Pilot and Feasibility of Combining a Medication Adherence Intervention and Group Diabetes Education for Patients with Type-2 Diabetes
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Group Assignment and Recruitment
2.3. Initial Assessment
2.4. Diabetes Education and Medication Synchronization Arm
2.5. Medication Synchronization Service Only Arm
2.6. Control Arm
2.7. Measurements and Variables
2.8. Data Collection
2.9. Data Analysis
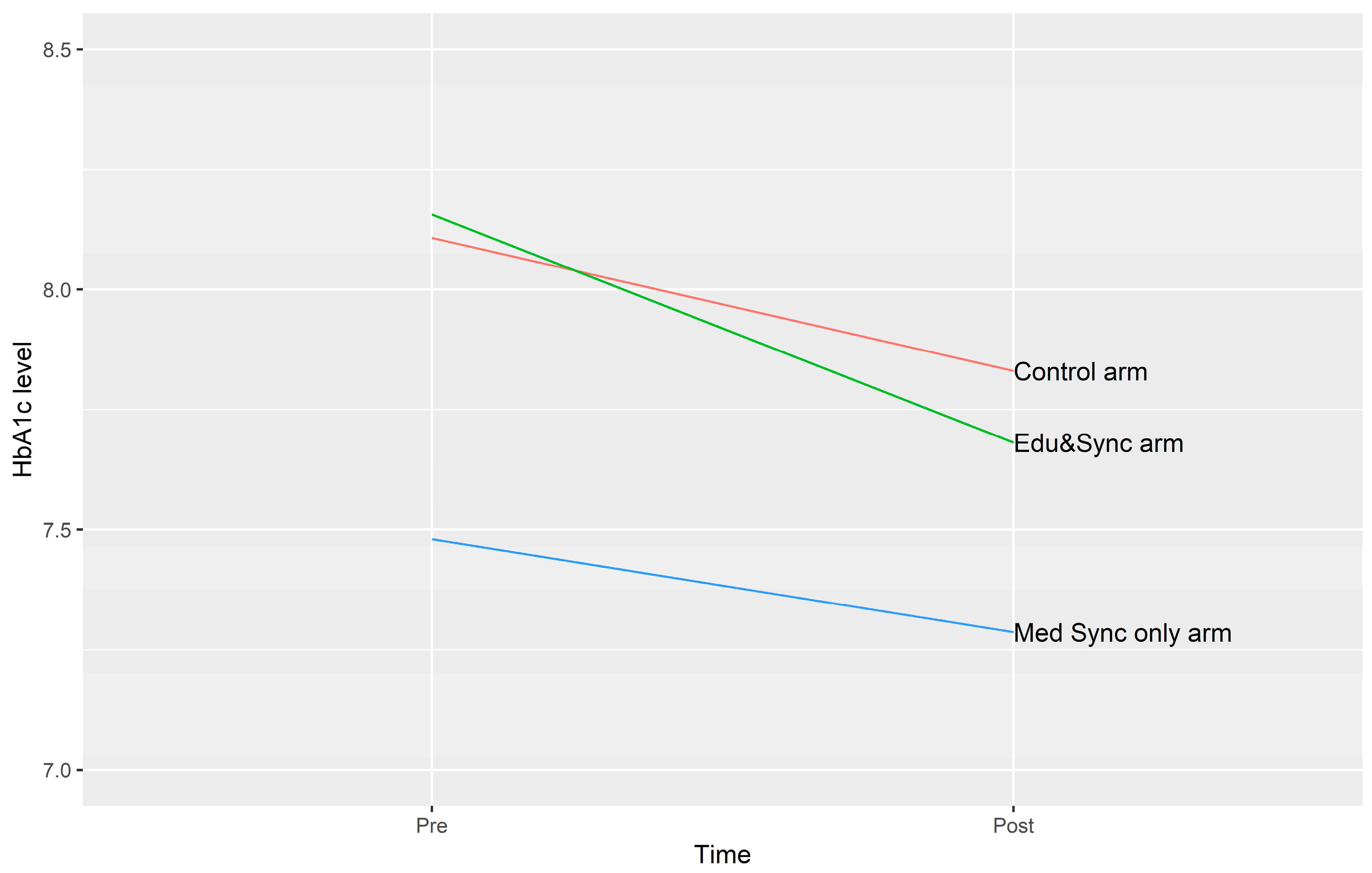
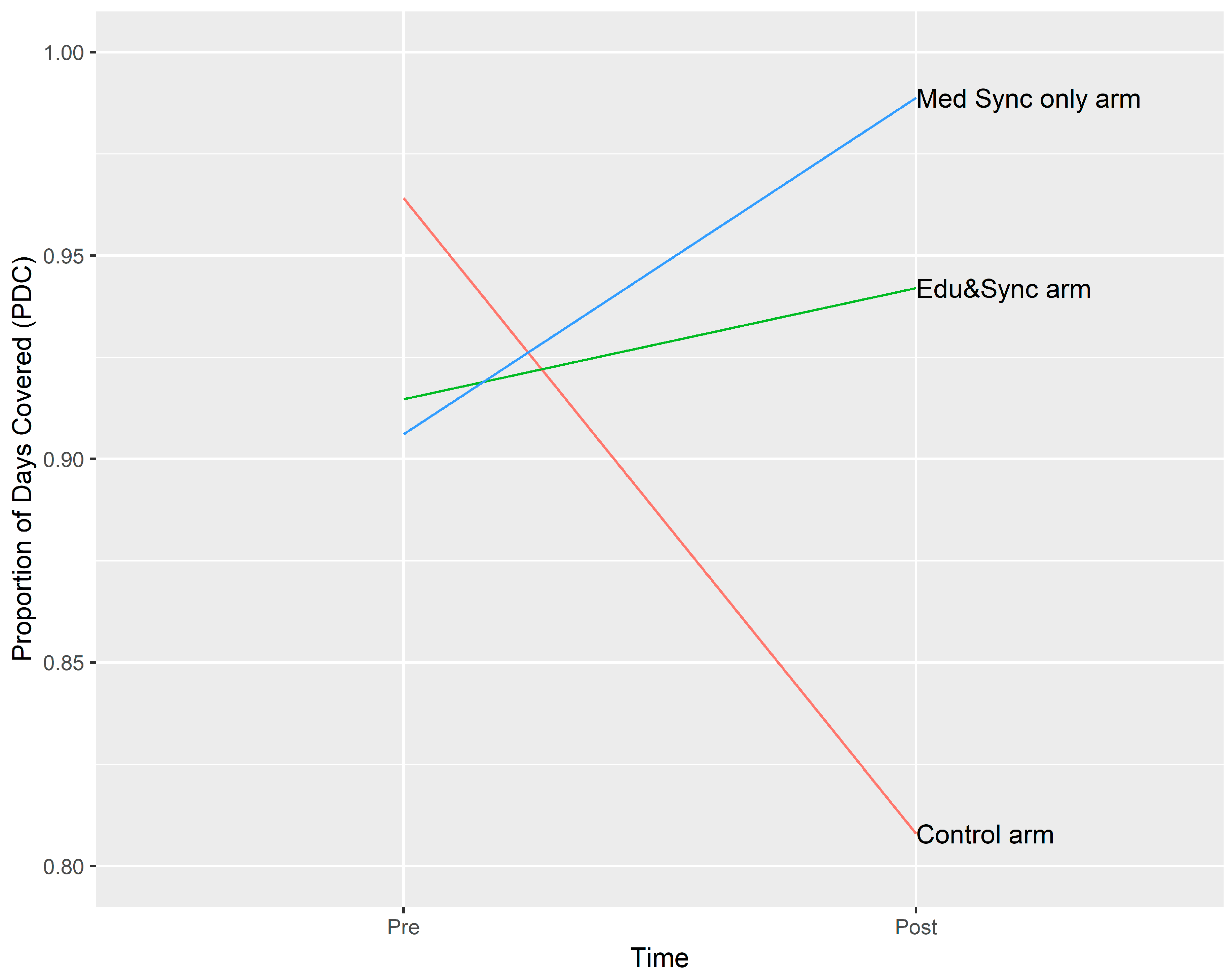
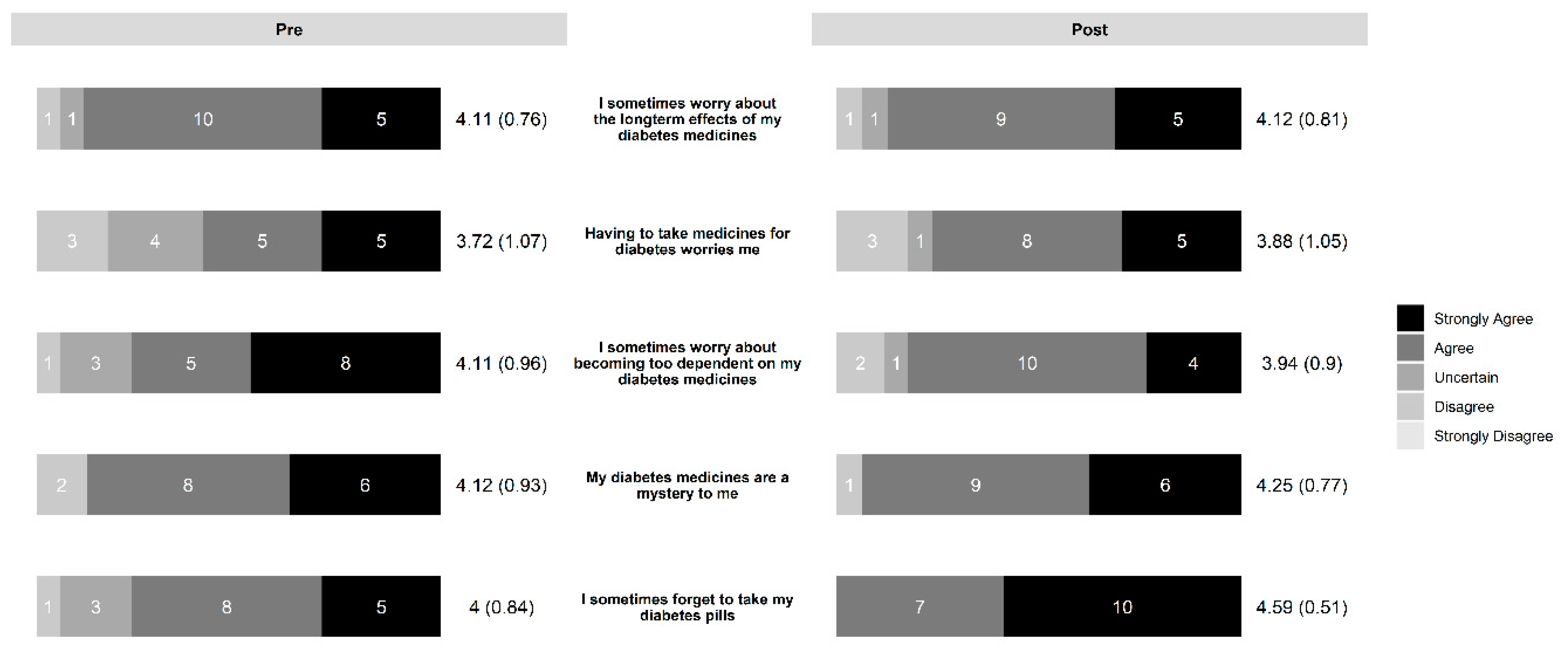
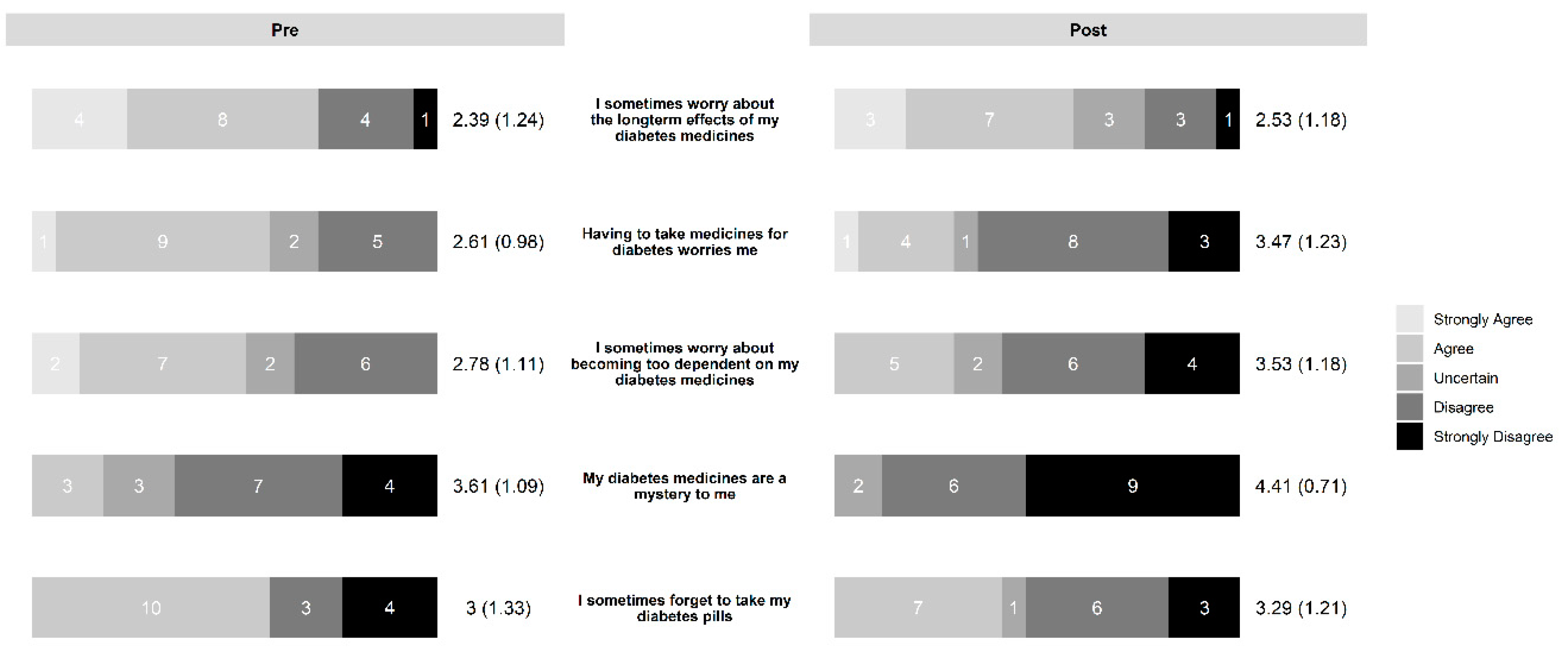
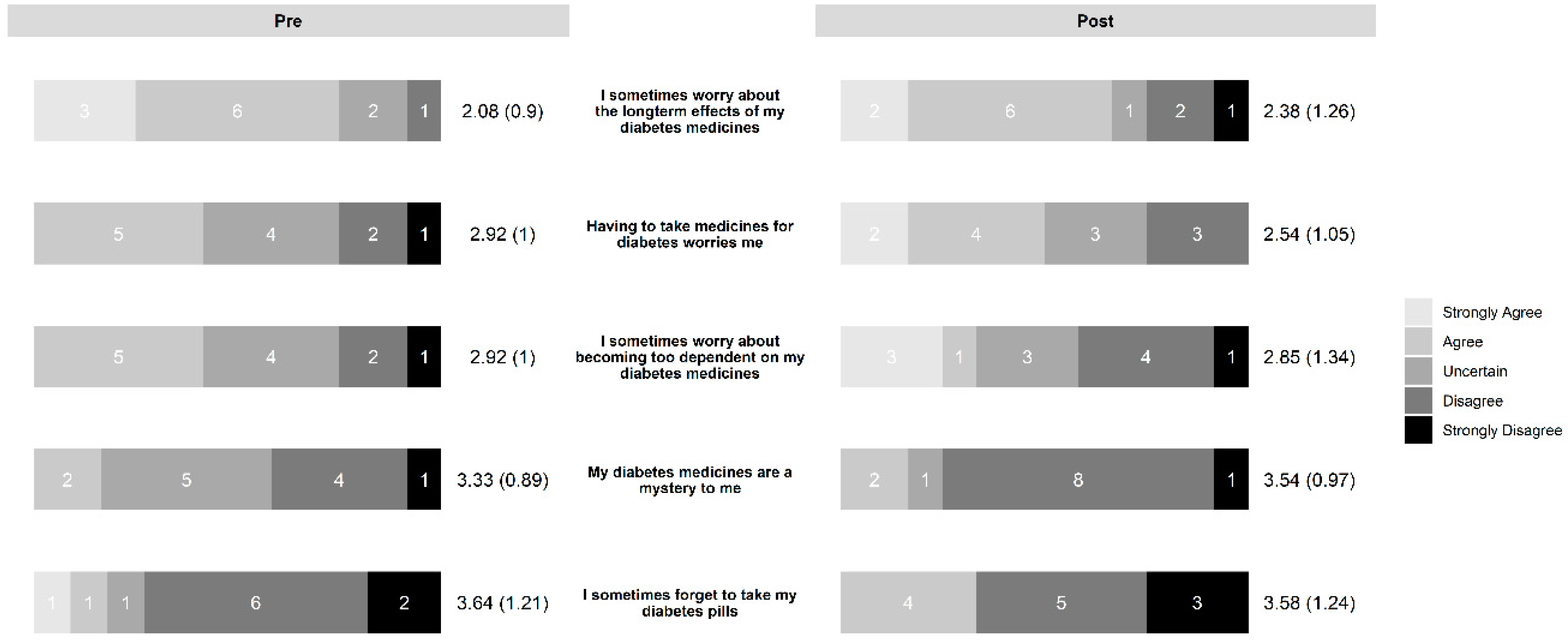
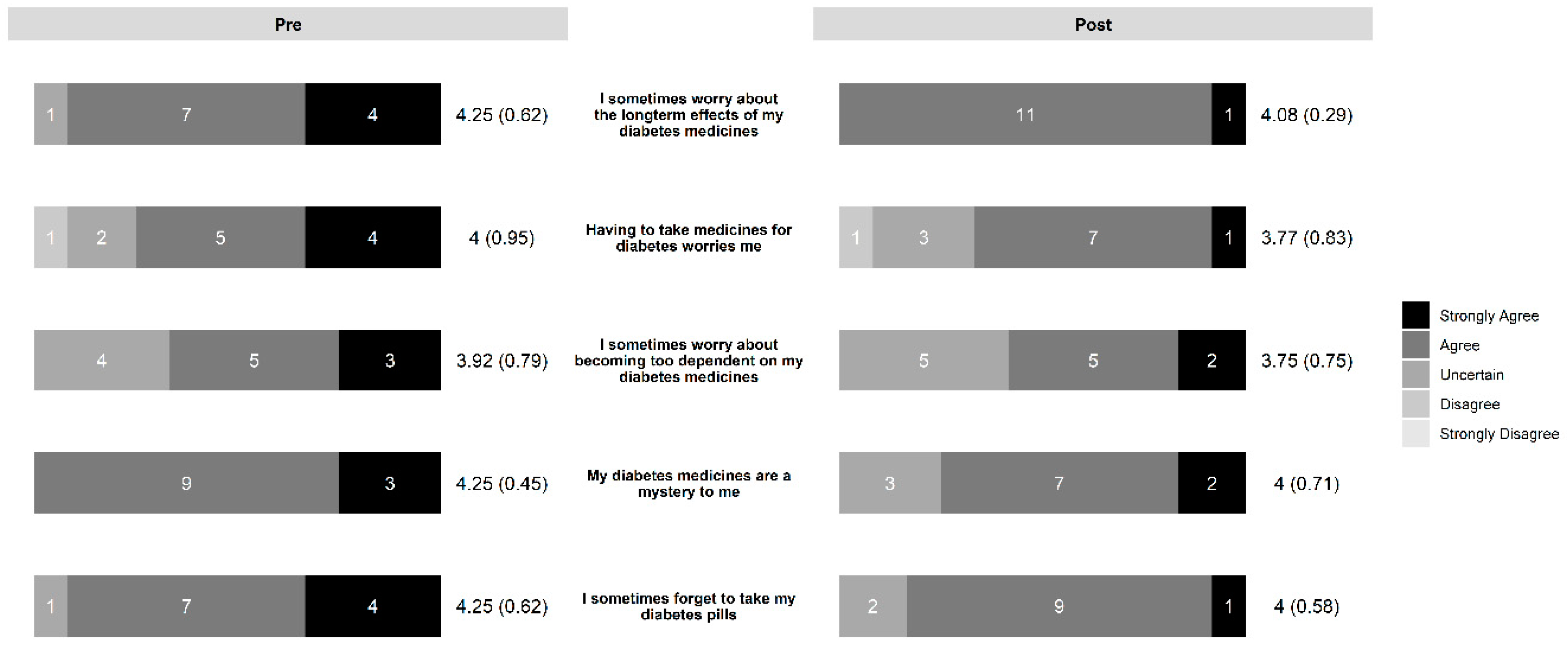
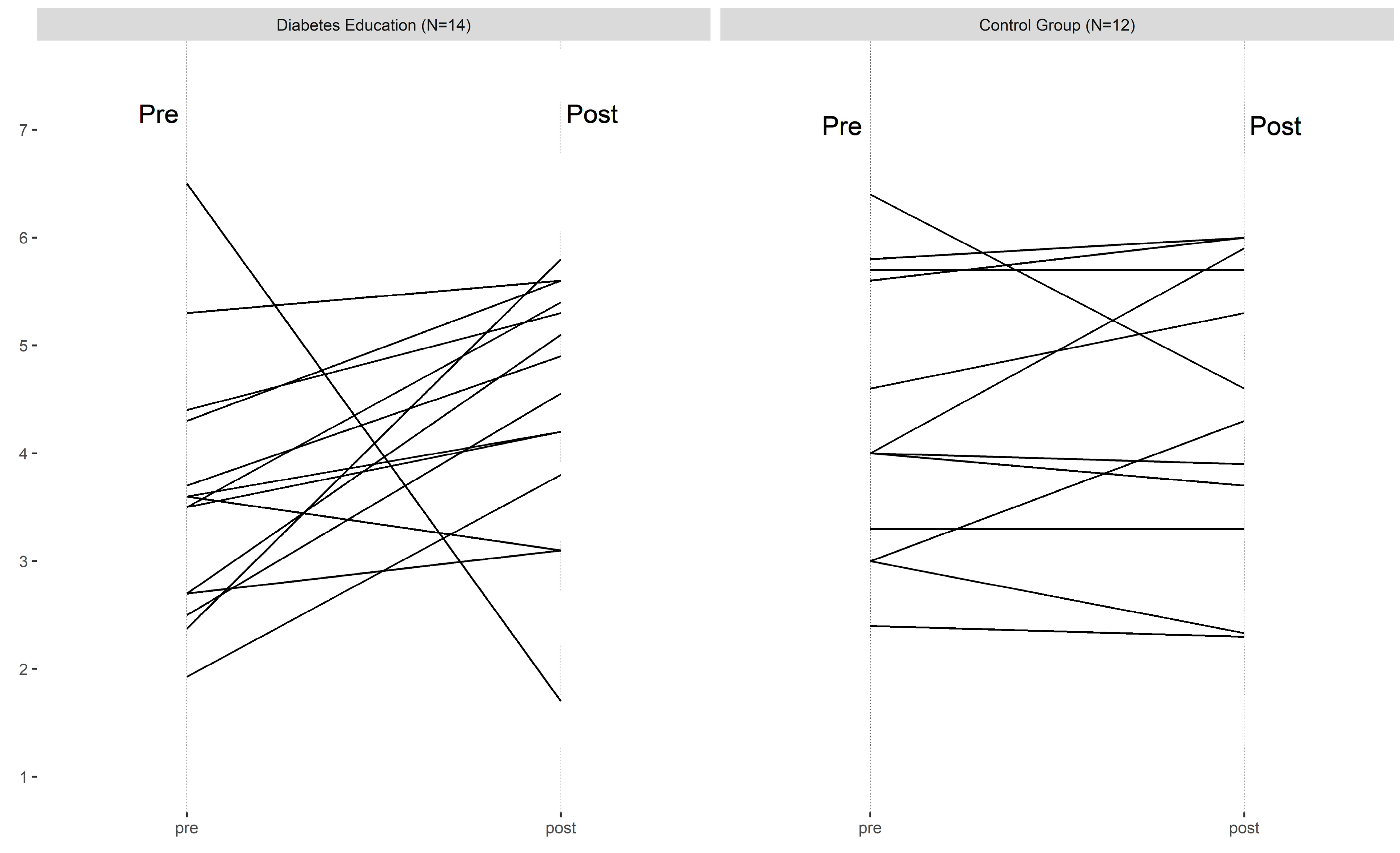
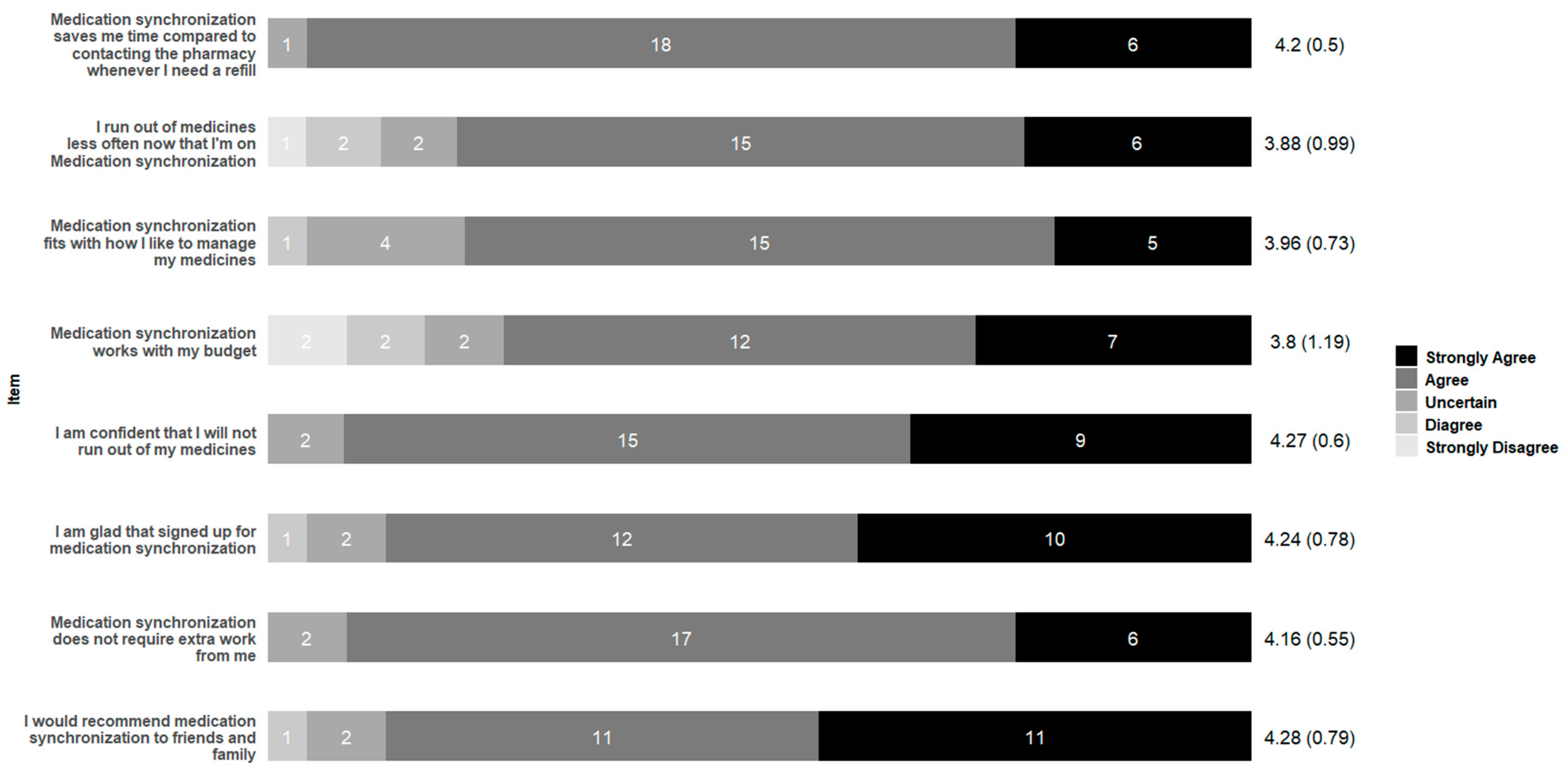
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| On How Many Days of the Last SEVEN DAYS Did You | DE Pre | DE Post | Control Pre | Control Post |
|---|---|---|---|---|
| Did you follow a healthy eating plan? | 3.69 (1.49) | 4.29 (1.59) | 4.08 (2.02) | 4.33 (1.3) |
| Did you eat five or more servings of fruits and vegetable? | 2.54 (1.81) | 4.07 (2.09) | 3.00 (1.86) | 3.83 (2.29) |
| Did you eat high fat foods such as red meat or full fat dairy products? | 3.00 (1.58) | 3 (1.8) | 3.50 (1.31) | 3.58 (1.78) |
| Did you do at least 30 min of physical activity? | 4.31 (2.39) | 4.79 (1.89) | 4.58 (2.43) | 4.33 (2.19) |
| Did you do specific exercise (such as swimming, walking, biking) other than what you do around the house or as part of your job? | 3.18 (2.32) | 3.86 (2.03) | 4.00 (2.63) | 3.92 (2.35) |
| Did you test your blood sugar? | 3.86 (2.8) | 4.86 (2.71) | 4.83 (2.41) | 5.33 (2.35) |
| Did you test your blood sugar the number of times recommended by your doctor? | 3.00 (2.72) | 4.46 (2.54) | 3.25 (3.11) | 5.42 (2.27) |
| Did you check your feet for sore? | 4.69 (2.84) | 4.93 (2.79) | 5.33 (2.42) | 3.83 (3.13) |
| Did you inspect the inside of your shoes before you put them on? | 2.77 (2.89) | 4.14 (3.06) | 3.67 (3.28) | 3.09 (3.33) |
| Did you take your diabetes medicines as recommended? | 6.07 (1.98) | 6.14 (1.66) | 6.92 (0.29) | 6.83 (0.58) |
