An Irish Multi-Centre Study of Behaviours, Attitudes and Barriers to Exercise in Inflammatory Bowel Disease, a Survey from the Patient’s Perspective
Abstract
:1. Introduction
2. Results
2.1. Results for Patient Demographics
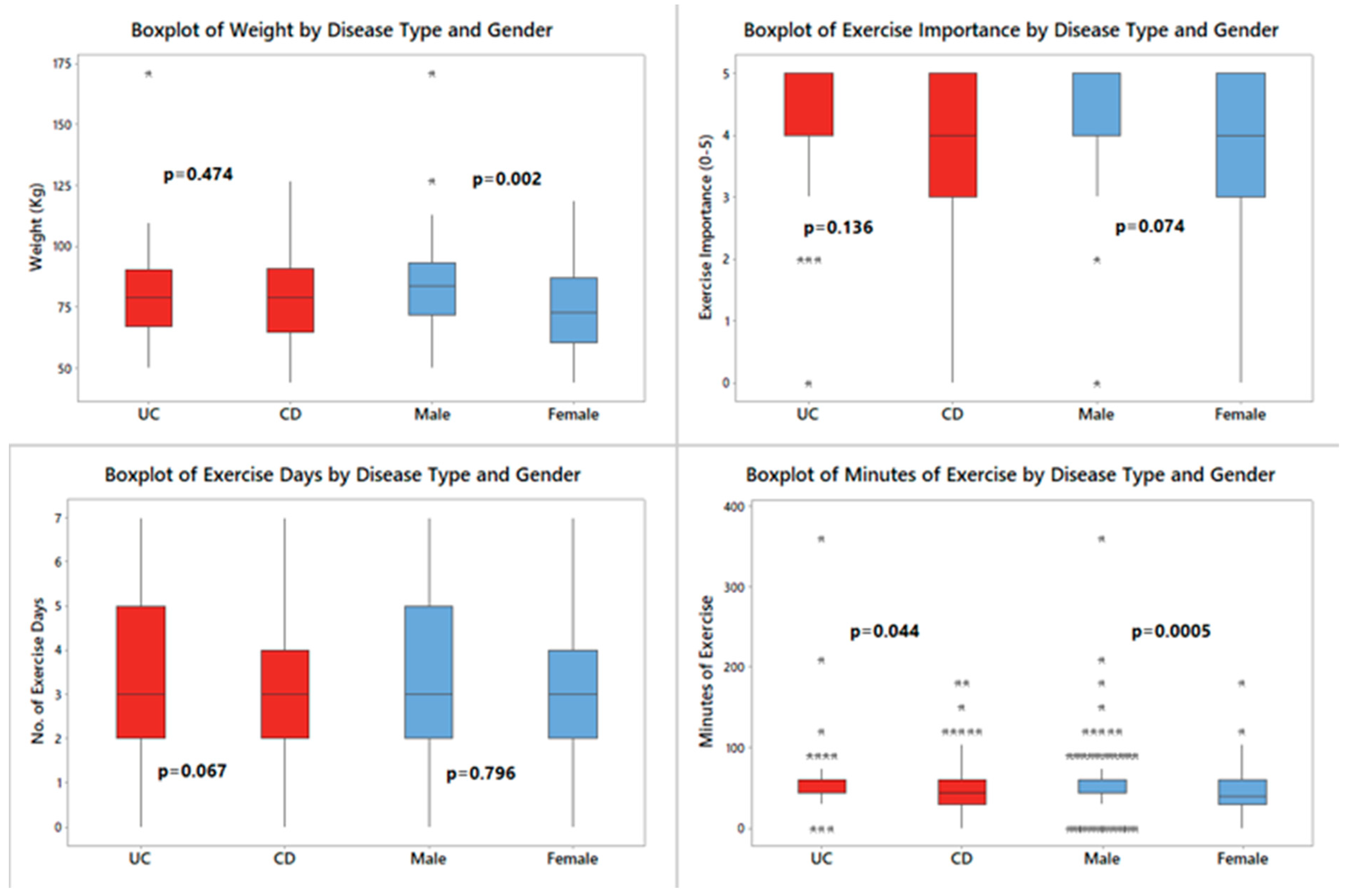
2.2. Participant-Reported Adherence to Exercise Programmes and Barriers to Exercise
2.3. Results of Participants’ Exercise Behaviours and Attitudes toward Exercise
2.4. Perceived Benefits of Exercise and Participant Interest in Exercise Programmes
2.5. Results of Novel Body Image Questions
3. Discussion
4. Materials and Methods
4.1. Ethical Considerations
4.2. Participants
4.3. Study Questionnaire
- Does exercise make you feel physically better?
