Characterising the Mould Rectification Process for Designing Scoliosis Braces: Towards Automated Digital Design of 3D-Printed Braces
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Population, Scanner, and Mesh Generation Software
2.2. Scanning of Patients and Moulds
Patient Geometry, Pre-Rectification, and Post-Rectification Mould Scans
2.3. Characterisation of the Casting and Rectification Process
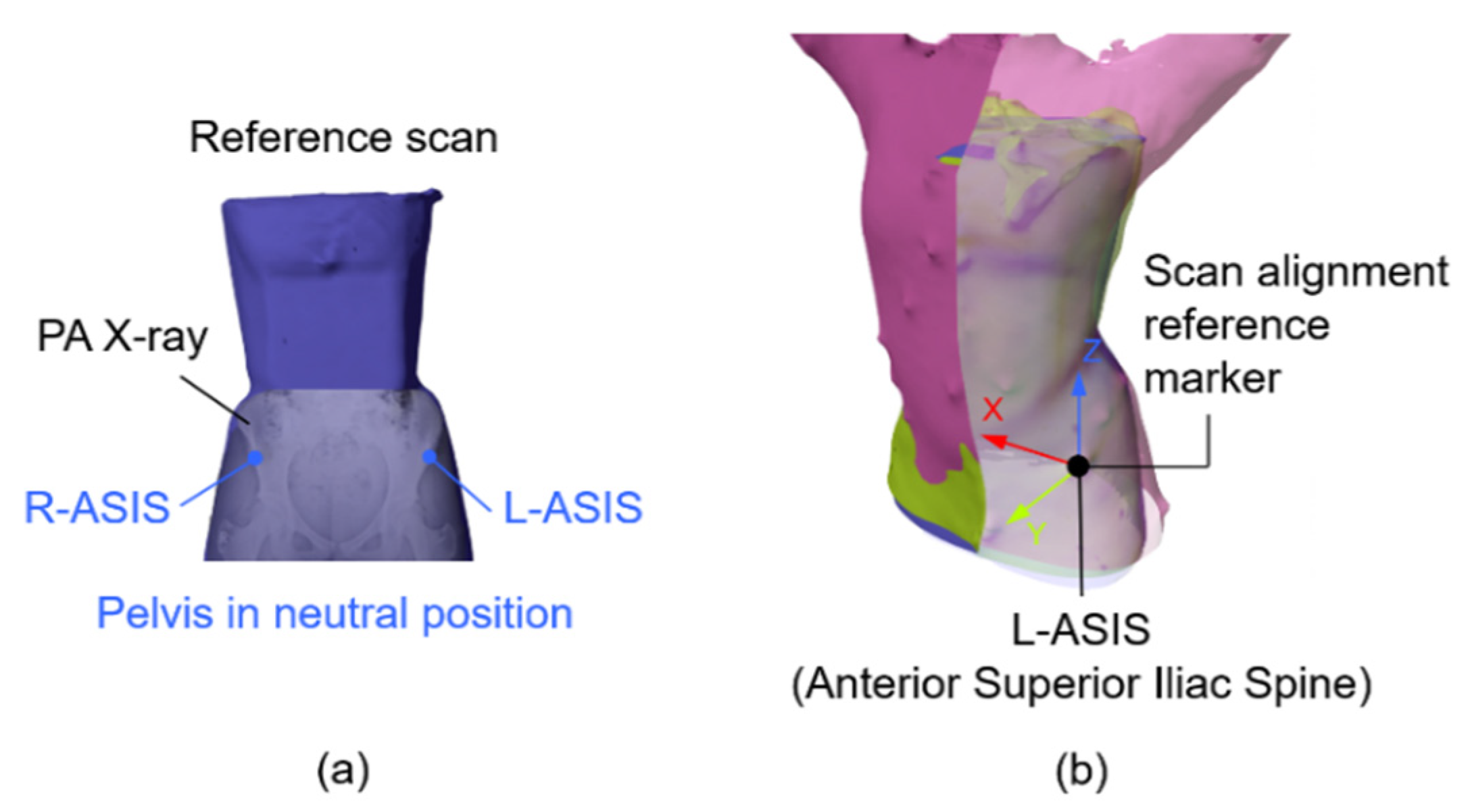
2.3.1. Alignment of the Scans
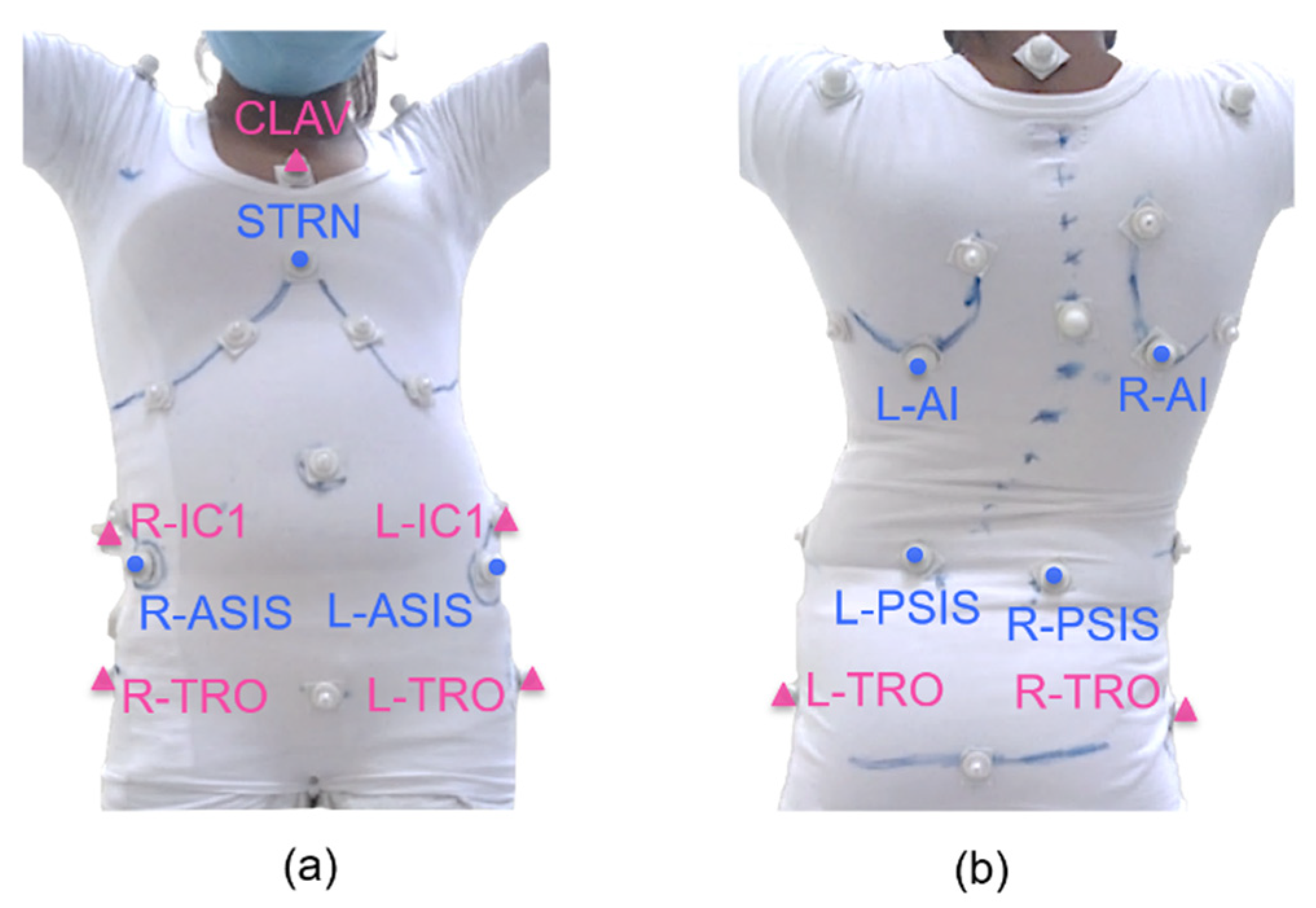
2.3.2. Anatomical Landmark Positions
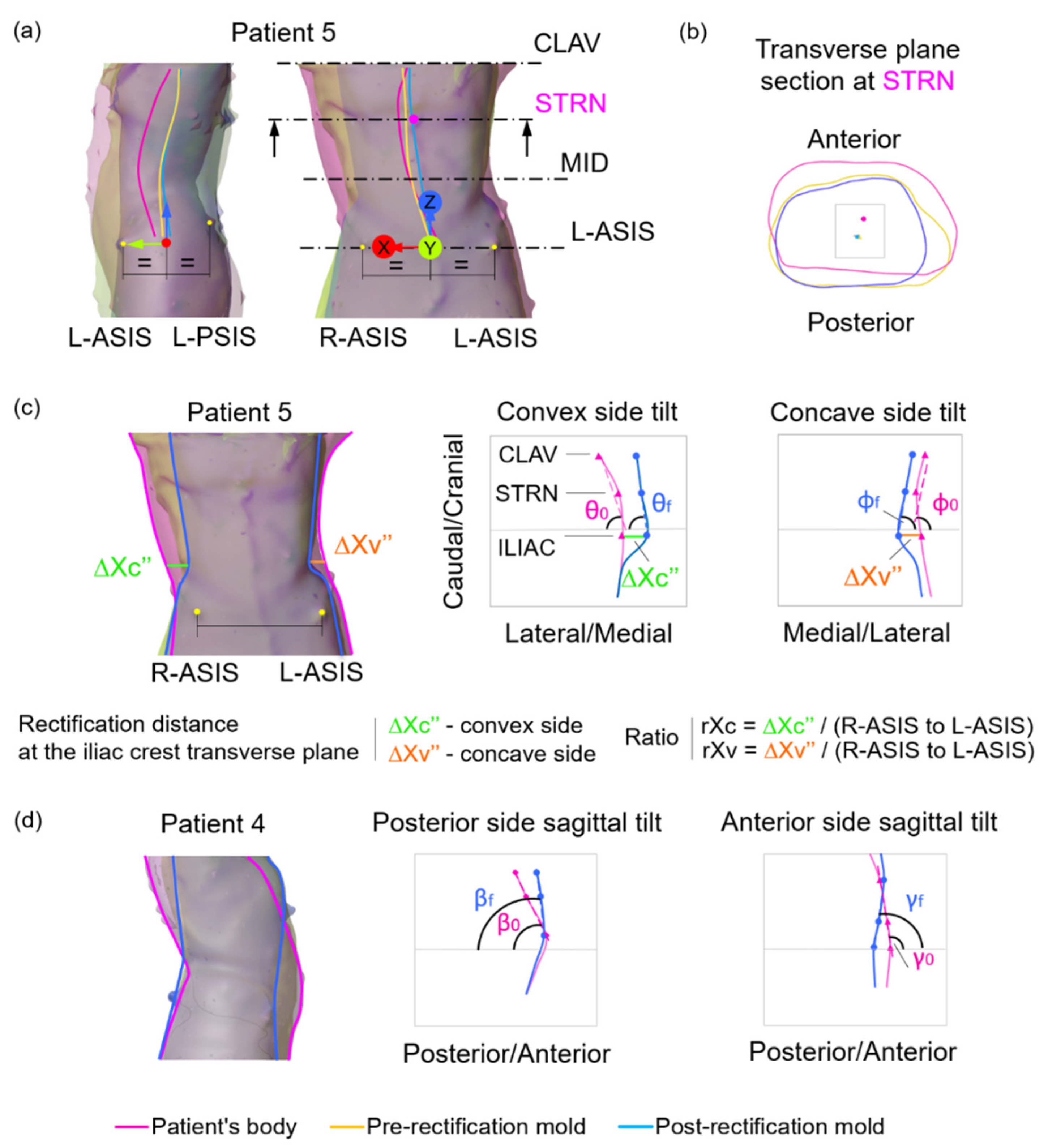
2.3.3. Surface Centroids
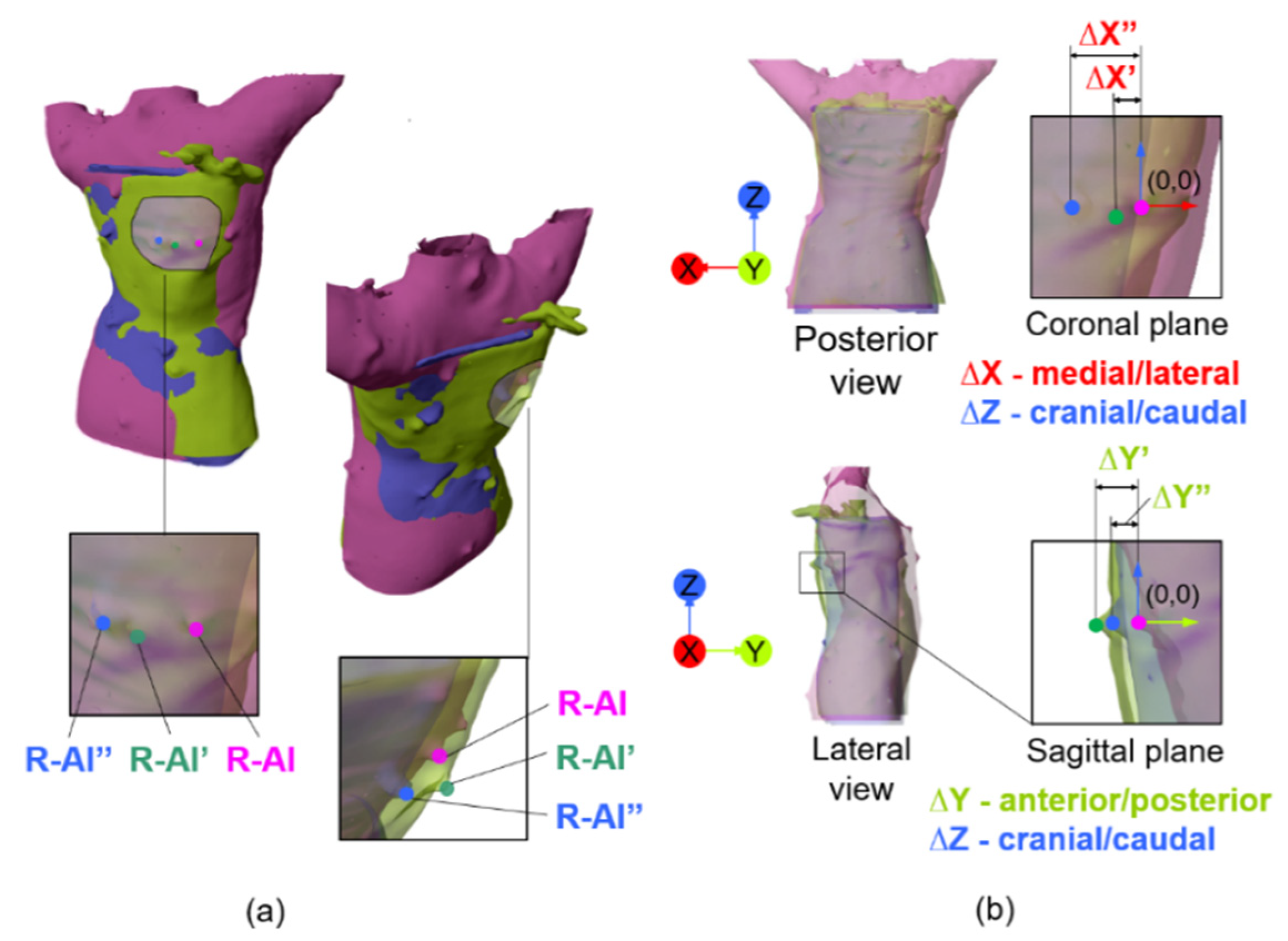
2.3.4. Three-Dimensional Surface Deviations
3. Results
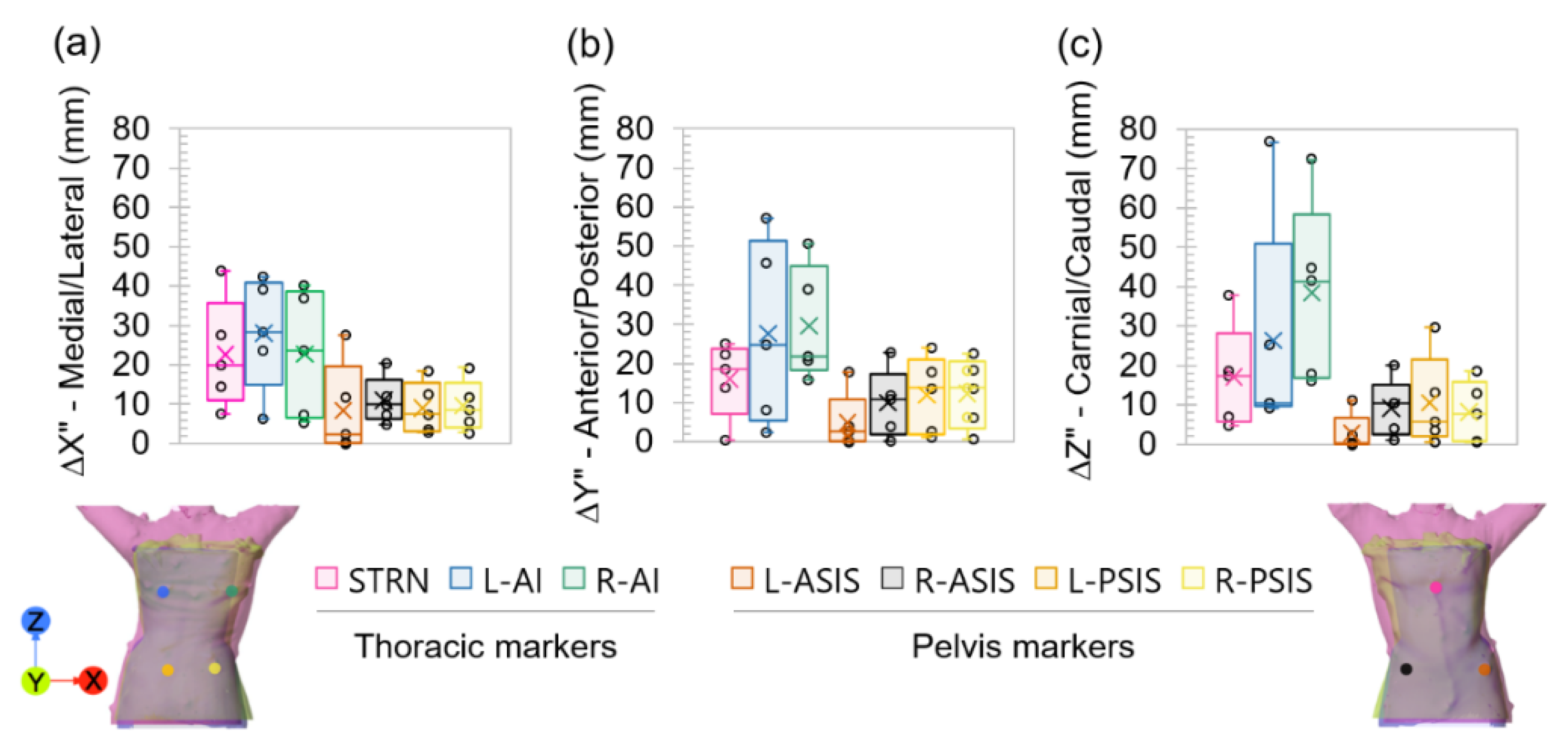
3.1. Anatomical Landmark Positions
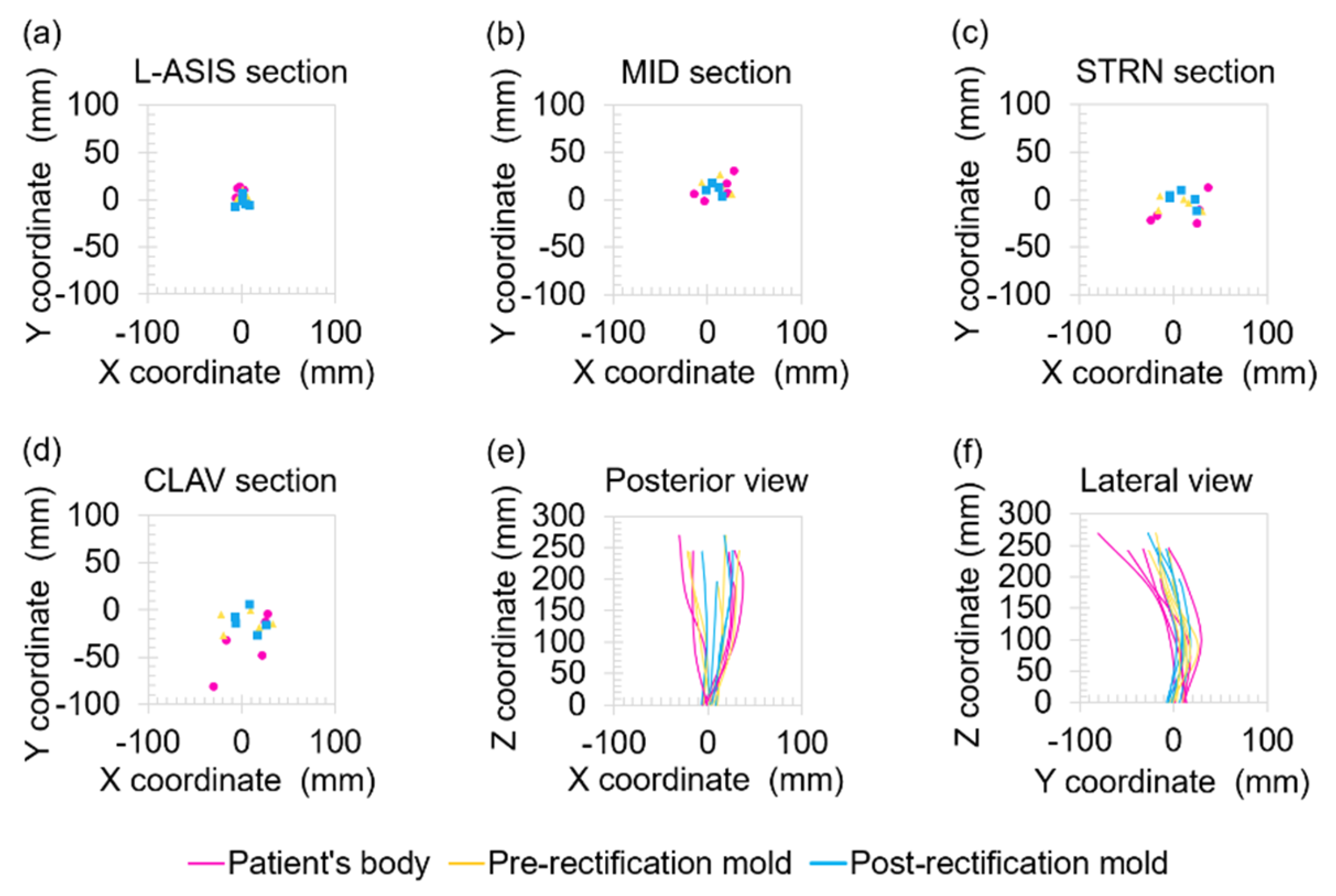
3.2. Surface Centroids
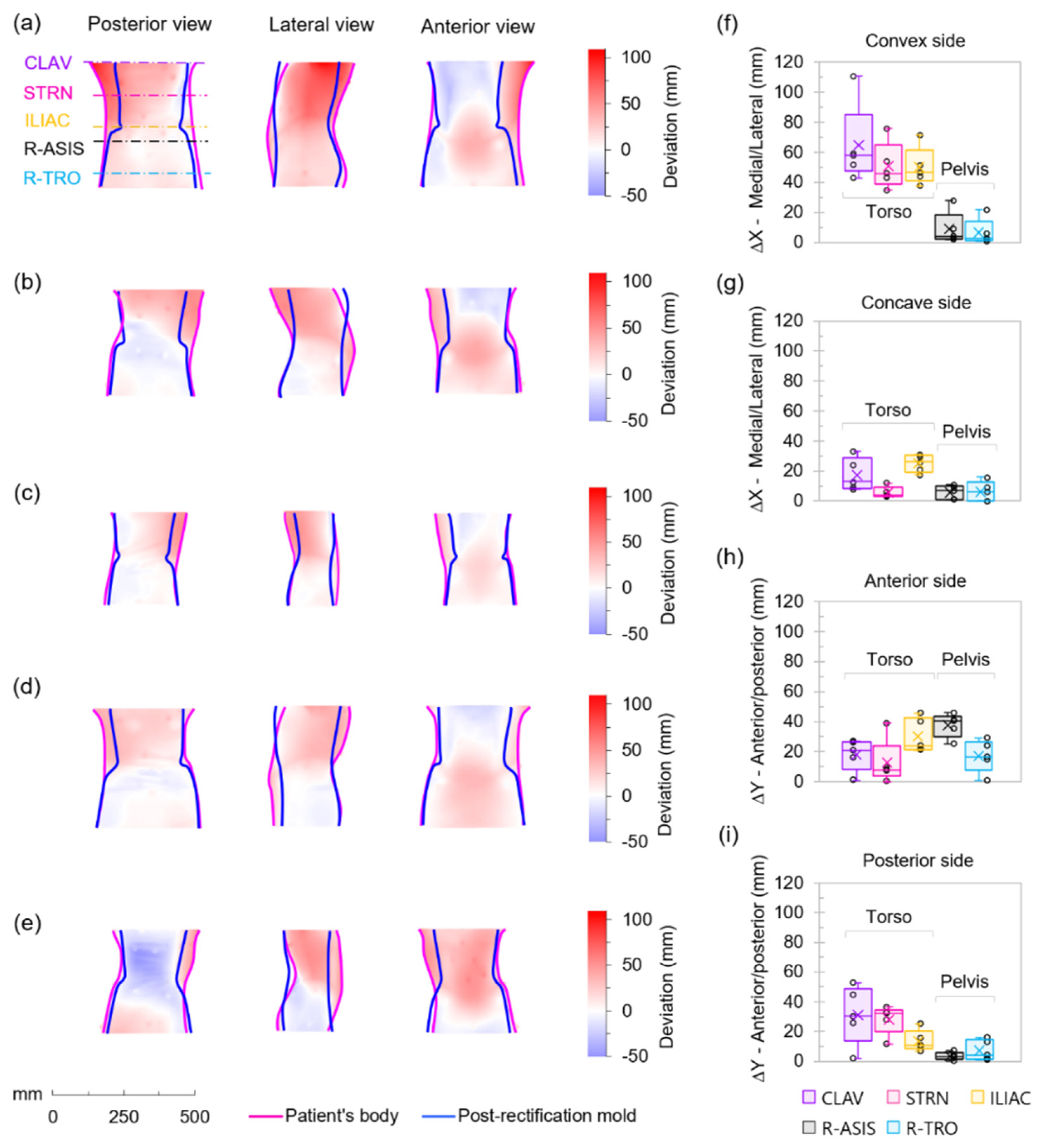
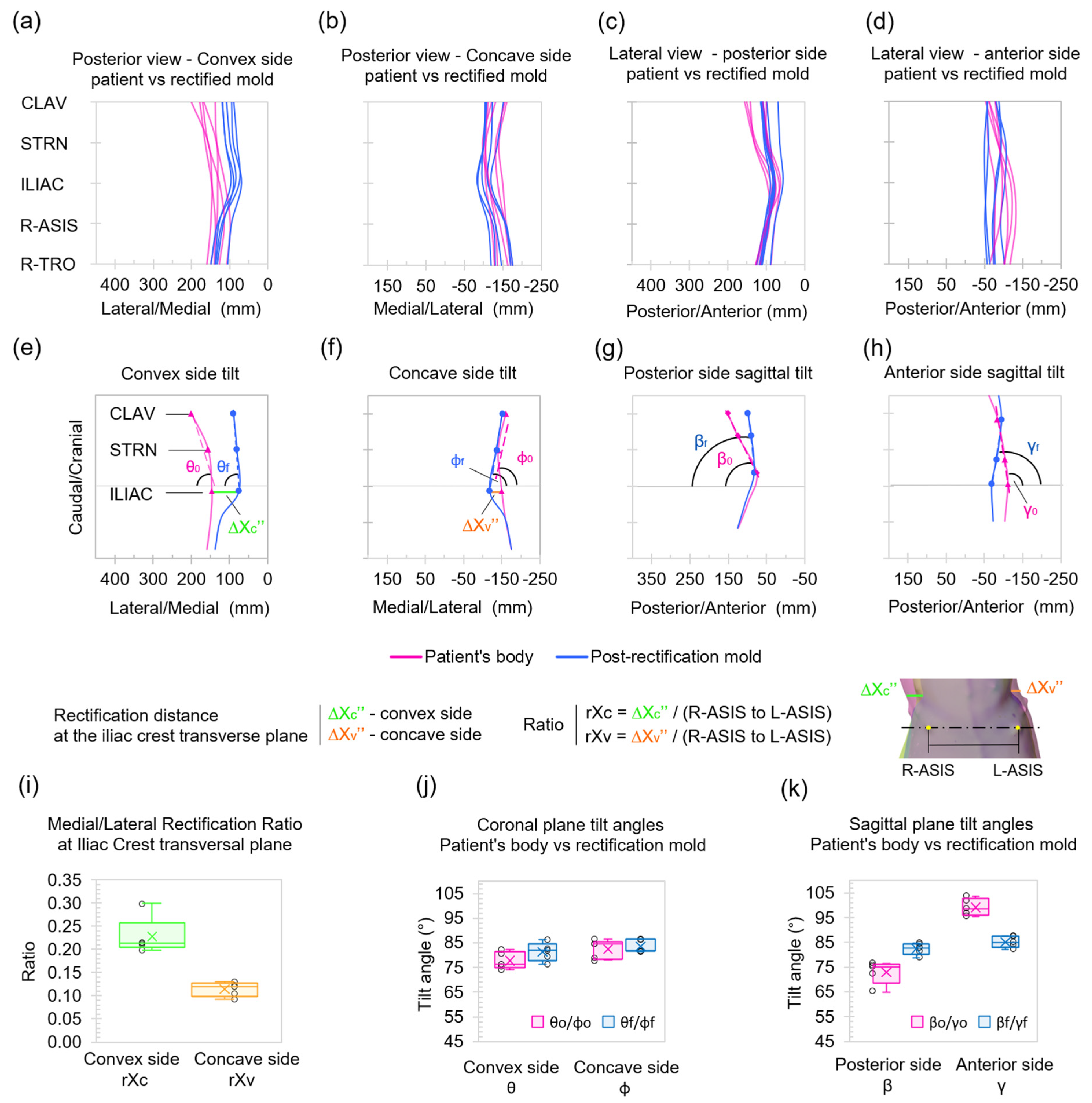
3.3. Three-Dimensional Surface Deviations
4. Discussion
4.1. Anatomical Landmark Position Analysis
4.2. Surface Centroid Analysis
4.3. Three-Dimensional Surface Deviation Analysis and Geometric Parameters
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kane, W.J. Scoliosis Prevalence: A Call for a Statement of Terms. Clin. Orthop. Relat. Res. 1977, 126, 43–46. [Google Scholar] [CrossRef]
