Insomnia and Neuroticism in Pakistani Medical Students: A Cross-Sectional Study
Abstract
1. Introduction
1.1. Sleep Disorders in Medical Education
1.2. Global Prevalence of Sleep Disturbances in Medical Students
1.3. Neuroticism and Its Association with Sleep Disturbances
1.4. The Intersection of Sleep, Personality, and Academic Performance
1.5. Environmental Factors and Living Arrangements in South Asian Medical Education
1.6. Study Rationale and Knowledge Gaps
1.7. Study Objectives
2. Methodology
2.1. Study Design and Setting
2.2. Study Population and Sampling
2.2.1. Target Population
2.2.2. Sample Size Calculation
2.2.3. Sampling Method and Selection Criteria
2.3. Data Collection Instruments
2.3.1. Study Questionnaire
2.3.2. Insomnia Severity Index (ISI)
2.3.3. Neuroticism (NEO-FFI) Assessment
2.3.4. Academic Performance Evaluation
2.4. Pilot Testing and Reliability Assessment
2.5. Ethical Considerations
2.6. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Descriptive Statistics for Primary Variables
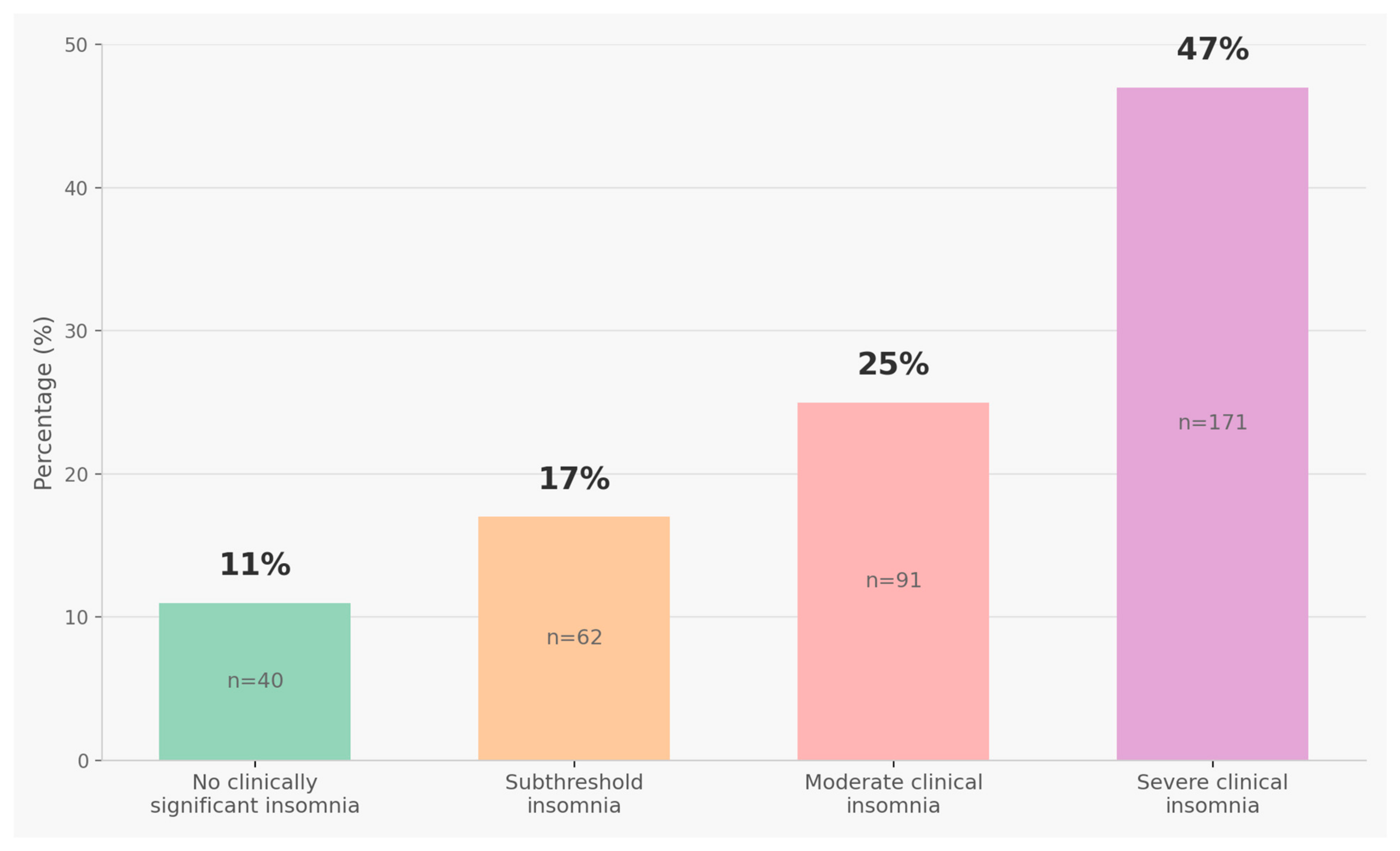
3.3. Insomnia Symptom Prevalence
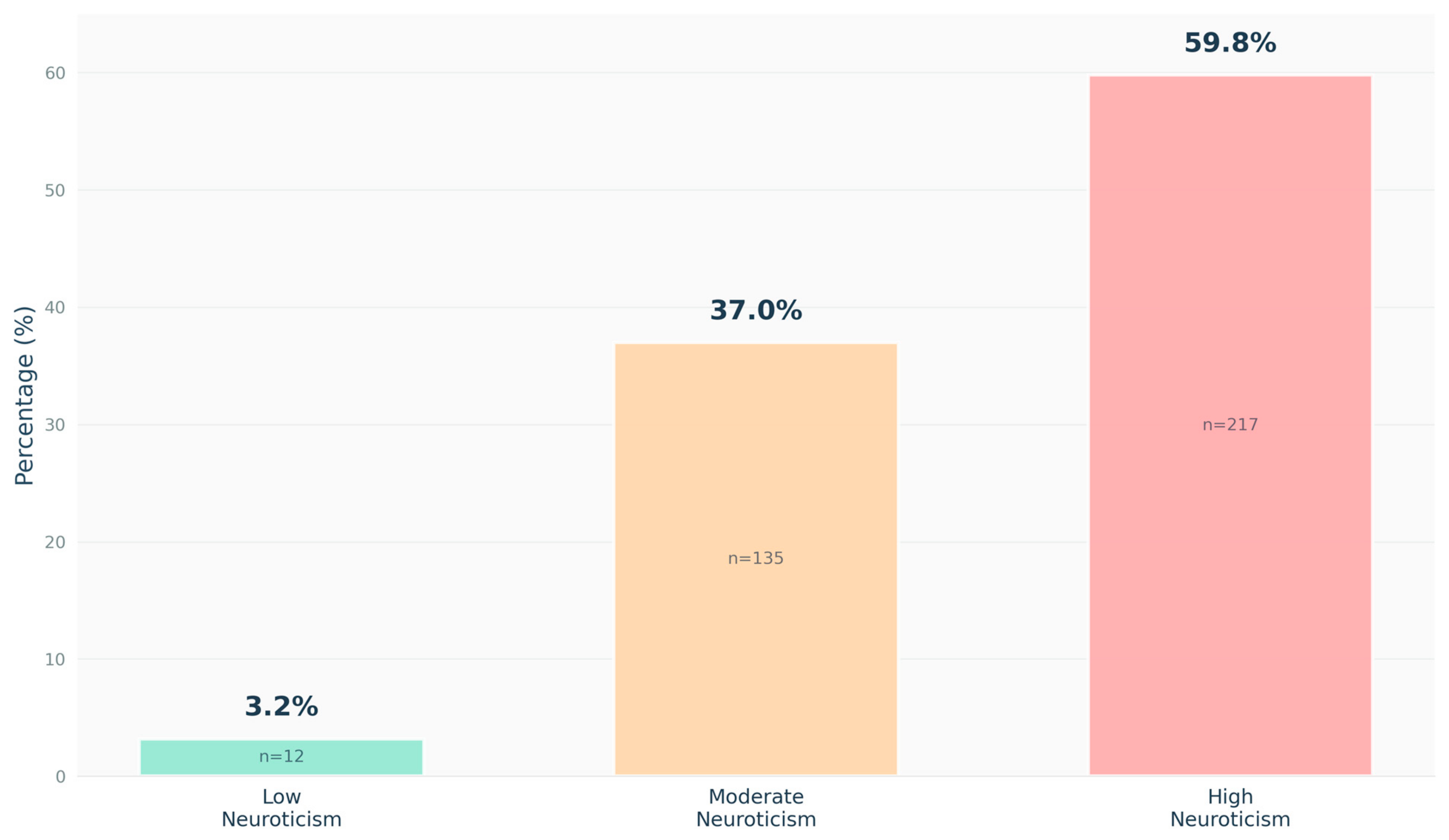
3.4. Neuroticism Level Distribution
3.5. Comparative Analysis by Living Arrangement
3.5.1. Insomnia Prevalence by Residence Type
3.5.2. Neuroticism Levels by Residence Type
3.6. Correlation Analysis
3.7. Multivariate Regression Analysis
3.7.1. Factors Associated with Insomnia Severity
3.7.2. Exploratory Interaction Effects Analysis
3.7.3. Model Diagnostics
4. Discussion
4.1. Principal Findings and Prevalence Context
4.2. Neuroticism-Insomnia Association: Mechanisms and Interpretation
4.3. Environmental Factors: Living Arrangements and Cultural Context
4.4. Academic Training Progression: Alternative Explanations
- Students experiencing severe insomnia and associated functional impairments may disproportionately withdraw from medical training before reaching clinical years, resulting in healthier clinical cohorts. Our cross-sectional design cannot address this possibility.
- Clinical students are older (confounded with academic year), and age showed marginal positive association with insomnia (p = 0.056), creating complex relationships.
- If data collection occurred during particularly stressful pre-clinical examination periods but routine clinical rotation periods, temporal variation in stress exposure could explain differences.