- Does exercise lead to an improvement in fatigue?
- Does exercise improve your mood?
- Does exercise help to relieve anxiety?
4.4. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Warburton, D.E.R.; Nicol, C.W.; Bredin, S.S.D. Health benefits of physical activity: The evidence. Can. Med. Assoc. J. 2006, 174, 801–809. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- Torres, J.; Mehandru, S.; Colombel, J.F.; Peyrin-Biroulet, L. Crohn’s disease. Lancet 2017, 389, 1741–1755. [Google Scholar] [CrossRef]
- Molodecky, N.A.; Soon, I.S.; Rabi, D.M.; Ghali, W.A.; Ferris, M.; Chernoff, G.; Benchimol, E.I.; Panaccione, R.; Ghosh, S.; Barkema, H.W.; et al. Increasing Incidence and Prevalence of the Inflammatory Bowel Diseases With Time, Based on Systematic Review. Gastroenterology 2012, 142, 46–54.e42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ng, S.C.; Shi, H.Y.; Hamidi, N.; Underwood, E.; Tang, W.; Benchimol, E.I.; Panaccione, R.; Ghosh, S.; Wu, J.C.Y.; Chan, F.K.L.; et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: A systematic review of population-based studies. Lancet 2018, 390, 2769–2778. [Google Scholar] [CrossRef] [PubMed]
- Cronin, O.; Barton, W.; Moran, C.; Sheehan, D.; Whiston, R.; Nugent, H.; McCarthy, Y.; Molloy, C.B.; O’Sullivan, O.; Cotter, P.D.; et al. Moderate-intensity aerobic and resistance exercise is safe and favorably influences body composition in patients with quiescent Inflammatory Bowel Disease: A randomized controlled cross-over trial. BMC Gastroenterol. 2019, 19, 29. [Google Scholar] [CrossRef]
- Eckert, K.G.; Abbasi-Neureither, I.; Köppel, M.; Huber, G. Structured physical activity interventions as a complementary therapy for patients with inflammatory bowel disease—A scoping review and practical implications. BMC Gastroenterol 2019, 19, 115. [Google Scholar] [CrossRef] [Green Version]
- Jones, K.; Baker, K.; Speight, R.A.; Thompson, N.P.; Tew, G.A. Randomised clinical trial: Combined impact and resistance training in adults with stable Crohn’s disease. Aliment. Pharmacol. Ther. 2020, 52, 964–975. [Google Scholar] [CrossRef]
- Tew, G.A.; Leighton, D.; Carpenter, R.; Anderson, S.; Langmead, L.; Ramage, J.; Faulkner, J.; Coleman, E.; Fairhurst, C.; Seed, M.; et al. High-intensity interval training and moderate-intensity continuous training in adults with Crohn’s disease: A pilot randomised controlled trial. BMC Gastroenterol. 2019, 19, 19. [Google Scholar] [CrossRef] [Green Version]
- Schreiner, P.; Rossel, J.-B.; Biedermann, L.; O Valko, P.; Baumann, C.R.; Greuter, T.; Scharl, M.; Vavricka, S.R.; Pittet, V.; Juillerat, P.; et al. Fatigue in inflammatory bowel disease and its impact on daily activities. Aliment. Pharmacol. Ther. 2021, 53, 138–149. [Google Scholar]
- Grimstad, T.; Norheim, K.B.; Isaksen, K.; Leitao, K.; Hetta, A.K.; Carlsen, A.; Karlsen, L.N.; Skoie, I.M.; Gøransson, L.; Harboe, E.; et al. Fatigue in Newly Diagnosed Inflammatory Bowel Disease. J. Crohn’s Colitis 2015, 9, 725–730. [Google Scholar] [CrossRef] [PubMed]
- Muller, K.R.; Prosser, R.; Bampton, P.; Mountifield, R.; Andrews, J.M. Female gender and surgery impair relationships, body image, and sexuality in inflammatory bowel disease: Patient perceptions. Inflamm. Bowel Dis. 2010, 16, 657–663. [Google Scholar] [CrossRef] [PubMed]
