The Safety of an Adjuvanted Autologous Cancer Vaccine Platform in Canine Cancer Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Outline and Aims
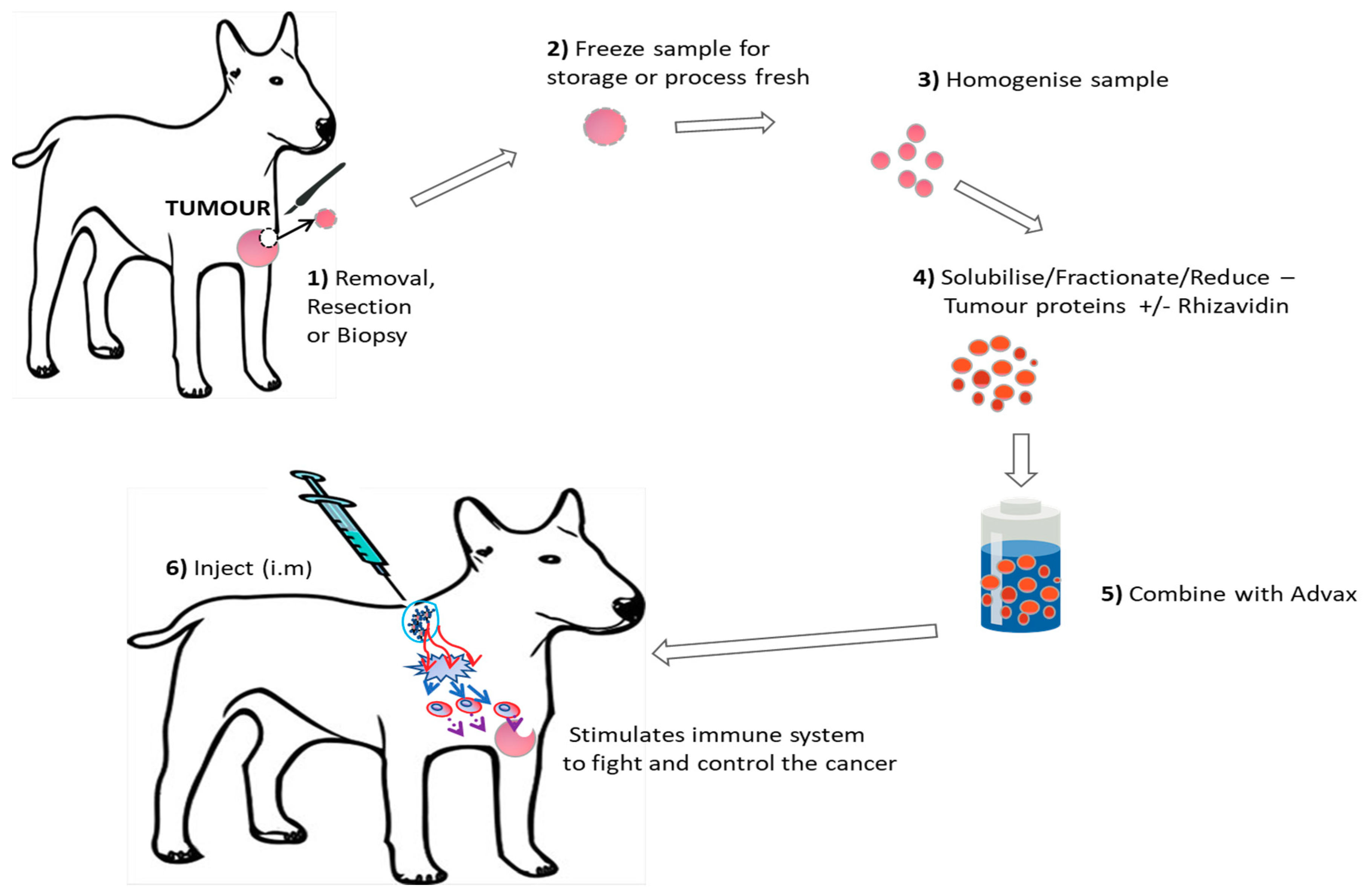
2.2. Vaccine Production
2.3. Vaccine Administration
2.4. Histopathology and Tumor Grading
2.5. Patient Status
3. Results
3.1. Treatment of Advanced Cancers with Autologous Tumor Vaccine
3.2. Vaccine Safety
3.3. Vaccine Efficacy
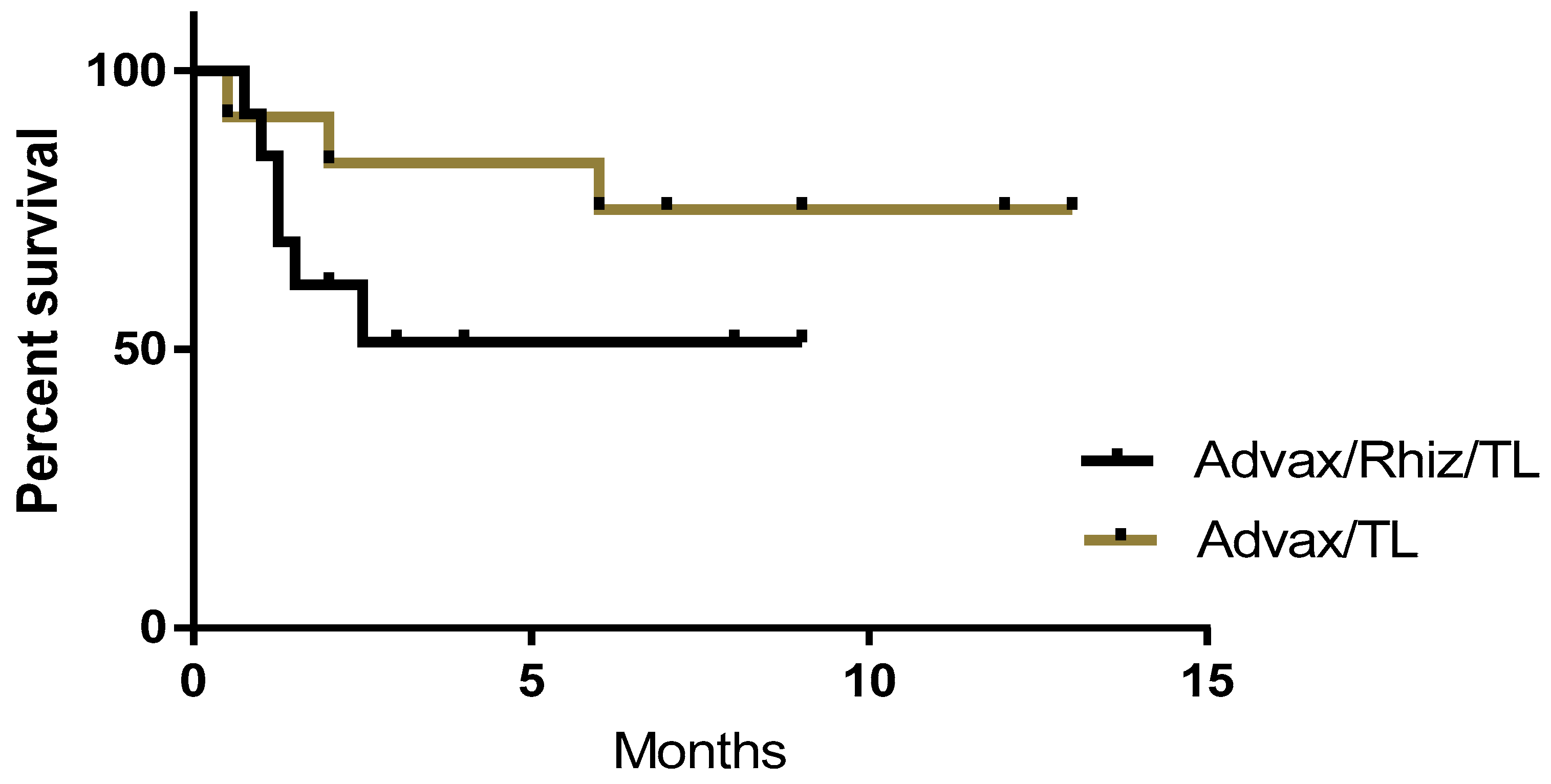
3.4. Vaccine Composition
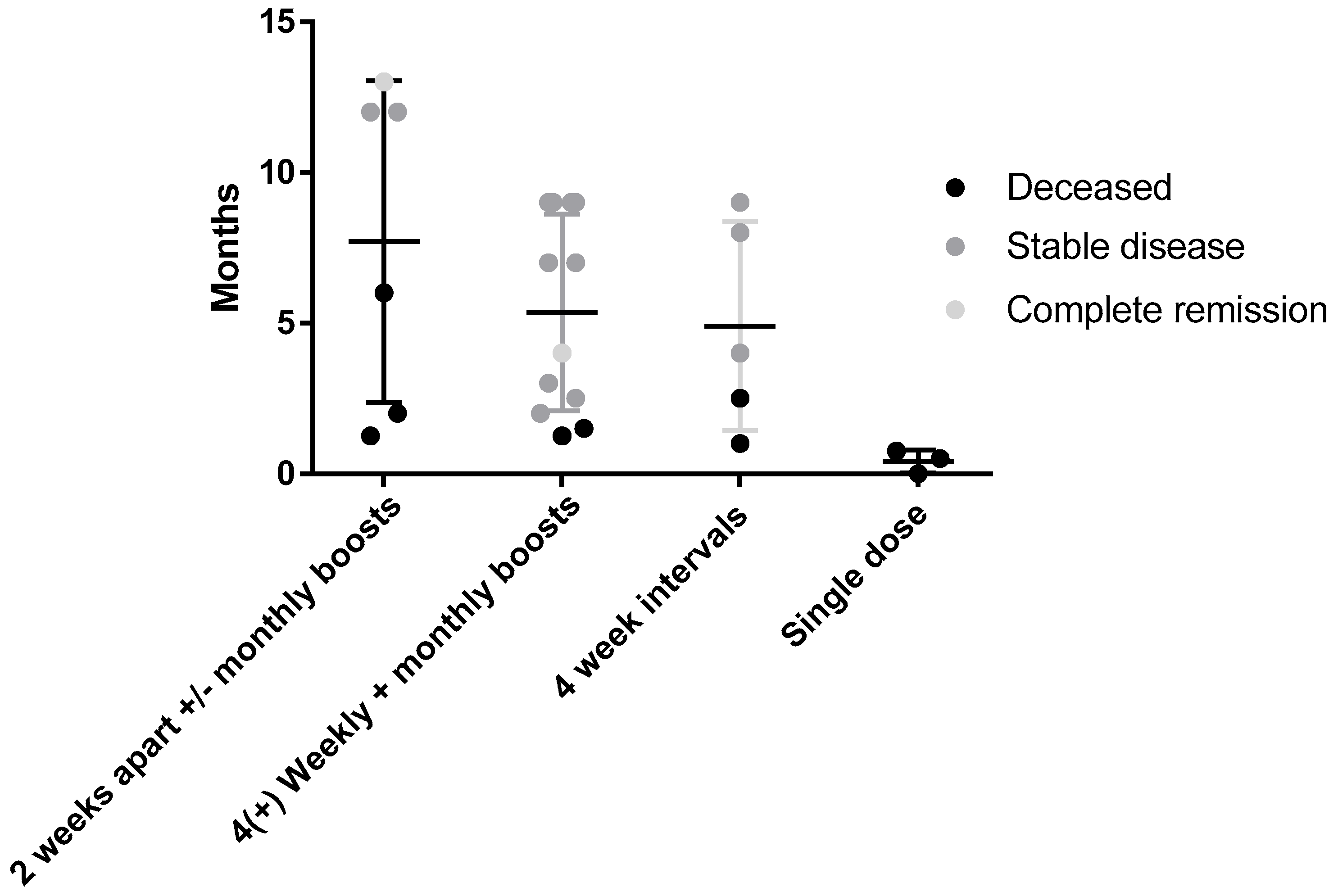
3.5. Dose Schedule
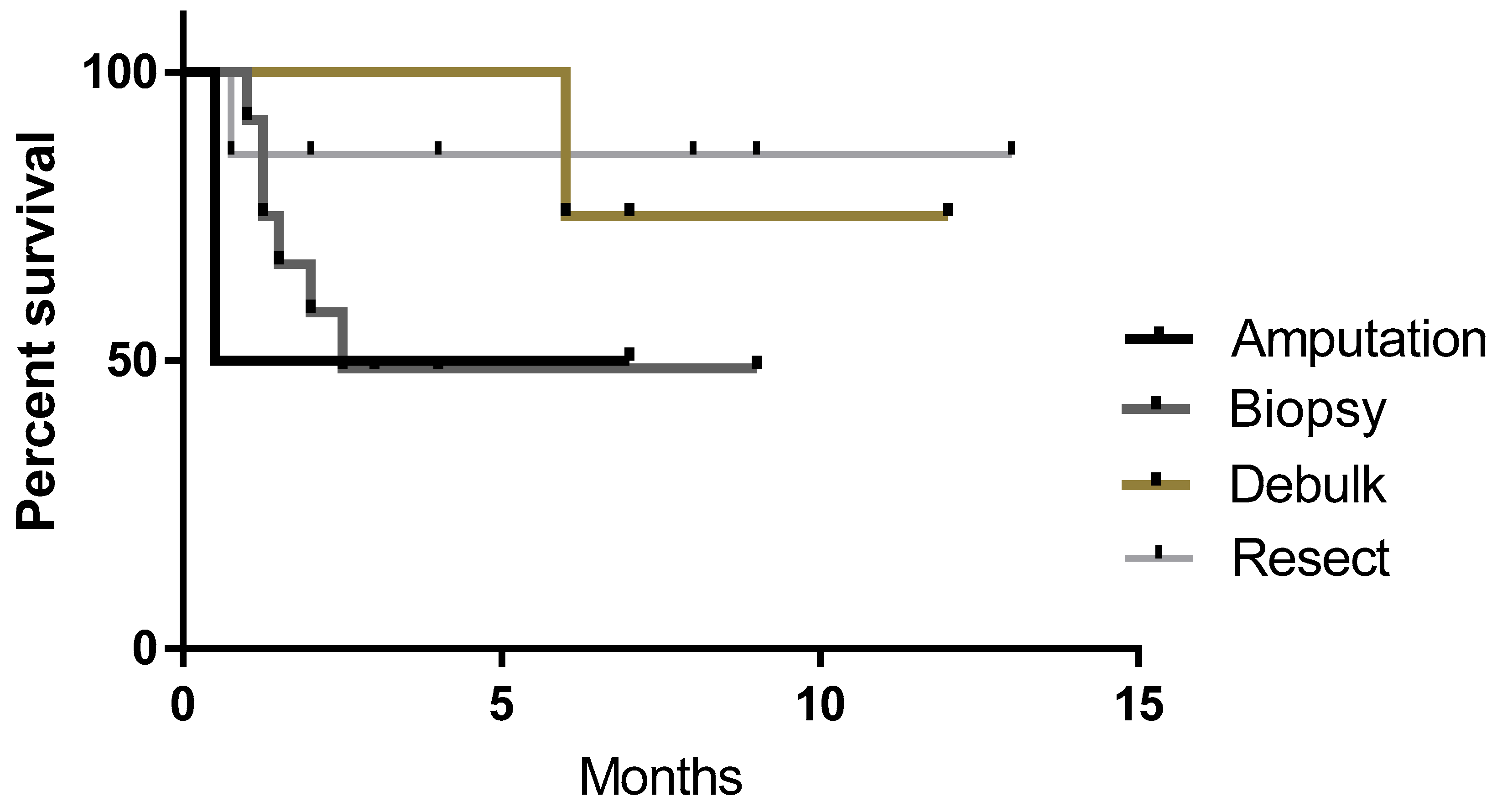
3.6. Surgery and Response
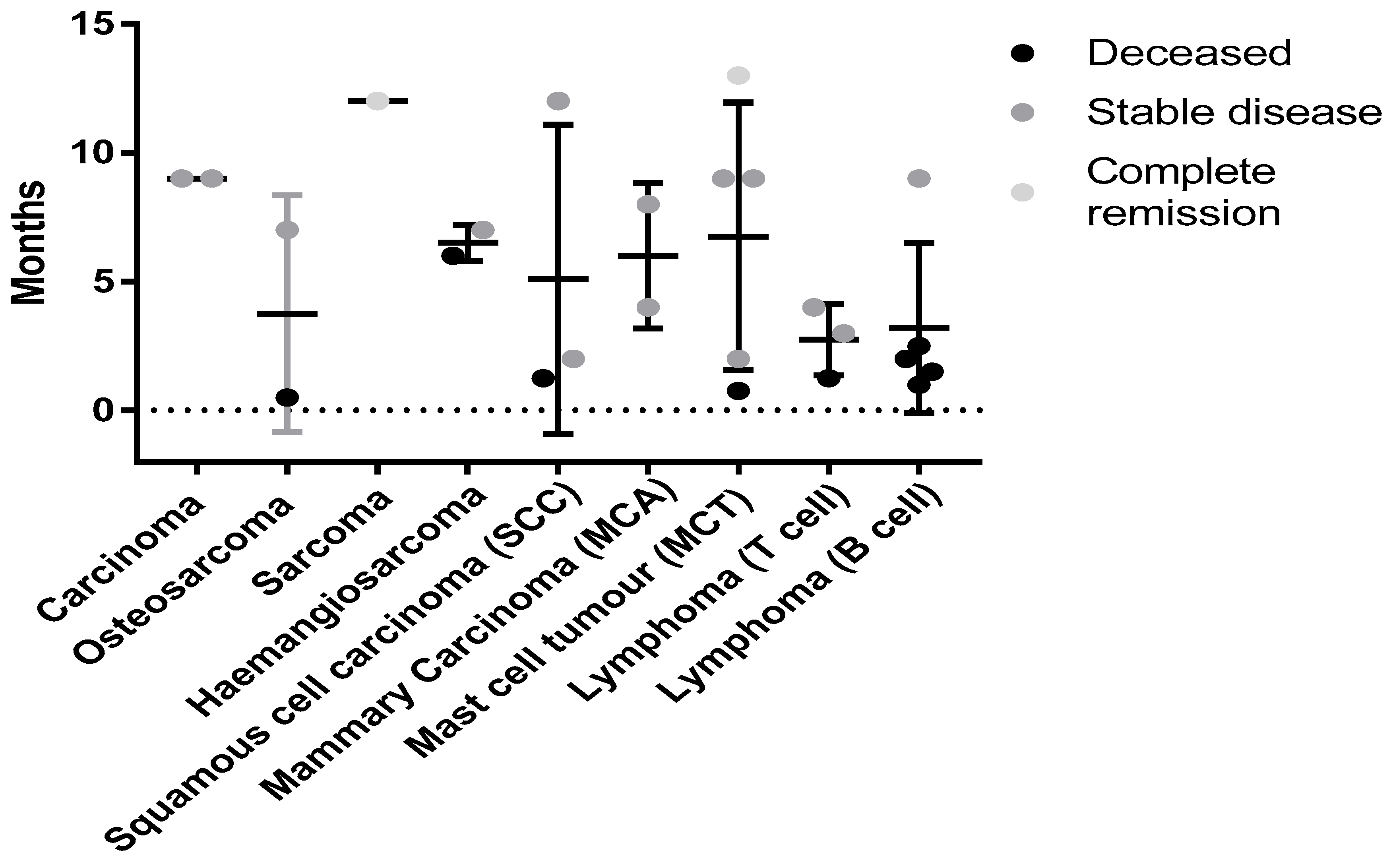
3.7. Response in Different Tumor Types
4. Discussion
5. Conclusions
6. Patents
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Aldrich, J.F.; Lowe, D.B.; Shearer, M.H.; Winn, R.E.; Jumper, C.A.; Kennedy, R.C. Vaccines and immunotherapeutics for the treatment of malignant disease. Clin. Dev. Immunol. 2010, 2010, 697158. [Google Scholar] [CrossRef] [PubMed]
- Schneider, B.; Balbas-Martinez, V.; Jergens, A.E.; Troconiz, I.F.; Allenspach, K.; Mochel, J.P. Model-Based Reverse Translation Between Veterinary and Human Medicine: The One Health Initiative. CPT Pharmacomet. Syst. Pharmacol. 2018, 7, 65–68. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, J.D.; Breen, M. Comparative oncology: What dogs and other species can teach us about humans with cancer. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2015, 370. [Google Scholar] [CrossRef] [PubMed]
- Ranieri, G.; Gadaleta, C.D.; Patruno, R.; Zizzo, N.; Daidone, M.G.; Hansson, M.G.; Paradiso, A.; Ribatti, D. A model of study for human cancer: Spontaneous occurring tumors in dogs. Biological features and translation for new anticancer therapies. Crit. Rev. Oncol. Hematol. 2013, 88, 187–197. [Google Scholar] [CrossRef] [PubMed]
- Gardner, H.L.; Fenger, J.M.; London, C.A. Dogs as a Model for Cancer. Annu. Rev. Anim. Biosci. 2016, 4, 199–222. [Google Scholar] [CrossRef] [PubMed]
- Dobson, J.M. Breed-predispositions to cancer in pedigree dogs. ISRN Vet. Sci. 2013, 2013, 941275. [Google Scholar] [CrossRef] [PubMed]
- Cullen, J.M.; Breen, M. An Overview of Molecular Cancer Pathogenesis, Prognosis, and Diagnosis. In Tumors in Domestic Animals; Meuten, D.J., Ed.; Wiley: Hoboken, NJ, USA, 2016. [Google Scholar]
