One Health Ethics and the Ethics of Zoonoses: A Silent Call for Global Action
Abstract
Simple Summary
Abstract
1. Introduction: Incremental Risks of Zoonotic Diseases
2. Zoonoethics, Global Bioethics, and One Health: We Need “One Bioethics”?
- (i)
- Primary prevention: zoonoethics, in close collaboration with the One Health ethics [29,30,139,158,159,160,161], can offer descriptive and epistemic resources for transforming our understanding of and interconnections with nonhuman beings and environments (both natural and built), as well as for clarifying our relationships with them. Primary prevention aims to anticipate risks before they become fully manifest. As Plowright et al. [162] (p. 2) show: “Primary pandemic prevention is the set of actions taken to reduce the risk of pathogen spillover from animals to humans, focusing on processes upstream of the spillover event”. The first preventive measure to reduce zoonotic risks and the spread of viruses with pandemic potential is to practice ecological wisdom related to the holistic protection of species and the care of the biodiversity of ecosystem hotspots. As highlighted by Vora et al. [163] (p. 420), “tropical and subtropical forests must be protected”.
- (ii)
- Secondary prevention: Primary prevention is, by definition, anticipatory, while secondary prevention focuses on the implementation of specific measures, such as early detection, vaccines, improved health systems, and drug therapy, but these are established in the ongoing process of preventing the outbreak from becoming an epidemic or pandemic [164,165]. At this stage, zoonoethics can provide a framework for setting standards and guiding policymakers on what actions are most effective, fair, and ethically relevant to prevent the escalation of the outbreak. One of the paradoxes of primary prevention is that it is largely undervalued as an effective strategy for responding to pandemic risks, while the great paradox of secondary prevention is that many interventions focus on implementing public health measures that may have adverse effects in order to contain the spread of spillover. However, there is sufficient evidence to support the idea that the most cost-effective, wise, and politically relevant strategy for preventing future pandemics is to invest in prevention and capacity building in the context of future sustainability [2,20,166,167].
- (iii)
- Antimicrobial Stewardship (AMS): Zoonoethics can help to address the problems associated with antimicrobial resistance and to develop a more robust and comprehensive approach to AMS [168,169,170]. As Shallcross et al. [76] (p. 4) stresses: “If AMR is allowed to continue unchecked, we may enter a ‘post-antibiotic era’ of medicine, in which treatments from minor surgery to major transplants could become impossible, mortality will rise, and healthcare costs will spiral as we resort to newer, more expensive antibiotics and sustain a greater number of longer hospital admissions”. AMS is an ethical approach that takes very seriously the growing threat of entering a “post-antibiotic era”. Curbing the emergence and spread of these resistant organisms and agents is a high priority not only in epidemiological surveillance and drug development programs but also in inclusive public policies aimed at reducing inequities in access to safe and affordable medicines for all. As Dyar et al. [171] (p. 793) states: “Although antimicrobial stewardship originated within human healthcare, it is increasingly applied in broader contexts including animal health and One Health”. Experts in zoonoethics can significantly contribute to the efforts of antimicrobial stewardship (AMS) in addressing this issue. Zoonoethics can provide valuable insights and frameworks that can enhance the AMS strategies across different domains—animal health, human health, agriculture, and livestock. Firstly, zoonoethics emphasizes the interconnectedness of ecosystems and the ethical considerations that arise from this interconnectedness. By integrating zoonoethics principles, AMS experts can develop more holistic policies that consider the welfare of all species affected by antimicrobial use. This approach aligns with the One Health perspective, which recognizes the interdependence of human, animal, and environmental health. Moreover, zoonoethics can offer tools such as ethical risk assessments and value-based decision-making frameworks. These tools enable stakeholders to evaluate the implications of antimicrobial use and resistance not only from a scientific standpoint but also through an ethical lens, considering the long-term consequences for all species. For instance, ethical risk assessments can help identify practices that may inadvertently contribute to AMR and propose alternatives that are ethically and ecologically sound. My perspective on the problem of antimicrobial resistance is enriched by the multispecies justice approach, which seeks to integrate other species and wildlife into risk analyses [172,173,174].
3. The Ethical Dilemmas of One Health: The Case of Animal Slaughter, Outline of One-Zoonoethics
| Guideline | Description | Problem/Challenge | Authors |
|---|---|---|---|
| 1. Develop Alternatives to Culling | Invest in research and development of alternatives to animal culling, such as vaccination or quarantine measures. | Reducing the need for mass culling and minimizing harm to animal populations. | [261,276] |
| 2. Strengthen Ethical Review Processes | Implement stringent ethical review processes for animal culling decisions, ensuring consideration of multispecies justice and ecological impacts. | Ensuring ethical considerations are thoroughly evaluated before making culling decisions. | [137,247] |
| 3. Surveillance and Monitoring | Establish systems for early detection and tracking of zoonotic diseases to respond quickly and effectively. | Timely detection and response to emerging zoonotic diseases. | [18,111,163,277] |
| 4. Research and Development | Promote interdisciplinary research and develop new vaccines and treatments to combat zoonotic diseases. | Addressing gaps in knowledge and developing effective interventions. | [278,279] |
| 5. One Health Education and Ecological Awareness | Incorporate OH core competencies and strengthening educational programs, including zoonoethics and AMR ethics for children, youth, and future professionals across the curriculum. | Increasing public understanding and engagement in zoonosis prevention. | [280,281,282,283,284] |
| 6. Policies and Regulations | Create and enforce regulations to manage human–animal interactions and support sustainable practices. | Implementing bioethical and legal frameworks to prevent zoonotic disease transmission. | [19,20,285,286] |
| 7. Ethical Disaster Management and Global Cooperation | Develop and implement ethical guidelines and rapid response plans for health crises and natural disasters, protecting animal welfare and preventing zoonotic outbreaks. | Ensure preparedness, minimize harm, and respond ethically to zoonotic outbreaks during crises. | [150,287,288,289,290] |
| 8. Open Science for Future Pandemic Resilience | Develop future-oriented OH policies that enhance data analysis capabilities to understand disease dynamics and ensure the availability, quality, and management of accurate data for evidence-based decision-making. | Open science can greatly enhance OH pandemic responses by enabling rapid data sharing and collaboration. | [291,292] |
| 9. Engage Local and Indigenous Communities | Engage local communities in zoonosis prevention and control, while fostering intercultural dialogue by integrating indigenous perspectives into One Health. | Ensuring local communities have a voice and active role in zoonosis prevention efforts in all levels. | [293,294,295] |
| 10. Sustainable and Resilient Health Systems (SRHS) | Health systems need to develop new capacities and build synergies with other sectors and organizations to address risks of ERIDs. | Build better, more climate-resilient and environmentally sustainable health systems. | [296,297,298] |
| 11. Enhance Biosecurity Measures | Implement comprehensive biosecurity protocols in intensive farming operations, including regular health monitoring and rapid response plans. | Preventing the spread of infectious diseases within and between animal populations to avoid large-scale outbreaks. | [55,164,298] |
| 12. Promote Sustainable and One Welfare Farming Practices | Encourage sustainable and farming practices guided by interspecies ethics, reducing animal density and improving living conditions to lower disease risk. | Mitigating the conditions that facilitate the spread of zoonotic diseases in high-density farming and livestock. | [299,300] |
4. Antimicrobial Resistance at the Human–Animal–Environment Interfaces: A Call for Global Action to Face the Antimicrobial Resistance (AMR)
5. Zoonoethics, Intercultural Dialogue, and Entangled Empathy: A Silent Call for Interspecies Solidarity
6. A Call for Urgent Action: Policy Recommendations for an Inclusive, Intercultural, and Gender-Sensitive One Health Approach
- Advance international legislation to recognize the international crime of ecocide and crimes against biodiversity, not only as circumscribed and peripheral damages that affect human health but as damages that affect the health of humans, animals, and environments and constitute an attack against future generations.
- Stop the illegal wildlife trade, the slaughter of wild animals in wet markets, and the illegal timber trade in tropical forests, especially in areas of high biodiversity in Asia, Africa, and the Americas. This requires deepening the partnership against wildlife crime and developing new intercultural capacities to reconnect human and nonhuman animals, places, and the planet.
- We need closer transdisciplinary collaboration, including gender and intercultural perspectives, to study the socioeconomic, cultural, and environmental determinants and drivers of zoonotic diseases: “Developing a multi-sectoral preparedness and response plans for control of zoonotic diseases through a comprehensive risk assessment, improving laboratory diagnostic capacities, joint surveillance activities at the animal-human interface” [111,350].
- Strengthen political commitment, national planning, and regional coordination mechanisms; this requires working towards a One Health approach based on principles of intersectionality, interculturality and global solidarity. These plans and long-term strategies should be evaluated from a complexity approach at the local, regional, and global levels [66,288,290].
- Promote equitable and long-term synergies between Western health systems and local and indigenous community health knowledge systems and practices. Additionally, we need to create innovative strategies and establish regional and global information networks to facilitate knowledge sharing and enhance collaborative efforts to manage risks across the various interfaces of One Health. In particular, the wildlife–livestock–human interface is one of the areas of greatest risk and vulnerability.
- Promoting a One Digital Health approach: Europe, the United States, and other high-income countries have strong epidemiological surveillance systems that provide access to comprehensive data, tables, and maps on infectious diseases, but low- and middle-income countries in regions such as South and Central Asia, Africa, and Central and South America do not yet have robust surveillance systems to develop systemic preparedness, mitigation, and prevention plans and strategies for zoonotic diseases.
- One of the challenges highlighted by the COVID-19 pandemic was the need to work together across sectors and regions to develop greater North–South synergies of cooperation, equity, and multispecies justice to lay the foundations for a sustainable One Health system based on a broad vision of health, common goods, and eco-solidarity.
7. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Horefti, E. The Importance of the One Health Concept in Combating Zoonoses. Pathogens 2023, 12, 977. [Google Scholar] [CrossRef]
- Konda, M.; Dodda, B.; Konala, V.M.; Naramala, S.; Adapa, S. Potential Zoonotic Origins of SARS-CoV-2 and Insights for Preventing Future Pandemics Through One Health Approach. Cureus 2020, 12, e8932. [Google Scholar] [CrossRef]
- Rüegg, S.R.; Häsler, B.; Zinsstag, J. Integrated Approaches to Health. A Handbook for the Evaluation of One Health; Wageningen Academic Publishers: Wageningen, The Netherlands, 2018. [Google Scholar] [CrossRef]
- Löscher, T.; Prüfer-Krämer, L. Emerging and Re-emerging Infectious Diseases. In Modern Infectious Disease Epidemiology. Concepts, Methods, Mathematical Models, and Public Health; Krämer, A., Kretzschmar, M., Krickeberg, K., Eds.; Springer: New York, NY, USA, 2009; Chapter 3; pp. 39–67. [Google Scholar] [CrossRef]
- WHO. A Health Perspective on the Role of the Environment in One Health. Copenhagen. 2022. Available online: http://apps.who.int/iris (accessed on 25 July 2023).
- Jones, K.E.; Patel, N.G.; Levy, M.A.; Storeygard, A.; Balk, D.; Gittleman, J.L.; Daszak, P. Global trends in emerging infectious diseases. Nature 2008, 451, 990–993. [Google Scholar] [CrossRef]
- Bezerra-Santos, M.A.; Mendoza-Roldan, J.A.; Thompson, R.A.; Dantas-Torres, F.; Otranto, D. Illegal Wildlife Trade: A Gateway to Zoonotic Infectious Diseases. Trends Parasitol. 2021, 23, 181–184. [Google Scholar] [CrossRef]
- Wyatt, T. Wildlife Trafficking. A Deconstruction of the Crime, Victims and Offenders; Palgrave Macmillan: Cham, Switzerland, 2021. [Google Scholar]
- Plowright, R.K.; Reaser, J.K.; Locke, H.; Woodley, S.J.; Patz, J.A.; Becker, D.J.; Oppler, G.; Hudson, P.J.; Tabor, G.M. Land use-induced spillover: A call to action to safeguard environmental, animal, and human health. Lancet Planet. Health 2021, 5, e237–e245. [Google Scholar] [CrossRef]
- Reaser, J.K.; Tabor, G.M.; Becker, D.J.; Muruthi, P.; Witt, A.; Woodley, S.J.; Ruiz-Aravena, M.; Patz, J.A.; Hickey, V.; Hudson, P.J.; et al. Land use-induced Spillover: Priority Actions for Protected and Conserved Area managers. PARKS 2021, 27, 161–178. [Google Scholar] [CrossRef]
- Maher, J.; Sollund, R. Wildlife Trafficking: Harms and Victimization. In Fighting Environmental Crime in Europe and Beyond; Sollund, R., Stefes, C., Germani, A., Eds.; Palgrave Macmillan: London, UK, 2016; pp. 99–128. [Google Scholar] [CrossRef]
- Rush, E.R.; Dale, E.; Aguirre, A.A. Illegal wildlife trade and emerging infectious diseases: Pervasive impacts to species, ecosystems and human health. Animals 2021, 11, 1821. [Google Scholar] [CrossRef]
- Sollund, R. The Use and Abuse of Animals in Wildlife Trafficking in Colombia: Practices and Injustice. In Environmental Crime in Latin America. The Theft of Nature and the Poisoning of the Land; Goyes, D.R., Mol, H., Brisman, A., South, N., Eds.; Palgrave Macmillan: London, UK, 2017; Chapter 10; pp. 215–243. [Google Scholar] [CrossRef]
- Sollund, R. Green Criminology: Its Foundation in Critical Criminology and the Way Forward. In Howard Journal of Crime and Justice; John Wiley and Sons Inc.: Hoboken, NJ, USA, 2021; pp. 304–322. [Google Scholar] [CrossRef]
- Gibbs, C.; Boratto, R. Environmental Crime. In Oxford Research Encyclopedia of Criminology and Criminal Justice; Pontell, H., Ed.; Oxford University Press: New York, NY, USA, 2017; pp. 1–33. [Google Scholar] [CrossRef]
- Wong, R.W.Y. The Harms and Crimes Against Terrestrial Wildlife (Nonhuman Animals). In Oxford Research Encyclopedia of Criminology and Criminal Justice; Pontell, H., Ed.; Oxford University Press: New York, NY, USA, 2023; pp. 1–19. [Google Scholar] [CrossRef]
- Gladkova, E. The Harms and Crimes of Farming/Food. In Oxford Research Encyclopedia of Criminology and Criminal Justice; Pontell, H., Ed.; Oxford University Press: New York, NY, USA, 2023. [Google Scholar] [CrossRef]
- Adisasmito, W.B.; Almuhairi, S.; Behravesh, C.B.; Bilivogui, P.; Bukachi, S.A.; Casas, N.; Becerra, N.C.; Charron, D.F.; Chaudhary, A.; Zanella, J.R.C.; et al. One Health: A new definition for a sustainable and healthy future. PLoS Pathog. 2022, 18, e1010537. [Google Scholar] [CrossRef]
- European Union Agencies. Cross-Agency Knowledge for One Health Action Joint Statement by European Union Agencies. 2023. Available online: https://www.efsa.europa.eu/sites/default/files/2023-11/one-health-2023-joint-statement.pdf (accessed on 27 March 2024).
