1. Introduction
According to the World Health Organization (WHO), by 2030, one in six people globally will be aged 60 years or older. Between 2020 and 2050, the global population aged ≥ 60 years is expected to double to 2.1 billion, while those aged ≥80 years will triple to reach 426 million [
1]. Ageing remains the most significant risk factor for neurodegenerative diseases (ND), particularly Alzheimer’s disease (AD), which is characterised by progressive neuronal loss leading to cognitive and memory decline. Importantly, ageing is closely linked to the disruption of host–microbiota homeostasis, resulting in gut dysbiosis—an imbalance that contributes to systemic inflammation and the onset of age-associated disorders, including ND and AD. López-Otín et al. [
2] recently expanded their framework of the nine hallmarks of ageing to include intestinal dysbiosis, highlighting its emerging role as a key contributor to age-related physiological decline. This addition underscores the central importance of the gut–brain axis in ageing biology and neurodegenerative disease development.
The human gut harbours trillions of microorganisms, including bacteria, fungi, archaea, and viruses—collectively referred to as the gut microbiome. This diverse community encodes over three million genes, vastly exceeding the 23,000 genes within the human genome, and comprises approximately 2000 bacterial species [
3]. The gut also contains an intricate network of neurons embedded in the gastrointestinal wall, known as the enteric nervous system (ENS), which houses about 168 million neurons, a number comparable to the 222 million neurons found in the spinal cord [
4]. Due to this extensive neuronal network, the gut is deeply involved in maintaining central nervous system (CNS) health, influencing cognition, memory, mood, and social behaviour, as well as modulating the ENS, autonomic nervous system, and hypothalamic–pituitary–adrenal (HPA) axis [
5]. Consequently, the gut is often referred to as the “second brain”. Communication between the gut and the brain occurs bidirectionally through the gut–brain axis, which integrates neural (vagus nerve), endocrine, immune, and circulatory pathways, alongside lymphatic and glymphatic systems. These pathways enable the gut microbiome to modulate brain activity, while the brain, in turn, regulates intestinal motility, permeability, and secretory responses [
5].
Gut microbiome composition undergoes dynamic changes with ageing and has been closely associated with the onset of ageing-related diseases. These shifts are influenced by genetic background, lifestyle, diet, environmental exposure, and geographical location, contributing to wide inter-individual variation. In general, ageing is accompanied by a decline in beneficial commensal taxa such as
Bifidobacterium,
Faecalibacterium,
Prevotella,
Lachnospira,
Ruminococcus,
Eubacterium rectale, and
Coprococcus, which are gradually replaced by other commensals such as
Butyricimonas,
Akkermansia,
Christensenellaceae,
Odoribacter, and
Butyricicoccus, and opportunistic pathobionts such as
Streptococcus,
Eggerthella,
Enterobacteriaceae,
Bilophila, and
Fusobacteria [
6,
7]. For instance, Lee et al. [
8] reported a higher abundance of
Lactobacillus in younger individuals compared to the elderly, who displayed increased levels of
Escherichia,
Bacteroides, and
Clostridium. Similarly, Sepp et al. [
9] found a decline in butyrate-producing bacteria such as
Faecalibacterium prausnitzii and
Lachnospiraceae in centenarians, consistent with studies from Chinese, Korean, and Italian cohorts [
10,
11,
12]. The loss of butyrate-producing bacteria in ageing may exacerbate metabolic dysfunction, given butyrate’s role in appetite regulation, insulin sensitivity, and maintaining a healthy gut barrier.
Emerging evidence indicates that gut dysbiosis contributes to neurodegenerative processes through the production of microbial metabolites that promote amyloid-beta aggregation, tau hyperphosphorylation, and neuroinflammation. For instance, Honarpisheh et al. [
13] demonstrated that dysbiosis in AD mouse models enhances amyloid-beta accumulation, whereas Kim et al. [
14] reported that faecal microbiota transplantation from healthy mice reduced amyloid and tau pathology, improved cognition, and decreased systemic inflammation. Similarly, transplanting an aged microbiome into young germ-free mice induced inflammation, increased gut permeability, and decreased
Akkermansia abundance, exhibiting traits of inflamm-ageing [
15]. These findings underscore the role of the aged gut microbiome as a potential driver of systemic and neuroinflammatory ageing mechanisms. Understanding these microbial shifts and their interactions with the gut–brain axis may enable the development of microbiome-based interventions to mitigate neurodegeneration.
Among various strategies to restore microbial balance, probiotics have shown promising effects in counteracting gut dysbiosis and age-associated inflammation [
16,
17,
18]. Probiotics—defined as live microorganisms that confer health benefits when administered in adequate amounts—can help restore microbial composition, reduce chronic inflammation and brain oxidative stress, and improve memory and lifespan, as observed in model organisms [
19,
20]. For example, Hor et al. [
21] demonstrated that administration of
Lactobacillus paracasei OFS 0291 and
Lactobacillus helveticus OFS 1515 reduced opportunistic
Bacteroides species in D-galactose-induced rats, while
Lactobacillus fermentum DR9 supplementation increased
Lactobacillus abundance and acetate levels. These findings suggest that probiotics may beneficially reshape gut microbial composition and metabolite production in the ageing gut.
Building on this concept, the present preliminary study explored the potential modulatory effects of Malaysian kefir water (a traditionally fermented beverage rich in
Lactobacillus and
Bifidobacterium species) on gut microbiota composition in D-galactose-induced ageing BALB/c mice. The D-galactose (D-gal)-induced ageing model was used as it closely mimics natural ageing processes through chronic oxidative stress and the accumulation of advanced glycation end products, leading to inflammation and neurodegeneration, making it a well-established system for studying age-related physiological and microbial changes, including gut dysbiosis [
22].
Kefir water, composed primarily of lactic acid bacteria, has previously been shown to modulate gut microbiota and improve gut barrier function [
23,
24]. Our previous research demonstrated that kefir water possesses antioxidant and neuroprotective activities, attenuating oxidative stress in human SH-SY5Y neuronal cells [
25], while ultra-high-performance liquid chromatography analysis identified flavonoid and phenolic acid derivatives as key bioactive constituents [
26]. However, its in vivo effects on gut microbial modulation during ageing remain largely unexplored.
Therefore, this study aimed to explore the feasibility of using kefir water as a dietary intervention to modulate gut microbial composition in an ageing mouse model. Specifically, we evaluated kefir water as a pre-treatment and co-treatment to examine its potential influence on microbial diversity, composition, and Lactobacillus enrichment. The findings from this exploratory investigation provide preliminary insight into the possible gut microbiota-modulating capacity of Malaysian kefir water, laying the groundwork for more comprehensive future studies on its anti-ageing and neuroprotective potential.
2. Materials and Methods
2.1. Preparation of Kefir Water
Kefir water grains were purchased from a local store, Kefir and Kombucha, in Kuala Lumpur, Malaysia (
https://www.kefirandkombucha.com, accessed on 1 June 2021). The kefir water was prepared as described in our previous studies [
25,
26].
2.2. Experimental Animals and Ethics Statement
This study received ethical approval from Universiti Putra Malaysia’s Institutional Animal Care and Use Committee (UPM/IACUC/AUP-R014/2020) and was conducted in accordance with their guidelines. All procedures complied with OECD and ARRIVE guidelines. A total of 48 male BALB/c mice (7 weeks old, weighing 18–22 g) were obtained from the Animal House of the Faculty of Veterinary Medicine, Universiti Putra Malaysia.
2.3. Experimental Design
Mice were acclimatised for 7 days upon arrival. They were housed in plastic cages at 22 ± 1 °C, with a 12 h light/dark cycle and approximately 60% relative humidity. Mice were provided with a standard pellet diet and distilled water ad libitum throughout the experiment. The dietary composition of the standard pellet (AIN-93G) is provided in
Table S1.
