Adolescent Self-Efficacy for Diet and Exercise Following a School-Based Multicomponent Lifestyle Intervention
Abstract
:1. Introduction
2. Materials and Methods
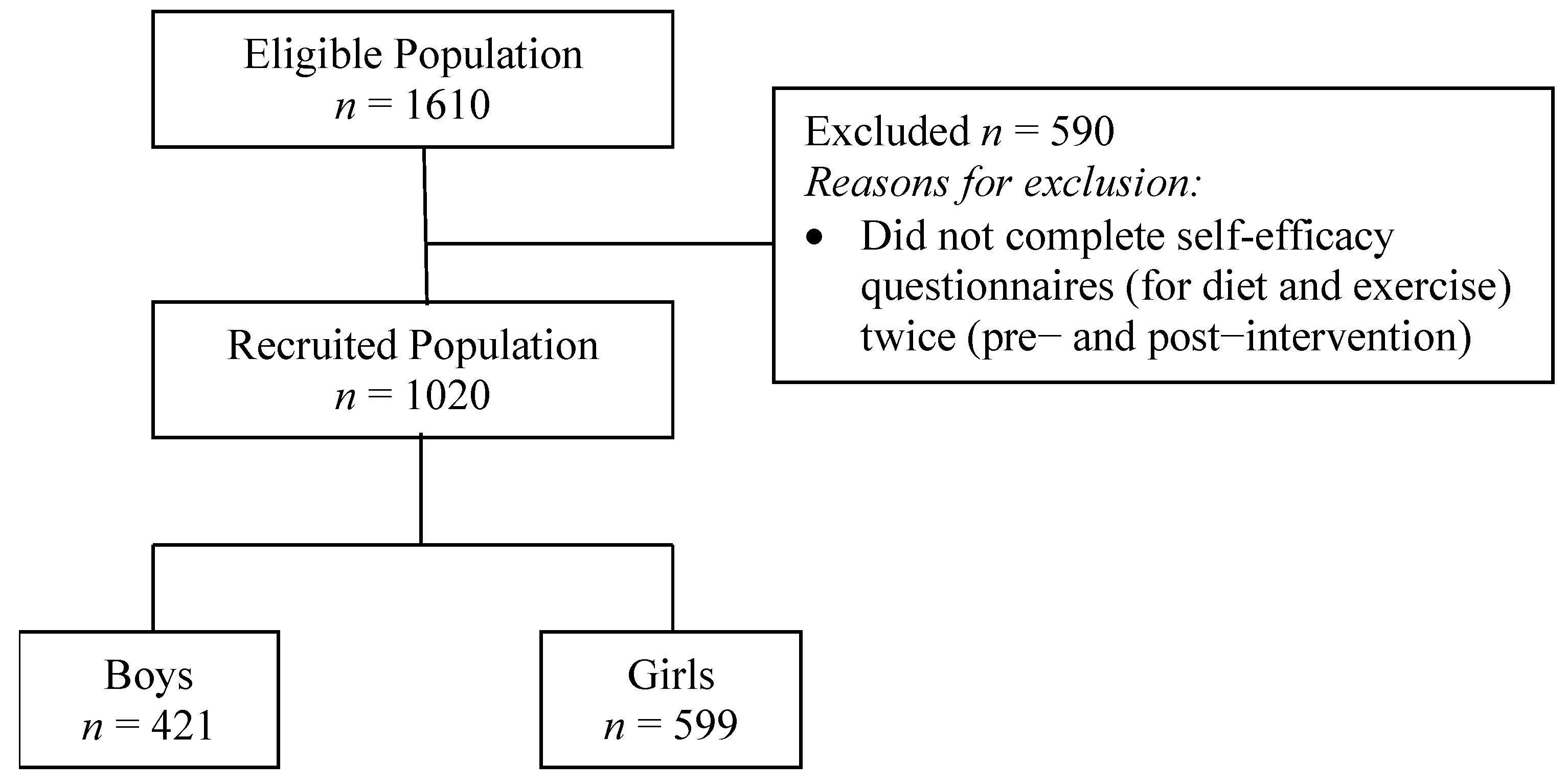
2.1. Participants
2.2. Multicomponent-Multilevel Intervention
2.3. Materials
2.3.1. Anthropometric Measurements
2.3.2. Sociodemographic Data
2.3.3. Self-Efficacy for Diet
2.3.4. Self-Efficacy for Exercise
2.3.5. Assessment of Dietary Habits
2.4. Statistical Analysis
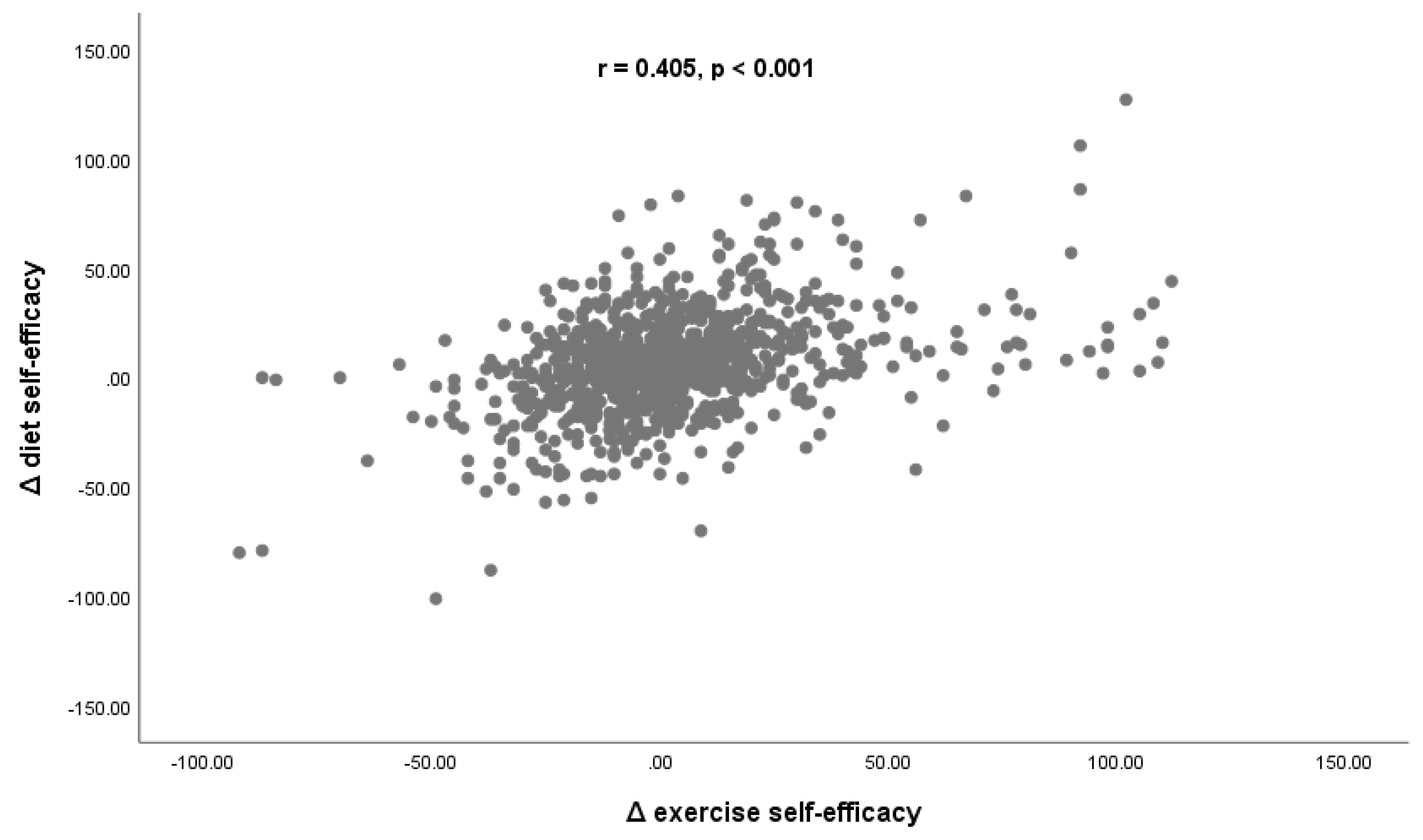
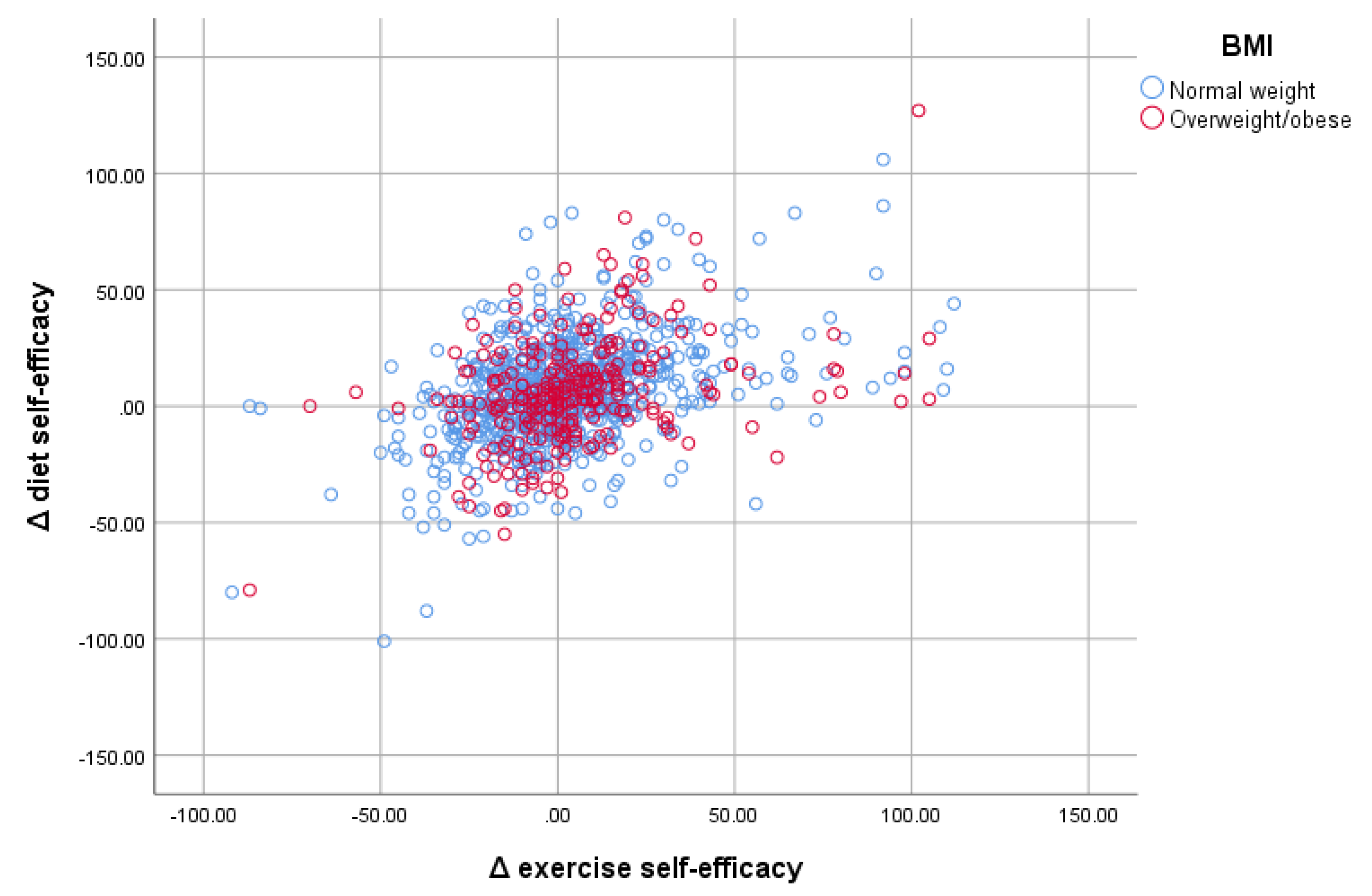
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bandura, A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol. Rev. 1977, 84, 191–215. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Self-Efficacy: The Exercise of Control; Freeman: New York, NY, USA, 1997. [Google Scholar]
- Ha, F.J.; Hare, D.L.; Cameron, J.D.; Toukhsati, S.R. Heart failure and exercise: A narrative review of the role of self-efficacy. Heart Lung Circ. 2018, 27, 22–27. [Google Scholar] [CrossRef] [PubMed]
- McGeown, S.P.; Putwain, D.; Simpson, E.G.; Boffey, E.; Markham, J.; Vince, A. Predictors of adolescents’ academic motivation: Personality, self-efficacy and adolescents’ characteristics. Learn Individ. Diff. 2014, 32, 278–286. [Google Scholar] [CrossRef]
- Valois, R.F.; Zullig, K.J.; Revels, A.A. Aggressive and violent behavior and emotional self-efficacy: Is there a relationship for adolescents? J. Sch. Health 2017, 87, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Cramm, J.M.; Strating, M.M.; Roebroeck, M.E.; Nieboer, A.P. The importance of general self-efficacy for the quality of life of adolescents with chronic conditions. Soc. Indic. Res. 2013, 113, 551–561. [Google Scholar] [CrossRef] [Green Version]
