1. Introduction
In March 2020, the World Health Organization (WHO) [
1] declared a state of global pandemic derived from COVID-19 disease. In the United States of America, there was an increase from 300 to 1.5 million cases of the contagion in a period of 2 months, while the number of deaths increased from 8000 to 100,000 in the same period [
2]. This situation, as in many countries, was caused by the rapid spread of the virus through people and in crowded places where there was no social distancing. In North American countries, during March 2020, cases of infection and deaths caused by the SARS-CoV-2 virus were reported, where the general probability of survival was 87.7% from day 24 of infection [
3]. Over time, it was observed that the mortality rate increased in the elderly and was associated with deaths from pneumopathies and neurological and cardiovascular deaths. This situation subsequently occurred in several countries and in other continents where the spread of the COVID-19 disease existed.
In Mexico, the number of infected cases of COVID-19 in May 2020 was 23,471, which increased to approximately 200,000 a month later [
4]. The increase in deaths and infections was mainly due to the accelerated reopening of the economy and the limited control in the restrictions of confinement and social distancing. The total number of confirmed deaths from COVID-19 was 221,200 from January 2020 to May 2021, and the total number of confirmed cases of the contagion was 2,576,029 during the same period, which represents approximately 2% of the total country population [
5].
Worldwide, there were 167,011,807 confirmed cases of the contagion and 3,472,068 deaths associated with COVID-19 until May 2021 according to data published on the official website of the World Health Organization (WHO) [
1], and the North American continent is ranked first as the region with the highest number of infections and deaths. As a result, the WHO has issued several recommendations to continue mitigating the rapid spread of COVID-19, mainly in developing countries. Some of the recommendations focus on the use of face masks or respirators, as well as promoting social distancing in public spaces.
Currently, there are several studies where it is highlighted that the main transmission of COVID-19 is carried out among people who do not present any symptoms. In addition, the main means of contagion in these cases is through contact with dirty or contaminated hands and surfaces [
6]. On the other hand, it has been shown that the SARS-CoV-2 virus remains active up to 1 h after its volatilization after a respiratory event, such as coughing or sneezing, a situation that does not occur with other viruses [
7]. In the last decade, there has been an increase in the studies and research on the behavior of airborne dispersal and contagion of viral and bacterial diseases among humans, such as influenza virus subtype AH1N1 and the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which generates the disease known as COVID-19.
The transmission of diseases between humans is caused mainly through respiratory events, such as talking, eating, coughing, and sneezing [
8,
9,
10]. Consequently, several studies have analyzed the dispersion and transport of particles to establish critical scenarios where it is necessary to maintain a minimum distance between people to avoid the spread of diseases; this concept has been called social distance [
11]. In addition, confined public spaces with adequate ventilation play a very important role in reducing the risk of infection. As a result, several studies have focused on analyzing the relationship and interaction between social distance, ventilation rate, and the probability of infection [
12].
Two of the main respiratory events that cause a greater risk of contagion through air transportation are coughing and sneezing. These events are considered violent and usually occur when an individual has a viral or bacterial disease. Coughing and sneezing generate the expulsion of particles with diameters <5–10 microns in the form of a cloud with an average exhalation velocity of 11.2 m/s and with falling velocities of the particles <3 mm/s [
8,
10].
Exhalation respiratory events, such as sneezing and coughing, have flow velocities of up to 50 m/s and 10 m/s, respectively, with particles of 60 and 100 microns in diameter expelled in these events travelling a distance up to 1–2 m before falling to the ground or evaporating [
13]. Therefore, several studies have been carried out with the purpose of examining the distribution of ventilation and protection systems in public spaces, such as hospitals, to control airborne particles and minimize the dispersion of particles related to diseases that could be transmitted [
9].
Based on the events that emerged in December 2019 around the contagion of the COVID-19 disease, the global need to use facial masks (made by different layer mallets or homemade clothes) or cone-shaped respirators (filtering facepiece respirators-FFR) with quality control that guarantees a retention of at least 95% of particles up to 0.3 microns (N95—United States NIOSH-42CFR84; FFP2—Europe EN 149-2001; KN95—China GB2626-2006) emerged to mitigate the spread of the virus between people. In this regard, Beesoon et al. [
14] present a discussion about the effectiveness of masks, especially those made of textile materials. In their research, the authors highlight the ideal characteristics that a mask should have to guarantee the protection of the user. Among the main characteristics are: (a) a good filtering capacity for inhalation and exhalation events; (b) low resistance to respiration and gas exchange efficiency; (c) washable or reusable; and, finally, (d) comfortable use.
Other studies that analyze the effect of wind in open spaces also suggest the use of face masks to prevent and reduce the risk of contagion by the possible presence of airborne pathogens. This condition has generated a greater number of respiratory diseases, so it is desirable to use comfortable, safe, and efficient masks with good air exchange and the effective filtration of particles. Thus, the use of masks can be a feasible alternative to mitigate the rapid contagion and transmission of diseases between individuals [
15]. Xi et al. [
16] studied the effects of wearing a surgical mask for inhalation events to evaluate the filtration and trajectories of virus-laden particles over the mask and respiratory tract. They found that masks can reduce the 10 microns particle penetration into the lungs regardless of the filtration efficiency of the mask. Another example is mentioned by Leonard et al. [
17] where they found that the dispersion of characterized particles in a therapy room can be prevented using surgical masks with the presence of low velocities at the outlets of the mask. In fact, some research [
18] recently found that suspended particulate matter with a diameter <2.5 microns (PM2.5), diameter <10 microns (PM10), as well as certain CO levels and temperatures are four variables that could potentially promote the sustained transmission of COVID-19 in their study in Mexico City in a situation designed for not wearing a mask for protection. On the other hand, López-Feldman et al. [
19] found evidence of a positive relationship between air pollution by PM2.5 and the probability that an individual will die after contracting COVID-19 in their case study developed in the city of Victoria, Mexico.
According to Asadi et al. [
6] and Morawaska et al. [
20], in a face-to-face conversation between a pair of individuals, there is an expulsion of particles with diameters between 0.8 and 2 microns for respiration events, while, when talking, there are particles up to 7 microns dispersed by the individuals. By using facial device protection, such as face masks or respirators, it is likely to reduce the risk of disease transmission even when there is no social distance between people. Pendar and Páscoa [
21] suggest a minimum of 4 m of social distance derived from their analysis of the length and width of the exhalated droplets from events of coughs and sneezes and found that the trajectories of the particles are influenced by their size, angle, velocity, and environment. Therefore, masks and their protective properties should facilitate health care and the reduction of pathogen dispersion to promote their use in situations of health contingencies where social distancing is required [
22].
Based on a recent literature review, there are studies that have analyzed the efficiency of particle filtration in conventional masks and their comparison with surgical masks with N95 standards, particularly for protection against the disease generated by the SARS-CoV-2 [
14]. It was found that masks made of cotton with a vacuum cleaning bag section or including a piece of wet towel (baby wipe) have a viral filtration efficiency of 99.5% [
23]. Masks made with other fabrics have an efficiency of lower than 50% [
24]. Dbouk and Drikakis [
25] applied a new criterion to evaluate the efficiency of a face mask’s performance considering the penetration dynamics of airborne droplet transmission and the leakage around the mask edges and one of their main conclusions is that wearing a commercial mask does not provide complete protection and it is necessary to maintain social distance. Thus, it is possible to improve the performance of the filter zones of a fabric mask only by incorporating layers of materials of daily use or enhancing the mask geometry and design.
On the other hand, few studies focus on an aerodynamic and comfortable design of masks. Currently, the problem around the discomfort generated by the continuous use of masks is mainly by users of the health sector, or even all those who have close contact with other people, such as waiters, taxi drivers, salesmen, among others, and otherwise those who use the masks for a prolonged and continuous time during the day. In addition, it is worth mentioning that users with respiratory problems do not use masks due to the sensation of suffocation, headache, shortness of breath, and dizziness caused by the inadequate exchange of exhalation and inhalation flows [
26].
Recent studies have focused on the analysis of the performance of facial masks and have found that there are some deficiencies with respect to the geometric design, as well as in the seal with the face. Indeed, Siddhartha et al. [
27] experimentally analyzed the flow through homemade fabric masks with optical techniques and their comparison with cone-type masks (KN95) for coughing and sneezing events. Among their main findings, they identified the presence of several leakage zones in all the mask models analyzed. These areas of leakage occurred mainly in the upper area of the nose because there was no airtight seal of the mask with the face. Although the use of masks reduces the dispersion of the exhaled air cloud, their poor design promotes a feeling of discomfort in the wearer, generates fogging of the lenses when they are worn, and represents false protection for the wearer’s health.
Siddhartha et al. [
28] also performed an analysis of the dispersion of exhalation flows using optical techniques. They compared the performance of various types of masks and respirators with an exhalation valve, as well as a comparison with a face shield. In their work, they emphasize that, with the use of facial protection, the dispersion of exhaled air is reduced; however, this is not generated effectively when there is a dispersion of the air that travels great distances around the mask and the mask with valves. In their work, they suggested improving the design of a mask that can reduce the flow and dispersion of exhaled air in the environment.