- McDermott, E.; Mullen, G.; Moloney, J.; Keegan, D.; Byrne, K.; Doherty, G.A.; Cullen, G.; Malone, K.; Mulcahy, H.E. Body image dissatisfaction: Clinical features, and psychosocial disability in inflammatory bowel disease. Inflamm. Bowel Dis. 2015, 21, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Beese, S.E.; Harris, I.M.; Dretzke, J.; Moore, D. Body image dissatisfaction in patients with inflammatory bowel disease: A systematic review. BMJ Open Gastroenterol. 2019, 6, e000255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kehoe, B.; Skelly, F.; Moyna, N.; Cantwell, M.; Boran, L.; Daly, L.; McCarren, A.; Dowd, K.; Woods, C.; McCaffrey, N.; et al. The effect of participating in MedEx Wellness, a community-based chronic disease exercise rehabilitation programme, on physical, clinical and psychological health: A study protocol for a cohort trial. Contemp. Clin. Trials Commun. 2020, 19, 100591. [Google Scholar] [CrossRef]
- Tully, R.; Loughney, L.; Bolger, J.; Sorensen, J.; McAnena, O.; Collins, C.G.; Carroll, P.A.; Arumugasamy, M.; Murphy, T.J.; Robb, W.B.; et al. The effect of a pre- and post-operative exercise programme versus standard care on physical fitness of patients with oesophageal and gastric cancer undergoing neoadjuvant treatment prior to surgery (The PERIOP-OG Trial): Study protocol for a randomised controlled trial. Trials 2020, 21, 638. [Google Scholar]
- Gatt, K.; Schembri, J.; Katsanos, K.H.; Christodoulou, D.; Karmiris, K.; Kopylov, U.; Pontas, C.; E Koutroubakis, I.; Foteinogiannopoulou, K.; Fabian, A.; et al. Inflammatory Bowel Disease [IBD] and Physical Activity: A Study on the Impact of Diagnosis on the Level of Exercise Amongst Patients With IBD. J. Crohn’s Colitis 2018, 13, 686–692. [Google Scholar] [CrossRef] [Green Version]
- Chan, D.; Robbins, H.; Rogers, S.; Clark, S.; Poullis, A. Inflammatory bowel disease and exercise: Results of a Crohn’s and Colitis UK survey. Front. Gastroenterol. 2013, 5, 44–48. [Google Scholar] [CrossRef] [Green Version]
- Chae, J.; Yang, H.I.; Kim, B.; Park, S.J.; Jeon, J.Y. Inflammatory Bowel Disease Patients’ Participation, Attitude and Preferences Toward Exercise. Int. J. Sport. Med. 2016, 37, 665–670. [Google Scholar] [CrossRef]
- Loudon, C.P.; Corroll, V.; Butcher, J.; Rawsthorne, P.; Bernstein, C.N. The effects of physical exercise on patients with Crohn’s disease. Am. J. Gastroenterol. 1999, 94, 697–703. [Google Scholar] [CrossRef]
- Seeger, W.A.; Thieringer, J.; Esters, P.; Allmendinger, B.; Stein, J.; Schulze, H.; Dignass, A. Moderate endurance and muscle training is beneficial and safe in patients with quiescent or mildly active Crohn’s disease. United Eur. Gastroenterol. J. 2020, 8, 804–813. [Google Scholar] [CrossRef] [PubMed]
- Klare, P.; Nigg, J.; Nold, J.; Haller, B.; Krug, A.B.; Mair, S.; Thoeringer, C.K.; Christle, J.W.; Schmid, R.M.; Halle, M.; et al. The Impact of a Ten-Week Physical Exercise Program on Health-Related Quality of Life in Patients with Inflammatory Bowel Disease: A Prospective Randomized Controlled Trial. Digestion 2015, 91, 239–247. [Google Scholar] [CrossRef] [PubMed]