- Bagherniya, M.; Sharma, M.; Mostafavi Darani, F.; Maracy, M.R.; Safarian, M.; Allipour Birgani, R.; Bitarafan, V.; Keshavarz, S.A. School-based nutrition education intervention using social cognitive theory for overweight and obese Iranian adolescent girls: A cluster randomized controlled trial. Int. Q. Community Health Educ. 2017, 38, 37–45. [Google Scholar] [CrossRef]
- Kuroko, S.; Black, K.; Chryssidis, T.; Finigan, R.; Hann, C.; Haszard, J.; Jackson, R.; Mahn, K.; Robinson, C.; Thomson, C.; et al. Create Our Own Kai: A randomised control trial of a cooking intervention with group interview insights into adolescent cooking behaviours. Nutrients 2020, 12, 796. [Google Scholar] [CrossRef] [Green Version]
- Saunders, J.F.; Frazier, L.D.; Nichols-Lopez, K.A. Self-esteem, diet self-efficacy, body mass index, and eating disorders: Modeling effects in an ethnically diverse sample. Eat Weight Disord. 2016, 21, 459–468. [Google Scholar] [CrossRef]
- Nastaskin, R.S.; Fiocco, A.J. A survey of diet self-efficacy and food intake in students with high and low perceived stress. Nutr. J. 2015, 14, 42. [Google Scholar] [CrossRef] [Green Version]
- Fitzgerald, A.; Heary, C.; Kelly, C.; Nixon, E.; Shevlin, M. Self-efficacy for healthy eating and peer support for unhealthy eating are associated with adolescents’ food intake patterns. Appetite 2013, 63, 48–58. [Google Scholar] [CrossRef]
- Glasofer, D.R.; Haaga, D.A.; Hannallah, L.; Field, S.E.; Kozlosky, M.; Reynolds, J.; Yanovski, J.A.; Tanofsky-Kraff, M. Self-efficacy beliefs and eating behavior in adolescent girls at-risk for excess weight gain and binge eating disorder. Int. J. Eat Disord. 2013, 46, 663–668. [Google Scholar] [CrossRef] [PubMed]
- Dishman, R.K.; Motl, R.W.; Saunders, R.; Felton, G.; Ward, D.S.; Dowda, M.; Pate, R.R. Self-efficacy partially mediates the effect of a school-based physical-activity intervention among adolescent girls. Prev. Med. 2004, 38, 628–636. [Google Scholar] [CrossRef] [PubMed]