- Sultan, F.; Ganaie, B.A. Comparative oncology: Integrating human and veterinary medicine. Open Vet. J. 2018, 8, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Sahin, U.; Tureci, O. Personalized vaccines for cancer immunotherapy. Science 2018, 359, 1355–1360. [Google Scholar] [CrossRef] [PubMed]
- Copier, J.; Dalgleish, A. Overview of tumor cell-based vaccines. Int. Rev. Immunol. 2006, 25, 297–319. [Google Scholar] [CrossRef] [PubMed]
- Pilla, L.; Ferrone, S.; Maccalli, C. Methods for improving the immunogenicity and efficacy of cancer vaccines. Expert Opin. Biol. Ther. 2018, 18, 765–784. [Google Scholar] [CrossRef] [PubMed]
- Godoy-Calderon, M.J.; Salazar, V.; González-Marcano, E.; Convit, A.F. Autologous tumor cells/bacillus Calmette-Guerin/formalin-based novel breast cancer vaccine induces an immune antitumor response. Oncotarget 2018, 9, 20222–20238. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mizutani, Y.; Nio, Y.; Fukumoto, M.; Yoshida, O. Effects of bacillus Calmette-Guerin on cytotoxic activities of peripheral blood lymphocytes against human T24 lined and freshly isolated autologous urinary bladder transitional carcinoma cells in patients with urinary bladder cancer. Cancer 1992, 69, 537–545. [Google Scholar] [CrossRef]
- Berry, J.; Vreeland, T.; Trappey, A.; Hale, D.; Peace, K.; Tyler, J.; Walker, A.; Brown, R.; Herbert, G.; Yi, F.; et al. Cancer vaccines in colon and rectal cancer over the last decade: Lessons learned and future directions. Expert Rev. Clin. Immunol. 2017, 13, 235–245. [Google Scholar] [CrossRef] [PubMed]
- Cheng, M.L.; Fong, L. Beyond sipuleucel-T: Immune approaches to treating prostate cancer. Curr. Treat. Options Oncol. 2014, 15, 115–126. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lee, A.; Sun, S.; Sandler, A.; Hoang, T. Recent progress in therapeutic antibodies for cancer immunotherapy. Curr. Opin. Chem. Biol. 2018, 44, 56–65. [Google Scholar] [CrossRef] [PubMed]
