Exploring the Role of Anti-Adhesion Gel in Outpatient Operative Hysteroscopy
Abstract
1. Introduction
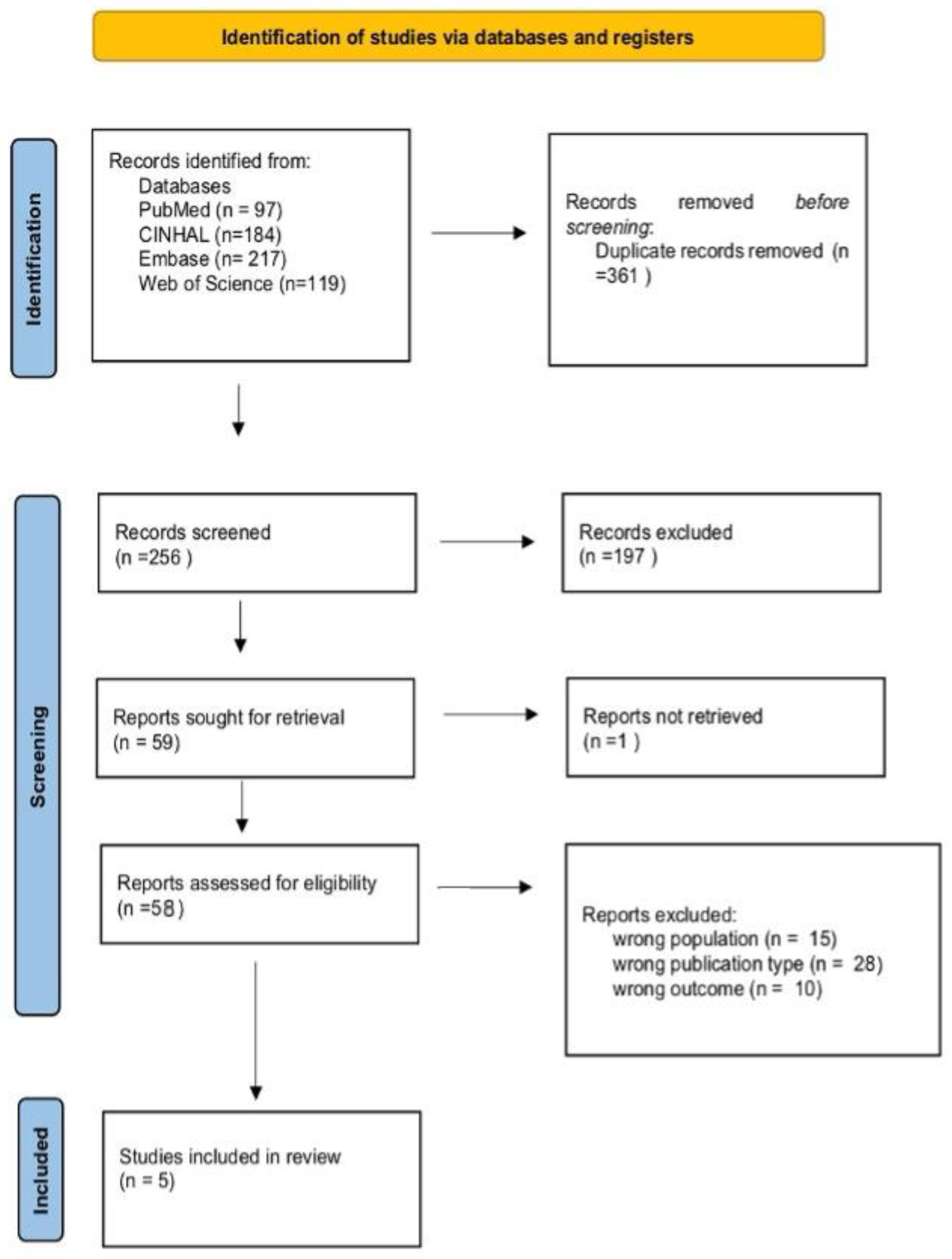
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion Criteria
2.3. Exclusion Criteria
2.4. Data Extraction
2.5. Risk of Bias and Quality Assessment
3. Results
3.1. Prevention of Intrauterine Adhesions
3.2. Reproductive Outcomes
3.3. Comparison Between Treatments
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| RCT | Randomized controlled trials |
| AFS | American Fertility Society |
| ACP | Auto-crosslinked hyaluronic acid |
| IUA | Intrauterine adhesion |
| NR | Not reported |
| HA | Hyaluronic acid gel |
| YD | Yangmo decoction |
| CMC | Sodium carboxymethylcellulose gel |
| CHC | Oral combined hormonal contraception |
| CHA | Cross-linked hyaluronan gel |
References
- Gkrozou, F.; Dimakopoulos, G.; Vrekoussis, T.; Lavasidis, L.; Koutlas, A.; Navrozoglou, I.; Stefos, T.; Paschopoulos, M. Hysteroscopy in Women with Abnormal Uterine Bleeding: A Meta-Analysis on Four Major Endometrial Pathologies. Arch. Gynecol. Obstet. 2015, 291, 1347–1354. [Google Scholar] [CrossRef]
- Carugno, J.; Grimbizis, G.; Franchini, M.; Alonso, L.; Bradley, L.; Campo, R.; Catena, U.; Carlo, D.A.; Attilio, D.S.S.; Martin, F.; et al. International Consensus Statement for Recommended Terminology Describing Hysteroscopic Procedures. J. Minim. Invasive Gynecol. 2022, 29, 385–391. [Google Scholar] [CrossRef]
- Nash, R.; Saidi, S. Outpatient Hysteroscopy: Suitable for All? A Retrospective Cohort Study of Safety, Success and Acceptability in Australia. Aust. N. Z. J. Obstet. Gynaecol. 2024, 64, 475–481. [Google Scholar] [CrossRef]
- Töz, E.; Sancı, M.; Özcan, A.; Beyan, E.; İnan, A.H. Comparison of Classic Terminology with the FIGO PALM-COEIN System for Classification of the Underlying Causes of Abnormal Uterine Bleeding. Int. J. Gynecol. Obstet. 2016, 133, 325–328. [Google Scholar] [CrossRef]
- Pounikar, M.; Shrivastava, D.; Sharma, S.; Tadghare, J. Role of Hysteroscopy in Patients with Previous In Vitro Fertilization Failure: An Institutional Experience in Rural Population. J. Obstet. Gynaecol. India 2023, 73, 77–82. [Google Scholar] [CrossRef]
- Genovese, F.; Di Guardo, F.; Monteleone, M.M.; D’Urso, V.; Colaleo, F.M.; Leanza, V.; Palumbo, M. Hysteroscopy as an Investigational Operative Procedure in Primary and Secondary Infertility: A Systematic Review. Int. J. Fertil. Steril. 2021, 15, 80–87. [Google Scholar] [CrossRef]
- Di Spiezio Sardo, A.; Iorio, G.G.; Guerra, S.; Isaacson, K.; Kafetzis, D.; Conforti, A.; De Angelis, M.C.; Zizolfi, B.; Alviggi, C. The Role of Hysteroscopy in Patients with Adenomyosis and Infertility: Bringing out the Submerged. Fertil. Steril. 2025, 123, 1140–1142. [Google Scholar] [CrossRef] [PubMed]
- Yu, D.; Wong, Y.-M.; Cheong, Y.; Xia, E.; Li, T.-C. Asherman Syndrome—One Century Later. Fertil. Steril. 2008, 89, 759–779. [Google Scholar] [CrossRef] [PubMed]