- Lee, L.L.; Kuo, Y.C.; Fanaw, D.; Perng, S.J.; Juang, I.F. The effect of an intervention combining self-efficacy theory and pedometers on promoting physical activity among adolescents. J. Clin. Nurs. 2012, 21, 914–922. [Google Scholar] [CrossRef]
- Luszczynska, A.; Sheng Cao, D.; Mallach, N.; Pietron, K.; Mazurkiewicz, M.; Schwarzer, R. Intentions, planning, and self-efficacy predict physical activity in Chinese and Polish adolescents: Two moderated mediation analyses. Int. J. Clin. Health Psychol. 2010, 10, 265–278. [Google Scholar]
- McAuley, E.; Lox, C.; Duncan, T.E. Long-term maintenance of exercise, self-efficacy, and physiological change in older adults. J. Gerontol. 1993, 48, P218–P224. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schroeder, K.; Kubik, M.Y.; Lee, J.; Sirard, J.R.; Fulkerson, J.A. Self-efficacy, not peer or parent support, is associated with more physical activity and less sedentary time among 8- to 12-year-old youth with elevated body mass index. J. Phys. Act. Health 2019, 17, 74–79. [Google Scholar] [CrossRef]
- Wurz, A.; Brunet, J. Describing and exploring self-esteem, physical self-perceptions, physical activity and self-efficacy in adolescent and young adult cancer survivors. Eur. J. Cancer Care 2020, 29, e13179. [Google Scholar] [CrossRef]
- Bergstrom, G.; Borjesson, M.; Schmidt, C. Self-efficacy regarding physical activity is superior to self-assessed activity level, in long-term prediction of cardiovascular events in middle-aged men. BMC Public Health 2015, 15, 820. [Google Scholar] [CrossRef] [Green Version]
- LeRouge, C.; Durneva, P.; Sangameswaran, S.; Gloster, A.M. Design guidelines for a technology-enabled nutrition education program to support overweight and obese adolescents: Qualitative user-centered design study. J. Med. Internet Res. 2019, 21, e14430. [Google Scholar] [CrossRef] [Green Version]
