Training and Toolkit Resources to Support Implementation of a Community Pharmacy Fall Prevention Service
Abstract
1. Introduction
2. Materials and Methods
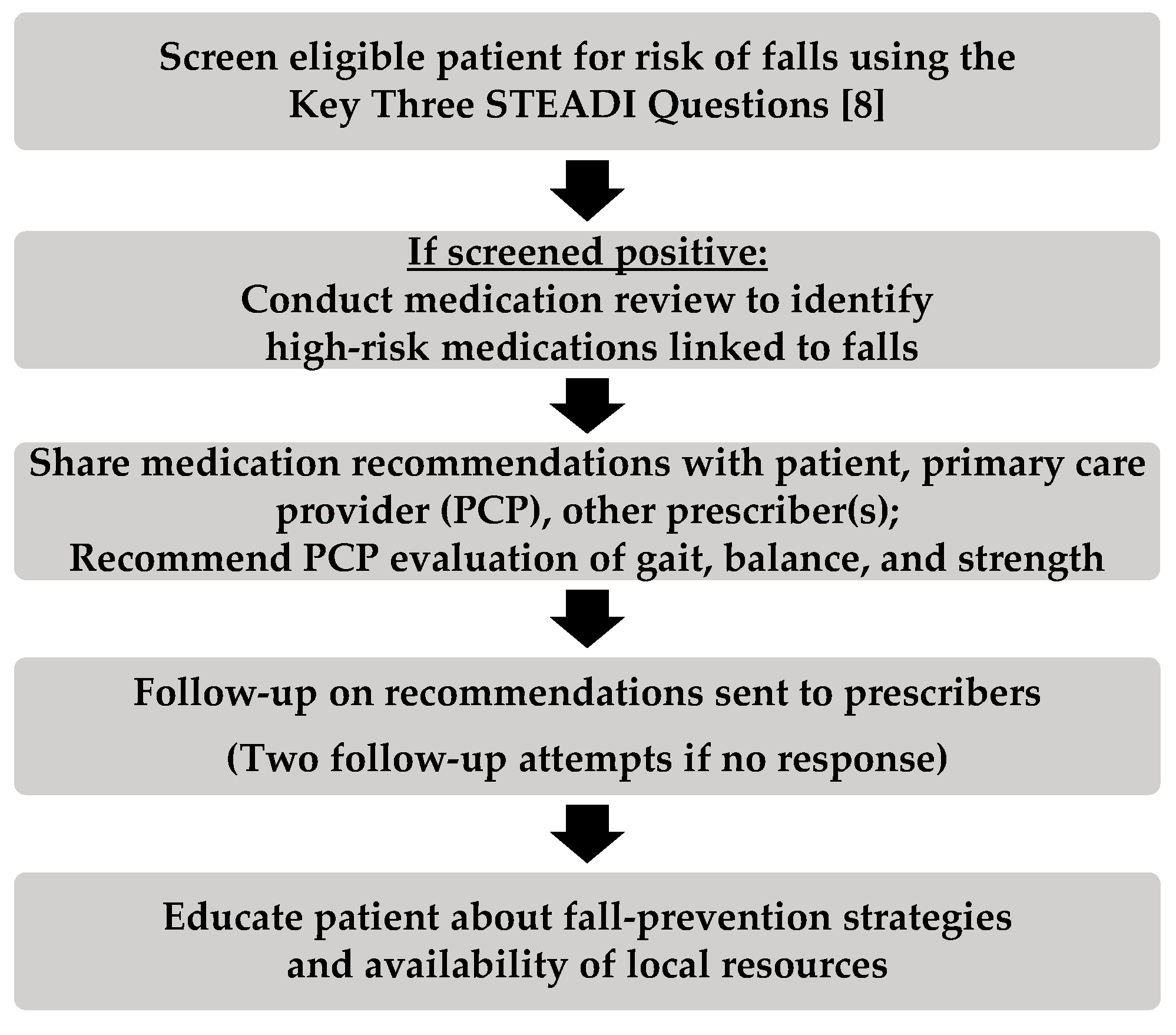
2.1. Service Description
2.2. Participants
2.3. Tool Development
2.4. Training Approach
2.5. Technical Support and Quality Assurance/Quality Improvement
2.6. Program Assessment
3. Results
3.1. Baseline Characteristics
3.2. Usefulness of Toolkit Resources
3.3. Participation and Usefulness of Training
3.4. Toolkit Resource Changes
3.5. Program Successes and Challenges
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bergen, G.; Stevens, M.R.; Burns, E.R. Falls and fall injuries among adults aged ≥65 years—United States, 2014. MMWR Morb. Mortal. Wkly. Rep. 2016, 65, 993–998. [Google Scholar] [CrossRef] [PubMed]
- Stel, V.S.; Smit, J.H.; Pluijm, S.M.F.; Lips, P. Consequences of falling in older men and women and risk factors for health service use and functional decline. Age Ageing 2004, 33(1), 58–65. [Google Scholar] [CrossRef] [PubMed]
- Florence, C.S.; Bergen, G.; Atherly, A.; Burns, E.; Stevens, J.; Drake, C. Medical costs of fatal and nonfatal falls in older adults. J. Am. Geriatr. Soc. 2018, 66, 693–698. [Google Scholar] [CrossRef] [PubMed]
- National Prevention Council. Healthy Aging in Action: Advancing the National Prevention Strategy; US Department of Health and Human Services, Office of the Surgeon General: Washington, DC, USA, 2016.
