Abstract
Background and Objectives: Hepatic resection offers promising outcomes for patients with hepatocellular carcinoma (HCC) but can be constrained by factors like patient suitability. Continuous advancements in laparoscopic and robotic technologies have made minimally invasive hepatectomies (MIHs) a viable alternative to open hepatectomies with benefits in terms of recovery and complications. Materials and Methods: We completed a retrospective review on 138 HCC patients who underwent OH or MIH between 2010 and 2020 at the Hume-Lee Transplant Center. Univariate and multivariate analyses were completed on demographic, clinical, and tumor-specific data to assess the impact of these variables on overall and disease-free survival at 1, 3, and 5 years. Preoperative metrics like length of hospital stay (LOS) and operation duration were also evaluated. Results: Of the 109 OH and 29 MIH patients, MIH patients demonstrated shorter LOS and operative times. However, overall survival (OS) and disease-free survival (DFS) were similar between groups, with no significant variations in 1-, 3-, and 5-year survival rates. Age > 60 years and a lack of preoperative transcatheter arterial chemoembolization (TACE) were significant predictors of inferior OS and DFS in multivariate analyses. Conclusions: MIH is an efficient substitute for OH with comparable survival, even in older patients. The reduced LOS and operation time enhance its feasibility, and older patients previously denied for curative resection may qualify for MIH. Preoperative TACE also enhances survival outcomes, emphasizing its general role in managing resectable HCCs. Both robotic and laparoscopic hepatectomies offer acceptable short- and long-term clinical outcomes, highlighting MIH as the standard choice for HCC patients.
1. Introduction
Hepatocellular carcinoma (HCC) is the third leading cause of cancer death worldwide, accounting for 70–85% of all primary liver cancers [1]. HCC is typically associated with hepatitis B or C, alcohol use, and non-alcoholic fatty liver disease [2]. With a 5-year survival rate of approximately 18%, its prognosis remains poor without treatment. The World Health Organization estimates more than 1 million cancer deaths from liver cancer by 2030 [2,3]. The stage of disease primarily determines treatment options for HCC. Surgical treatment offers the highest cure rates but is reserved for early-stage (I/II) HCC with minimal liver disease [2,4,5,6]. Liver transplantation, while preferred for HCC patients with cirrhosis (80% of HCC cases), is limited by organ shortage and strict selection criteria [7,8]. Thus, the role of surgical resection in patients with localized HCC has garnered greater interest, along with improvements in clinical decision algorithms [9,10]. Previously, surgical resection was reserved for patients with a solitary tumor of any size or up to three nodules of <3 cm [11,12]. However, technological advancements in techniques and devices have allowed major hepatectomies to be performed in patients with larger, more malignant liver lesions [13]. Laparoscopic techniques have long been established as a safe and effective alternative to open surgery, providing improved visualization, magnification, less intraoperative blood loss, and more meticulous dissection [14,15,16]. Smaller incisions in the anterior abdominal wall minimize interruption in portosystemic collateral vessels, reducing liver failure and ascites recurrence in patients with severe cirrhosis [17,18,19,20].
Furthermore, robotic platforms have addressed constraints associated with laparoscopic hepatectomies [21]. Robotic systems can achieve safer surgical margins by adhering to curvilinear resection planes through well-articulated instruments and contact ultrasonography via robotic probes [22,23]. Improved visualization, ergonomics, and range of motion within the abdominal cavity may enhance handling, dexterity, and fine dissection maneuvers [24]. The present study evaluates the short- and long-term outcomes of patients receiving open hepatectomy surgery (OH) versus minimally invasive hepatectomy surgery (MIH) for hepatocellular carcinoma. Through a decade of experience at a tertiary referral center, this study aims to assess the effectiveness and safety of MIH in managing HCC, potentially influencing surgical protocols and patient care.
2. Materials and Methods
Patient confidentiality and privacy were strictly maintained, and all data were anonymized to protect the participants’ identities. The Institutional Review Board at Virginia Commonwealth University approved our study under protocol number HM20007405 in 2021.
2.1. Patient Selection
This single-center, retrospective study evaluated the medical records of 134 HCC patients who underwent liver resections at the Hume-Lee Transplant Center in Richmond, Virginia, from 1 January 2010 to 31 December 2020. Patients were stratified into OH and MIH groups. Patients with American Joint Committee on Cancer (AJCC) stages I–IV diagnoses who underwent curative-intent liver resection were included, as well as those who had undergone preoperative treatment including TACE, RFA, resection, or a combination of treatments.