- Dickson, R.A. Scoliosis in the community. Br. Med. J. 1983, 286, 615–618. [Google Scholar] [CrossRef] [Green Version]
- Weinstein, S. Adolescent idiopathic scoliosis: Prevalence and natural history. In The Pediatric Spine: Principles and Practice; Weinstein, S., Ed.; Raven Press: New York, NY, USA, 1994; pp. 463–478. [Google Scholar]
- Soucacos, P.N.; Soucacos, P.K.; Zacharis, K.C.; Beris, A.E.; Xenakis, T.A. School-screening for scoliosis. A prospective epidemiological study in northwestern and central Greece. J. Bone Jt. Surg. Am. 1997, 79, 1498–1503. [Google Scholar] [CrossRef]
- Pin, L.H.; Mo, L.Y.; Lin, L.; Hua, L.K.; Hui, H.P.; Hui, D.S.; Chang, B.D.; Chang, Y.Y.; Yuan, L. Early diagnosis of scoliosis based on school-screening. J. Bone Jt. Surg. Am. Vol. 1985, 67, 1202–1205. [Google Scholar] [CrossRef]
- Schlenzka, D.; Yrjönen, T. Bracing in adolescent idiopathic scoliosis. J. Child. Orthop. 2013, 7, 51–55. [Google Scholar] [CrossRef] [Green Version]
- Fayssoux, R.S.; Cho, R.H.; Herman, M.J. A History of Bracing for Idiopathic Scoliosis in North America. Clin. Orthop. Relat. Res. 2010, 468, 654–664. [Google Scholar] [CrossRef] [Green Version]