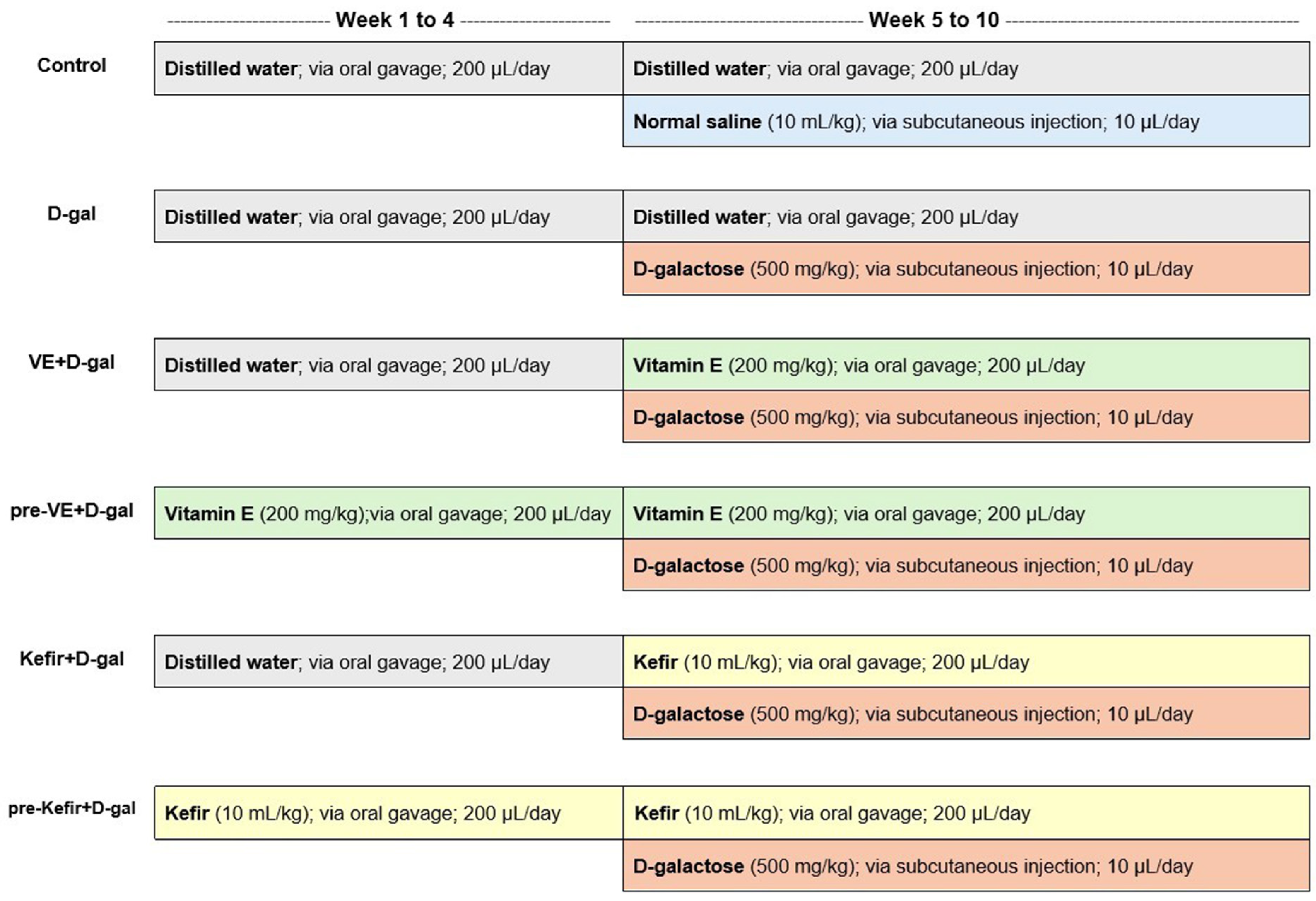
After one week of acclimatisation, mice were randomly assigned to six groups (
n = 8 per group) and treated daily for ten weeks as follows: (i) the control group served as the normal control, (Control,
n = 8), (ii) D-gal group served as the negative control (D-gal,
n = 8), (iii) the vitamin E + D-gal group served as the co-treatment positive control (VE+D-gal,
n = 8), (iv) the pre-treatment vitamin E + D-gal group served as the pre-treatment positive control (pre-VE + D-gal,
n = 8), (v) the kefir + D-gal group served as the co-treatment with kefir water (Kefir + D-gal,
n = 8), and (vi) the pre-treatment kefir + D-gal group served as the pre-treatment with kefir water (pre-Kefir+D-gal,
n = 8). The experimental design and treatment administration are summarised in
Figure 1. Treatments, including kefir water (10 mL/kg/day), VE (200 mg/kg/day), and distilled water, were administered via oral gavage at 200 µL, while D-gal was administered via subcutaneous injection at 10 µL of 500 mg/kg/day to the respective treatment groups.
The concentrations of D-gal and vitamin E, as well as the treatment duration, were selected based on previous studies [
27,
28]. According to the study timeline (
Figure 1), all mice except those in the control group were induced with D-gal at week 5 (when mice were 12 weeks old), an age considered suitable for D-gal induction [
27,
28,
29]. Changes in physical appearance, behaviour, and body weight were recorded weekly. At the end of the treatment period, faecal samples were collected into sterilised 1.5 mL tubes and stored at −80 °C for 16S rRNA metagenomic analysis. Mice were sacrificed via terminal exsanguination under general anaesthesia using ketamine-xylazine (100 mg/kg: 10 mg/kg), administered intraperitoneally.
2.4. Faecal DNA Extraction
Genomic DNA was extracted from mouse faeces using the QIAamp® Fast DNA Stool Mini Kit (Qiagen, Hilden, Germany) following the manufacturer’s protocol. Briefly, 220 mg of faeces was homogenised in 1 mL InhibitEX buffer using a D1000-E handheld homogeniser (Benchmark Scientific, Sayreville, NJ, USA) and incubated at 95 °C for 15 min to lyse microbial cells. The sample was centrifuged at 14,000× g for 10–15 min, and 200 µL of the supernatant was mixed with 15 µL Proteinase K and 200 µL Buffer AL, followed by incubation at 70 °C for 20 min. An equal volume of ethanol (96–100%) was then added, and the lysate was transferred to a QIAamp spin column for purification according to the manufacturer’s instructions. DNA yield and quality were assessed using a Qubit 2.0 Fluorometer (Life Technologies, Waltham, MA, USA) and an Agilent Bioanalyzer 2100 (Agilent Technologies, Santa Clara, CA, USA). Extracted DNA was stored at −20 °C until further use.
2.5. Amplicon Generation
Purified genomic DNA that passed quality control (QC) was used as a template for amplification with locus-specific primers as follows:
Forward primer: CCTACGGGNGGCWGCAG
Reverse primer: GACTACHVGGGTATCTAATCC
PCR reactions were performed using REDiant 2× PCR Master Mix (1st BASE, Singapore) following the manufacturer’s protocol. A 50 µL reaction contained REDiant 2× PCR Master Mix (1×), forward and reverse primers (1 µM each), 5 ng DNA template, and nuclease-free water. Reactions were briefly centrifuged and amplified in a thermal cycler with an initial denaturation at 95 °C for 5 min, followed by 25–35 cycles of 95 °C for 1 min, 65 °C for 1 min, and 72 °C for 1 min, with a final extension at 72 °C for 15 min.
2.6. Quantification and Qualification of PCR Products
The ~450 bp PCR products were electrophoresed on a 1% (w/v) Tris–acetate EDTA (TAE) agarose gel and visualised under UV light using the Bio-Rad Imager documentation system (Bio-Rad, Hercules, CA, USA).
2.7. Primary Phase of Library Construction (1st Stage PCR)
The 16S rRNA gene amplicons were prepared for sequencing on the Illumina MiSeq System (Illumina, San Diego, CA, USA) using the two-stage PCR protocol described in the Illumina 16S Metagenomic Library Preparation Guide. In the first PCR stage, the bacterial 16S rRNA gene targeting the V3–V4 regions was amplified using locus-specific primers with Illumina overhang adapters as follows:
Forward overhang:
27F 5′-TCGTCGGCAGCGTCAGATGTGTATAAGAGACAG-[CCTACGGGNGGCWGCAG]-3′
Reverse overhang:
1492R 5′-GTCTCGTGGGCTCGGAGATGTGTATAAGAGACAG-[GACTACHVGGGTATCTAATCC]-3′
PCR reactions were performed using KOD-Multi & Epi® (Toyobo, Osaka, Japan) according to the manufacturer’s protocol. Each 50 µL reaction contained 2× PCR buffer (1×), forward and reverse primers (0.3 µM each), ≤50 ng DNA template, 1 µL KOD-Multi & Epi®, and PCR-grade water. Reactions were briefly centrifuged and amplified in a thermal cycler with an initial denaturation at 94 °C for 2 min, followed by 30–40 cycles of 98 °C for 10 s, 65 °C for 10 s, and 68 °C for 30 s.
2.8. Secondary Phase of Library Construction (2nd Stage PCR)
Dual indices were attached to the amplicon PCR using the Illumina Nextera XT Index Kit v2 according to the manufacturer’s protocol (Agilent Technologies, Santa Clara, CA, USA). Briefly, 5 µL of PCR product was combined with Nextera XT Index Primers 1 (N7xx) and 2 (S5xx) (5 µL each), 2× KAPA HiFi HotStart ReadyMix (25 µL), and PCR-grade water (10 µL) in a 50 µL reaction. The mixture was gently mixed, covered with Microseal ‘A’, and briefly centrifuged. PCR amplification consisted of an initial denaturation at 95 °C for 3 min, followed by 8 cycles of 95 °C for 30 s, 55 °C for 30 s, and 72 °C for 30 s, with a final extension at 72 °C for 5 min. Library quality was assessed using the Agilent Bioanalyzer 2100 System with the Agilent DNA 1000 Kit, and fluorometric quantification was performed using Helixyte GreenTM (AAT Bioquest®, Inc., Pleasanton, CA, USA).
2.9. Next-Generation Sequencing
Libraries were normalised and pooled according to Illumina’s recommended protocol and sequenced on the MiSeq platform (Illumina, San Diego, CA, USA) using a 300-cycle paired-end (PE) run. The final concentrated library was diluted to 4 nM with resuspension buffer (RSB) or 10 mM Tris (pH 8.5), and 5 µL from each diluted library was pooled to create the final sequencing mix containing unique index combinations.