- March, C.M. Management of Asherman’s Syndrome. Reprod. Biomed. Online 2011, 23, 63–76. [Google Scholar] [CrossRef]
- Hooker, A.; De Leeuw, R.; Twisk, J.; Huirne, J. Reproductive Performance Following Application of Hyaluronic Acid Gel after Dilatation and Curettage for Miscarriage in Women with at Least One Previous Curettage. Hum. Reprod. 2020, 35, i137. [Google Scholar]
- Ma, J.; Gao, W.; Li, D. Recurrent Implantation Failure: A Comprehensive Summary from Etiology to Treatment. Front. Endocrinol. 2022, 13, 1061766. [Google Scholar] [CrossRef]
- Hooker, A.B.; de Leeuw, R.; van de Ven, P.M.; Bakkum, E.A.; Thurkow, A.L.; Vogel, N.E.A.; van Vliet, H.A.A.M.; Bongers, M.Y.; Emanuel, M.H.; Verdonkschot, A.E.M.; et al. Prevalence of Intrauterine Adhesions after the Application of Hyaluronic Acid Gel after Dilatation and Curettage in Women with at Least One Previous Curettage: Short-Term Outcomes of a Multicenter, Prospective Randomized Controlled Trial. Fertil. Steril. 2017, 107, 1223–1231.e3. [Google Scholar] [CrossRef]
- Capella-Monsonís, H.; Kearns, S.; Kelly, J.; Zeugolis, D.I. Battling Adhesions: From Understanding to Prevention. BMC Biomed. Eng. 2019, 1, 5. [Google Scholar] [CrossRef]
- Liu, Y.-R.; Liu, B.; Yang, B.-P.; Lan, Y.; Chi, Y.-G. Efficacy of Hyaluronic Acid on the Prevention of Intrauterine Adhesion and the Improvement of Fertility: A Meta-Analysis of Randomized Trials. Complement. Ther. Clin. Pract. 2022, 47, 101575. [Google Scholar] [CrossRef]
- Anvari-Yazdi, A.F.; Badea, I.; Chen, X. Biomaterials in Postoperative Adhesion Barriers and Uterine Tissue Engineering. Gels 2025, 11, 441. [Google Scholar] [CrossRef]
- Vasvani, S.; Kulkarni, P.; Rawtani, D. Hyaluronic Acid: A Review on Its Biology, Aspects of Drug Delivery, Route of Administrations and a Special Emphasis on its Approved Marketed Products and Recent Clinical Studies. Int. J. Biol. Macromol. 2020, 151, 1012–1029. [Google Scholar] [CrossRef]
- Unanyan, A.; Pivazyan, L.; Krylova, E.; Obosyan, L.; Ishchenko, A. Comparison of Effectiveness of Hyaluronan Gel, Intrauterine Device and Their Combination for Prevention Adhesions in Patients after Intrauterine Surgery: Systematic Review and Meta-Analysis. J. Gynecol. Obstet. Hum. Reprod. 2022, 51, 102334. [Google Scholar] [CrossRef]
- Zheng, F.; Xin, X.; He, F.; Liu, J.; Cui, Y. Meta-Analysis on the Use of Hyaluronic Acid Gel to Prevent Intrauterine Adhesion after Intrauterine Operations. Exp. Ther. Med. 2020, 19, 2672–2678. [Google Scholar] [CrossRef]
- Schmerold, L.; Martin, C.; Mehta, A.; Sobti, D.; Jaiswal, A.K.; Kumar, J.; Feldberg, I.; Munro, M.G.; Lee, W.C. A Cost-Effectiveness Analysis of Intrauterine Spacers Used to Prevent the Formation of Intrauterine Adhesions Following Endometrial Cavity Surgery. J. Med. Econ. 2024, 27, 170–183. [Google Scholar] [CrossRef]