- UNEP. Preventing the Next Pandemic. Zoonotic Diseases and How to Break the Chain of Transmission. 2020. Available online: https://www.unep.org/resources/report/preventing-future-zoonotic-disease-outbreaks-protecting-environment-animals-and (accessed on 4 August 2024).
- van Langevelde, F.; Mondoza, H.R.R.; Matson, K.D.; Esser, H.J.; de Boer, W.F.; Schindler, S. The Link between Biodiversity Loss and the Increasing Spread of Zoonotic Diseases; European Parliament: Strasbourg, France, 2020. [Google Scholar]
- de Castañeda, R.R.; Villers, J.; Guzmán, C.A.F.; Eslanloo, T.; de Paula, N.; Machalaba, C.; Zinsstag, J.; Utzinger, J.; Flahault, A.; Bolon, I. One Health and planetary health research: Leveraging differences to grow together. Lancet Planet. Health 2023, 7, e109–e111. [Google Scholar] [CrossRef]
- Zinsstag, J.; Kaiser-Grolimund, A.; Heitz-Tokpa, K.; Sreedharan, R.; Lubroth, J.; Caya, F.; Stone, M.; Brown, H.; Bonfoh, B.; Dobell, E.; et al. Advancing One human–animal–environment Health for global health security: What does the evidence say? Lancet 2023, 401, 591–604. [Google Scholar] [CrossRef]
- Lerner, H.; Berg, C. A Comparison of Three Holistic Approaches to Health: One Health, EcoHealth, and Planetary Health. Front. Vet. Sci. 2017, 4, 163. [Google Scholar] [CrossRef]
- Jer, S.B. Conceptual Precedents for an Ecosuicidology. Topicos 2023, 67, 453–477. [Google Scholar] [CrossRef]
- White, R. Loving the Planet to Death: Tourism and Ecocide. In Deviant Leisure. Palgrave Studies in Crime, Media and Culture; Raymen, T., Smith, O., Eds.; Palgrave Macmillan: Cham, Switzerland, 2019; Available online: https://doi-org.ezproxy2.acu.edu.au/10.1007/978-3-030-17736-2_13 (accessed on 11 August 2024).
- Crook, M.; Short, D.; South, N. Ecocide, genocide, capitalism and colonialism: Consequences for indigenous peoples and glocal ecosystems environments. Theor. Criminol. 2018, 22, 298–317. [Google Scholar] [CrossRef]
- Schwegler, V. The Disposable Nature: The Case of Ecocide and Corporate Accountability. Amst. Law Forum 2017, 9, 71. [Google Scholar] [CrossRef]
- Capps, B. One Health Environmentalism; Cambridge University Press: Cambridge, UK, 2024. [Google Scholar]
- Capps, B. One health ethics. Bioethics 2021, 36, 348–355. [Google Scholar] [CrossRef]
- Pollowitz, M.; Allick, C.; Campbell, K.B.; Ellison, N.L.K.; Perez-Aguilar, G.; Vera, M.; Ramirez, V.; Nadal, D.; Meisner, J. One Health, many perspectives: Exploring Indigenous and Western epistemologies. CABI One Health 2024. [Google Scholar] [CrossRef]
- Redvers, N.; Celidwen, Y.; Schultz, C.; Horn, O.; Githaiga, C.; Vera, M.; Perdrisat, M.; Plume, L.M.; Kobei, D.; Kain, M.C.; et al. The determinants of planetary health: An Indigenous consensus perspective. Lancet Planet. Health 2022, 6, e156–e163. [Google Scholar] [CrossRef]
- Riley, T.; Anderson, N.E.; Lovett, R.; Meredith, A.; Cumming, B.; Thandrayen, J. One Health in Indigenous Communities: A Critical Review of the Evidence. Int. J. Environ. Res. Public Health 2021, 18, 11303. [Google Scholar] [CrossRef]
- CBD. Biodiversity and Health. Nairobi, May 2024. Available online: https://www.cbd.int/cop (accessed on 11 June 2024).
- Whitmee, S.; Haines, A.; Beyrer, C.; Boltz, F.; Capon, A.G.; de Souza Dias, B.F.; Ezeh, A.; Frumkin, H.; Gong, P.; Head, P.; et al. Safeguarding human health in the Anthropocene epoch: Report of The Rockefeller Foundation—Lancet Commission on planetary health. Lancet 2015, 386, 1973–2028. [Google Scholar] [CrossRef]
- Romanello, M.; di Napoli, C.; Green, C.; Kennard, H.; Lampard, P.; Scamman, D.; Walawender, M.; Ali, Z.; Ameli, N.; Ayeb-Karlsson, S.; et al. The 2023 report of the Lancet Countdown on health and climate change: The imperative for a health-centred response in a world facing irreversible harms. Lancet 2023, 402, 2346–2394. [Google Scholar] [CrossRef]
- The Lancet Planetary Health. Can the Paris Agreement save us from a climate catastrophe? Lancet Planet. Health 2018, 2, e140. [Google Scholar] [CrossRef]
- IPCC. Climate Change 2022-Impacts, Adaptation and Vulnerability-Summary for Policymakers. Switzerland. 2022. Available online: https://www.ipcc.ch/report/ar6/wg2/downloads/report/IPCC_AR6_WGII_SummaryForPolicymakers.pdf (accessed on 10 March 2023).
- IPCC. Climate Change 2023. Synthesis Report. In Climate Change 2023: Synthesis Report. Contribution of Working Groups I, II and III to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change; Lee, H., Romero, J., Eds.; IPCC: Geneva, Switzerland, 2023; pp. 1–34. [Google Scholar] [CrossRef]
- Correia, T.; Daniel-Ribeiro, C.T.; Ferrinho, P. Calling for a planetary and one health vision for global health. One Health 2021, 13, 100342. [Google Scholar] [CrossRef]
- Fernando, J. The Virocene Epoch: The Vulnerability Nexus of Viruses, Capitalism and Racism. J. Polit. Ecol. 2020, 27, 635–684. Available online: https://commons.clarku.edu/faculty_idce/145 (accessed on 5 August 2024).
- Correia, T. The precariousness of political management of the SARS-CoV-2 pandemic in the search for scientific answers: Calling for prudence in public health emergencies. Int. J. Health Plan. Manag. 2021, 36, 1387–1391. [Google Scholar] [CrossRef]
- Correia, T.; Ricciardi, W.; McKee, M. Preparing for the ‘next pandemic’: Why we need to escape from our silos. Int. J. Health Plan. Manag. 2024, 39, 973–979. [Google Scholar] [CrossRef]
- Correia, T. SARS-CoV-2 pandemics: The lack of critical reflection addressing short- and long-term challenges. Int. J. Health Plan. Manag. 2020, 35, 669–672. [Google Scholar] [CrossRef]
- Kaplan, S.; Lefler, J.; Zilberman, D. The political economy of COVID-19. Appl. Econ. Perspect. Policy 2021, 44, 477–488. [Google Scholar] [CrossRef] [PubMed]
- Rozzi, R. Earth Stewardship and the Biocultural Ethic: Latin American Perspectives. In Earth Stewardship: Ecology and Ethics; Rozzi, R., Ed.; Springer: Cham, Switzerland, 2015; Volume 2, pp. 87–112. [Google Scholar]
- Sonne, C.; Langebæk, R.; Dietz, R.; Andersen-Ranberg, E.; Houser, G.; Hansen, A.J.; Sinding, M.-H.S.; Olsen, M.T.; Egevang, C.; Gilbert, M.T.P.; et al. Greenland sled dogs at risk of extinction. Science 2018, 360, 1080. [Google Scholar] [CrossRef]
- Dirzo, R.; Ceballos, G.; Ehrlich, P.R. Circling the drain: The extinction crisis and the future of humanity. Philos. Trans. R. Soc. B Biol. Sci. 2022, 377, 20210378. [Google Scholar] [CrossRef]
- Sell, S.K.; Williams, O.D. Health under capitalism: A global political economy of structural pathogenesis. Rev. Int. Political Econ. 2019, 27, 1–25. [Google Scholar] [CrossRef]
- Gill, S.R.; Benatar, S.R. Reflections on the political economy of planetary health. Rev. Int. Political Econ. 2019, 27, 167–190. [Google Scholar] [CrossRef]
- Baer, H.A.; Singer, M. Planetary Health: Capitalism, Ecology and Eco-Socialism. Capital. Nat. Social. 2023, 34, 20–38. [Google Scholar] [CrossRef]
- Sathyamala, C. COVID-19: The Political Economy of a Global Pandemic; John Wiley and Sons Inc.: Hoboken, NJ, USA, 2022. [Google Scholar] [CrossRef]
- Antoine-Moussiaux, N.; de Bisthoven, L.J.; Leyens, S.; Assmuth, T.; Keune, H.; Jakob, Z.; Hugé, J.; Vanhove, M.P.M. The good, the bad and the ugly: Framing debates on nature in a One Health community. Sustain. Sci. 2019, 14, 1729–1738. [Google Scholar] [CrossRef]
- Layton, D.S.; Choudhary, A.; Bean, A.G. Breaking the chain of zoonoses through biosecurity in livestock. Vaccine 2017, 35, 5967–5973. [Google Scholar] [CrossRef]
- Rahman, T.; Sobur, A.; Islam, S.; Ievy, S.; Hossain, J.; El Zowalaty, M.E.; Rahman, A.T.; Ashour, H.M. Zoonotic Diseases: Etiology, Impact, and Control. Microorganisms 2020, 8, 1405. [Google Scholar] [CrossRef] [PubMed]
- Zinsstag, J.; Hediger, K.; Osman, Y.M.; Abukhattab, S.; Crump, L.; Kaiser-Grolimund, A.; Mauti, S.; Ahmed, A.; Hattendorf, J.; Bonfoh, B.; et al. The Promotion and Development of One Health at Swiss TPH and Its Greater Potential. Diseases 2022, 10, 65. [Google Scholar] [CrossRef] [PubMed]
- Ghai, R.; Behravesh, C. Zoonoses—The One Health Approach. In CDC Yellow Book 2024: Health Information for International Travel; Nemhauser, J., Ed.; Oxford University Press: New York, NY, USA, 2023; pp. 222–224. [Google Scholar]
- Nemhauser, J. CDC Yellow Book 2024: Health Information for International Travel; Oxford University Press: New York, NY, USA, 2023. [Google Scholar]
- Walker, A.; LaRocque, R. Introduction. Disease Patterns in Travels. In CDC Yellow Book 2024: Health Information for International Travel; Nemhauser, J., Ed.; Oxford University Press: New York, NY, USA, 2023; pp. 1–12. [Google Scholar] [CrossRef]
- Allouche, J. Ebola and Extractive Industry. 2015. Available online: https://opendocs.ids.ac.uk/opendocs/handle/20.500.12413/5854 (accessed on 28 July 2023).
- Andrade, D. Neoliberal extractivism: Brazil in the twenty-first century. J. Peasant. Stud. 2022, 49, 793–816. [Google Scholar] [CrossRef]
- Bruna, N. A climate-smart world and the rise of Green Extractivism. J. Peasant. Stud. 2022, 49, 839–864. [Google Scholar] [CrossRef]
- Ormsby, M.J.; Woodford, L.; Quilliam, R.S. Can plastic pollution drive the emergence and dissemination of novel zoonotic diseases? Environ. Res. 2024, 246, 118172. [Google Scholar] [CrossRef]
- Maquart, P.-O.; Froehlich, Y.; Boyer, S. Plastic pollution and infectious diseases. Lancet Planet. Health 2022, 6, e842–e845. [Google Scholar] [CrossRef]
- FAO; UNEP; WHO; WOAH. One Health Joint Plan of Action, 2022–2026. Working together for The Planet of Humans, Animals, Plants and The Environment; FAO, UNEP, WHO, and WOAH: Rome, Italy, 2022. [Google Scholar] [CrossRef]
- Littmann, J. Antimicrobial resistance and Distributive Justice. Doctoral Dissertation, UCL (University College London), London, UK, 2014. [Google Scholar]
- Rollin, B. Ethics, Science, and Antimicrobial Resistance. J. Agric. Environ. Ethic 2001, 14, 29–37. [Google Scholar] [CrossRef]
- WHO. Global Action Plan on Antimicrobial Resistance. Geneva. 2015. Available online: https://www.amcra.be/swfiles/files/WHOactieplan_90.pdf (accessed on 10 July 2024).
- Littmann, J.; Viens, A.M. The Ethical Significance of Antimicrobial Resistance. Public Health Ethics 2015, 8, 209–224. [Google Scholar] [CrossRef]
- Prestinaci, F.; Pezzotti, P.; Pantosti, A. Antimicrobial resistance: A global multifaceted phenomenon. Pathog. Glob. Health 2015, 109, 309–318. [Google Scholar] [CrossRef]
- McEwen, S.A.; Collignon, P.J. Antimicrobial Resistance: A One Health Perspective. Microbiol. Spectr. 2018, 6, 1–26. [Google Scholar] [CrossRef]
- Kahn, L.H. Antimicrobial resistance: A One Health perspective. Trans. R. Soc. Trop. Med. Hyg. 2017, 111, 255–260. [Google Scholar] [CrossRef] [PubMed]
- Parsonage, B.; Hagglund, P.K.; Keogh, L.; Wheelhouse, N.; Brown, R.E.; Dancer, S.J. Control of Antimicrobial Resistance Requires an Ethical Approach. Front. Microbiol. 2017, 8, 2124. [Google Scholar] [CrossRef]
- Kahn, L. One Health and the Politics of Antimicrobial Resistance; Johns Hopkins University Press: Baltimore, MD, USA, 2016. [Google Scholar]
- European Commission. A European One Health Action Plan against Antimicrobial Resistance (AMR). 2017. Available online: https://health.ec.europa.eu/document/download/353f40d1-f114-4c41-9755-c7e3f1da5378_en?filename=amr_2017_action-plan.pdf (accessed on 16 July 2024).
