statistical Analysis
ITS analysis with a segmented regression approach [26] was adopted. ITS analysis is regarded as one of the strongest quasi-experimental methods that can be used to capture the longitudinal effects of policy interventions when a control group is lacking [27,28]. The segmented regression model was employed to detect the level and trend of outcome variables before the implementation of the CII policy, and the changes in level and trend after the implementation of the policy. Level change indicates the change at the moment of intervention. Slope change indicates a long-term effect of the policy. The regression model is as follows:
where represents the mean value of each evaluation indicator, and represents a continuous variable indicating time in years at time t from the start of the observation period. represents an indicator for time t occurring before (intervention = 0) or after (intervention = 1) the implementation of the CII policy. May 2013 was defined as the start time of the intervention. represents a continuous variable counting the number of months after the intervention at , coded 0 before the CII (from January 2010 to April 2013) and coded 1–44 after the CII (from May 2013 to December 2016). Detailed information is presented in Appendix A.
estimates the baseline level of the outcome at time 0. estimates the change that occurs per month before the CII (baseline slope). estimates the immediate level change after the CII (level change after the CII). estimates the change in the trend after the CII (slope change after the CII), compared with the monthly trend before the CII. is an error term.
The Durbin–Watson test was conducted to detect autocorrelations. The Cochrane–Orcutt auto-regression procedure was used to correct for first-order serially correlated errors when needed. All analyses were performed using STATA 12.0 (STATA Corp., College Station, TX, USA).
3. Results
3.1. Changes of Indicators before and after the Implementation of the CII Policy
Table 2 shows that after the introduction of the CII policy, the total high-cost inpatient visits increased, and the proportion of high-cost inpatient visits covered by the CII accounted for 44% of monthly visits on average. The proportion of in-county inpatient visits increased and accounted for 86.9% of monthly visits on average. The average monthly hospitalization expenses and OOP expenses per high-cost inpatient visit all increased. By contrast, the average monthly BMI RR and non-reimbursable expenses ratio per high-cost inpatient visit decreased.

Table 2.
Key indicators of policy effects in Xiantao.
3.2. Trends of Out-of-Pocket Expenses and Reimbursement Ratio (RR) in 2010–2016
Figure 2 and Figure 3 present the time series of OOP expenses and RR of high-cost visits from 2010 to 2016. Figure 2 displays a rough upward tendency of average monthly OOP expenses per high-cost visit, which increased from US$1081 to US$1927. Figure 3 shows the process of average monthly RR per high-cost visit, where it first descended and then slightly rose. The average monthly OOP expenses per visit out-of-county were higher than those in-county, whereas the situation of RR was the reverse. After the implementation of the CII policy, the average monthly OOP expenses and RR per visit of high-cost visits covered by the CII were higher than those uncovered by the CII. That is, those covered by CII indeed had a larger financial burden than those uncovered and those who received additional help from the CII policy.
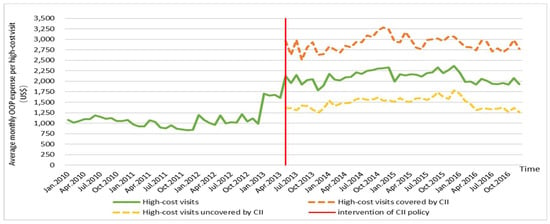
Figure 2.
Trends of out-of-pocket (OOP) expenses in 2010–2016.
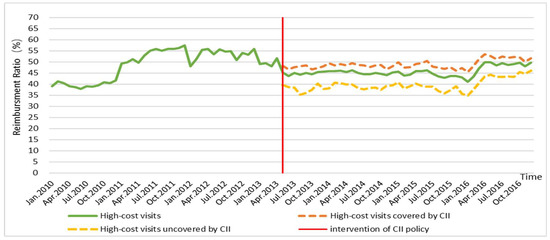
Figure 3.
Trends of reimbursement ratio (RR) in 2010–2016.
