Perceived Barriers to Exercise in Adults with Traumatic Brain Injury Vary by Age
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Demographics
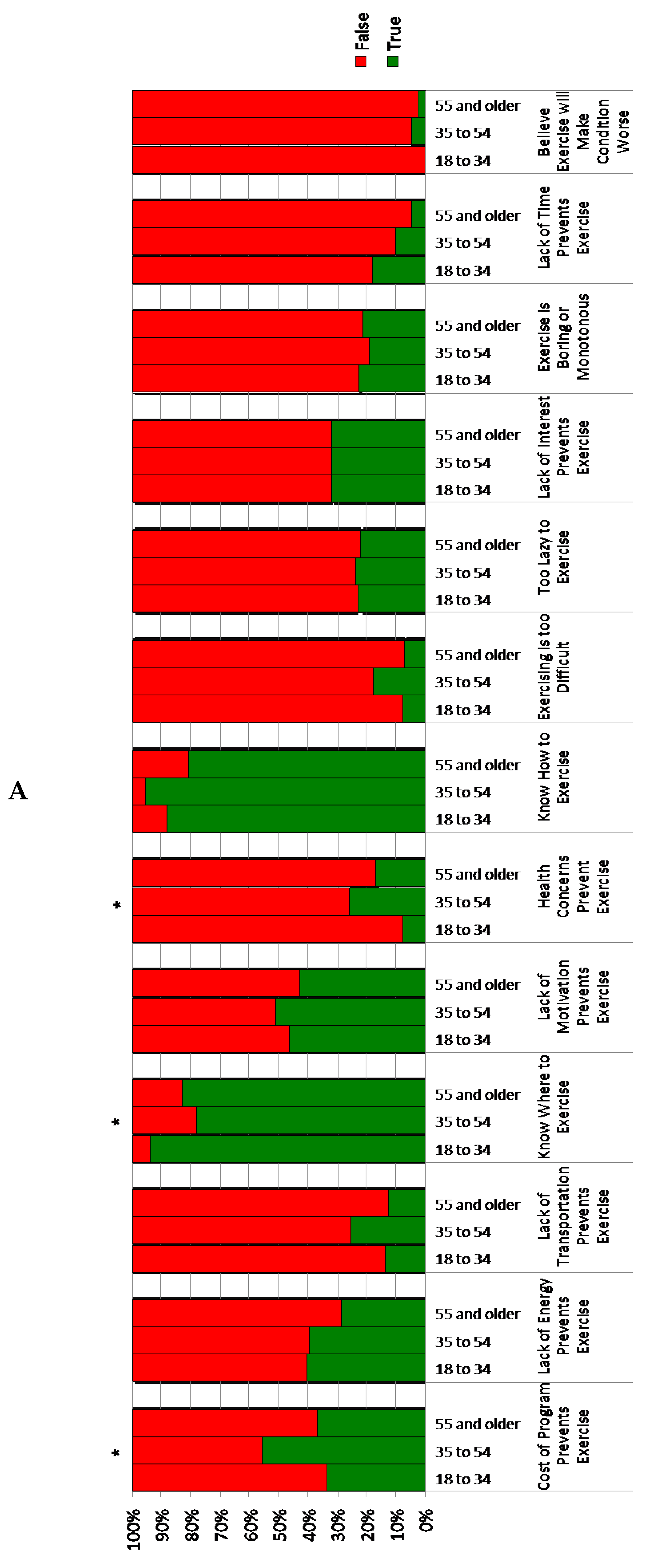
3.2. Perceived Barriers to Exercise Participation by Age Group
4. Discussion
4.1. Personal Factors
4.2. Environmental Factors
4.3. Strengths/Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Centers for Disease Control and Prevention. Centers for Disease Control and Prevention Report to Congress on Traumatic Brain Injury in the United States: Epidemiology and Rehabilitation 2015; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2015.