- Woolcott, J.C.; Richardson, K.J.; Wiens, M.O.; Patel, B.; Marin, J.; Khan, K.M.; Marra, C.A. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch. Intern. Med. 2009, 169, 1952–1960. [Google Scholar] [CrossRef] [PubMed]
- Dhalwani, N.N.; Fahami, R.; Sathanapally, H.; Seidu, S.; Davies, M.J.; Khunti, K. Association between polypharmacy and falls in older adults: A longitudinal study from England. BMJ Open 2017, 7, e016358. [Google Scholar] [CrossRef] [PubMed]
- Stevens, J.A.; Phelan, E.A. Development of STEADI: A fall prevention resource for health care providers. Health Promot. Pract. 2013, 14, 706–714. [Google Scholar] [CrossRef] [PubMed]
- Stevens, J.A. The STEADI tool kit: A fall prevention resource for health care providers. IHS Prim. Care Provid. 2013, 39, 162–166. [Google Scholar] [PubMed]
- Jones, T.S.; Ghosh, T.S.; Horn, K.; Smith, J.; Vogt, R.L. Primary care physicians perceptions and practices regarding fall prevention in adult’s 65 years and over. Accid. Anal. Prev. 2011, 43, 1605–1609. [Google Scholar] [CrossRef]
- Howland, J.; Hackman, H.; Taylor, A.; O’Hara, K.; Liu, J.; Brusch, J. Older adult fall prevention practices among primary care providers at accountable care organizations: A pilot study. PLoS ONE 2018, 13, e0205279. [Google Scholar] [CrossRef]
- Kantor, E.D.; Rehm, C.D.; Haas, J.S.; Chan, A.T.; Giovannucci, E.L. Trends in prescription drug use among adults in the United States from 1999–2012. JAMA 2015, 314, 1818–1831. [Google Scholar] [CrossRef]
- Barnett, M.L.; Song, Z.; Landon, B.E. Trends in physician referrals in the United States, 1999–2009. Arch. Intern. Med. 2012, 172, 163–170. [Google Scholar] [CrossRef] [PubMed]
- Wright, D.J.; Twigg, M.J. Community pharmacy: An untapped patient data resource. Integr. Pharm. Res. Pr. 2016, 5, 19–25. [Google Scholar] [CrossRef][Green Version]
- Casteel, C.; Blalock, S.J.; Ferreri, S.; Roth, M.T.; Demby, K.B. Implementation of a community pharmacy–Based falls prevention program. Am. J. Geriatr. Pharmacother. 2011, 9, 310–319. [Google Scholar] [CrossRef] [PubMed]
- Blalock, S.J.; Casteel, C.; Roth, M.T.; Ferreri, S.; Demby, K.B.; Shankar, V. Impact of enhanced pharmacologic care on the prevention of falls: A randomized controlled trial. Am. J. Geriatr. Pharmacother. 2010, 8, 428–440. [Google Scholar] [CrossRef] [PubMed]
- Ferreri, S.; Roth, M.T.; Casteel, C.; Demby, K.B.; Blalock, S.J. Methodology of an ongoing, randomized controlled trial to prevent falls through enhanced pharmaceutical care. Am. J. Geriatr. Pharmacother. 2008, 6, 61–81. [Google Scholar] [CrossRef]
- Turner, K.; Trogdon, J.G.; Weinberger, M.; Stover, A.M.; Ferreri, S.; Farley, J.F.; Ray, N.; Patti, M.; Renfro, C.; Shea, C.M. Testing the organizational theory of innovation implementation effectiveness in a community pharmacy medication management program: A hurdle regression analysis. Implement. Sci. 2018, 13, 105. [Google Scholar] [CrossRef] [PubMed]
- Turner, K.; Renfro, C.; Ferreri, S.; Roberts, K.; Pfeiffenberger, T.; Shea, C.M. Supporting community pharmacies with implementation of a web-based medication management application. Appl. Clin. Inform. 2018, 9, 391–402. [Google Scholar] [CrossRef]
- Wandersman, A.; Chien, V.H.; Katz, J. Toward an evidence-based system for innovation support for implementing innovations with quality: Tools, training, technical assistance, and quality assurance/quality improvement. Am. J. Community Psychol. 2012, 50, 445–459. [Google Scholar] [CrossRef]
- Check for Safety: A Home Fall Prevention Checklist for Older Adults. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. 2015. Available online: https://www.cdc.gov/steadi/pdf/check_for_safety_brochure-a.pdf (accessed on 28 June 2019).