- Mouhayar, Y.; Yin, O.; Mumford, S.L.; Segars, J.H. Hysteroscopic Polypectomy Prior to Infertility Treatment: A Cost Analysis and Systematic Review. Eur. J. Obstet. Gynecol. Reprod. Biol. 2017, 213, 107–115. [Google Scholar] [CrossRef]
- AAGL. Practice Report: Practice Guidelines on Intrauterine Adhesions Developed in Collaboration with the European Society of Gynaecological Endoscopy (ESGE). Gynecol. Surg. 2017, 14, 6. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Tammy, C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brenna, S.E. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. Br. Med. J. 2021, 372, n71. [Google Scholar] [CrossRef]
- De Silva, P.M.; Smith, P.P.; Cooper, N.A.M.; Clark, T.J.; the Royal College of Obstetricians and Gynaecologists. Outpatient Hysteroscopy. Int. J. Obstet. Gynaecol. 2024, 131, 669–678. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A Web and Mobile App for Systematic Reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed]
- Mao, X.; Tao, Y.; Cai, R.; Zhang, J.; Gao, H.; Chen, Q.; Kuang, Y.; Zhang, S. Cross-Linked Hyaluronan Gel to Improve Pregnancy Rate of Women Patients with Moderate to Severe Intrauterine Adhesion Treated with IVF: A Randomized Controlled Trial. Arch. Gynecol. Obstet. 2020, 301, 199–205. [Google Scholar] [CrossRef]
- Esteban Manchado, B.; Lopez-Yarto, M.; Fernandez-Parra, J.; Rodriguez-Oliver, A.; Gonzalez-Paredes, A.; Laganà, A.S.; Garzon, S.; Haimovich, S. Office Hysteroscopic Metroplasty with Diode Laser for Septate Uterus: A Multicenter Cohort Study. Minim. Invasive Ther. Allied Technol. 2022, 31, 441–447. [Google Scholar] [CrossRef]
- Di Spiezio Sardo, A.; Campo, R.; Zizolfi, B.; Santangelo, F.; Meier Furst, R.; Di Cesare, C.; Bettocchi, S.; Vitagliano, A.; Om-belet, W. Long-Term Reproductive Outcomes after Hysteroscopic Treatment of Dysmorphic Uteri in Women with Reproductive Failure: An European Multicenter Study. J. Minim. Invasive Gynecol. 2020, 27, 755–762. [Google Scholar] [CrossRef]
- Dan, J.; Cao, Y. Yangmo Decoction versus Hyaluronic Acid Gel in Women with Intrauterine Re-Adhesion after Hysteroscopic Adhesiolysis: A Retrospective Efficacy and Safety Analysis. BMC Womens Health 2023, 23, 25. [Google Scholar] [CrossRef]
- Trinh, T.T.; Nguyen, K.D.; Pham, H.V.; Ho, T.V.; Nguyen, H.T.; O’Leary, S.; Le, H.T.T.; Pham, H.M. Effectiveness of Hyaluronic Acid Gel and Intrauterine Devices in Prevention of Intrauterine Adhesions after Hysteroscopic Adhesiolysis in Infertile Women. J. Minim. Invasive Gynecol. 2022, 29, 284–290. [Google Scholar] [CrossRef]
- Luerti, M.; Vitagliano, A.; Di Spiezio Sardo, A.; Angioni, S.; Garuti, G.; De Angelis, C.; Del Zoppo, S.; Dealberti, D.; Nappi, L.; Perrini, G. Effectiveness of Hysteroscopic Techniques for Endometrial Polyp Removal: The Italian Multicenter Trial. J. Minim. Invasive Gynecol. 2019, 26, 1169–1176. [Google Scholar] [CrossRef]
