EEG–Metabolic Coupling and Time Limit at
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants Recruitment and Ethical Approval
2.2. Experimental Sessions
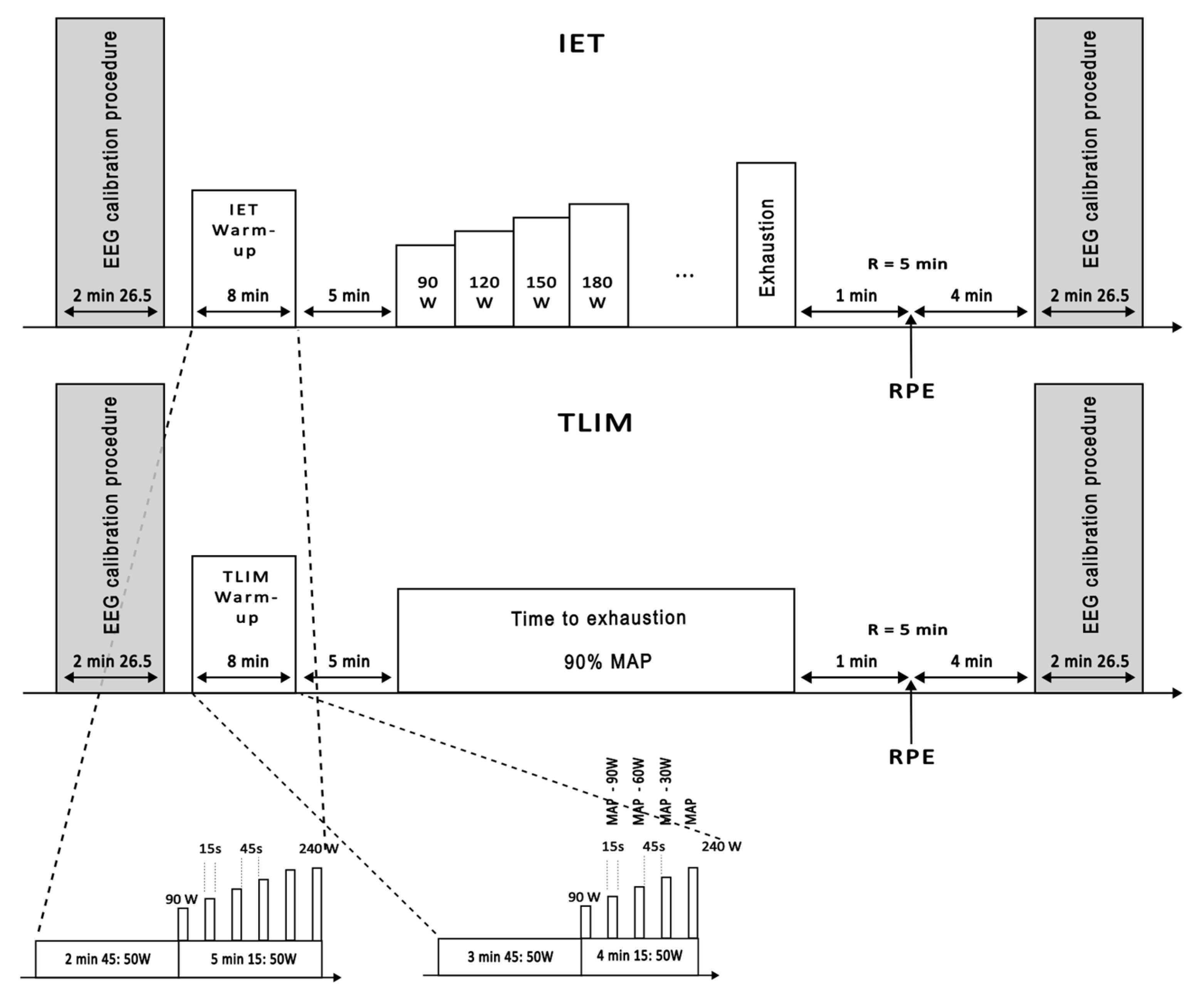
2.2.1. Incremental Exercise Test
- Exhaustion criteria and subjective effort
- Determination of O2max, MAP, and VT2
- ➢
- The O2 increase between two 30 s intervals was <50% of the expected submaximal rise, or
- ➢
- The O2 increase was ≤150 mL·min−1 despite continued workload increase.
2.2.2. Time-to-Exhaustion Test
- TLIM duration: the total time elapsed from the start of the constant-load phase to volitional exhaustion.
- Time to reach O2max: the time between exercise onset and the first point at which O2max was reached, based on plateau criteria.
- Time spent at O2max: the remaining time between O2max attainment and exhaustion, during which O2 remained at maximal levels.
- Exhaustion criteria and O2max Confirmation
2.3. Measurements and Synchronization
2.3.1. Measurements
- Cycling parameters: A CycleOps 400 Pro Indoor Cycle (Saris Cycling Group, Inc. 5253 Verona Road Madison WI 53711, USA) measured power output (W), cadence (rpm), torque (Nm), and heart rate (bpm) via ANT+ sensors connected to the Joule 3.0 CPU. Protocols were pre-programmed for consistency across participants. Data was recorded at 1 Hz and analyzed using PowerAgent software (v7.8.28) (Saris Cycling Group, Inc.).
- Electroencephalography: Brain activity was recorded using a 32-channel ActiCap system (Brain Products, Gilching, Germany), with active gel electrodes placed according to the 10–10 international system; analyses focused on a subset of electrodes (Fp1, Fp2, Fz, C3, Cz, C4, Pz, O1, Oz, O2). To ensure high signal quality and minimize artifacts inherent to intense exercise, a custom-fitted EEG cap was used, with high-quality conductive gel applied to ensure stable contact with the scalp. Impedance was kept <5 kΩ. The reference was placed on the right mastoid and the ground on the lateral third of the spine of the right scapula. We acknowledge that this montage can be susceptible to electromyographic (EMG) or movement artifacts; however, these limitations were specifically addressed during our preprocessing, as detailed in Section 2.4.1. on Artifact Rejection. Signals were amplified (BrainAmp®, band-pass 0.016–1000 Hz), sampled at 5000 Hz, then downsampled to 1000 Hz using anti-aliasing filters. Brain Vision Recorder® (v1.20.0601, Brain Products) was used to capture data. Calibration sequences (eyes open/closed, movements) were performed before and after each test.