References
- Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2017; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2017. [Google Scholar]
- American Diabetes Association. Economic Costs of Diabetes in the US in 2017. Diabetes Care 2018, 41, 917–928. [Google Scholar] [CrossRef] [PubMed]
- Dall, T.M.; Mann, S.E.; Zhang, Y.; Quick, W.W.; Seifert, R.F.; Martin, J.; Huang, E.A.; Zhang, S. Distinguishing the economic costs associated with type 1 and type 2 diabetes. Popul. Health Manag. 2009, 12, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Rhee, M.K.; Slocum, W.; Ziemer, D.C.; Culler, S.D.; Cook, C.B.; El-Kebbi, I.M.; Gallina, D.L.; Barnes, C.; Phillips, L.S. Patient adherence improves glycemic control. Diabetes Educ. 2005, 31, 240–250. [Google Scholar] [CrossRef]
- Ho, P.M.; Rumsfeld, J.S.; Masoudi, F.A.; McClure, D.L.; Plomondon, M.E.; Steiner, J.F.; Magid, D.J. Effect of medication nonadherence on hospitalization and mortality among patients with diabetes mellitus. Arch. Intern. Med. 2006, 166, 1836–1841. [Google Scholar] [CrossRef]
- Khairnar, R.; Kamal, K.M.; Giannetti, V.; Dwibedi, N.; McConaha, J. Barriers and facilitators to diabetes self-management in a primary care setting—Patient perspectives. Res. Soc. Adm. Pharm. 2019, 15, 279–286. [Google Scholar] [CrossRef] [PubMed]
- Sapkota, S.; Brien, J.-A.; Greenfield, J.; Aslani, P. A systematic review of interventions addressing adherence to anti-diabetic medications in patients with type 2 diabetes—Impact on adherence. PLoS ONE 2015, 10, e0118296. [Google Scholar] [CrossRef]
- Choi, Y.J.; Smaldone, A.M. Factors Associated with Medication Engagement Among Older Adults with Diabetes: Systematic Review and Meta-Analysis. Diabetes Educ. 2018, 44, 15–30. [Google Scholar] [CrossRef] [PubMed]
- Vluggen, S.; Hoving, C.; Schaper, N.; de Vries, H. Exploring beliefs on diabetes treatment adherence among Dutch type 2 diabetes patients and healthcare providers. Patient Educ. Couns. 2018, 101, 92–98. [Google Scholar] [CrossRef]
