What Combination of Generic Bedside Screening Tools Is Optimal to Capture Patients with Penetration/Aspiration Due to Dysphagia? Comparing Single Bedside Tools Versus Combinations of Tools for Sensitivity and Specificity
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Data Collection
2.3. Barthel Index (BI)
2.4. The Four-Question Test (4QT)
- Do you cough or choke when eating or drinking?
- Does it take longer to finish your meals than it used to?
- Have you altered the types of food you eat?
- Does your voice change after eating or drinking?
2.5. The Minimal Eating Observation Form—II (MEOF-II)
2.6. Volume–Viscosity Swallow Test (V-VST)
2.7. The Flexible Endoscopic Evaluation of Swallowing (FEES) and the Penetration–Aspiration Scale (PAS)
2.8. Analysis
2.9. Ethical Considerations
3. Results
3.1. Patient Characteristics
3.2. Criterion-Related Validity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BI | Barthel Index |
| FEES | Flexible Endoscopic Evaluation of Swallowing |
| MEOF-II | Minimal Eating Observation Form—Version II |
| MEOF-IIs | Minimal Eating Observation Form—Version II, swallowing component |
| MS | Multiple Sclerosis |
| PAS | Penetration–Aspiration Scale |
| PD | Parkinson’s disease |
| V-VST | Volume–Viscosity Swallow Test |
| 4QT | Four-question test |
References
- Westergren, A.; Smithard, D.; Westergaard, M.; Norup, A.; Riis, J.; Krarup, A.; Hansen, L.E.M.; Emborg, C.; Melgaard, D. Convergent and discriminant validity of the Minimal Eating Observation Form—Version II: A cross-sectional study. BMC Geriatr. 2024, 24, 27. [Google Scholar] [CrossRef]
- Benfield, J.K.; Everton, L.F.; Bath, P.M.; England, T.J. Accuracy and clinical utility of comprehensive dysphagia screening assessments in acute stroke: A systematic review and meta-analysis. J. Clin. Nurs. 2020, 29, 1527–1538. [Google Scholar] [CrossRef] [PubMed]