- Heart Rate Monitoring: Heart rate (HR) was recorded using two systems. First, a Polar® chest strap synchronized with gas exchange data. Second, a 3-lead electrocardiogram (ECG) with silver electrodes in precordial placement. Instantaneous HR (IHR) was derived from the D2 derivation signal, representing the interval between consecutive R-waves. To address artifacts or missed detections, an offline algorithm corrected IHR variations exceeding a ten beats per minute (bpm) threshold by interpolating between adjacent below-threshold values, producing a clean, resampled signal. The smallest appreciable variation was 0.5 bpm, and the calibrated HR range spanned from 0 to 200 bpm. The IHR time-series was resampled at 10 Hz for subsequent analyses.
- Gas Exchange: Breath-by-breath O2 and CO2, and respiratory exchange ratio (RER) were recorded using a Metamax® 3B analyzer (Cortex Biophysik GmbH, Leipzig, Germany), calibrated before each test according to the manufacturer’s recommendations. Data were synchronized with heart rate recordings and analyzed post-exercise using Metasoft® software (version 3.9.9 SR5, Cortex Biophysik GmbH).
2.3.2. Synchronization
2.4. EEG Analysis
2.4.1. Artifact Rejection
- Initial detection: Sudden signal deviations were flagged using a 2 s sliding window with amplitude thresholding.
- Signal reconstruction: Clean EEG signals were reconstructed via Wiener filtering, preserving cerebral oscillations while minimizing distortions [56].
2.4.2. Spectral Analysis
2.4.3. Slope-Based Indicators
- EEG PSD Slopes: The evolution of spectral power over the entire duration of the TLIM protocol was quantified using Sen’s slope estimator, a robust, non-parametric method suited for monotonic trends in non-normally distributed data.
- EEG–Metabolic Ratio Slopes: To assess the coupling between neural and metabolic responses, EEG power was divided by breath-by-breath values of O2 and CO2, yielding time series such as Theta/O2, Alpha/CO2, or Beta/O2. Sen’s slope was again applied to these ratio time series to evaluate trend in neuro-metabolic interaction during exercise.
2.5. Statistics
2.5.1. Normality and Justification for Non-Parametric Methods
2.5.2. Correlation Analyses
2.5.3. Trend Detection and Slope Estimation
- The Mann–Kendall test was applied to detect monotonic trends in EEG and ventilatory variables across time.
- Sen’s slope estimator was used to calculate the rate of change (slope) for:
- ➢
- EEG power (theta, alpha, and beta bands),
- ➢
- Ventilatory responses (O2 and CO2),
- ➢
- EEG–metabolic ratios (e.g., Alpha/CO2, Beta/O2).
2.5.4. Exploratory Regression Analyses
2.5.5. Focus on Dynamic Adaptation
2.5.6. Software
3. Results
3.1. EEG Activity Is Differentially Modulated Across Frequency Bands
3.2. Correlations Between the EEG–Metabolic Ratios Dynamics and Time-to-Exhaustion, Time to Reach O2max or TLIM at O2max
3.3. Relationships Between EEG PSD Slopes and O2 and CO2 Dynamics During the TLIM Test
3.4. Regression Analyses of EEG–Metabolic Slopes and Endurance Outcomes
- Beta power was negatively correlated with time spent at O2max and positively correlated with both O2 and CO2.
- Alpha power showed a significant positive correlation with Beta power.
- RPE was positively correlated with Beta power.
- The time to reach O2max was positively correlated with Alpha/O2 and Alpha/CO2 ratios, while the time spent at O2max was significantly correlated with Theta/O2 and Theta/CO2 ratios.
- TLIM duration was correlated with Theta/CO2 and Alpha/CO2 ratios.
- The Beta/CO2 ratio was also found to be positively correlated with time to reach O2max.
- Exploratory regression analyses showed that slopes of O2 and CO2 were significantly associated with TLIM duration after Bonferroni correction. No other associations remained significant after correction.
4. Discussion
4.1. EEG Activity Differentially Modulated Across Frequency Bands
4.1.1. Beta Power and Endurance
4.1.2. Alpha Power and Endurance Maintenance
4.1.3. EEG–Metabolic Interactions and Acute Fatigue Regulation
4.2. The Interplay Between Metabolic and Neurophysiological Power During Endurance Exercise
4.2.1. EEG–Metabolic Ratios and Endurance Performance
4.2.2. Beta Oscillations: Neuromuscular Compensation Rather than Metabolic Efficiency
4.2.3. Theta Oscillations: Autonomic Integration and Ventilatory Efficiency
4.2.4. Alpha Oscillations: Balancing Attention, Motor Efficiency, and Metabolic Strain
4.2.5. Perceived Exertion and Its Partial Dissociation from Endurance Regulation
4.2.6. Exploratory Regression Analyses
4.3. Practical Implications
4.4. Study Limitations
4.5. Future Research Directions
- Integrative neurophysiological assessments: Combining EEG with complementary methods such as functional near-infrared spectroscopy, EMG, heart rate variability, or respiratory monitoring may help characterize the dynamic interplay between cortical, muscular, and cardiorespiratory systems during fatigue development.
- Experimental modulation of brain activity: Real-time EEG-based interventions (e.g., neurofeedback, transcranial stimulation) could help determine whether altering specific oscillatory patterns, such as reducing Beta or enhancing Theta, is associated with changes in endurance performance or perceived exertion.