We collected comprehensive demographics and clinical data, including tumor-specific characteristics like the number, total and largest size, AJCC three-tier grading, microvascular and macrovascular invasion, and lymphatic and capsular invasion. Preoperative labs and morbidity-related data on the length of hospital stay, operative duration, transfusion, and estimated resection margins were reported. Our primary outcomes were overall survival at 1-, 3-, and 5-year intervals, defined as the time interval between the liver resection and death or the most recent follow-up. Our secondary outcomes were disease-free survival at these time intervals, defined as the period after hepatectomy without signs of HCC recurrence.
2.2. Statistical Analysis
Categorical variables were reported as percentages, and continuous variables as means with standard deviations (SDs). Surgical factors like the resection margin and technique were also evaluated. For comparing patients undergoing OH or MIH, Pearson’s Chi-square test or Fisher’s exact test were used for categorical variables and the Kruskal–Wallis rank-sum test was used for continuous variables. Kaplan–Meier plots were used to analyze overall and disease-free survival at 1-, 3-, and 5-year intervals. Cox proportional hazards regression analyzed predictors of overall survival and of disease-free survival, with significant variables (age and prior TACE) from univariate analysis included in the multivariate model. Hazard ratios (HRs) and 95% confidence intervals (CIs) were used to determine significance for predicting overall survival. Statistical analyses were conducted using Python (Ver. 3.8.18), where p-values were based on two-sided statistical tests with p < 0.05 considered significant.
3. Results
3.1. Patient Characteristics
Between 2010 and 2020, 109 patients diagnosed with HCC received OH while 29 received MIH (Table 1). Within the MIH cohort, 15 patients underwent robotic surgery (2016–2020). Fourteen patients underwent conventional laparoscopic surgery (only two cases were performed throughout 2018 and 2019). There was no significant difference between the MIH and OH groups in terms of gender (82.8% vs. 66.1%; p = 0.112) or racial distribution (p = 0.070). However, the mean age at the time of surgery was significantly higher in the MIH group than the OH group (66.9 years vs. 60.1 years; p = 0.015).

Table 1.
Baseline characteristics of patients undergoing open or minimally invasive hepatectomies.
Both groups had similar rates of cirrhosis, prior cancers, and preoperative therapy (p = 0.233; p = 0.767; p = 0.732). However, a higher proportion of the MIH group had three or fewer tumors than the OH group (96.6% vs. 80.7%; p = 0.045). While the largest tumor sizes found were similar, the MIH group showed a smaller total tumor size (4.9 cm vs. 7.3 cm; p = 0.031). There were no significant differences in differentiation grading, microvascular or macrovascular invasion, lymphatic or capsular invasion, or AJCC staging.
3.2. Clinical Outcomes
Univariate analysis showed that age > 60 was associated with worse overall survival (OS) (HR 1.891, CI: 1.156–3.093; p = 0.011) (Table 2). Multivariate analysis confirmed the significance between age and overall survival (HR 1.848, CI: 1.122–3.046; p = 0.016). A lack of preoperative TACE showed improved overall survival in univariate analyses (HR 0.393, CI: 0.221–0.698; PI = 0.001) and multivariate analyses (HR 0.398, CI: 0.222–0.712; p = 0.002).

Table 2.
Cox regression analysis of predictors of overall survival.
Age ≥ 60 years and the absence of preoperative TACE showed significant association with disease-free survival (DFS) as well (Table 3). Age > 60 years worsened disease-free survival in both univariate (HR 1.918, CI: 1.076–3.418; p = 0.027) and multivariate analyses (HR 1.982, CI: 1.169–3.359; p = 0.024). A lack of preoperative TACE was associated with improved DFS in univariate analysis (HR 0.360, CI: 0.178–0.727; p = 0.004).

Table 3.
Cox regression analysis of predictors of disease-free survival.
Surgical technique did not impact OS (p = 0.484) between OH and MIH patients. For MIH patients, the 1-, 3-, and 5-year OS rates were 79.7%, 52.9%, and 44.1%, while the 1-, 3-, and 5-year OS rates for OH patients were 79.3%, 64.2%, and 47.9% (Figure 1). The disease-free survival rates were comparable as well (p = 0.729). For MIH patients, the 1-, 3-, and 5-year DFS rates were 73.2%, 53.4%, and 40.0%, while the 1-, 3-, and 5-year OS rates for OH patients were 70.5%, 48.3%, and 40.0% (Figure 2). No MIH patients survived beyond 6.67 years.