- Miri, S.F.; Javadi, M.; Lin, C.Y.; Griffiths, M.D.; Björk, M.; Pakpour, A.H. Effectiveness of cognitive-behavioral therapy on nutrition improvement and weight of overweight and obese adolescents: A randomized controlled trial. Diabetes Metab. Syndr. 2019, 13, 2190–2197. [Google Scholar] [CrossRef] [Green Version]
- Schapiro, N.A.; Green, E.K.; Kaller, S.; Brindis, C.D.; Rodriguez, A.; Alkebulan-Abakah, M.; Chen, J.L. Impact on Healthy Behaviors of Group Obesity Management Visits in Middle School Health Centers. J. Sch. Nurs. 2019, 37, 87–98. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oman, R.F.; King, A.C. Predicting the adoption and maintenance of exercise participation using self-efficacy and previous exercise participation rates. Am. J. Health Promot. 1998, 12, 154–161. [Google Scholar] [CrossRef]
- Slovinec D’Angelo, M.E.; Pelletier, L.G.; Reid, R.D.; Huta, V. The roles of self-efficacy and motivation in the prediction of short- and long-term adherence to exercise among patients with coronary heart disease. Health Psychol. 2014, 33, 1344–1353. [Google Scholar] [CrossRef] [Green Version]
- McAuley, E. The role of efficacy cognitions in the prediction of exercise behavior in middle-aged adults. J. Behav. Med. 1992, 15, 65–88. [Google Scholar] [CrossRef] [PubMed]
- Rothman, A.J.; Baldwin, A.S.; Hertel, A.W. Self-regulation and behavior change disentangling behavioral initiation and behavioral maintenance. In Handbook of Self-Regulation: Research, Theory, and Applications; Baumeister, R., Voh, K., Eds.; Guilford: New York, NY, USA, 2007; Volume 3, pp. 154–196. [Google Scholar]
- Bacopoulou, F.; Efthymiou, V.; Landis, G.; Rentoumis, A.; Chrousos, G.P. Waist circumference, waist-to-hip ratio and waist-to-height ratio reference percentiles for abdominal obesity among Greek adolescents. BMC Pediatr. 2015, 15, 50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bacopoulou, F.; Landis, G.; Rentoumis, A.; Tsitsika, A.; Efthymiou, V. Mediterranean diet decreases adolescent waist circumference. Eur. J. Clin. Investig. 2017, 47, 447–455. [Google Scholar] [CrossRef] [PubMed]