- Individual variability and adaptation: Investigating how factors such as training status, aerobic capacity, cognitive profile, or psychological resilience influence EEG–metabolic responses may inform the development of more personalized approaches for athletes with distinct performance profiles.
- Field-based EEG applications: The design of portable, motion-resistant EEG systems coupled with biofeedback capabilities may eventually allow exploratory monitoring and adjustment of effort pacing in naturalistic endurance environments.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hill, A.V.; Lupton, H. Muscular Exercise, Lactic Acid, and the Supply and Utilization of Oxygen. QJM Int. J. Med. 1923, 16, 135–171. [Google Scholar] [CrossRef]
- Bassett, D.R.; Howley, E.T. Limiting factors for maximum oxygen uptake and determinants of endurance performance. Med. Sci. Sports Exerc. 2000, 32, 70. [Google Scholar] [CrossRef]
- Joyner, M.J.; Coyle, E.F. Endurance exercise performance: The physiology of champions. J. Physiol. 2008, 586, 35–44. [Google Scholar] [CrossRef] [PubMed]
- Noakes, T.D. Testing for maximum oxygen consumption has produced a brainless mode of human exercise performance. Br. J. Sports Med. 2008, 42, 551–555. [Google Scholar] [CrossRef]
- Billat, V.L.; Blondel, N.; Berthoin, S. Determination of the velocity associated with the longest time to exhaustion at maximal oxygen uptake. Eur. J. Appl. Physiol. 1999, 80, 159–161. [Google Scholar] [CrossRef]
- Noakes, T.D. Fatigue is a Brain-Derived Emotion that Regulates the Exercise Behavior to Ensure the Protection of Whole Body Homeostasis. Front. Physiol. 2012, 3, 82. [Google Scholar] [CrossRef] [PubMed]
- Hill, D.W.; Rowell, A.L. Significance of time to exhaustion during exercise at the velocity associated with VO2max. Eur. J. Appl. Physiol. 1996, 72, 383–386. [Google Scholar] [CrossRef]
- Billat, L.V. Interval Training for Performance: A Scientific and Empirical Practice: Special Recommendations for Middle- and Long-Distance Running. Part I: Aerobic Interval Training. Sports Med. 2001, 31, 13–31. [Google Scholar] [CrossRef]
- Billat, L.V. Interval Training for Performance: A Scientific and Empirical Practice: Special Recommendations for Middle- and Long-Distance Running. Part II: Anaerobic Interval Training. Sports Med. 2001, 31, 75–90. [Google Scholar] [CrossRef]
- Lepretre, P.M.; Koralsztein, J.P.; Billat, V.L. Effect of Exercise Intensity on Relationship between VO2max and Cardiac Output. Med. Sci. Sports Exerc. 2004, 36, 1357–1363. [Google Scholar] [CrossRef] [PubMed]
- Murgatroyd, S.R.; Ferguson, C.; Ward, S.A.; Whipp, B.J.; Rossiter, H.B. Pulmonary O2 uptake kinetics as a determinant of high-intensity exercise tolerance in humans. J. Appl. Physiol. 2011, 110, 1598–1606. [Google Scholar] [CrossRef]
- Faina, M.; Billat, V.; Squadrone, R.; Angelis, M.D.; Koralsztein, J.P.; Monte, A.D. Anaerobic contribution to the time to exhaustion at the minimal exercise intensity at which maximal oxygen uptake occurs in elite cyclists, kayakists and swimmers. Eur. J. Appl. Physiol. 1997, 76, 13–20. [Google Scholar] [CrossRef]
- Amann, M.; Calbet, J.A.L. Convective oxygen transport and fatigue. J. Appl. Physiol. 2008, 104, 861–870. [Google Scholar] [CrossRef] [PubMed]
- Marcora, S.M.; Staiano, W.; Manning, V. Mental fatigue impairs physical performance in humans. J. Appl. Physiol. 2009, 106, 857–864. [Google Scholar] [CrossRef]
- Marcora, S.M.; Staiano, W. The limit to exercise tolerance in humans: Mind over muscle? Eur. J. Appl. Physiol. 2010, 109, 763–770, Erratum in Eur. J. Appl. Physiol. 2010, 110, 1305. [Google Scholar] [CrossRef]
- Whipp, J.B.; Ward, A.S. Pulmonary Gas Exchange Dynamics and the Tolerance to Muscular Exercise: Effects of Fitness and Training. Ann. Physiol. Anthropol. 1992, 11, 207–214. [Google Scholar] [CrossRef]
- Whipp, B.J.; Ward, S.A. Determinants and control of breathing during muscular exercise. Br. J. Sports Med. 1998, 32, 199–211. [Google Scholar] [CrossRef]
- Poole, D.C.; Barstow, T.J.; Mcdonough, P.; Jones, A.M. Control of Oxygen Uptake during Exercise. Med. Sci. Sports Exerc. 2008, 40, 462–474. [Google Scholar] [CrossRef]
- Nattie, E. CO2, brainstem chemoreceptors and breathing. Prog. Neurobiol. 1999, 59, 299–331. [Google Scholar] [CrossRef] [PubMed]