- Selassie, A.W.; Varma, A.; Saunders, L.L. Current trends in venous thromboembolism among persons hospitalized with acute traumatic spinal cord injury: Does early access to rehabilitation matter? Arch. Phys. Med. Rehabil. 2011, 92, 1534–1541. [Google Scholar] [CrossRef] [PubMed]
- Zaloshnja, E.; Miller, T.; Langlois, J.A.; Selassie, A.W. Prevalence of long-term disability from traumatic brain injury in the civilian population of the United States, 2005. J. Head Trauma Rehabil. 2008, 23, 394–400. [Google Scholar] [CrossRef] [PubMed]
- Coronado, V.G.; Thomas, K.E.; Sattin, R.W.; Johnson, R.L. The CDC traumatic brain injury surveillance system: Characteristics of persons aged 65 years and older hospitalized with a TBI. J. Head Trauma Rehabil. 2005, 20, 215–228. [Google Scholar] [CrossRef] [PubMed]
- Dams-O’Connor, K.; Cuthbert, J.P.; Whyte, J.; Corrigan, J.D.; Faul, M.; Harrison-Felix, C. Traumatic brain injury among older adults at level I and II trauma centers. J. Neurotrauma 2013, 30, 2001–2013. [Google Scholar] [CrossRef] [PubMed]
- Corrigan, J.D.; Cuthbert, J.P.; Harrison-Felix, C.; Whiteneck, G.G.; Bell, J.M.; Miller, A.C.; Coronado, V.G.; Pretz, C.R. US population estimates of health and social outcomes 5 years after rehabilitation for traumatic brain injury. J. Head Trauma Rehabil. 2014, 29, E1-9. [Google Scholar] [CrossRef] [PubMed]
- Frankel, J.E.; Marwitz, J.H.; Cifu, D.X.; Kreutzer, J.S.; Englander, J.; Rosenthal, M. A follow-up study of older adults with traumatic brain injury: Taking into account decreasing length of stay. Arch. Phys. Med. Rehabil. 2006, 87, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Devine, J.M.; Wong, B.; Gervino, E.; Pascual-Leone, A.; Alexander, M.P. Independent, Community-Based Aerobic Exercise Training for People with Moderate-to-Severe Traumatic Brain Injury. Arch. Phys. Med. Rehabil. 2016, 97, 1392–1397. [Google Scholar] [CrossRef] [PubMed]
- Lorenz, L.S.; Charrette, A.L.; O’Neil-Pirozzi, T.M.; Doucett, J.M.; Fong, J. Healthy body, healthy mind: A mixed methods study of outcomes, barriers and supports for exercise by people who have chronic moderate-to-severe acquired brain injury. Disabil. Health J. 2018, 11, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Schwandt, M.; Harris, J.E.; Thomas, S.; Keightley, M.; Snaiderman, A.; Colantonio, A. Feasibility and effect of aerobic exercise for lowering depressive symptoms among individuals with traumatic brain injury: A pilot study. J. Head Trauma Rehabil. 2012, 27, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Wise, E.K.; Hoffman, J.M.; Powell, J.M.; Bombardier, C.H.; Bell, K.R. Benefits of exercise maintenance after traumatic brain injury. Arch. Phys. Med. Rehabil. 2012, 93, 1319–1323. [Google Scholar] [CrossRef] [PubMed]
- Chin, L.M.K.; Chan, L.; Woolstenhulme, J.G.; Christensen, E.J.; Shenouda, C.N.; Keyser, R.E. Improved Cardiorespiratory Fitness with Aerobic Exercise Training in Individuals With Traumatic Brain Injury. J. Head Trauma Rehabil. 2015, 30, 382–390. [Google Scholar] [CrossRef] [PubMed]
- Hassett, L.; Moseley, A.M.; Harmer, A.R. Fitness training for cardiorespiratory conditioning after traumatic brain injury. Cochrane Database Syst. Rev. 2017, 12, CD006123. [Google Scholar] [PubMed]
- Weinstein, A.A.; Chin, L.M.K.; Collins, J.; Goel, D.; Keyser, R.E.; Chan, L. Effect of Aerobic Exercise Training on Mood in People with Traumatic Brain Injury: A Pilot Study. J. Head Trauma Rehabil. 2017, 32, E49–E56. [Google Scholar] [CrossRef] [PubMed]