2.10. Metagenomics Data Analysis
Raw sequencing data from Illumina 16S rRNA metagenomics sequencing were processed using the QIIME2 v.2020.06 pipeline (
https://doi.org/10.1038/s41587-019-0209-9, accessed on 28 July 2022). Sequence adaptors and low-quality reads were trimmed using BBDuk from the BBTools package (
https://sourceforge.net/projects/bbmap/, accessed on 28 July 2022), and paired-end reads were merged with USEARCH v11.0.667 (
https://www.drive5.com/usearch/, accessed on 28 July 2022). After filtering out reads shorter than 150 bp or longer than 600 bp, error correction and chimera removal were performed using the DADA2 v1.18 pipeline (
https://benjjneb.github.io/dada2/, accessed on 28 July 2022). The resulting amplicon sequence variants (ASVs) were aligned against the SILVA 132 16S rRNA database using VSEARCH v2.6.2. Operational taxonomic units (OTUs) were clustered at 97% similarity with UPARSE v11.0.667, and low-abundance OTUs (fewer than two reads) were excluded from downstream analysis. Multiple sequence alignments were generated using MAFFT, and a phylogenetic tree for UniFrac analysis was constructed with FastTree2.
2.11. Statistical Analysis
Data analysis was performed using R Studio (version 3.6.2) with the phyloseq package (
https://www.bioconductor.org/packages/release/bioc/html/phyloseq.html, accessed on 28 July 2022) for metagenomic bioinformatics analysis. The Kruskal–Wallis test, a non-parametric method suitable for small sample sizes and non-normally distributed data, was performed to compare treatment groups. However, no significant differences were detected, which may be attributed to the limited number of biological replicates. Observed outcomes were therefore interpreted descriptively to identify potential trends in gut microbiota modulation. As this is a preliminary study, future investigations will include 5–10 biological replicates per group to ensure adequate statistical power and allow for more robust functional validation.
3. Results
3.1. Effects of Kefir Water on the Alpha Diversity of Gut Microbial Species
A total of 1,761,238 sequence reads were obtained from 12 faecal samples (2 per group). After trimming and quality filtering, 84.75% of reads were retained, resulting in 1,492,634 high-quality sequences, with an average of 56,725 per sample (
Table S2).
Alpha diversity, assessed through observed operational taxonomic units (OTUs), species richness (Abundance-based coverage estimator (ACE)), and diversity indices (Chao1, Shannon, Simpson), is summarised in
Table 1. Operational taxonomic units which represent clusters of microbial taxa based on sequence similarity, are commonly used to assess microbial richness and community composition. Abundance-based coverage estimator and Chao1 estimate species richness, accounting for both abundant and rare taxa, while Shannon and Simpson indices consider both richness and evenness to describe overall diversity.
Both kefir water-treated groups showed comparatively lower observed OTUs (Kefir + D-gal: 281.00 ± 22.00; pre-Kefir + D-gal: 308.50 ± 4.50) relative to the D-gal (338.50 ± 0.50), control (359.50 ± 5.50), VE co-treated (316.00 ± 33.00), and VE pre-treated (433.00 ± 2.00) groups (p = 0.097). Similarly, kefir-treated mice exhibited lower species richness (ACE: 281.10 ± 22.10 and 311.87 ± 5.68; p = 0.097) and diversity indices (Chao1: 281.00 ± 22.00 and 315.17 ± 8.83 (p = 0.096); Shannon: 4.73 ± 0.12 and 4.48 ± 0.07 (p = 0.095); Simpson: 57.19 ± 10.52 and 46.33 ± 4.09 (p = 0.122)) compared to other groups. In contrast, the pre-VE+D-gal group had the highest OTUs (433.00 ± 2.00, p = 0.097), species richness (ACE: 435.28 ± 2.66; p = 0.097), and diversity indices (Chao1: 435.11 ± 2.44 (p = 0.096); Shannon: 5.09 ± 0.08 (p = 0.095); Simpson: 82.45 ± 10.45 (p = 0.122)).
3.2. Effects of Kefir Water on UPGMA Tree Analysis
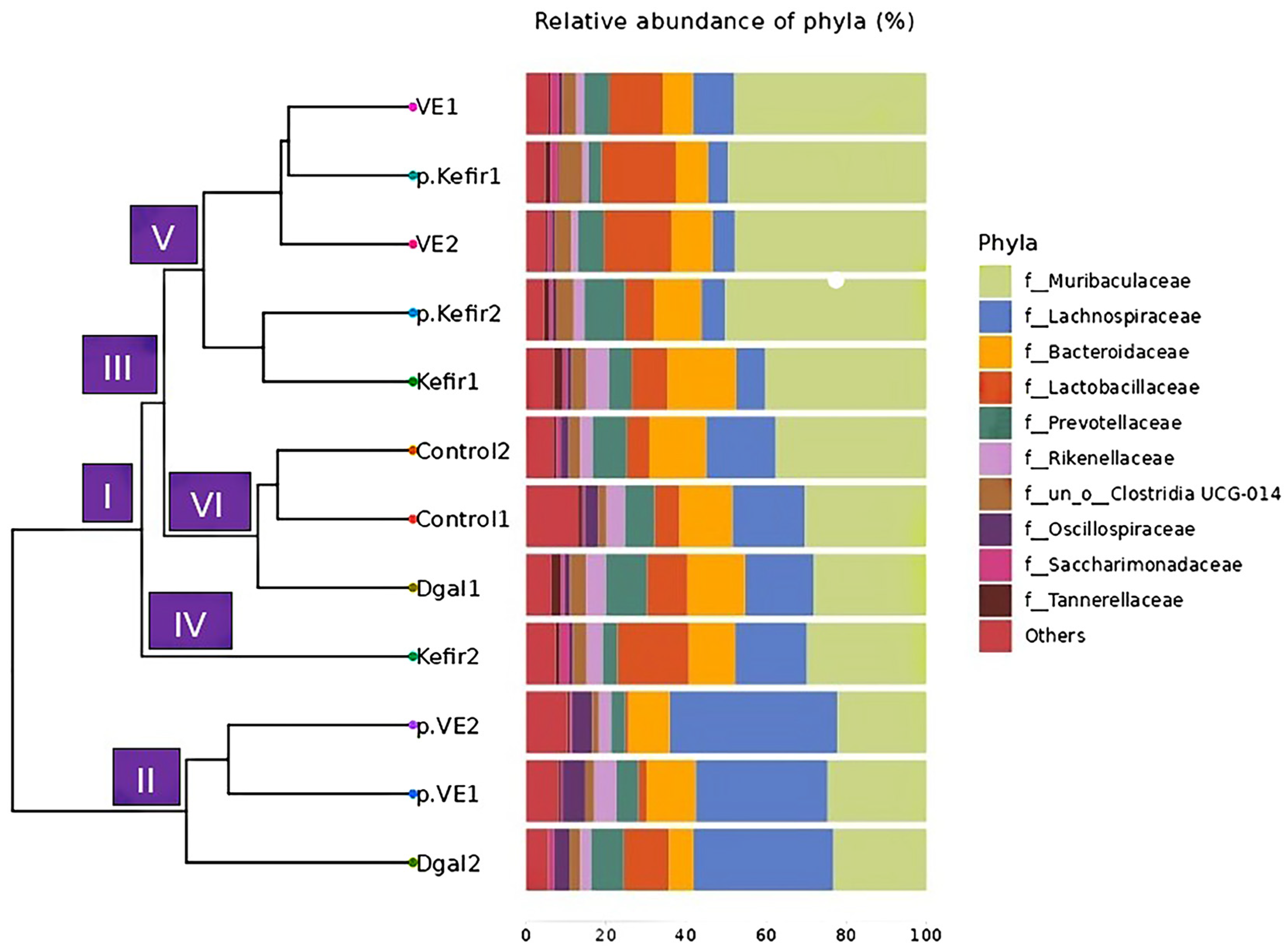
Beta diversity, assessed via hierarchical clustering using the unweighted pair group method with arithmetic mean (UPGMA) tree, was applied to evaluate compositional differences among treatment groups. The UPGMA analysis classified the microbial communities into two main clusters, designated as Groups I and II, both originating from a common ancestral root (
Figure 2). Group II primarily consisted of the pre-VE+D-gal treatment, whereas Group I encompassed the control, D-gal (sample 1), kefir-treated, and VE-co-treated groups.
Within Group I, additional branching was observed, forming two sub-clusters (III and IV), with sub-cluster III further dividing into branches V and VI. The phylogenetic distribution revealed that the control and D-gal (sample 1) (branch VI) clustered closely, while the kefir pre-treated, kefir co-treated, and VE-co-treated groups (branches V and IV) diverged into distinct yet related lineages. Interestingly, D-gal (sample 2) grouped with the pre-VE+D-gal treatment (Group II) rather than clustering with D-gal (sample 1), suggesting a degree of intra-group variability among the D-gal samples.