- What You Can Do to Prevent Falls. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. 2015. Available online: https://www.cdc.gov/HomeandRecreationalSafety/pubs/English/brochure_Eng_desktop-a.pdf (accessed on 28 June 2019).
- Postural Hypotension What it is & How to Manage it. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Available online: https://stacks.cdc.gov/view/cdc/30739 (accessed on 8 August 2019).
- Brown, T.; Robinson, J.M.; Renfro, C.P.; Blalock, S.J.; Ferreri, S. Analysis of the relationship between patients’ fear of falling and prescriber acceptance of community pharmacists’ recommendations. Cogent Med. 2019. [Google Scholar] [CrossRef]
- STEADI: The Pharmacist’s Role in Older Adult Fall Prevention. American Pharmacists Association. 2017. Available online: http://elearning.pharmacist.com/products/4721/steadi-cdc?sectionId=ecaf7f86-3245-4b25-92f7-ccf1681d0f50 (accessed on 28 June 2019).
- Fritsch, M.; Shelton, P.; Bell, A.; Schneider, E. Collaborative approach to falls assessment and prevention: Pharmacists’ use of the ASCP/NCOA falls risk reduction toolkit. In Proceedings of the North Carolina Association of Pharmacists Annual Meeting, Winston-Salem, NC, USA, 21–22 September 2017. [Google Scholar]
- Langley, G.L.; Moen, R.; Nolan, K.M.; Nolan, T.W.; Norman, C.L.; Provost, L.P. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance, 2nd ed.; Jossey-Bass Publishers: San Francisco, CA, USA, 2009. [Google Scholar]
- Schultz, P.W.; Nolan, J.M.; Cialdini, R.B.; Goldstein, N.J.; Griskevicius, V. The Constructive, destructive, and reconstructive power of social norms. Psychol. Sci. 2007, 18, 429–434. [Google Scholar] [CrossRef]
- Law, A.V.; Okamoto, M.P.; Chang, P.S. Prevalence and types of disease management programs in community pharmacies in California. J. Manag. Care Pharm. 2005, 11, 505–512. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.G.; Ferreri, S.P.; Brown, P.; Wines, K.; Shea, C.M.; Pfeiffenberger, T.M. Implementing an integrated care management program in community pharmacies: A focus on medication management services. J. Am. Pharm. Assoc. 2017, 57, 229–235. [Google Scholar] [CrossRef] [PubMed]
- Dosea, A.S.; Brito, G.C.; Santos, L.M.C.; Marques, T.C.; Balisa-Rocha, B.; Pimentel, D.; Lyra, D.P., Jr. Establishment, implementation, and consolidation of clinical pharmacy services in community Pharmacies: perceptions of a group of pharmacists. Qual. Health Res. 2017, 27, 363–373. [Google Scholar] [CrossRef] [PubMed]
- Law, A.V.; Okamoto, M.P.; Brock, K. Ready, willing, and able to provide MTM services? A survey of community pharmacists in the USA. Res. Soc. Adm. Pharm. 2009, 5, 376–381. [Google Scholar] [CrossRef] [PubMed]
- Fixsen, D.L.; Blase, K.A.; Naoom, S.F.; Wallace, F. Core implementation components. Res. Soc. Work Pract. 2009, 19, 531–540. [Google Scholar] [CrossRef]
- Hausknecht, J.P.; Trevor, C.O. Collective turnover at the group, unit, and organizational levels: Evidence, issues, and implications. J. Manag. 2011, 37, 352–388. [Google Scholar] [CrossRef]
- STEADI: The Pharmacist’s Role in Older Adult Fall Prevention Resources List. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. 2017. Available online: https://www.cdc.gov/steadi/pdf/STEADIPharmacistTrainingResources-508.pdf (accessed on 28 June 2019).