- Chanpimol, S.; Seamon, B.; Hernandez, H.; Harris-Love, M.; Blackman, M.R. Using Xbox kinect motion capture technology to improve clinical rehabilitation outcomes for balance and cardiovascular health in an individual with chronic TBI. Arch. Physiother. 2017, 7. [Google Scholar] [CrossRef] [PubMed]
- Blake, H.; Batson, M. Exercise intervention in brain injury: A pilot randomized study of Tai Chi Qigong. Clin. Rehabil. 2009, 23, 589–598. [Google Scholar] [CrossRef] [PubMed]
- Chin, L.M.; Keyser, R.E.; Dsurney, J.; Chan, L. Improved cognitive performance following aerobic exercise training in people with traumatic brain injury. Arch. Phys. Med. Rehabil. 2015, 96, 754–759. [Google Scholar] [CrossRef] [PubMed]
- Gordon, W.A.; Sliwinski, M.; Echo, J.; McLoughlin, M.; Sheerer, M.S.; Meili, T.E. The benefits of exercise in individuals with traumatic brain injury: A retrospective study. J. Head Trauma Rehabil. 1998, 13, 58–67. [Google Scholar] [CrossRef] [PubMed]
- Palmer-McLean, K.; Harbst, K.B. Chapter 36: Stroke and Brain Injury. In ACSM’s Exercise Management for Persons with Chronic Diseases and Disabilities; Human Kinetics: Champaign, IL, USA, 2003. [Google Scholar]
- Reavenall, S.; Blake, H. Determinants of physical activity participation following traumatic brain injury. Int. J. Ther. Rehabil. 2010, 17, 360–369. [Google Scholar] [CrossRef] [Green Version]
- Hamilton, M.; Williams, G.; Bryant, A.; Clark, R.; Spelman, T. Which factors influence the activity levels of individuals with traumatic brain injury when they are first discharged home from hospital? Brain Inj. 2015, 29, 1572–1580. [Google Scholar] [CrossRef] [PubMed]
- Driver, S.; Ede, A.; Dodd, Z.; Stevens, L.; Warren, A.M. What barriers to physical activity do individuals with a recent brain injury face? Disabil. Health J. 2012, 5, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, M.; Khan, M.; Clark, R.; Williams, G.; Bryant, A. Predictors of physical activity levels of individuals following traumatic brain injury remain unclear: A systematic review. Brain Inj. 2016, 30, 819–828. [Google Scholar] [CrossRef] [PubMed]
- Self, M.; Driver, S.; Stevens, L.; Warren, A.M. Physical activity experiences of individuals living with a traumatic brain injury: A qualitative research exploration. Adapt. Phys. Act. Q. APAQ 2013, 30, 20–39. [Google Scholar] [CrossRef]
- Hassett, L.M.; Tate, R.L.; Moseley, A.M.; Gillett, L.E. Injury severity, age and pre-injury exercise history predict adherence to a home-based exercise programme in adults with traumatic brain injury. Brain Inj. 2011, 25, 698–706. [Google Scholar] [CrossRef] [PubMed]
- Sendroy-Terrill, M.; Whiteneck, G.G.; Brooks, C.A. Aging with traumatic brain injury: Cross-sectional follow-up of people receiving inpatient rehabilitation over more than 3 decades. Arch. Phys. Med. Rehabil. 2010, 91, 489–497. [Google Scholar] [CrossRef] [PubMed]
- Whiteneck, G.; Meade, M.A.; Dijkers, M.; Tate, D.G.; Bushnik, T.; Forchheimer, M.B. Environmental factors and their role in participation and life satisfaction after spinal cord injury. Arch. Phys. Med. Rehabil. 2004, 85, 1793–1803. [Google Scholar] [CrossRef] [PubMed]
- Franco, M.R.; Tong, A.; Howard, K.; Sherrington, C.; Ferreira, P.H.; Pinto, R.Z.; Ferreira, M.L. Older people’s perspectives on participation in physical activity: A systematic review and thematic synthesis of qualitative literature. Br. J. Sports Med. 2015, 49, 1268–1276. [Google Scholar] [CrossRef] [PubMed]