- Bacopoulou, F.; Efthymiou, V.; Palaiologos, G.; Tsarouhas, K.; Landis, G.; Fostiropoulos, I.; Kaklea, M.; Rentoumis, A.; Papassotiriou, I. Telemedicine screening adolescent metabolic syndrome in Greek schools. Eur. J. Clin. Investig. 2019, 49, e13075. [Google Scholar] [CrossRef]
- American Dietetic Association (ADA). Position of the American Dietetic Association: Individual-, family, school-, and community- based interventions for pediatric overweight. J. Am. Diet. Assoc. 2006, 106, 925–945. [Google Scholar] [CrossRef]
- Van Cauwenberghe, E.; Maes, L.; Spittaels, H.; van Lenthe, F.J.; Brug, J.; Oppert, J.M.; De Bourdeaudhuij, I. Effectiveness of school-based interventions in Europe to promote healthy nutrition in children and adolescents: Systematic review of published and ‘grey’ literature. Br. J. Nutr. 2010, 103, 781–797. [Google Scholar] [CrossRef]
- Hoelscher, D.M.; Kirk, S.; Ritchie, L.; Cunningham-Sabo, L.; Academy Positions Committee. Position of the academy of nutrition and dietetics: Interventions for the prevention and treatment of pediatric overweight and obesity. J. Acad. Nutr. Diet. 2013, 113, 1375–1394. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Guide for constructing self-efficacy scales. In Self-Efficacy Beliefs of Adolescents; Pajares, F., Urdan, T., Eds.; CT: Information Age Publishing: Greenwich, London, UK, 2006; Volume 5, pp. 307–337. [Google Scholar]
- Becher, S. Adolescents’ Self-Efficacy toward Healthy Lifestyle Behaviors after Attending a School-Based Intervention Course Focused on Physical Activity and Healthy Eating. (Electronic Thesis or Dissertation), 2009. Available online: https://etd.ohiolink.edu/ (accessed on 14 May 2021).