- Huang, Y.-M.; Shiyanbola, O.O.; Chan, H.-Y. A path model linking health literacy, medication self-efficacy, medication adherence, and glycemic control. Patient Educ. Couns. 2018, 101, 1906–1913. [Google Scholar] [CrossRef]
- Alatawi, Y.M.; Kavookjian, J.; Ekong, G.; Alrayees, M.M. The association between health beliefs and medication adherence among patients with type 2 diabetes. Res. Soc. Adm. Pharm. 2016, 12, 914–925. [Google Scholar] [CrossRef]
- Brundisini, F.; Vanstone, M.; Hulan, D.; DeJean, D.; Giacomini, M. Type 2 diabetes patients’ and providers’ differing perspectives on medication nonadherence: A qualitative meta-synthesis. BMC Health Serv. Res. 2015, 15, 516. [Google Scholar] [CrossRef] [PubMed]
- Jaam, M.; Awaisu, A.; Mohamed Ibrahim, M.I.; Kheir, N. A holistic conceptual framework model to describe medication adherence in and guide interventions in diabetes mellitus. Res. Soc. Adm. Pharm. 2018, 14, 391–397. [Google Scholar] [CrossRef]
- Haynes, R.B.; Ackloo, E.; Sahota, N.; McDonald, H.P.; Yao, X. Interventions for enhancing medication adherence. Cochrane Database Syst. Rev. 2008, 2, CD000011. [Google Scholar] [CrossRef] [PubMed]
- Presley, B.; Groot, W.; Pavlova, M. Pharmacy-led interventions to improve medication adherence among adults with diabetes: A systematic review and meta-analysis. Res. Soc. Adm. Pharm. 2018. [Google Scholar] [CrossRef] [PubMed]
- Kini, V.; Ho, P.M. Interventions to improve medication adherence: A review. JAMA 2018, 320, 2461–2473. [Google Scholar] [CrossRef] [PubMed]
- Kent, D.; D’Eramo Melkus, G.; Stuart, P.M.W.; McKoy, J.M.; Urbanski, P.; Boren, S.A.; Coke, L.; Winters, J.E.; Horsley, N.L.; Sherr, D. Reducing the risks of diabetes complications through diabetes self-management education and support. Popul. Health Manag. 2013, 16, 74–81. [Google Scholar] [CrossRef] [PubMed]
- Norris, S.L.; Lau, J.; Smith, S.J.; Schmid, C.H.; Engelgau, M.M. Self-management education for adults with type 2 diabetes: A meta-analysis of the effect on glycemic control. Diabetes Care 2002, 25, 1159–1171. [Google Scholar] [CrossRef] [PubMed]