- Son, C.H.; Bae, J.H.; Shin, D.Y.; Lee, H.R.; Choi, Y.J.; Jo, W.S.; Jung, M.H.; Kang, C.D.; Yang, K.; Park, Y.S. CTLA-4 blockade enhances antitumor immunity of intratumoral injection of immature dendritic cells into irradiated tumor in a mouse colon cancer model. J. Immunother. 2014, 37, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Soares, K.C.; Rucki, A.A.; Wu, A.A.; Olino, K.; Xiao, Q.; Chai, Y.; Wamwea, A.; Bigelow, E.; Lutz, E.; Liu, L.; et al. PD-1/PD-L1 blockade together with vaccine therapy facilitates effector T-cell infiltration into pancreatic tumors. J. Immunother. 2015, 38, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Hailemichael, Y.; Woods, A.; Fu, T.; He, Q.; Nielsen, M.C.; Hasan, F.; Roszik, J.; Xiao, Z.; Vianden, C.; Khong, H.; et al. Cancer vaccine formulation dictates synergy with CTLA-4 and PD-L1 checkpoint blockade therapy. J. Clin. Investig. 2018, 128, 1338–1354. [Google Scholar] [CrossRef] [PubMed]
- Petrovsky, N.; Cooper, P.D. Advax, a novel microcrystalline polysaccharide particle engineered from delta inulin, provides robust adjuvant potency together with tolerability and safety. Vaccine 2015, 33, 5920–5926. [Google Scholar] [CrossRef] [PubMed]
- Larena, M.; Prow, N.A.; Hall, R.A.; Petrovsky, N.; Lobigs, M. JE-ADVAX vaccine protection against Japanese encephalitis virus mediated by memory B cells in the absence of CD8(+) T cells and pre-exposure neutralizing antibody. J. Virol. 2013, 87, 4395–4402. [Google Scholar] [CrossRef] [PubMed]
- Lobigs, M.; Pavy, M.; Hall, R.A.; Lobigs, P.; Cooper, P.; Komiya, T.; Toriniwa, H.; Petrovsky, N. An inactivated Vero cell-grown Japanese encephalitis vaccine formulated with Advax, a novel inulin-based adjuvant, induces protective neutralizing antibody against homologous and heterologous flaviviruses. J. Gen. Virol. 2010, 91 Pt 6, 1407–1417. [Google Scholar] [CrossRef]
- Petrovsky, N.; Larena, M.; Siddharthan, V.; Prow, N.A.; Hall, R.A.; Lobigs, M.; Morrey, J. An inactivated cell culture Japanese encephalitis vaccine (JE-ADVAX) formulated with delta inulin adjuvant provides robust heterologous protection against West Nile encephalitis via cross-protective memory B cells and neutralizing antibody. J. Virol. 2013, 87, 10324–10333. [Google Scholar] [CrossRef] [PubMed]
- Saade, F.; Honda-Okubo, Y.; Trec, S.; Petrovsky, N. A novel hepatitis B vaccine containing Advax, a polysaccharide adjuvant derived from delta inulin, induces robust humoral and cellular immunity with minimal reactogenicity in preclinical testing. Vaccine 2013, 31, 1999–2007. [Google Scholar] [CrossRef] [PubMed]