- McAuley, E.; Jacobson, L. Self-efficacy and exercise participation in sedentary adult females. Am. J. Health Promot. 1991, 5, 185–191. [Google Scholar] [CrossRef]
- Simonavice, E.M.; Wiggins, M.S. Exercise barriers, self-efficacy, and stages of change. Percept. Mot. Ski. 2008, 107, 946–950. [Google Scholar] [CrossRef]
- Bartholomew, J.B.; Loukas, A.; Jowers, E.M.; Allua, S. Validation of the physical activity self-efficacy scale: Testing measurement invariance between Hispanic and Caucasian children. J. Phys. Act. Health 2006, 3, 70–78. [Google Scholar] [CrossRef]
- Sallis, J.F.; Pinski, R.B.; Grossman, R.M.; Patterson, T.L.; Nader, P.R. The development of self-efficacy scales for health related diet and exercise behaviors. Health Educ. Res. 1988, 3, 283–292. [Google Scholar] [CrossRef]
- Jago, R.; Baranowski, T.; Watson, K.; Bachman, C.; Baranowski, J.C.; Thompson, D.; Hernández, A.E.; Venditti, E.; Blackshear, T.; Moe, E. Development of new physical activity and sedentary behavior change self-efficacy questionnaires using item response modeling. Int. J. Behav. Nutr. Phys. Act. 2009, 6, 20. [Google Scholar] [CrossRef] [Green Version]
- Ornelas, I.J.; Perreira, K.M.; Ayala, G.X. Parental influences on adolescent physical activity: A longitudinal study. Int. J. Behav. Nutr. Phys. Act 2007, 4, 3. [Google Scholar] [CrossRef] [Green Version]
- Jago, R.; Brockman, R.; Fox, K.R.; Cartwright, K.; Page, A.S.; Thompson, J.L. Friendship groups and physical activity: Qualitative findings on how physical activity is initiated and maintained among 10–11 year old children. Int. J. Behav. Nutr. Phys. Act. 2009, 6, 4. [Google Scholar] [CrossRef] [PubMed]
- Ries, A.V.; Voorhees, C.C.; Gittelsohn, J.; Roche, K.M.; Astone, N.M. Adolescents’ perceptions of environmental influences on physical activity. Am. J. Health Behav. 2008, 32, 26–39. [Google Scholar] [CrossRef]
- Zabinski, M.F.; Norman, G.J.; Sallis, J.F.; Calfas, K.J.; Patrick, K. Patterns of sedentary behavior among adolescents. Health Psychol. 2007, 26, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Serra-Majem, L.; Ribas, L.; Ngo, J.; Ortega, R.M.; García, A.; Pérez-Rodrigo, C.; Aranceta, J. Food, youth and the Mediterranean diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in children and adolescents. Public Health Nutr. 2004, 7, 931–935. [Google Scholar] [CrossRef] [PubMed]
- Aparicio-Ugarriza, R.; Cuenca-García, M.; Gonzalez-Gross, M.; Julián, C.; Bel-Serrat, S.; Moreno, L.A.; Breidenassel, C.; Kersting, M.; Arouca, A.B.; Michels, N.; et al. Relative validation of the adapted Mediterranean diet score for adolescents by comparison with nutritional bio- markers and nutrient and food intakes: The Healthy Lifestyle in Europe by Nutrition in Adolescence (HELENA) study. Public Health Nutr. 2019, 22, 2381–2397. [Google Scholar] [CrossRef] [PubMed]
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000, 320, 1240–1243. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dewar, D.L.; Lubans, D.R.; Plotnikoff, R.C.; Morgan, P.J. Development and evaluation of social cognitive measures related to adolescent dietary behaviors. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 36. [Google Scholar] [CrossRef] [Green Version]
- Grammatikopoulou, M.G.; Poulimeneas, D.; Gounitsioti, I.S.; Gerothanasi, K.; Tsigga, M.; Kiranas, E.; Group, A.S. Prevalence of simple and abdominal obesity in Greek adolescents: The ADONUT study. Clin. Obes. 2014, 4, 303–308. [Google Scholar] [CrossRef]
- Mohr, B.; Dolgopolova, I.; Roosen, J. The influence of sex and self-control on the efficacy of nudges in lowering the energy content of food during a fast food order. Appetite 2019, 141, 104314. [Google Scholar] [CrossRef] [PubMed]
- Fallon, A.E.; Rozin, P. Sex differences in perceptions of desirable body shape. J. Abnorm. Psychol. 1985, 94, 102–105. [Google Scholar] [CrossRef]
- Pajares, F.; Urdan, T. Self-Efficacy Beliefs of Adolescents (Adolescence and Education); CT: Information Age: Greenwich, London, UK, 2006; Volume 5. [Google Scholar]
- Bani-Issa, W.; Dennis, C.L.; Brown, H.K.; Ibrahim, A.; Almomani, F.M.; Walton, L.M.; Al-Shujairi, A.M. The influence of parents and schools on adolescents’ perceived diet and exercise self-efficacy: A school-based sample from the United Arab Emirates. J. Transcult. Nurs. 2019, 31, 479–491. [Google Scholar] [CrossRef]
- Dasgupta, U.; Mani, S.; Sharma, S.; Singhal, S. Caste Differences in Behaviour and Personality: Evidence from India. WIDER Working Paper Series 060. World Institute for Development Economic Research (UNU-WIDER), 2016. Available online: https://ideas.repec.org/p/unu/wpaper/wp2016-060.html (accessed on 14 May 2020).
