Normal Versus Slowly Processed Pasta and Post-Prandial Glucose Homeostasis in Healthy Subjects: A Pilot Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Study Protocol
2.3. Mixed-Meal Test
2.4. Pasta Types, Relative Composition, and Manufacturing Process
2.5. Analytical Procedures
2.6. Statistical Analysis
3. Results
3.1. Protocol Results
3.2. Metabolic Outcomes
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- American Diabetes Association. 3. Prevention or Delay of Type 2 Diabetes: Standards of Medical Care in Diabetes—2020. Diabetes Care 2020, 43, S32–S36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yau, J.W.; Thor, S.M.; Ramadas, A. Nutritional Strategies in Prediabetes: A Scoping Review of Recent Evidence. Nutrients 2020, 12, 2990. [Google Scholar] [CrossRef] [PubMed]
- Nesti, L.; Mengozzi, A.; Tricò, D. Impact of Nutrient Type and Sequence on Glucose Tolerance: Physiological Insights and Therapeutic Implications. Front. Endocrinol. 2019, 10, 144. [Google Scholar] [CrossRef] [PubMed]
- Hodges, C.; Archer, F.; Chowdhury, M.; Evans, B.L.; Ghelani, D.J.; Mortoglou, M.; Guppy, F.M. Method of Food Preparation Influences Blood Glucose Response to a High-Carbohydrate Meal: A Randomised Cross-over Trial. Foods 2019, 9, 23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Robertson, T.M.; Brown, J.E.; Fielding, B.A.; Robertson, M.D. The cumulative effects of chilling and reheating a carbohydrate-based pasta meal on the postprandial glycaemic response: A pilot study. Eur. J. Clin. Nutr. 2020. [Google Scholar] [CrossRef] [PubMed]
- Papadaki, A.; Nolen-Doerr, E.; Mantzoros, C.S. The Effect of the Mediterranean Diet on Metabolic Health: A Systematic Review and Meta-Analysis of Controlled Trials in Adults. Nutrients 2020, 12, 3342. [Google Scholar] [CrossRef] [PubMed]
- Bonaccio, M.; Di Castelnuovo, A.; Costanzo, S.; Persichillo, M.; De Curtis, A.; Donati, M.B.; de Gaetano, G.; Iacoviello, L.; MOLI-SANI Study Investigators. Adherence to the traditional Mediterranean diet and mortality in subjects with diabetes. Prospective results from the MOLI-SANI study. Eur. J. Prev. Cardiol. 2016, 23, 400–407. [Google Scholar] [CrossRef] [PubMed]
- Montemurro, M.; Coda, R.; Rizzello, C.G. Recent Advances in the Use of Sourdough Biotechnology in Pasta Making. Foods 2019, 8, 129. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vandevijvere, S.; Seck, M.; Pedroni, C.; De Ridder, K.; Castetbon, K. Food cost and adherence to guidelines for healthy diets: Evidence from Belgium. Eur. J. Clin. Nutr. 2020. [Google Scholar] [CrossRef] [PubMed]