- Only students who successfully pass professional examinations progress to clinical years, potentially selecting for resilience factors.
4.5. Clinical Implications for Sleep Medicine Practice
4.6. Study Limitations
4.7. Future Research Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Krystal, A.D.; Ashbrook, L.H.; Prather, A.A. What is insomnia? JAMA 2021, 326, 2444. [Google Scholar] [CrossRef] [PubMed]
- Yassin, A.; Al-Mistarehi, A.H.; Beni Yonis, O.; Aleshawi, A.J.; Momany, S.M.; Khassawneh, B.Y. Prevalence of sleep disorders among medical students and their association with poor academic performance: A cross-sectional study. Ann. Med. Surg. 2020, 58, 124–129. [Google Scholar] [CrossRef] [PubMed]
- Becker, S.P.; Jarrett, M.A.; Luebbe, A.M.; Garner, A.A.; Burns, G.L.; Kofler, M.J. Sleep in a large, multi-university sample of college students: Sleep problem prevalence, sex differences, and mental health correlates. Sleep Health 2018, 4, 174–181. [Google Scholar] [CrossRef]
- Schlarb, A.A.; Claßen, M.; Grünwald, J.; Vögele, C. Sleep disturbances and mental strain in university students: Results from an online survey in Luxembourg and Germany. Int. J. Ment. Health. Syst. 2017, 11, 24. [Google Scholar] [CrossRef]
- Rao, W.W.; Li, W.; Qi, H.; Hong, L.; Chen, C.; Li, C.Y.; Ng, C.H.; Ungvari, G.S.; Xiang, Y.T. Sleep quality in medical students: A comprehensive meta-analysis of observational studies. Sleep Breath 2020, 24, 1151–1165. [Google Scholar] [CrossRef]
- Binjabr, M.A.; Alalawi, I.S.; Alzahrani, R.A.; Albalawi, O.S.; Hamzah, R.H.; Ibrahim, Y.S.; Buali, F.; Husni, M.; BaHammam, A.S.; Vitiello, M.V.; et al. The worldwide prevalence of sleep problems among medical students by problem, country, and COVID-19 status: A systematic review, meta-analysis, and meta-regression of 109 studies involving 59427 participants. Curr. Sleep Med. Rep. 2023, 9, 161–179. [Google Scholar] [CrossRef]
- Javaid, R.; Momina, A.; Sarwar, M.Z.; Naqi, S.A. Quality of sleep and academic performance among medical university students. J. Coll. Physicians Surg. Pak. 2020, 30, 1281–1285. [Google Scholar] [CrossRef]
- Yusoff, M.S.B.; Hadie, S.N.H.; Yasin, M.A.M. The roles of emotional intelligence, neuroticism, and academic stress on the relationship between psychological distress and burnout in medical students. BMC Med. Educ. 2021, 21, 293. [Google Scholar] [CrossRef]