- Rofes, L.; Arreola, V.; Mukherjee, R.; Clavé, P. Sensitivity and specificity of the Eating Assessment Tool and the Volume-Viscosity Swallow Test for clinical evaluation of oropharyngeal dysphagia. Neurogastroenterol. Motil. 2014, 26, 1256–1265. [Google Scholar] [CrossRef] [PubMed]
- Velasco, L.C.; Imamura, R.; Rêgo, A.P.V.; Alves, P.R.; Peixoto, L.P.d.S.; Siqueira, J.d.O. Sensitivity and Specificity of Bedside Screening Tests for Detection of Aspiration in Patients Admitted to a Public Rehabilitation Hospital. Dysphagia 2021, 36, 821–830. [Google Scholar] [CrossRef]
- Gagnier, J.J.; Lai, J.; Mokkink, L.B.; Terwee, C.B. COSMIN reporting guideline for studies on measurement properties of patient-reported outcome measures. Qual. Life Res. 2021, 30, 2197–2218. [Google Scholar] [CrossRef]
- Lindh, M.G.; Johansson, M.B.; Jennische, M.; Koyi, H. Prevalence of swallowing dysfunction screened in Swedish cohort of COPD patients. Int. J. Chron. Obs. Pulmon Dis. 2017, 12, 331–337. [Google Scholar] [CrossRef]
- Aghaz, A.; Alidad, A.; Hemmati, E.; Jadidi, H.; Ghelichi, L. Prevalence of dysphagia in multiple sclerosis and its related factors: Systematic review and meta-analysis. Iran J. Neurol. 2018, 17, 180–188. [Google Scholar] [CrossRef]
- Gong, S.; Gao, Y.; Liu, J.; Li, J.; Tang, X.; Ran, Q.; Tang, R.; Liao, C. The prevalence and associated factors of dysphagia in Parkinson’s disease: A systematic review and meta-analysis. Front. Neurol. 2022, 13, 1000527. [Google Scholar] [CrossRef]
- Westergren, A.; Karlsson, S.; Andersson, P.; Ohlsson, O.; Hallberg, I.R. Eating difficulties, need for assisted eating, nutritional status and pressure ulcers in patients admitted for stroke rehabilitation. J. Clin. Nurs. 2001, 10, 257–269. [Google Scholar] [CrossRef]
- Mahoney, F.I.; Barthel, D.W. FUNCTIONAL EVALUATION: THE BARTHEL INDEX. Md. State Med. J. 1965, 14, 61–65. [Google Scholar]