- Fagan, G.; Schultz, M.; Osborne, H. Sa1877—Individualised, Unsupervised Exercise Program Achieves High Levels of Compliance and Improvements in Patient Reported Outcomes—A Prospective Cohort Study in Patients with Ibd. Gastroenterology 2019, 156, S-438. [Google Scholar] [CrossRef]
- Lamers, C.R.; de Roos, N.M.; Bongers, C.C.W.G.; Haaf, D.S.M.T.; Hartman, Y.A.W.; Witteman, B.J.M.; Hopman, M.T.E. Repeated prolonged moderate-intensity walking exercise does not appear to have harmful effects on inflammatory markers in patients with inflammatory bowel disease. Scand. J. Gastroenterol. 2020, 56, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Spijkerman, R.; Hesselink, L.; Bertinetto, C.; Bongers, C.C.W.G.; Hietbrink, F.; Vrisekoop, N.; Leenen, L.P.H.; Hopman, M.T.E.; Jansen, J.J.; Koenderman, L. Refractory neutrophils and monocytes in patients with inflammatory bowel disease after repeated bouts of prolonged exercise. Cytom. Part B Clin. Cytom. 2021, 100, 676–682. [Google Scholar] [CrossRef] [PubMed]
- Tew, G.A.; Jones, K.; Mikocka-Walus, A. Physical Activity Habits, Limitations, and Predictors in People with Inflammatory Bowel Disease: A Large Cross-sectional Online Survey. Inflamm. Bowel Dis. 2016, 22, 2933–2942. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fagan, G.; Osborne, H.; Schultz, M. Physical Activity in Patients with Inflammatory Bowel Disease: A Cross-Sectional Study. Inflamm. Intest. Dis. 2021, 6, 61–69. [Google Scholar] [CrossRef]
- Chew, H.; Lopez, V. Global Impact of COVID-19 on Weight and Weight-Related Behaviors in the Adult Population: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 1876. [Google Scholar] [CrossRef]
- Heterogeneous contributions of change in population distribution of body mass index to change in obesity and underweight. NCD Risk Factor Collaboration, Lurilli et al. Elife 2021, 10, e60060.
- Rising rural body-mass index is the main driver of the global obesity epidemic in adults. Nature 2019, 569, 260–264. [CrossRef] [Green Version]
- Farrell, D.; McCarthy, G.; Savage, E. Self-reported Symptom Burden in Individuals with Inflammatory Bowel Disease. J. Crohn’s Colitis 2015, 10, 315–322. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Farrell, D. Symptom Burden in Individuals with Inflammatory Bowel Disease: A Mixed Methods Study; University College Cork: Cork, Ireland, 2013. [Google Scholar]
- D’Silva, A.; Fox, D.E.; Nasser, Y.; Vallance, J.K.; Quinn, R.R.; Ronksley, P.E.; Raman, M. Prevalence and Risk Factors for Fatigue in Adults With Inflammatory Bowel Disease: A Systematic Review With Meta-Analysis. Clin. Gastroenterol. Hepatol. 2021, 20, 995–1009.e7. [Google Scholar] [CrossRef] [PubMed]
- McNelly, A.S.; Monti, M.; Grimble, G.K.; Norton, C.; Bredin, F.; Czuber-Dochan, W.J.; Berliner, S.; Forbes, A. The effect of increasing physical activity and/or omega-3 supplementation on fatigue in inflammatory bowel disease. Gastrointest. Nurs. 2016, 14, 39–50. [Google Scholar] [CrossRef]
