Assessing Healthcare Professionals’ Identification of Paediatric Dermatological Conditions in Darker Skin Tones
Abstract
1. Introduction
2. Methods
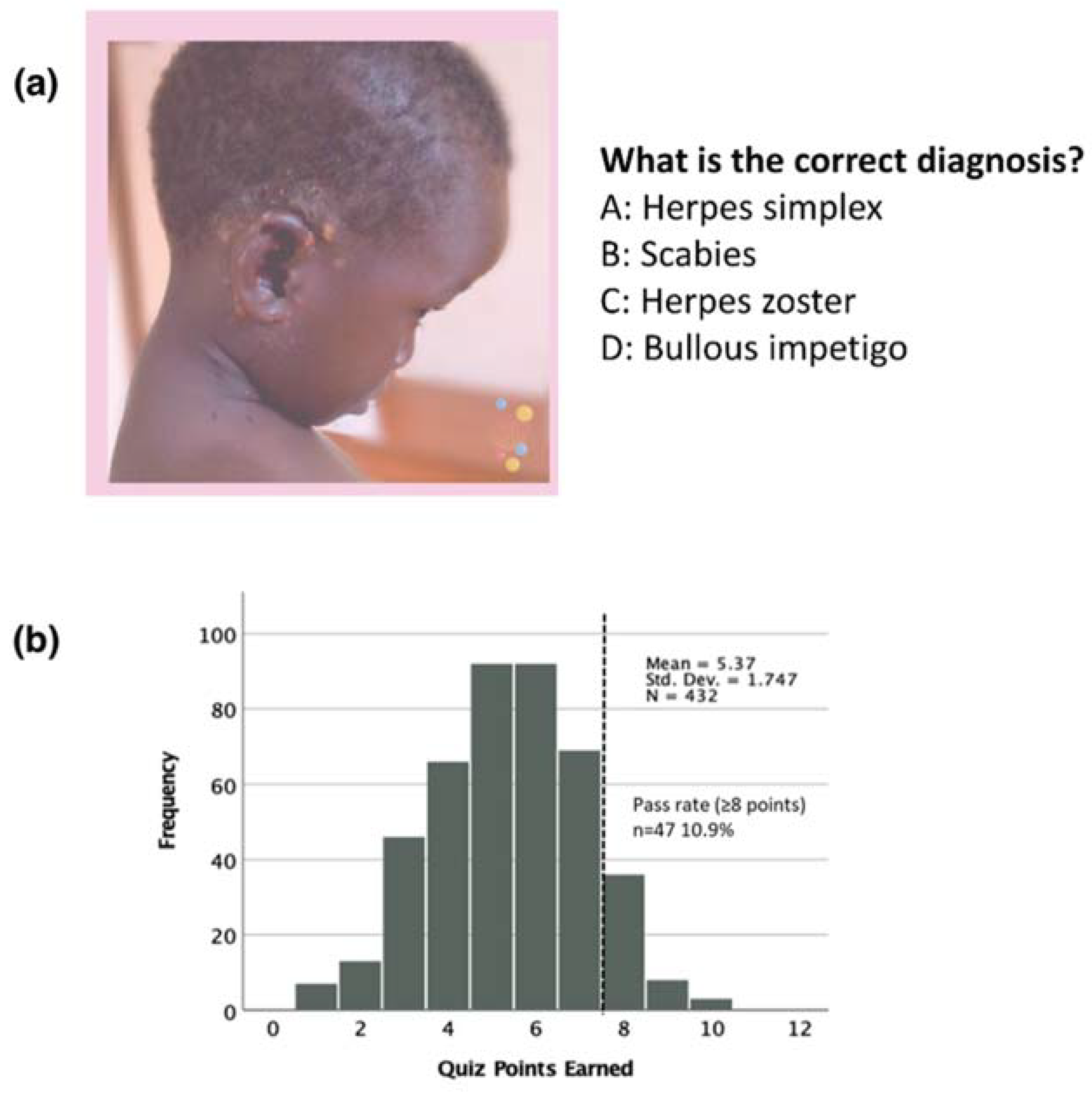
2.1. Quiz and Scoring
2.2. Statistical Analysis
3. Results
3.1. Quiz Participants
3.2. Quiz Results
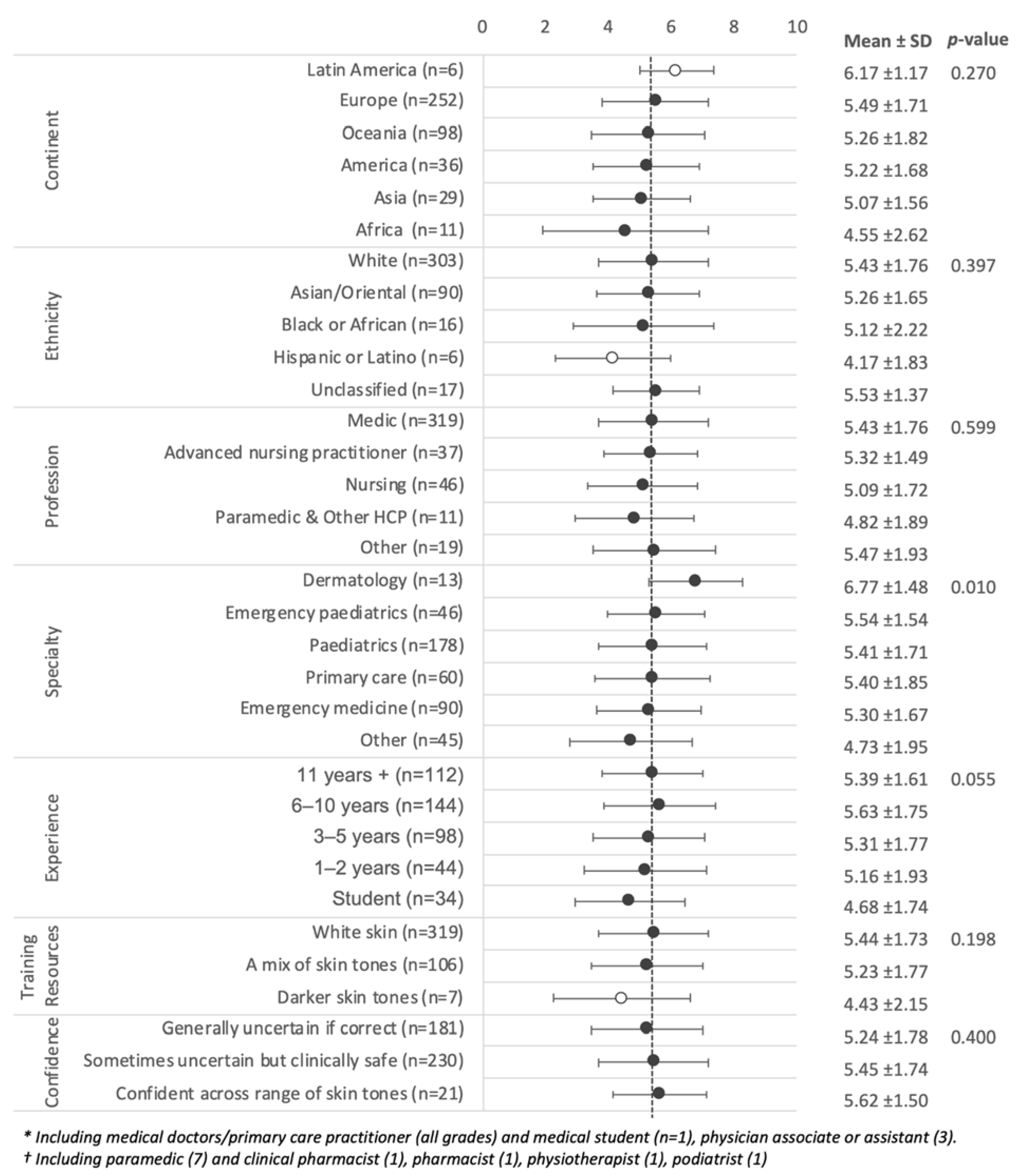
3.3. Quiz Scores by Demographic and Professional Background
3.4. Quiz Scores and Training Resources
3.5. Quiz Scores and Self-Reported Confidence
3.6. Well and Poorly Recognised Diagnoses
4. Discussion
5. Strength and Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Buonsenso, D.; Roland, D.; Abela, N.; Shanmugavadivel, D.; Platt, R.; Davis, T. Time to improve the diversity of paediatric skin images. Lancet Child Adolesc. Health 2020, 4, e44. [Google Scholar] [CrossRef]
- Lester, J.C.; Taylor, S.C.; Chren, M.-M. Under-representation of skin of colour in dermatology images: Not just an educational issue. Br. J. Dermatol. 2019, 180, 1521–1522. [Google Scholar] [CrossRef] [PubMed]
- Massie, J.P.; Cho, D.Y.; Kneib, C.J.; Sousa, J.D.; Morrison, S.D.; Friedrich, J.B. A Picture of modern medicine: Race and visual representation in medical literature. J. Natl. Med. Assoc. 2021, 113, 88–94. [Google Scholar] [CrossRef] [PubMed]
- Louie, P.; Wilkes, R. Representations of race and skin tone in medical textbook imagery. Soc. Sci. Med. 2018, 202, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Cho, D.Y.; Kneib, C.J.; Massie, J.P.; Sobol, D.L.; Crowe, C.S.; Shakir, A.; Burns, J.R.; Lane, M.; Morrison, S.D.; Sabin, J.; et al. Visual representation of racial diversity in aesthetic surgery literature. J. Plast. Reconstr. Aesthet. Surg. 2021, 74, 223–243. [Google Scholar] [CrossRef]
- Martin, G.C.; Kirgis, J.; Sid, E.; Sabin, J.A. Equitable imagery in the preclinical medical school curriculum: Findings from one medical school. Acad. Med. 2016, 91, 1002–1006. [Google Scholar] [CrossRef]