- Guyenet, P.G.; Stornetta, R.L.; Bayliss, D.A. Central respiratory chemoreception. J. Comp. Neurol. 2010, 518, 3883–3906. [Google Scholar] [CrossRef] [PubMed]
- Ryan, B.J.; Seeley, A.D.; Pitsas, D.M.; Mayer, T.A.; Caldwell, A.R.; Ceaser, T.G.; Luippold, A.J.; Charkoudian, N.; Salgado, R.M. Influence of graded hypercapnia on endurance exercise performance in healthy humans. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2022, 323, R638–R647. [Google Scholar] [CrossRef]
- Nybo, L.; Rasmussen, P. Inadequate Cerebral Oxygen Delivery and Central Fatigue during Strenuous Exercise. Exerc. Sport. Sci. Rev. 2007, 35, 110–118. [Google Scholar] [CrossRef]
- Noakes, T.D.; St Clair Gibson, A.; Lambert, E.V. From catastrophe to complexity: A novel model of integrative central neural regulation of effort and fatigue during exercise in humans. Br. J. Sports Med. 2004, 38, 511–514. [Google Scholar] [CrossRef]
- St Clair Gibson, A.; Noakes, T.D. Evidence for complex system integration and dynamic neural regulation of skeletal muscle recruitment during exercise in humans. Br. J. Sports Med. 2004, 38, 797–806. [Google Scholar] [CrossRef]
- Amann, M. Central and Peripheral Fatigue: Interaction during Cycling Exercise in Humans. Med. Sci. Sports Exerc. 2011, 43, 2039–2045. [Google Scholar] [CrossRef]
- Kayser, B. Exercise starts and ends in the brain. Eur. J. Appl. Physiol. 2003, 90, 411–419. [Google Scholar] [CrossRef]
- Enders, H.; Cortese, F.; Maurer, C.; Baltich, J.; Protzner, A.B.; Nigg, B.M. Changes in cortical activity measured with EEG during a high-intensity cycling exercise. J. Neurophysiol. 2016, 115, 379–388. [Google Scholar] [CrossRef]
- Cheron, G.; Petit, G.; Cheron, J.; Leroy, A.; Cebolla, A.; Cevallos, C.; Petieau, M.; Hoellinger, T.; Zarka, D.; Clarinval, A.M.; et al. Brain Oscillations in Sport: Toward EEG Biomarkers of Performance. Front. Psychol. 2016, 7, 246. [Google Scholar] [CrossRef] [PubMed]
- Schneider, S.; Rouffet, D.M.; Billaut, F.; Strüder, H.K. Cortical current density oscillations in the motor cortex are correlated with muscular activity during pedaling exercise. Neuroscience 2013, 228, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Engel, A.K.; Fries, P. Beta-band oscillations—Signalling the status quo? Curr. Opin. Neurobiol. 2010, 20, 156–165. [Google Scholar] [CrossRef] [PubMed]
- Kilavik, B.E.; Zaepffel, M.; Brovelli, A.; MacKay, W.A.; Riehle, A. The ups and downs of beta oscillations in sensorimotor cortex. Exp. Neurol. 2013, 245, 15–26. [Google Scholar] [CrossRef]
- Tanaka, M.; Ishii, A.; Watanabe, Y. Neural Correlates of Central Inhibition during Physical Fatigue. PLoS ONE 2013, 8, e70949. [Google Scholar] [CrossRef] [PubMed]
- Cavanagh, J.F.; Frank, M.J. Frontal theta as a mechanism for cognitive control. Trends Cogn. Sci. 2014, 18, 414–421. [Google Scholar] [CrossRef] [PubMed]
- Womelsdorf, T.; Vinck, M.; Leung, L.S.; Everling, S. Selective Theta-Synchronization of Choice-Relevant Information Subserves Goal-Directed Behavior. Front. Hum. Neurosci. 2010, 4, 210. [Google Scholar] [CrossRef] [PubMed]
- Del Percio, C.; Babiloni, C.; Marzano, N.; Iacoboni, M.; Infarinato, F.; Vecchio, F.; Lizio, R.; Aschieri, P.; Fiore, A.; Toràn, G.; et al. “Neural efficiency” of athletes’ brain for upright standing: A high-resolution EEG study. Brain Res. Bull. 2009, 79, 193–200. [Google Scholar] [CrossRef]
- Klimesch, W. EEG alpha and theta oscillations reflect cognitive and memory performance: A review and analysis. Brain Res. Rev. 1999, 29, 169–195. [Google Scholar] [CrossRef]
- Del Percio, C.; Marzano, N.; Tilgher, S.; Fiore, A.; Di Ciolo, E.; Aschieri, P.; Lino, A.; Toràn, G.; Babiloni, C.; Eusebi, F. Pre-stimulus alpha rhythms are correlated with post-stimulus sensorimotor performance in athletes and non-athletes: A high-resolution EEG study. Clin. Neurophysiol. 2007, 118, 1711–1720. [Google Scholar] [CrossRef]
- Ludyga, S.; Gronwald, T.; Hottenrott, K. Effects of high vs. low cadence training on cyclists’ brain cortical activity during exercise. J. Sci. Med. Sport 2016, 19, 342–347. [Google Scholar] [CrossRef]
- Bailey, S.P.; Hall, E.E.; Folger, S.E.; Miller, P.C. Changes in EEG during graded exercise on a recumbent cycle ergometer. J. Sports Sci. Med. 2008, 7, 505–511. [Google Scholar]
- Brümmer, V.; Schneider, S.; Strüder, H.K.; Askew, C.D. Primary motor cortex activity is elevated with incremental exercise intensity. Neuroscience 2011, 181, 150–162. [Google Scholar] [CrossRef]