3.3. Impact of the Critical Illness Insurance Policy
Table 3 presents the impact of the CII policy on OOP expenses and RR. Before the introduction of CII, an increasing trend existed in the OOP expenses. After the CII was implemented, a significant abrupt level change was observed, with an increase of US$682.6 (p < 0.01, 95% confidence interval (CI) = 446 to 919.2). The slope change showed a decrease of US$9.1, but was not statistically significant (p = 0.19, 95% CI = −22.6 to 4.4). A decrease trend occurred in the RR during the pre-implementation period. During the post-implementation period, a significant abrupt level change was noted, with a decrease of 7.9% (p < 0.01, 95% CI = −12.1 to −3.7). The slope change showed an increase of 0.3%, but was not statistically significant (p = 0.11, 95% CI = −0.7 to 0.1). These changes can be seen in Appendix B.

Table 3.
Interrupted time series (ITS) analysis results of policy effect on OOP expenses and reimbursement ratio (RR) in Xiantao.
4. Discussion
This study described an overview of the changes in the OOP expenses and RR of high-cost inpatient visits among rural residents after the implementation of the CII policy in May 2013. Through ITS analysis, we estimated a statistically significant decrease in OOP expenses (p < 0.01) and rise in RR (p < 0.01) for the high-cost group after the introduction of CII. This finding indicates that CII has an immediate impact on easing the financial burden of this group. In the short term, the CII is an effective policy because it provides further protection beyond BMI. This result is in line with those shown in previous studies [17,18,19].
However, the decrease trend of OOP expenses (p = 0.19) and the rising trend of RR (p = 0.11) after CII were not statistically significant. Therefore, the CII policy cannot effectively ease the burden of high-cost rural residents in the long term. To the best of our knowledge, our study is the first quantitative research to investigate the long-term effects of the CII policy on financial burden.
Several possible reasons may account for these invalid long-term effects.
First, the hospitalization expenses greatly increased. The uncovered medical expenses were a considerable element of total hospitalization expenses. According to the research of Pavón-León et al., uncovered medical expenses rise from 12.8% to 27.5% as total medical costs increase [29]. The high-cost group usually needs additional medical consumable materials and drugs that are not included in the reimbursement list. This part of the medical expenses is ignored and not reimbursed by either BMI or CII. We found that non-reimbursable expenses accounted for more than a quarter of the total expense for high-cost inpatient visits, even after the implementation of the CII policy.
Although the CII policy helps keep inpatient visits in-county, we found nearly 15% of high-cost inpatient visits were out-of-county. However, reimbursement rules were typically not that generous for out-of-county visits, thus aggregating the financial burden of the high-cost group.
Moreover, the high-cost beneficiaries of the CII policy are limited. In this study, no more than half high-cost visits were found to be covered by the CII policy; and the OOP expenses covered by the CII were higher than those uncovered. On the one hand, the population insured with CII consisted of patients whose OOP expenses still exceeded the deductible after being reimbursed by BMI. The medical costs of this group are much higher than those of the uninsured. On the other hand, only costs within the scope of the CII can be reimbursed, and the CII has the same limited reimbursement list as BMI. In addition, the PRR is not high enough, and thus the proportion of reimbursement was insufficient to make up for the gap of medical costs between the insured and uninsured groups. These factors may explain why the OOP expenses of the population insured with CII can be higher than those uninsured.
The CII fund comes from the BMI fund pool, giving rise to great pressure on the BMI fund pool over time and thus comprising the sustainability of the safeguard. Xiantao City has lowered the BMI PRR to alleviate fund pressure, which explains why the BMI effective RR decreased by nearly 5% after the introduction of the CII policy.
To further ease the financial burden of high-cost beneficiaries of the CII policy in the long run, many rules can be improved. We suggest considering other aspects, such as cost of critical illness at the local level, when setting deductibles, not just going by per capita income of rural residents. An additional and specific reimbursement list which contains commonly used drugs and materials for the high-cost group is needed. Raising extra funds for the CII policy through diversified financing channels, such as government finance, charity, and civil administration, would be a feasible way to ensure sustainability.
The limitations of this study should be mentioned. We only conducted the study in one city in central China. However, as the CII policy operates at the city level, we acquired complete and high-quality data focusing on a single city. The synergistic effects of other health policies, such as medical financial assistance, were not considered.