- Lester, J.; Jia, J.; Zhang, L.; Okoye, G.; Linos, E. Absence of images of skin of colour in publications of COVID-19 skin manifestations. Br. J. Dermatol. 2020, 183, 593–595. [Google Scholar] [CrossRef]
- Buster, K.J.; Stevens, E.I.; Elmets, C.A. Dermatologic health disparities. Dermatol. Clin. 2012, 30, 53–59. [Google Scholar] [CrossRef]
- Fenton, A.; Elliott, E.; Shahbandi, A.; Ezenwa, E.; Morris, C.; McLawhorn, J.; Jackson, J.G.; Allen, P.; Murina, A. Medical students’ ability to diagnose common dermatologic conditions in skin of color. J. Am. Acad. Dermatol. 2020, 83, 957–958. [Google Scholar] [CrossRef]
- Perlman, K.L.; Williams, N.M.; Egbeto, I.A.; Gao, D.X.; Siddiquee, N.; Park, J.H. Skin of color lacks representation in medical student resources: A cross-sectional study. Int. J. Women’s Dermatol. 2021, 7, 195–196. [Google Scholar] [CrossRef]
- Rodrigues, M.A.; Ross, A.L.; Gilmore, S.; Daniel, B.S. Australian dermatologists’ perspective on skin of colour: Results of a national survey. Australas. J. Dermatol. 2018, 59, e23–e30. [Google Scholar] [CrossRef] [PubMed]
- Shanmugavadivel, D.; Buonsenso, D.; Chantiluke, K.; Arora, M. Importance and impact of diversity in paediatric medical education. Arch. Dis. Child. Educ. Amp. Pract. Ed. 2021, 320796. [Google Scholar] [CrossRef]
- Shanmugavadivel, S.; Buonsenso, D.; Liu, J.-F.; Davis, T.; Roland, D. 926 Impact of diversity in training resources on self-confidence in diagnosing skin conditions across a range of skin tones: An international survey. Arch. Dis. Child. 2021, 106 (Suppl. S1). [Google Scholar] [CrossRef]
- Bell, G.; Holmes, S.; Gillespie, S.; Wood, A.; Murray, B.L. Images of dark skin in top emergency medicine journals: A cross-sectional analysis of images of emergent cutaneous disorders. AEM Educ. Train. 2021, 5 (Suppl. S1), S76–S81. [Google Scholar] [CrossRef] [PubMed]
- Fourniquet, S.E.; Garvie, K.; Beiter, K. Exposure to dermatological pathology on skin of color increases physician and student confidence in diagnosing pathology in patients of color. FASEB J. 2019, 33 (Suppl. S1), 606.18. [Google Scholar] [CrossRef]