- Chrvala, C.A.; Sherr, D.; Lipman, R.D. Diabetes self-management education for adults with type 2 diabetes mellitus: A systematic review of the effect on glycemic control. Patient Educ. Couns. 2016, 99, 926–943. [Google Scholar] [CrossRef]
- Gary, T.L.; Genkinger, J.M.; Guallar, E.; Peyrot, M.; Brancati, F.L. Meta-Analysis of Randomized Educational and Behavioral Interventions in Type 2 Diabetes. Diabetes Educ. 2003, 29, 488–501. [Google Scholar] [CrossRef]
- Ragucci, K.R.; Fermo, J.D.; Wessell, A.M.; Chumney, E.C. Effectiveness of pharmacist-administered diabetes mellitus education and management services. Pharmacotherapy 2005, 25, 1809–1816. [Google Scholar] [CrossRef]
- Gonzalvo, J.D.; Kruckeberg, E.; Newton, M.L.; Chang, E.; Olenik, N.L.; Gernant, S.A. Advanced diabetes credentials for the community pharmacist: A pilot study. J. Am. Pharm. Assoc. 2016, 56, 274–279. [Google Scholar] [CrossRef] [PubMed]
- Olenik, N.L.; Fletcher, L.M.; Gonzalvo, J.D. The community pharmacist as diabetes educator. AADE Pract. 2015, 3, 46–50. [Google Scholar] [CrossRef]
- Goedken, A.M.; Butler, C.M.; McDonough, R.P.; Deninger, M.J.; Doucette, W.R. Continuous Medication Monitoring (CoMM): A foundational model to support the clinical work community pharmacists. Res. Social Adm. Pharm. 2017, 14, 106–111. [Google Scholar] [CrossRef] [PubMed]
- Witry, M.J.; Doucette, W.R. Community pharmacists, medication monitoring, and the routine nature of refills: A qualitative study. J. Am. Pharm. Assoc. 2014, 54, 594–603. [Google Scholar] [CrossRef] [PubMed]
- Witry, M. Any Questions? Yes, do pharmacists monitor medications at refill? J. Am. Pharm. Assoc. 2017, 57, 591–595. [Google Scholar] [CrossRef] [PubMed]
- Pousinho, S.; Morgado, M.; Falcão, A.; Alves, G. Pharmacist interventions in the management of type 2 diabetes mellitus: A systematic review of randomized controlled trials. J. Manag. Care Spec. Pharm. 2016, 22, 493–515. [Google Scholar] [CrossRef] [PubMed]
- Krumme, A.A.; Isaman, D.L.; Stolpe, S.F.; Dougherty, S.; Choudhry, N.K. Prevalence, effectiveness, and characteristics of pharmacy-based medication synchronization programs. Am. J. Manag. Care 2016, 22, 179–186. [Google Scholar] [PubMed]