As described in Martinez-Perez et al. [
29], the existence of non-sealed areas between the mask and the face can generate health problems, such as dry eyes. It was found that most people presented symptoms of visual diseases caused by the continuous mask usage. Furthermore, people change contact lenses more frequently compared with before the pandemic and the need of wearing a mask. In this context, the mask has been accepted with more difficulty by the users because of such symptoms related to the deficient seal and design of a mask.
Other studies have used techniques such as computational fluid dynamics (CFD) in the simulation of the operation of conventional cone-type FFR masks (KN95 respirator) to verify that their use can avoid the dispersion of particles associated with the SARS-CoV-2 in closed environments. The particles exhaled when coughing can travel up to a distance of 2.6 m, and this distance can be reduced to 0.48 m and 0.73 m with the use of surgical or conventional masks according to the information reported in Khosronjejad et al. [
30]. However, in studies where it is possible to reduce the dispersion of particles, the correct functioning of the mask is not guaranteed because it does not have an airtight seal or an adequate exchange of flows in the events of inhalation and exhalation to offer greater comfort to the user.
Cornejo et al. [
31] made a CFD simulation considering the effect of the turbulent flow in the aerodynamic dispersion of droplets and aerosol coming from people during respiratory events. They found a significant droplets transport effect considering the action of the turbulent airflow. Particles up to 900 microns can be spread up to 5 m, and particles up to 200 microns can be dispersed at distances up to 18 m by the action of the airflow and turbulence. It is important to consider the wind velocity in the spread of droplets out of the mask to mitigate the propagation of the particles at longer distances.
Lei et al. [
26] analyzed the flows through an FFR N95 mask using computational fluid dynamics (CFD) and optical techniques with an infrared camera (IRC). In particular, they studied the presence of different leaking gaps, highlighting that the area with the greatest leakage flow is found over the nose and eyes, followed by the cheeks. In addition, with the analysis of temperature variability, they detected that there is an increase in heat in the area near the mouth and lips, relating it to thermal discomfort for the user. In their research, the use of CFD is highlighted as an alternative for the study of fluids at a low cost and with results that allow improving the design of this type of mask.
The presence of gaps between the face and the mask reduces the volume of filtered air in the inhalation and exhalation events. This situation causes a greater dispersion of unfiltered air that favors the danger of infection between individuals. Peric and Peric [
32] conducted an investigation using numerical simulation to evaluate the design and flow inside a mask used as protection against COVID-19. They analyzed the exhalation and inhalation flow with air flow rates of up to 3095 L/min considering gaps with different geometric shapes and in different areas of the face (on the nose, close to the eyes). They found that, for gaps with openings of 0.4–1 mm, 30–70% of the total flow comes out through the gaps and, in some cases, up to 80% for FFP-2 masks. Derived from this, the inherent need arises to make an adjustment or modification to the designs of conventional masks to guarantee the largest volume of filtered air and thus reduce the risk of contagion between individuals.
On the other hand, with technological advances in the area of medicine and health, it is possible to design and manufacture devices that improve the behavior of masks. The use of technologies, such as 3D printing, PIM (plastic injection molding), CAM (computer-aided manufacturing), and CNC (computerized numerical control), among others, allows creating parts with high precision that previously, due to a lack of technology, was not possible. Additionally, the use of three-dimensional simulation technologies and the manufacture of prototypes allows establishing a design that can be verified and experimentally validated at a low cost [
33].
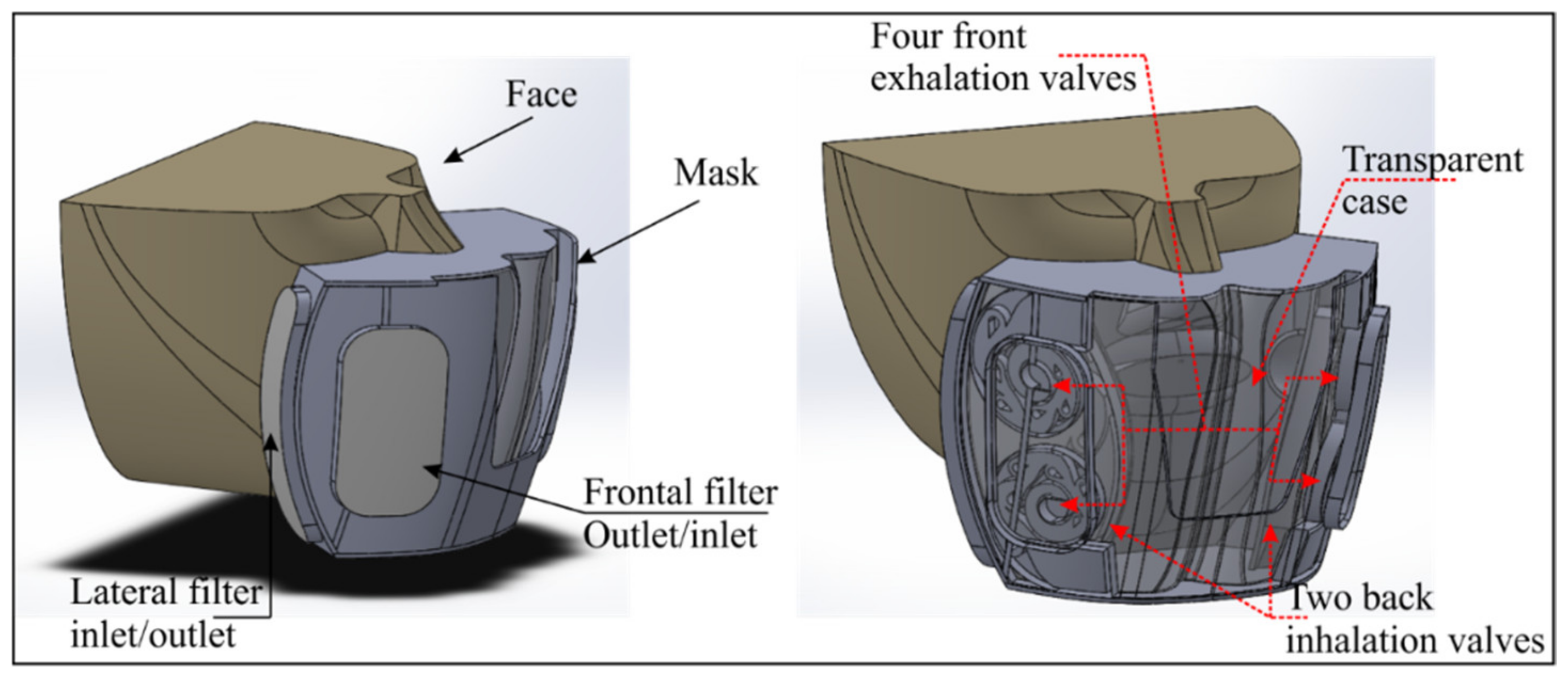
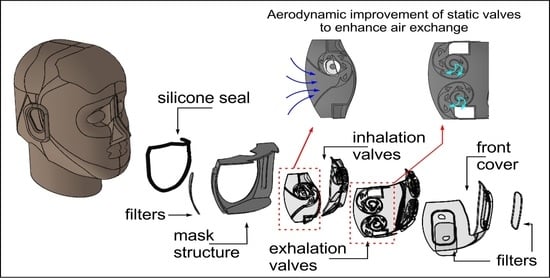
Given the need to improve the performance and design of protective masks against the SARS-CoV-2, the objective of this work was to conceive an enhanced interior aerodynamic geometry of a mask maintaining the best filtering properties available to date and to compare the flow fields through a CFD analysis between the new geometric proposal and the FFR-KN95 mask assumed to be the best option for the protection of the user considering one of the main topics in the design of a comfortable, aerodynamic, and effective mask [
34].
Governing Equations
A CFD analysis implies the solution through iterative and numerical methods of the fluid mechanics governing equations. In this study, the aerodynamics through the turbulence
k-ε model was used to analyze the performance of the valves located at the interior of the mask. The Reynolds-averaged Navier–Stokes (RANS) equations of mass (1) and momentum ((2)–(4)) conservation in a tridimensional and cartesian scheme [
35] were solved to obtain the velocity and turbulence fields in a stationary scheme and non-compressible state according to the absence of supersonic velocities into the mask.
where
u,
v, and
w are the velocity,
is the fluid density,
p is the absolute pressure, ν is the kinematic viscosity of the fluid, and
is the eddy viscosity.
The
k-
ε turbulence model was selected because it offers a good approximation of the estimation of the turbulent kinetic energy (
k) and the dissipation rate (
ε) in circular flows, confined fluids that have considerable Reynolds stresses in the domain. Computationally, it is one of the most efficient and reliable models [
35,
36].
where:
is the turbulent kinetic energy;
ε the dissipation rate of the kinetic energy;
is the eddy viscosity;
,
,
,
, and
are adjustable constants according to the experimental data proposed and described in literature [
36,
37,
38].
The filter medium idealized as porous media was defined to simulate the flow resistance through the filter areas. Assuming laminar flow, the pressure drop is proportional to the flow velocity and the Darcy’s law (12) replaces the momentum equation.
where
is the air viscosity, 1/
α is the viscous resistance coefficient (1/m),
is the air velocity, and
is the pressure. The viscous and inertial resistance coefficients are described in [
38] and can be estimated with the expressions ((13) and (14)), respectively, and are used in the Ergun Equation (15).
where
pressure drops per length unit,
is the dynamic viscosity,
the fluid density,
the porosity of the medium,
the sphericity of the particles making the medium, and
the diameter of the particles making the medium.