- Collin, C.; Wade, D.T.; Davies, S.; Horne, V. The Barthel ADL Index: A reliability study. Int. Disabil. Stud. 1988, 10, 61–63. [Google Scholar] [CrossRef] [PubMed]
- Staal, S.; Christensen, K.B.; Smithard, D.; Westergren, A.; Melgaard, D. Screening for dysphagia in older people: Psychometric properties of the Danish 4 Question Test (4QT-DK)—A validation study. Geriatr. Gerontol. Int. 2025, 25, 294–299. [Google Scholar] [CrossRef] [PubMed]
- Tsang, K.; Lau, E.S.; Shazra, M.; Eyres, R.; Hansjee, D.; Smithard, D.G. A New Simple Screening Tool-4QT: Can It Identify Those with Swallowing Problems? A Pilot Study. Geriatrics 2020, 5, 11. [Google Scholar] [CrossRef] [PubMed]
- Westergren, A.; Melgaard, D. The Minimal Eating Observation Form—II (MEOF-II) Danish Version—Psychometric and metrological perspectives. J. Nurs. Meas. 2020, 28, 168–184. [Google Scholar] [CrossRef]
- Westergren, A. The Minimal Eating Observation Form-Version II Revisited: Validity and Reliability. J. Nurs. Meas. 2019, 27, 478–492. [Google Scholar] [CrossRef]
- Wang, T.; Jiang, H.; Westergren, A.; Wang, J.; Wang, L. The Minimal Eating Observation Form-II (MEOF-II): Cross-cultural validation of the Chinese version for people with stroke. J. Eval. Clin. Pract. 2016, 22, 207–212. [Google Scholar] [CrossRef]
- Jørgensen, L.W.; Søndergaard, K.; Melgaard, D.; Warming, S. Interrater reliability of the Volume-Viscosity Swallow Test; screening for dysphagia among hospitalized elderly medical patients. Clin. Nutr. ESPEN 2017, 22, 85–91. [Google Scholar] [CrossRef]
- Clavé, P.; Arreola, V.; Romea, M.; Medina, L.; Palomera, E.; Serra-Prat, M. Accuracy of the volume-viscosity swallow test for clinical screening of oropharyngeal dysphagia and aspiration. Clin. Nutr. 2008, 27, 806–815. [Google Scholar] [CrossRef]