- Honda-Okubo, Y.; Saade, F.; Petrovsky, N. Advax, a polysaccharide adjuvant derived from delta inulin, provides improved influenza vaccine protection through broad-based enhancement of adaptive immune responses. Vaccine 2012, 30, 5373–5381. [Google Scholar] [CrossRef] [PubMed]
- Cristillo, A.D.; Ferrari, M.G.; Hudacik, L.; Lewis, B.; Galmin, L.; Bowen, B.; Thompson, D.; Petrovsky, N.; Markham, P.; Pal, R. Induction of mucosal and systemic antibody and T-cell responses following prime-boost immunization with novel adjuvanted human immunodeficiency virus-1-vaccine formulations. J. Gen. Virol. 2011, 92 Pt 1, 128–140. [Google Scholar] [CrossRef]
- McPherson, C.; Chubet, R.; Holtz, K.; Honda-Okubo, Y.; Barnard, D.; Cox, M.; Petrovsky, N. Development of a SARS Coronavirus Vaccine from Recombinant Spike Protein Plus Delta Inulin Adjuvant. Methods Mol. Biol. 2016, 1403, 269–284. [Google Scholar] [PubMed]
- Rodriguez-Del Rio, E.; Marradi, M.; Calderon-Gonzalez, R.; Frande-Cabanes, E.; Penadés, S.; Petrovsky, N.; Alvarez-Dominguez, C. A gold glyco-naoparticle carrying a Listeriolysin O peptide and formulated with Advax delta inulin adjuvant induces robust T-cell protection against listeria infection. Vaccine 2015, 33, 1465–1473. [Google Scholar] [CrossRef] [PubMed]
- Feinen, B.; Petrovsky, N.; Verma, A.; Merkel, T.J. Advax-adjuvanted recombinant protective antigen provides protection against inhalational anthrax that is further enhanced by addition of murabutide adjuvant. Clin. Vaccine Immunol. 2014, 21, 580–586. [Google Scholar] [CrossRef] [PubMed]
- Davtyan, H.; Zagorski, K.; Rajapaksha, H.; Hovakimyan, A.; Davtyan, A.; Petrushina, I.; Kazarian, K.; Cribbs, D.H.; Petrovsky, N.; Agadjanyan, M.G.; et al. Alzheimer’s disease Advax(CpG)-adjuvanted MultiTEP-based dual and single vaccines induce high-titer antibodies against various forms of tau and Abeta pathological molecules. Sci. Rep. 2016, 6, 28912. [Google Scholar] [CrossRef] [PubMed]
- Gordon, D.; Kelley, P.; Heinzel, S.; Cooper, P.; Petrovsky, N. Immunogenicity and safety of Advax, a novel polysaccharide adjuvant based on delta inulin, when formulated with hepatitis B surface antigen: A randomized controlled Phase 1 study. Vaccine 2014, 32, 6469–6477. [Google Scholar] [CrossRef] [PubMed]