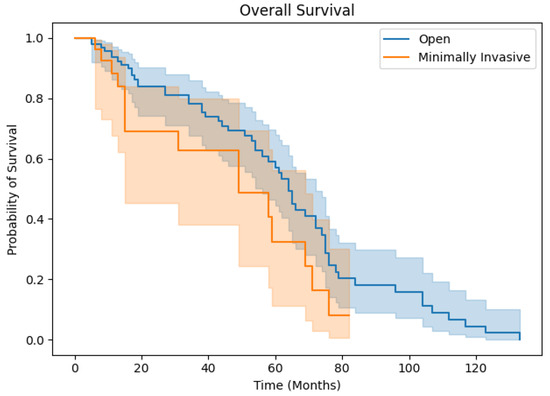
Figure 1.
Overall survival for OH and MIH patients.
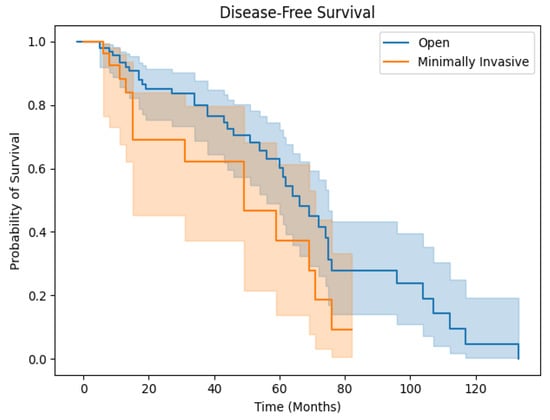
Figure 2.
Disease-free survival for OH and MIH patients.
Patients undergoing MIH had shorter LOS than those in the open surgery group (5.4 days vs. 8.8 days; p = 0.003) and shorter operation times (261.0 min vs. 338.8 min; p = 0.004 (Table 4). There were no considerable differences in intraoperative blood transfusion volume between MIH and OH patients (700.0 mL vs. 1161.6 mL; p = 0.263) or resection margins (negative margins < 10 mm: 11 vs. 55; >10 mm: 11 vs. 30; positive margins: 3 vs. 16; p = 0.392).

Table 4.
Comparisons of clinical outcomes between open and minimally invasive hepatectomies.
4. Discussion
Hepatic resection for HCC remains challenging for patients and surgeons, but laparoscopic approaches have remained popular for over three decades thanks to advancements in surgical techniques and improved equipment [25]. Several studies have illustrated the benefits of laparoscopic approaches among HCC patients, including reduced hospitalization, blood loss, and postoperative morbidity while maintaining comparable oncological results to open resection [14,26,27,28]. With the recent emergence of robot-assisted liver resections, the safety and feasibility of MIH are subject to continual assessment. Our analysis represents a decade of experience with conventional and robot-assisted laparoscopic liver resections at a high-volume, tertiary referral center, in comparison to traditional open procedures.
OH and MIH patients were similar in terms of demographics, comorbidities, and tumor characteristics, with the notable exception of age. Despite no definitive consensus regarding the outcomes of OH and MIH among higher-risk elderly patients, it is crucial to identify patients who may benefit most from minimally invasive alternatives. A recent meta-analysis indicates that elderly patients are more prone to postoperative morbidity and short-term mortality with laparoscopic hepatectomies [29]. The associated risk rises as individuals age, peaking when patients reach their seventies, before stabilizing in septuagenarians [29]. However, our data demonstrate that patients undergoing MIH (robotic and laparoscopic) may experience similar survival benefits compared to those undergoing OH, despite the age discrepancy.
This supports studies showing MIH’s safety and feasibility profiles among elderly patients, possibly attributed to the significantly decreased length of hospital stay among MIH patients [30,31]. Elderly patients who spend a longer time in the Intensive Care Unit (ICU) may develop disabilities that impact overall quality of life, with national analysis reporting a median LOS of 3 days among MIH recipients compared to 6 days among OH patients [14,32]. Other centers reported a slightly higher LOS of 7 days for MIH patients, but still lower than the 9 days seen in OH patients [33]. Our data regarding LOS are within these reported ranges. Additionally, postoperative infections are among the most frequent complications in elderly patients. While not addressed in this study, it is plausible that reducing severe postoperative wound infections and hastening the recovery process may have contributed to similar complication rates in both groups [14].
As the screening apparatus for liver cirrhosis continues to improve globally, elderly patients face higher risks of complications following liver resection and HCC [34]. Our experience indicates that sexagenarians had increased rates of mortality. Despite our patients being mostly sexagenarians, there were no differences in the presence of cirrhosis between OH and MIH groups. The benefits of the minimally invasive approach may decrease in patients aged 80 and above [35]. Nevertheless, this has not been demonstrated among our patients undergoing MIH. Liver transplantation is another important alternative to resection in HCC patients with cirrhosis, but elderly patients nearing their 70s are mostly excluded due to comorbidities [36]. Our data demonstrate that elderly patients previously denied an opportunity for a potentially curative liver resection can be offered the viable and potentially favorable treatment option of MIH.