- Bedini, L.A. “Just sit down so we can talk”: Perceived Stigma and Community Recreation Pursuits of People with Disabilities. Ther. Recreat. J. 2000, 34, 55–68. [Google Scholar]
- Cardinal, B.J.; Kosma, M.; McCubbin, J.A. Factors influencing the exercise behavior of adults with physical disabilities. Med. Sci. Sports Exerc. 2004, 36, 868–875. [Google Scholar] [CrossRef] [PubMed]
- Ellis, R.; Kosma, M.; Cardinal, B.J.; Bauer, J.J.; McCubbin, J.A. Physical activity beliefs and behaviour of adults with physical disabilities. Disabil. Rehabil. 2007, 29, 1221–1227. [Google Scholar] [CrossRef] [PubMed]
- Nosek, M.A.; Hughes, R.B.; Robinson-Whelen, S.; Taylor, H.B.; Howland, C.A. Physical activity and nutritional behaviors of women with physical disabilities: Physical, psychological, social, and environmental influences. Womens Health Issues Off. Publ. Jacobs Inst. Womens Health 2006, 16, 323–333. [Google Scholar] [CrossRef] [PubMed]
- Rimmer, J.H.; Rubin, S.S.; Braddock, D. Barriers to exercise in African American women with physical disabilities. Arch. Phys. Med. Rehabil. 2000, 81, 182–188. [Google Scholar] [CrossRef]
- Scelza, W.M.; Kalpakjian, C.Z.; Zemper, E.D.; Tate, D.G. Perceived barriers to exercise in people with spinal cord injury. Am. J. Phys. Med. Rehabil. 2005, 84, 576–583. [Google Scholar] [CrossRef] [PubMed]
- Menon, D.K.; Schwab, K.; Wright, D.W.; Maas, A.I. Demographics and Clinical Assessment Working Group of the International and Interagency Initiative toward Common Data Elements for Research on Traumatic Brain Injury and Psychological Health Position statement: Definition of traumatic brain injury. Arch. Phys. Med. Rehabil. 2010, 91, 1637–1640. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Classification of Functioning, Disability and Health: ICF; World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Fekete, C.; Rauch, A. Correlates and determinants of physical activity in persons with spinal cord injury: A review using the International Classification of Functioning, Disability and Health as reference framework. Disabil. Health J. 2012, 5, 140–150. [Google Scholar] [CrossRef] [PubMed]
- Bhalerao, S.U.; Geurtjens, C.; Thomas, G.R.; Kitamura, C.R.; Zhou, C.; Marlborough, M. Understanding the neuropsychiatric consequences associated with significant traumatic brain injury. Brain Inj. 2013, 27, 767–774. [Google Scholar] [CrossRef] [PubMed]
- Ponsford, J.L.; Ziino, C.; Parcell, D.L.; Shekleton, J.A.; Roper, M.; Redman, J.R.; Phipps-Nelson, J.; Rajaratnam, S.M.W. Fatigue and sleep disturbance following traumatic brain injury—Their nature, causes, and potential treatments. J. Head Trauma Rehabil. 2012, 27, 224–233. [Google Scholar] [CrossRef] [PubMed]
- Starkstein, S.E.; Pahissa, J. Apathy following traumatic brain injury. Psychiatr. Clin. North Am. 2014, 37, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Buffart, L.M.; Westendorp, T.; van den Berg-Emons, R.J.; Stam, H.J.; Roebroeck, M.E. Perceived barriers to and facilitators of physical activity in young adults with childhood-onset physical disabilities. J. Rehabil. Med. 2009, 41, 881–885. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kinne, S.; Patrick, D.L.; Maher, E.J. Correlates of exercise maintenance among people with mobility impairments. Disabil. Rehabil. 