- Gordon, D.L.; Sajkov, D.; Woodman, R.J.; Honda-Okubo, Y.; Cox, M.M.; Heinzel, S.; Petrovsky, N. Randomized clinical trial of immunogenicity and safety of a recombinant H1N1/2009 pandemic influenza vaccine containing Advax polysaccharide adjuvant. Vaccine 2012, 30, 5407–5416. [Google Scholar] [CrossRef] [PubMed]
- Heddle, R.; Russo, P.; Petrovsky, N.; Hanna, R.; Smith, A. Immunotherapy—2076. A controlled study of delta inulin-adjuvanted honey bee venom immunotherapy. World Allergy Organ. J. 2013, 6, P158. [Google Scholar] [CrossRef]
- Helppolainen, S.H.; Nurminen, K.P.; Määttä, J.A.; Halling, K.K.; Slotte, J.P.; Huhtala, T.; Liimatainen, T.; Ylä-Herttuala, S.; Airenne, K.J.; Närvänen, A.; et al. Rhizavidin from Rhizobium etli: The first natural dimer in the avidin protein family. Biochem. J. 2007, 405, 397–405. [Google Scholar] [CrossRef] [PubMed]
- Weir, C.; Hudson, A.L.; Moon, E.; Ross, A.; Alexander, M.; Peters, L.; Langova, V.; Clarke, S.J.; Pavlakis, N.; Davey, R.; et al. Streptavidin: A novel immunostimulant for the selection and delivery of autologous and syngeneic tumor vaccines. Cancer Immunol. Res. 2014, 2, 469–479. [Google Scholar] [CrossRef] [PubMed]
- Valli, V.E.; Myint, M.S.; Barthel, A.; Bienzle, D.; Caswell, J.; Colbatzky, F.; Durham, A.; Ehrhart, E.J.; Johnson, Y.; Jones, C.; et al. Classification of canine malignant lymphomas according to the World Health Organization criteria. Vet. Pathol. 2011, 48, 198–211. [Google Scholar] [CrossRef] [PubMed]
- Kiupel, M.; Webster, J.D.; Bailey, K.L.; Best, S.; DeLay, J.; Detrisac, C.J.; Fitzgerald, S.D.; Gamble, D.; Ginn, P.E.; Goldschmidt, M.H.; et al. Proposal of a 2-tier histologic grading system for canine cutaneous mast cell tumors to more accurately predict biological behavior. Vet. Pathol. 2011, 48, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Goldschmidt, M.; Peña, L.; Rasotto, R.; Zappulli, V. Classification and grading of canine mammary tumors. Vet. Pathol. 2011, 48, 117–131. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, S.M.; Thamm, D.H.; Vail, D.M.; London, C.A. Response evaluation criteria for solid tumours in dogs (v1.0): A Veterinary Cooperative Oncology Group (VCOG) consensus document. Vet. Comp. Oncol. 2015, 13, 176–183. [Google Scholar] [CrossRef] [PubMed]