- Blumenthal, D.; James, C.V. A data infrastructure for clinical trial diversity. N. Engl. J. Med. 2022, 386, 2355–2356. [Google Scholar] [CrossRef]
- Dunlop, H.; Fitzpatrick, E.; Kurti, K.; Deeb, S.; Gillespie, E.F.; Dover, L.; Yerramilli, D.; Gomez, S.L.; Chino, F.; Tsai, C.J. Participation of patients from racial and ethnic minority groups in phase 1 early cancer drug development trials in the US, 2000–2018. JAMA Netw. Open 2022, 5, e2239884. [Google Scholar] [CrossRef]
- Buonsenso, D.; Sollena, P.; Eke Tchangou, M.; De Rose, C.; Turriziani Colonna, A.; Sinatti, D.; Valentini, P.; Black Kids Matter Study Group. Black kids matter initiative calls for greater inclusion of black children in clinical trials. Acta Paediatr. 2021, 110, 1961–1962. [Google Scholar] [CrossRef]
- Chen, A.; Demaestri, S.; Schweiberger, K.; Sidani, J.; Wolynn, R.; Chaves-Gnecco, D.; Hernandez, R.; Rothenberger, S.; Mickievicz, E.; Cowden, J.D.; et al. Inclusion of non-english-speaking participants in pediatric health research: A review. JAMA Pediatr. 2022. [Google Scholar] [CrossRef]
- Nguyen, M.; Chaudhry, S.I.; Asabor, E.; Desai, M.M.; Lett, E.; Cavazos, J.E.; Mason, H.R.C.; Boatright, D. Variation in research experiences and publications during medical school by sex and race and ethnicity. JAMA Netw. Open 2022, 5, e2238520. [Google Scholar] [CrossRef]
- Guevara, J.P.; Wade, R.; Aysola, J. Racial and ethnic diversity at medical schools—Why aren’t we there yet? N. Engl. J. Med. 2021, 385, 1732–1734. [Google Scholar] [CrossRef] [PubMed]
- Israel, E.; Cardet, J.C.; Carroll, J.K.; Fuhlbrigge, A.L.; She, L.; Rockhold, F.W.; Maher, N.E.; Fagan, M.; Forth, V.E.; Yawn, B.P.; et al. Reliever-triggered inhaled glucocorticoid in black and latinx adults with asthma. N. Engl. J. Med. 2022, 386, 1505–1518. [Google Scholar] [CrossRef] [PubMed]
- Hicks, P.M.; Woodward, M.A.; Newman-Casey, P.A. Considerations for using large data sets to assess disparities in eye care and vision health. JAMA Ophthalmol. 2022, 4, 601. [Google Scholar] [CrossRef]