- Emans, J.B.; Kaelin, A.; Bancel, P.; Hall, J.E.; Miller, M.E. The Boston Bracing System for Idiopathic Scoliosis: Follow-up Results in 295 Patients. Spine 1986, 11, 792–801. [Google Scholar] [CrossRef]
- Allington, N.J.; Bowen, J.R. Adolescent idiopathic scoliosis: Treatment with the Wilmington brace. A comparison of full-time and part-time use. J. Bone Jt. Surg. Am. Vol. 1996, 78, 1056–1062. [Google Scholar] [CrossRef]
- Piazza, M.R.; Bassett, G.S. Curve progression after treatment with the Wilmington brace for idiopathic scoliosis. J. Pediatr. Orthop. 1990, 10, 39–43. [Google Scholar] [CrossRef]
- Watts, H.G.; Hall, J.E.; Stanish, W. The Boston brace system for the treatment of low thoracic and lumbar scoliosis by the use of a girdle without superstructure. Clin. Orthop. Relat. Res. 1977, 87–92. [Google Scholar] [CrossRef]
- Weinstein, S.L.; Dolan, L.A.; Wright, J.G.; Dobbs, M.B. Effects of bracing in adolescents with idiopathic scoliosis. N. Engl. J. Med. 2013, 369, 1512–1521. [Google Scholar] [CrossRef] [Green Version]
- Katz, D.E.; Herring, J.A.; Browne, R.H.; Kelly, D.M.; Birch, J.G. Brace wear control of curve progression in adolescent idiopathic scoliosis. J. Bone Jt. Surg. Am. Vol. 2010, 92, 1343–1352. [Google Scholar] [CrossRef] [PubMed]