- Shallcross, L.J.; Howard, S.J.; Fowler, T.; Davies, S.C. Tackling the threat of antimicrobial resistance: From policy to sustainable action. Philos. Trans. R. Soc. B Biol. Sci. 2015, 370, 20140082. [Google Scholar] [CrossRef]
- Anthony, R.; Vieira, A.D.P. One Health Animal Disaster Management: An Ethics of Care Approach. J. Appl. Anim. Welf. Sci. 2022, 25, 180–194. [Google Scholar] [CrossRef]
- Collignon, P.J.; McEwen, S.A. One Health—Its Importance in Helping to Better Control Antimicrobial Resistance. Trop. Med. Infect. Dis. 2019, 4, 22. [Google Scholar] [CrossRef] [PubMed]
- Lammie, S.L.; Hughes, J.M. Antimicrobial Resistance, Food Safety, and One Health: The Need for Convergence. Annu. Rev. Food Sci. Technol. 2016, 7, 287–312. [Google Scholar] [CrossRef] [PubMed]
- Belay, E.D.; Kile, J.C.; Hall, A.J.; Barton-Behravesh, C.; Parsons, M.B.; Salyer, S.; Walke, H. Zoonotic Disease Programs for Enhancing Global Health Security. Emerg. Infect. Dis. 2017, 23, S65–S70. [Google Scholar] [CrossRef] [PubMed]
- Marchese, A.; Hovorka, A. Zoonoses Transfer, Factory Farms and Unsustainable Human–Animal Relations. Sustainability 2022, 14, 12806. [Google Scholar] [CrossRef]
- Sánchez, C.A.; Venkatachalam-Vaz, J.; Drake, J.M. Spillover of zoonotic pathogens: A review of reviews. Zoonoses Public Health 2021, 68, 563–577. [Google Scholar] [CrossRef]
- Broom, D.M. Animal welfare complementing or conflicting with other sustainability issues. Appl. Anim. Behav. Sci. 2019, 219, 104829. [Google Scholar] [CrossRef]
- Steenson, S.; Buttriss, J.L. The challenges of defining a healthy and ‘sustainable’ diet. Nutr. Bull. 2020, 45, 206–222. [Google Scholar] [CrossRef]
- Rohr, J.R.; Barrett, C.B.; Civitello, D.J.; Craft, M.E.; Delius, B.; DeLeo, G.A.; Hudson, P.J.; Jouanard, N.; Nguyen, K.H.; Ostfeld, R.S.; et al. Emerging human infectious diseases and the links to global food production. Nat. Sustain. 2019, 2, 445–456. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.A.; Flórez, M.G.; Karanis, P. The impact of water crises and climate changes on the transmission of protozoan parasites in Africa. Ann. Trop. Med. Parasitol. 2018, 112, 281–293. [Google Scholar] [CrossRef]
- Ristaino, J.B.; Anderson, P.K.; Bebber, D.P.; Brauman, K.A.; Cunniffe, N.J.; Fedoroff, N.V.; Finegold, C.; Garrett, K.A.; Gilligan, C.A.; Jones, C.M.; et al. The persistent threat of emerging plant disease pandemics to global food security. Proc. Natl. Acad. Sci. USA 2021, 118, e2022239118. [Google Scholar] [CrossRef]
- Mardones, F.O.; Rich, K.M.; Boden, L.A.; Moreno-Switt, A.I.; Caipo, M.L.; Zimin-Veselkoff, N.; Alateeqi, A.M.; Baltenweck, I. The COVID-19 Pandemic and Global Food Security. Front. Vet. Sci. 2020, 7, 578508. [Google Scholar] [CrossRef]
- Brooks, D.R.; Hoberg, E.P.; Boeger, W.A.; Trivellone, V. Emerging infectious disease: An underappreciated area of strategic concern for food security. Transbound. Emerg. Dis. 2021, 69, 254–267. [Google Scholar] [CrossRef]
- Vercauteren, K.C.; Gortázar, C.; Beltrán-Alcrudo, D.; Vicente, J. Host Community Interfaces: The Wildlife-Livestock. In Diseases at the Wildlife-Livestock Interface. Wildlife Research Monographs; Vicente, J., Vercauteren, K.C., Gortázar, C., Eds.; Springer: Cham, Switzerland, 2021; Volume 3, pp. 3–32. [Google Scholar] [CrossRef]
- Schlundt, J.; Toyofuku, H.; Fisher, J.; Artois, M.; Morner, T.; Tate, C. The role of wildlife in emerging and re-emerging zoonoses. Rev. Sci. Et Tech. De L’oie 2004, 23, 485–496. [Google Scholar] [CrossRef]
- Moreno, R.D.; Valera, V.; Borgoño, C.; Castilla, J.C.; and Riveros, J.L. Gene Drives, Mosquitoes, and Ecosystems: An Interdisciplinary Approach to Emerging Ethical Concerns. Front. Environ. Sci. 2023, 11, 1–13. [Google Scholar] [CrossRef]
- Escudero-Pérez, B.; Lalande, A.; Mathieu, C.; Lawrence, P. Host–Pathogen Interactions Influencing Zoonotic Spillover Potential and Transmission in Humans. Viruses 2023, 15, 599. [Google Scholar] [CrossRef]
- Marie, V.; Gordon, M.L. The (Re-)Emergence and Spread of Viral Zoonotic Disease: A Perfect Storm of Human Ingenuity and Stupidity. Viruses 2023, 15, 1638. [Google Scholar] [CrossRef] [PubMed]
- Tomori, O.; Oluwayelu, D.O. Domestic Animals as Potential Reservoirs of Zoonotic Viral Diseases. Annu. Rev. Anim. Biosci. 2023, 11, 33–55. [Google Scholar] [CrossRef]
- WHO. A Tripartite Guide to Addressing Zoonotic Diseases in Countries Taking a Multisectoral, One Health Approach. 2019. Available online: https://www.woah.org/fileadmin/Home/eng/Media_Center/docs/EN_TripartiteZoonosesGuide_webversion.pdf (accessed on 4 April 2024).
- WHO. WHO Director-General Declares Mpox Outbreak a Public Health Emergency of International Concern. World Health Organization, August 14. 2024. Available online: https://www.who.int/europe/emergencies/situations/monkeypox (accessed on 14 August 2024).
- Gaard, G. Ecofeminism. In The Routledge Companion to Gender and Animals; Taylor, C., Ed.; Routledge: New York, NY, USA, 2024; pp. 49–70. [Google Scholar]
- Laird, T. Zoonoses. In The Routledge Companion to Gender and Animals; Taylor, C., Ed.; Routledge: New York, NY, USA, 2024; pp. 680–696. [Google Scholar]
- Gruen, L. Critical Terms for Animal Studies; The University of Chicago Press: Chicago, IL, USA; London, UK, 2018. [Google Scholar]
- Gruen, L. Entangled Empathy: Politics and Practice. In Animal Encounters Kontakt, Interaktion und Relationalität; Böhm, A., Ullrich, J., Eds.; The University of Chicago Press: Chicago, IL, USA; London, UK, 2018; pp. 77–83. [Google Scholar]
- Gruen, L. Entangled Empathy: An Alternative Ethic for our Relationships with Animals; Lantern Press: Brooklyn, NY, USA, 2015. [Google Scholar]
- Yoo, H.S.; Yoo, D. COVID-19 and veterinarians for one health, zoonotic- and reverse-zoonotic transmissions. J. Veter. Sci. 2020, 21, e51. [Google Scholar] [CrossRef]
- Messenger, A.M.; Barnes, A.N.; Gray, G.C. Reverse Zoonotic Disease Transmission (Zooanthroponosis): A Systematic Review of Seldom-Documented Human Biological Threats to Animals. PLoS ONE 2014, 9, e89055. [Google Scholar] [CrossRef]
- Glud, H.A.; George, S.; Skovgaard, K.; Larsen, L.E. Zoonotic and reverse zoonotic transmission of viruses between humans and pigs. APMIS 2021, 129, 675–693. [Google Scholar] [CrossRef]
- CDC. Centers for Diseases Control and Prevention. Zoonotic Diseases. Available online: https://www.cdc.gov/one-health/about/about-zoonotic-diseases.html (accessed on 22 April 2022).
- Eskew, E.A.; Olival, K.J. De-urbanization and Zoonotic Disease Risk. Ecohealth 2018, 15, 707–712. [Google Scholar] [CrossRef]
- Olival, K.J.; Cryan, P.M.; Amman, B.R.; Baric, R.S.; Blehert, D.S.; Brook, C.E.; Calisher, C.H.; Castle, K.T.; Coleman, J.T.H.; Daszak, P.; et al. Possibility for reverse zoonotic transmission of SARS-CoV-2 to free-ranging wildlife: A case study of bats. PLoS Pathog. 2020, 16, e1008758. [Google Scholar] [CrossRef]
- Sing, A. Zoonoses: Infections Affecting Humans and Animals; Springer: Cham, Switzerland, 2023. [Google Scholar] [CrossRef]
- Wilcox, B.A.; Steele, J.A. One Health and Emerging Zoonotic Diseases. In Handbook of Global Health; Kickbusch, I., Ganten, D., Moeti, M., Eds.; Springer: Cham, Switzerland, 2021; pp. 2099–2147. [Google Scholar]
- WHO. (2024, June 9). Neglected Tropical Diseases. Available online: https://www.who.int/news-room/questions-and-answers/item/neglected-tropical-diseases (accessed on 2 August 2024).
- ECDC. Worsening Spread of Mosquito-Borne Disease Outbreaks in EU/EEA, According to Latest ECDC Figures; European Centre for Disease Prevention and Control: Solna, Sweden, 2024; Available online: https://www.ecdc.europa.eu/en/news-events/worsening-spread-mosquito-borne-disease-outbreaks-eueea-according-latest-ecdc-figures (accessed on 11 August 2024).
- WHO. World Health Statistics 2023. Monitoring Health for the SDGs Sustainable Development Goals. Geneva. 2023. Available online: https://reliefweb.int/report/world/world-health-statistics-2023-monitoring-health-sdgs-sustainable-development-goals (accessed on 17 July 2024).
- Augusto, L.G.d.S.; Gurgel, A.M.; Costa, A.M.; Diderichsen, F.; Lacaz, F.A.; Parra-Henao, G.; Rigotto, R.M.; Nodari, R.; Santos, S.L. Aedes aegypti control in Brazil. Lancet 2016, 387, 1052–1053. [Google Scholar] [CrossRef]
- Franco-Paredes, C.; Villamil-Gómez, W.E.; Schultz, J.; Henao-Martínez, A.F.; Parra-Henao, G.; Rassi, A.; Rodríguez-Morales, A.J.; Suarez, J.A. A deadly feast: Elucidating the burden of orally acquired acute Chagas disease in Latin America–Public health and travel medicine importance. Travel Med. Infect. Dis. 2020, 36, 101565. [Google Scholar] [CrossRef] [PubMed]
- Chapungu, L.; Nhamo, G. Interfacing vector-borne disease dynamics with climate change: Implications for the attainment of SDGs in Masvingo city, Zimbabwe. Jamba J. Disaster Risk Stud. 2021, 13, 12. [Google Scholar] [CrossRef]
- Ainsworth, C. Tropical Diseases Move North. Nat. Outlook Neglected Trop. Dis. 2023. [Google Scholar] [CrossRef]
- Gibb, R.; Redding, D.W.; Chin, K.Q.; Donnelly, C.A.; Blackburn, T.M.; Newbold, T.; Jones, K.E. Zoonotic host diversity increases in human-dominated ecosystems. Nature 2020, 584, 398–402. [Google Scholar] [CrossRef] [PubMed]
- Mahon, M.B.; Sack, A.; Aleuy, O.A.; Barbera, C.; Brown, E.; Buelow, H.; Civitello, D.J.; Cohen, J.M.; de Wit, L.A.; Forstchen, M.; et al. A meta-analysis on global change drivers and the risk of infectious disease. Nature 2024, 629, 830–836. [Google Scholar] [CrossRef] [PubMed]
- Alexander, K.A.; Carlson, C.J.; Lewis, B.L.; Getz, W.M.; Marathe, M.V.; Eubank, S.G.; Sanderson, C.E.; Blackburn, J.K. The Ecology of Pathogen Spillover and Disease Emergence at the Human-Wildlife-Environment Interface. In The Connections between Ecology and Infectious Disease; Springer International Publishing: Cham, Switzerland, 2018; pp. 267–298. [Google Scholar] [CrossRef]
- Benbow, M.E.; Pechal, J.L.; Tomberlin, J.K.; Jordan, H.R. Interkingdom Community Interactions in Disease Ecology. In The Connections Between Ecology and Infectious Disease, Advances in Environmental Microbiology; Hurst, C.J., Ed.; Springer: Cham, Switzerland, 2018; Volume 5, Chapter 1; pp. 3–38. [Google Scholar] [CrossRef]
- Grubaugh, N.D.; Ladner, J.T.; Lemey, P.; Pybus, O.G.; Rambaut, A.; Holmes, E.C.; Andersen, K.G. Tracking virus outbreaks in the twenty-first century. Nat. Microbiol. 2018, 4, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Plowright, R.K.; Parrish, C.R.; McCallum, H.; Hudson, P.J.; Ko, A.I.; Graham, A.L.; Lloyd-Smith, J.O. Pathways to zoonotic spillover. Nat. Rev. Microbiol. 2017, 15, 502–510. [Google Scholar] [CrossRef] [PubMed]
- Valera, L. New Technologies. Rethinking Ethics and the Environment; Springer: Cham, Switzerland, 2020. [Google Scholar] [CrossRef]
- Baker, R.E.; Mahmud, A.S.; Miller, I.F.; Rajeev, M.; Rasambainarivo, F.; Rice, B.L.; Takahashi, S.; Tatem, A.J.; Wagner, C.E.; Wang, L.-F.; et al. Infectious disease in an era of global change. Nat. Rev. Microbiol. 2022, 20, 193–205. [Google Scholar] [CrossRef]
- Cohen, M.L. Changing patterns of infectious disease. Nature 2000, 406, 762–767. [Google Scholar] [CrossRef]
- Price-Smith, A. Contagion and Chaos: Disease, Ecology, and National Security in the Era of Globalization; MIT Press: Cambridge, UK, 2009. [Google Scholar]
- Price-Smith, A. The Plagues of Affluence: Human Ecology and the Case of the SARS Epidemic. Environ. Hist. 2015, 20, 765–778. Available online: https://www.jstor.org/stable/24690826 (accessed on 16 July 2024).