For the static structural analysis, the stress–strain relationship for linear materials was used, where the stress is related to the strain according to the Equation (16).
where
is the stress vector known as
S =
;
is the elasticity or elastic stiffness matrix;
elastic strain vector. The elastic stiffness matrix depends on Young’s modulus (
E), Poisson’s ratio (
ν), and the shear modulus (
G). These properties are specified according to the material used in the analysis.
3. Results and Discussion
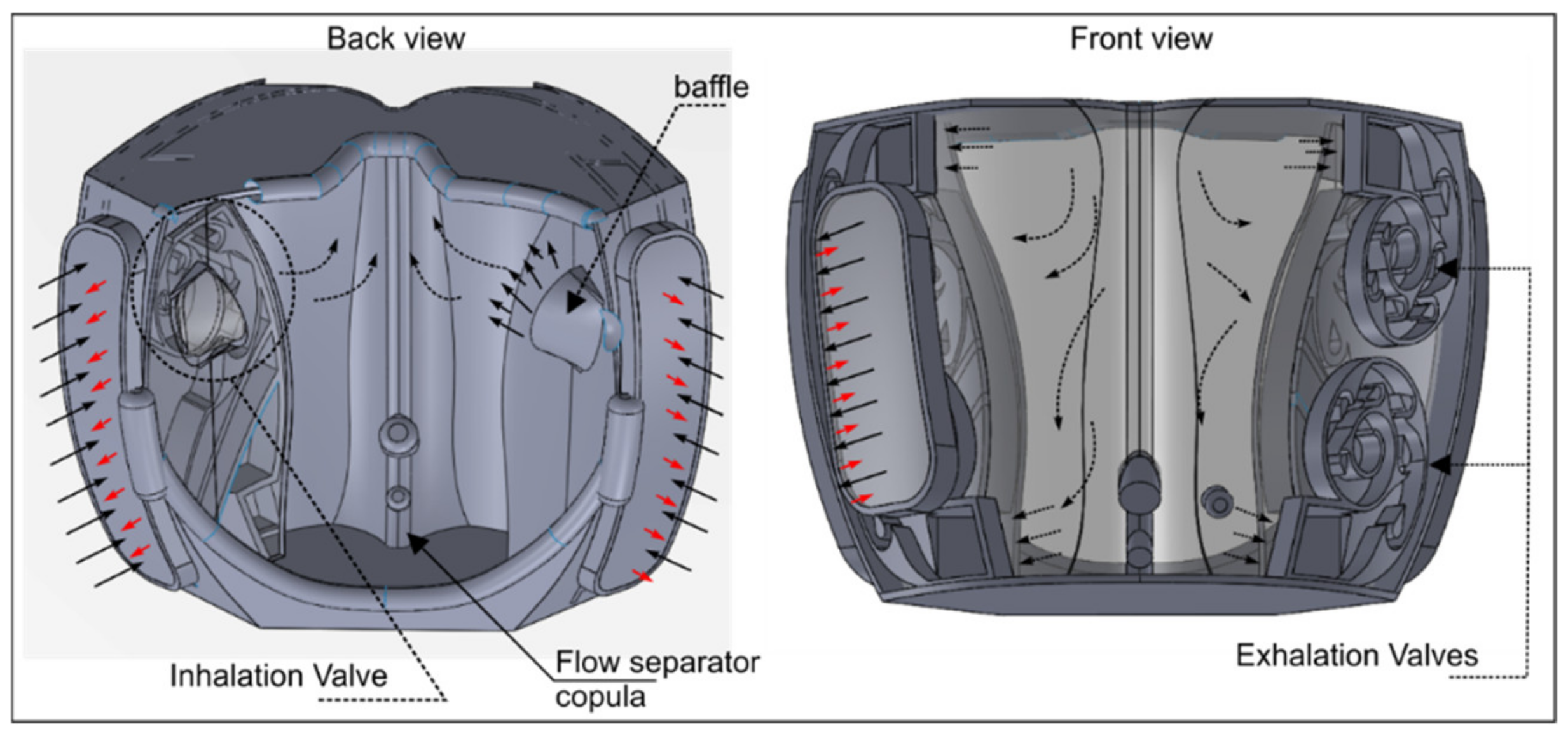
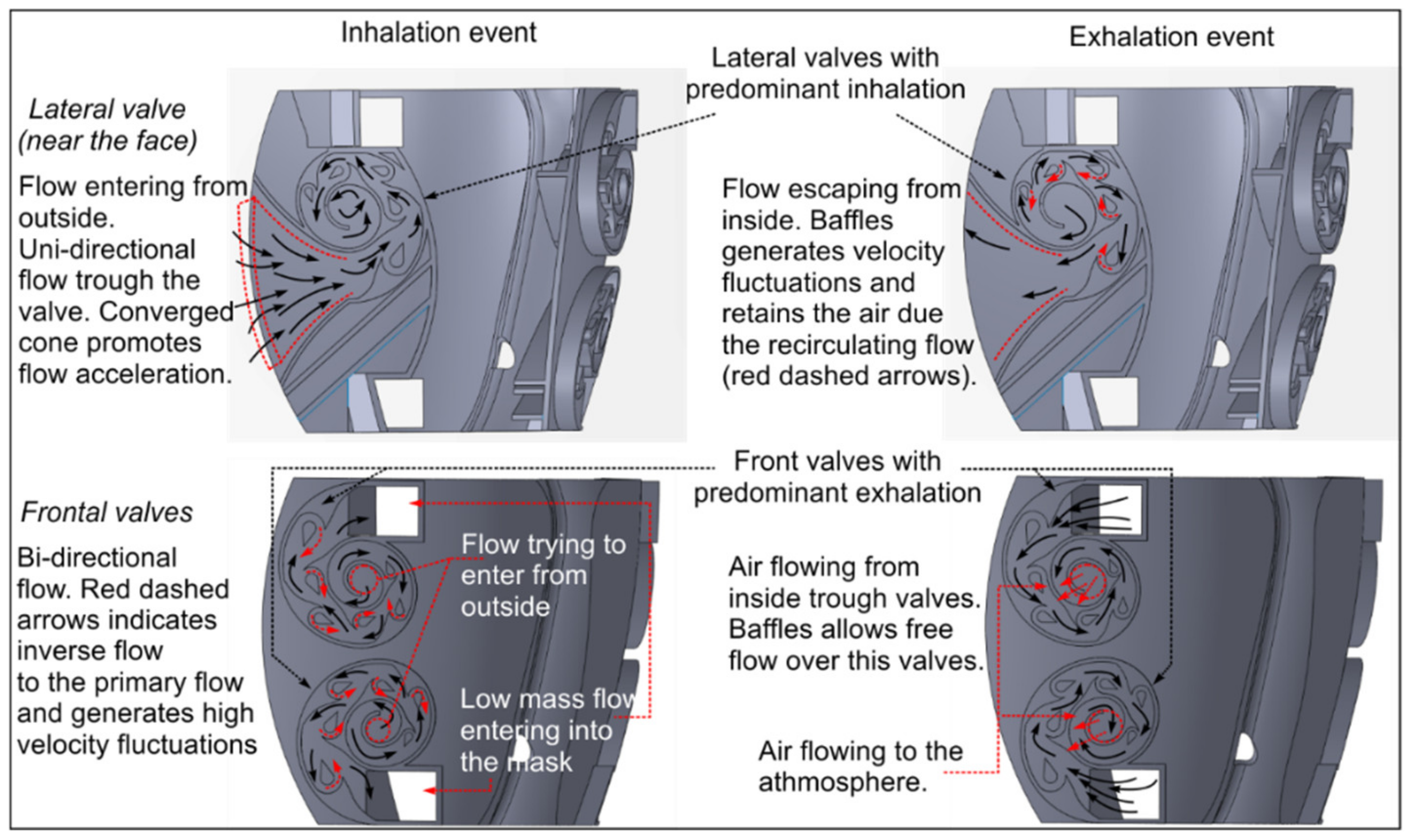
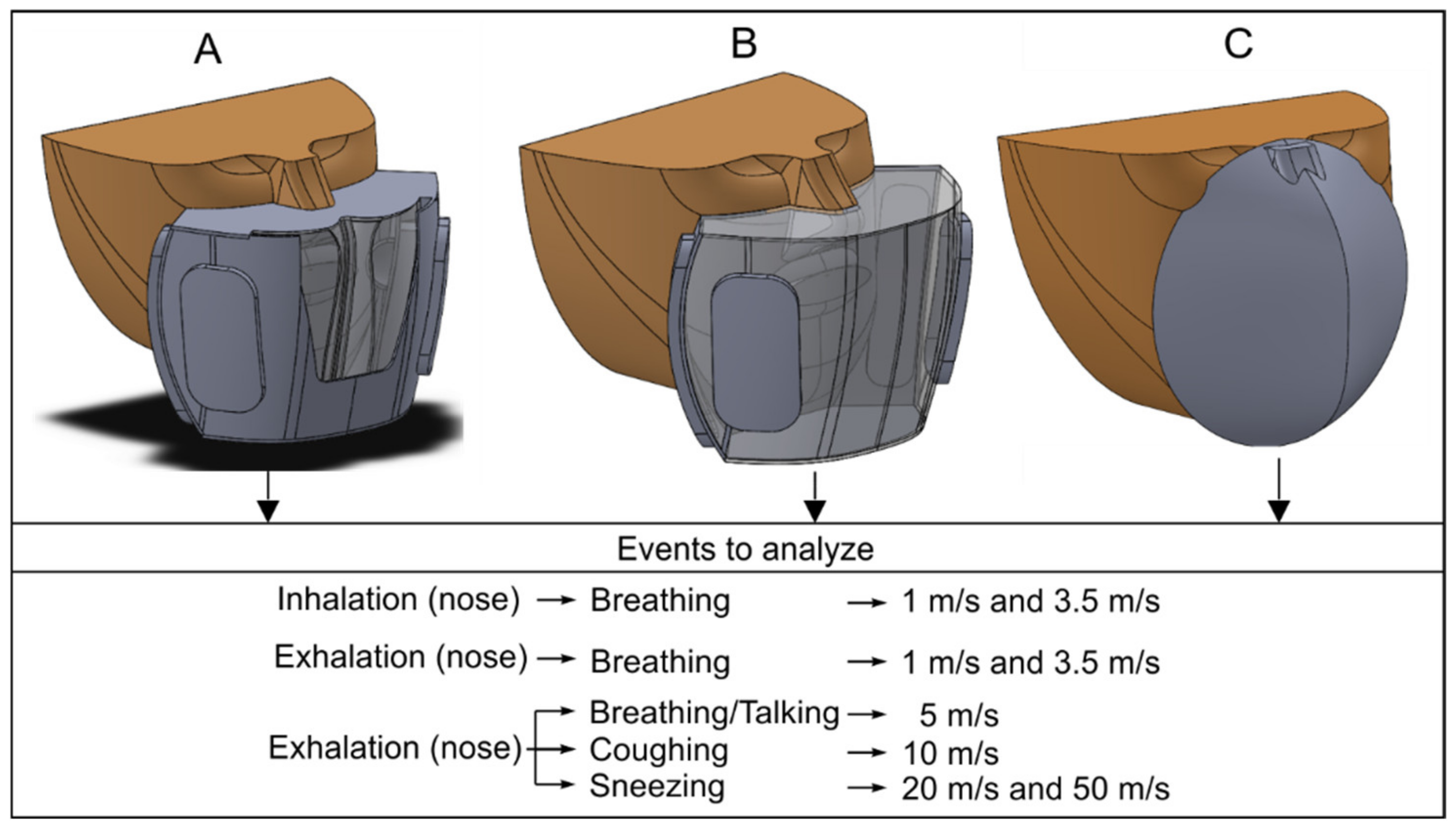
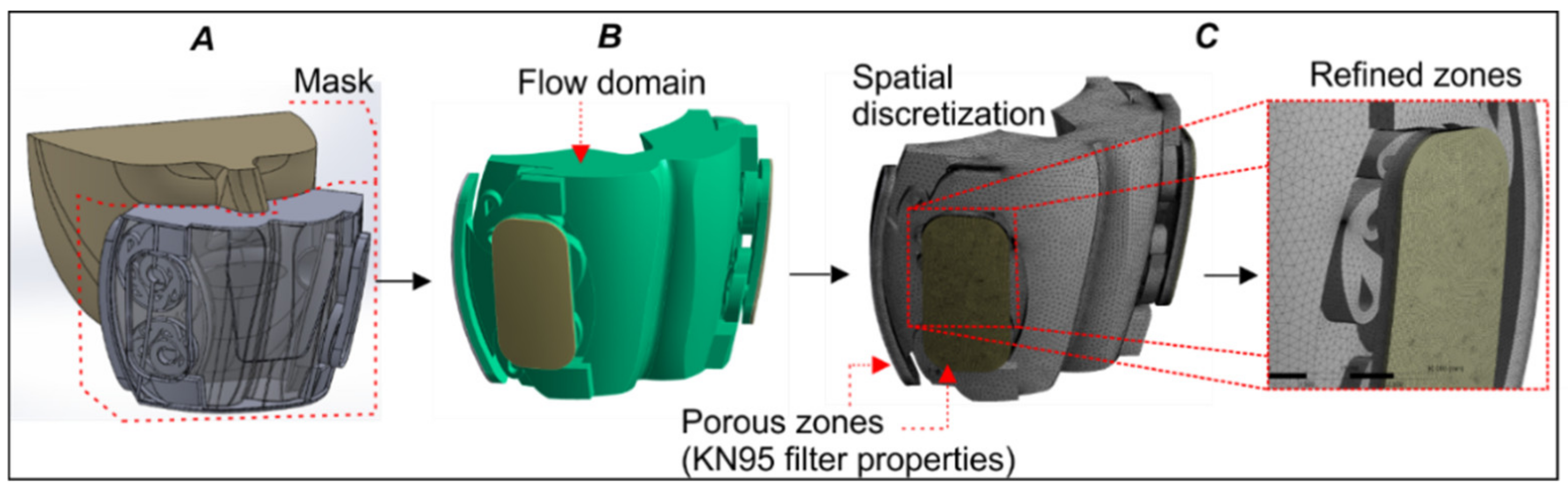
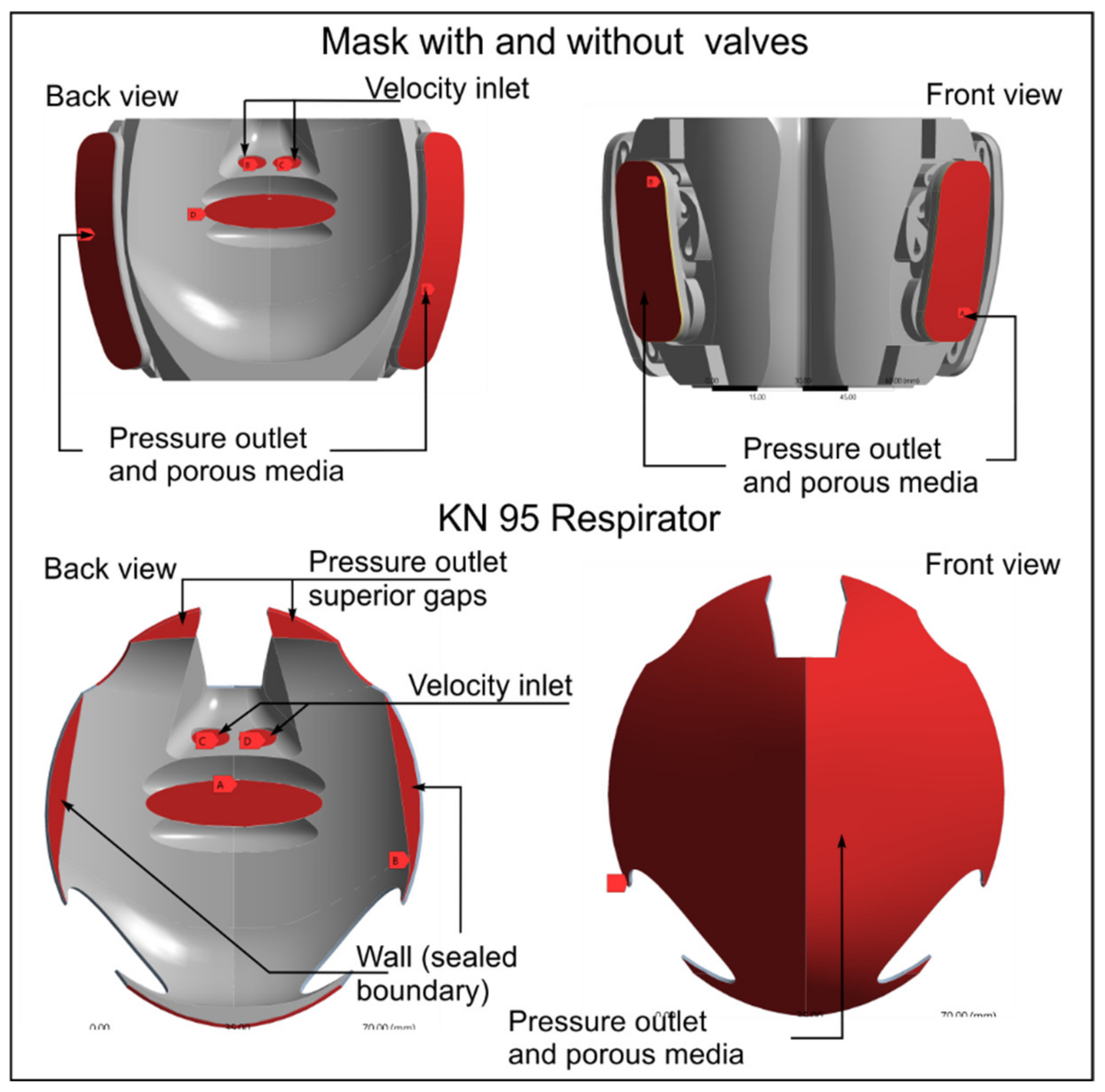
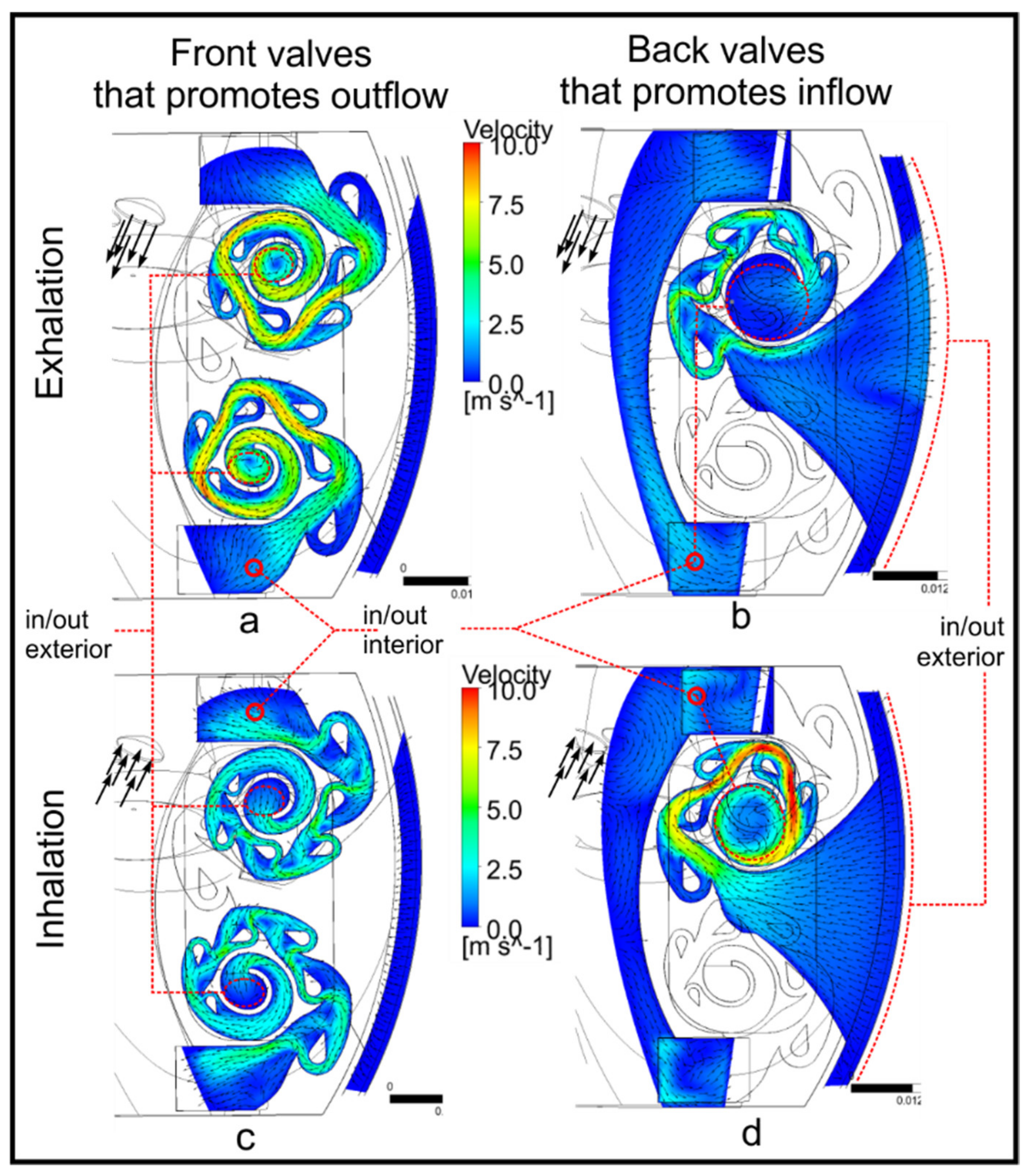
The results of the CFD analysis are shown graphically, in particular the velocity and turbulence fields of the mask prototype with internal valves without considering filtering media. To appreciate the operation of the inner valves, the results of the flow fields for inhalation and exhalation events in the nose at a velocity of 3.5 m/s are shown.
Figure 8 shows the velocity fields for the inhalation and exhalation events in a lateral plane located in the middle of the inner valves. In this figure, it can be observed that the air flows with greater velocity in the frontal valves whose objective is the air outlet (