- Renfro, C.P.; Patti, M.; Ballou, J.M.; Ferreri, S.P. Development of a medication synchronization common language for community pharmacies. J. Am. Pharm. Assoc. 2018, 58, 515–521. [Google Scholar] [CrossRef]
- Watson, L.L.; Bluml, B.M. Pharmacy’s Appointment-Based Model: Implementation Guide for Pharmacy Practices; APhA Foundation: Washington, DC, USA, 2013. [Google Scholar]
- Krumme, A.A.; Glynn, R.J.; Schneeweiss, S.; Gagne, J.J.; Dougherty, J.S.; Brill, G.; Choudhry, N.K. Medication Synchronization Programs Improve Adherence to Cardiovascular Medications and Health Care Use. Health Aff. (Millwood) 2018, 37, 125–133. [Google Scholar] [CrossRef]
- Girdish, C.; Shrank, W.; Freytag, S.; Chen, D.; Gebhard, D.; Bunton, A.; Choudhry, N.; Polinski, J. The impact of a retail prescription synchronization program on medication adherence. J. Am. Pharm. Assoc. 2017, 57, 579–584. [Google Scholar] [CrossRef]
- Witry, M.; Hoang, T. Community Pharmacist Attitudes on Medication Synchronization Programs. Inov. Pharm. 2017, 8. [Google Scholar] [CrossRef]
- Butler, K.T.; Ruisinger, J.F.; Bates, J.; Prohaska, E.S.; Melton, B.L. Participant satisfaction with a community-based medication synchronization program. J. Am. Pharm. Assoc. 2015, 55, 534–539. [Google Scholar] [CrossRef] [PubMed]
- Horne, R.; Weinman, J.; Hankins, M. The beliefs about medicines questionnaire: The development and evaluation of a new method for assessing the cognitive representation of medication. Psychol. Health 1999, 14, 1–24. [Google Scholar] [CrossRef]
- Toobert, D.J.; Hampson, S.E.; Glasgow, R.E. The summary of diabetes self-care activities measure: Results from 7 studies and a revised scale. Diabetes Care 2000, 23, 943–950. [Google Scholar] [CrossRef] [PubMed]
- Schommer, J.C.; Kucukarslan, S.N. Measuring patient satisfaction with pharmaceutical services. Am. J. Health Syst. Pharm. 1997, 54, 2721–2732. [Google Scholar] [PubMed]
- Tickle-Degnen, L. Nuts and bolts of conducting feasibility studies. Am. J. Occup. Ther. 2013, 67, 171–176. [Google Scholar] [CrossRef]