- Sanders, J.O.; Newton, P.O.; Browne, R.H.; Katz, D.E.; Birch, J.G.; Herring, J.A. Bracing for idiopathic scoliosis: How many patients require treatment to prevent one surgery? J. Bone Jt. Surg. Am. Vol. 2014, 96, 649–653. [Google Scholar] [CrossRef] [PubMed]
- Sankar, W.N.; Albrektson, J.; Lerman, L.; Tolo, V.T.; Skaggs, D.L. Scoliosis in-brace curve correction and patient preference of CAD/CAM versus plaster molded TLSOs. J. Child. Orthop. 2007, 1, 345–349. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wong, M.S. Computer-aided design and computer-aided manufacture (CAD/CAM) system for construction of spinal orthosis for patients with adolescent idiopathic scoliosis. Physiother. Theory Pract. 2011, 27, 74–79. [Google Scholar] [CrossRef]
- Lou, E.H.; Chan, A.C.Y.; Donauer, A.; Tilburn, M.; Hill, D.L. Ultrasound-assisted brace casting for adolescent idiopathic scoliosis, IRSSD Best research paper 2014. Scoliosis 2015, 10, 13. [Google Scholar] [CrossRef] [Green Version]
- Cobetto, N.; Aubin, C.-E.; Clin, J.; Le May, S.; Desbiens-Blais, F.; Labelle, H.; Parent, S. Braces Optimized with Computer-Assisted Design and Simulations Are Lighter, More Comfortable, and More Efficient Than Plaster-Cast Braces for the Treatment of Adolescent Idiopathic Scoliosis. Spine Deform. 2014, 2, 276–284. [Google Scholar] [CrossRef]