3.3. Beta-Diversity Analysis Based on KEGG Orthologues
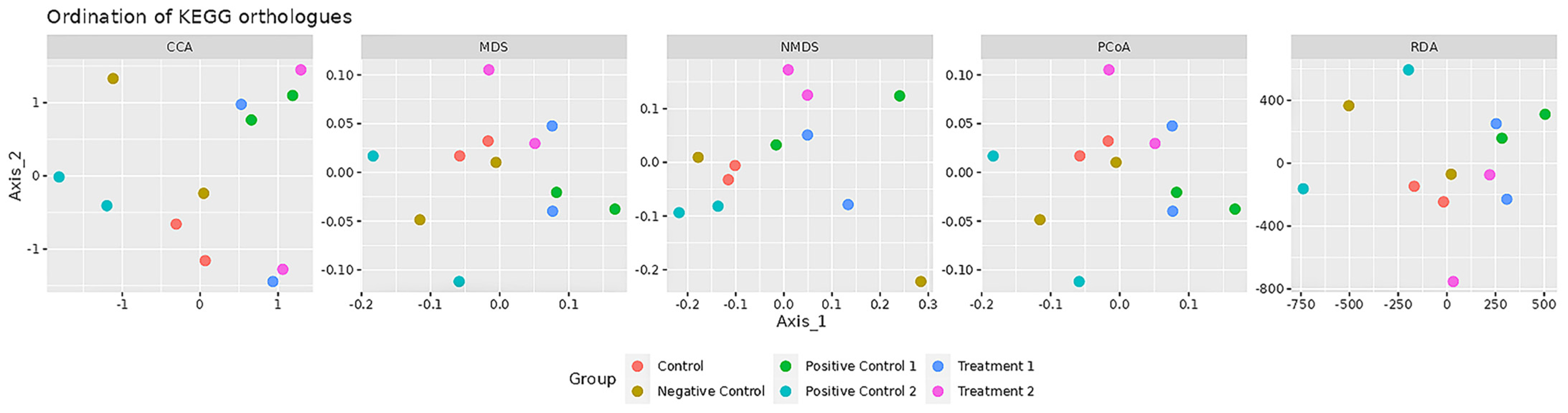
To examine functional differences in the gut microbiome across treatment groups, multiple ordination analyses were performed using KEGG orthologue profiles, including Canonical Correspondence Analysis (CCA), Redundancy Analysis (RDA), Multidimensional Scaling (MDS), Non-metric Multidimensional Scaling (NMDS), and Principal Coordinates Analysis (PCoA) (
Figure 3).
CCA and RDA, as constrained ordination methods, assess how well treatment groups explain variation in microbial functional profiles. In both analyses, kefir co-treated (Treatment 1, blue) and pre-treated (Treatment 2, purple) groups formed clusters distinct from the control (red), D-gal (Negative Control, mustard), and VE pre-treatment (Positive Control 2, cyan) groups. Notably, the kefir groups were positioned closer to the VE co-treatment group (Positive Control 1, green), indicating that kefir administration induced functional shifts in the gut microbiome that were more similar to VE co-treatment than to the untreated control.
MDS, NMDS, and PCoA, as unconstrained ordination methods, visualised overall sample similarity without prior group constraints. These plots show a comparable pattern: the control and D-gal groups clustered separately, while the kefir-treated groups consistently appeared near the VE co-treatment cluster. Partial overlap between kefir and VE co-treatment was observed, suggesting that kefir treatments shared functional features with VE co-treatment.
Overall, these ordinations indicate that kefir water pre-treatment and co-treatment modulate the gut microbiome in a manner more aligned with VE co-treatment than with the untreated control. This preliminary observation suggests that kefir and VE co-treatment may exert comparable modulatory effects on microbial functional profiles. However, further targeted analyses with larger sample sizes are required to identify the specific functional pathways involved.
3.4. Effects of Kefir Water on the Rank Abundance and Rarefaction Curves of Gut Microbiota
The rank abundance and rarefaction curves (
Figures S1 and S2) were used to provide an overview of microbial diversity and sequencing depth across the treatment groups. The rank abundance curves revealed that kefir pre-treatment exhibited the widest and smoothest profile, suggesting greater species richness and more even distribution of taxa. In contrast, the VE co-treatment group displayed a steep decline, indicative of a few dominant species and lower evenness, while the other groups showed intermediate diversity patterns.
Similarly, the rarefaction curves demonstrated variation in observed species richness among the groups. The VE pre-treatment group exhibited the highest richness, whereas kefir water pre- and co-treatment groups reached saturation at lower read depths, suggesting a moderate microbial diversity compared to controls. These findings, though preliminary, provide supportive evidence of treatment-dependent modulation in microbial richness and evenness.
3.5. Effects of Kefir Water on the Phylum-Level Bacterial Taxonomic Composition
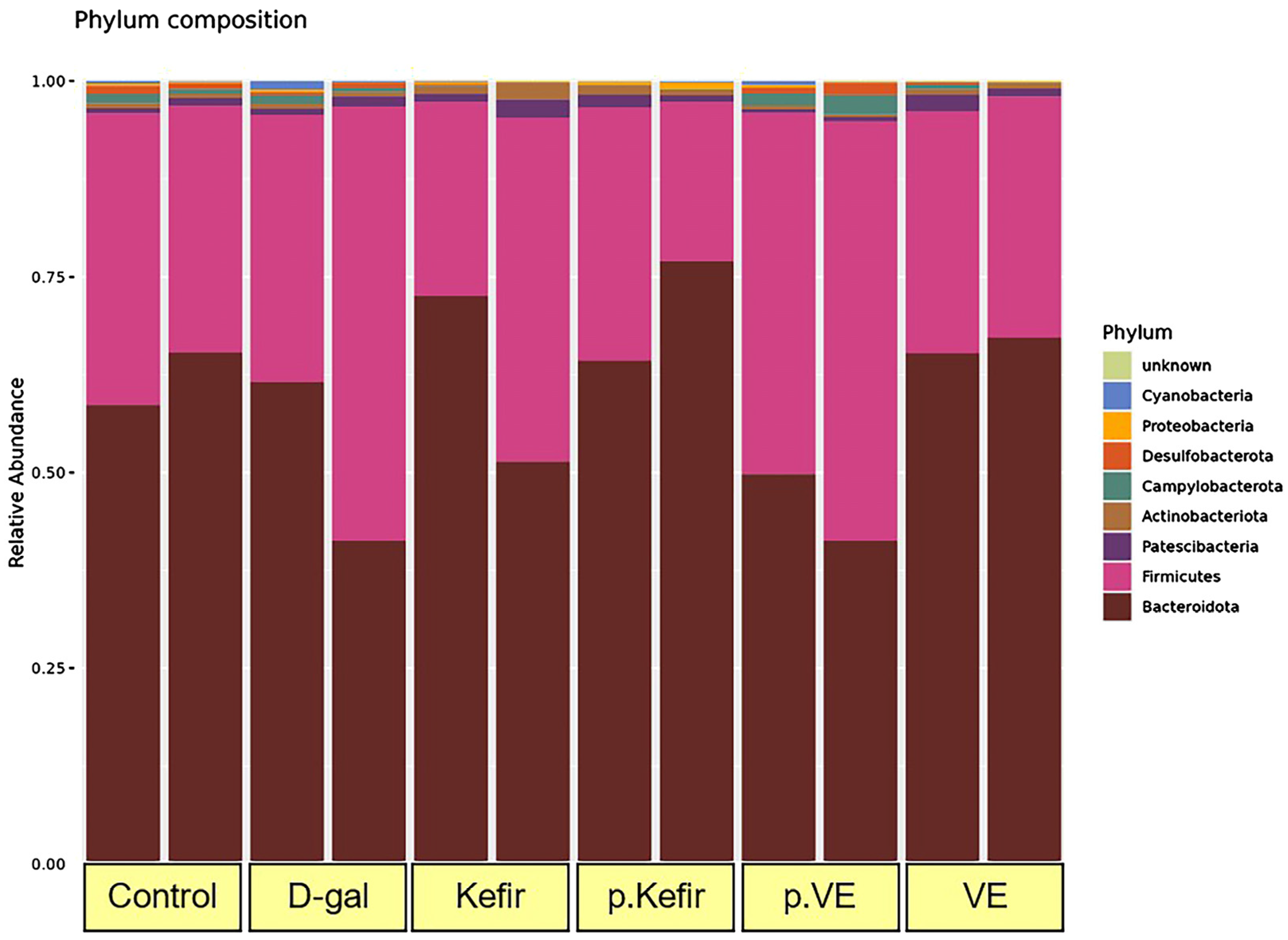
As shown in
Figure 4, eight bacterial phyla were identified in the gut microbiota of D-gal-induced mice across all treatment groups:
Bacteroidota,
Firmicutes,
Patescibacteria,
Actinobacteriota,
Campylobacterota,
Desulfobacterota,
Proteobacteria, and
Cyanobacteria. Among these,
Bacteroidota and
Firmicutes were the most predominant phyla, though their relative abundances did not differ significantly among groups (
Bacteroidota:
p = 0.251;
Firmicutes:
p = 0.238,
Table 2).
The relative abundance of Bacteroidota decreased in the D-gal-treated group (0.515 ± 0.101%) compared to the control group (0.620 ± 0.034%). Interestingly, kefir pre-treatment increased Bacteroidota abundance to 0.707 ± 0.064%, while kefir co-treatment maintained a level similar to that of the control (0.620 ± 0.034%). The VE pre-treated group showed the lowest Bacteroidota abundance (0.456 ± 0.043%), whereas the VE co-treated group demonstrated a relatively high abundance (0.663 ± 0.010%).