1999, 21, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Dams-O’Connor, K.; Gibbons, L.E.; Landau, A.; Larson, E.B.; Crane, P.K. Health Problems Precede Traumatic Brain Injury in Older Adults. J. Am. Geriatr. Soc. 2016, 64, 844–848. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kumar, R.G.; Juengst, S.B.; Wang, Z.; Dams-O’Connor, K.; Dikmen, S.S.; O’Neil-Pirozzi, T.M.; Dahdah, M.N.; Hammond, F.M.; Felix, E.R.; Arenth, P.M.; et al. Epidemiology of Comorbid Conditions Among Adults 50 Years and Older with Traumatic Brain Injury. J. Head Trauma Rehabil. 2017. [Google Scholar] [CrossRef] [PubMed]
- Thompson, H.J.; Weir, S.; Rivara, F.P.; Wang, J.; Sullivan, S.D.; Salkever, D.; MacKenzie, E.J. Utilization and costs of health care after geriatric traumatic brain injury. J. Neurotrauma 2012, 29, 1864–1871. [Google Scholar] [CrossRef] [PubMed]
- Harrison-Felix, C.; Kolakowsky-Hayner, S.A.; Hammond, F.M.; Wang, R.; Englander, J.; Dams-O’Connor, K.; Kreider, S.E.D.; Novack, T.A.; Diaz-Arrastia, R. Mortality after surviving traumatic brain injury: Risks based on age groups. J. Head Trauma Rehabil. 2012, 27, E45–E56. [Google Scholar] [CrossRef] [PubMed]
- Ventura, T.; Harrison-Felix, C.; Carlson, N.; Diguiseppi, C.; Gabella, B.; Brown, A.; Devivo, M.; Whiteneck, G. Mortality after discharge from acute care hospitalization with traumatic brain injury: A population-based study. Arch. Phys. Med. Rehabil. 2010, 91, 20–29. [Google Scholar] [CrossRef] [PubMed]
- Cockerham, W.C.; Sharp, K.; Wilcox, J.A. Aging and perceived health status. J. Gerontol. 1983, 38, 349–355. [Google Scholar] [CrossRef] [PubMed]
- Idler, E.L. Age differences in self-assessments of health: Age changes, cohort differences, or survivorship? J. Gerontol. 1993, 48, S289–S300. [Google Scholar] [CrossRef] [PubMed]
- Cuthbert, J.P.; Harrison-Felix, C.; Corrigan, J.D.; Bell, J.M.; Haarbauer-Krupa, J.K.; Miller, A.C. Unemployment in the United States after traumatic brain injury for working-age individuals: Prevalence and associated factors 2 years postinjury. J. Head Trauma Rehabil. 2015, 30, 160–174. [Google Scholar] [CrossRef] [PubMed]
- Johnstone, B.; Mount, D.; Schopp, L.H. Financial and vocational outcomes 1 year after traumatic brain injury. Arch. Phys. Med. Rehabil. 2003, 84, 238–241. [Google Scholar] [CrossRef] [PubMed]
- Justine, M.; Azizan, A.; Hassan, V.; Salleh, Z.; Manaf, H. Barriers to participation in physical activity and exercise among middle-aged and elderly individuals. Singapore Med. J. 2013, 54, 581–586. [Google Scholar] [CrossRef] [PubMed]
- Devitt, R.; Colantonio, A.; Dawson, D.; Teare, G.; Ratcliff, G.; Chase, S. Prediction of long-term occupational performance outcomes for adults after moderate to severe traumatic brain injury. Disabil. Rehabil. 2006, 28, 547–559. [Google Scholar] [CrossRef] [PubMed]
- Forslund, M.V.; Roe, C.; Arango-Lasprilla, J.C.; Sigurdardottir, S.; Andelic, N. Impact of personal and environmental factors on employment outcome two years after moderate-to-severe traumatic brain injury. J. Rehabil. Med. 2013, 45, 801–807. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dondzila, C.J.; Swartz, A.M.; Keenan, K.G.; Harley, A.E.; Azen, R.; Strath, S.J. Geospatial Relationships between Awareness and Utilization of Community Exercise Resources and Physical Activity Levels in Older Adults. J. Aging Res. 2014, 2014, 302690. [Google Scholar] [CrossRef] [PubMed]