- Mansell, K.; Perepelkin, J. Patient awareness of specialized diabetes services provided in community pharmacies. Res. Soc. Adm. Pharm. 2011, 7, 396–405. [Google Scholar] [CrossRef]
- Holdford, D.A.; Saxena, K. Impact of appointment-based Medication Synchronization on existing users of Chronic Medications. Value Health 2015, 18, A260. [Google Scholar] [CrossRef]
- Machado, M.; Bajcar, J.; Guzzo, G.C.; Einarson, T.R. Sensitivity of patient outcomes to pharmacist interventions. Part I: Systematic review and meta-analysis in diabetes management. Ann. Pharm. 2007, 41, 1569–1582. [Google Scholar] [CrossRef]
- Stanton-Robinson, C.; Al-Jumaili, A.A.; Jackson, A.; Catney, C.; Veach, S.; Witry, M.J. Evaluation of Community Pharmacist-Provided Telephone Interventions to Improve Adherence to Hypertension and Diabetes Medications. J. Am. Pharm. Assoc. 2018, 58, 120–124. [Google Scholar] [CrossRef]
- Singleton, J.; Veach, S.; Catney, C.; Witry, M. Analysis of a Community Pharmacy Intervention to Improve Low Adherence Rates to Oral Diabetes Medications. Pharmacy 2017, 5, 58. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Bae, Y.; Worley, M.; Law, A. Validating the modified drug adherence Work-Up (M-DRAW) Tool to identify and address barriers to medication adherence. Pharmacy 2017, 5, 52. [Google Scholar] [CrossRef] [PubMed]
- Colvin, N.N.; Mospan, C.M.; Buxton, J.A.; Gillette, C. Using Indian Health Service (IHS) counseling techniques in an independent community pharmacy to improve adherence rates among patients with diabetes, hypertension, or hyperlipidemia. J. Am. Pharm. Assoc. 2018, 58, 59–63. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg-Yunger, Z.R.; Verweel, L.; Gionfriddo, M.R.; MacCallum, L.; Dolovich, L. Community pharmacists’ perspectives on shared decision-making in diabetes management. Int. J. Pharm. Pract. 2018, 26, 414–422. [Google Scholar] [CrossRef] [PubMed]