- Pham, H.H.; Sandberg, N.; Trinkl, J.; Thayer, J. Racial and ethnic differences in rates and age of diagnosis of autism spectrum disorder. JAMA Netw. Open 2022, 5, e2239604. [Google Scholar] [CrossRef] [PubMed]
- Elliott, T.; Floyd James, K.; Coleman, K.J.; Skrine Jeffers, K.; Nau, C.L.; Choi, K. Cross-sectional comparison of disparities by race using white vs hispanic as reference among children and youths with developmental disabilities referred for speech therapy. JAMA Netw. Open 2022, 5, e2234453. [Google Scholar] [CrossRef]
- Bavli, I.; Jones, D.S. Race correction and the X-ray machine—The controversy over increased radiation doses for black americans in 1968. N. Engl. J. Med. 2022, 387, 947–952. [Google Scholar] [CrossRef]
- Rubaltelli, F.F. Current drug treatment options in neonatal hyperbilirubinaemia and the prevention of kernicterus. Drugs. 1998, 56, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Constantinou, S.; Evans, J.; Goodwin, R.G. Fifteen-minute consultation: How to manage eczema in children. Arch. Dis. Child. Educ. Pr. Ed. 2021, 320560. [Google Scholar] [CrossRef]
- LINNET; JEMEC. An assessment of anxiety and dermatology life quality in patients with atopic dermatitis. Br. J. Dermatol. 1999, 140, 268–272. [Google Scholar] [CrossRef]
- Sharip, A.; Sorvillo, F.; Redelings, M.D.; Mascola, L.; Wise, M.; Nguyen, D.M. Population-based analysis of meningococcal disease mortality in the United States: 1990–2002. Pediatr. Infect. Dis. J. 2006, 25, 191–194. [Google Scholar] [CrossRef]


| n | Col% | |
|---|---|---|
| Continent | ||
| Europe | 252 | 58% |
| Oceania | 98 | 23% |
| America | 36 | 8% |
| Asia | 29 | 7% |
| Africa | 11 | 3% |
| Latin America | 6 | 1% |
| Ethnicity | ||
| White | 303 | 70% |
| Asian/Oriental | 90 | 21% |
| Black or African | 16 | 4% |
| Hispanic or Latino | 6 | 1% |
| Unclassified | 17 | 4% |
| Profession | ||
| Medic * | 319 | 74% |
| Nursing | 46 | 11% |
| Advanced nursing practitioner | 37 | 9% |