In contrast, Firmicutes abundance was elevated in the D-gal-treated group (0.448 ± 0.107%) compared to the control (0.344 ± 0.029%). The kefir pre-treated group showed the lowest Firmicutes abundance (0.263 ± 0.060%), while the kefir co-treated group (0.344 ± 0.029%) remained comparable to the control. The VE pre-treated group exhibited the highest Firmicutes abundance (0.499 ± 0.037%), whereas the VE co-treated group showed 0.309 ± 0.309%, which was not higher than that of the control or D-gal-treated groups.
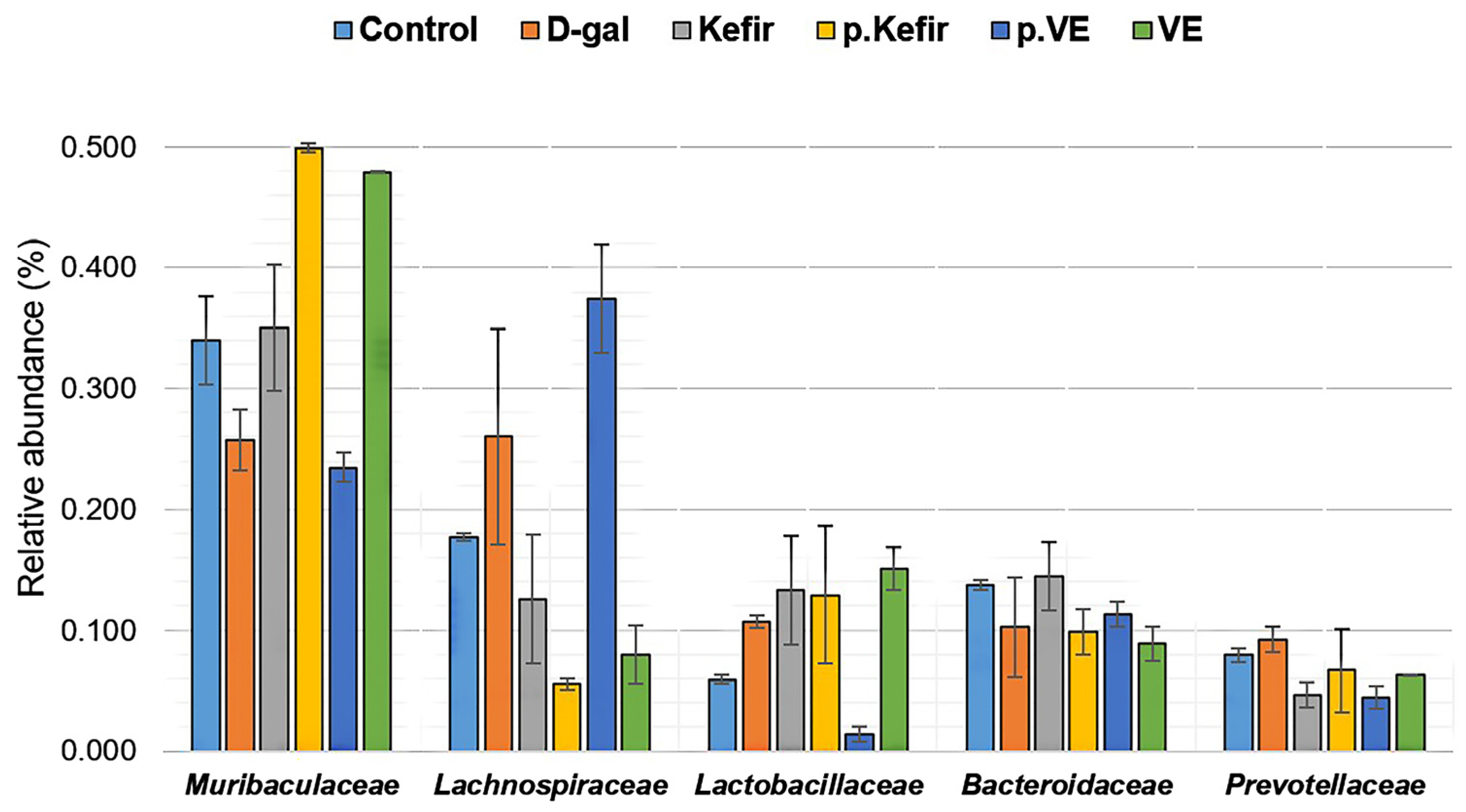
3.6. Effects of Kefir Water on Bacterial Taxonomic Composition at the Family Level
A total of 35 bacterial families were identified across all treatment groups (
Figure S3). The most notable gut microbial families observed in the kefir water-treated groups—
Muribaculaceae,
Lachnospiraceae,
Lactobacillaceae,
Bacteroidaceae, and
Prevotellaceae—are illustrated in
Figure 5.
Both kefir water pre-treatment and co-treatment appeared to non-significantly increase the relative abundance of Muribaculaceae (pre-Kefir+D-gal: 0.499 ± 0.004; Kefir+D-gal: 0.350 ± 0.052) and Lactobacillaceae (pre-Kefir+D-gal: 0.129 ± 0.057; Kefir+D-gal: 0.133 ± 0.045), compared to the D-gal-treated group (0.257 ± 0.025, p = 0.069 and 0.107 ± 0.005, p = 0.156, respectively). Similarly, kefir water co-treatment resulted in a slight, non-significant increase in Bacteroidaceae abundance (0.144 ± 0.028), whereas pre-treatment showed a non-significant decrease (0.099 ± 0.019) compared to the D-gal-treated group (0.103 ± 0.041, p = 0.465).
In contrast, the relative abundance of Lachnospiraceae and Prevotellaceae was non-significantly reduced in both kefir-treated groups (pre-Kefir+D-gal: 0.055 ± 0.004; 0.067 ± 0.034; Kefir+D-gal: 0.126 ± 0.053; 0.047 ± 0.010) compared to the D-gal-treated group (Lachnospiraceae: 0.260 ± 0.090, p = 0.125; Prevotellaceae: 0.092 ± 0.011, p = 0.277).
Among the VE-treated groups, an increased abundance of Muribaculaceae was observed (0.479 ± 0.001, p = 0.069) for the co-treatment group, whereas pre-treatment showed a reduced abundance of Muribaculaceae (0.235 ± 0.012, p = 0.069) and an increasing abundance of Lachnospiraceae (0.374 ± 0.045, p = 0.125), relative to the D-gal-treated group (Muribaculaceae: 0.257 ± 0.025; Lachnospiraceae: 0.260 ± 0.090).
VE pre-treatment also resulted in a lower Lactobacillaceae abundance (0.014 ± 0.006, p = 0.156), while VE co-treatment showed a higher abundance (0.151 ± 0.018, p = 0.156) than the D-gal-treated group (0.107 ± 0.005).
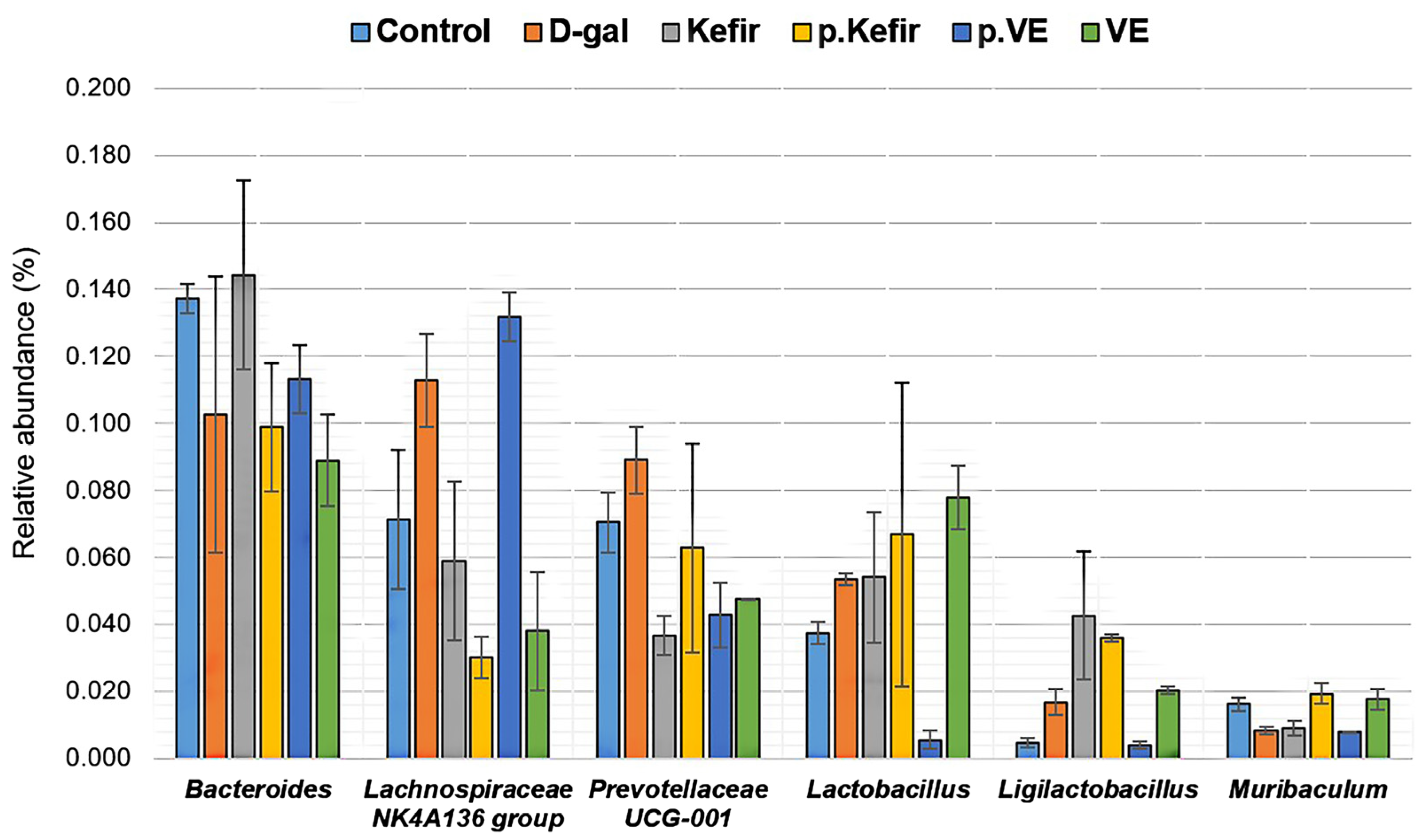
3.7. Effects of Kefir Water on Bacterial Taxonomic Composition at the Genus Level
A total of 71 bacterial genera were identified across all treatment groups, with a relatively high abundance of an unclassified genus observed (
Figure S4). At the genus level, notable variations were detected in
Bacteroides,
Lachnospiraceae NK4A136 group,
Prevotellaceae UCG-001,
Lactobacillus,
Ligilactobacillus, and
Muribaculum (
Figure 6). However, these changes were not statistically significant (
p > 0.05).