- Group, V.C.O. Veterinary cooperative oncology group—Common terminology criteria for adverse events (VCOG-CTCAE) following chemotherapy or biological antineoplastic therapy in dogs and cats v1.1. Vet. Comp. Oncol. 2011, 14, 417–446. [Google Scholar]
- Kiupel, M. Special focus: Diagnosis and prognosis of neoplastic diseases in companion animals. Vet. Pathol. 2011, 48, 6. [Google Scholar] [CrossRef] [PubMed]
- Rowell, J.L.; McCarthy, D.O.; Alvarez, C.E. Dog models of naturally occurring cancer. Trends Mol. Med. 2011, 17, 380–388. [Google Scholar] [CrossRef] [PubMed]
| Tumour Type | Stage/Grade/Location | Breed/Sex/Age | Sample size | Vaccine Composition | Vaccine doses | Survival time | Status | Medication/Observations |
|---|---|---|---|---|---|---|---|---|
| Diffuse large B-cell lymphoma (DLBCL) | stage IIIB | American Staffordshire Bullterrier (M5) | Biopsy 1.2 g | Advax/Rhiz/TL | 2 (4 weeks apart) | 10 weeks | Euthanased | Prednisolone 1 mg/kg BID |
| stage V | Australian Kelpie X (FN 10) | Biopsy 1.4 g | 2 (4 weeks apart) | 4 weeks | Euthanased | Prednisolone 1 mg/kg BID | ||
| stage V | Japanese Spitz X (MN 5) | Biopsy 1.4 g | 4 (weekly) | 6 weeks | Euthanased | Prednisolone 1 mg/kg BID | ||
| Mammary carinoma (MCA) | Bernese Mountain Dog (F10) | Resection 1.6 g | 8 (4 weeks apart) | Still alive 8 months | New cancer | New, unrelated malignant tumour developed 7 months after starting vaccination | ||
| Australian Cattle dog X (F13) | Resection 1.3 g | 4 (4 weeks apart) | Still alive 4 months | New cancer | Histopathology pending on new cancer, might start vaccines again. New cancer 3 months after starting vaccination | |||
| Mast Cell tumour (MCT) | high grade (multiple tumours) | Golden Retriever (FN7) | Resection 1 g | 5 (initially weekly × 4, then 4 weeks apart) | Still alive 2 months | CR | Had curative intent surgery for MCT recurrence and multiple new lesions. | |
| high grade | Rhodesian Ridgeback X (MN9) | Biopsy 0.6 g | 9 (4 weeks apart) | Still alive 9 months | SD | Tumour no progression in size, no metastases | ||
| high grade (multiple + mets in draining lymph nodes) | Staffordshire Bullterrier (M8) | Resection 1.1 g | 1 | 3 weeks | Euthanased | Ranitidine 2 mg/kg BID, chlorpheniramine 8 mg BID | ||