- Sharma, S.; Akhtar, F.; Singh, R.K.; Mehra, S. Relationships between nutrition-related knowledge, attitude, and self-efficacy among adolescents: A community-based survey. J. Fam. Med. Prim. Care 2019, 8, 2012–2016. [Google Scholar] [CrossRef]
- Deka, M.K.; Malhotra, A.K.; Yadav, R.; Gupta, S. Dietary pattern and nutritional deficiencies among urban adolescents. J. Fam. Med. Prim. Care 2015, 4, 364–368. [Google Scholar] [CrossRef]
- Dixit, S.; Singh, J.V.; Kant, S.; Agarwal, G.G.; Dubey, A.; Kumari, N. A cross-sectional study on predictors and significance of eating behavior of adolescent girls. Vulnerable Child Youth Stud. 2014, 9, 10–16. [Google Scholar] [CrossRef]
- Hall, E.; Chai, W.; Albrecht, J.A. Relationships between nutrition-related knowledge, self-efficacy, and behavior for fifth grade students attending Title I and non-Title I schools. Appetite 2016, 96, 245–253. [Google Scholar] [CrossRef] [Green Version]
- Dzielska, A.; Mazur, J.; Nałęcz, H.; Oblacińska, A.; Fijałkowska, A. Importance of self-efficacy in eating behavior and physical activity change of overweight and non-overweight adolescent girls participating in Healthy Me: A lifestyle intervention with mobile technology. Nutrients 2020, 12, 2128. [Google Scholar] [CrossRef] [PubMed]
- Olander, E.K.; Fletcher, H.; Williams, S.; Atkinson, L.; Turner, A.; French, D.P. What are the most effective techniques in changing obese individuals’ physical activity self-efficacy and behaviour: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 29. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, R.; Ranganathan, P. Study designs: Part 4–Interventional studies. Perspect. Clin. Res. 2019, 10, 137–139. [Google Scholar] [CrossRef] [PubMed]
- Riaz Ahmad, Z.; Yasien, S.; Ahmad, R. Relationship between perceived social self-efficacy and depression in adolescents. Iran J. Psychiatry Behav. Sci. 2014, 8, 65. [Google Scholar] [PubMed]
- Wang, Y.; Yao, L.; Liu, L.; Yang, X.; Wu, H.; Wang, J.; Wang, L. The mediating role of self-efficacy in the relationship between Big five personality and depressive symptoms among Chinese unemployed population: A cross-sectional study. BMC Psychiatry 2014, 14, 61. [Google Scholar] [CrossRef] [Green Version]
- Brown, T.; Moore, T.H.; Hooper, L.; Gao, Y.; Zayegh, A.; Ijaz, S.; Elwenspoek, M.; Foxen, S.C.; Magee, L.; O’Malley, C.; et al. Interventions for preventing obesity in children. Cochrane Database Syst. Rev. 2019, 7, CD001871. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blüher, S.; Kromeyer-Hauschild, K.; Graf, C.; Widhalm, K.; Korsten-Reck, U.; Jödicke, B.; Markert, J.; Müller, M.J.; Moss, A.; Wabitsch, M.; et al. Current guidelines for obesity prevention in childhood and adolescence. Obes. Facts 2018, 11, 263–276. [Google Scholar] [CrossRef] [PubMed]
- Ricotti, R.; Caputo, M.; Monzani, A.; Pigni, S.; Antoniotti, V.; Bellone, S.; Prodam, F. Breakfast skipping, weight, cardiometabolic risk, and nutrition quality in children and adolescents: A systematic review of randomized controlled and intervention longitudinal trials. Nutrients 2021, 13, 3331. [Google Scholar] [CrossRef]
| Total Sample | Normal Weight | Overweight/Obesity | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention | p‡ | Intervention | p‡ | Intervention | p‡ | ||||
| Pre | Post | Pre | Post | Pre | Post | ||||
| Males (%) † | 421 (41.3) | 285 (38.5) | 124 (47.5) | ||||||