Kefir water pre-treatment showed a slightly lower relative abundance of Bacteroides (0.099 ± 0.019, p = 0.465) but an increasing abundance of Lactobacillus (0.067 ± 0.045, p = 0.257), Ligilactobacillus (0.036 ± 0.001, p = 0.075), and Muribaculum (0.019 ± 0.003, p = 0.125), compared to the D-gal-treated group (Bacteroides: 0.103 ± 0.041; Lactobacillus: 0.054 ± 0.002; Ligilactobacillus: 0.017 ± 0.004; Muribaculum: 0.008 ± 0.001). Kefir co-treatment similarly showed an increased abundance of Bacteroides (0.144 ± 0.028, p = 0.465), Ligilactobacillus (0.042 ± 0.019, p = 0.075), and Muribaculum (0.009 ± 0.002, p = 0.125), while maintaining comparable Lactobacillus abundance (0.054 ± 0.020, p = 0.257) relative to the D-gal-treated group.
Both kefir water treatments, however, showed a trend toward reduced abundance of Lachnospiraceae NK4A136 group (Kefir+D-gal: 0.059 ± 0.023; pre-Kefir+D-gal: 0.030 ± 0.006) and Prevotellaceae UCG-001 (Kefir+D-gal: 0.037 ± 0.006; pre-Kefir+D-gal: 0.063 ± 0.031) compared to the D-gal-treated group (Lachnospiraceae NK4A136: 0.113 ± 0.014, p = 0.125; Prevotellaceae UCG-001: 0.089 ± 0.010, p = 0.271).
Among the VE-treated groups, pre-treatment demonstrated an increased Lachnospiraceae NK4A136 group (0.132 ± 0.007, p = 0.125) but reduced Ligilactobacillus (0.004 ± 0.001, p = 0.075) and Lactobacillus (0.006 ± 0.003, p = 0.257) compared to the D-gal-treated group. In contrast, VE co-treatment showed slightly increased Ligilactobacillus (0.020 ± 0.001, p = 0.075) and Lactobacillus (0.078 ± 0.009, p = 0.257), while showing a reduced abundance of Prevotellaceae UCG-001 (0.047 ± 0.000, p = 0.271). The abundance of Muribaculum remained comparable to kefir-treated groups, with an observable increase in the VE co-treatment group (0.018 ± 0.003, p = 0.125) and unchanged levels in the VE pre-treatment group (0.008 ± 0.001, p = 0.125).
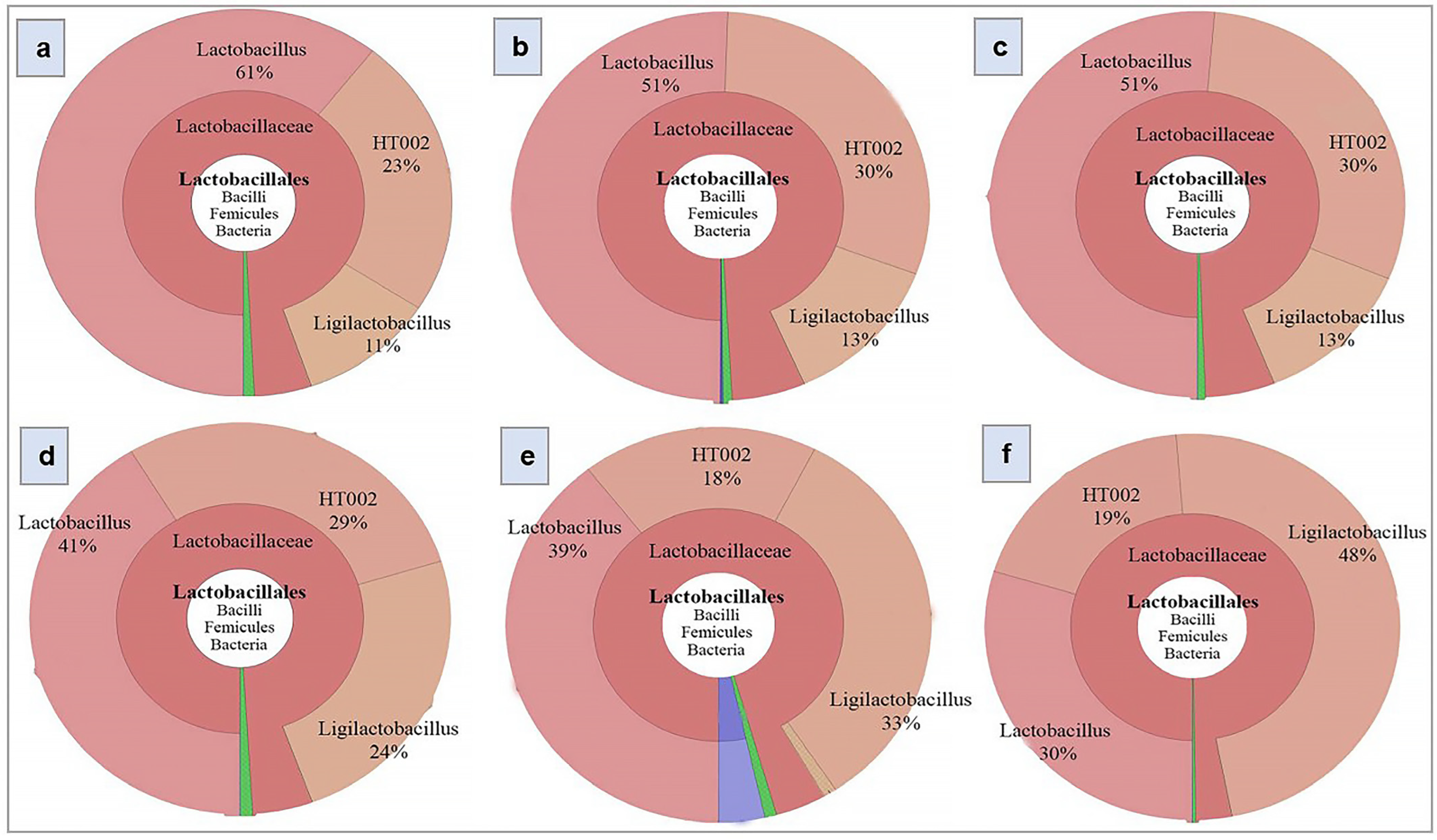
3.8. Effect of Kefir Water on the Abundance of Lactobacillus, Ligilactobacillus, and HT002
A Krona chart was used to visualise the relative abundance of bacterial taxa across multiple phylogenetic levels within each sample (
Figure 7). Notably, the distribution of
Lactobacillus and
Ligilactobacillus varied among treatment groups. As shown in
Table 3, the control group was dominated by
Lactobacillus (63%), followed by
Ligilactobacillus (8%). In D-gal-treated mice, the relative abundance of
Lactobacillus decreased to 50% (
p = 0.202), accompanied by a moderate increase in
Ligilactobacillus (15.5%,
p = 0.098). A comparable trend was observed in the VE co-treatment group, with
Lactobacillus and
Ligilactobacillus comprising 51% (
p = 0.202) and 13.5% (
p = 0.098) of the microbiota, respectively.