- Riera, S.A.; Marin, S.; Serra-Prat, M.; Tomsen, N.; Arreola, V.; Ortega, O.; Walshe, M.; Clavé, P. A Systematic and a Scoping Review on the Psychometrics and Clinical Utility of the Volume-Viscosity Swallow Test (V-VST) in the Clinical Screening and Assessment of Oropharyngeal Dysphagia. Foods 2021, 10, 1900. [Google Scholar] [CrossRef]
- Borders, J.C.; Brates, D. Use of the Penetration-Aspiration Scale in Dysphagia Research: A Systematic Review. Dysphagia 2020, 35, 583–597. [Google Scholar] [CrossRef]
- Rosenbek, J.C.; Robbins, J.A.; Roecker, E.B.; Coyle, J.L.; Wood, J.L. A penetration-aspiration scale. Dysphagia 1996, 11, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Altman, D.G. Practical Statistics for Medical Research, 1st ed.; Chapman and Hall: London, UK; New York, NY, USA, 1991; Volume xii, 611p. [Google Scholar]
- Loong, T.W. Understanding sensitivity and specificity with the right side of the brain. BMJ 2003, 327, 716–719. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, M.J.; Bauer, J.M.; Ramsch, C.; Uter, W.; Guigoz, Y.; Cederholm, T.; Thomas, D.R.; Anthony, P.; Charlton, K.E.; Maggio, M.; et al. Validation of the Mini Nutritional Assessment short-form (MNA-SF): A practical tool for identification of nutritional status. J. Nutr. Health Aging 2009, 13, 782–788. [Google Scholar] [CrossRef] [PubMed]
- Vesey, S. Dysphagia and quality of life. Br. J. Community Nurs. 2013, S16 (Suppl. S14), S14–S19. [Google Scholar] [CrossRef]
- Jones, E.; Speyer, R.; Kertscher, B.; Denman, D.; Swan, K.; Cordier, R. Health-Related Quality of Life and Oropharyngeal Dysphagia: A Systematic Review. Dysphagia 2018, 33, 141–172. [Google Scholar] [CrossRef]
- Tamura, B.K.; Bell, C.L.; Masaki, K.H.; Amella, E.J. Factors associated with weight loss, low BMI, and malnutrition among nursing home patients: A systematic review of the literature. J. Am. Med. Dir. Assoc. 2013, 14, 649–655. [Google Scholar] [CrossRef]