- Valencia, J.; Frikson, C. The relationship between neuroticism, emotion regulation, and academic stress with depression symptoms in Indonesian medical students. Open Access Maced. J. Med. Sci. 2022, 10, 233–237. [Google Scholar] [CrossRef]
- Kim, C.; Lee, S.; Youn, S.; Park, B.; Chung, S. Insomnia and neuroticism are related with depressive symptoms of medical students. Sleep Med. Res. 2019, 8, 33–38. [Google Scholar] [CrossRef]
- Yin, X.; Yuan, C.; Sun, M.; Sun, J.; Zhang, N.; Qin, W.; Liu, F.; Xue, H.; Ding, H.; Wang, S.; et al. Personality and brain contribute to academic achievements of medical students. Front. Neurosci. 2022, 16, 964904. [Google Scholar] [CrossRef] [PubMed]
- Hintsanen, M.; Puttonen, S.; Smith, K.; Törnroos, M.; Jokela, M.; Pulkki-Råback, L.; Hintsa, T.; Merjonen, P.; Dwyer, T.; Raitakari, O.T.; et al. Five-factor personality traits and sleep: Evidence from two population-based cohort studies. Health Psychol. 2014, 33, 1214–1223. [Google Scholar] [CrossRef] [PubMed]
- Morin, C.M.; Belleville, G.; Bélanger, L.; Ivers, H. The Insomnia Severity Index: Psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep 2011, 34, 601–608. [Google Scholar] [CrossRef] [PubMed]
- Bastien, C.H.; Vallières, A.; Morin, C.M. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. 2001, 2, 297–307. [Google Scholar] [CrossRef]
- Costa, P.T.; McCrae, R.R. Revised NEO Personality Inventory (NEO-PI-R) and NEO Five-Factor Inventory (NEO-FFI) Professional Manual; Psychological Assessment Resources: Odessa, FL, USA, 1992. [Google Scholar]
- Anupama, M.; Kulkarni, H.; Nisarga, V.; Sushravya. Perceived stress and insomnia among medical residents in South India: A cross-sectional study. Ann. Indian Psychiatry 2022, 6, 142–148. [Google Scholar] [CrossRef]
- Mohamed, E.Y.; Abdulrahim, S.A.; Sami, W. Insomnia and anxiety in medical students: A cross-sectional study at Majmaah University, Saudi Arabia. J. Res. Med. Dent. Sci. 2019, 8, 112–118. [Google Scholar]
- Rehman, F.; Naiyar, I.; Umar, M.; Rehman, A.; Shahzad, A.; Un Nisa, H. Pattern and associated factors of exam anxiety among students of private medical college Pakistan. Pak. J. Med. Health Sci. 2020, 14, 669–671. [Google Scholar]