- Kholina, K.; Grant, A.; Waddington, M.; Egbe, M.; Grant, S.; Terashima, M.; Williams, P.L. In-store food environment for adults and children in Nova Scotia, Canada. Can. J. Public Health 2020. [Google Scholar] [CrossRef] [PubMed]
- Migliori, M.; Gabriele, D.; de Cindio, B.; Pollini, C.M. Modelling of high quality pasta drying: Quality indices and industrial application. J. Food Eng. 2005, 71, 242–251. [Google Scholar] [CrossRef]
- Güler, S.; Köksel, H.; Ng, P.K.W. Effects of industrial pasta drying temperatures on starch properties and pasta quality. Food Res. Int. 2002, 35, 421–427. [Google Scholar] [CrossRef]
- Del Prato, S. In search of normoglycaemia in diabetes: Controlling postprandial glucose. Int. J. Obes. Relat. Metab. Disord. 2002, 26, S9–S17. [Google Scholar] [CrossRef] [Green Version]
- Wolever, T.M. Effect of blood sampling schedule and method of calculating the area under the curve on validity and precision of glycaemic index values. Br. J. Nutr. 2004, 91, 295–301. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cavagnuolo, L.; Bozzetto, L.; Franco, L.; Costabile, G.; Riccardi, G.; Rivellese, A.A.; Annuzzi, G. Pizza Leavening Technique Influences Postprandial Glucose Response: A Randomized Controlled Trial in Patients With Type 1 Diabetes. Diabetes Care 2019, 42, e157–e158. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stamataki, N.S.; Yanni, A.E.; Karathanos, V.T. Bread making technology influences postprandial glucose response: A review of the clinical evidence. Br. J. Nutr. 2017, 117, 1001–1012. [Google Scholar] [CrossRef] [Green Version]
- Nauck, M.A.; Meier, J.J. Incretin hormones: Their role in health and disease. Diabetes Obes. Metab. 2018, 20, 5–21. [Google Scholar] [CrossRef] [PubMed]
- Marinangeli, C.P.; Kassis, A.N.; Jones, P.J. Glycemic responses and sensory characteristics of whole yellow pea flour added to novel functional foods. J. Food Sci. 2009, 74, S385–S389. [Google Scholar] [CrossRef]
- Zavitsanou, S.; Massa, J.; Deshpande, S.; Pinsker, J.E.; Church, M.M.; Andre, C.; Doyle, F.J., III; Michelson, A.; Creason, J.; Dassau, E.; et al. The Effect of Two Types of Pasta Versus White Rice on Postprandial Blood Glucose Levels in Adults with Type 1 Diabetes: A Randomized Crossover Trial. Diabetes Technol. Ther. 2019, 21, 458–492. [Google Scholar] [CrossRef]