- Cichero, J.A.Y. Age-Related Changes to Eating and Swallowing Impact Frailty: Aspiration, Choking Risk, Modified Food Texture and Autonomy of Choice. Geriatrics 2018, 3, 69. [Google Scholar] [CrossRef]
- Chang, M.; Geirsdottir, O.G.; Launer, L.J.; Gudnasson, V.; Visser, M.; Gunnarsdottir, I. A poor appetite or ability to eat and its association with physical function amongst community-dwelling older adults: Age, gene/environment susceptibility-Reykjavik study. Eur. J. Ageing 2021, 18, 405–415. [Google Scholar] [CrossRef]
- Westergren, A.; Edfors, E.; Hedin, G.; Hagell, P. Improving nursing students research knowledge through participation in a study about nutrition, its associated factors and assessment. J. Nurs. Educ. Pract. 2013, 3, 50–58. [Google Scholar] [CrossRef]
| All Patients, n = 100 | |
|---|---|
| Age, median (q1–q3) | 72 (63–77) |
| Female/male, n | 42/58 |
| Activities of daily living, Barthel Index, high score = better, median (q1–q3) | 90 (60–100) |
| MEOF–II, low score = better | |
| Food intake, median (q1–q3) | 0 (0–1) |
| Food intake problems, n | 32 |
| Swallowing, median (q1–q3) | 0 (0–2) |
| Swallowing problems, n | 38 |
| Energy/appetite, median (q1–q3) | 1 (0–1) |
| Energy/appetite problems, n | 64 |
| Total score, median (q1–q3) | 2 (1–4) |
| Challenged in one or more eating categories (intake/swallowing/energy), n | |
| One category | 35 |
| Two categories | 30 |
| Three categories | 13 |
| Any problems, n | 78 |
| Dysphagia, 4QT, low score = better, median (q1–q3) | 2 (0–3) |
| Any problems, n | 69 |
| Volume–Viscosity Swallow Test, V-VST | |
| Dysphagia, n | 62 |
| Viscosity, managing unmodified/nectar/pudding, n | 89/7/1 |
| Volume, managing high (20 mL)/middle (10 mL)/low (5 mL), n | 63/26/8 |
| Penetration–Aspiration, PAS, low score = better, median (q1–q3) | 1 (1–1.2) |
| Having penetration/aspiration, n | 29 |