Figure 8a), and this velocity is much lower in the inhalation event for the same valve zone (
Figure 8c). With respect to the behavior of the valve system for the inhalation event, there is a higher velocity in the lateral valves whose objective is to favor the entry of air (
Figure 8d), and this velocity is significantly reduced in the same area when the event of exhalation (
Figure 8b) restricts free flow in this area.
The effect that occurs inside the valves to promote flow in one direction and restrict it in the other is attributed to the innovative geometric design of the ducts and baffles that generate velocity fluctuations associated with turbulence.
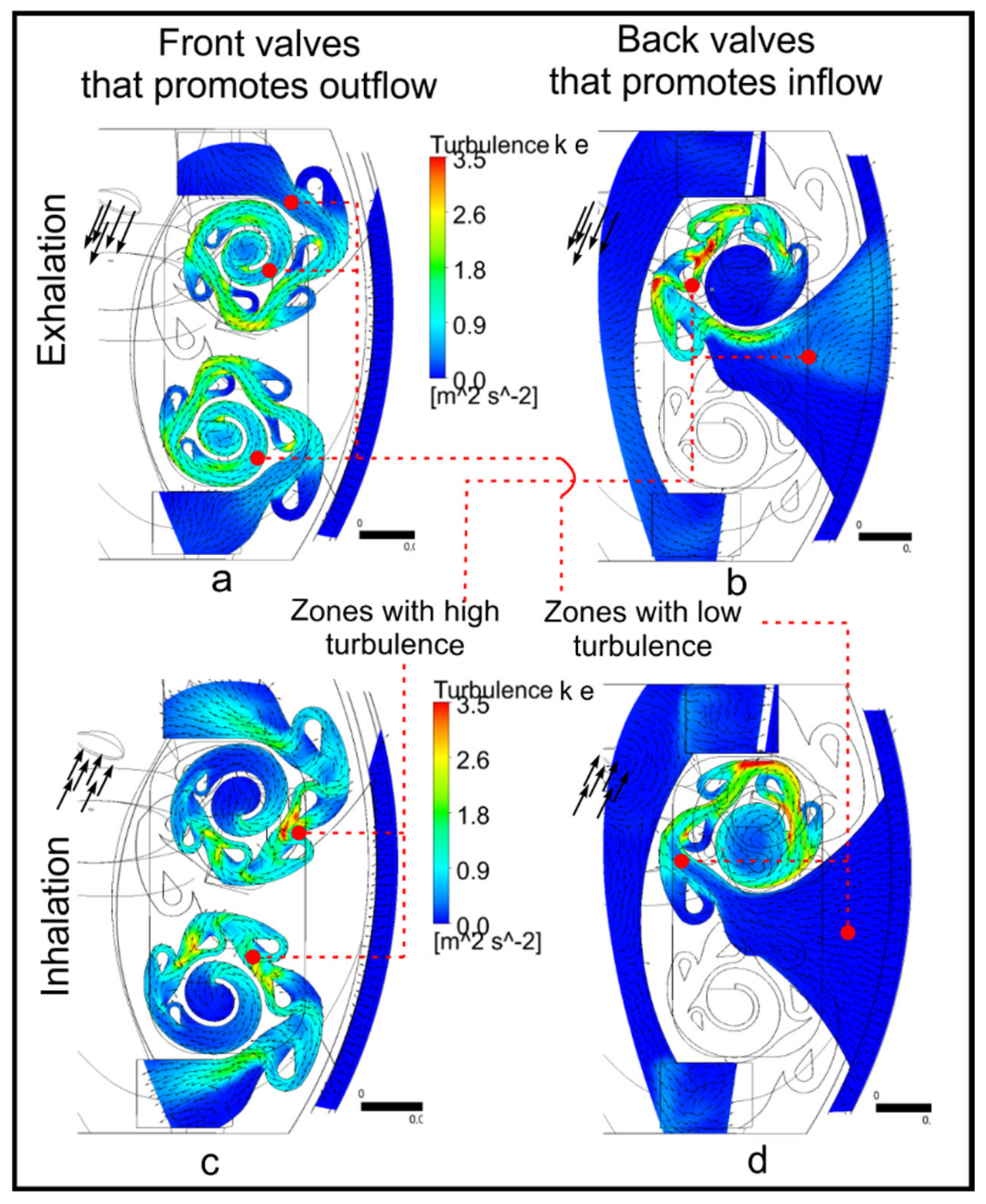
Figure 9 shows the turbulence fields in each valve in the inhalation and exhalation events for a velocity of 3.5 m/s in the mask without considering filtering media. It is observed that the performance found of the orientation and shape of the baffles effectively promotes the shock of flows and velocity fluctuation in the valves shown in
Figure 9b,c for the exhalation and inhalation events, respectively.
Figure 9a,d shows that there is turbulence in the range of 0.9–2.6 m
2/s
2; however, the air flows uniformly, as indicated by the vectors, and there is less turbulence at the inlets and outlets of the flow.
The aerodynamic analysis of the proposed mask allowed us to know the mass flow that enters and leaves each of the valves for the inhalation and exhalation events. According to the inhalation and exhalation velocities described in the literature, it is possible to know the mass flow that a person inhales and exhales through the nose and mouth [
26]. Thanks to the CFD analysis, it was possible to compare the inhalation and exhalation flows in the different inlets and outlets of the mask proposed in this work. The priority that was established in the geometric design of the mask was to achieve the rapid and effective exit of the air through the front of the mask in the event of exhalation, avoiding the stagnation of the flow within the mask. On the other hand, the proposed geometric design allows the prioritization of air intake from the lateral area of the mask, and the flow is directed towards the nose for early inhalation, thus avoiding breathing again the air that had previously been exhaled from the front. This ensures the flow exchange, a situation that is not found with any of the conventional masks.