- Ashworth, N.L.; Chad, K.E.; Harrison, E.L.; Reeder, B.A.; Marshall, S.C. Home versus center based physical activity programs in older adults. Cochrane Database Syst. Rev. 2005, CD004017. [Google Scholar] [CrossRef]
- Wee, C.C.; McCarthy, E.P.; Davis, R.B.; Phillips, R.S. Physician counseling about exercise. JAMA 1999, 282, 1583–1588. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, N.U.; Delgado, M.; Saxena, A. Trends and disparities in the prevalence of physicians’ counseling on exercise among the U.S. adult population, 2000–2010. Prev. Med. 2017, 99, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Hébert, E.T.; Caughy, M.O.; Shuval, K. Primary care providers’ perceptions of physical activity counselling in a clinical setting: A systematic review. Br. J. Sports Med. 2012, 46, 625–631. [Google Scholar] [CrossRef] [PubMed]
- Dacey, M.L.; Kennedy, M.A.; Polak, R.; Phillips, E.M. Physical activity counseling in medical school education: A systematic review. Med. Educ. Online 2014, 19, 24325. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pugh, M.J.; Swan, A.A.; Carlson, K.F.; Jaramillo, C.A.; Eapen, B.C.; Dillahunt-Aspillaga, C.; Amuan, M.E.; Delgado, R.E.; McConnell, K.; Finley, E.P.; et al. Trajectories of Resilience and Complex Comorbidity Study Team Traumatic Brain Injury Severity, Comorbidity, Social Support, Family Functioning, and Community Reintegration Among Veterans of the Afghanistan and Iraq Wars. Arch. Phys. Med. Rehabil. 2018, 99, S40–S49. [Google Scholar] [CrossRef] [PubMed]
- Ricker, J.H.; Rosenthal, M.; Garay, E.; DeLuca, J.; Germain, A.; Abraham-Fuchs, K.; Schmidt, K.-U. Telerehabilitation needs: A survey of persons with acquired brain injury. J. Head Trauma Rehabil. 2002, 17, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Tolleson, C.; Guillamondegui, O. The success of traumatic brain injury registry outreach. Brain Inj. 2014, 28, 286–291. [Google Scholar] [CrossRef] [PubMed]

| Participant Characteristic | 18 to 34 Years (n = 67) | 35 to 54 Years (n = 63) | 55 Years and Older (n = 42) | p-Value |
|---|---|---|---|---|
| Female sex | 25 (37.31%) | 23 (36.51%) | 15 (35.71%) | 0.9856 |
| Cause of TBI | <0.0001 * | |||
| -- Motor Vehicle | 66 (98.51%) | 24 (38.10%) | 26 (61.90%) | |
| -- Fall | 0 (0%) | 24 (38.10%) | 0 (0%) | |
| -- Pedestrian | 0 (0%) | 2 (3.17%) | 13 (30.95%) | |
| -- Sport | 0 (0%) | 6 (9.52%) | 0 (0%) | |
| -- Assault/GSW | 0 (0%) | 6 (9.52%) | 0 (0%) | |
| -- Other/Unknown | 1 (1.49%) | 1 (1.59%) | 3 (7.14%) | |
| >5 years since TBI | 37 (56.06%) | 31 (49.21%) | 28 (66.67%) | 0.2101 |
| Household income | 0.0009 * | |||
| -- <$20,000/year | 28 (45.90%) | 34 (55.74%) | 9 (23.68%) | |
| -- $20,000–$49,999/year | 15 (24.59%) | 16 (26.23%) | 12 (31.58%) | |
| -- $50,000–$99,999/year | 17 (27.87%) | 5 (8.20%) | 15 (39.47%) | |
| -- >$100,000/year | 1 (1.64%) | 6 (9.84%) | 2 (5.26%) | |
| Employed | <0.0001 * | |||
| -- Full/part time | 25 (37.88%) | 9 (14.29%) | 9 (21.95%) | |
| -- Volunteer | 2 (3.03%) | 1 (1.59%) | 6 (14.63%) | |
| -- Student | 9 (13.64%) | 3 (4.76%) | 0 (0%) | |
| -- Not employed | 30 (45.45%) | 50 (79.37%) | 26 (63.41%) |
| Desire to Exercise | 18 to 34 Years (n = 67) | 35 to 54 Years (n = 63) | 55 Years and Older (n = 42) | p-Value |
|---|---|---|---|---|
| Like to Exercise | 58 (86.57%) | 44 (73.33%) | 29 (69.05%) | 0.1729 |
| Like to Begin Exercise Program | 42 (63.64%) | 39 (61.90%) | 21 (53.85%) | 0.3831 |
| Ever Exercised | 66 (98.51%) | 57 (90.48%) | 41 (97.62%) | 0.1917 |
| Exercise since TBI | 62 (92.54%) | 50 (79.37%) | 34 (82.93%) | 0.2522 |