- Pazos, V.; Cheriet, F.; Danserau, J.; Ronsky, J.; Zernicke, R.; Labelle, H. Reliability of trunk shape measurements based on 3-D surface reconstructions. Eur. Spine J. 2007, 16, 1882–1891. [Google Scholar] [CrossRef] [Green Version]
- Eldeeb, H.; Asfour, S.; Boubekri, N. CT/MR imaging: A design tool for custom orthosis. Disabil. Rehabil. 2000, 22, 583–590. [Google Scholar] [CrossRef]
- De Santis, R.; Gloria, A.; Viglione, S.; Maietta, S.; Nappi, F.; Ambrosio, L.; Ronca, D. 3D laser scanning in conjunction with surface texturing to evaluate shift and reduction of the tibiofemoral contact area after meniscectomy. J. Mech. Behav. Biomed. Mater. 2018, 88, 41–47. [Google Scholar] [CrossRef]
- Wong, M.S.; Cheng, J.C.Y.; Lo, K.H. A comparison of treatment effectiveness between the CAD/CAM method and the manual method for managing adolescent idiopathic scoliosis. Prosthet. Orthot. Int. 2005, 29, 105–111. [Google Scholar] [CrossRef]
- Desbiens-Blais, F.; Clin, J.; Parent, S.; Labelle, H.; Aubin, C.-E. New brace design combining CAD/CAM and biomechanical simulation for the treatment of adolescent idiopathic scoliosis. Clin. Biomech. 2012, 27, 999–1005. [Google Scholar] [CrossRef]