5. Conclusions
This study adopted ITS analysis to evaluate the impact of the CII on the burden of high-cost group in central rural China with a seven-year longitudinal dataset. The short and long-term effects were investigated. The results indicated that the short-term effect was significant and contributed to decreasing the OOP expenses and raising the RR of the high-cost group. By contrast, the long-term effect was non-significant. Explanations such as increasing hospitalization expenses, large non-reimbursable expenses, low coverage for the high-cost group, and unsustainability of financing methods were also explored. Suggestions have been made to improve the CII policy and alleviate the financial burden of the high-cost group, for example, setting the deductible with reference to the cost of critical illness at the local level, developing an additional and specific reimbursement list, and raising extra funds for the CII policy through diversified financing channels. Further research is necessary to evaluate the long-term effects of the CII policy with a wide scope.
Author Contributions
Conceptualization, L.L. and L.X.; methodology, L.L., J.J.; formal analysis, L.L.; investigation, J.J., X.W., L.Z. and Z.Z.; data curation, L.L., J.J.; writing—original draft preparation, L.L.; writing—review and editing, L.L., J.J. and L.X.; supervision, L.X.; project administration, L.X.; funding acquisition, L.X.
Funding
This study is supported by the National Natural Science Foundation of China, grant number 71573095.
Acknowledgments
We would like to acknowledge the Health and Planning Commission of Xiantao city for their support on the research.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A

Table A1.
Detailed information of interrupted time series (ITS) analysis, medical expenses and medical services utilization.
Table A1.
Detailed information of interrupted time series (ITS) analysis, medical expenses and medical services utilization.
| Year | Observation | Time | Intervention | Time after Intervention | THE 1 (US$) | OOP 2 (US$) | RR 3 (%) | Inpatient Visits |
|---|---|---|---|---|---|---|---|---|
| Jan. 2010 | 1 | 1 | 0 | 0 | 1770.3 | 1080.5 | 39.0 | 359 |
| Feb. 2010 | 2 | 2 | 0 | 0 | 1724.1 | 1014.6 | 41.2 | 261 |
| Mar. 2010 | 3 | 3 | 0 | 0 | 1757.8 | 1047.1 | 40.4 | 475 |
| Apr. 2010 | 4 | 4 | 0 | 0 | 1798.5 | 1095.9 | 39.1 | 480 |
| May 2010 | 5 | 5 | 0 | 0 | 1791.5 | 1098.6 | 38.7 | 444 |
| June 2010 | 6 | 6 | 0 | 0 | 1913.7 | 1190.0 | 37.8 | 455 |
| July 2010 | 7 | 7 | 0 | 0 | 1881.4 | 1147.2 | 39.0 | 429 |