| Feel exercise will help | 53 (79.10%) | 45 (70.97%) | 36 (85.37%) | 0.2004 |
| 18 to 34 Years (n = 67) | 35 to 54 Years (n = 63) | 55 Years and Older (n = 42) |
|---|---|---|
| Lack of Motivation Prevents Exercise (46.7%) | Cost of Program Prevents Exercise (55.56%) * | Do Not Use Exercise Equipment at Home (45.00%) |
| Do Not Use Exercise Equipment at Home (44.78%) | Lack of Motivation Prevents Exercise (50.79%) | Lack of Motivation Prevents Exercise (42.86%) |
| Lack of Energy Prevents Exercise (40.30%) | Do Not Use Exercise Equipment at Home (47.62%) | Doctor Never Told to Exercise (38.1%)/Something Specific (42.86%) |
| Doctor Never Told to Exercise (38.81%)/Something Specific (22.73%) | Doctor Never Told to Exercise (39.68%)/Something Specific (29.03%) | Cost of Program Prevents Exercise (36.59%) * |
| Cost of Program Prevents Exercise (33.33%) * | Lack of Energy Prevents Exercise (39.68%) | Lack of Interest Prevents Exercise (31.71%) |
| Lack of Interest Prevents Exercise (31.82%) | Lack of Interest Prevents Exercise (31.75%) | Lack of Energy Prevents Exercise (28.57%) |
| Too Lazy to Exercise (22.73%) | Do Not Know Fitness Center That Can Get to (28.57%) * | Did Not Know Fitness Center That Can Get To (24.39%) * |
| Exercise is Boring or Monotonous (22.39%) | Health Concerns Prevent Exercise (25.81%) * | Too Lazy to Exercise (21.95%) |
| Lack of Transportation Prevents Exercise (25.4%) | Fitness Instructor Does Not Meet Needs (21.95%) | |
| Ever Afraid to Leave Home (23.81%) * | Exercise is Boring or Monotonous (21.43%) | |
| Too Lazy to Exercise (23.81%) | ||
| Do Not Know Where to Exercise (22.22%) * |
| Age Group | |||
|---|---|---|---|
| ICFDH Factor, Barrier | 18–34 | 35–54 | 55+ |
| 1. Physical Environmental Factors | |||
| Cost of the program | ✓ | ✓ | ✓ |
| Do not use home equipment | ✓ | ✓ | ✓ |
| Do not know fitness center to get to | ✓ | ✓ | ✓ |
| Do not know where to exercise | ✓ | ||
| Fitness instructor does not meet needs | ✓ | ||
| Lack of transportation | ✓ | ||
| 2. Social Environmental Factors | |||
| Lack of encouragement from doctor | ✓ | ✓ | ✓ |
| 3. Body Function/Structures Factors | |||
| Lack of motivation | ✓ | ✓ | ✓ |
| Lack of energy | ✓ | ✓ | ✓ |
| Too lazy to exercise | ✓ | ✓ | ✓ |
| Health concerns prevent exercise | ✓ | ||
| Too afraid to leave the home | ✓ | ||
| 4. Personal Factors (Beliefs) | |||
| Lack of interest | ✓ | ✓ | ✓ |
| Exercise is boring | ✓ | ||
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pinto, S.M.; Newman, M.A.; Hirsch, M.A. Perceived Barriers to Exercise in Adults with Traumatic Brain Injury Vary by Age. J. Funct. Morphol. Kinesiol. 2018, 3, 47. https://doi.org/10.3390/jfmk3030047
Pinto SM, Newman MA, Hirsch MA. Perceived Barriers to Exercise in Adults with Traumatic Brain Injury Vary by Age. Journal of Functional Morphology and Kinesiology. 2018; 3(3):47. https://doi.org/10.3390/jfmk3030047
Chicago/Turabian StylePinto, Shanti M., Mark A. Newman, and Mark A. Hirsch. 2018. "Perceived Barriers to Exercise in Adults with Traumatic Brain Injury Vary by Age" Journal of Functional Morphology and Kinesiology 3, no. 3: 47. https://doi.org/10.3390/jfmk3030047
APA StylePinto, S. M., Newman, M. A., & Hirsch, M. A. (2018). Perceived Barriers to Exercise in Adults with Traumatic Brain Injury Vary by Age. Journal of Functional Morphology and Kinesiology, 3(3), 47. https://doi.org/10.3390/jfmk3030047