- Labelle, H.; Bellefleur, C.; Joncas, J.; Aubin, C.-E.; Cheriet, F. Preliminary evaluation of a computer-assisted tool for the design and adjustment of braces in idiopathic scoliosis: A prospective and randomized study. Spine 2007, 32, 835–843. [Google Scholar] [CrossRef]
- Cottalorda, J.; Kohler, R.; Garin, C.; Genevois, P.; Lecante, C.; Berge, B. Orthoses for mild scoliosis: A prospective study comparing traditional plaster mold manufacturing with fast, noncontact, 3-dimensional acquisition. Spine 2005, 30, 399–405. [Google Scholar] [CrossRef]
- Rigo, M.D.; Gallo, D.; Dallmayer, R. In-brace correction of the Cobb angle with RSC-CAD CAM compared with “hand made” from the original author. Scoliosis 2010, 5, O68. [Google Scholar] [CrossRef] [Green Version]
- De Santis, R.; Gloria, A.; Russo, T.; D’Amora, U.; Zeppetelli, S.; Tampieri, A.; Herrmannsdörfer, T.; Ambrosio, L. A route toward the development of 3D magnetic scaffolds with tailored mechanical and morphological properties for hard tissue regeneration: Preliminary study. Virtual Phys. Prototyp. 2011, 6, 189–195. [Google Scholar] [CrossRef]