- van Erp, L.W.; Roosenboom, B.; Komdeur, P.; Dijkstra-Heida, W.; Wisse, J.; Horje, C.S.H.T.; Liem, C.S.; van Cingel, R.E.H.; Wahab, P.J.; Groenen, M.J.M. Improvement of Fatigue and Quality of Life in Patients with Quiescent Inflammatory Bowel Disease Following a Personalized Exercise Program. Dig. Dis. Sci. 2021, 66, 597–604. [Google Scholar] [CrossRef]
- Davelaar, C.M.F. Body Image and its Role in Physical Activity: A Systematic Review. Cureus 2021, 13, e13379. [Google Scholar] [CrossRef]
- Carraça, E.V.; Encantado, J.; Battista, F.; Beaulieu, K.; Blundell, J.E.; Busetto, L.; Baak, M.; Dicker, D.; Ermolao, A.; Farpour-Lambert, N.; et al. Effect of exercise training on psychological outcomes in adults with overweight or obesity: A systematic review and meta-analysis. Obes. Rev. 2021, 22 (Suppl. 4), e13261. [Google Scholar] [CrossRef]
- Duarte, L.S.; Palombo, C.N.T.; Cordero, K.S.; Kurihayashi, A.Y.; Steen, M.; Borges, A.L.V.; Fujimori, E. The association between body weight dissatisfaction with unhealthy eating behaviors and lack of physical activity in adolescents: A systematic review. J. Child Health Care 2020, 25, 44–68. [Google Scholar] [CrossRef]
- Rodrigues, L.; Sim-Sim, M.M.F.; Sousa, L.; Faria-Schützer, D.B.; Surita, F.G. Self-concept and body image of people living with lupus: A systematic review. Int. J. Rheum. Dis. 2021, 24, 1339–1353. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.L.; Yngve, A.; Sallis, J.F.; et al. International Physical Activity Questionnaire: 12-Country Reliability and Validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [Green Version]
- DeFilippis, E.M.; Tabani, S.; Warren, R.U.; Christos, P.J.; Bosworth, B.P.; Scherl, E.J. Exercise and Self-Reported Limitations in Patients with Inflammatory Bowel Disease. Dig. Dis. Sci. 2015, 61, 215–220. [Google Scholar] [CrossRef]
- Lamers, C.R.; de Roos, N.M.; Koppelman, L.J.M.; Hopman, M.T.E.; Witteman, B.J.M. Patient experiences with the role of physical activity in inflammatory bowel disease: Results from a survey and interviews. BMC Gastroenterol. 2021, 21, 172. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.; Chae, J.; Kim, E.H.; Yang, H.I.; Cheon, J.H.; Kim, T.I.; Kim, W.H.; Jeon, J.Y.; Park, S.J. Physical activity and quality of life of patients with inflammatory bowel disease. Medicine 2021, 100, e26290. [Google Scholar] [CrossRef] [PubMed]



| Demographic | Result n (%) |
|---|---|
| Disease type | |
| Crohn’s disease | 126 (62%) |
| Ulcerative colitis | 69 (34%) |
| Indeterminate | 1 (0.5%) |
| Unknown to patient | 7 (3.5%) |
| Gender | |
| Male | 115 (57%) |
| Female | 86 (42%) |
| Non-binary | 1 (0.5%) |
| Rather not disclose | 1 (0.5%) |
| Age category (years) | |
| 18–25 | 37 (18%) |
| 25–35 | 43 (21%) |
| 35–45 | 48 (24%) |
| 45–60 | 55 (27%) |
| 60–70 | 13 (6.4%) |
| 70–80 | 5 (2.5%) |
| 80+ | 2 (1%) |
| Weight (self-reported) | |
| Total responses | 176/203 (87%) |
| Unsure of weight | 26 (13%) |
| Rather not say | 1 (0.5%) |
| Weight result (n, mean kg) | |
| Male | 97, 83 (SD 19.16) |
| Female | 73, 75 (SD 17.82) |
| Crohn’s disease | 107, 79 (SD18.1) |
| Ulcerative colitis | 61, 81 (SD 19.0) |
| Barrier | Result (n, %) |
|---|---|
| Total Response | 117/203 (58%) |
| No energy | 63/117 (54%) |