The differences in operative time between OH and MIH are notable, as a longer operative time is a significant predictor of surgical morbidity after laparoscopic liver resections [37]. Unlike recent national and institutional retrospective analyses showing no difference in operative times, our experience demonstrates a significantly reduced duration of operation in favor of MIH [14,33]. This may be due to MIH patients having lower tumor numbers and sizes. Indeed, minor resections have decreased operative times in laparoscopic liver resections and may be associated with lower blood loss and intraoperative transfusion rates [38]. While our study showed no significant difference in intraoperative transfusion rates, MIH patients tended to require less overall transfusion volume.
A prior history of TACE was associated with lower mortality in patients undergoing both OH and MIH. Preoperative TACE identifies latent intrahepatic metastatic foci, improves the resectability of HCCs by reducing tumors that are initially borderline resectable or unresectable, allows adequate time for therapy when liver function is compromised, and enhances the overall survival and disease-free survival rates following curative resection [39]. Multiple retrospective studies have demonstrated its effectiveness in patients with intermediate-stage HCC who benefit from superior oncological results with OH or MIH [40]. These patients tend to have large and multifocal HCC without intrahepatic macrovascular invasion or extrahepatic metastases [41]. This is a salient point for patients undergoing OH who have larger and more numerous tumors compared to MIH patients, albeit a statistically insignificant difference. Certain clinicians may not advocate for preoperative TACE in patients with resectable HCC being evaluated for surgical intervention. One of the key factors to consider is that TACE may affect well-differentiated HCC while incompletely eradicating poorly differentiated cells [42]. Consequently, preoperative TACE may increase the chance of HCC metastasis via the portal venous system. However, our experience shows selective chemoembolization of HCC tumors prior to hepatectomy may confer additional survival benefits for HCC patients.
Furthermore, it is known that MIH has a steep learning curve that requires concomitant training in both laparoscopic and robotic techniques [43]. Despite increasing variation in operator experience as MIH evolves, MIH offers several key advantages compared to OH. Unlike OH, MIH may minimize the damage to adherent structures and the liver through manipulation only inside the subphrenic rib cage. Laparoscopic instruments can directly access the space caudally with minimal damage to the cage and minimal mobilization or compression of the liver [44]. Second, MIH may have advantages for the treatment of intrahepatic recurrence compared to OH. While our short- and long-term data showed non-inferior DFS of MIH compared to OH, it is likely that reoperation on the liver is made more difficult once adhesions are formed. Notably, MIH may be associated with lower rates of adhesion formation, allowing for better visibility and maneuverability even in the small surgical fields between adhesions [44]. Comparable OS and DFS after MIH may be due to reduced functional deterioration of the liver [25]. With reduced adhesions, the process of repeat treatments becomes more accessible, decreasing mortality among patients with liver insufficiency.
MIH has its disadvantages, as maintaining orientation can be difficult due to the lack of fine perceptible sensation and visibility of the entire surgical field. However, effective simulation of minor anatomical resections can ensure precise localization of the tumor within the resected area and adequate surgical margins. This may result in reduced postoperative complications, diminished residual ischemic/congestive parenchyma, and potentially lower recurrence risk [45]. Robotic technology also confers numerous benefits compared to conventional laparoscopic techniques [46]. Features such as Endowrist technology provide a remarkable seven degrees of freedom in hand manipulation. Additionally, robotic systems enable operating surgeons to access lesions located in the posterior superior region, enhance their suturing, reduce physiological tremors, and promote better ergonomics [46]. Overall, these advancements in MIH have likely reduced operative time and other morbidities at our institution, and we resultantly demonstrate acceptable short- and long-term clinical results with both robotic and laparoscopic techniques.
Limitations
While our study provides valuable insight into the outcomes and survival rates of patients who have undergone OH and MIH for HCC, there are several limitations. First, this was a single-center analysis, which limits the generalizability of the findings. Second, the retrospective nature of our study introduces a certain level of selection bias, as the choice between OH and MIH was determined by physicians based on clinical judgment and patient characteristics. Third, the lack of statistical significance in certain variables may be due to the insufficient power to identify a potential association. Fourth, another limitation of our study includes the unequal distribution of sample sizes between the OH group and MIH group, with only 29 MIH patients (including 15 robotic-assisted cases) in contrast to the 109 patients in the OH group. Such variation potentially limits the generalizability of our findings and underscores the need for more equitably matched groups in future studies to better evaluate the differences between these surgical approaches. Finally, this study did not account for adjuvant therapies. Future studies with larger, multi-center cohorts and prospective design are needed for validating our findings and further exploring the benefits and limitations of MIH in the treatment of HCC, especially in the evaluation of postoperative complications to better detail the safety profiles of each surgical technique. More studies are also needed to compare clinical outcomes between laparoscopic surgeries and robotic surgeries using large sets of single-center or multi-center clinical data. Further research on the implications of robotic surgeries specifically on perioperative management and outcomes in the scope of hepatectomies on patients with HCC will be needed as they become more commonplace due to improving learning curves. Cost analysis studies are also needed to determine the financial impact of robotic and laparoscopic resections on optimizing resource allocation and decision-making.