- Ren, H.; Zhao, L.; Zhang, A.; Song, L.; Liao, Y.; Lu, W.; Cui, C. Early forecasting of the potential risk zones of COVID-19 in China’s megacities. Sci. Total. Environ. 2020, 729, 138995. [Google Scholar] [CrossRef]
- Sridhar, K.S. Urbanization and COVID-19 Prevalence in India. Reg. Sci. Policy Pract. 2021, 15, 493–506. [Google Scholar] [CrossRef]
- Ali, S.H.; Connolly, C.; Keil, R. Pandemic Urbanism: Infectious Diseases on a Planet of Cities; Polity Press: Cambridge, UK, 2023. [Google Scholar]
- Jonas, H. The Imperative of Responsability. In Search of an Ethics for the Technological Age; The University of Chicago Press: Chicago, IL, USA; London, UK, 1984. [Google Scholar]
- Cummings, L. Emerging infectious diseases: Coping with uncertainty. Argumentation 2009, 23, 171–188. [Google Scholar] [CrossRef]
- Baekkeskov, E. Explaining science-led policy-making: Pandemic deaths, epistemic deliberation and ideational trajectories. Policy Sci. 2016, 49, 395–419. [Google Scholar] [CrossRef]
- Tulodziecki, D. How (not) to think about theory-change in epidemiology. Synthese 2021, 198, 2569–2588. [Google Scholar] [CrossRef]
- Alter, H.J. Pathogen Reduction: A Precautionary Principle Paradigm. Transfus. Med. Rev. 2008, 22, 97–102. [Google Scholar] [CrossRef]
- van Herten, J.; Bovenkerk, B. The Precautionary Principle in Zoonotic Disease Control. Public Health Ethics 2021, 14, 180–190. [Google Scholar] [CrossRef]
- Nichol, A.; Magnus, D. The One Health Approach to Zoonotic Emerging Infectious Diseases. Am. J. Bioeth. 2018, 18, 1–2. [Google Scholar] [CrossRef]
- Coghlan, S.; Coghlan, B. One Health, Bioethics, and Nonhuman Ethics. Am. J. Bioeth. 2018, 18, 3–5. [Google Scholar] [CrossRef] [PubMed]
- Lindenmayer, J.M.; Kaufman, G.E.; Baker, L.; Coghlan, S.; Koontz, F.W.; Nieuwland, J.; Stewart, K.L.; Lynn, W.S. One health ethics: “What then must we do?”. CABI One Health 2022, 4, 1–4. [Google Scholar] [CrossRef]
- Capps, B.; Lederman, Z. One Health, Vaccines and Ebola: The Opportunities for Shared Benefits. J. Agric. Environ. Ethics 2015, 28, 1011–1032. [Google Scholar] [CrossRef] [PubMed]
- Wispelwey, B.; Osuagwu, C.; Mills, D.; Goronga, T.; Morse, M. Towards a bidirectional decoloniality in academic global health: Insights from settler colonialism and racial capitalism. Lancet Glob. Health 2023, 11, e1469–e1474. [Google Scholar] [CrossRef]
- Rodriguez, J. A Bridge towards the One Health Approach: Rediscovering Environmental Bioethics. Rev. Iberoam. Bioet. 2021, 17, 1–13. [Google Scholar] [CrossRef]
- Manguvo, A.; Mafuvadze, B. The impact of traditional and religious practices on the spread of Ebola in West Africa: Time for a strategic shift. Pan. Afr. Med. J. 2015, 22, 9. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, D.V.B.; da Silva, J.F.; de Sousa Araújo, T.A.; Albuquerque, U.P. Influence of Religiosity and Spirituality on the Adoption of Behaviors of Epidemiological Relevance in Emerging and Re-Emerging Diseases: The Case of Dengue Fever. J. Relig. Health 2022, 61, 564–585. [Google Scholar] [CrossRef]
- Griffith, D.M.; Efird, C.R.; Baskin, M.L.; Hooper, M.W.; Davis, R.E.; Resnicow, K. Cultural Sensitivity and Cultural Tailoring: Lessons Learned and Refinements After Two Decades of Incorporating Culture in Health Communication Research. Annu. Rev. Public Health 2024, 48, 195–212. [Google Scholar] [CrossRef]
- ten Have, H. Globalizing Bioethics Through, Beyond and Despite Governments. In Global Bioethics: The Impact of the UNESCO International Bioethics Committee; Bagheri, A., Moreno, J.D., Semplici, S., Eds.; Springer: Cham, Switzerland, 2016; Volume 5, Chapter 1; pp. 1–11. [Google Scholar] [CrossRef]
- Lee, L.M. A Bridge Back to the Future: Public Health Ethics, Bioethics, and Environmental Ethics. Am. J. Bioeth. 2017, 17, 5–12. [Google Scholar] [CrossRef]
- Rüegg, S.R.; Nielsen, L.R.; Buttigieg, S.C.; Santa, M.; Aragrande, M.; Canali, M.; Ehlinger, T.; Chantziaras, I.; Boriani, E.; Radeski, M.; et al. A Systems Approach to Evaluate One Health Initiatives. Front. Veter. Sci. 2018, 5, 23. [Google Scholar] [CrossRef]
- Zinsstag, J.; Schelling, E.; Crump, L.; Whittaker, M.; Tanner, M.; Stephen, C. One Health: The Theory and Practice of Integrated Health Approaches; CAB International: London, UK, 2021. [Google Scholar]
- Sinclair, J.R. Importance of a One Health approach in advancing global health security and the Sustainable Development Goals. Rev. Sci. Et Tech. Int. Off. Epizoot. 2019, 38, 145–154. [Google Scholar] [CrossRef]
- Pettan-Brewer, C.; Penn, G.; Biondo, A.W.; Jaenisch, T.; Grützmacher, K.; Kahn, L.H. Who coined the term “One Health”? Cooperation amid the siloization. One Health 2024, 18, 100678. [Google Scholar] [CrossRef]
- Have, H.T. The challenges of global bioethics. Glob. Bioeth. 2022, 33, 41–44. [Google Scholar] [CrossRef] [PubMed]
- Ten Have, H.; Gordijn, B. Handbook of Global Bioethics; Springer: Berlin/Heidelberg, Germany, 2014; pp. 1–1685. [Google Scholar] [CrossRef]
- Valera, J.; Rodriguez, L. Technology, Ecology and Survival Science: A Look at Barry Commoner’s Thought for the Future. In Techonological Society and Human Future; Velázquez, H., Ed.; Tirant Lo Blanch: Santiago, Chile, 2021; pp. 165–188. [Google Scholar]
- Potter, V.R. Bioethics, the Science of Survival. Perspect. Biol. Med. 1970, 14, 127–153. [Google Scholar] [CrossRef]
- Potter, V.R. Bioethics: Bridge to the Future; Prentice-Hall: Englewood Cliffs, NJ, USA, 1971. [Google Scholar]
- Beever, J.; Morar, N. The epistemic and ethical onus of ‘One Health’. Bioethics 2018, 33, 185–194. [Google Scholar] [CrossRef]
- Beever, J.; Morar, N. Interconnectedness and Interdependence: Challenges for Public Health Ethics. Am. J. Bioeth. 2017, 17, 19–21. [Google Scholar] [CrossRef]
- Capps, B.; Bailey, M.M.; Bickford, D.; Coker, R.; Lederman, Z.; Lover, A.; Lysaght, T.; Tambyah, P. Introducing One Health to the Ethical Debate About Zoonotic Diseases in Southeast Asia. Bioethics 2015, 29, 588–596. [Google Scholar] [CrossRef] [PubMed]
- Meagher, K.M. Can One Health Policy Help Us Expand an Ethics of Interconnection and Interdependence? AMA J. Ethics 2024, 26, E162–E170. [Google Scholar] [CrossRef]
- Plowright, R.K.; Ahmed, A.N.; Coulson, T.; Crowther, T.W.; Ejotre, I.; Faust, C.L.; Frick, W.F.; Hudson, P.J.; Kingston, T.; Nameer, P.O.; et al. Ecological countermeasures to prevent pathogen spillover and subsequent pandemics. Nat. Commun. 2024, 15, 2577. [Google Scholar] [CrossRef] [PubMed]
- Vora, N.M.; Hannah, L.; Lieberman, S.; Vale, M.M.; Plowright, R.K.; Bernstein, A.S. Want to prevent pandemics? Stop spillovers. Nature 2022, 605, 419–422. [Google Scholar] [CrossRef] [PubMed]
- OHHLEP. Prevention of Zoonotic Spilover. From Relying to Reducing the Risks at Source. Available online: https://www.who.int/publications/m/item/prevention-of-zoonotic-spillover (accessed on 6 August 2024).
- Vora, N.M.; Hannah, L.; Walzer, C.; Vale, M.M.; Lieberman, S.; Emerson, A.; Jennings, J.; Alders, R.; Bonds, M.H.; Evans, J.; et al. Interventions to Reduce Risk for Pathogen Spillover and Early Disease Spread to Prevent Outbreaks, Epidemics, and Pandemics. Emerg. Infect. Dis. 2023, 29, 1–9. [Google Scholar] [CrossRef]
- Aguirre, A.A.; Catherina, R.; Frye, H.; Shelley, L. Illicit Wildlife Trade, Wet Markets, and COVID-19: Preventing Future Pandemics. World Med. Health Policy 2020, 12, 256–265. [Google Scholar] [CrossRef] [PubMed]
- Aguirre, A. Developing Global Capacity in Conservation Medicine: Predicting and Preventing the Next Epidemic from Wildlife. Glob. Bioeth. 2011, 24, 51–54. [Google Scholar] [CrossRef]
- Doron, S.; Davidson, L.E. Antimicrobial Stewardship. Mayo Clin. Proc. 2011, 86, 1113–1123. [Google Scholar] [CrossRef]
- Aryee, A.; Price, N. Antimicrobial stewardship—Can we afford to do without it? Br. J. Clin. Pharmacol. 2015, 79, 173–181. [Google Scholar] [CrossRef] [PubMed]
- Johnson, T. Developing an Ethical Evaluation Framework for Coercive Antimicrobial Stewardship Policies. Public Health Ethics 2024, 17, 11–23. [Google Scholar] [CrossRef]
- Dyar, O.J.; Huttner, B.; Schouten, J.; Pulcini, C.; ESGAP (ESCMID Study Group for Antimicrobial Stewardship). What is antimicrobial stewardship? Clin. Microbiol. Infect. 2017, 23, 793–798. [Google Scholar] [CrossRef]
- Baquero, F.; Coque, T.M.; Martínez, J.-L.; Aracil-Gisbert, S.; Lanza, V.F. Gene Transmission in the One Health Microbiosphere and the Channels of Antimicrobial Resistance. Front. Microbiol. 2019, 10, 2892. [Google Scholar] [CrossRef]
- Malfrán, Y.I.M.; Baquero, O.S. Problematizing alterities for a feminist and decolonial understanding of One Health of Peripheries. Saude E Soc. 2023, 32, e220301pt. [Google Scholar] [CrossRef]
- Baquero, O.S.; Fernández, M.N.B.; Aguilar, M.A. From Modern Planetary Health to Decolonial Promotion of One Health of Peripheries. Front. Public Health 2021, 9, 637897. [Google Scholar] [CrossRef]
- DeGrazia, D. Animal Rights: A Very Short Introduction; Oxford University Press: Oxford, UK, 2002. [Google Scholar]
- Rowlands, M. Making light of the ethical? The ethics and politics of animal rights. In Ethical and Political Approaches to Nonhuman Animal Issues; Springer International Publishing: Berlin/Heidelberg, Germany, 2017; pp. 21–38. [Google Scholar] [CrossRef]
- Rowlands, M. Can Animals Be Moral? Oxford University Press: New York, NY, USA, 2013. [Google Scholar]
- Francione, G. Animals—Property or Persons? In Animal Rights: Current Debates and New Directions; Sunstein, C.R., Nussbaum, M.C., Eds.; Oxford University Press: Oxford, UK, 2004; pp. 108–142. [Google Scholar]
- Regan, T. The Case for Animal Rights; University of California Press: Berkeley, CA, USA; Los Angeles, CA, USA, 1983. [Google Scholar]
- Singer, P. Animal Liberation: A New Ethics for Our Treatment of Animals, 40th ed.; Open Road Media: New York, NY, USA, 2015. [Google Scholar]
- Kasperbauer, T.J.; Sandøe, P. Killing as a Welfare Issue. In The Ethics of Killing Animals; Višak, T., Garner, R., Eds.; Oxford University Press: Oxford, UK, 2015; pp. 17–31. [Google Scholar] [CrossRef]
- Persson, K.; Selter, F.; Neitzke, G.; Kunzmann, P. Philosophy of a “Good Death” in Small Animals and Consequences for Euthanasia in Animal Law and Veterinary Practice. Animals 2020, 10, 124. [Google Scholar] [CrossRef]
- UlAin, Q.; Whiting, T.L. Is a “Good Death” at the Time of Animal Slaughter an Essentially Contested Concept? Animals 2017, 7, 99. [Google Scholar] [CrossRef]
- Browning, H.; Veit, W. Is Humane Slaughter Possible? Animals 2020, 10, 799. [Google Scholar] [CrossRef]
- Yeates, J.W. Death is a Welfare Issue. J. Agric. Environ. Ethics 2009, 23, 229–241. [Google Scholar] [CrossRef]
- Higgin, M.; Evans, A.; Miele, M. A Good Kill: Socio-Technical Organizations of Farm Animal Slaughter. In Human and Other Animals; Carter, B.C.N., Ed.; Palgrave Macmillan: London, UK, 2011; Chapter 9; pp. 173–194. [Google Scholar] [CrossRef]
- Browning, H. No Room at the Zoo: Management Euthanasia and Animal Welfare. J. Agric. Environ. Ethics 2018, 31, 483–498. [Google Scholar] [CrossRef]
- Lecaros, J.A. Ecological Ethics: The road of Responsability towards Global Bioethics. Ramon Llull J. Appl. Ethics 2013, 4, 201–215. Available online: https://raco.pre.csuc.cat/index.php/rljae/article/view/281043 (accessed on 22 November 2022).