| Aug. 2010 | 8 | 8 | 0 | 0 | 1812.8 | 1108.4 | 38.9 | 436 |
| Sep. 2010 | 9 | 9 | 0 | 0 | 1852.1 | 1120.5 | 39.5 | 433 |
| Oct. 2010 | 10 | 10 | 0 | 0 | 1771.0 | 1048.5 | 40.8 | 345 |
| Nov. 2010 | 11 | 11 | 0 | 0 | 1766.0 | 1051.7 | 40.4 | 537 |
| Dec. 2010 | 12 | 12 | 0 | 0 | 1840.6 | 1074.2 | 41.6 | 769 |
| Jan. 2011 | 13 | 13 | 0 | 0 | 1909.8 | 971.2 | 49.1 | 398 |
| Feb. 2011 | 14 | 14 | 0 | 0 | 1841.5 | 924.3 | 49.8 | 329 |
| Mar. 2011 | 15 | 15 | 0 | 0 | 1895.4 | 924.7 | 51.2 | 599 |
| Apr. 2011 | 16 | 16 | 0 | 0 | 2111.4 | 1065.3 | 49.5 | 562 |
| May 2011 | 17 | 17 | 0 | 0 | 2182.2 | 1029.5 | 52.8 | 627 |
| June 2011 | 18 | 18 | 0 | 0 | 1994.8 | 896.5 | 55.1 | 750 |
| July 2011 | 19 | 19 | 0 | 0 | 1982.1 | 875.9 | 55.8 | 789 |
| Aug. 2011 | 20 | 20 | 0 | 0 | 2116.7 | 953.2 | 55.0 | 785 |
| Sep. 2011 | 21 | 21 | 0 | 0 | 1975.2 | 872.2 | 55.8 | 719 |
| Oct. 2011 | 22 | 22 | 0 | 0 | 1930.3 | 853.3 | 55.8 | 655 |
| Nov. 2011 | 23 | 23 | 0 | 0 | 1899.0 | 833.1 | 56.1 | 759 |
| Dec. 2011 | 24 | 24 | 0 | 0 | 1964.4 | 838.3 | 57.3 | 926 |
| Jan. 2012 | 25 | 25 | 0 | 0 | 2304.4 | 1199.2 | 48.0 | 608 |
| Feb. 2012 | 26 | 26 | 0 | 0 | 2217.3 | 1081.6 | 51.2 | 828 |
| Mar. 2012 | 27 | 27 | 0 | 0 | 2246.2 | 1003.4 | 55.3 | 960 |
| Apr. 2012 | 28 | 28 | 0 | 0 | 2167.4 | 959.1 | 55.7 | 911 |
| May 2012 | 29 | 29 | 0 | 0 | 2550.1 | 1189.8 | 53.3 | 1035 |
| June 2012 | 30 | 30 | 0 | 0 | 2243.0 | 996.3 | 55.6 | 1019 |
| July 2012 | 31 | 31 | 0 | 0 | 2263.6 | 1027.4 | 54.6 | 1140 |
| Aug. 2012 | 32 | 32 | 0 | 0 | 2245.7 | 1015.0 | 54.8 | 1057 |
| Sep. 2012 | 33 | 33 | 0 | 0 | 2459.3 | 1211.7 | 50.7 | 1064 |
| Oct. 2012 | 34 | 34 | 0 | 0 | 2260.9 | 1037.9 | 54.1 | 1041 |
| Nov. 2012 | 35 | 35 | 0 | 0 | 2380.8 | 1115.4 | 53.1 | 1077 |
| Dec. 2012 | 36 | 36 | 0 | 0 | 2244.2 | 989.7 | 55.9 | 1041 |
| Jan. 2013 | 37 | 37 | 0 | 0 | 3340.6 | 1702.5 | 49.0 | 963 |
| Feb. 2013 | 38 | 38 | 0 | 0 | 3274.3 | 1656.1 | 49.4 | 564 |
| Mar. 2013 | 39 | 39 | 0 | 0 | 3231.4 | 1677.5 | 48.1 | 888 |
| Apr. 2013 | 40 | 40 | 0 | 0 | 3314.3 | 1605.7 | 51.6 | 931 |
| May 2013 | 41 | 41 | 1 | 1 | 3863.9 | 2117.3 | 45.2 | 725 |
| June 2013 | 42 | 42 | 1 | 2 | 3461.8 | 1954.2 | 43.5 | 729 |
| July 2013 | 43 | 43 | 1 | 3 | 3907.3 | 2146.2 | 45.1 | 925 |
| Aug. 2013 | 44 | 44 | 1 | 4 | 3448.6 | 1919.8 | 44.3 | 905 |
| Sep. 2013 | 45 | 45 | 1 | 5 | 3689.0 | 2030.8 | 44.9 | 773 |
| Oct. 2013 | 46 | 46 | 1 | 6 | 3691.9 | 2048.7 | 44.5 | 1010 |
| Nov. 2013 | 47 | 47 | 1 | 7 | 3285.1 | 1790.1 | 45.5 | 1051 |