| Non-epitheliotrophic T-cell lymphoma | Rottweiler (MN3) | Biopsy 0.6 g | 11 (initially weekly, then 4 weeks apart) | Still alive 4 months | CR | No other medications, no lesions currently, 12 at beginning of vaccination | ||
| Epitheliotrophic T-cell lymphoma | Boxer (MN13) | Biopsy 0.5 g | 9 (weekly, a bit random) | Still alive 3 months | SD | Some lesions have disappeared, but there are new ones also | ||
| Labrador (MN11) | Biopsy 0.7 g | 6 (weekly) | 5 weeks | Euthanased | Went into complete remission with CCNU chemo but developed hepatopathy. Concurrent Prednisolone 0.75 mg/kg SID. PD | |||
| Squamous cell carcinoma (SCC) | oral | Shih Tzu X (MN12) | Biopsy 0.6 g | 5 (initially weekly × 4, then 4 weeks apart) | Still alive 2 months | SD | Has undiagnosed masses in liver, adrenal and lungs | |
| oral | Cross breed (MN10) | Biopsy (0.1 g) | 2 | 5 weeks | Euthanased | Unrelated causes | ||
| Soft tissue sarcoma (STS) | shoulder | Maltese Terrier (MN13) | Resection | Advax 2/Rhiz/TL | 2 (2 weeks apart) | Unknown | LTFU | Owners uncontactable |
| Squamous cell carcinoma | left tonsil | Cross breed (MN8) | Multiple biopsies (0.36 g) | 4 (2 × 2 weeks apart) then monthly | Unknown | LTFU | Owners uncontactable | |
| Lymphoma (B cell) | multiple nodes | Terrier cross (MN11) | Biopsy (0.26 g) | Advax/TL | 2 doses 2 weeks apart | 2 months | Euthanased | Relapse |
| multiple nodes | Groodle X (FN2.5) | Biopsy 0.4 g | 4 × 1 weekly then monthly boosts | Still Alive 9 months | SD | Had prednisone initially | ||
| Mast Cell tumour | Low grade | Labrador (FN12) | Resection 7.27 g | > 4 doses—2 × 2 weekly then monthly | Still Alive 13 months | CR | No recurrance sice vaccination | |
| grade 3 neck | Beagle (FN10) | 0.3 g Incomplete Resection | 4 × 1 weekly then monthly boosts | Still Alive 9 months | SD | No tumour progression | ||
| Haemangiosarcoma | nasal | Staffordshire Bull terrier (MN9) | Debulk (0.6 g) | 4 doses—2 × 2 weekly then Monthly | 6 months | Euthanased | Aggressive disease | |
| spleenic | German Shepherd X (FN9) | Debulk > 1 g | 4 × 1 weekly then monthly boosts | Still Alive 7 months | SD | Stable disease exceeding expectations | ||
| Squamous cell Carcinoma | nasal | Alaskan Malamute (MN9) | Debulk 1.6 g | > 4 doses—2 × 2 weekly then monthly | Still Alive 12 months | SD | Still residual disease | |