- Valdés, E.; Lecaros, J.A. Handbook of Bioethical Decisions. Volume II Scientific Integrity and Institutional Ethics; Springer: Cham, Switzerland, 2023. [Google Scholar]
- Valdés, E.; Lecaros, J.A. Handbook of Bioethical Decisions. Volume I Decisions at the Bench; Springer: Cham, Switzerland, 2023. [Google Scholar]
- Muzur, A.; Rinčić, I. Two kinds of globality: A comparison of Fritz Jahr and Van Rensselaer Potter’s bioethics. Glob. Bioeth. 2015, 26, 23–27. [Google Scholar] [CrossRef]
- Ortiz-Millán, G. Bioethics, globalization and pandemics. Glob. Bioeth. 2022, 33, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Fiore, R. Bioethics: Environmental. In Encyclopedia of Global Bioethics; ten Have, H., Ed.; Springer International Publishing: Cham, Switzerland, 2016; pp. 313–324. [Google Scholar] [CrossRef]
- Whitehouse, P.J. The Rebirth of Bioethics: Extending the Original Formulations of Van Rensselaer Potter. Am. J. Bioeth. 2003, 3, 26–31. [Google Scholar] [CrossRef]
- Potter, V.-R. Global Bioethics-Building on the Leopold Legacy; Michigan State University Press: East Lansing, MI, USA, 1988; Volume 11, Available online: www.jstor.org/stable/10.14321/j.ctt7ztc2s (accessed on 7 July 2024).
- Gardiner, S.M. Environmentalizing Bioethics: Planetary Health in a Perfect Moral Storm. Perspect. Biol. Med. 2022, 65, 569–585. [Google Scholar] [CrossRef]
- Macklin, R. A new definition for global bioethics: COVID-19, a case study. Glob. Bioeth. 2022, 33, 4–13. [Google Scholar] [CrossRef]
- Diller, E.R.; Williamson, L. Supporting One Health for Pandemic Prevention: The Need for Ethical Innovation. J. Bioethical. Inq. 2023, 20, 345–352. [Google Scholar] [CrossRef]
- Macpherson, C. Global bioethics: It’s past and future. Glob. Bioeth. 2022, 33, 45–49. [Google Scholar] [CrossRef]
- Tong, R. Towards a feminist global ethics. Glob. Bioeth. 2022, 33, 14–31. [Google Scholar] [CrossRef]
- Missoni, E. Global health, planetary health, One Health: Conceptual and ethical challenges and concerns. Theor. Med. Bioeth. 2024, 45, 241–250. [Google Scholar] [CrossRef]
- Bonilla-Aldana, D.K.; Holguin-Rivera, Y.; Perez-Vargas, S.; Trejos-Mendoza, A.E.; Balbin-Ramon, G.J.; Dhama, K.; Barato, P.; Lujan-Vega, C.; Rodriguez-Morales, A.J. Importance of the One Health approach to study the SARS-CoV-2 in Latin America. One Health 2020, 10, 100147. [Google Scholar] [CrossRef]
- Becerra, N.M.C.; Medellin, A.M.O.; Tomassone, L.; Chiesa, F.; De Meneghi, D. A Survey on One Health Approach in Colombia and Some Latin American Countries: From a Fragmented Health Organization to an Integrated Health Response to Global Challenges. Front. Public Health 2021, 9, 649240. [Google Scholar] [CrossRef]
- Cediel-Becerra, N.M.; Prieto-Quintero, S.; Garzon, A.D.M.; Villafañe-Izquierdo, M.; Rúa-Bustamante, C.V.; Jimenez, N.; Hernández-Niño, J.; Garnier, J. Woman-Sensitive One Health Perspective in Four Tribes of Indigenous People from Latin America: Arhuaco, Wayuú, Nahua, and Kamëntsá. Front. Public Health 2022, 10, 774713. [Google Scholar] [CrossRef]
- Hemida, M.G.; Abduallah, M.M.B. The SARS-CoV-2 outbreak from a one health perspective. One Health 2020, 10, 100127. [Google Scholar] [CrossRef]
- Hayman, D.T.; Adisasmito, W.B.; Almuhairi, S.; Behravesh, C.B.; Bilivogui, P.; Bukachi, S.A.; Casas, N.; Becerra, N.C.; Charron, D.F.; Chaudhary, A.; et al. Developing One Health surveillance systems. One Health 2023, 17, 100617. [Google Scholar] [CrossRef]
- Pepin, K.M.; Carlisle, K.; Anderson, D.; Baker, M.G.; Chipman, R.B.; Benschop, J.; French, N.P.; Greenhalgh, S.; McDougall, S.; Muellner, P.; et al. Steps towards operationalizing One Health approaches. One Health 2024, 18, 100740. [Google Scholar] [CrossRef] [PubMed]
- Arredondo-Rivera, M.; Barois, Z.; Monti, G.E.; Steketee, J.; Daburon, A. Bridging Food Systems and One Health: A key to preventing future pandemics? One Health 2024, 18, 100727. [Google Scholar] [CrossRef]
- Hattingh, J. Protection of the environment, the biosphere and biodiversity. In Handbook of Global Bioethics; ten Have, H.A.M.J., Gordijn, B., Eds.; Springer: Cham, Switzerland, 2014; Chapter 15; pp. 225–250. [Google Scholar] [CrossRef]
- Rawlinson, M.C. The concept of a feminist bioethics. Int. J. Fem. Approaches Bioeth. 2017, 10, 1–6. [Google Scholar] [CrossRef]
- Bhakuni, H. Glocalization of bioethics. Glob. Bioeth. 2022, 33, 65–77. [Google Scholar] [CrossRef]
- LeBlanc, A.B.; Williams-Jones, B. Applying the ecosystem approach to global bioethics: Building on the Leopold legacy. Glob. Bioeth. 2023, 34, 2280289. [Google Scholar] [CrossRef]
- Parker, M. A Deliberative Approach to Clinical Bioethics. In Clinical Bioethics. International Library of Ethics, Law, and the New Medicine; Drane, J.F., Thomasma, D.C., Nairn, W.D., Kipnis, K.T., Eds.; Springer: Dordrecht, The Netherlands, 2005; Volume 26, pp. 61–71. [Google Scholar]
- Finkler, K. Can bioethics be global and local, or must it be both? J. Contemp. Ethnogr. 2008, 37, 155–179. [Google Scholar] [CrossRef]
- Gielen, J. Dealing with Bioethical Issues in a Globalized World. Normativity in Bioethics; Springer: Cham, Switzerland, 2020. [Google Scholar] [CrossRef]
- Boudreau LeBlanc, A. At the confluence of ethics, laws and society: Global working theory merging bio-ethics. SN Soc. Sci. 2023, 4, 5. [Google Scholar] [CrossRef]
- LeBlanc, A.B.; Williams-Jones, B.; Aenishaenslin, C. Bio-Ethics and One Health: A Case Study Approach to Building Reflexive Governance. Front. Public Health 2022, 10, 648593. [Google Scholar] [CrossRef]
- Whitehouse, P.J. The Ecosystem of Bioethics: Building Bridges to Public Health. 2017. Available online: https://commons.case.edu/facultyworks/47 (accessed on 11 June 2024).
- Brescia, T. The rediscovery of Potterian bioethics. Glob. Bioeth. 2015, 26, 190–197. [Google Scholar] [CrossRef]
- Stepke, F.L. The Hermeutical Dimension of The Bioethics Enterprise. Notes on the Dialogical/Narrative Foundations of Bioethics. Acta Bioeth. 2018, 24, 153–159. Available online: https://actabioethica.uchile.cl/index.php/AB/article/view/51618 (accessed on 11 March 2024).
- Árnason, V. Toward Critical Bioethics. Camb. Q. Health Ethics 2015, 24, 154–164. [Google Scholar] [CrossRef]
- Ferrarello, S. Phenomenology of Bioethics: Technoethics and Lived-Experience; Springer: Cham, Switzerland, 2021; Available online: http://www.springer.com/series/16538 (accessed on 11 July 2024).
- Ten Have, H. Global health and global bioethics. Cad. Ibero-Am. De Direito Sanitário 2021, 10, 50–65. [Google Scholar] [CrossRef]
- Marshall, P.; Thomasma, D.C.; Bergsma, J. Intercultural Reasoning: The Challenge for International Bioethics. Camb. Q. Healthc. Ethics 1994, 5, 321–328. [Google Scholar]
- Griffiths, J.O. Bioethics, the Ontology of Life, and the Hermeneutics of Biology. In Phenomenology of Bioethics: Technoethics and Lived-Experience; Farrarello, S., Ed.; Springer: Cham, Switzerland, 2021; Chapter 1; pp. 1–21. [Google Scholar] [CrossRef]
- Thompson, P.B. From Synthetic Bioethics to One Bioethics: A Reply to Critics. Ethics Policy Environ. 2015, 18, 215–224. [Google Scholar] [CrossRef]
- Thompson, P.B.; List, M. Ebola Needs One Bioethics. Ethics Policy Environ. 2015, 18, 96–102. [Google Scholar] [CrossRef]
- Lederman, Z.; Capps, B. One Health Ethics: A Response to Pragmatism. J. Med. Ethics 2020, 46, 632–633. [Google Scholar] [CrossRef]
- Celermajer, D.; Schlosberg, D.; Wadiwel, D.; Winter, C. A Political Theory for a Multispecies, Climate-Challenged World: 2050. Political Theory 2023, 51, 39–53. [Google Scholar] [CrossRef]
- Chao, S.; Bolender, K.; Kirksey, E. The Promise of Multispecies Justice; Duke University Press: Durham, NC, USA; London, UK, 2022. [Google Scholar] [CrossRef]
- Heise, U.K. Stories for a multispecies future. Dialogues Hum. Geogr. 2018, 8, 96–99. [Google Scholar] [CrossRef]
- Emel, J.; Nirmal, P. A feminist research agenda for multispecies justice. In A Research Agenda for Animal Geographies; Hovorka, A., McCubbin, S., Van Patter, L., Eds.; Edward Elgar Publishing: Cheltenham, UK, 2021; Chapter 2. [Google Scholar] [CrossRef]
- Tschakert, P.; Schlosberg, D.; Celermajer, D.; Rickards, L.; Winter, C.; Thaler, M.; Stewart-Harawira, M.; Verlie, B. Multispecies justice: Climate-just futures with, for and beyond humans. Wiley Interdiscip. Rev. Clim. Change 2020, 12, e699. [Google Scholar] [CrossRef]
- Schlosberg, D. ‘Ecological Justice for the Anthropocene’. In Political Animals and Animal Politics; Wissenburg, M., Schlosberg, D., Eds.; Palgrave Macmillan: Houndmills, UK, 2023; pp. 75–89. [Google Scholar]
- Berkey, B. Prospects for an Inclusive Theory of Justice: The Case of Non-Human Animals. J. Appl. Philos. 2015, 34, 679–695. [Google Scholar] [CrossRef]
- Nussbaum, M. Justice for Animals: Our Collective Responsibility; Simon & Schuster: New York, NY, USA, 2022. [Google Scholar]
- Attfield, R. The Ethics of the Global Environment, 2nd ed.; Edinburgh University Press: Edinburgh, Scotland, 2015; Available online: http://ebookcentral.proquest.com/lib/acu/detail.action?docID=4306096 (accessed on 14 May 2024).
- Anthony, R.; Miller, D.S.; Hoenig, D.E.; Millar, K.M.; Goodwin, J.; Dean, W.R.; Grimm, H.; Meijboom, F.L.; Murphy, J.; Persico Murphy, E.; et al. Incorporate ethics into US public health plans. Science 2024, 383, 1066–1067. [Google Scholar] [CrossRef] [PubMed]
- Tauro, A.; Ojeda, J.; Caviness, T.; Moses, K.P.; Moreno-Terrazas, R.; Wright, T.; Zhu, D.; Poole, A.K.; Massardo, F.; Rozzi, R. Field Environmental Philosophy: A Biocultural Ethic Approach to Education and Ecotourism for Sustainability. Sustainability 2021, 13, 4526. [Google Scholar] [CrossRef]
- Valera, L. Intrinsic Values, Pantheism, and Ecology: Where Does Value Come From? In Pantheism and Ecology. Cosmological, Philosophical, and Theological Perspectives; Valera, L., Ed.; Springer: Cham, Switzerland, 2023; pp. 301–311. [Google Scholar]
- Palmer, C. Does nature matter? The place of the nonhuman in the ethics of climate change. In The Ethics of Global Climate Change; Arnold, D., Ed.; Cambridge University Press: Cambridge, UK, 2010; Chapter 13; pp. 272–291. [Google Scholar] [CrossRef]
- Palmer, C. Living Individuals: Biocentrism in Environmental Ethics. In The Oxford Handbook of Environmental Ethics; Gardiner, S.M., Thompson, A., Eds.; Oxford University Press: New York, NY, USA, 2017. [Google Scholar] [CrossRef]
- Palmer, C.; Fischer, B.; Gamborg, C.; Hampton, J.; Sandoe, P. Wildlife Ethics: The Ethics of Wildlife Management and Conservation; Wiley-Blackwell: Oxford, UK, 2023. [Google Scholar]
- Gruen, L. Expressing Entangled Empathy: A Reply. Hypatia 2017, 32, 452–462. [Google Scholar] [CrossRef]
- Cochrane, A.; Garner, R.; O’sullivan, S. Animal ethics and the political. Crit. Rev. Int. Soc. Political Philos. 2016, 21, 261–277. [Google Scholar] [CrossRef]
- Cochrane, A. Sentientist Politics; Oxford University Press: Oxford, UK, 2018; Volume 1. [Google Scholar] [CrossRef]
- van Herten, J.; Bovenkerk, B.; Verweij, M. One Health as a moral dilemma: Towards a socially responsible zoonotic disease control. Zoonoses Public Health 2018, 66, 26–34. [Google Scholar] [CrossRef]
- Su, Z.; McDonnell, D.; Cheshmehzangi, A.; Bentley, B.L.; Šegalo, S.; da Veiga, C.P.; Xiang, Y.T. Where should “Humans” be in “One Health”? Lessons from COVID-19 for One Health. Glob. Health 2024, 20, 24. [Google Scholar] [CrossRef]
- Brown, H.L.; Pursley, I.G.; Horton, D.L.; La Ragione, R. One health: A structured review and commentary on trends and themes. One Health Outlook 2024, 6, 17. [Google Scholar] [CrossRef]
- AVMA. One Health Initiative Task Force: A New Professional Imperative. July 2008. Available online: https://www.avma.org/sites/default/files/resources/onehealth_final.pdf (accessed on 1 September 2023).