- Gwin, J.T.; Ferris, D.P. Beta- and gamma-range human lower limb corticomuscular coherence. Front. Hum. Neurosci. 2012, 6, 258. [Google Scholar] [CrossRef]
- Bigliassi, M.; Filho, E. Functional significance of the dorsolateral prefrontal cortex during exhaustive exercise. Biol. Psychol. 2022, 175, 108442. [Google Scholar] [CrossRef]
- Billat, V.; Berthomier, C.; Clémençon, M.; Brandewinder, M.; Essid, S.; Damon, C.; Rigaud, F.; Bénichoux, A.; Maby, E.; Fornoni, L.; et al. Electroencephalography Response during an Incremental Test According to the VO2max Plateau Incidence. Appl. Sci. 2024, 14, 5411. [Google Scholar] [CrossRef]
- Bentley, D.J.; Newell, J.; Bishop, D. Incremental Exercise Test Design and Analysis: Implications for Performance Diagnostics in Endurance Athletes. Sports Med. 2007, 37, 575–586. [Google Scholar] [CrossRef]
- Borg, G.A.V. Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Niemeyer, M.; Knaier, R.; Beneke, R. The Oxygen Uptake Plateau—A Critical Review of the Frequently Misunderstood Phenomenon. Sports Med. 2021, 51, 1815–1834. [Google Scholar] [CrossRef]
- Poole, D.C.; Wilkerson, D.P.; Jones, A.M. Validity of criteria for establishing maximal O2 uptake during ramp exercise tests. Eur. J. Appl. Physiol. 2008, 102, 403–410. [Google Scholar] [CrossRef] [PubMed]
- Poole, D.C.; Jones, A.M. Measurement of the maximum oxygen uptake VO2max: VO2peak is no longer acceptable. J. Appl. Physiol. 2017, 122, 997–1002. [Google Scholar] [CrossRef]
- Midgley, A.; McNaughton, L.; Carroll, S. Time at VO2max during Intermittent Treadmill Running: Test Protocol Dependent or Methodological Artefact? Int. J. Sports Med. 2007, 28, 934–939. [Google Scholar] [CrossRef]
- Hill, D.W.; Glass, L.W.; Vingren, J.L. Critical Speed, Thresholds for VO2max and Boundaries of the Severe Exercise Intensity Domain. Rev. Bras. Med. Esporte 2024, 30, e2021_0311. [Google Scholar] [CrossRef]
- Damon, C.; Liutkus, A.; Gramfort, A.; Essid, S. Non-negative Tensor Factorization for single-channel EEG artifact rejection. In Proceedings of the 2013 IEEE International Workshop on Machine Learning for Signal Processing (MLSP), Southampton, UK, 22–25 September 2013; IEEE: New York, NY, USA, 2013; pp. 1–6. [Google Scholar] [CrossRef]
- Lee, H.; Kim, Y.D.; Cichocki, A.; Choi, S. Nonnegative Tensor Factorization for Continuous EEG Classification. Int. J. Neural Syst. 2007, 17, 305–317. [Google Scholar] [CrossRef]
- Damon, C.; Liutkus, A.; Gramfort, A.; Essid, S. Non-negative matrix factorization for single-channel EEG artifact rejection. In Proceedings of the 2013 IEEE International Conference on Acoustics, Speech and Signal Processing, Vancouver, BC, Canada, 26–31 May 2013; IEEE: New York, NY, USA, 2013; pp. 1177–1181. [Google Scholar] [CrossRef]
- Lins, O.G.; Picton, T.W.; Berg, P.; Scherg, M. Ocular artifacts in EEG and event-related potentials I: Scalp topography. Brain Topogr. 1993, 6, 51–63. [Google Scholar] [CrossRef] [PubMed]
- De Clercq, W.; Vergult, A.; Vanrumste, B.; Van Paesschen, W.; Van Huffel, S. Canonical Correlation Analysis Applied to Remove Muscle Artifacts From the Electroencephalogram. IEEE Trans. Biomed. Eng. 2006, 53, 2583–2587. [Google Scholar] [CrossRef] [PubMed]
- Liutkus, A.; Badeau, R.; Richard, G. Gaussian Processes for Underdetermined Source Separation. IEEE Trans. Signal Process 2011, 59, 3155–3167. [Google Scholar] [CrossRef]
- Peng, H.; Wang, S.; Wang, X. Consistency and asymptotic distribution of the Theil–Sen estimator. J. Stat. Plan. Inference 2008, 138, 1836–1850. [Google Scholar] [CrossRef]
- Wilcox, R.R. A Heteroscedastic Method for Comparing Regression Lines at Specified Design Points When Using a Robust Regression Estimator. J. Data Sci. 2021, 11, 281–291. [Google Scholar] [CrossRef]
- Londeree, B.R.; Moeschberger, M.L. Effect of Age and Other Factors on Maximal Heart Rate. Res. Q. Exerc. Sport 1982, 53, 297–304. [Google Scholar] [CrossRef]
- Poinsard, L.; Palacin, F.; Hashemi, I.S.; Billat, V. Neural and Cardio-Respiratory Responses During Maximal Self-Paced and Controlled-Intensity Protocols at Similar Perceived Exertion Levels: A Pilot Study. Appl. Sci. 2024, 14, 10551. [Google Scholar] [CrossRef]
- Matta, P.M.; Baurès, R.; Duclay, J.; Alamia, A. Modulation of beta oscillatory dynamics in motor and frontal areas during physical fatigue. Commun. Biol. 2025, 8, 687. [Google Scholar] [CrossRef]