| Paramedic and other HCP | 11 | 3% |
| Other (not specified) | 19 | 4% |
| Specialty | ||
| Paediatrics | 178 | 41% |
| Emergency medicine | 90 | 21% |
| Primary care | 60 | 14% |
| Emergency paediatrics | 46 | 11% |
| Dermatology | 13 | 3% |
| Other † | 45 | 10% |
| Experience | ||
| Student | 34 | 8% |
| 1–2 years | 44 | 10% |
| 3–5 years | 98 | 23% |
| 6–10 years | 144 | 33% |
| 11 years + | 112 | 26% |
| Majority Training Resources | ||
| White skin | 319 | 74% |
| A mix of skin tones | 106 | 25% |
| Darker skin tones | 7 | 2% |
| Confidence in Diagnoses | ||
| Generally uncertain if correct | 181 | 42% |
| Sometimes uncertain but clinically safe | 230 | 53% |
| Confident across range of skin tones | 21 | 5% |
| Experience | Confidence | Quiz Score | |
|---|---|---|---|
| Experience | 1.000 | ||
| Confidence | 0.286 ** | 1.000 | |
| Quiz score | 0.087 | 0.076 | 1.000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shanmugavadivel, D.; Liu, J.-F.; Buonsenso, D.; Davis, T.; Roland, D. Assessing Healthcare Professionals’ Identification of Paediatric Dermatological Conditions in Darker Skin Tones. Children 2022, 9, 1749. https://doi.org/10.3390/children9111749
Shanmugavadivel D, Liu J-F, Buonsenso D, Davis T, Roland D. Assessing Healthcare Professionals’ Identification of Paediatric Dermatological Conditions in Darker Skin Tones. Children. 2022; 9(11):1749. https://doi.org/10.3390/children9111749
Chicago/Turabian StyleShanmugavadivel, Dhurgshaarna, Jo-Fen Liu, Danilo Buonsenso, Tessa Davis, and Damian Roland. 2022. "Assessing Healthcare Professionals’ Identification of Paediatric Dermatological Conditions in Darker Skin Tones" Children 9, no. 11: 1749. https://doi.org/10.3390/children9111749
APA StyleShanmugavadivel, D., Liu, J.-F., Buonsenso, D., Davis, T., & Roland, D. (2022). Assessing Healthcare Professionals’ Identification of Paediatric Dermatological Conditions in Darker Skin Tones. Children, 9(11), 1749. https://doi.org/10.3390/children9111749