- Yusoff, M.S.B.; Esa, A.R.; Mat Pa, M.N.; Mey, S.C.; Aziz, R.A.; Abdul Rahim, A.F. A longitudinal study of relationships between previous academic achievement, emotional intelligence and personality traits with psychological health of medical students during stressful periods. Educ. Health 2013, 26, 39–47. [Google Scholar] [CrossRef]
- Al-Shahrani, R.M.; Al-Moalwi, N.M.; Al Qahtani, A.A.; Siddiqui, A.F. The prevalence and associated factors of academic stress among medical students of King Khalid University: An analytical cross-sectional study. Healthcare 2023, 11, 2029. [Google Scholar] [CrossRef]
- Zahid, S.; Hamid, Y.; Maqsood, M.; Khan, H.; Bukhari, A. Prevalence of anxiety, depression, and stress among medical students: A cross-sectional study at Nishtar Medical University, Multan, Pakistan. J. Pak. Med. Assoc. 2022, 72, 596–601. [Google Scholar]
- Khalid, S.; Khan, F.; Bukhari, A.H.S.; Yasin, H.; Munir, M.; Younas, H. Poor sleep and its deprivation factors in medical students: A comparative cross-sectional study between hostelites and day scholar. Hist. Med. 2024, 10, 1026–1034. [Google Scholar]
- Khan, M.A.; Malik, F.R. A comparative descriptive study of sleep quality impact among day scholar and hostel dweller medical undergraduates upon academic performance. Isra Med. J. 2021, 13, 275–280. [Google Scholar]
- Qureshi, A.; Aslam, M.; Kamran, H.; Sandhu, K.; Fatima, D. Comparison of Dietary Habits and Psychological Outcomes in Hostelites and Day Scholars: Dietary Habits and Outcomes in Hostelites and Day Scholars. Diet Factor J. Nutr. Food Sci. 2022, 3, 22–27. [Google Scholar] [CrossRef]
- Zakiei, A.; Sadeghi-Bahmani, D.; Khazaie, H.; Lorestani, Z.; Sadeghi, M.; Korani, D.; Sahraei, Z.; Komasi, S.; Stanga, Z.; Brühl, A.B.; et al. Associations between sleep disturbances, personality traits, and self-regulation in a sample of healthy adults. J. Clin. Med. 2024, 13, 2143. [Google Scholar] [CrossRef] [PubMed]
- Nechita, F.; Alexandru, D.O.; Turcu-Ştiolică, R.; Nechita, D. The influence of personality factors and stress on academic performance. Curr. Health Sci. J. 2015, 41, 47–61. [Google Scholar] [CrossRef]
- Mohamed, Z.; Jit Singh, G.K.; Dediwadon, N.S.; Mohamad Saleh, N.A.; Jupri, N.N.; Ganesan, Y. Adult personality and its relationship with stress level, coping mechanism and academic performance among undergraduate nursing students. Malays. J. Med. Sci. 2022, 29, 117–125. [Google Scholar] [CrossRef]