- Litta, P.; Cosmi, E.; Saccardi, C.; Esposito, C.; Rui, R.; Ambrosini, G. Outpatient Operative Polypectomy Using a 5 mm-Hysteroscope without Anaesthesia and/or Analgesia: Advantages and Limits. Eur. J. Obstet. Gynecol. Reprod. Biol. 2008, 139, 210–214. [Google Scholar] [CrossRef]
- Walker, S.H.; Gokhale, L. Safety Aspects of Hysteroscopy, Specifically in Relation to Entry and Specimen Retrieval: A UK Survey of Practice. Gynecol. Surg. 2018, 15, 2. [Google Scholar] [CrossRef]
- Vitale, S.G.; Riemma, G.; Carugno, J.; Perez-Medina, T.; Alonso Pacheco, L.; Haimovich, S.; Parry, J.P.; Di Spiezio Sardo, A.; De Franciscis, P. Postsurgical Barrier Strategies to Avoid the Recurrence of Intrauterine Adhesion Formation after Hysteroscopic Adhesiolysis: A Network Meta-Analysis of Randomized Controlled Trials. Am. J. Obstet. Gynecol. 2022, 226, 487–498.e8. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Fang, T.; Dong, Y.; Mao, J.; Wang, J.; Zhao, M.; Wu, R. Comparison of Secondary Prevention Following Hysteroscopic Adhesiolysis in the Improvement of Reproductive Outcomes: A Retrospective Cohort Study. J. Clin. Med. 2024, 13, 73. [Google Scholar] [CrossRef]
- Tang, R.; Zhang, W.; Xiao, X.; Li, W.; Chen, X.; Wang, X. Intrauterine Interventions Options for Preventing Recurrence after Hysteroscopic Adhesiolysis: A Systematic Review and Network Meta-Analysis of Randomized Controlled Trials. Arch. Gynecol. Obstet. 2024, 309, 1847–1861. [Google Scholar] [CrossRef]
- Pan, L.-Z.; Wang, Y.; Chen, X. A Randomized Controlled Study on an Integrated Approach to Prevent and Treat Re-Adhesion after Transcervical Resection of Moderate-to-Severe Intrauterine Adhesions. Clinics 2021, 76, e1987. [Google Scholar] [CrossRef] [PubMed]
- Winata, I.G.S.; Pradnyana, I.W.A.S.; Yusrika, M.U.; Pradnyaan, I.G.B.M.A.; Hartano, E. The Role of Hysteroscopy in Patients with Recurrent Implantation Failure before Starting in Vitro Fertilization: A Systematic Review and Meta-Analysis. Trocar 2023, 4, 10–25. [Google Scholar] [CrossRef]
- Sroussi, J.; Bourret, A.; Pourcelot, A.-G.; Thubert, T.; Lesavre, M.; Legendre, G.; Tuffet, S.; Rousseau, A.; Benifla, J.-L.; HYFACO Group. Does Hyaluronic Acid Gel Reduce Intrauterine Adhesions after Dilation and Curettage in Women with Miscarriage? A Multicentric Randomized Controlled Trial (HYFACO Study). Am. J. Obstet. Gynecol. 2022, 227, 597.e1–597.e8. [Google Scholar] [CrossRef]
- George, J.S.; Naert, M.N.; Lanes, A.; Yin, S.; Bharadwa, S.; Ginsburg, E.S.; Srouji, S.S. Utility of Office Hysteroscopy in Diagnosing Retained Products of Conception in Women with Normal or Inconclusive Ultrasound Scans. Obstet. Gynecol. 2023, 142, 100–110. [Google Scholar] [CrossRef]
- Bailey, A.P.; Jaslow, C.R.; Kutteh, W.H. Minimally Invasive Surgical Options for Congenital and Acquired Uterine Factors Associated with Recurrent Pregnancy Loss. Womens Health 2015, 11, 239–249. [Google Scholar] [CrossRef]