- Twigg, M.J.; Poland, F.; Bhattacharya, D.; Desborough, J.A.; Wright, D.J. The current and future roles of community pharmacists: Views and experiences of patients with type 2 diabetes. Res. Soc. Adm. Pharm. 2013, 9, 777–789. [Google Scholar] [CrossRef] [PubMed]
- Machen, M.L.; Borden, H.C.; Hohmeier, K.C. The Impact of a Community Pharmacy Diabetes Self-Management Education Program on Diabetes Distress. J. Pharm. Technol. 2019, 35, 3–10. [Google Scholar] [CrossRef]
- Ernzen, M.; Pape, A.; Witry, M. Experience of an Iowa community pharmacist in seeking reimbursement for group diabetes education. J. Iowa Pharm. Assoc. 2019, 24–27. [Google Scholar] [CrossRef]
| Characteristic | Education and Medication Synchronization Arm | Medication Synchronization Service Only Arm | Control Arm |
|---|---|---|---|
| Gender | |||
| Male | 7 (38.89%) | 6 (40%) | 5 (38.5%) |
| Female | 11 (61%) | 7 (46.6%) | 8 (61.5%) |
| Age | |||
| 18–29 | 1 (5.5%) | ||
| 30–39 | 2 (11.1%) | 1 (6.6%) | |
| 40–49 | 3 (16.6%) | 1 (7.6%) | |
| 50–59 | 6 (33.3%) | 4 (26.6%) | 3 (23%) |
| 60–69 | 5 (27.7%) | 8 (53.3%) | 7 (53.8%) |
| 70 or older | 1 (5.5%) | 2 (13.3%) | 2 (15.3%) |
| Education | |||
| Grade school | 1 (5.5%) | 2 (13.3%) | 1 (7.6%) |
| High school | 7 (38.8%) | 6 (40%) | 5 (38.4%) |
| Technical/2-yr | 3 (16.6%) | 3 (20%) | 2 (15.3%) |
| Some college | 2 (11.1%) | 4 (30.7%) | |
| College Graduate | 2 (11.1%) | 4 (26.6%) | |
| Advanced degree | 1 (5.5%) | 1 (7.6%) | |
| Insurance | |||
| None | 1 (6.6%) | ||
| Medicaid | 4 (22.2%) | 9 (60%) | 6 (46.15%) |
| Medicare | 6 (33.3%) | 5 (33.3%) | 4 (30.77%) |
| Plan through work | 7 (38.8%) | 2 (13.3%) | 2 (15.4%) |
| Individual plan | 3 (16.6%) | 5 (33.3%) | 2 (15.4%) |
| Currently live with? | |||
| No one | 5 (27.78%) | 6 (40%) | 4 (30%) |
| Spouse or Partner | 9 (50%) | 7 (46.6%) | 6 (46.1%) |
| Dependent Children | 1 (5.56%) | 2 (15.3%) | |
| Adult Children | 1 (5.56%) | 2 (15.3%) | |
| Friend or Room mate | 2 (11.11%) | 1 (6.6%) | 1 (7.7%) |
| Altogether, how many prescription medicines do you take every day? (Not just for diabetes) (mean (SD)) | 8.07 (2.81) | 7.33 (3.37) | 9.00 (4.44) |
| How would you rate your overall health? a (mean (SD)) | 2.86 (0.68) | 2.67 (0.72) | 3.00 (0.71) |