- Johnson, L.S.M.; Ferdowsian, H.; Pierce, J. How One Health Instrumentalizes Nonhuman Animals. AMA J. Ethics 2024, 26, E184–E190. [Google Scholar] [CrossRef] [PubMed]
- Meisner, J.; McLeland-Wieser, H.; Traylor, E.E.; Hermesh, B.; Berg, T.; Roess, A.; Van Patter, L.; Rosenthal, A.; Davidovitch, N.; Rabinowitz, P.M. Relational One Health: A more-than-biomedical framework for more-than-human health, and lessons learned from Brazil, Ethiopia, and Israel. One Health 2024, 18, 100676. [Google Scholar] [CrossRef]
- Waltner-Toews, D. Zoonoses, One Health and complexity: Wicked problems and constructive conflict. Philos. Trans. R. Soc. B Biol. Sci. 2017, 372, 20160171. [Google Scholar] [CrossRef]
- Zinsstag, J.; Meyer, J.M.; Bonfoh, B.; Fink, G.; Dimov, A. One Health in human-environment systems: Linking health and the sustainable use of natural resources. CABI One Health 2024, 3, 1–11. [Google Scholar] [CrossRef]
- Pelluchon, C. Manifiesto animalista. Politizar la Causa Animal; Reservoir Books: Barcelona, Spain, 2018. [Google Scholar]
- Pelluchon, C. Reparemos el Mundo: Humanos, Animales, Naturaleza; Ned Ediciones: Barcelona, Spain, 2022. [Google Scholar]
- Turner, P.N. “Harm” and Mill’s Harm Principle. Ethics 2014, 124, 299–326. [Google Scholar] [CrossRef]
- Arato, J.; Claussen, K.; Heath, J.B. The Perils of Pandemic Exceptionalism. Am. J. Int. Law 2020, 114, 627–636. [Google Scholar] [CrossRef]
- Kirk, J.; McDonald, M. The Politics of Exceptionalism: Securitization and COVID-19. Glob. Stud. Q. 2021, 1, ksab024. [Google Scholar] [CrossRef]
- Roth, E. “Bats Who Harm” and “Bats Who May Be Harmed”: The Interspecies Politics of Virus Sampling. Soc. Anim. 2024, 1, 1–15. [Google Scholar] [CrossRef]
- Mysterud, A.; Rauset, G.R.; Van Moorter, B.; Andersen, R.; Strand, O.; Rivrud, I.M. The last moves: The effect of hunting and culling on the risk of disease spread from a population of reindeer. J. Appl. Ecol. 2020, 57, 2509–2518. [Google Scholar] [CrossRef]
- Lederman, Z.; Magalhães-Sant’ana, M.; Voo, T.C. Stamping Out Animal Culling: From Anthropocentrism to One Health Ethics. J. Agric. Environ. Ethics 2021, 34, 27. [Google Scholar] [CrossRef]
- Frutos, R.; Devaux, C. Mass culling of minks to protect the COVID-19 vaccines: Is it rational? New Microbes New Infect. 2020, 38, 100816. [Google Scholar] [CrossRef]
- Lesté-Lasserre, C. Pandemic dooms Danish mink—And mink research. Science 2020, 370, 754. [Google Scholar] [CrossRef] [PubMed]
- Cripps, E. Harming and Protecting Non-Humans. In Climate Change and the Moral Agent: Individual Duties in an Interdependent World; Oxford University Press: New York, NY, USA, 2013. [Google Scholar] [CrossRef]
- Degeling, C.; Lederman, Z.; Rock, M. Culling and the Common Good: Re-evaluating Harms and Benefits under the One Health Paradigm. Public Health Ethics 2016, 9, 244–254. [Google Scholar] [CrossRef]
- Halteman, M.C. Varieties of Harm to Animals in Industrial Farming. J. Anim. Ethics 2011, 1, 122–131. [Google Scholar] [CrossRef]
- Halabowski, D.; Rzymski, P. Taking a lesson from the COVID-19 pandemic: Preventing the future outbreaks of viral zoonoses through a multi-faceted approach. Sci. Total. Environ. 2020, 757, 143723. [Google Scholar] [CrossRef]
- Sebo, J.; White, A.; Sims, T. One Health and Multispecies Urban Infrastructure (peer reviewed). In One Health and the Law: Existing Frameworks, Intersections and Future Pathways; Kotzmann, J., Woolaston, K., Eds.; 2024; pp. 1–17. Available online: https://doi.org/10.2139/ssrn.4883654 (accessed on 11 August 2024).
- Origgi, G. Fear of principles? A cautious defense of the Precautionary Principle. Mind Soc. 2014, 13, 215–225. [Google Scholar] [CrossRef]
- von Essen, E.; Redmalm, D. License to Cull: A Research Agenda for Investigating the Necropolitics of Countryside Culling and Urban Pest Control. Soc. Anim. 2023, 1, 1–16. [Google Scholar] [CrossRef]
- Resnik, D.B. Human Health and the Environment: In Harmony or in Conflict? Health Care Anal. 2009, 17, 261–276. [Google Scholar] [CrossRef] [PubMed]
- McCulloch, S.P.; Reiss, M.J. Bovine Tuberculosis and Badger Control in Britain: Science, Policy and Politics. J. Agric. Environ. Ethics 2017, 30, 469–484. [Google Scholar] [CrossRef]
- Lynch, K.E.; Blumstein, D.T. Hidden ethical costsof conservation. Science 2020, 370, 179. [Google Scholar] [CrossRef]
- Park, J.M.; Koh, J.H.; Kim, J.M. Consumer awareness of culling and animal welfare. Food Control 2022, 133, 108495. [Google Scholar] [CrossRef]
- Van Herten, J. Considerations for an Ethic of One Health Towards a Socially Responsible Zoonotic Disease Control; Wageningen University: Wageningen, The Netherlands, 2021. [Google Scholar]
- Benis, A.; Haghi, M.; Deserno, T.M.; Tamburis, O. One Digital Health Intervention for Monitoring Human and Animal Welfare in Smart Cities: Viewpoint and Use Case. MIR Med. Inform. 2023, 11, e43871. [Google Scholar] [CrossRef]
- Farlow, A.; Torreele, E.; Gray, G.; Ruxrungtham, K.; Rees, H.; Prasad, S.; Gomez, C.; Sall, A.; Magalhães, J.; Olliaro, P.; et al. The Future of Epidemic and Pandemic Vaccines to Serve Global Public Health Needs. Vaccines 2023, 11, 690. [Google Scholar] [CrossRef] [PubMed]
- Destoumieux-Garzón, D.; Matthies-Wiesler, F.; Bierne, N.; Binot, A.; Boissier, J.; Devouge, A.; Garric, J.; Gruetzmacher, K.; Grunau, C.; Guégan, J.-F.; et al. Getting out of crises: Environmental, social-ecological and evolutionary research is needed to avoid future risks of pandemics. Environ. Int. 2021, 158, 106915. [Google Scholar] [CrossRef]
- Wilkes, M.S.; Conrad, P.A.; Winer, J.N. One Health–One Education: Medical and Veterinary Inter-Professional Training. J. Vet. Med. Educ. 2019, 46, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Lerner, H.; Berg, C. The concept of health in One Health and some practical implications for research and education: What is One Health? Infect. Ecol. Epidemiol. 2015, 5, 25300. [Google Scholar] [CrossRef] [PubMed]
- Nieuwland, J.; Meijboom, F.L.B. One Health: How Interdependence Enriches Veterinary Ethics Education. Animals 2019, 10, 13. [Google Scholar] [CrossRef] [PubMed]
- Togami, E.; Gardy, J.L.; Hansen, G.R.; Poste, G.H.; Rizzo, D.M.; Wilson, M.E.; Mazet, J.A.K.; University of British Columbia; Consulting, L.H.; Arizona State University. Core Competencies in One Health Education: What Are We Missing? NAM Perspect. 2018, 8, 14–20. [Google Scholar] [CrossRef]
- Spanjol, K.; Zucca, P. Biophilia, One Health, and Humane Education: Mitigating global risk through embracing humanity’s interconnection with the natural world. In Socio-Political Risk Management. Assessing and Managing Global Insecurity; Engemann, K.J., Lavery, C.F., Sheehan, J.M., Eds.; De Gruyter: Berlin, Germany; London, UK, 2023; Chapter 7; pp. 109–132. [Google Scholar]
- European Food Safety Authority (EFSA) and European Centre for Disease Prevention and Control (ECDC). The European Union One Health 2022 Zoonoses Report. EFSA J. 2023, 21, 1–222. [Google Scholar] [CrossRef]
- Lehtimaki, S.; Hannon, E.; Hanbali, L.; Soltan, D.-F.; Peek, K.; Nassiri-Ansari, T.; Schwalbe, N. Where there is a will, there is a way: Independent assessment of member state compliance with the pandemic agreement. Lancet Glob. Health 2024, 12, e18–e19. [Google Scholar] [CrossRef]
- Semenza, J.C.; Rocklöv, J.; Ebi, K.L. Climate Change and Cascading Risks from Infectious Disease. Infect. Dis. Ther. 2022, 11, 1371–1390. [Google Scholar] [CrossRef]
- Agyarko, R.; Al Slail, F.; Garrett, D.O.; Gentry, B.; Gresham, L.; Underwood, M.L.K.; Macfarlane, S.B.; Moussif, M. The imperative for global cooperation to prevent and control pandemics. In Modernizing Global Health Security to Prevent, Detect, and Respond; McNabb, S.J.N., Shaikh, A.T., Haley, C.J., Eds.; Academic Press: London, UK, 2024; Chapter 4. [Google Scholar]
- Scully, J.L. COVID, Vulnerability, and the Death of Solidarity: “Who Do We Not Save?”. J. Bioethical Inq. 2023, 20, 601–606. [Google Scholar] [CrossRef]
- Tomasini, F. Solidarity in the Time of COVID-19? Camb. Q. Health Ethics 2020, 30, 234–247. [Google Scholar] [CrossRef]
- Branda, F. Social impact: Trusting open science for future pandemic resilience. Soc. Impacts 2024, 3, 100058. [Google Scholar] [CrossRef]
- Besançon, L.; Peiffer-Smadja, N.; Segalas, C.; Jiang, H.; Masuzzo, P.; Smout, C.; Billy, E.; Deforet, M.; Leyrat, C. Open science saves lives: Lessons from the COVID-19 pandemic. BMC Med. Res. Methodol. 2021, 21, 117. [Google Scholar] [CrossRef]
- Pettan-Brewer, C.; Martins, A.F.; de Abreu, D.P.B.; Brandão, A.P.D.; Barbosa, D.S.; Figueroa, D.P.; Cediel, N.; Kahn, L.H.; Brandespim, D.F.; Velásquez, J.C.C.; et al. From the Approach to the Concept: One Health in Latin America-Experiences and Perspectives in Brazil, Chile, and Colombia. Front. Public Health 2021, 9, 687110. [Google Scholar] [CrossRef]
- WHO. Intergovernmental Negotiating Body to Draft and Negotiate a WHO Convention, Agreement or Other International Instrument on Pandemic Prevention, Preparedness and Response. Geneva, May 2024. Available online: https://apps.who.int/gb/inb/ (accessed on 10 June 2024).
- Rink, E.; Stotz, S.A.; Johnson-Jennings, M.; Huyser, K.; Collins, K.; Manson, S.M.; Berkowitz, S.A.; Hebert, L.; Shanks, C.B.; Begay, K.; et al. “We don’t separate out these things. Everything is related”: Partnerships with Indigenous Communities to Design, Implement, and Evaluate Multilevel Interventions to Reduce Health Disparities. Prev. Sci. 2024, 25, 474–485. [Google Scholar] [CrossRef]
- A Barrett, M.; A Bouley, T.; Stoertz, A.H.; Stoertz, R.W. Integrating a One Health approach in education to address global health and sustainability challenges. Front. Ecol. Environ. 2010, 9, 239–245. [Google Scholar] [CrossRef]
- Reaser, J.K.; Witt, A.; Tabor, G.M.; Hudson, P.J.; Plowright, R.K. Ecological countermeasures for preventing zoonotic disease outbreaks: When ecological restoration is a human health imperative. Restor. Ecol. 2021, 29, e13357. [Google Scholar] [CrossRef] [PubMed]
- FAO. The Emergency Prevention System for Animal Health Enhancing the Prevention and Control of High-Impact Animal and Zoonotic Diseases through Biosecurity and One Health Strategic Plan (2023–2026). 2023. Available online: https://openknowledge.fao.org/server/api/core/bitstreams/cbea52a7-8b1f-46ff-a3d1-3d6acc72decd/content (accessed on 10 June 2024).
- Ritter, C.; King, M. One Health Une santé One Welfare: The role of veterinary professionals. Can. Vet. J. 2023, 64, 784–786. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10352033/ (accessed on 26 June 2024).
- Marchant-Forde, J.N.; Boyle, L.A. COVID-19 Effects on Livestock Production: A One Welfare Issue. Front. Vet. Sci. 2020, 7, 585787. [Google Scholar] [CrossRef]
- Moreno-Madriñan, M.J.; Kontowicz, E. Stocking Density and Homogeneity, Considerations on Pandemic Potential. Zoonotic Dis. 2023, 3, 85–92. [Google Scholar] [CrossRef]
- Guo, Y.; Ryan, U.; Feng, Y.; Xiao, L. Association of Common Zoonotic Pathogens with Concentrated Animal Feeding Operations. Front. Microbiol. 2022, 12, 810142. [Google Scholar] [CrossRef]
- Stel, M.; Eggers, J.; Alonso, W.J. Mitigating Zoonotic Risks in Intensive Farming: Solutions for a Sustainable Change. Ecohealth 2022, 19, 324–328. [Google Scholar] [CrossRef]
- Butler, C.D. Bioethics, climate change, and civilization. J. Clim. Chang. Health 2024, 18, 100329. [Google Scholar] [CrossRef]
- Okeke, I.N.; de Kraker, M.E.; Van Boeckel, T.P.; Kumar, C.K.; Schmitt, H.; Gales, A.C.; Bertagnolio, S.; Sharland, M.; Laxminarayan, R. The scope of the antimicrobial resistance challenge. Lancet 2024, 403, 2426–2438. [Google Scholar] [PubMed]
- Djordjevic, S.P.; Jarocki, V.M.; Seemann, T.; Cummins, M.L.; Watt, A.E.; Drigo, B.; Wyrsch, E.R.; Reid, C.J.; Donner, E.; Howden, B.P. Genomic surveillance for antimicrobial resistance—A One Health perspective. Nat. Rev. Genet. 2023, 25, 142–157. [Google Scholar] [CrossRef]
- Hernández, A.C. Poultry and Avian Diseases. In Encyclopedia of Agriculture and Food Systems, 2nd ed.; Van Alfen, N., Ed.; Elsevier: San Diego, CA, USA, 2014. [Google Scholar]
- Alam, M.-U.; Rahman, M.; Masud, A.A.; Islam, M.A.; Asaduzzaman, M.; Sarker, S.; Rousham, E.; Unicomb, L. Human exposure to antimicrobial resistance from poultry production: Assessing hygiene and waste-disposal practices in Bangladesh. Int. J. Hyg. Environ. Health 2019, 222, 1068–1076. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.K.; Hussein, S.; Qurbani, K.; Ibrahim, R.H.; Fareeq, A.; Mahmood, K.A.; Mohamed, M.G. Antimicrobial resistance: Impacts, challenges, and future prospects. J. Med. Surg. Public Health 2024, 2, 100081. [Google Scholar] [CrossRef]
- Alonso, A.I.; South, N. Incorporating a One Health Approach into the Study of Environmental Crimes and Harms: Towards a ‘One Health Green Criminology. Br. J. Criminol. 2024, azae047. [Google Scholar] [CrossRef]
- Barrett, M.A.; Osofsky, S.A. One Health: Interdependence of People, other Species and the Planet; Saunders Elsevier: Philadelphia, PA, USA, 2013. [Google Scholar]
- Leboeuf, A. Making Sense of One Health: Cooperating at the Human-Animal-Ecosystem Health Interface, IFRI. Heath and Environment Reports, No. 7, April 2011. Available online: https://www.ifri.org/en/publications/etudes-de-lifri/making-sense-one-health-cooperating-human-animal-ecosystem-health (accessed on 20 July 2024).