5. Conclusions
This paper represents a recent decade of experience with both OH and MIH at a tertiary referral center. For patients with HCC, MIH—both robot-assisted and conventional laparoscopic—may confer faster recovery and reduced operative times compared to OH. Selected patients may also receive survival benefits when preoperatively treated with TACE. Despite significantly increased age among patients undergoing MIH, these procedures showed comparable short- and long-term oncologic outcomes when compared to OH.
Author Contributions
S.D.L. conceptualized and designed the study. A.M.-G.P., Y.I.C.K., K.S. and A.S. (Aadi Sharma) collectively conducted the data analysis and interpretation. All authors contributed to data collection, analysis, manuscript review, and critical revisions. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The Institutional Review Board at Virginia Commonwealth University approved our study under protocol number HM20007405 in 5 March 2021.
Informed Consent Statement
Patient confidentiality and privacy were strictly maintained, and all data were anonymized to protect participant identities.
Data Availability Statement
Research data are not shared.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Polyzos, S.A.; Chrysavgis, L.; Vachliotis, I.D.; Chartampilas, E.; Cholongitas, E. Nonalcoholic fatty liver disease and hepatocellular carcinoma: Insights in epidemiology, pathogenesis, imaging, prevention and therapy. Semin. Cancer Biol. 2023, 93, 20–35. [Google Scholar] [CrossRef] [PubMed]
- Rumgay, H.; Arnold, M.; Ferlay, J.; Lesi, O.; Cabasag, C.J.; Vignat, J.; Laversanne, M.; McGlynn, K.A.; Soerjomataram, I. Global burden of primary liver cancer in 2020 and predictions to 2040. J. Hepatol. 2022, 77, 1598–1606. [Google Scholar] [CrossRef] [PubMed]
- Villanueva, A. Hepatocellular Carcinoma. N. Engl. J. Med. 2019, 380, 1450–1462. [Google Scholar] [CrossRef] [PubMed]
- Galle, P.R.; Forner, A.; Llovet, J.M.; Mazzaferro, V.; Piscaglia, F.; Raoul, J.L.; Schirmacher, P.; Vilgrain, V. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2018, 69, 182–236, Erratum in J. Hepatol. 2019, 70, 817. [Google Scholar] [CrossRef]
- Forner, A.; Reig, M.; Bruix, J. Hepatocellular carcinoma. Lancet 2018, 391, 1301–1314. [Google Scholar] [CrossRef]
- Gordan, J.D.; Kennedy, E.B.; Abou-Alfa, G.K.; Beg, M.S.; Brower, S.T.; Gade, T.P.; Goff, L.; Gupta, S.; Guy, J.; Harris, W.P.; et al. Systemic Therapy for Advanced Hepatocellular Carcinoma: ASCO Guideline. J. Clin. Oncol. 2020, 38, 4317–4345. [Google Scholar] [CrossRef]
- Llovet, J.M.; Kelley, R.K.; Villanueva, A.; Singal, A.G.; Pikarsky, E.; Roayaie, S.; Lencioni, R.; Koike, K.; Zucman-Rossi, J.; Finn, R.S. Hepatocellular carcinoma. Nat. Rev. Dis. Primers 2021, 7, 6. [Google Scholar] [CrossRef]
- Sapisochin, G.; Bruix, J. Liver transplantation for hepatocellular carcinoma: Outcomes and novel surgical approaches. Nat. Rev. Gastroenterol. Hepatol. 2017, 14, 203–217. [Google Scholar] [CrossRef]
- Vitale, A.; Trevisani, F.; Farinati, F.; Cillo, U. Treatment of Hepatocellular Carcinoma in the Precision Medicine Era: From Treatment Stage Migration to Therapeutic Hierarchy. Hepatology 2020, 72, 2206–2218. [Google Scholar] [CrossRef]
- Di Sandro, S.; Benuzzi, L.; Lauterio, A.; Botta, F.; De Carlis, R.; Najjar, M.; Centonze, L.; Danieli, M.; Pezzoli, I.; Rampoldi, A.; et al. Single Hepatocellular Carcinoma approached by curative-intent treatment: A propensity score analysis comparing radiofrequency ablation and liver resection. Eur. J. Surg. Oncol. 2019, 45, 1691–1699. [Google Scholar] [CrossRef]