- Hosang, L.; Mouchlianitis, E.; Guérin, S.M.R.; Karageorghis, C.I. Effects of exercise on electroencephalography-recorded neural oscillations: A systematic review. Int. Rev. Sport Exerc. Psychol. 2024, 17, 926–979. [Google Scholar] [CrossRef]
- Chung, J.W.; Ofori, E.; Misra, G.; Hess, C.W.; Vaillancourt, D.E. Beta-band activity and connectivity in sensorimotor and parietal cortex are important for accurate motor performance. NeuroImage 2017, 144, 164–173. [Google Scholar] [CrossRef]
- Mechau, D.; Mücke, S.; Liesen, H.; Weiss, M. Effect of increasing running velocity on electroencephalogram in a field test. Eur. J. Appl. Physiol. 1998, 78, 340–345. [Google Scholar] [CrossRef]
- St Clair Gibson, A.; Lambert, M.I.; Noakes, T.D. Neural Control of Force Output During Maximal and Submaximal Exercise. Sports Med. 2001, 31, 637–650. [Google Scholar] [CrossRef]
- Pires, F.O.; Dos Anjos, C.A.; Covolan, R.J.; Pinheiro, F.A.; St Clair Gibson, A.; Noakes, T.D.; Magalhães, F.H.; Ugrinowitsch, C. Cerebral Regulation in Different Maximal Aerobic Exercise Modes. Front. Physiol. 2016, 7, 253. [Google Scholar] [CrossRef]
- Blondel, N.; Berthoin, S.; Billat, V.; Lensel, G. Relationship Between Run Times to Exhaustion at 90, 100, 120, and 140% of vVO2max and Velocity Expressed Relatively to Critical Velocity and Maximal Velocity. Int. J. Sports Med. 2001, 22, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Poole, D.C.; Burnley, M.; Vanhatalo, A.; Rossiter, H.B.; Jones, A.M. Critical Power: An Important Fatigue Threshold in Exercise Physiology. Med. Sci. Sports Exerc. 2016, 48, 2320–2334. [Google Scholar] [CrossRef] [PubMed]
- Pfurtscheller, G.; Lopes Da Silva, F.H. Event-related EEG/MEG synchronization and desynchronization: Basic principles. Clin. Neurophysiol. 1999, 110, 1842–1857. [Google Scholar] [CrossRef]
- Klimesch, W. Alpha-band oscillations, attention, and controlled access to stored information. Trends Cogn. Sci. 2012, 16, 606–617. [Google Scholar] [CrossRef] [PubMed]
- Haegens, S.; Händel, B.F.; Jensen, O. Top-Down Controlled Alpha Band Activity in Somatosensory Areas Determines Behavioral Performance in a Discrimination Task. J. Neurosci. 2011, 31, 5197–5204. [Google Scholar] [CrossRef]
- Craig, A.D. How do you feel—Now? The anterior insula and human awareness. Nat. Rev. Neurosci. 2009, 10, 59–70. [Google Scholar] [CrossRef]
- Nybo, L.; Secher, N.H. Cerebral perturbations provoked by prolonged exercise. Prog. Neurobiol. 2004, 72, 223–261. [Google Scholar] [CrossRef] [PubMed]
- Billaut, F.; Buchheit, M. Repeated-sprint performance and vastus lateralis oxygenation: Effect of limited O2 availability. Scand. Med. Sci. Sports 2013, 23, e185–e193. [Google Scholar] [CrossRef] [PubMed]
- De Wachter, J.; Proost, M.; Habay, J.; Verstraelen, M.; Diaz-Garcia, J.; Hurst, P.; Meeusen, R.; Van Cutsem, J.; Roelands, B. Prefrontal Cortex Oxygenation During Endurance Performance: A Systematic Review of Functional Near-Infrared Spectroscopy Studies. Front. Physiol. 2021, 12, 761232. [Google Scholar] [CrossRef] [PubMed]
- Beaver, W.L.; Wasserman, K.; Whipp, B.J. A new method for detecting anaerobic threshold by gas exchange. J. Appl. Physiol. 1986, 60, 2020–2027. [Google Scholar] [CrossRef]
- Wasserman, K.; Whipp, B.J.; Koyl, S.N.; Beaver, W.L. Anaerobic threshold and respiratory gas exchange during exercise. J. Appl. Physiol. 1973, 35, 236–243. [Google Scholar] [CrossRef]
- Marcora, S. Perception of effort during exercise is independent of afferent feedback from skeletal muscles, heart, and lungs. J. Appl. Physiol. 2009, 106, 2060–2062. [Google Scholar] [CrossRef]
- Pageaux, B.; Marcora, S.M.; Lepers, R. Prolonged Mental Exertion Does Not Alter Neuromuscular Function of the Knee Extensors. Med. Sci. Sports Exerc. 2013, 45, 2254–2264. [Google Scholar] [CrossRef]
- De Morree, H.M.; Klein, C.; Marcora, S.M. Perception of effort reflects central motor command during movement execution. Psychophysiology 2012, 49, 1242–1253. [Google Scholar] [CrossRef]
- Mehta, R.K.; Parasuraman, R. Neuroergonomics: A review of applications to physical and cognitive work. Front. Hum. Neurosci. 2013, 7, 889. [Google Scholar] [CrossRef]
- Grossman, P.; Niemann, L.; Schmidt, S.; Walach, H. Mindfulness-based stress reduction and health benefits. J. Psychosom. Res. 2004, 57, 35–43. [Google Scholar] [CrossRef]