- Talking about Fall Prevention with Your Patients. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. 2017. Available online: https://www.cdc.gov/steadi/pdf/Talking_about_Fall_Prevention_with_Your_Patients-print.pdf (accessed on 28 June 2019).
| Tool | Function |
|---|---|
| High-risk medication algorithms (nine total) | Identify drug class-specific risk factors and alternative treatment strategies |
| High-risk medication index | Identify high-risk medications and correlating drug class |
| Prescriber communication form [23] | Transmit patient screening results and pharmacists’ recommendations to prescriber and/or primary care provider |
| Cover fax form | Prompt other health care providers to recall purpose of community pharmacy fall prevention service |
| Prescriber response form [23] | Gather prescriber acceptance/rejection of pharmacists’ recommendations |
| Medication checklist | Collect list of high-risk medications and relevant health information |
| Prescriber flyer | Promote community pharmacy fall prevention service to prescribers and/or primary care provider |
| Patient education brochures † | Educate patients about risk factors and evidence-based strategies to prevent falls |
| Community resources | Identify local/regional evidence-based fall prevention resources for patient referral |
| Characteristic | N (%) |
|---|---|
| Role (N = 31) | |
| Technician | 1 (3) |
| Owner Pharmacist | 6 (19) |
| Staff Pharmacist | 24 (77) |
| Education and Training (N = 23) †,‡ | |
| Technician Certification (CPhT) | 1 (4) |
| Board Certification | 2 (9) |
| Clinical Pharmacy Practitioner | 2 (9) |
| Residency | 3 (13) |
| Pharmacist graduate (BS Pharm) | 8 (35) |
| Pharmacist graduate (PharmD) | 14 (61) |
| Years Worked at Site (N = 23) † | |
| <1 year | 1 (4) |
| 1–5 years | 7 (30) |
| >5 years | 15 (65) |
| Resources | Mean (SD) † |
|---|---|
| High-risk medication algorithms (N = 22) * | 2.95 (SD = 0.21) |
| High-risk medication index (N = 22) * | 2.91 (SD = 0.29) |
| Prescriber communication form (N = 22) * | 2.91 (SD = 0.29) |
| Cover fax form (N = 22) * | 2.77 (SD = 0.43) |
| Prescriber response form (N = 22) * | 2.77 (SD = 0.43) |
| Medication review checklist (N = 18) * | 2.67 (SD = 0.59) |
| Prescriber marketing flyer (N = 18) * | 2.50 (SD = 0.62) |
| STEADI patient education brochures (N = 20) * | 2.45 (SD = 0.60) |
| Community resources (N = 19) * | 2.11 (SD = 0.66) |
| Training Activities | Mean (SD) † |
|---|---|
| Live workshop (N = 3) *,‡ | 3.00 (SD = 0) |
| Onboard training webinar (N = 22) * | 2.86 (SD = 0.35) |
| Site visit (N = 21) * | 2.71 (SD = 0.56) |
| Coaching (N = 17) * | 2.59 (SD = 0.51) |
| Quick tips webinars (N = 17) * | 2.35 (SD = 0.61) |
| Quick tips emails (N = 21) * | 2.29 (SD = 0.56) |
| APhA Online CPE (N = 15) * | 2.27 (SD = 0.59) |
| Webinar Topics | |
| Workflow integration (N = 17) * | 2.41 (SD = 0.62) |
| Engaging with prescribers (N = 17) * | 2.38 (SD = 0.62) |
| Engaging with patients (N = 16) * | 2.35 (SD = 0.61) |
| Peer examples (N = 17) * | 2.35 (SD = 0.49) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Robinson, J.M.; Renfro, C.P.; Shockley, S.J.; Blalock, S.J.; Watkins, A.K.; Ferreri, S.P. Training and Toolkit Resources to Support Implementation of a Community Pharmacy Fall Prevention Service. Pharmacy 2019, 7, 113. https://doi.org/10.3390/pharmacy7030113
Robinson JM, Renfro CP, Shockley SJ, Blalock SJ, Watkins AK, Ferreri SP. Training and Toolkit Resources to Support Implementation of a Community Pharmacy Fall Prevention Service. Pharmacy. 2019; 7(3):113. https://doi.org/10.3390/pharmacy7030113
Chicago/Turabian StyleRobinson, Jessica M., Chelsea P. Renfro, Sarah J. Shockley, Susan J. Blalock, Alicia K. Watkins, and Stefanie P. Ferreri. 2019. "Training and Toolkit Resources to Support Implementation of a Community Pharmacy Fall Prevention Service" Pharmacy 7, no. 3: 113. https://doi.org/10.3390/pharmacy7030113
APA StyleRobinson, J. M., Renfro, C. P., Shockley, S. J., Blalock, S. J., Watkins, A. K., & Ferreri, S. P. (2019). Training and Toolkit Resources to Support Implementation of a Community Pharmacy Fall Prevention Service. Pharmacy, 7(3), 113. https://doi.org/10.3390/pharmacy7030113