| Aspiration/Penetration Assessed Through the Flexible Endoscopic Evaluation of Swallowing (FEES) and Documented According to the Penetration–Aspiration Scale (PAS) | ||||||||
|---|---|---|---|---|---|---|---|---|
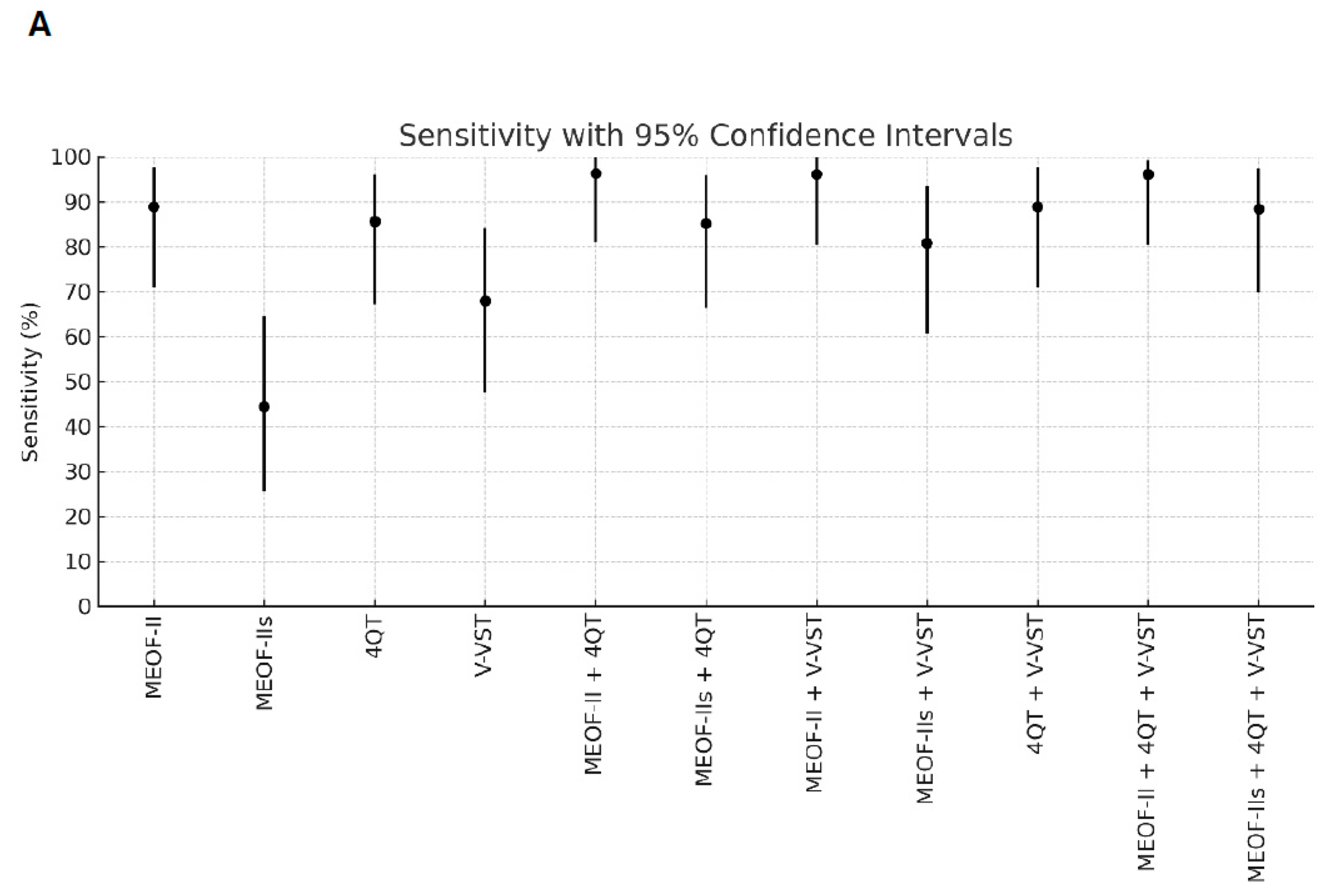
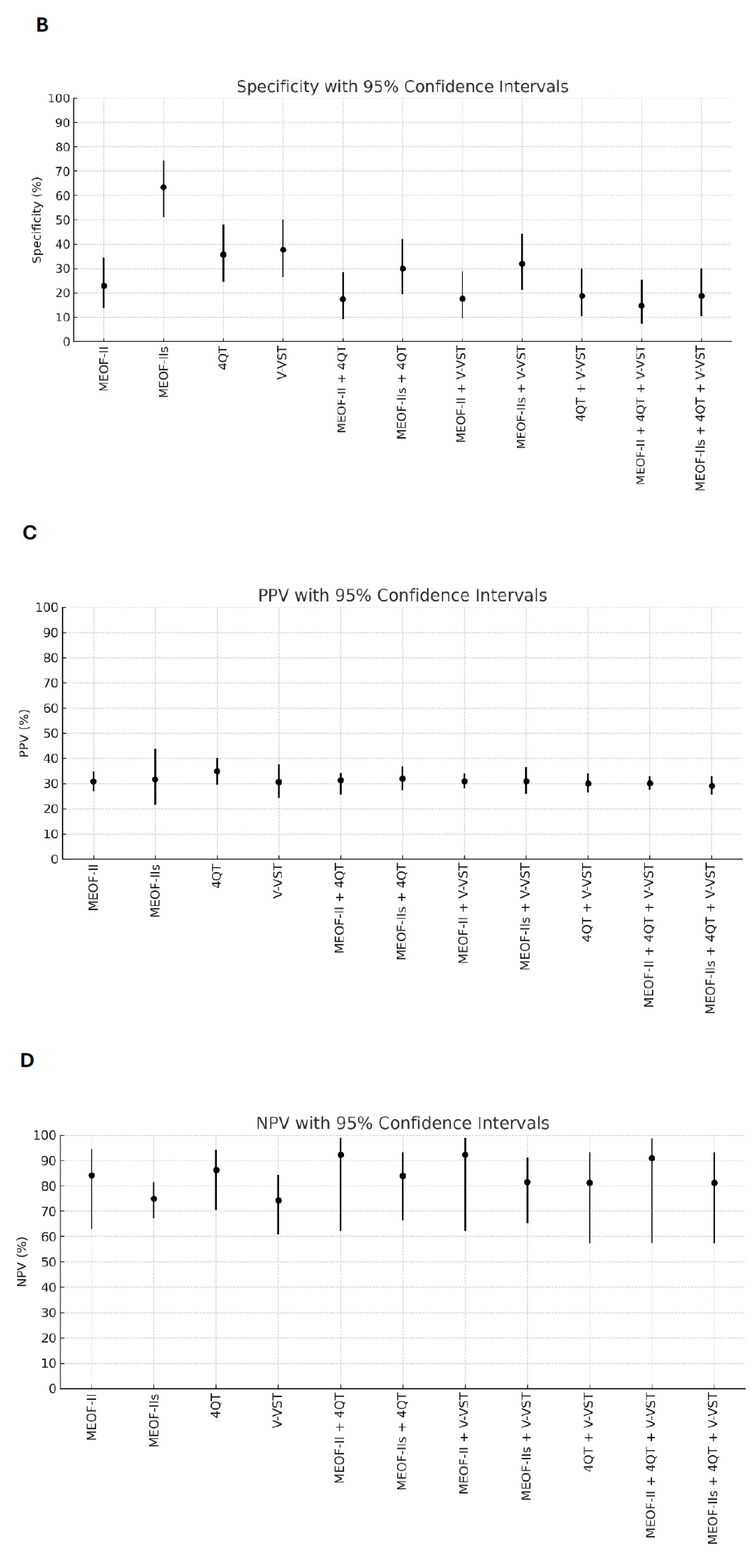
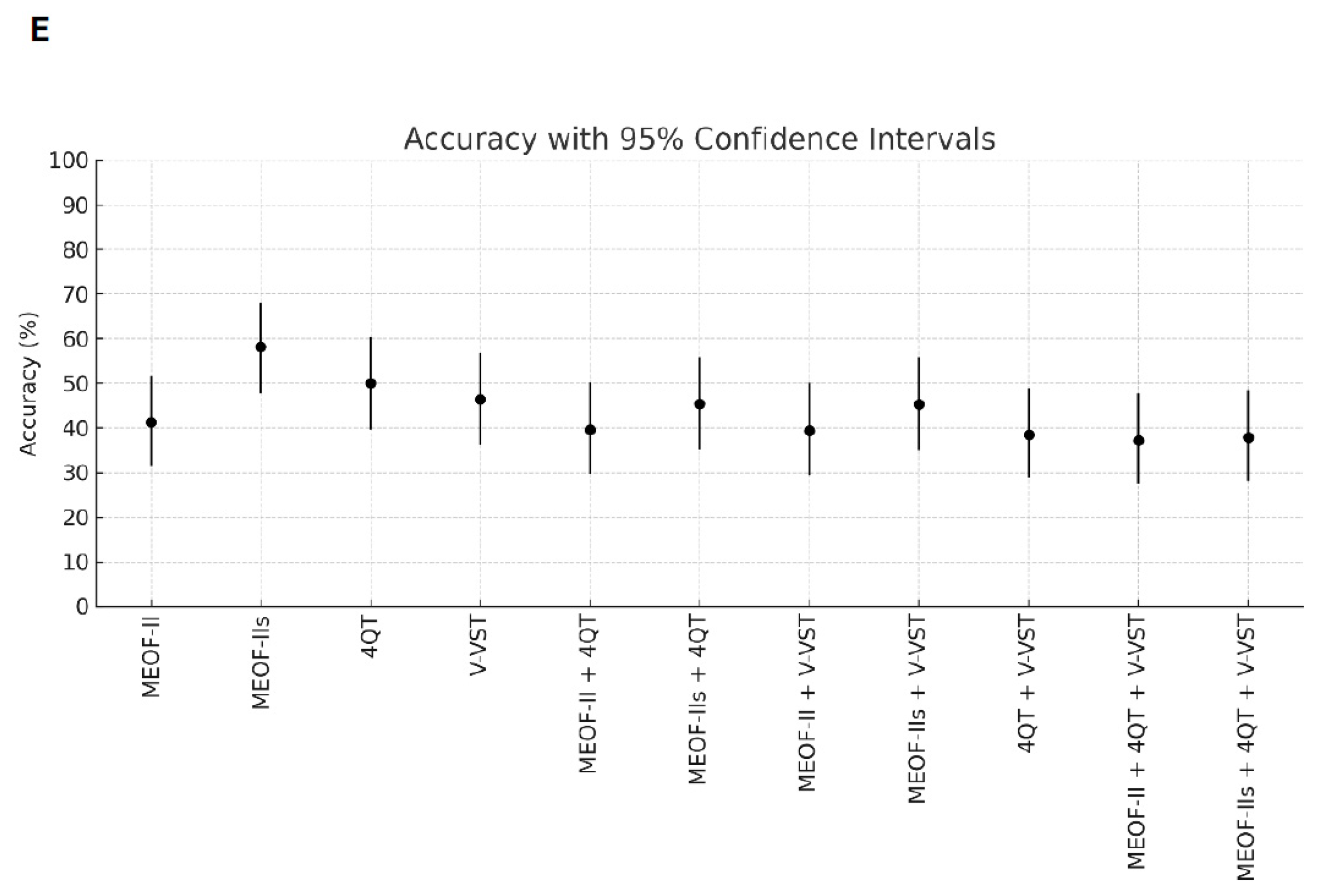
| Screening Tests | Problem Bedside | Yes, n = 27 | No, n = 70 | Sens (95% CI) | Spec (95% CI) | PPV (95% CI) | NPV (95% CI) | Accuracy (95% CI) |
| MEOF-II | Yes | 24 | 54 | 88.9 (70.8–97.6) | 22.9 (13.7–34.4) | 30.8 (27.0–34.8) | 84.2 (62.8–94.4) | 41.2 (31.3–51.7) |
| No | 3 | 16 | ||||||
| MEOF-IIs | Yes | 12 | 26 | 44.4 (25.5–64.7) | 63.4 (51.1–74.5) | 31.6 (21.5–43.7) | 75.0 (67.2–81.4) | 58.2 (47.8–68.0) |
| No | 15 | 45 | ||||||
| 4QT | Yes | 24 | 45 | 85.7 (67.3–96.0) | 35.7 (24.6–48.1) | 34.8 (29.7–40.2) | 86.2 (70.5–94.2) | 50.0 (39.7–60.3) |
| No | 4 | 25 | ||||||
| V-VST (dysphagia) | Yes | 19 | 43 | 67.9 (47.6–84.1) | 37.7 (26.3–50.2) | 30.6 (24.4–37.7) | 74.3 (60.9–84.3) | 46.4 (36.2–56.8) |
| No | 9 | 26 | ||||||
| Combined tests | ||||||||
| MEOF-II and 4QT | Yes | 26 | 57 | 96.3 (81.0–99.9) | 17.4 (9.3–28.4) | 31.3 (25.6–34.2) | 92.3 (62.1–98.9) | 39.6 (29.7–50.1) |
| No | 1 | 12 | ||||||
| MEOF-IIs and 4QT | Yes | 23 | 49 | 85.2 (66.3–95.8) | 30.0 (19.6–42.1) | 31.9 (27.4–36.9) | 84.0 (66.5–93.3) | 45.4 (35.2–55.8) |
| No | 4 | 21 | ||||||
| MEOF-II and V-VST | Yes | 25 | 56 | 96.1 (80.4–99.9) | 17.6 (9.5–28.8) | 30.9 (28.1–33.8) | 92.3 (62.1–98.9) | 39.4 (29.4–50.0) |
| No | 1 | 12 | ||||||
| MEOF-IIs and V-VST | Yes | 21 | 47 | 80.8 (60.6–93.4) | 31.9 (21.2–44.2) | 30.9 (25.9–36.4) | 81.5 (65.1–91.2) | 45.3 (35.0–55.8) |
| No | 5 | 22 | ||||||
| 4QT and V-VST | Yes | 24 | 56 | 88.9 (70.8–97.6) | 18.8 (10.4–30.1) | 30.0 (26.4–33.8) | 81.2 (57.3–93.3) | 38.5 (28.8–49.0) |
| No | 3 | 13 | ||||||