- Vogel, A.; Martinelli, E. ESMO Guidelines Committee Updated treatment recommendations for hepatocellular carcinoma (HCC) from the ESMO Clinical Practice Guidelines. Ann. Oncol. 2021, 32, 801–805. [Google Scholar] [CrossRef] [PubMed]
- Reich, H.; McGlynn, F.; DeCaprio, J.; Budin, R. Laparoscopic excision of benign liver lesions. Obstet. Gynecol. 1991, 78 Pt 2, 956–958. [Google Scholar] [PubMed]
- Wakabayashi, G.; Cherqui, D.; Geller, D.A.; Buell, J.F.; Kaneko, H.; Han, H.S.; Asbun, H.; O’Rourke, N.; Tanabe, M.; Koffron, A.J.; et al. Recommendations for laparoscopic liver resection: A report from the second international consensus conference held in Morioka. Ann. Surg. 2015, 261, 619–629. [Google Scholar] [CrossRef] [PubMed]
- Bagante, F.; Spolverato, G.; Strasberg, S.M.; Gani, F.; Thompson, V.; Hall, B.L.; Bentrem, D.J.; Pitt, H.A.; Pawlik, T.M. Minimally Invasive vs. Open Hepatectomy: A Comparative Analysis of the National Surgical Quality Improvement Program Database. J. Gastrointest. Surg. 2016, 20, 1608–1617. [Google Scholar] [CrossRef]
- Cho, J.Y.; Han, H.S.; Yoon, Y.S.; Shin, S.H. Feasibility of laparoscopic liver resection for tumors located in the posterosuperior segments of the liver, with a special reference to overcoming current limitations on tumor location. Surgery 2008, 144, 32–38. [Google Scholar] [CrossRef]
- Nguyen, K.T.; Marsh, J.W.; Tsung, A.; Steel, J.J.L.; Gamblin, T.C.; Geller, D.A. Comparative Benefits of Laparoscopic vs. Open Hepatic Resection: A Critical Appraisal. Arch. Surg. 2011, 146, 348–356. [Google Scholar] [CrossRef]
- Simillis, C.; Constantinides, V.A.; Tekkis, P.P.; Darzi, A.; Lovegrove, R.; Jiao, L.; Antoniou, A. Laparoscopic versus open hepatic resections for benign and malignant neoplasms—A meta-analysis. Surgery 2007, 141, 203–211. [Google Scholar] [CrossRef]
- Morino, M.; Morra, I.; Rosso, E.; Miglietta, C.; Garrone, C. Laparoscopic vs open hepatic resection: A comparative study. Surg. Endosc. Other Interv. Tech. 2003, 17, 1914–1918. [Google Scholar] [CrossRef]
- Dagher, I.; Di Giuro, G.; Dubrez, J.; Lainas, P.; Smadja, C.; Franco, D. Laparoscopic versus open right hepatectomy: A comparative study. Am. J. Surg. 2009, 198, 173–177. [Google Scholar] [CrossRef]
- Xiong, J.J.; Altaf, K.; Javed, M.A.; Huang, W.; Mukherjee, R.; Mai, G.; Sutton, R.; Liu, X.B.; Hu, W.M. Meta-analysis of laparoscopic vs. open liver resection for hepatocellular carcinoma. World J. Gastroenterol. 2012, 18, 6657–6668. [Google Scholar] [CrossRef]
- Tsung, A.; Geller, D.A.; Sukato, D.C.; Sabbaghian, S.; Tohme, S.; Steel, J.; Marsh, W.; Reddy, S.K.; Bartlett, D.L. Robotic versus laparoscopic hepatectomy: A matched comparison. Ann. Surg. 2014, 259, 549–555. [Google Scholar] [CrossRef] [PubMed]
- Viganὸ, L.; Ferrero, A.; Amisano, M.; Russolillo, N.; Capussotti, L. Comparison of laparoscopic and open intraoperative ultrasonography for staging liver tumours. Br. J. Surg. 2013, 100, 535–542. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.Y.; Han, H.S.; Yoon, Y.S.; Shin, S.H. Experiences of laparoscopic liver resection including lesions in the posterosuperior segments of the liver. Surg. Endosc. 2008, 22, 2344–2349. [Google Scholar] [CrossRef] [PubMed]
- Giulianotti, P.C.; Coratti, A.; Sbrana, F.; Addeo, P.; Bianco, F.M.; Buchs, N.C.; Annechiarico, M.; Benedetti, E. Robotic liver surgery: Results for 70 resections. Surgery 2011, 149, 29–39. [Google Scholar] [CrossRef]