In contrast, VE pre-treatment led to a reduction in Lactobacillus abundance (38%, p = 0.202) and a corresponding increase in Ligilactobacillus (30%, p = 0.098) relative to the D-gal group. Kefir water treatments induced more pronounced and balanced shifts in these genera, particularly favouring Ligilactobacillus. In the kefir co-treatment group, Lactobacillus decreased to 38.5% (p = 0.202), while Ligilactobacillus increased to 29.5% (p = 0.098). Similarly, kefir pre-treatment showed in 45% Lactobacillus (p = 0.202) and 34% Ligilactobacillus (p = 0.098).
Additionally, a taxon identified as HT002, a bacterium within the
Lactobacillus genus of the
Lactobacillaceae family, was consistently detected across all treatment groups (
Figure 6,
Table 3). Its relative abundance was 24% in the control group, increasing to 28.5% in both the D-gal-treated and VE pre-treated groups (
p = 0.149). A slight increase was observed in the VE co-treatment group (29.5%,
p = 0.149), whereas kefir water co- and pre-treatments showed lower levels (23% and 17.5%,
p = 0.149, respectively).
4. Discussion
The 16S rRNA metagenomic analysis of alpha and beta diversity revealed that kefir water pre-treatment and co-treatment did not produce statistically significant changes in gut microbial species richness or diversity under the conditions tested. Nevertheless, several notable trends were observed. The D-gal-treated group showed a reduction in alpha diversity compared to the control group, consistent with previous findings linking ageing and oxidative stress to decreased microbial richness [
21,
22]. Interestingly, both kefir water-treated groups demonstrated a further decline in alpha diversity, a pattern also observed in the vitamin E co-treated group. Although this reduction could suggest a lower microbial diversity, the rarefaction and rank abundance curves provide additional insight. The kefir-treated groups showed lower rarefaction profiles but higher rank abundance dominance, indicating that kefir water may promote the selective modulation of specific microbial taxa while maintaining a lower overall diversity. In particular, the combination of lower alpha diversity and a high rank-abundance curve suggests a selective enrichment pattern, where a few dominant species are favoured over broader community diversity. This pattern may reflect an early stage of microbial adaptation, where selective taxa expand in abundance before a broader diversification occurs. In contrast, the vitamin E pre-treated group displayed higher OTUs, ACE, and alpha diversity indices than the other groups, suggesting that early antioxidant intervention may help stabilise microbial richness under ageing-associated stress. Collectively, these observations suggest that kefir water may influence gut microbial ecology through targeted compositional shifts rather than broad diversity enhancement, reflecting an adaptive modulation within the ageing gut microenvironment.
These findings are consistent with previous reports showing that kefir modulates gut microbiota composition more than overall diversity. For instance, Desnilasari et al. [
30] observed that kefir and kefir–glucomannan supplementation in rats with metabolic syndrome did not significantly change microbial diversity but selectively enriched
Lactobacillus (14.61%) and
Bifidobacterium (2.2%) while reducing
Clostridium (38.15%) and
Bacteroides (22.51%). Similarly, Bellikci-Koyu et al. [
23] reported enrichment of
Actinobacteria following kefir consumption without significant alterations in other dominant phyla such as
Bacteroidetes,
Proteobacteria, and
Verrucomicrobia.
Consistent with these studies, Bourrie et al. [
31] also found that kefir supplementation in high-fat diet-fed mice did not significantly alter microbial community structure or increase alpha diversity, while Wastyk et al. [
32] reported no increase in alpha diversity following fermented food consumption in humans. Gupta et al. [
24] similarly observed no increase in alpha diversity among critically ill patients, although gut microbiome wellness indices improved. Together, these findings suggest that kefir’s beneficial effects may not stem from enhancing overall microbial diversity but from the selective enrichment of specific beneficial taxa and their metabolites. Descriptively, this study suggests that kefir water promotes adaptive microbial shifts that could precede a broader ecological rebalancing, warranting further investigation with larger cohorts and extended treatment durations.
The dominant bacterial taxa at the phylum, family, and genus levels across the treatment groups are shown in
Figure 4,
Figure 5 and
Figure 6. At the phylum level,
Bacteroidota and
Firmicutes were the most abundant. In the D-gal-treated group, there was an increase in
Firmicutes and a decrease in
Bacteroidota which led to an elevated
Firmicutes/
Bacteroidota ratio, a pattern often associated with gut dysbiosis [
33,
34]. This observation aligns with previous reports where D-gal administration in mice was linked to an increased
Firmicutes/
Bacteroidota ratio, indicative of gut dysbiosis [
33,
34]. Notably, kefir water co-treatment appeared to reverse this trend, restoring the
Firmicutes/
Bacteroidota ratio to levels similar to the control group, suggesting a potential rebalancing of the gut microbial profile. Kefir pre-treatment for 28 days further reduced the
Firmicutes/
Bacteroidota ratio due to increased
Bacteroidota and decreased
Firmicutes abundance. This observation is consistent with findings by Peluzio et al. [
35], who reported that kefir administration reduced
Firmicutes and
Proteobacteria while increasing
Bacteroidetes,
Lactobacillus, and
Lactococcus. Similar effects were also noted by Kim et al. [
36] and Bellikci-Koyu et al. [
23], where kefir supplementation modulated the gut microbiota, enhancing
Bacteroidota abundance and reducing
Firmicutes. These trends suggest that kefir supplementation may promote a favourable shift in the gut microbial composition, increasing
Bacteroidota while reducing
Firmicutes, potentially due to the probiotic content and the fermentation-derived metabolites present in kefir, which could create a gut environment supportive of certain beneficial bacterial taxa, particularly those classified under
Bacteroidota [
23,
35,
36].
The dominant bacterial families observed in this preliminary study were
Bacteroidaceae,
Muribaculaceae, and
Prevotellaceae within the phylum
Bacteroidota, and
Lachnospiraceae and
Lactobacillaceae within
Firmicutes (
Figure 4). The predominant genera included
Bacteroides,
Lachnospiraceae NK4A136 group,
Prevotellaceae UCG-001,
Lactobacillus,
Ligilactobacillus, and
Muribaculum. D-galactose treatment reduced the abundance of
Muribaculaceae (and its genus
Muribaculum) and
Bacteroidaceae (and its genus
Bacteroides), while increasing
Lachnospiraceae (and its genus
Lachnospiraceae NK4A136 group) and
Prevotellaceae (and its genus
Prevotellaceae UCG-001). These compositional changes align with previous studies reporting similar bacterial shifts associated with ageing and gut dysbiosis [
37,
38].
Conversely, both kefir water pre-treatment and co-treatment appeared to modulate the gut microbiota in an opposing manner to D-gal treatment. Kefir administration increased the abundance of Muribaculaceae (Muribaculum) and Lactobacillaceae (and its genera Lactobacillus and Ligilactobacillus), while reducing Lachnospiraceae (Lachnospiraceae NK4A136 group) and Prevotellaceae (Prevotellaceae UCG-001). These compositional trends suggest that kefir water may alleviate ageing-associated dysbiosis by selectively enriching potentially beneficial bacterial taxa, even though the changes were not statistically significant.
Interestingly, the D-gal-treated group also showed a higher relative abundance of
Lactobacillaceae and
Lactobacillus compared to the control group. A plausible explanation is that certain
Lactobacillus species are capable of surviving and transiently proliferating under stressful conditions, such as oxidative stress, potentially as an adaptive or compensatory mechanism to maintain gut homeostasis. Previous studies have reported similar transient proliferation of
Lactobacillus strains under stress or inflammatory conditions [
39,
40]. However, this selective increase does not necessarily reflect a healthier microbial state, as it occurs alongside other dysbiotic features, such as the increased
Firmicutes/
Bacteroidota ratio observed in the D-gal group. These findings represent preliminary observations and warrant further validation with larger sample sizes and functional analyses to confirm the modulatory effects of kefir water on gut microbiota during ageing.
Muribaculaceae has recently attracted attention as a promising next-generation probiotic due to its role in host health. It primarily produces short-chain fatty acids (SCFAs), especially propionate and interacts with other probiotics such as
Bifidobacterium and
Lactobacillus to support SCFA production [
41,
42]. Propionate is associated with enhanced gut barrier function, immune modulation, and lifespan extension in mice [
42]. Similar observations were reported by Albuquerque et al. [
43], where kefir administration increased
Muribaculaceae abundance in Salmonella Typhimurium-infected C57BL/6 mice.
Kefir is naturally rich in
Lactobacillaceae, and several studies have reported that its consumption can increase the abundance of
Lactobacillus and
Ligilactobacillus in the host gut, as observed in the present study [
24,
30,
32,
36]. This is thought to be due to kefir’s polysaccharide matrix, which harbours a microbiota dominated by
Lactobacillus species. The formation of kefir grains begins with the self-aggregation of
Lactobacillus kefiranofaciens and
Saccharomyces spp., forming small granules. Subsequently,
Lentilactobacillus kefiri, a known biofilm producer, adheres to the surface of these granules and co-aggregates with other microorganisms and milk- or water-derived components to form mature kefir grains [
44]. As a result, the fermented kefir solution, whether derived from milk or water, typically contains a microbiota enriched in
Lactobacillus species, consistent with our previous findings where 16S rRNA sequencing of kefir water revealed
Lactobacillus hilgardii,
Lactobacillus harbinensis,
Lactobacillus satsumensis, and
Lactobacillus zeae as the most abundant species [
26]. These species were also associated with higher levels of flavonoids and phenolic acids, as key bioactive compounds contributing to the antioxidant and neuroprotective effects of kefir water [
25].