| MEOF-II, 4QT, and V-VST | Yes | 25 | 58 | 96.1 (80.4–99.3) | 14.7 (7.3–25.4) | 30.1 (27.5–32.8) | 90.9 (57.4–98.7) | 37.2 (27.5–47.8) |
| No | 1 | 10 | ||||||
| MEOF-IIs, 4QT, and V-VST | Yes | 23 | 56 | 88.4 (69.8–97.5) | 18.8 (10.4–30.1) | 29.1 (25.5–32.9) | 81.2 (57.3–93.3) | 37.9 (28.1–48.4) |
| No | 3 | 13 | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Westergren, A.; Smithard, D.; Riis, J.; Emborg, C.; Krarup, A.L.; Melgaard, D. What Combination of Generic Bedside Screening Tools Is Optimal to Capture Patients with Penetration/Aspiration Due to Dysphagia? Comparing Single Bedside Tools Versus Combinations of Tools for Sensitivity and Specificity. Geriatrics 2025, 10, 63. https://doi.org/10.3390/geriatrics10030063
Westergren A, Smithard D, Riis J, Emborg C, Krarup AL, Melgaard D. What Combination of Generic Bedside Screening Tools Is Optimal to Capture Patients with Penetration/Aspiration Due to Dysphagia? Comparing Single Bedside Tools Versus Combinations of Tools for Sensitivity and Specificity. Geriatrics. 2025; 10(3):63. https://doi.org/10.3390/geriatrics10030063
Chicago/Turabian StyleWestergren, Albert, David Smithard, Johannes Riis, Christina Emborg, Anne Lund Krarup, and Dorte Melgaard. 2025. "What Combination of Generic Bedside Screening Tools Is Optimal to Capture Patients with Penetration/Aspiration Due to Dysphagia? Comparing Single Bedside Tools Versus Combinations of Tools for Sensitivity and Specificity" Geriatrics 10, no. 3: 63. https://doi.org/10.3390/geriatrics10030063
APA StyleWestergren, A., Smithard, D., Riis, J., Emborg, C., Krarup, A. L., & Melgaard, D. (2025). What Combination of Generic Bedside Screening Tools Is Optimal to Capture Patients with Penetration/Aspiration Due to Dysphagia? Comparing Single Bedside Tools Versus Combinations of Tools for Sensitivity and Specificity. Geriatrics, 10(3), 63. https://doi.org/10.3390/geriatrics10030063