- Barbiroli, A.; Bonomi, F.; Casiraghi, M.C.; Iametti, S.; Pagani, M.A.; Marti, A. Process conditions affect starch structure and its interactions with proteins in rice pasta. Carbohydr. Polym. 2013, 92, 1865–1872. [Google Scholar] [CrossRef] [PubMed]
| Variables (Units) | Baseline (n = 14) |
|---|---|
| Age (years) | 31 ± 9 |
| BMI (Kg∙m−2) | 21.3 ± 1.9 |
| Fasting plasma glucose (mmol∙L−1) | 4.7 ± 0.6 |
| HbA1c (mmol∙mol−1) | 32 ± 3 |
| Total cholesterol (mmol∙L−1) | 4.4 ± 0.6 |
| LDL cholesterol (mmol/L) | 2.7 ± 0.7 |
| HDL cholesterol (mmol∙L−1) | 1.4 ± 0.3 |
| Triglycerides (mmol∙L−1) | 0.8 ± 0.5 |
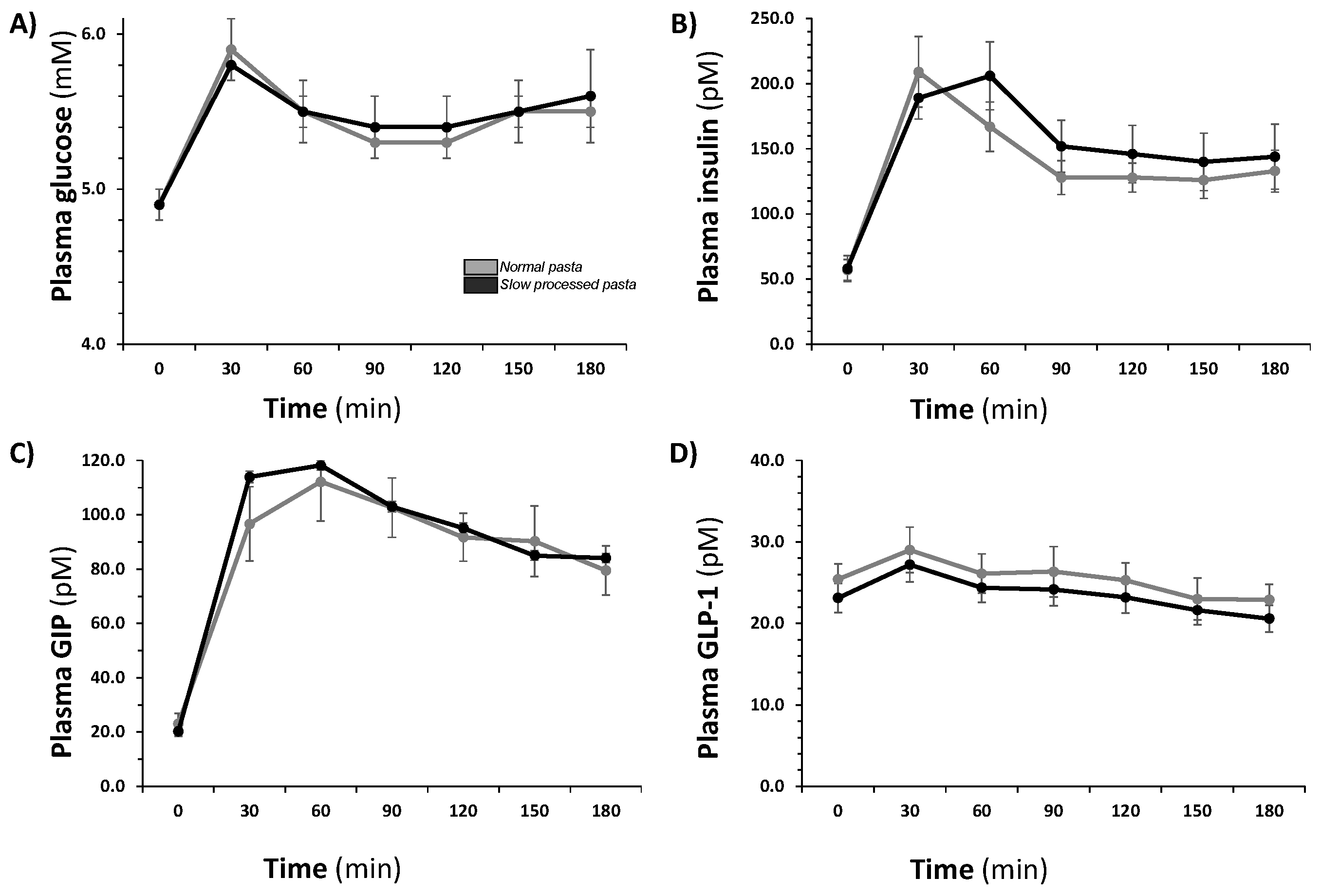
| Variables (Units) | NP | SP | p-Value |
|---|---|---|---|
| Fasting plasma glucose (mmol∙L−1) | 4.9 ± 0.1 | 4.9 ± 0.1 | ns |
| 2-h plasma glucose (mmol∙min∙L−1) | 5.3 ± 0.1 | 5.4 ± 0.2 | ns |
| Plasma glucose iAUC (mmol∙L−1) | 181.4 ± 19.3 | 186.1 ± 22.4 | ns |
| Fasting plasma insulin (pmol∙L−1) | 56.9 ± 7.9 | 59.9 ± 9.5 | ns |
| 2-h plasma insulin (pmol∙L−1) | 127.6 ± 11.3 | 151.7 ± 19.8 | ns |
| Plasma insulin iAUC (pmol∙min∙L−1) | 18,109 ± 1924 | 19,968 ± 2069 | ns |
| Fasting plasma GIP (pmol∙L−1) | 23.0 ± 4.0 | 20.3 ± 3.0 | ns |
| 2-h plasma GIP (pmol∙L−1) | 91.7 ± 8.8 | 95.1 ± 13.0 | ns |
| Plasma GIP iAUC (pmol∙min∙L−1) | 11,968 ± 1448 | 13,100 ± 1638 | ns |
| Fasting plasma GLP-1 (pmol∙L−1) | 24.7 ± 1.9 | 23.1 ± 1.7 | ns |
| 2-h plasma GLP-1 (pmol∙L−1) | 25.3 ± 1.9 | 23.2 ± 1.9 | ns |
| Plasma GLP-1 iAUC (pmol∙min∙L−1) | 797 ± 277 | 688 ± 196 | ns |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mengozzi, A.; Biancalana, E.; Parolini, F.; Baldi, S.; Raggi, F.; Solini, A. Normal Versus Slowly Processed Pasta and Post-Prandial Glucose Homeostasis in Healthy Subjects: A Pilot Study. Nutrients 2021, 13, 678. https://doi.org/10.3390/nu13020678
Mengozzi A, Biancalana E, Parolini F, Baldi S, Raggi F, Solini A. Normal Versus Slowly Processed Pasta and Post-Prandial Glucose Homeostasis in Healthy Subjects: A Pilot Study. Nutrients. 2021; 13(2):678. https://doi.org/10.3390/nu13020678
Chicago/Turabian StyleMengozzi, Alessandro, Edoardo Biancalana, Federico Parolini, Simona Baldi, Francesco Raggi, and Anna Solini. 2021. "Normal Versus Slowly Processed Pasta and Post-Prandial Glucose Homeostasis in Healthy Subjects: A Pilot Study" Nutrients 13, no. 2: 678. https://doi.org/10.3390/nu13020678