Kefir-derived
Lactobacillus has additional functional roles. Van et al. [
45] reported that kefir increased the gut microbial capacity to produce γ-aminobutyric acid (GABA) via enrichment of
Lactobacillus reuteri, which was linked to improving memory and reducing repetitive behaviours in mice.
Lactobacillus species, as dominant lactic acid bacteria in the human diet, contribute to SCFA production (acetate, propionate, butyrate), which exerts anti-inflammatory effects by modulating NF-κB signalling, inactivating regulatory T-cells, and reducing pro-inflammatory cytokine production [
46]. They also strengthen the intestinal barrier, preserving immune tolerance and mitigating gut-related disorders such as irritable bowel syndrome, gastrointestinal infections, and inflammatory bowel disease. Moreover,
Lactobacillus converts glutamate into GABA, a CNS neurotransmitter that inhibits neuronal excitability and may alleviate pain [
47]. Zhang et al. [
48] further demonstrated that fermented
Lactobacillus kefiri supernatant modulated autophagy, oxidative stress, and ageing-related gene expression in hydrogen peroxide-damaged human skin fibroblasts, delaying cellular ageing and senescence.
The Krona results showed that both kefir water co-treatment and pre-treatment appeared to enrich the intestines of D-gal-induced mice with Ligilactobacillus compared to the D-gal-treated and control groups. A noticeable shift was observed in the relative abundance from Lactobacillus to Ligilactobacillus. While the D-gal-treated and control groups showed relative abundances of 15.5% and 8%, respectively, the kefir co-treatment and pre-treatment groups exhibited higher abundances of 29.5% and 34%, suggesting that either early or concurrent kefir administration may promote more stable colonisation of Ligilactobacillus in the gut. Although these changes were not statistically significant, the trends suggest that kefir water may favour the enrichment of Ligilactobacillus over Lactobacillus under ageing-associated conditions. This pattern could indicate a selective modulatory effect, where kefir water supports the growth of specific beneficial taxa linked to gut microbial resilience. As a preliminary observation, this finding warrants further investigation to validate the role of Ligilactobacillus enrichment and its potential gut microbiome-modulatory and neuroprotective relevance in ageing models.
Ligilactobacillus is a genus of lactic acid bacteria that has recently gained attention as a potential probiotic candidate [
48]. Before March 2020, approximately 260 species were classified under the genus
Lactobacillus. However, following a major taxonomic reclassification of the families
Lactobacillaceae and
Leuconostocaceae, the genus was divided into 25 new genera, resulting in the reclassification of
Lactobacillus salivarius as
Ligilactobacillus salivarius [
49].
Ligilactobacillus salivarius is a Gram-positive, anaerobic rod commonly found in the intestines of mammals and birds [
50]. Several in vitro and in vivo studies have demonstrated its potential anti-inflammatory properties, including the upregulation of anti-inflammatory cytokines such as IL-10 and downregulation of pro-inflammatory cytokines such as TNF-α, IL-6, and IL-1β [
51,
52]. Similarly, studies by Lv et al. [
53] and Shi et al. [
54] reported that
Ligilactobacillus salivarius Li01, isolated from healthy human faeces, helped protect intestinal barrier integrity, reduce bacterial translocation and serum cytokine levels, and enhance gut microbial diversity. While the present findings tentatively suggest a similar enrichment pattern, further investigations are required to determine whether the increased
Ligilactobacillus abundance observed here translates into measurable functional or anti-inflammatory outcomes.
The decrease in
Lachnospiraceae and
Prevotellaceae observed in both kefir-treated groups compared to the D-gal-treated group was not statistically significant but may indicate a potential trend towards reduced abundance. Nevertheless, this preliminary observation is in line with the findings of Van et al. [
45], who reported that administration of kefir strains Fr1 and UK4 in mice led to a reduced prevalence of
Lachnospiraceae. Members of the
Lachnospiraceae family are part of the core gut microbiota and are among the main producers of SCFAs, particularly butyrate, an essential energy source for colonic epithelial cells. Butyrate contributes to shaping the gut microbial environment, strengthening the gut barrier, modulating host immunity, and potentially influencing brain function and behaviour via the gut–brain axis [
55].
Although
Lachnospiraceae are often considered beneficial for maintaining host gut and brain health, their effects appear to be complex and context-dependent. Different taxa within this family have been associated with both protective and pathogenic roles in various intraintestinal and extraintestinal disorders [
55]. Some studies have linked reduced
Lachnospiraceae abundance to neurodegenerative conditions, whereas others have reported certain
Lachnospiraceae species promoting neuroinflammation and neurodegeneration through metabolite production. For instance, Nguyen et al. [
56] reported increased
Lachnospiraceae levels in patients with schizophrenia, while Zhang et al. [
57] observed a decrease in the same family in a similar patient group. These inconsistencies underscore the need for further studies to clarify the context-specific functions of
Lachnospiraceae and their relevance to gut–brain health.
Prevotella, a Gram-negative bacterium, exhibits both beneficial and detrimental effects in humans, depending on the strain. Beneficially, certain strains improve cardiovascular health and enhance glucose metabolism. However, others display pathobiontic properties, contributing to obesity, metabolic syndrome, inflammatory bowel disease, and various inflammatory conditions such as asthma, bacterial vaginitis, rheumatoid arthritis, and HIV infection. A higher abundance of
Prevotella has also been associated with Alzheimer’s disease [
58], Parkinson’s disease [
59], and other inflammatory disorders [
60], suggesting its potential role in promoting intestinal dysbiosis and inflammation. Iljazovic et al. [
61] demonstrated that
Prevotella disrupts the gut microbiome and decreases SCFA levels in gnotobiotic mice and experimental colitis models, thereby exacerbating intestinal inflammation. Likewise, Macia et al. [
62] reported that colonisation with
Prevotella reduced SCFA production in mice, which was associated with decreased colonic IL-18 levels, a cytokine crucial for maintaining intestinal homeostasis and defence against infection. Kim et al. [
63] further showed that D-gal administration in 2,4-dinitrochlorobenzene-induced atopic dermatitis in BALB/c mice increased the relative abundance of
Prevotella and
Ruminococcus, while decreasing
Bacteroides at the genus level. In addition, HS [
58] reported that
Prevotella interacts with dendritic cells and may contribute to Alzheimer’s disease development.
Prevotella-associated gut microbiota changes can enhance the production of pro-inflammatory cytokines, leading to an inflammatory environment characterised by elevated TNF-α and IL-1 levels [
58]. This heightened inflammation may drive neuroinflammation in the CNS, ultimately resulting in neuronal damage.
This preliminary study acknowledges several limitations that warrant careful consideration. The small sample size may have constrained statistical power, reducing the ability to detect subtle microbial shifts with confidence and increasing the likelihood that observed differences represent biological trends rather than definitive effects. Additionally, the absence of functional analyses such as PICRUSt2 prediction, LEfSe profiling, and SCFA quantification limits the interpretation of how specific microbial alterations translate into host physiological outcomes. Therefore, while the microbial patterns identified here provide valuable exploratory insights into kefir water’s modulatory potential, they should be interpreted with caution. Future investigations incorporating larger sample sizes and integrative metagenomic and metabolomic approaches will be essential to validate these preliminary findings and clarify the underlying functional mechanisms.
To further substantiate the biological relevance of these microbial trends and confirm the successful establishment of the ageing model, our related study (submitted as a separate manuscript) demonstrated that D-gal administration induced marked ageing-related physiological alterations, including elevated liver and kidney biochemical parameters (serum AST, ALT, urea, triglycerides, and LDL), increased serum pro-inflammatory cytokines (TNF-α, IL-2, IL-6, IL-β, and IFN-γ), and evident histopathological damage in the liver, spleen, frontal cortex, and hippocampus. These changes collectively validate the establishment of the D-gal-induced ageing model. Notably, both kefir water treatments markedly ameliorated these alterations, restoring biochemical, histopathological alterations, and inflammatory markers toward control levels. Transcriptomic and qPCR analyses further demonstrated regulation of key neuroinflammatory pathways, including chemokine, PI3K–AKT–mTOR, and MAPK signalling cascades in both kefir-treated groups, collectively supporting its systemic anti-inflammatory and neuroprotective potential. Neither D-gal nor kefir-treated groups significantly affected body weight or organ indices. Consistent with these findings, the current microbiome analysis showed that both kefir pre-treatment and co-treatment groups exhibited similar enrichment within the family Lactobacillaceae, particularly the genus Ligilactobacillus. This pattern suggests that either early or concurrent kefir administration may facilitate more stable colonisation of beneficial bacteria in the gut. Such microbial modulation could underlie the observed neuroprotective and anti-inflammatory effects of kefir water through gut–brain axis communication. Collectively, these findings highlight the importance of future investigations integrating functional, metagenomic, and metabolomic analyses to elucidate the mechanistic links between kefir-induced gut microbiota modulation and gut–brain axis-mediated neuroprotection.