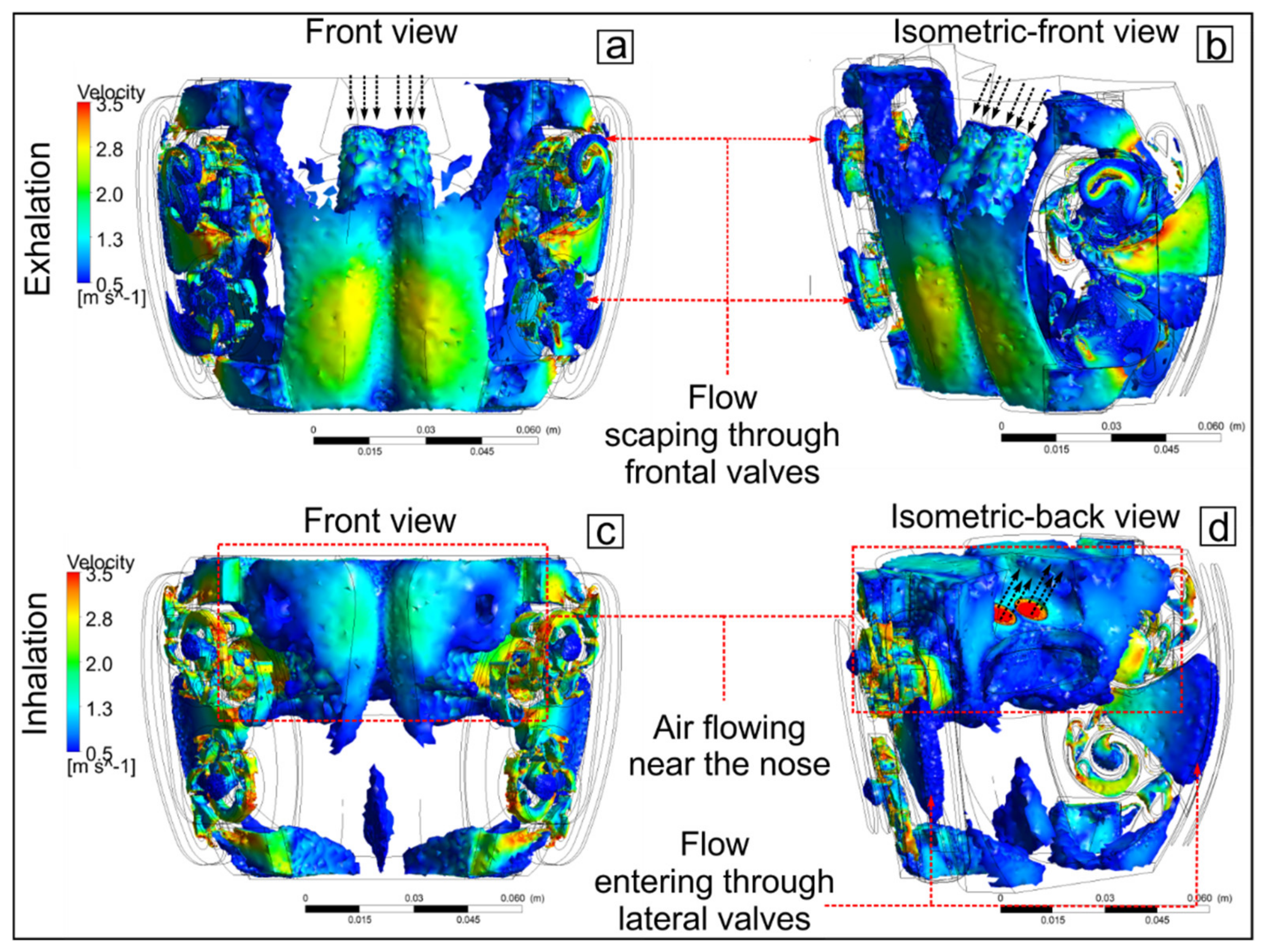
Figure 10 shows an iso-volume of the air and its velocity inside the mask and valves for the inhalation and exhalation events for a velocity of 3.5 m/s.
Figure 10a,b shows that the air that comes out through the nose in the exhalation event impacts the mask and is directed towards the frontal and lateral valves, preventing its recirculation within the mask. In
Figure 10c,d, the air from the lateral inlets is directed directly to the nose and mouth, ensuring that the greatest amount of air volume is inhaled during the duration of the inhalation event, which is approximately 1.5 s [
26,
41].
The results obtained prove that the geometry of the valves and the mask allow an effective bidirectionality of the flow in the inhalation and exhalation events. However, to perform the functional contrast with respect to a commercial mask type KN95, it was necessary to include in the boundaries the conditions of a porous medium representing the resistance to the free flow of air through a filter with KN95 characteristics. The inclusion of the filter in the borders of the mask presented in this work decreased its efficiency with respect to the scenarios presented without filters. However, the flow exchange is still evident, as is the efficiency of the air flow towards the inlets and outlets. Likewise, it was considered important to make the comparison with the commercial mask model to demonstrate that the interior valves allow the entry and exit of air more efficiently than in those masks that do not have an interior aerodynamic design. For this, the flow fields were also compared with the geometry of the mask proposed in this work without valves and interior baffles, with the purpose of verifying that the valves effectively direct the air towards the inlet and outlet zones.
Table 4 shows the air flows and the corresponding percentage in each zone for the case of the mask with valves for different operating scenarios. For the most frequent operating scenarios, such as breathing, 62% of the air was inhaled through the lateral valves, and 38% was inhaled through the front valves. These percentages change significantly for the exhalation event, where 77% of the air leaves through the frontal valves, while 26% leaves through the lateral valves for a velocity of 3.5 m/s in the nose. For the case of respiration associated with a velocity of 1 m/s, the percentages of the air volumes change for the inhalation and exhalation events compared to the case of respiration of 3.5 m/s. However, the operation of the valves maintains a greater volume of air exhaled through the frontal area and a greater volume inhaled through the lateral areas. In addition, for the cases of talking, coughing, and sneezing, 77% of the air comes out of the frontal valves. This situation allows that, at the time of inhalation, there is an entry of clean air that enters through the side valves, avoiding the entry of air that was previously exhaled through the frontal area. This exchange of volumes in each zone and for each event was achieved thanks to the innovative geometry designed inside the spiral valves with convergent channels, thus improving the behavior of the mask proposed in this work.
Table 5 shows the values of the air flows and the corresponding percentage in each zone for the cases of masks with valves, without valves, and the KN95 model considering filters in all cases and an entry velocity through the nose of 3.5 m/s. It is observed that the mask with valves presents a greater volume of exhalation flow in the frontal zone with 60% of the total flow. For the inhalation event, it is observed that the flow is divided into equal parts for each zone, where 50% of the total flow enters through the frontal zone while the other 50% enters through the lateral zone. With these values of air volume, it is also observed that there is a change in the behavior of the mask with valves when considering the filtering medium at the boundaries. However, this scenario offers an ideal approximation to the real behavior of masks with filter media.
For the case of the mask without valves where there are only filters at the borders, there is an inflow and outflow of the frontal zone of 55% and the lateral zones of 45%. This is achieved by idealizing a hermetic seal of the mask with the face but without internal aerodynamic movement. This case of a mask guarantees the entry and exit of air, but, with recirculation inside, a situation very similar to that of a KN95 mask. For the case of a KN95 mask, only 4–5% of the flow is in and out of the filter from which the mask is made. This causes the greatest amount of flow to enter and exit through the gaps between the face and the seal of the mask. Ninety-five percent of the air enters and exits through different areas, such as the upper part of the nose, because it does not have an airtight seal with the face, a situation that occurs with the majority of users of this type of mask [
26,
27,
28,
30,
32].
The results shown above were obtained through CFD analysis, and, in practice, these results may vary slightly because the analysis of the porous medium applied in the simulation is numerical and simplified. However, it is a good alternative to complement the aerodynamic analysis of the mask with valves since the comparison of the flow fields with the mask without valves and the KN95 mask was performed considering the same filter conditions at the borders in all cases.