- Mrazek, M.D.; Franklin, M.S.; Phillips, D.T.; Baird, B.; Schooler, J.W. Mindfulness Training Improves Working Memory Capacity and GRE Performance While Reducing Mind Wandering. Psychol. Sci. 2013, 24, 776–781. [Google Scholar] [CrossRef]
- Casson, A.J. Wearable EEG and beyond. Biomed. Eng. Lett. 2019, 9, 53–71. [Google Scholar] [CrossRef]
- Giangrande, A.; Botter, A.; Piitulainen, H.; Cerone, G.L. Motion Artifacts in Dynamic EEG Recordings: Experimental Observations, Electrical Modelling, and Design Considerations. Sensors 2024, 24, 6363. [Google Scholar] [CrossRef]
- Seok, D.; Lee, S.; Kim, M.; Cho, J.; Kim, C. Motion Artifact Removal Techniques for Wearable EEG and PPG Sensor Systems. Front. Electron. 2021, 2, 685513. [Google Scholar] [CrossRef]
- Garcin, M.; Billat, V. Perceived Exertion Scales Attest to Both Intensity and Exercise Duration. Percept. Mot. Ski. 2001, 93, 661–671. [Google Scholar] [CrossRef] [PubMed]
- Garcin, M.; Mille-Hamard, L.; Billat, V. Influence of Aerobic Fitness Level on Measured and Estimated Perceived Exertion During Exhausting Runs. Int. J. Sports Med. 2004, 25, 270–277. [Google Scholar] [CrossRef]
- Abbiss, C.R.; Laursen, P.B. Describing and Understanding Pacing Strategies during Athletic Competition. Sports Med. 2008, 38, 239–252. [Google Scholar] [CrossRef]
- Foster, C.; Florhaug, J.A.; Franklin, J.; Gottschall, L.; Hrovatin, L.A.; Parker, S.; Doleshal, P.; Dodge, C. A New Approach to Monitoring Exercise Training. J. Strength. Cond. Res. 2001, 15, 109–115. [Google Scholar] [CrossRef]
- Eston, R. Use of Ratings of Perceived Exertion in Sports. Int. J. Sports Physiol. Perform. 2012, 7, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Gramann, K.; Gwin, J.T.; Bigdely-Shamlo, N.; Ferris, D.P.; Makeig, S. Visual Evoked Responses During Standing and Walking. Front. Hum. Neurosci. 2010, 4, 202. [Google Scholar] [CrossRef]
- Kilicarslan, A.; Contreras Vidal, J.L. Characterization and real-time removal of motion artifacts from EEG signals. J. Neural Eng. 2019, 16, 056027. [Google Scholar] [CrossRef] [PubMed]
- De Vos, M.; Debener, S. Mobile EEG: Towards brain activity monitoring during natural action and cognition. Int. J. Psychophysiol. 2014, 91, 1–2. [Google Scholar] [CrossRef] [PubMed]


| Subjects (n = 30) | Mean | SD | Min | Max |
|---|---|---|---|---|
| Age (years) | 25.4 | 4.5 | 18.0 | 35.0 |
| Height (cm) | 180.4 | 6.3 | 170.0 | 193.0 |
| Weight (kg) | 73.5 | 9.6 | 59.0 | 102.0 |
| Body Mass Index (kg/m2) | 22.5 | 1.9 | 18.4 | 27.4 |
| Training per week (hour) | 8.3 | 5.3 | 3.0 | 25.0 |
| O2max (mL·kg−1·min−1) | 58.3 | 7.5 | 44.0 | 75.0 |
| Subjects (n = 30) | Mean | SD | Min | Max |
|---|---|---|---|---|
| O2max (mL·kg−1·min−1) | 58.3 | 7.5 | 44.0 | 75.0 |
| Absolute MAP (W) | 308.0 | 38.5 | 240.0 | 420.0 |
| Relative MAP (W/kg) | 4.2 | 0.7 | 2.6 | 5.6 |
| HRmax (beats·min−1) | 186.4 | 8.2 | 171 | 200 |
| %HRmax | 95.9 | 5.3 | 82.4 | 105.3 |
| RER | 1.2 | 0.1 | 1.1 | 1.3 |
| Variable | Mean | SD | Min | Max |
|---|---|---|---|---|
| Time to exhaustion (s) | 732.4 | 319.8 | 217.0 | 1600.0 |
| Time to reach O2max (s) | 290.5 | 179.6 | 75.0 | 917.0 |
| Time spent at O2max (s) | 441.9 | 258.9 | 96.0 | 1257.0 |
| RER | 1.1 | 0.1 | 1.0 | 1.3 |
| RPE | 17.4 | 1.4 | 15.0 | 20.0 |
| Variable | Theta | Alpha | Beta | TLIM Duration | Time to Reach O2max | Time Spent at O2max |
|---|---|---|---|---|---|---|
| Theta | 1 | 0.460 (p = 0.011) [0.101, 0.714] | 0.270 (p = 0.148) [−0.106, 0.579] | −0.051 (p = 0.787) [−0.404, 0.315] | 0.032 (p = 0.867) [−0.332, 0.388] | −0.123 (p = 0.516) [−0.464, 0.250] |
| Alpha | 0.460 (p = 0.011) [0.101, 0.714] | 1 | 0.569 (p = 0.001) * [0.235, 0.783] | −0.176 (p = 0.352) [−0.506, 0.200] | 0.281 (p = 0.132) [−0.095, 0.587] | −0.498 (p = 0.006) [−0.738, −0.146] |
| Beta | 0.270 (p = 0.148) [−0.106, 0.579] | 0.569 (p = 0.001) * [0.235, 0.783] | 1 | −0.385 (p = 0.036) [−0.662, −0.015] | 0.001 (p = 0.996) [−0.359, 0.361] | −0.542 (p = 0.002) * [−0.766, −0.201] |
| Alpha/beta | 0.239 (p = 0.203) [−0.138, 0.555] | 0.441 (p = 0.015) [0.078, 0.701] | −0.253 (p = 0.177) [−0.566, 0.124] | 0.220 (p = 0.243) [−0.157, 0.541] | 0.410 (p = 0.025) [0.043, 0.680] | 0.043 (p = 0.821) [−0.322, 0.397] |
| RPE | −0.055 (p = 0.774) [−0.407, 0.312] | 0.314 (p = 0.091) [−0.061, 0.612] | 0.559 (p = 0.002) * [0.222, 0.777] | −0.073 (p = 0.700) [−0.423, 0.295] | 0.262 (p = 0.161) [−0.114, 0.573] | −0.208 (p = 0.270) [−0.531, 0.169] |