- Lessey, B.A.; Young, S.L. Physiological and Molecular Determinants of Embryo Implantation. Mol. Hum. Reprod. 2014, 20, 12–22. [Google Scholar] [CrossRef]
- Chung, J.P.W.; Chau, O.S.Y.; Law, T.S.M.; Ng, K.; Ip, P.N.P.; Ng, E.Y.L.; Tso, T.K.Y.; Sahota, D.S.; Li, T.C. Incidence of Intrauterine Adhesion after Ultrasound-Guided Manual Vacuum Aspiration for First-Trimester Miscarriages: A Prospective Cohort Study. Arch. Gynecol. Obstet. 2024, 309, 669–678. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Shi, X.; Song, D.; Liu, Y.; Huang, X.; Xiao, Y.; Yang, L.; Xia, E.; Li, T.-C. The Efficacy of Auto-Cross-Linked Hyaluronic Acid Gel in Addition to Oestradiol and Intrauterine Balloon Insertion in the Prevention of Adhesion Reformation after Hysteroscopic Adhesiolysis. Reprod. Biomed. Online 2022, 45, 501–507. [Google Scholar] [CrossRef]
- Torres-de la Roche, L.A.; Bérard, V.; de Wilde, M.S.; Devassy, R.; Wallwiener, M.; De Wilde, R.L. Chemically Modified Hyaluronic Acid for Prevention of Post-Surgical Adhesions: New Aspects of Gel Barriers Physical Profiles. J. Clin. Med. 2022, 11, 931. [Google Scholar] [CrossRef]
- Dou, Y.; Yu, T.; Li, Z.; Wang, J.; Jiang, Y.; Liu, Y. Short- and Long-Term Outcomes of Postoperative Intrauterine Application of Hyaluronic Acid Gel: A Meta-Analysis of Randomized Controlled Trials. J. Minim. Invasive Gynecol. 2022, 29, 934–942. [Google Scholar] [CrossRef] [PubMed]
| Author (Year) [Ref] | Study Design | Sample Size | Strengths | Limitations |
|---|---|---|---|---|
| Mao et al. (2020) [25] | RCT | 306 | Randomized design; moderate sample size; standardized intervention protocol | No blinding; single-center |
| Berta Esteban Manchado et al. (2022) [26] | Prospective cohort | 40 | Clear inclusion criteria; detailed reproductive outcomes | Small sample size; single-center |
| Di Spiezio Sardo et al. (2020) [27] | Retrospective multicenter cohort | 214 | Multicenter design; long follow-up | Retrospective nature; variability in protocols |
| Dan et al. (2023) [28] | Retrospective cohort | 395 | Large sample; direct comparison with alternative therapy | Retrospective design; unclear blinding |
| Trinh et al. (2022) [29] | Retrospective study | 200 | Multigroup comparison; clinically relevant endpoints | Retrospective design; incomplete follow-up data |
| Author Country (Ordered by Year) | Study Type | Sample Size | Type of Patients/Setting/Type of Hysteroscope | Intervention | Control | Results | Follow-Up |
|---|---|---|---|---|---|---|---|