- Zainah, M.; Akmal, M.N.; Syazwani, N.; Sim, T.S.; Nur, E.A.; Wan Norshafika, W.M.Z. Adult personality and its relationship with stress level and coping mechanism among final year medical students. Med. Health 2019, 14, 154–167. [Google Scholar] [CrossRef]
- Varo, C.; Aires-González, M.D.M.; García-Jiménez, M. Effective coping with academic stress is a matter of personality types: Revisiting the person-centred approach. Behav. Sci. 2023, 13, 687. [Google Scholar] [CrossRef]
- Slavish, D.C.; Graham-Engeland, J.E.; Sliwinski, M.J.; Smyth, J.M.; Lipton, R.B.; Katz, M.J.; Almeida, D.M. Neuroticism, rumination, negative affect, and sleep: Examining between- and within-person associations. Pers. Individ. Dif. 2017, 123, 217–222. [Google Scholar] [CrossRef]
- Wang, R.; Mu, Z.; Li, X.; Cheung, F.T.W.; Chan, N.Y.; Chan, J.W.Y.; Wing, Y.K.; Li, S.X. The relationship between NEO-five personality traits and sleep-related characteristics: A systematic review and meta-analysis. Sleep Med. Rev. 2025, 81, 102081. [Google Scholar] [CrossRef]
- Haylı, Ç.M.; Avcı, M.Z. Determining the factors that affect and enhance sleep quality of students in nursing departments: A qualitative study. Sleep Med. Res. 2023, 14, 207–212. [Google Scholar] [CrossRef]

| Variable | Category | n (%) |
|---|---|---|
| Age | Mean ± SD | 21.33 ± 2.26 years |
| Gender | Male | 174 (47.8%) |
| Female | 190 (52.2%) | |
| Academic Level | Pre-clinical (Years 2–3) | 84 (23.1%) |
| Clinical (Years 4–5) | 280 (76.9%) | |
| Institution Type | Public | 116 (31.9%) |
| Private | 248 (68.1%) | |
| Living Arrangement | Hostel resident | 195 (53.6%) |
| Day scholar | 169 (46.4%) | |
| Academic Performance | 35–60% | 35 (9.6%) |
| 60–85% | 278 (76.4%) | |
| 85–100% | 51 (14.0%) |
| Variable | Mean ± SD | Median | Range | Skewness | Kurtosis |
|---|---|---|---|---|---|
| ISI Total Score | 17.82 ± 6.53 | 18.0 | 3–28 | −0.21 | −0.69 |
| Neuroticism Score | 32.45 ± 8.76 | 33.0 | 13–58 | 0.08 | −0.42 |
| Variable | Category | Hostel Residents n (%) | Day Scholars n (%) | χ2 | p-Value | Effect Size |
|---|---|---|---|---|---|---|
| Any Insomnia Symptoms (ISI ≥ 8) | Present | 147 (75.4%) | 117 (69.2%) | 1.579 | 0.209 | h = 0.14 |
| Absent | 48 (24.6%) | 52 (30.8%) | ||||
| Clinical Insomnia (ISI ≥ 15) | Present | 148 (75.9%) | 114 (67.5%) | 3.047 | 0.081 | h = 0.19 |