| Dec. 2013 | 48 | 48 | 1 | 8 | 3486.2 | 1892.4 | 45.7 | 1135 |
| Jan. 2014 | 49 | 49 | 1 | 9 | 4016.0 | 2172.4 | 45.9 | 1067 |
| Feb. 2014 | 50 | 50 | 1 | 10 | 3760.6 | 2037.1 | 45.8 | 677 |
| Mar. 2014 | 51 | 51 | 1 | 11 | 3749.1 | 2025.6 | 46.0 | 1095 |
| Apr. 2014 | 52 | 52 | 1 | 12 | 3836.3 | 2096.7 | 45.3 | 984 |
| May 2014 | 53 | 53 | 1 | 13 | 3904.6 | 2100.3 | 46.2 | 1004 |
| June 2014 | 54 | 54 | 1 | 14 | 4028.7 | 2212.2 | 45.1 | 1056 |
| July 2014 | 55 | 55 | 1 | 15 | 3911.0 | 2173.0 | 44.4 | 1170 |
| Aug. 2014 | 56 | 56 | 1 | 16 | 4034.8 | 2244.4 | 44.4 | 1032 |
| Sep. 2014 | 57 | 57 | 1 | 17 | 4136.9 | 2270.9 | 45.1 | 1071 |
| Oct. 2014 | 58 | 58 | 1 | 18 | 4153.6 | 2300.6 | 44.6 | 1025 |
| Nov. 2014 | 59 | 59 | 1 | 19 | 4136.7 | 2313.0 | 44.1 | 1016 |
| Dec. 2014 | 60 | 60 | 1 | 20 | 4254.8 | 2330.0 | 45.2 | 1397 |
| Jan. 2015 | 61 | 61 | 1 | 21 | 3673.4 | 1996.6 | 45.6 | 898 |
| Feb. 2015 | 62 | 62 | 1 | 22 | 3857.2 | 2167.3 | 43.8 | 997 |
| Mar. 2015 | 63 | 63 | 1 | 23 | 3834.0 | 2140.5 | 44.2 | 1388 |
| Apr. 2015 | 64 | 64 | 1 | 24 | 4005.1 | 2168.1 | 45.9 | 1207 |
| May 2015 | 65 | 65 | 1 | 25 | 3969.7 | 2154.0 | 45.7 | 1190 |
| June 2015 | 66 | 66 | 1 | 26 | 3928.5 | 2114.2 | 46.2 | 1260 |
| July 2015 | 67 | 67 | 1 | 27 | 3966.8 | 2198.5 | 44.6 | 1407 |
| Aug. 2015 | 68 | 68 | 1 | 28 | 3918.8 | 2216.5 | 43.4 | 1328 |
| Sep. 2015 | 69 | 69 | 1 | 29 | 4077.6 | 2328.7 | 42.9 | 1200 |
| Oct. 2015 | 70 | 70 | 1 | 30 | 3892.7 | 2193.2 | 43.7 | 1160 |
| Nov. 2015 | 71 | 71 | 1 | 31 | 4015.3 | 2265.3 | 43.6 | 1188 |
| Dec. 2015 | 72 | 72 | 1 | 32 | 4153.8 | 2367.1 | 43.0 | 1368 |
| Jan. 2016 | 73 | 73 | 1 | 33 | 3734.3 | 2201.7 | 41.0 | 1359 |
| Feb. 2016 | 74 | 74 | 1 | 34 | 3519.7 | 1988.5 | 43.5 | 1201 |
| Mar. 2016 | 75 | 75 | 1 | 35 | 3764.9 | 1996.9 | 47.0 | 1523 |
| Apr. 2016 | 76 | 76 | 1 | 36 | 3830.5 | 1919.4 | 49.9 | 1152 |
| May 2016 | 77 | 77 | 1 | 37 | 4106.5 | 2059.6 | 49.8 | 1165 |
| June 2016 | 78 | 78 | 1 | 38 | 3911.4 | 2015.6 | 48.5 | 1178 |
| July 2016 | 79 | 79 | 1 | 39 | 3824.6 | 1937.5 | 49.3 | 1292 |
| Aug. 2016 | 80 | 80 | 1 | 40 | 3748.3 | 1926.7 | 48.6 | 1288 |
| Sep. 2016 | 81 | 81 | 1 | 41 | 3837.0 | 1955.5 | 49.0 | 1095 |
| Oct. 2016 | 82 | 82 | 1 | 42 | 3829.5 | 1926.1 | 49.7 | 1007 |
| Nov. 2016 | 83 | 83 | 1 | 43 | 4005.1 | 2078.4 | 48.1 | 1145 |
| Dec. 2016 | 84 | 84 | 1 | 44 | 3832.3 | 1926.9 | 49.7 | 1466 |
1 THE: total hospitalization expenses, 2 OOP: Out-of-pocket, 3 RR: reimbursement ratio.
Appendix B
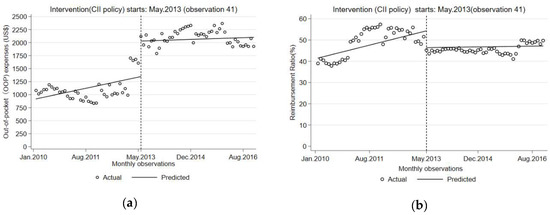
Figure A1.