| Dan et al. (2023), China [28] | Retrospective cohort study | 395 | Infertile patients with mild or severe IUAs (AFS from 1 to 12) Unclear Hysteroscope with a diameter of 3–5 mm Pain control: NR | Hysteroscopy adhesiolysis by cold scissors separation + HA gel monthly for 6 months | 1. Hysteroscopy adhesiolysis by cold scissors separation + Oral YD for 6 months and 2. Hysteroscopy adhesiolysis by cold scissors separation + no secondary treatment (EP group) | Intrauterine re-adhesion rate at 6 months: significantly lower re-adhesion in YD vs. HA (p-value = 0.0019) and EP group (p-value = 0.0001). No significant difference between HA and EP (p-value = 0.6171). Pregnancy outcomes: the pregnancy rate was significantly higher in the YD group (52%) compared to HA (36%, p-value = 0.0161) and EP group (21%, p-value < 0.0001). The HA group also had a significantly higher pregnancy rate than the EP group (p-value = 0.0077). Intrauterine re-adhesion: re-adhesion occurred less frequently in the YD group (14%) than in the HA (32%, p-value = 0.0019) and EP group (35%, p-value = 0.0001) groups. No significant difference was found between HA and EP group (p-value = 0.6171). Postoperative AFS score (among women with re-adhesion): the AFS score was significantly lower in the YD group (median 2, IQR 2–1) than in the HA (4, IQR 4–3) and EP group (4, IQR 4–4, (p-value < 0.001). The HA group also showed significantly lower scores than the EP group (p-value< 0.05). Pregnancy after re-adhesion: only women in the YD group achieved pregnancy after re-adhesion treatment (10 out of 15, 67%). No successful pregnancies were reported in the HA or EP group (p-value < 0.0001). Endometrial thickness: no significant difference in endometrial thickness among the groups: YD (3.0 mm, IQR 3.4–2.8), HA (3.45 mm, IQR 4.1–2.85), EP group (3.05 mm, IQR 3.5–2.8) (p-value > 0.05 for all comparisons). | 6 months |
| Berta Esteban Manchado et al. (2022), Spain [26] | Prospective cohort study | 40 | Patients with a septate uterus diagnosis and primary infertility (failed conception after 1 year of regular intercourse) or recurrent pregnancy loss (≥2 miscarriages) Outpatient setting Hysteroscope with 4.3 mm outer sheath diameter (Bettocchi Office Hysteroscope size 5, Karl Storz, Tuttlingen, Germany) Pain control: Conscious sedation (600 mg ibuprofen with 10 mg diazepam orally) | Hysteroscopic metroplasty with diode laser + HA (Hyalobarrier, Nordic Pharma, Zurich, Switzerland) | Hysteroscopic metroplasty with diode laser + CHC | Clinical pregnancy rate: 30/38 (78.9%). Mode of conception: Spontaneous: 17/30 (56.7%). Assisted reproductive technologies (ART): 13/30 (43.3%). Miscarriage rate: 6/30 pregnancies (20%). Live birth rate (per woman): 24/38 (63.2%). Live birth rate (per pregnancy): 24/30 (80%). Term deliveries: 21/30 (70%). Preterm deliveries: 3/30 (10%), including the following: One case of premature rupture of membranes (PROM) at 35 weeks. One case of preeclampsia at 35 weeks. One case of intrauterine growth restriction (IUGR) at 29 weeks. Mode of delivery: Vaginal delivery: 14/24 (58.3%). Cesarean section: 9/24 (37.5%). Maternal complications: No cases of postpartum hemorrhage or uterine rupture were reported | 24 months |