| No time | 36/117 (31%) |
| Too unwell from IBD symptoms | 39/117 (33%) |
| Joint pains | 36/117 (31%) |
| Toilet concerns | 36/117 (31%) |
| Cost | 10/117 (9%) |
| Do not like exercising | 13/117 (11%) |
| Stoma issues | 5/117 (4%) |
| Exercise Variable | Result n (%) |
|---|---|
| Regular exercise (n, %) | |
| Yes | 148 (73%) |
| No | 55 (27%) |
| No. of days of exercise/week | |
| Total responses | 148/148 (100%) |
| Mean, SD | 4, 1.42 |
| No. of minutes exercising/day | |
| Total responses | 140/148 (95%) |
| Median, IQR | 60, 41.25–60 |
| Rating of exercise importance (0–5) | |
| Total responses | 197/203 (97%) |
| Mean, SD | 4, 0.97 |
| Benefits of exercise (n, %) | |
| 181/196 (92%) |
| 165/196 (84%) |
| 182/196 (93%) |
| 165/190 (87%) |
| Preferred location of exercise (more than one answer allowed) | |
| Total responses | 201/203 (99%) |
| 141/201 (70%) |
| 40/201 (20%) |
| 49/201 (24%) |
| Difficulty adhering to exercise programmes | |
| Total responses | 198/203 (98%) |
| Yes | 133/198 (67%) |
| Adherence difficulty due to IBD diagnosis | |
| Total responses | 131/133 (99%) |
| Yes | 83/131 (63%) |
| Change in exercise pattern post-diagnosis | |
| Total responses | 188/203 (93%) |
| Yes | 124/188 (66%) |
| If yes, did you exercise more/less: | |
| Total responses | 124/124 (100%) |
| Less | 93/124 (75%) |
| Categorical Data | Pearson Chi-Square | DF | p Value | Fisher’s Exact Test |
|---|---|---|---|---|
| Gender | ||||
| Female vs. Male | 7.206 | 1 | 0.007 | 0.010 |
| Disease Type | ||||
| CD vs. UC | 0.202 | 1 | 0.653 | 0.753 |
| Age | ||||
| <45 yrs. vs. >45 yrs. | 1.982 | 1 | 0.020 | 0.029 |
| Exercise pattern | ||||
| Irregular vs. Regular | 0.707 | 1 | 0.400 | 0.506 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gettigan Mc, N.; Allen, K.; Foley, C.; Bennett, S.; Lardner, C.; Lukose, T.; Kelly, O.; O’Toole, A.; Boland, K. An Irish Multi-Centre Study of Behaviours, Attitudes and Barriers to Exercise in Inflammatory Bowel Disease, a Survey from the Patient’s Perspective. Gastrointest. Disord. 2022, 4, 312-323. https://doi.org/10.3390/gidisord4040029
Gettigan Mc N, Allen K, Foley C, Bennett S, Lardner C, Lukose T, Kelly O, O’Toole A, Boland K. An Irish Multi-Centre Study of Behaviours, Attitudes and Barriers to Exercise in Inflammatory Bowel Disease, a Survey from the Patient’s Perspective. Gastrointestinal Disorders. 2022; 4(4):312-323. https://doi.org/10.3390/gidisord4040029
Chicago/Turabian StyleGettigan Mc, N., K. Allen, C. Foley, S. Bennett, C. Lardner, T. Lukose, O. Kelly, A. O’Toole, and K. Boland. 2022. "An Irish Multi-Centre Study of Behaviours, Attitudes and Barriers to Exercise in Inflammatory Bowel Disease, a Survey from the Patient’s Perspective" Gastrointestinal Disorders 4, no. 4: 312-323. https://doi.org/10.3390/gidisord4040029
APA StyleGettigan Mc, N., Allen, K., Foley, C., Bennett, S., Lardner, C., Lukose, T., Kelly, O., O’Toole, A., & Boland, K. (2022). An Irish Multi-Centre Study of Behaviours, Attitudes and Barriers to Exercise in Inflammatory Bowel Disease, a Survey from the Patient’s Perspective. Gastrointestinal Disorders, 4(4), 312-323. https://doi.org/10.3390/gidisord4040029