| Absent | 47 (24.1%) | 55 (32.5%) | ||||
| Neuroticism Level | High | 111 (56.9%) | 106 (62.7%) | 4.502 | 0.069 | V = 0.11 |
| Moderate/Low | 84 (43.1%) | 63 (37.3%) |
| Variable | ISI Score | Neuroticism |
|---|---|---|
| ISI Score | 1.000 | - |
| Neuroticism | 0.351 ** | 1.000 |
| Predictor | Unstandardized β (95% CI) | Standardized β | p-Value | Cohen’s d |
|---|---|---|---|---|
| Intercept | 0.754 (−4.125, 5.633) | - | 0.762 | - |
| Neuroticism | 0.239 (0.173, 0.305) | 0.342 | <0.001 * | 0.32 |
| Age | 0.217 (−0.006, 0.441) | 0.075 | 0.056 | - |
| Female | 0.470 (−0.813, 1.753) | 0.036 | 0.473 | - |
| Clinical Year | −1.271 (−1.826, −0.717) | −0.097 | <0.001 * | 0.19 |
| Hostel Resident | 1.179 (−0.109, 2.467) | 0.090 | 0.073 | - |
| Predictor | β (95% CI) | p-Value |
|---|---|---|
| Neuroticism | 0.190 (0.102, 0.279) | <0.001 * |
| Age | 0.239 (0.027, 0.451) | 0.027 * |
| Female | 0.504 (−0.781, 1.789) | 0.442 |
| Clinical Year | −1.262 (−1.809, −0.714) | <0.001 * |
| Hostel Resident | −2.025 (−6.265, 2.214) | 0.349 |
| Neuroticism × Hostel | 0.100 (−0.025, 0.225) | 0.118 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Qazi, S.; Ahmad, A.; Khan, M.A.; Qureshi, Y.A.; Qasim, M.; Farooq, H.; Shuaib, S.; Irshad, L.; Tajwali, S.; Ali, H.; et al. Insomnia and Neuroticism in Pakistani Medical Students: A Cross-Sectional Study. Healthcare 2025, 13, 2778. https://doi.org/10.3390/healthcare13212778
Qazi S, Ahmad A, Khan MA, Qureshi YA, Qasim M, Farooq H, Shuaib S, Irshad L, Tajwali S, Ali H, et al. Insomnia and Neuroticism in Pakistani Medical Students: A Cross-Sectional Study. Healthcare. 2025; 13(21):2778. https://doi.org/10.3390/healthcare13212778
Chicago/Turabian StyleQazi, Sadia, Abdal Ahmad, Muhammad Awais Khan, Yameen Ahmed Qureshi, Muhammad Qasim, Hamza Farooq, Sara Shuaib, Laiba Irshad, Sanam Tajwali, Hamza Ali, and et al. 2025. "Insomnia and Neuroticism in Pakistani Medical Students: A Cross-Sectional Study" Healthcare 13, no. 21: 2778. https://doi.org/10.3390/healthcare13212778
APA StyleQazi, S., Ahmad, A., Khan, M. A., Qureshi, Y. A., Qasim, M., Farooq, H., Shuaib, S., Irshad, L., Tajwali, S., Ali, H., & Wazir, N. U. (2025). Insomnia and Neuroticism in Pakistani Medical Students: A Cross-Sectional Study. Healthcare, 13(21), 2778. https://doi.org/10.3390/healthcare13212778