| Trinh et al. (2022), Vietnam [29] | Retrospective study | 200 | Infertile patients with mild or severe IUAs (AFS from 1 to 12) Unclear 5-French hysteroscope (Karl Storz, Tuttlingen, Germany) Pain control: NR | Hysteroscopy adhesiolysis with a monopolar energy source + TCu 380A IUD + 1.1 mL of HA gel (Protad, Unimed Pharm Inc, Republic of Korea) | 1. Hysteroscopy adhesiolysis with a monopolar energy source + TCu 380A IUD (SMB Corporation of India) and 2. Hysteroscopy adhesiolysis with a monopolar energy source + 1.1 mL of HA gel (Protad, Unimed Pharm Inc, Korea) | Recurrence rate: significantly lower in the HA gel + IUD group compared to the IUD group (p-value < 0.0001) and the HA gel group (p-value = 0.0001). No significant difference was found between the IUD and HA gel groups (p-value = 0.6171). | 2 months |
| Di Spiezio Sardo et al. (2020), Italy [27] | Retrospective multicenter cohort study | 214 | Patients with dysmorphic uterus with a history of primary unexplained infertility, and with a history of repeated early miscarriages. Outpatient setting Hysteroscopes with a 4 to 5 mm diameter (Trophy and Integrated Office operative hysteroscopes; Karl Storz, Tüttlingen, Germany) Pain control: Conscious sedation (i.v. midazolam 10 mg and fentanyl 100 g) | Group 1: Primary infertility Hysteroscopy metroplasty using bipolar electrode or scissors + 10 to 15 mL of CMC gel or ACP gel | Group 2: Repeated early spontaneous miscarriage Hysteroscopy metroplasty using bipolar electrode or scissors + 10 to 15 mL of CMC gel or ACP gel | Clinical Pregnancy Rate at 6 months: higher in group 2 vs. group 1 (77% vs. 71.6%, p-value= NR). Miscarriage Rate: Higher in group 2 vs. group 1 (21.6% vs. 19.3%, p-value = NR). Term Delivery Rate: higher in group 1 vs. group 2 (90.6% vs. 72.4%, p-value = NR). Live Birth Rate (per woman): higher in group 2 vs. group 1 (60.4% vs. 57.8%, p-value = NR). Live Birth Rate (per pregnancy): higher in group 1 vs. group 2 (80.6% vs. 78.3%, p-value = NR). Mode of Delivery (Cesarean Section): no significant difference between group 2 and group 1 (55.2% vs. 54.2%, p-value = NR). Vaginal Delivery: no significant difference between group 1 and group 2 (45.8% vs. 44.8%, p-value = NR). Mode of Conception (Spontaneous): higher in group 2 vs. group 1 (56.7% vs. 44.5%, p-value = NR). Assisted Reproductive Technology: higher in group 1 vs. group 2 (55.4% vs. 43.2%, p-value = NR). | 60 months |