- The Pandemic Treaty: Shameful and unjust. Lancet 2024, 403, 781. [CrossRef]
- van Vliet, N.; Muhindo, J.; Nyumu, J.; Enns, C.; Massé, F.; Bersaglio, B.; Cerutti, P.; Nasi, R. Understanding Factors that Shape Exposure to Zoonotic and Food-Borne Diseases Across Wild Meat Trade Chains. Hum. Ecol. 2022, 50, 983–995. [Google Scholar] [CrossRef]
- European Commission. EU One Health Action Plan against AMR. 2017, p. 24. Available online: http://www.who.int/entity/drugresistance/documents/surveillancereport/en/index.html%0A (accessed on 11 June 2024).
- Hibbard, R.; Mendelson, M.; Page, S.W.; Ferreira, J.P.; Pulcini, C.; Paul, M.C.; Faverjon, C. Antimicrobial stewardship: A definition with a One Health perspective. npj Antimicrob. Resist. 2024, 2, 15. [Google Scholar] [CrossRef]
- Osińska, A.; Korzeniewska, E.; Harnisz, M.; Felis, E.; Bajkacz, S.; Jachimowicz, P.; Niestępski, S.; Konopka, I. Small-scale wastewater treatment plants as a source of the dissemination of antibiotic resistance genes in the aquatic environment. J. Hazard. Mater. 2020, 381, 121221. [Google Scholar] [CrossRef]
- ten Have, H. Equity, Justice and Responsibility in the Perspective of Global Health. In Healing Mission: The Catholic Church in the Era of Global Public Health; Gabric, B., Hofmann, S., Eds.; Verlag Friedrich Pustet: Regensburg, Germany, 2023; pp. 173–198. [Google Scholar]
- Singer, A.C.; Shaw, H.; Rhodes, V.; Hart, A. Review of Antimicrobial Resistance in the Environment and Its Relevance to Environmental Regulators. Front. Microbiol. 2016, 7, 1728. [Google Scholar] [CrossRef]
- Garcia, S.N.; Osburn, B.I.; Jay-Russell, M.T. One Health for Food Safety, Food Security, and Sustainable Food Production. Front. Sustain. Food Syst. 2020, 4, 1. [Google Scholar] [CrossRef]
- Koutsoumanis, K.P.; Lianou, A.; Sofos, J.N. Food Safety: Emerging Pathogens. In Encyclopedia of Agriculture and Food Systems; Elsevier: San Diego, CA, USA, 2014; Available online: https://search.credoreference.com/articles/Qm9va0FydGljbGU6MzE4MTc0NQ==?aid=257358</div> (accessed on 9 June 2024).
- Nieuwland, J.; Meijboom, F.L.B. One-Health as a normative concept: Implications for food safety at the wildlife interface. In Know Your Food: Food Ethics and Innovation; Wageningen Academic Publishers: Wageningen, The Netherlands, 2013; pp. 132–137. [Google Scholar]
- Berry, S.L.; Chipman, S.; Gregg, M.E.; Haffey, H.; Devenot, N.; McMullin, J. Justice, Equity, Diversity, Inclusion, and Belonging: A Health Humanities Consortium Initiative. J. Med. Humanit. 2024, 45, 283–324. [Google Scholar] [CrossRef] [PubMed]
- Sharan, M.; Vijay, D.; Yadav, J.P.; Bedi, J.S.; Dhaka, P. Surveillance and response strategies for zoonotic diseases: A comprehensive review. Sci. One Health 2023, 2, 100050. [Google Scholar] [CrossRef]
- Ballash, G.A.; Parker, E.M.; Mollenkopf, D.F.; Wittum, T.E. The One Health dissemination of antimicrobial resistance occurs in both natural and clinical environments. J. Am. Vet. Med. Assoc. 2024, 262, 1–8. [Google Scholar] [CrossRef]
- Vezeau, N.; Kahn, L. Spread and mitigation of antimicrobial resistance at the wildlife-urban and wildlife-livestock interfaces. J. Am. Vet. Med. Assoc. 2024, 262, 1–7. [Google Scholar] [CrossRef]
- Mitchell, J.; Cooke, P.; Ahorlu, C.; Arjyal, A.; Baral, S.; Carter, L.; Dasgupta, R.; Fieroze, F.; Fonseca-Braga, M.; Huque, R.; et al. Community engagement: The key to tackling Antimicrobial Resistance (AMR) across a One Health context? Glob. Public Health 2021, 17, 2647–2664. [Google Scholar] [CrossRef]
- Marvasi, M.; Casillas, L.; Vassallo, A.; Purchase, D. Educational Activities for Students and Citizens Supporting the One-Health Approach on Antimicrobial Resistance. Antibiotics 2021, 10, 1519. [Google Scholar] [CrossRef]
- Khazatzadeh-Mahani, A.; Ruckert, A.; Labonté, R. Global Health Diplomacy. In The Oxford Handbook of Global Health Politics; McInnes, C., Lee, K., Youde, J., Eds.; Oxford University Press: New York, NY, USA, 2020; Chapter 6; pp. 102–121. [Google Scholar] [CrossRef]
- Rushton, S. Security and Health. In The Oxford Handbook of Global Health Politics; McInnes, C., Lee, K., Youde, J., Eds.; Oxford University Press: New York, NY, USA, 2020; Chapter 7; pp. 122–141. [Google Scholar] [CrossRef]
- Oyekan, A.O.; Balogun, W.A. Borders, Boundaries, and Identities: Navigating the Barriers to Solidarity and Cohesion in a Pandemic. In Global Health, Humanity and the COVID-19 Pandemic; Egbokhare, F., Afolayan, A., Eds.; Palgrave Macmillan: Cham, Switzerland, 2023; pp. 197–222. [Google Scholar] [CrossRef]
- WHO. Ethical Issues Associated with Vector-Borne Diseases. Report of a WHO Scoping Meeting. Geneva. 2017. Available online: http://apps.who.int/bookorders (accessed on 16 March 2019).
- Waltner-Toews, D. One ecosystem, one food system: The social and ecological context of food safety strategies. J. Agric. Environ. Ethics 1991, 4, 49–59. [Google Scholar] [CrossRef]
- LeBlanc, A.B.; Motulsky, A.; Moreault, M.-P.; Liang, M.Q.; Feze, I.N.; Côteaux, L.D. Building a Logic Model to Foster Engagement and Learning Using the Case of a Province-Wide Multispecies Antimicrobial Use Monitoring System. Eval. Rev. 2023, 48, 736–765. [Google Scholar] [CrossRef]
- van Dam, A.; van Engelen, W.; Müller-Mahn, D.; Agha, S.; Junglen, S.; Borgemeister, C.; Bollig, M. Complexities of multispecies coexistence: Animal diseases and diverging modes of ordering at the wildlife–livestock interface in Southern Africa. Environ. Plan. E Nat. Space 2023, 7, 353–374. [Google Scholar] [CrossRef]
- Mota-Rojas, D.; Monsalve, S.; Lezama-García, K.; Mora-Medina, P.; Domínguez-Oliva, A.; Ramírez-Necoechea, R.; Garcia, R.d.C.M. Animal Abuse as an Indicator of Domestic Violence: One Health, One Welfare Approach. Animals 2022, 12, 977. [Google Scholar] [CrossRef] [PubMed]
- Quadripartite. Quadripartite Key Recommendations and Priorities for the 2024 UNGA High-Level Meeting on Antimicrobial Resistance (AMR). 2024. Available online: https://www.unep.org/resources/policy-and-strategy/quadripartite-key-recommendations-and-priorities-2024-unga-high-level (accessed on 8 August 2024).
- IACG-UN. No Time to Wait: Securing the Future from Drug-Resistant Infections Report to the Secretary-General of the United Nations. 2019. Available online: https://www.who.int/publications/i/item/no-time-to-wait-securing-the-future-from-drug-resistant-infections (accessed on 8 August 2024).
- Rozzi, R. Inter-species and Inter-cultural Encounters: The Biocultural Education Program of the Omora Ethnobotanical Park. In Field Environmental Philosophy: Education for Biocultural Conservation; Springer: Berlin/Heidelberg, Germany, 2023; pp. 153–174. [Google Scholar] [CrossRef]
- Hourdequin, M. Environmental Ethics, From Theory and Practice; Bloomsbury: London, UK, 2015. [Google Scholar]
- Rozzi, R.; Tauro, A.; Avriel-Avni, N.; Wright, T.; May, R.H., Jr. Field Environmental Philosophy. Education for Biocultural Conservation; Springer: Cham, Switzerland, 2023. [Google Scholar]
- Boyd, K. Global health justice: Epistemic theory and pandemic practice. J. Med. Ethics 2023, 49, 303–304. [Google Scholar] [CrossRef]
- de Vries, J.; Pratt, B. Epistemic justice in bioethics: Interculturality and the possibility of reparations. J. Med. Ethics 2023, 49, 347. [Google Scholar] [CrossRef]
- Broadbent, A.; Ncube, L. Intercultural Medical Disagreements: Ebola vs. COVID-19. In The Politics of Knowledge in the Biomedical Sciences; Jansen, J., Auerbach, J., Eds.; Springer: Cham, Switzerland, 2023. [Google Scholar]
- Chao, S.; Celermajer, D. Introduction: Multispecies Justice. Cult. Politics 2023, 19, 1–17. [Google Scholar] [CrossRef]
- Sandler, R. De-extinction: Costs, benefits and ethics. Nat. Ecol. Evol. 2017, 1, 105. [Google Scholar] [CrossRef] [PubMed]
- Sandler, R. De-extinction and Conservation Genetics in the Anthropocene. Häst. Cent. Rep. 2017, 47, S43–S47. [Google Scholar] [CrossRef]
- Sandler, R. On the Massness of Mass Extinction. Philosophia 2022, 50, 2205–2220. [Google Scholar] [CrossRef]
- Gardiner, S.M. On the Scope of Institutions for Future Generations: Defending an Expansive Global Constitutional Convention That Protects against Squandering Generations. In Ethics and International Affairs; Cambridge University Press: Cambridge, UK, 2022; pp. 157–178. [Google Scholar] [CrossRef]
- WHO. Compendium of WHO and Other UN Guidance on Health and Environment 2024 Update. 2023. Available online: https://reliefweb.int/report/world/compendium-who-and-other-un-guidance-health-and-environment-2024-update (accessed on 14 July 2024).
- Benis, A.; Tamburis, O. The Need for Green and Responsible Medical Informatics and Digital Health: Looking Forward with One Digital Health. Yearb. Med. Inform. 2023, 32, 007–009. [Google Scholar] [CrossRef]
- Tamburis, O.; Benis, A. One Digital Health for more FAIRness. Methods Inf. Med. 2022, 61, E116–E124. [Google Scholar] [CrossRef] [PubMed]
- Bankoff, G. The Historical Geography of Disaster: ‘Vulnerability’ and ‘Local Knowledge’ in Western Discourse. In Mapping Vulnerability: Disasters, Development and People; Bankoff, G., Frerks, G., Hilhorst, D., Eds.; Taylor and Francis: New York, NY, USA, 2004; Chapter 2; pp. 25–36. [Google Scholar]
- Bankoff, G. Rendering the World Unsafe: ‘Vulnerability’ as Western Discourse. Disasters 2001, 25, 19–35. [Google Scholar] [CrossRef]
- Lederberg, J. Infectious History. Science 2000, 288, 287–293. [Google Scholar] [CrossRef] [PubMed]
- Cassidy, A. Humans, Other Animals and ‘One Health’ in the Early Twenty-First Century. In Animals and the Shaping of Modern Medicine. One Health and its Histories; Woods, A., Bresalier, M., Cassidy, A., Dentiger, R.M., Eds.; Palgrave Macmillan: Cham, Switzerland, 2018; Chapter 6; pp. 193–224. [Google Scholar]
- Woods, A.; Bresalier, M.; Cassidy, A.; Mason Dentinger, R. Animals and the Shaping of Modern Medicine. One Health and Its Histories; Palgrave Macmillan: Cham, Switzerland, 2018; Available online: http://www.springer.com/series/15183 (accessed on 18 October 2018).