| Age (years) | 14.08 ± 1.63 | 14.17 ± 1.63 | 13.84 ± 1.62 | ||||||
| WC (cm) | 70.97 ± 9.14 | 70.52 ± 9.04 | 0.007 | 67.39 ± 5.54 | 67.16 ± 5.72 | 0.166 | 81.08 ± 9.59 | 80.02 ± 9.81 | 0.019 |
| WHtR | 0.435 ± 0.053 | 0.432 ± 0.052 | 0.006 | 0.413 ± 0.030 | 0.412 ± 0.032 | 0.140 | 0.496 ± 0.056 | 0.489 ± 0.057 | 0.019 |
| WHR | 0.758 ± 0.069 | 0.753 ± 0.065 | 0.015 | 0.745 ± 0.061 | 0.741 ± 0.056 | 0.141 | 0.796 ± 0.078 | 0.787 ± 0.077 | 0.023 |
| BMI (kg/m2) | 21.38 ± 3.54 | 21.81 ± 3.62 | <0.001 | 19.77 ± 1.97 | 20.25 ± 2.07 | <0.001 | 25.95 ± 2.98 | 26.23 ± 3.42 | <0.001 |
| BMI z-score | 0.47 ± 0.86 | 0.59 ± 0.82 | <0.001 | 0.09 ± 0.64 | 0.25 ± 0.62 | 0.005 | 1.54 ± 0.36 | 1.55 ± 0.43 | 0.001 |
| Diet self-efficacy score | 94.21 ± 24.04 | 100.49 ± 23.00 | <0.001 | 93.90 ± 23.79 | 100.22 ± 23.07 | <0.001 | 95.92 ± 24.35 | 102.50 ± 21.92 | 0.001 |
| Exercise self-efficacy score | 82.18 ± 25.31 | 85.25 ± 19.80 | <0.001 | 82.94 ± 24.74 | 85.44 ± 19.80 | <0.001 | 79.72 ± 26.75 | 84.93 ± 19.82 | 0.170 |
| Δ Diet Self-Efficacy § | Δ Exercise Self-Efficacy § | |||
|---|---|---|---|---|
| Mean ± SD | p * | Mean ± SD | p * | |
| Sex | ||||
| Male | 4.10 ± 22.99 | 0.010 | 1.57 ± 23.48 | 0.102 |
| Female | 7.82 ± 22.30 | 4.13 ± 25.46 | ||
| Family structure | ||||
| Two parents | 6.63 ± 22.28 | 0.470 | 2.76 ± 24.28 | 0.157 |
| One parent | 8.22 ± 25.08 | 6.68 ± 28.97 | ||
| Maternal age | ||||
| 30–49 | 6.82 ± 22.90 | 0.593 | 2.93 ± 25.20 | 0.747 |
| 50+ | 7.96 ± 20.91 | 3.69 ± 23.52 | ||
| Paternal age | ||||
| 30–49 | 7.17 ± 22.55 | 0.544 | 3.78 ± 26.02 | 0.403 |
| 50+ | 6.24 ± 22.45 | 2.35 ± 23.41 | ||
| Maternal educational level | ||||
| Low-Medium | 7.53 ± 23.37 | 0.338 | 3.95 ± 25.90 | 0.395 |
| High | 6.12 ± 21.88 | 2.57 ± 23.97 | ||
| Paternal educational level | ||||
| Low–medium | 7.36 ± 22.40 | 0.455 | 4.14 ± 24.98 | 0.257 |
| High | 6.25 ± 22.93 | 2.29 ± 24.93 | ||
| Family income | ||||
| <10,000 EUR | 7.45 ± 22.65 | 0.093 | 3.55 ± 24.76 | 0.487 |
| 10,001+ EUR | 4.35 ± 22.53 | 2.14 ± 25.78 | ||
| KIDMED Score | Diet Self-Efficacy | Exercise Self-Efficacy | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | p | Post Intervention | p | Baseline | p | Post Intervention | p | |
| ≥8 | 104.97 ± 21.44 | <0.001 ‡,a,b,c | 112.27 ± 17.64 | <0.001 ‡,a,b,c | 87.58 ± 25.76 | <0.001 ‡,a,b | 92.57 ± 16.11 | <0.001 ‡,a,b,c |
| 4–7 | 94.17 ± 22.47 | 99.79 ± 21.57 | 81.46 ± 25.15 | 84.17 ± 19.97 | ||||
| <3 | 81.32 ± 25.61 | 85.51 ± 25.83 | 77.57 ± 23.76 | 78.39 ± 21.14 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Efthymiou, V.; Charmandari, E.; Vlachakis, D.; Tsitsika, A.; Pałasz, A.; Chrousos, G.; Bacopoulou, F. Adolescent Self-Efficacy for Diet and Exercise Following a School-Based Multicomponent Lifestyle Intervention. Nutrients 2022, 14, 97. https://doi.org/10.3390/nu14010097
Efthymiou V, Charmandari E, Vlachakis D, Tsitsika A, Pałasz A, Chrousos G, Bacopoulou F. Adolescent Self-Efficacy for Diet and Exercise Following a School-Based Multicomponent Lifestyle Intervention. Nutrients. 2022; 14(1):97. https://doi.org/10.3390/nu14010097
Chicago/Turabian StyleEfthymiou, Vasiliki, Evangelia Charmandari, Dimitrios Vlachakis, Artemis Tsitsika, Artur Pałasz, George Chrousos, and Flora Bacopoulou. 2022. "Adolescent Self-Efficacy for Diet and Exercise Following a School-Based Multicomponent Lifestyle Intervention" Nutrients 14, no. 1: 97. https://doi.org/10.3390/nu14010097