| Variable | TLIM Duration | Time to Reach O2max | Time Spent at O2max | RPE |
|---|---|---|---|---|
| Theta/O2 | 0.488 (p = 0.007) [0.134, 0.732] | 0.159 (p = 0.401) [−0.216, 0.493] | 0.561 (p = 0.002) * [0.224, 0.778] | −0.155 (p = 0.411) [−0.490, 0.219] |
| Alpha/O2 | 0.527 (p = 0.003) [0.182, 0.757] | 0.666 (p < 0.001) * [0.368, 0.840] | 0.254 (p = 0.175) [−0.123, 0.567] | −0.095 (p = 0.616) [−0.441, 0.275] |
| Beta/O2 | 0.063 (p = 0.741) [−0.305, 0.414] | 0.151 (p = 0.424) [−0.223, 0.487] | −0.119 (p = 0.528) [−0.461, 0.253] | 0.444 (p = 0.015) [0.081, 0.702] |
| Theta/CO2 | 0.607 (p < 0.001) * [0.285, 0.805] | 0.277 (p = 0.138) [−0.099, 0.584] | 0.635 (p < 0.001) * [0.324, 0.822] | −0.123 (p = 0.515) [−0.464, 0.249] |
| Alpha/CO2 | 0.611 (p < 0.001) * [0.290, 0.808] | 0.722 (p < 0.001) * [0.453, 0.871] | 0.318 (p = 0.087) [−0.057, 0.615] | −0.048 (p = 0.800) [−0.402, 0.318] |
| Beta/CO2 | 0.506 (p = 0.005) [0.156, 0.744] | 0.557 (p = 0.002) * [0.219, 0.775] | 0.275 (p = 0.141) [−0.101, 0.583] | 0.289 (p = 0.122) [−0.088, 0.593] |
| Variables | O2 | CO2 |
|---|---|---|
| Theta | 0.339 (p = 0.067) [−0.035, 0.630] | 0.273 (p = 0.144) [−0.103, 0.582] |
| Alpha | 0.512 (p = 0.004) [0.163, 0.747] | 0.385 (p = 0.037) [0.015, 0.662] |
| Beta | 0.677 (p < 0.001) * [0.384, 0.846] | 0.557 (p = 0.002) * [0.219, 0.775] |
| Alpha/beta | −0.027 (p = 0.888) [−0.384, 0.337] | −0.076 (p = 0.688) [−0.425, 0.292] |
| Theta/O2 | −0.413 (p = 0.024) [−0.681, −0.046] | −0.362 (p = 0.05) [−0.646, 0.010] |
| Alpha/O2 | −0.208 (p = 0.269) [−0.532, 0.169] | −0.268 (p = 0.152) [−0.577, 0.109] |
| Beta/O2 | 0.124 (p = 0.511) [−0.248, 0.465] | 0.078 (p = 0.681) [−0.291, 0.427] |
| Theta/CO2 | −0.435 (p = 0.017) [−0.697, −0.071] | −0.471 (p = 0.009) [−0.720, −0.113] |
| Alpha/CO2 | −0.217 (p = 0.248) [−0.538, 0.160] | −0.343 (p = 0.064) [−0.632, 0.031] |
| Beta/CO2 | −0.222 (p = 0.238) [−0.542, 0.155] | −0.368 (p = 0.046) [−0.650, 0.004] |
| RPE | 0.372 (p = 0.044) [0.001, 0.653] | 0.246 (p = 0.189) [−0.131, 0.561] |
| Predictor | TLIM Duration (β (SE), R2) | p-Value | Time to Reach O2max (β (SE), R2) | p-Value | Time Spent at O2max (β (SE), R2) | p-Value |
|---|---|---|---|---|---|---|
| Theta | −0.039 (0.189), 0.005 | 0.837 | 0.107 (0.188), 0.011 | 0.575 | −0.122 (0.188), 0.015 | 0.520 |
| Alpha | −0.107 (0.188), 0.011 | 0.573 | 0.289 (0.181), 0.084 | 0.121 | −0.333 (0.178), 0.111 | 0.072 |
| Beta | −0.349 (0.177), 0.122 | 0.058 | −0.092 (0.188), 0.008 | 0.631 | −0.368 (0.176), 0.135 | 0.045 |
| Theta/O2 | 0.350 (0.177), 0.123 | 0.058 | 0.225 (0.184), 0.051 | 0.232 | 0.277 (0.182), 0.076 | 0.139 |
| Alpha/O2 | 0.363 (0.176), 0.132 | 0.049 | 0.472 (0.167), 0.222 | 0.009 | 0.121 (0.188), 0.015 | 0.525 |
| Beta/O2 | −0.037 (0.189), 0.001 | 0.847 | 0.125 (0.187), 0.016 | 0.510 | −0.132 (0.187), 0.017 | 0.486 |
| Theta/CO2 | 0.444 (0.169), 0.198 | 0.014 | 0.269 (0.182), 0.072 | 0.151 | 0.362 (0.176), 0.131 | 0.049 |
| Alpha/CO2 | 0.401 (0.173), 0.161 | 0.028 | 0.449 (0.169), 0.202 | 0.013 | 0.183 (0.186), 0.033 | 0.333 |
| Beta/CO2 | 0.451 (0.169), 0.203 | 0.012 | 0.371 (0.176), 0.137 | 0.044 | 0.299 (0.180), 0.089 | 0.108 |
| O2 | −0.546 (0.158), 0.298 | 0.002 * | −0.243 (0.183), 0.059 | 0.195 | −0.505 (0.163), 0.255 | 0.004 |
| CO2 | −0.556 (0.157), 0.309 | 0.001 * | −0.303 (0.180), 0.092 | 0.104 | −0.477 (0.166), 0.227 | 0.008 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Poinsard, L.; Berthomier, C.; Clémençon, M.; Brandewinder, M.; Essid, S.; Damon, C.; Rigaud, F.; Bénichoux, A.; Maby, E.; Fornoni, L.;
et al. EEG–Metabolic Coupling and Time Limit at
Poinsard L, Berthomier C, Clémençon M, Brandewinder M, Essid S, Damon C, Rigaud F, Bénichoux A, Maby E, Fornoni L,
et al. EEG–Metabolic Coupling and Time Limit at
Poinsard, Luc, Christian Berthomier, Michel Clémençon, Marie Brandewinder, Slim Essid, Cécilia Damon, François Rigaud, Alexis Bénichoux, Emmanuel Maby, Lesly Fornoni,
and et al. 2025. "EEG–Metabolic Coupling and Time Limit at
Poinsard, L., Berthomier, C., Clémençon, M., Brandewinder, M., Essid, S., Damon, C., Rigaud, F., Bénichoux, A., Maby, E., Fornoni, L., Bouchet, P., Beers, P. V., Massot, B., Revol, P., Creveaux, T., Collet, C., Mattout, J., Pialoux, V., & Billat, V.
(2025). EEG–Metabolic Coupling and Time Limit at