Graphical demonstration of interrupted time series (ITS) analysis. (a) CII policy effect on OOP expenses; (b) CII policy effect on Reimbursement Ratio (RR).
References
- Zook, C.J.; Moore, F.D. High-cost users of medical care. N. Engl. J. Med. 1980, 302, 996–1002. [Google Scholar] [CrossRef]
- Hayes, S.L.; Salzberg, C.A.; Mccarthy, D.; Radley, D.C.; Abrams, M.K.; Shah, T.; Anderson, G.F. High-Need, High-Cost Patients: Who Are They and How Do They Use Health Care? A Population-Based Comparison of Demographics, Health Care Use, and Expenditures. Issue Brief 2016, 26, 1. [Google Scholar]
- Wammes, J.J.G.; van der Wees, P.J.; Tanke, M.A.C.; Westert, G.P.; Jeurissen, P.P.T. Systematic review of high-cost patients’ characteristics and healthcare utilisation. BMJ Open 2018, 8, e023113. [Google Scholar] [CrossRef]
- Wodchis, W.P.; Austin, P.C.; Henry, D.A. A 3-year study of high-cost users of health care. Can. Med Assoc. J. 2016, 188, 182–188. [Google Scholar] [CrossRef]
- Ku, L.J.E.; Chiou, M.J.; Liu, L.F. Variations in the persistence of health expenditures and the implications for the design of capitation payments in Taiwan. J. Health Serv. Res. Policy 2015, 20, 146–153. [Google Scholar] [CrossRef]
- Zulman, D.M.; Chee, C.P.; Wagner, T.H.; Yoon, J.; Cohen, D.M.; Holmes, T.H.; Ritchie, C.; Asch, S.M. Multimorbidity and healthcare utilisation among high-cost patients in the US Veterans Affairs Health Care System. BMJ Open 2015, 5, e007771. [Google Scholar] [CrossRef]
- Feder, J.L. Predictive Modeling and Team Care for High-Need Patients at HealthCare Partners. Health Aff. 2011, 30, 416–418. [Google Scholar] [CrossRef][Green Version]
- Xin, H. How Do High Cost-Sharing Policies for Physician Care Affect Inpatient Care Use and Costs Among People with Chronic Disease? J. Ambul. Care Manag. 2015, 38, 100–108. [Google Scholar] [CrossRef]
- Blumenthal, D.; Chernof, B.; Fulmer, T.; Lumpkin, J.; Selberg, J. Caring for High-Need, High-Cost Patients—An Urgent Priority. N. Engl. J. Med. 2016, 375, 909–911. [Google Scholar] [CrossRef]
- Anderson, G.F.; Ballreich, J.; Bleich, S.; Boyd, C.; Dugoff, E.; Leff, B.; Salzburg, C.; Wolff, J. Attributes Common to Programs That Successfully Treat High-Need, High-Cost Individuals. Am. J. Manag. Care 2015, 21, e597–e600. [Google Scholar]
- Brown, R.S.; Peikes, D.; Peterson, G.; Schore, J.; Razafindrakoto, C.M. Six Features Of Medicare Coordinated Care Demonstration Programs That Cut Hospital Admissions Of High-Risk Patients. Health Aff. 2012, 31, 1156–1166. [Google Scholar] [CrossRef]
- Progress of Critical Illness Insurance Program Based on New Rural Cooperative Medical System. Available online: http://www.nhc.gov.cn/xcs/s3574/201408/3b8402adec4843f0bf36e114227e09de.shtml (accessed on 3 April 2019).
- General Office of the State Council Guiding Opinions on Carrying out Critical Disease Insurance Work for Urban and Rural Residents. Available online: http://www.gov.cn/zhengce/content/2015-08/02/content_10041.htm (accessed on 27 Feburary 2019).