- Lanzotti, A.; Martorelli, M.; Maietta, S.; Gerbino, S.; Penta, F.; Gloria, A. A comparison between mechanical properties of specimens 3D printed with virgin and recycled PLA. Procedia Cirp 2019, 79, 143–146. [Google Scholar] [CrossRef]
- Thometz, J.G.; Lamdan, R.; Liu, X.C.; Lyon, R. Relationship between Quantec measurement and Cobb angle in patients with idiopathic scoliosis. J. Pediatr. Orthop. 2000, 20, 512–516. [Google Scholar] [CrossRef]
- Mínguez, M.F.; Buendía, M.; Cibrián, R.M.; Salvador, R.; Laguía, M.; Martín, A.; Gomar, F. Quantifier variables of the back surface deformity obtained with a noninvasive structured light method: Evaluation of their usefulness in idiopathic scoliosis diagnosis. Eur. Spine J. 2007, 16, 73–82. [Google Scholar] [CrossRef] [Green Version]
- Adankon, M.M.; Chihab, N.; Dansereau, J.; Labelle, H.; Cheriet, F. Scoliosis follow-up using noninvasive trunk surface acquisition. IEEE Trans. Biomed. Eng. 2013, 60, 2262–2270. [Google Scholar] [CrossRef]
- Klos, S.S.; Liu, X.-C.; Lyon, R.M.; Tassone, J.C.; Thometz, J.G. Reliability of a functional classification system in the monitoring of patients with idiopathic scoliosis. Spine 2007, 32, 1662–1666. [Google Scholar] [CrossRef]
