Responding to the Pandemic: Geriatric Care Models
A topical collection in Geriatrics (ISSN 2308-3417).
Viewed by 61152Editor
2. Clinical Associate Director, Tennessee Valley Geriatric Research, Education, and Clinical Center, Nashville, TN 37232, USA
Interests: geriatrics education; long-term care; geriatric nutrition; frail elderly; quality improvement; geriatric care models
Special Issues, Collections and Topics in MDPI journals
Topical Collection Information
Dear Colleagues,
I am delighted to edit this Topical Collection of Geriatrics focusing on “Responding to the Pandemic: Geriatric Care Models”. I invite you to contribute your innovative work focused on geriatric clinical care and caregiver support across the continuum of care.
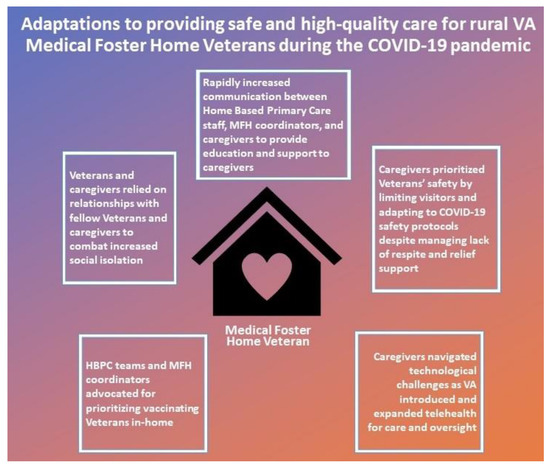
Around the world, the coronavirus pandemic (severe acute respiratory syndrome coronavirus 2, SARS-CoV-2, COVID-19) has produced enormous economic, medical, political, and social changes. Older adults, especially those with chronic illness and residing in residential care facilities, have been disproportionately affected, accounting for over 50% of the mortality. Families, caregivers, medical systems, and support services have adapted processes to respond to this challenge. The responses to this crisis have created a defining time which will affect the provision of health care, as well as the attitudes and expectations of providers and society for decades to come. We are truly all in this together. The sharing of creative approaches to prevent, prepare, and respond to access, safety, and isolation in the care of older adults in response to the COVID pandemic is invited in this Topical Collection.
Potential contributors to this Topical Collection of Geriatrics may include investigators and participants in innovative models of care such as transitions of care models, telehealth programs, primary care, caregiver support, acute care for elderly units, person centered care, new payment and healthcare policy models, and quality assessment and performance improvement programs. Submissions with data and analyses are particularly welcome. Additionally, thoughtful descriptive proposals of best practices and new approaches to geriatric syndromes as well as the promotion of healthy aging and attitudes regarding aging and society, health policy concerns, and successful team-based and collaborative care models are welcome.
We hope you and your colleagues will be willing to submit your creative work for this exciting Topical Collection of Geriatrics. I look forward to hearing from you.
Dr. James S. Powers
Collection Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 250 words) can be sent to the Editorial Office for assessment.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Geriatrics is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 1800 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- geriatric models of care
- transitions of care
- caregiver support
- healthcare access
- isolation
- telehealth
- health policy
Related Special Issue
- Responding to the Pandemic: Geriatric Care Models in Geriatrics (24 articles)