- Li, H.; Jiang, L. Catastrophic medical insurance in China. Lancet 2017, 390, 1724–1725. [Google Scholar] [CrossRef]
- Zhang, Y.; Vanneste, J.; Xu, J.; Liu, X. Critical Illness Insurance to alleviate catastrophic health expenditures: New evidence from China. Int. J. Health Econ. Manag. 2019, 19, 193–212. [Google Scholar] [CrossRef]
- Liu, P.; Jiang, L.; Li, C.; Sun, M.; Rieger, A.; Hao, M. How to deal with burden of critical illness: A comparison of strategies in different areas of China. Pak. J. Med. Sci. 2014, 30, 659–663. [Google Scholar] [CrossRef]
- Zhao, S.W.; Zhang, X.Y.; Dai, W.; Ding, Y.X.; Chen, J.Y.; Fang, P.Q. Effect of the catastrophic medical insurance on household catastrophic health expenditure: Evidence from China. Gac. Sanit. 2019, in press. [Google Scholar] [CrossRef]
- Fang, P.; Pan, Z.; Zhang, X.; Bai, X.; Gong, Y.; Yin, X. The effect of critical illness insurance in China. Medicine 2018, 97, e11362. [Google Scholar] [CrossRef]
- Jiang, J.; Chen, S.; Xin, Y.; Wang, X.; Zeng, L.; Zhong, Z.; Xiang, L. Does the critical illness insurance reduce patients’ financial burden and benefit the poor more: A comprehensive evaluation in rural area of China. J. Med. Econ. 2019, 22, 455–463. [Google Scholar] [CrossRef]
- Figueroa, J.F.; Zhou, X.; Jha, A.K. Characteristics and Spending Patterns of Persistently High-Cost Medicare Patients. Health Aff. 2019, 38, 107–114. [Google Scholar] [CrossRef]
- Nguyen, N.H.; Khera, R.; Ohno-Machado, L.; Sandborn, W.J.; Singh, S. Annual Burden and Costs of Hospitalization for High-Need, High-Cost Patients with Chronic Gastrointestinal and Liver Diseases. Clin. Gastroenterol. Hepatol. 2018, 16, 1284. [Google Scholar] [CrossRef]
- Zeng, Y.; Li, J.; Yuan, Z.; Fang, Y. The effect of China’s new cooperative medical scheme on health expenditures among the rural elderly. Int. J. Equity Health 2019, 18, 27. [Google Scholar] [CrossRef]
- Ma, J.; Xu, J.; Zhang, Z.; Wang, J. New cooperative medical scheme decreased financial burden but expanded the gap of income-related inequity: Evidence from three provinces in rural China. Int. J. Equity Health 2016, 15, 72. [Google Scholar] [CrossRef]
- Li, X.; Zhou, Q.; Wang, X.; Su, S.; Zhang, M.; Jiang, H.; Wang, J.; Liu, M. The effect of low insurance reimbursement on quality of care for non-small cell lung cancer in China: A comprehensive study covering diagnosis, treatment, and outcomes. BMC Cancer 2018, 18, 683. [Google Scholar] [CrossRef]
- Xiang, L.; Pan, Y.; Hou, S.; Zhang, H.; Sato, K.D.; Li, Q.; Wang, J.; Tang, S. The impact of the new cooperative medical scheme on financial burden of tuberculosis patients: Evidence from six counties in China. Infect. Dis. Poverty 2016, 5, 8. [Google Scholar] [CrossRef]
- Linden, A. Conducting interrupted time-series analysis for single- and multiple-group comparisons. Stata J. 2015, 15, 480–500. [Google Scholar] [CrossRef]
- Wagner, A.K.; Soumerai, S.B.; Zhang, F.; Ross-Degnan, D. Segmented regression analysis of interrupted time series studies in medication use research. J. Clin. Pharm. Ther. 2002, 27, 299–309. [Google Scholar] [CrossRef]
- Sloboda, B. Introduction to Time Series Analysis and Forecasting. Int. J. Forecast. 2009, 25, 209–211. [Google Scholar] [CrossRef]
- Pavon-Leon, P.; Reyes-Morales, H.; Martinez, A.J.; Maria Mendez-Main, S.; del Carmen Gogeascoechea-Trejo, M.; Blazquez-Morales, M.S.L. Out-of-pocket expenditure by elderly adults enrolled in a public health insurance programme in Mexico. Gac. Sanit. 2017, 31, 286–291. [Google Scholar]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).