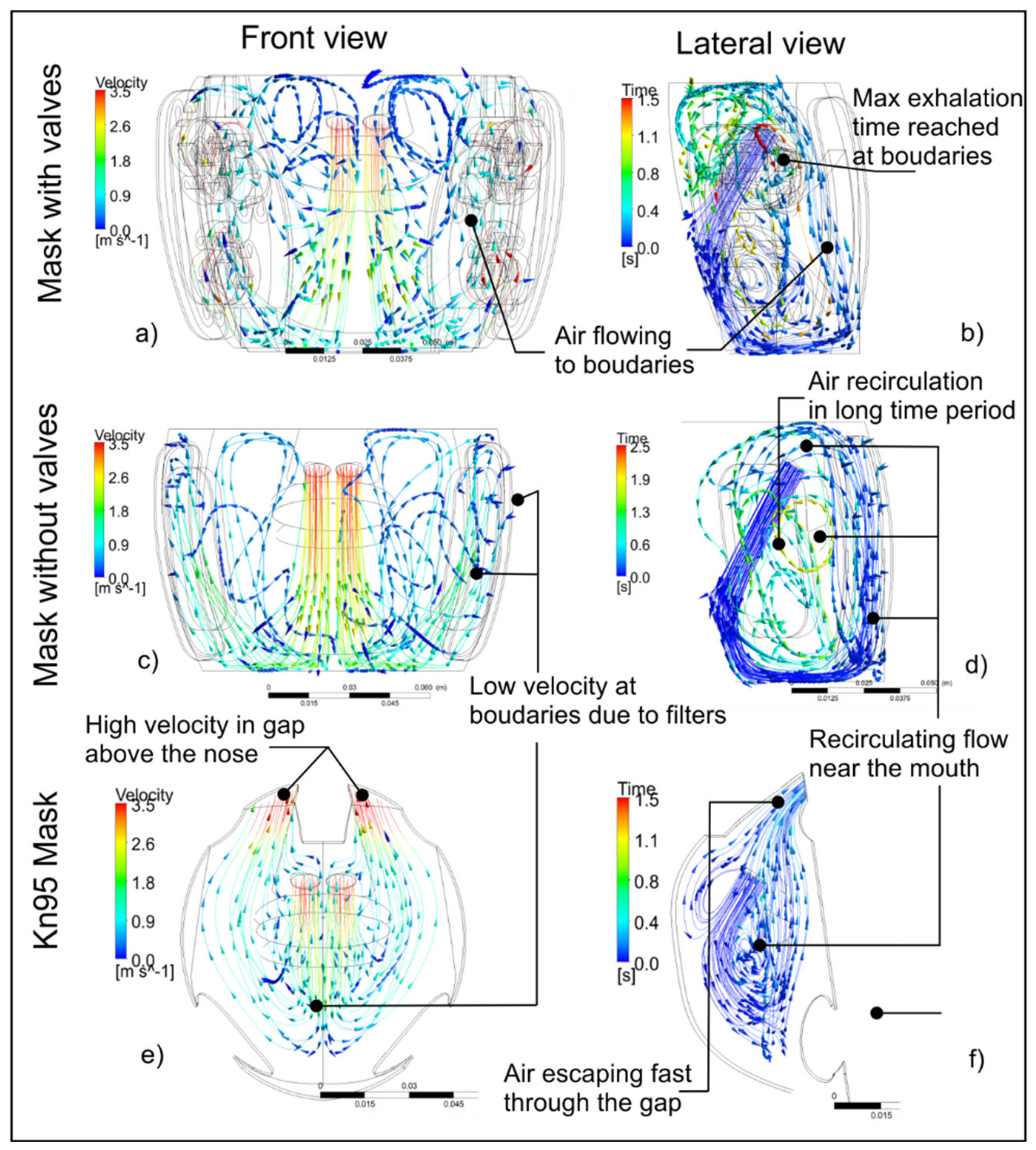
Figure 11 shows the flow velocity streams for the mask with valves and baffles, the mask without valves, and the KN95 respirator considering the exhalation flow through the nose of 3.5 m/s. In
Figure 11a,b, it can be observed that the air flow path flows towards the front and side valves. In addition, considering that the maximum duration of an exhalation event is 1.5 s, it is observed that, at that instant of time, the flow is already close to the outlets, guaranteeing its expulsion outside the mask. On the other hand, in
Figure 11d, it is observed that there is a recirculation of the flow inside the mask by not having the valves and the baffles to direct the flow towards the outlets. Consequently, the air recirculates for approximately 2 s, a time that exceeds the maximum value of an exhalation event. This causes the air that cannot escape to the outside of the mask to be re-inhaled by the user. Finally,
Figure 11e,f shows the flow velocity and exhalation timelines for the KN95 respirator, considering the frontal area as the filter and a gap over the nose. It is observed that the air leaves through the upper gap in a very short time (<0.5 s) since the geometry of the mask and the characteristics of the porous medium prevent it from leaving through the frontal area. In addition, it is observed that there is a recirculation of air in the area near the mouth, causing a sensation of suffocation for the user, as well as a headache from inhaling CO
2 when the mask is used for long periods.
The results obtained from the analysis of the mask without valves and the KN95 mask show that the flow has a longer time and recirculation path within the mask before exiting. In addition, the filters (porous medium) operate as a barrier, preventing the flow through them efficiently. By using the valves and deflectors inside the mask proposed in this work, it is guaranteed that there is no recirculation of the flow near the mouth or nose. In the case of the mask with valves, the presence of the filters in the borders allows the flow out more efficiently since the valves accelerate the air flow, so the resistance to flow caused by the filters is overcome.
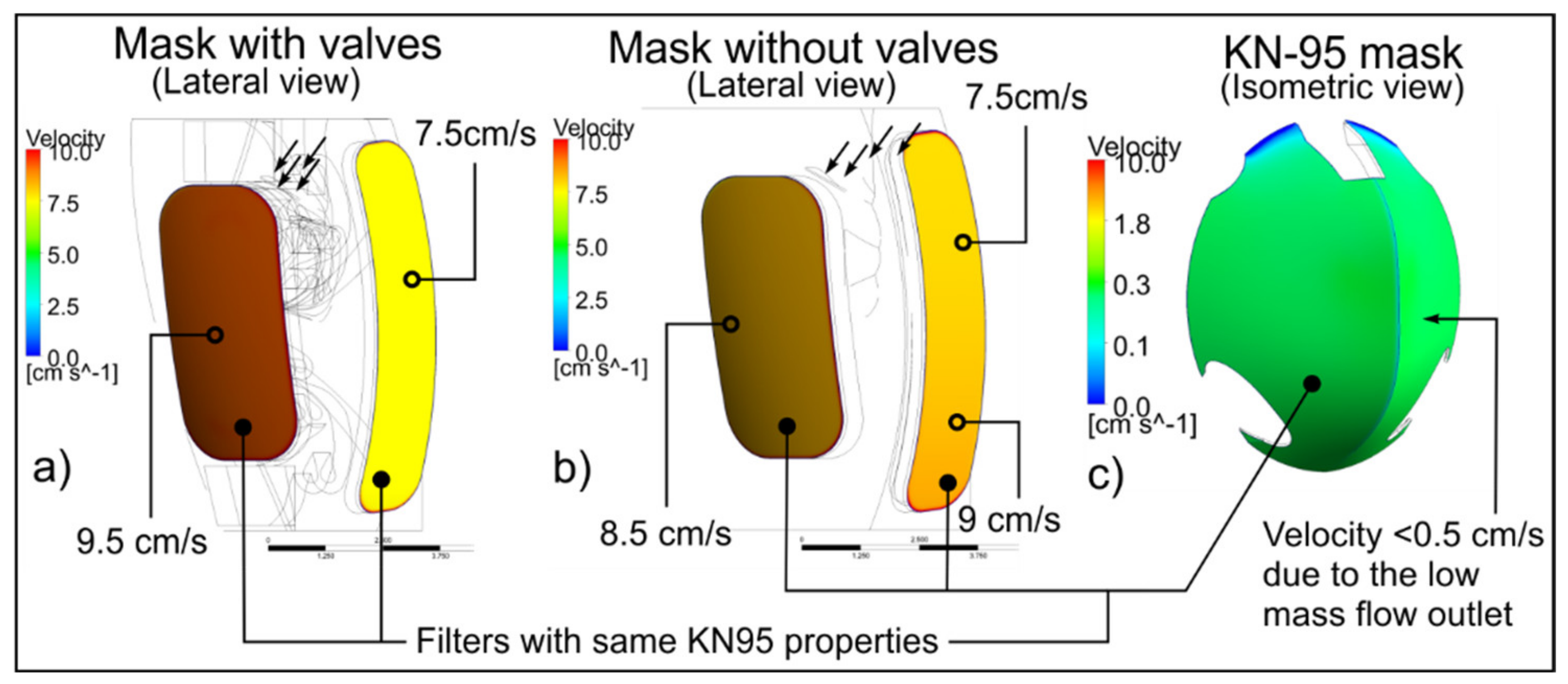
To verify the behavior of the outflow air in each mask,
Figure 12 shows the velocity contours at the boundaries considering the exhalation event in the nose of 3.5 m/s and maintaining the filter conditions (porous medium) in all the scenarios. For the mask with valves shown in
Figure 12a, the exit velocity in the frontal zone is approximately 9.5 cm/s, while the air velocity in the lateral zone is maintained at 7.5 cm/s. For the case of the mask without valves shown in
Figure 12b, the flow velocity in the frontal zone is approximately 8.5 cm/s, while, in the lateral outlet, it varies between 7.5 and 9 cm/s. For the case of the KN95 mask, there is a velocity <0.5 cm/s in the frontal area (
Figure 12c). This velocity occurs because the amount of air that comes out through this area is barely 5% of the total exhaled flow. The highest airflow velocity occurs in the gaps, a situation that prevents the exhaled air from passing through a filter before its release into the atmosphere.