- Navarro, I.J.R.L.; da Rosa, B.N.; Candotti, C.T. Anatomical reference marks, evaluation parameters and reproducibility of surface topography for evaluating the adolescent idiopathic scoliosis: A systematic review with meta-analysis. Gait Posture 2019, 69, 112–120. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sanz-Pena, I.; Arachchi, S.; Halwala-Vithanage, D.; Mallikarachchi, S.; Kirumbara-Liyanage, J.; McGregor, A.; Silva, P.; Newell, N. Characterising the Mould Rectification Process for Designing Scoliosis Braces: Towards Automated Digital Design of 3D-Printed Braces. Appl. Sci. 2021, 11, 4665. https://doi.org/10.3390/app11104665
Sanz-Pena I, Arachchi S, Halwala-Vithanage D, Mallikarachchi S, Kirumbara-Liyanage J, McGregor A, Silva P, Newell N. Characterising the Mould Rectification Process for Designing Scoliosis Braces: Towards Automated Digital Design of 3D-Printed Braces. Applied Sciences. 2021; 11(10):4665. https://doi.org/10.3390/app11104665
Chicago/Turabian StyleSanz-Pena, Inigo, Shanika Arachchi, Dhammika Halwala-Vithanage, Sanjaya Mallikarachchi, Jeewantha Kirumbara-Liyanage, Alison McGregor, Pujitha Silva, and Nicolas Newell. 2021. "Characterising the Mould Rectification Process for Designing Scoliosis Braces: Towards Automated Digital Design of 3D-Printed Braces" Applied Sciences 11, no. 10: 4665. https://doi.org/10.3390/app11104665