- Morise, Z. Current status of minimally invasive liver surgery for cancers. World J. Gastroenterol. 2022, 28, 6090–6098. [Google Scholar] [CrossRef]
- Takahara, T.; Wakabayashi, G.; Beppu, T.; Aihara, A.; Hasegawa, K.; Gotohda, N.; Hatano, E.; Tanahashi, Y.; Mizuguchi, T.; Kamiyama, T.; et al. Long-term and perioperative outcomes of laparoscopic versus open liver resection for hepatocellular carcinoma with propensity score matching: A multi-institutional Japanese study. J. Hepatobiliary Pancreat. Sci. 2015, 22, 721–727. [Google Scholar] [CrossRef]
- Haney, C.M.; Studier-Fischer, A.; Probst, P.; Fan, C.; Müller, P.C.; Golriz, M.; Diener, M.K.; Hackert, T.; Müller-Stich, B.P.; Mehrabi, A.; et al. A systematic review and meta-analysis of randomized controlled trials comparing laparoscopic and open liver resection. HPB 2021, 23, 1467–1481. [Google Scholar] [CrossRef]
- Endo, Y.; Tsilimigras, D.I.; Munir, M.M.; Woldesenbet, S.; Yang, J.; Katayama, E.; Guglielmi, A.; Ratti, F.; Marques, H.P.; Cauchy, F.; et al. Textbook outcome in liver surgery: Open vs. minimally invasive hepatectomy among patients with hepatocellular carcinoma. J. Gastrointest. Surg. 2024, 28, 417–424. [Google Scholar] [CrossRef]
- Okinaga, H.; Yasunaga, H.; Hasegawa, K.; Fushimi, K.; Kokudo, N. Short-Term Outcomes following Hepatectomy in Elderly Patients with Hepatocellular Carcinoma: An Analysis of 10,805 Septuagenarians and 2381 Octo- and Nonagenarians in Japan. Liver Cancer 2018, 7, 55–64. [Google Scholar] [CrossRef]
- Wabitsch, S.; Haber, P.K.; Ekwelle, N.; Kästner, A.; Krenzien, F.; Benzing, C.; Atanasov, G.; Bellingrath, J.-S.; Bauer, G.; Schöning, W.; et al. Minimally Invasive Liver Surgery in Elderly Patients-A Single-Center Experience. J. Surg. Res. 2019, 239, 92–97. [Google Scholar] [CrossRef]
- Chan, A.C.Y.; Poon, R.T.P.; Cheung, T.T.; Chok, K.S.H.; Dai, W.C.; Chan, S.C.; Lo, C.M. Laparoscopic versus open liver resection for elderly patients with malignant liver tumors: A single-center experience. J. Gastroenterol. Hepatol. 2014, 29, 1279–1283. [Google Scholar] [CrossRef] [PubMed]
- Demiselle, J.; Duval, G.; Hamel, J.-F.; Renault, A.; Bodet-Contentin, L.; Martin-Lefèvre, L.; Vivier, D.; Villers, D.; Lefèvre, M.; Robert, R.; et al. Determinants of hospital and one-year mortality among older patients admitted to intensive care units: Results from the multicentric SENIOREA cohort. Ann. Intensive Care 2021, 11, 35. [Google Scholar] [CrossRef] [PubMed]
- Duarte, V.C.; Coelho, F.F.; Valverde, A.; Danoussou, D.; Kruger, J.A.P.; Zuber, K.; Fonseca, G.M.; Jeismann, V.B.; Herman, P.; Lupinacci, R.M. Minimally invasive versus open right hepatectomy: Comparative study with propensity score matching analysis. BMC Surg. 2020, 20, 260. [Google Scholar] [CrossRef] [PubMed]
- Yoon, Y.-I.; Kim, K.-H.; Kang, S.-H.; Kim, W.-J.; Shin, M.-H.; Lee, S.-K.; Jung, D.-H.; Park, G.-C.; Ahn, C.-S.; Moon, D.-B.; et al. Pure Laparoscopic Versus Open Right Hepatectomy for Hepatocellular Carcinoma in Patients with Cirrhosis: A Propensity Score Matched Analysis. Ann. Surg. 2017, 265, 856–863. [Google Scholar] [CrossRef]
- Martínez-Cecilia, D.; Cipriani, F.; Vishal, S.; Ratti, F.; Tranchart, H.; Barkhatov, L.; Tomassini, F.; Montalti, R.; Halls, M.; Troisi, R.I.; et al. Laparoscopic Versus Open Liver Resection for Colorectal Metastases in Elderly and Octogenarian Patients: A Multicenter Propensity Score Based Analysis of Short- and Long-Term Outcomes. Ann. Surg. 2017, 265, 1192–1200. [Google Scholar] [CrossRef]