According to the previous results, it is guaranteed that the geometric design of the valves and baffles inside the mask is effective and efficient. The results and their comparisons with the other masks showed that there is a total exchange of air within the maximum period of the inhalation and exhalation events. The enhanced geometry of the valves and baffles promotes a greater outflow in the frontal part in the exhalation, while, in the inhalation, a greater amount of air is sucked through the lateral zones. In addition, the outlet velocities in the filters do not exceed 10 cm/s. With the design and location of the valves and filters at the boundaries, a low air outlet velocity is generated to avoid dispersion in the environment and thus reduce social distance and the danger of contagion mainly in crowded public places, such as land and air transport, schools, and offices.
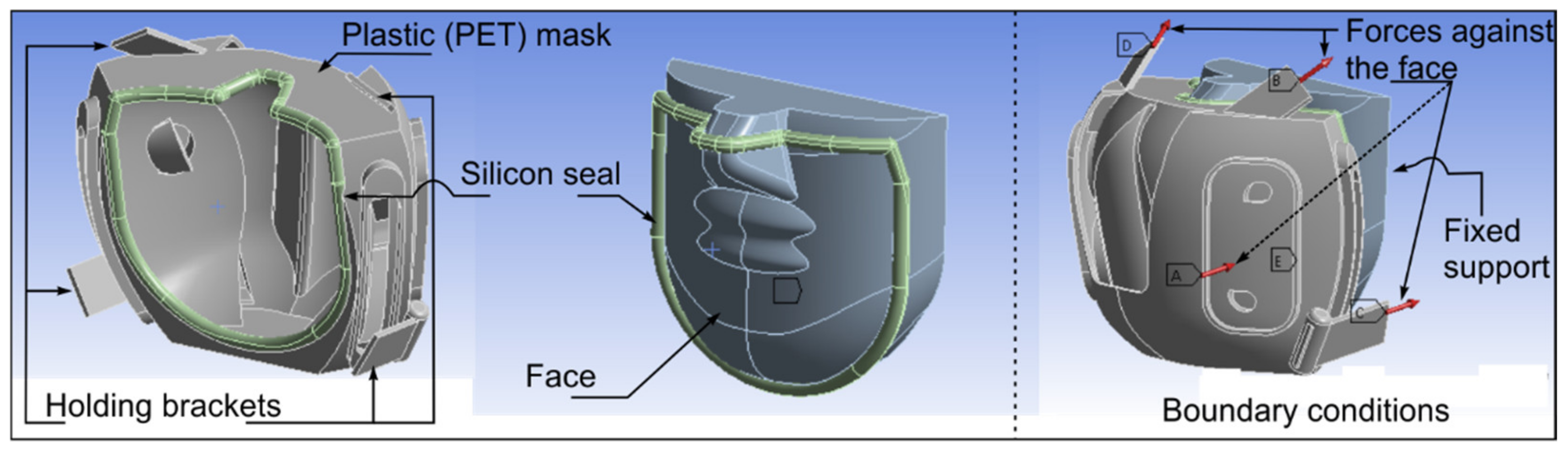
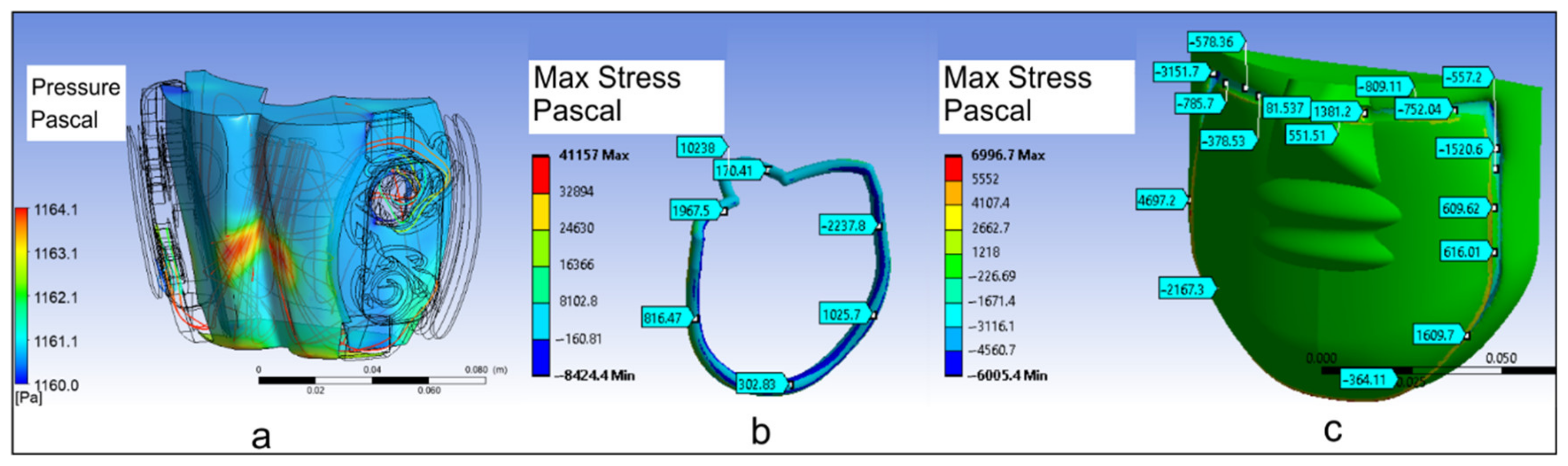
It is assumed that the aerodynamic results mentioned above are valid with the existence of the seal between the mask and the face, which was an important hypothesis in this work. Therefore, as part of the structural analysis, the total internal pressure was used from the sum of the differential pressures within the fluid domain after the aerodynamic analysis.
Figure 13a shows the pressure field on the inner surface of the mask. The magnitude of the force on each mask holding bracket is proportional and calculated from the internal aerodynamic pressure uniformly applied over the cross-sectional area of the seal against the face. For the exhalation event with a velocity of 3.5 m/s, the total pressure resulting from the aerodynamic analysis inside the mask is 1131 Pa and up to 1164 Pa in the surface. The perimeter area of the seal in contact with the face was proposed as 0.0015 m
2, and the total force was approximately 1.7 N. The force corresponding to each holding bracket is 0.42 N.
Figure 13b,c shows the maximum stresses on the face and seal. It is observed that, in both cases, there are minimum values between 80–170 Pa and maximum values of 1600–2300 Pa. With the presence of these values, it is established that the position of the proposed holding supports in the mask allows the sufficient deformation on the seal and face that can be associated with the tightness between them, avoiding areas of vacuum or air leakage from inside the mask.
By maintaining efficient aerodynamics inside the mask, the discomfort towards the user is reduced, promoting its prolonged use in daily activities. This situation will allow the user to use the mask to avoid the spread of viral and bacterial diseases in closed and public spaces. In addition, due to the COVID-19 pandemic, the World Health Organization (WHO) [
1] constantly suggests the use of masks even in healthy individuals and mainly in places where it is not possible to maintain social distancing to avoid the spread of diseases among individuals. Although there is a rejection by society towards the use of masks due to the discomfort they generate, with the proposal made in this research, it is possible to offer an alternative mask with qualities of efficiency in air exchange, comfort, and reusability with a scope for civil and medical use. Thus, government health agencies in various countries can establish a mandatory use of the mask in social, economic, and service activities where there are face-to-face interactions between individuals and, at the same time, promote an acceptance of its use in society [
48].
4. Conclusions
The proposal of a mask with enhanced interior aerodynamic geometry allows establishing a solution to the deficiencies of conventional masks that are usually uncomfortable and do not guarantee adequate protection for the user. The KN95 commercial masks lack a geometric design that allows adequate air exchange. In general, there is no airtight seal with the face, causing the entry and exit of air through gaps in the lateral part and mainly in the upper part of the nose. The implementation of static valves and baffles inside the mask proposed in this work allows directing the flow of inhalation and exhalation towards the inlets and outlets, avoiding recirculation at the interior. By guaranteeing a total exchange of flow, the re-inhalation of air that has been previously exhaled is reduced, offering greater comfort and convenience to the user.
The CFD analysis of the proposed mask allowed us to visualize and quantify the movement of air inside in a three-dimensional way and at a low cost. In fact, with the numerical analysis and simulation, it was possible to observe the change in the flow fields and percentages of air entry and exit in the inhalation and exhalation events. With this, it is verified that the proposed valves and baffles work correctly in two directions, allowing greater air flow in one direction and restricting it in the opposite direction. In addition, based on the various operating scenarios (breathing, talking, coughing, and sneezing), the expulsion of the greatest amount of air through the frontal zone and a greater amount of air entry through the lateral zones is guaranteed for all cases.
The analysis performed considering the filter (porous medium) at the boundaries of the masks facilitated a comparison of the flow fields, allowing the entry and exit of air even when there is the condition of flow restriction. In addition, having filters with KN95 characteristics at the borders guarantees the approval by competent health authorities for their civil and medical use because the same filtering materials of conventional masks are used. It is important to emphasize that, based on the performance comparison of the masks with the same characteristics of the filter, a better aerodynamic behavior was obtained in the mask proposed. Particularly compared to the traditional model, since the recirculation of air to the interior was avoided, it favored the efficient exit of air across the boundaries. Moreover, with the static structural analysis, it was possible to evaluate the pressure and tension between the seal and the face to guarantee an adequate support of the mask and avoid leaks around the perimeter of the seal.
Finally, the design of the internal and external components of the mask proposed in this work are intended to be manufactured at a low production cost, even with recycled PET material, and be washable and reusable, which constitutes a socially, economically, and environmentally sustainable proposal.