- Schwalbe, N.; Hannon, E.; Lehtimaki, S. The new pandemic treaty: Are we in safer hands? Probably not. BMJ 2024, 384, q477. [Google Scholar] [CrossRef] [PubMed]
- Bortolotti, L.; Murphy-Hollies, K. Exceptionalism at the Time of covid-19: Where Nationalism Meets Irrationality. Dan. Yearb. Philos. 2022, 55, 90–111. [Google Scholar] [CrossRef]
- Ricard, J.; Medeiros, J. Using misinformation as a political weapon: COVID-19 and Bolsonaro in Brazil. Harv. Kennedy Sch. Misinformation Rev. 2020, 1, 1–6. [Google Scholar] [CrossRef]
- Rodriguez, J. God, Home, and Thinking in the Place: What Kind of Pantheism Did Thoreau Endorse? In Pantheism and Ecology. Cosmological, Philosophical, and Theological Perspectives; Valera, L., Ed.; Springer: Berlin/Heidelberg, Germany, 2023; pp. 183–200. [Google Scholar] [CrossRef]
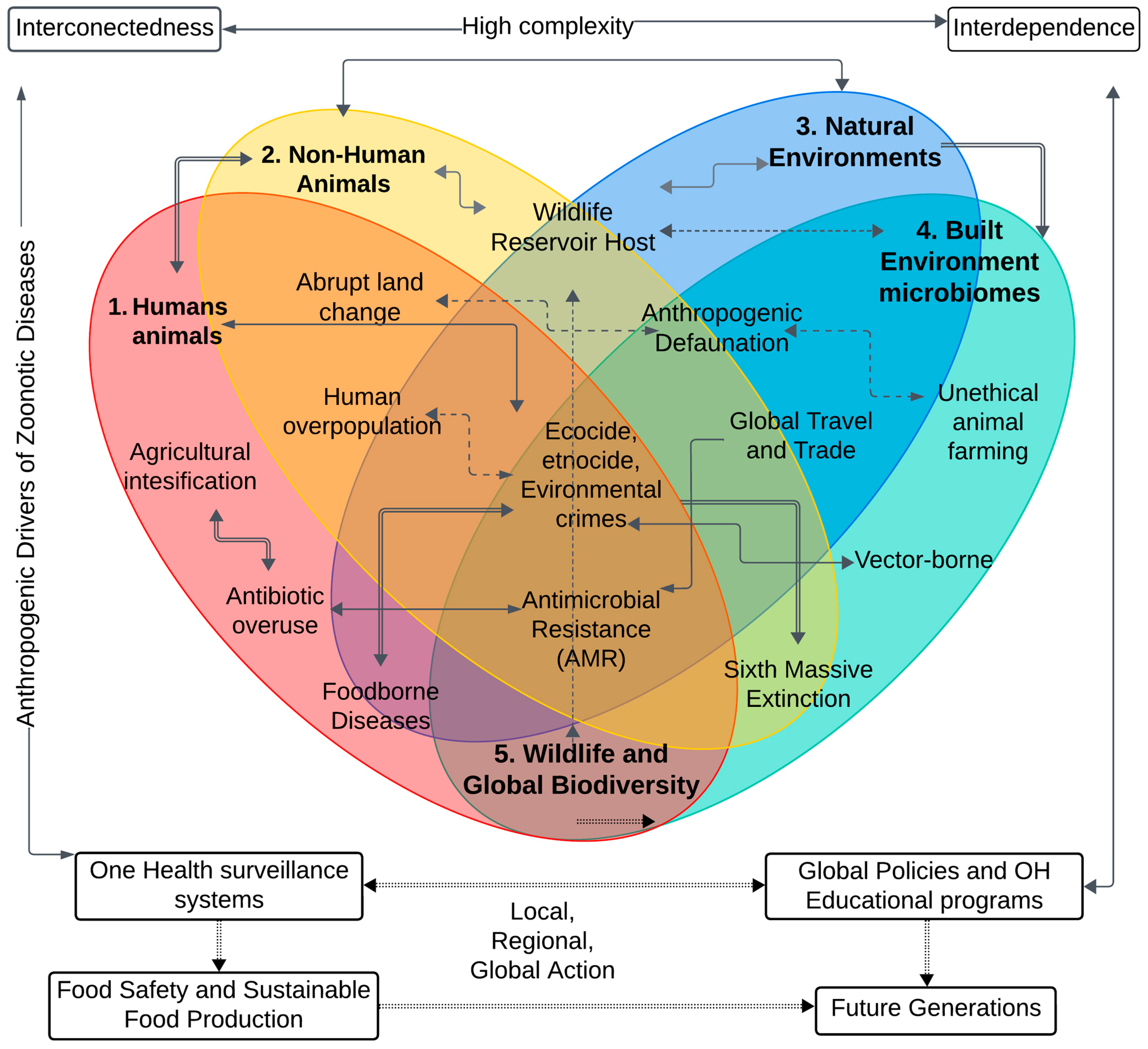
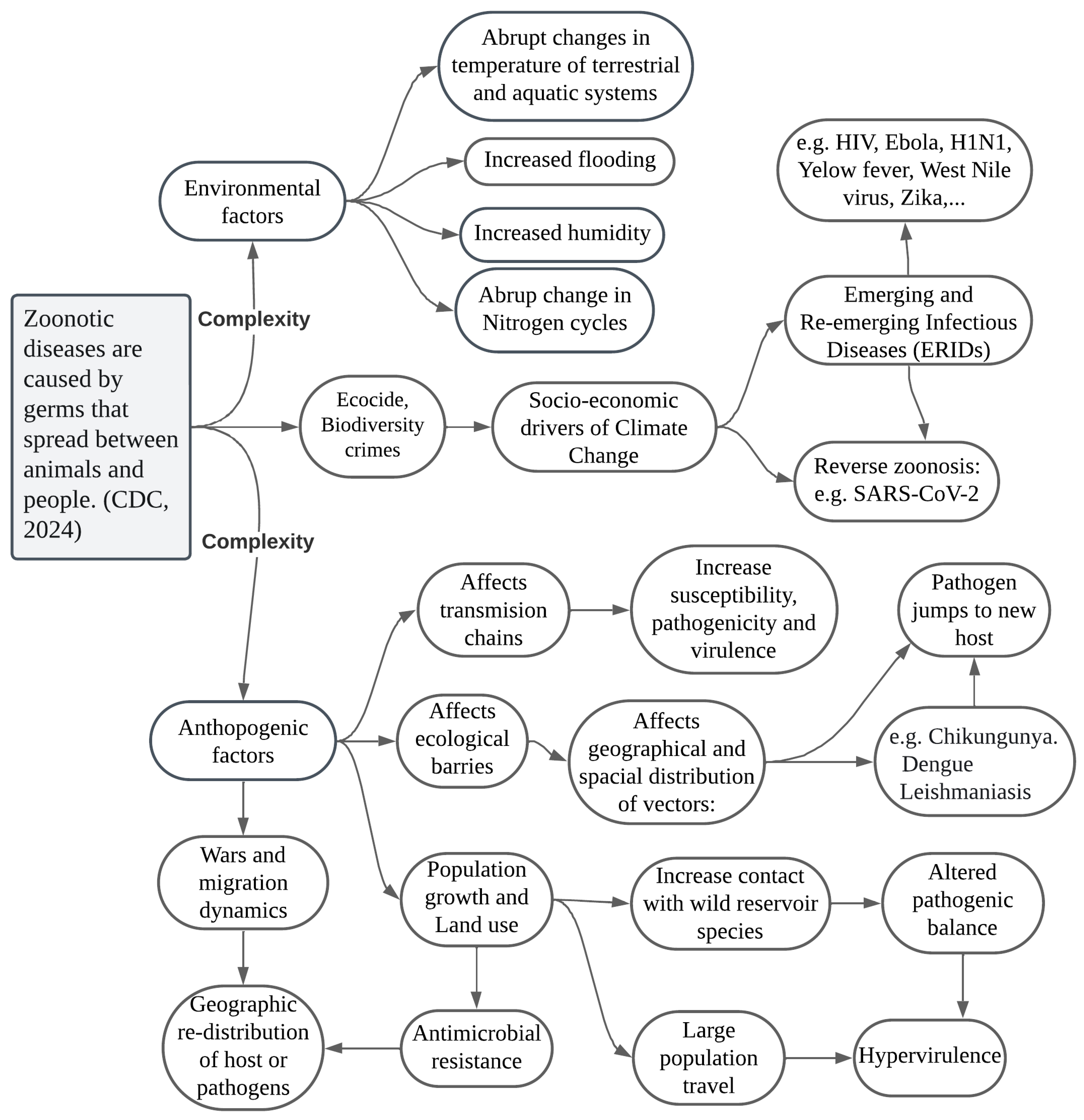
| Ethical Principles | Zoonotic Ethics Guidelines | Problem/Challenge |
|---|---|---|
| Autonomy | Respect the autonomy of communities and individuals in One Health decision-making. | Ensuring individual and community rights are upheld during public health interventions. |
| Beneficence | Implement measures that maximize well-being and minimize harm for both humans, animals, and environments. | Balancing the benefits of interventions against potential risks and harms. |
| Non-maleficence | Avoid actions that cause unnecessary harm, such as the indiscriminate culling of animals without comprehensive ethical analysis. | Preventing unethical practices that could cause harm to animals and ecosystems. |
| Justice | Ensure the equitable distribution of resources and treatments to prevent and control zoonotic diseases. Ensuring universal access to health innovations and vaccines. | Addressing disparities in access to healthcare and resources for disease prevention and control. |
| Ethical Deliberation/ Constructive Conflict | Consider all relevant interests at stake and integrate the value and welfare of human animals when implementing management plans and measures to control zoonoses. Strategies: Multi-layered and multi-actor assessment. Context-dependent analysis | Mitigate the negative impacts and side-effects on nonhuman animals of strategies and plans to control zoonoses and epidemic risks. |
| Environmental Responsibility | It is imperative to adopt responsible practices in all sectors that safeguard ecosystems and biodiversity, acknowledging their integral role in One Health and the secure survival of future generations. | Mitigating the impact of human activities on ecosystems and preventing biodiversity loss. |
| Transparency and Communication | Maintain open and honest communication with the public about risks and measures taken to control zoonoses. | Building public trust and ensuring informed participation in public health measures. |
| Respect for Life | Value and protect the lives of all living beings, recognizing the interdependence between humans, animals, and environments. | Promoting a holistic view of life that includes the well-being of all species. |
| Solidarity and Cooperation | Promote international collaboration and solidarity among nations to combat global zoonotic threats. | Fostering global cooperation to address transboundary zoonotic disease threats. |
| Precaution and Prudence | Adopt preventive and prudent measures in the face of scientific uncertainty and potential risks of new zoonoses. | Taking proactive steps to prevent outbreaks even when full scientific certainty is not available. |
| Intergenerational Equity | Make decisions that do not compromise the health and well-being of future generations. Avoid practices and policies that transfer risks and damages to future generations. Inter/trans-generational justices. | Ensuring sustainable practices that do not deplete resources or harm future generations. |
| Care | It is imperative that robust legislation be enacted to address the crime of ecocide, including the introduction of criminal laws to deter and punish the systematic destruction of biodiversity and the trafficking of wildlife. | Mitigation of large-scale species extinction and crimes against biodiversity |
| Category | Recommendation | Rationale |
|---|---|---|
| Preventive Action | Accelerate the implementation of the One Health approach from a preventive and anticipatory lens. Shifting from reactive to proactive zoonotic risk mitigation model is essential. | Implement a preventive One Health strategy with a precautionary approach helps to address the root causes of AMR and promotes sustainable practices [135,318]. |
| Biosecurity Processes | Ensure that all medical and veterinary waste undergoes effective decontamination processes, such as autoclaving or chemical disinfection, to eliminate pathogens and reduce the risk of AMR. | Proper waste management and biosecurity tools minimizes the ecological footprint of animal and healthcare practices, reducing environmental pollution and the spread of AMR [319]. |
| Sustainable Food and Agricultural Practices | Promote sustainable agriculture and livestock practices, reducing antimicrobial use in food production to prevent resistant pathogens. | Sustainable practices prevent AMR by reducing unnecessary antimicrobial use and promoting ethical treatment of animals and the environment [317,320,321,322]. |
| Public Policy | Educate public policy experts on the complexity of zoonoses, EIDs, and AMR from a One Health and multispecies justice perspective. | Informed policymakers can develop more effective policies to address AMR, considering its broader impact on public health and the environment [253,323,324]. |
| Antimicrobial Stewardship | Promote interdisciplinary and Antimicrobial Stewardship programs to ensure the responsible use of antimicrobials in human and animal healthcare, agriculture, and food-chains. | Antimicrobial Stewardship programs help mitigate the overuse and misuse of antimicrobials, reducing the development of resistant pathogens [319,325,326,327]. |
| Infrastructure Improvement | Improve infrastructure for clean water, sanitation, and waste management to prevent the spread of resistant microbes. | Improving infrastructure tackles AMR’s root causes in low-resource settings by addressing inadequate sanitation and waste management [322,327]. |
| Ethical Reflection | Encourage ethical reflection on healthcare practices, animal treatment, and environmental impact in decision-making processes. | Ethical considerations ensure that actions taken to address AMR are just, sustainable, and responsible, benefiting all stakeholders involved [67,68,70,72]. |
| One Health Education and Antibiotic Awareness | Increase public awareness and education about the causes and consequences of AMR and the importance of responsible antimicrobial use. | One Health education promotes responsible behavior and support for AMR-reducing policies, making ethical reflection on AMR crucial for a sustainable and just future [77,328]. |
| Global Cooperation | Strengthen international cooperation and coordination in monitoring, research, and response to AMR. | Global cooperation is crucial for addressing AMR, as it is a transboundary issue that requires coordinated efforts across countries and regions. [329,330,331]. |
| Food Chains and Water Systems | Strengthen and enforce regulations on the use of antibiotics in agriculture and aquaculture. | By regulating the use of antibiotics in food production, we can reduce the development of antibiotic-resistant bacteria in the environment, which can be transferred to humans through the food chain [323,324,332,333]. |
| Multispecies Justice | Implement comprehensive OH policies that prioritize the welfare and the intrinsic value of all including environments, human, and nonhuman animals affected by AMR. | Addressing AMR ethically requires considering the impact on diverse species and ecosystems, ensuring fair treatment and health outcomes for all [253,334,335]. |
| One Welfare | One Welfare by integrating animal, environmental, and public health in antimicrobial stewardship policies. | Integrating this approach into AMR strategies enables sustainable, equitable solutions across all sectors [299,300,336]. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodriguez, J. One Health Ethics and the Ethics of Zoonoses: A Silent Call for Global Action. Vet. Sci. 2024, 11, 394. https://doi.org/10.3390/vetsci11090394
Rodriguez J. One Health Ethics and the Ethics of Zoonoses: A Silent Call for Global Action. Veterinary Sciences. 2024; 11(9):394. https://doi.org/10.3390/vetsci11090394
Chicago/Turabian StyleRodriguez, Jeyver. 2024. "One Health Ethics and the Ethics of Zoonoses: A Silent Call for Global Action" Veterinary Sciences 11, no. 9: 394. https://doi.org/10.3390/vetsci11090394
APA StyleRodriguez, J. (2024). One Health Ethics and the Ethics of Zoonoses: A Silent Call for Global Action. Veterinary Sciences, 11(9), 394. https://doi.org/10.3390/vetsci11090394