- Clavien, P.-A.; Lesurtel, M.; Bossuyt, P.M.; Gores, G.J.; Langer, B.; Perrier, A.; OLT for HCC Consensus Group. Recommendations for liver transplantation for hepatocellular carcinoma: An international consensus conference report. Lancet Oncol. 2012, 13, e11–e22. [Google Scholar] [CrossRef]
- Heise, D.; Bednarsch, J.; Kroh, A.; Schipper, S.; Eickhoff, R.; Lang, S.; Neumann, U.; Ulmer, F. Operative Time, Age, and Serum Albumin Predict Surgical Morbidity after Laparoscopic Liver Surgery. Surg. Innov. 2021, 28, 714–722. [Google Scholar] [CrossRef]
- Chen, J.; Li, H.; Liu, F.; Li, B.; Wei, Y. Surgical outcomes of laparoscopic versus open liver resection for hepatocellular carcinoma for various resection extent. Medicine 2017, 96, e6460. [Google Scholar] [CrossRef]
- Choi, G.; Kim, D.; Kang, C.; Kim, K.; Choi, J.; Lee, W.; Kim, B. Is preoperative transarterial chemoembolization needed for a resectable hepatocellular carcinoma? World J. Surg. 2007, 31, 2370–2377. [Google Scholar] [CrossRef]
- Zhou, Q.; Tuo, F.; Li, R.; Wang, X.; Wang, J.; Huang, Z.; Chen, M.; Huang, J. Transarterial Chemoembolization Combined with Hepatectomy for the Treatment of Intermediate-Stage Hepatocellular Carcinoma. Front. Oncol. 2020, 10, 578763. [Google Scholar] [CrossRef]
- Lin, C.-W.; Chen, Y.-S.; Lo, G.-H.; Hsu, Y.-C.; Hsu, C.-C.; Wu, T.-C.; Yeh, J.-H.; Hsiao, P.; Hsieh, P.-M.; Lin, H.-Y.; et al. Comparison of overall survival on surgical resection versus transarterial chemoembolization with or without radiofrequency ablation in intermediate stage hepatocellular carcinoma: A propensity score matching analysis. BMC Gastroenterol. 2020, 20, 99. [Google Scholar] [CrossRef] [PubMed]
- Bruix, J.; Llovet, J.M.; Castells, A.; Montañá, X.; Brú, C.; Ayuso, M.D.C.; Vilana, R.; Rodés, J. Transarterial embolization versus symptomatic treatment in patients with advanced hepatocellular carcinoma: Results of a randomized, controlled trial in a single institution. Hepatology 1998, 27, 1578–1583. [Google Scholar] [CrossRef] [PubMed]
- Bernardi, L.; Balzano, E.; Roesel, R.; Ghinolfi, D.; Vagelli, F.; Menconi, G.; Petrusic, A.; Mongelli, F.; Majno-Hurst, P.; De Simone, P.; et al. Concomitant training in robotic and laparoscopic liver resections of low-to-intermediate difficulty score: A retrospective analysis of the learning curve. Sci. Rep. 2024, 14, 3595. [Google Scholar] [CrossRef] [PubMed]
- Endo, T.; Morise, Z.; Katsuno, H.; Kikuchi, K.; Matsuo, K.; Asano, Y.; Horiguchi, A. Caudal Approach to Laparoscopic Liver Resection-Conceptual Benefits for Repeated Multimodal Treatment for Hepatocellular Carcinoma and Extended Right Posterior Sectionectomy in the Left Lateral Position. Front. Oncol. 2022, 12, 950283. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.Y.; Han, H.-S.; Choi, Y.; Yoon, Y.-S.; Kim, S.; Choi, J.K.; Jang, J.S.; Kwon, S.U.; Kim, H. Association of Remnant Liver Ischemia with Early Recurrence and Poor Survival after Liver Resection in Patients with Hepatocellular Carcinoma. JAMA Surg. 2017, 152, 386–392. [Google Scholar] [CrossRef]
- Fukumori, D.; Tschuor, C.; Penninga, L.; Hillingsø, J.; Svendsen, L.B.; Larsen, P.N. Learning curves in robot-assisted minimally invasive liver surgery at a high-volume center in Denmark: Report. of the first 100 patients and review of literature. Scand. J. Surg. 2023, 112, 164–172. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).