| Sarcoma | grade 1 nose | Australian Terrier (MN12) | Debulk 1 g | > 4 doses—2 × 2 weekly then monthly | Still Alive 12 months | SD | Radiotherapy as well (stable disease) | |
| Osteosarcoma | grade 3 | Pyrenean Mt Dog (MN12) | 0.5 g Amputation | 1 dose | 2 weeks | Euthanased | Complications from Surgery | |
| grade 3 (MI 15) | Labrador (MN10) | Amputation 0.1 g biopsy | 4 × 1 weekly then monthly boosts | Still Alive 7 months | SD | Sample depleted for vaccine production | ||
| Carcinoma | primary (right hind leg) + lymph node (mets) | Springer Spaniel (MN11) | 0.6 g Resect | 4 × 1 weekly then monthly boosts | Still Alive 9 months | SD | Stable even with metastatic disease | |
| Hepatocelluar Carcinoma | liver + lipoma on outer sections | Border Collie X (MN12) | Biopsy < 0.1 g | 4 × 1 weekly then monthly boosts | Still Alive 9 months | SD | Sample depleted for vaccine production |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Weir, C.; Oksa, A.; Millar, J.; Alexander, M.; Kynoch, N.; Walton-Weitz, Z.; Mackenzie-Wood, P.; Tam, F.; Richards, H.; Naylor, R.; et al. The Safety of an Adjuvanted Autologous Cancer Vaccine Platform in Canine Cancer Patients. Vet. Sci. 2018, 5, 87. https://doi.org/10.3390/vetsci5040087
Weir C, Oksa A, Millar J, Alexander M, Kynoch N, Walton-Weitz Z, Mackenzie-Wood P, Tam F, Richards H, Naylor R, et al. The Safety of an Adjuvanted Autologous Cancer Vaccine Platform in Canine Cancer Patients. Veterinary Sciences. 2018; 5(4):87. https://doi.org/10.3390/vetsci5040087
Chicago/Turabian StyleWeir, Chris, Annika Oksa, Jennifer Millar, Miles Alexander, Nicola Kynoch, Zoe Walton-Weitz, Peter Mackenzie-Wood, Felicia Tam, Hope Richards, Richard Naylor, and et al. 2018. "The Safety of an Adjuvanted Autologous Cancer Vaccine Platform in Canine Cancer Patients" Veterinary Sciences 5, no. 4: 87. https://doi.org/10.3390/vetsci5040087
APA StyleWeir, C., Oksa, A., Millar, J., Alexander, M., Kynoch, N., Walton-Weitz, Z., Mackenzie-Wood, P., Tam, F., Richards, H., Naylor, R., Cheng, K., Bennett, P., Petrovsky, N., & Allavena, R. (2018). The Safety of an Adjuvanted Autologous Cancer Vaccine Platform in Canine Cancer Patients. Veterinary Sciences, 5(4), 87. https://doi.org/10.3390/vetsci5040087