| Mao et al. (2020), China [25] | Randomized controlled trial | 306 | Patients with moderate to severe IUA (AFS score ≥ 5); expected to undergo IVF/ICSI and FET Outpatient setting 2.9 mm rigid hysteroscope (Karl Storz, Germany) Pain control: Local anesthesia with lidocaine | Hysteroscopy adhesiolysis + cHA gel (MateRegen® gel; BioRegen Biomedical Ltd., Inc., Changzhou, China) during hysteroscopy and 5–7 days after operation | Hysteroscopy adhesiolysis + no secondary treatment | Adhesion Score (Post Operation): significant decrease in both groups (intervention: from 9.03 ± 1.15 to 2.00 ± 1.58, control: from 8.28 ± 1.71 to 2.13 ± 1.76, p-value ≤ 0.001) Re-adhesion Incidence: higher in control group (75.0% vs. 72.4%, p-value = 0.845) Adhesion Score ≥ 5 (Follow-up): higher in control group (9.4% vs. 6.9%, p-value = 0.483) Average Percentage Change in Adhesion Score: larger change in treatment group (−78.0% vs. −75.6%, p-value = 0.536) Endometrial Thickness: significant increase in both groups (intervention: from 6.35 ± 0.92 to 7.97 ± 1.37, control: from 6.28 ± 0.69 to 7.50 ± 0.60, p-value ≤ 0.001) Endometrial Thickness on Transfer Day: higher in intervention group (p-value ≤ 0.001) Average Percentage Decrease in Endometrial Thickness: higher in intervention group (p-value = 0.048) Clinical Pregnancy Rate: higher in intervention group (p-value < 0.05) Chemical Pregnancy Rate: higher in intervention group (p-value < 0.05) Implantation Rate: higher in intervention group (p-value < 0.05) Singleton Pregnancy Rate: similar between groups (p-value > 0.05) Multiple Pregnancy Rate: similar between groups (p-value > 0.05) Ectopic Pregnancy Rate: similar between groups (p-value > 0.05) Abortion Rate: similar between groups (p-value > 0.05) Live Birth Rate: similar between groups (p-value > 0.05) Histological Assessment (Tubular Glands): trend of increasing tubular glands in intervention group (15.1 ± 13.2 vs. 28.8 ± 30.4, p-value = 0.166) Histological Assessment (Fibrotic Tissue): more fibrotic tissue observed in the endometrium before operation in intervention group | 6 months |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Messina, A.; El Motarajji, S.; Giovannini, I.; Libretti, A.; Savasta, F.; Remorgida, V.; Leo, L.; Masturzo, B. Exploring the Role of Anti-Adhesion Gel in Outpatient Operative Hysteroscopy. Reprod. Med. 2025, 6, 22. https://doi.org/10.3390/reprodmed6030022
Messina A, El Motarajji S, Giovannini I, Libretti A, Savasta F, Remorgida V, Leo L, Masturzo B. Exploring the Role of Anti-Adhesion Gel in Outpatient Operative Hysteroscopy. Reproductive Medicine. 2025; 6(3):22. https://doi.org/10.3390/reprodmed6030022
Chicago/Turabian StyleMessina, Alessandro, Safae El Motarajji, Ilaria Giovannini, Alessandro Libretti, Federica Savasta, Valentino Remorgida, Livio Leo, and Bianca Masturzo. 2025. "Exploring the Role of Anti-Adhesion Gel in Outpatient Operative Hysteroscopy" Reproductive Medicine 6, no. 3: 22. https://doi.org/10.3390/reprodmed6030022
APA StyleMessina, A., El Motarajji, S., Giovannini, I., Libretti, A., Savasta, F., Remorgida, V., Leo, L., & Masturzo, B. (2025). Exploring the Role of Anti-Adhesion Gel in Outpatient Operative Hysteroscopy. Reproductive Medicine, 6(3), 22. https://doi.org/10.3390/reprodmed6030022