| How often do you need to have someone help you when you read instructions, pamphlets, or other written materials from your doctor of pharmacy? b (mean (SD)) | 3.88 (1.52) | 3.6 (1.35) | 4.38 (0.96) |
| Do you use an insulin injection? | |||
| Yes | 5 (27.7%) | 5 (33.3%) | 6 (46.1%) |
| No | 13 (72.3%) | 10 (66.6%) | 7 (53.9%) |
| How long have you had your Type 2 diabetes? (Years) (mean (SD)) | 6.62 (5.20) | 7.47 (5.84) | 8.08 (6.62) |
| Item | Agreement Mean (SD) |
|---|---|
| The time for the diabetes education classes was convenient. | 4.38 (0.51) |
| Traveling to the diabetes education classes was easy. | 4.38 (0.51) |
| The pharmacist talked in a way that was easy to understand. | 4.77 (0.44) |
| Talking to other people with diabetes was helpful. | 4.54 (0.66) |
| The pharmacist was good about answering my questions. | 4.69 (0.48) |
| The pharmacist made good suggestions about how to eat healthier. | 4.69 (0.48) |
| The pharmacist made good suggestions about how to fit exercise into my day. | 4.46 (0.52) |
| I am delighted with the diabetes education classes. | 4.69 (0.48) |
| I am glad that I signed up to take these diabetes education classes. | 4.69 (0.48) |
| Coming to the diabetes education classes was worth my time. | 4.62 (0.51) |
| What I got from the diabetes education classes was worth me showing up. | 4.54 (0.52) |
| I am more confident that l can manage my diabetes sense taking these classes. | 4.38 (0.65) |
| The quality of the diabetes education classes met my standards. | 4.54 (0.52) |
| The quality of the diabetes education classes exceeded my expectations. | 4.31 (0.85) |
| I am confident that I were have better control of my blood sugars because of these classes. | 4.38 (0.65) |
| I am confident that can keep up with my diabetes management long-term. | 4.31 (0.63) |
| The classes motivated me to stay in control of my diabetes. | 4.31 (0.95) |
| I would recommend group diabetes education from this pharmacy to my friends and family. | 4.77 (0.44) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Witry, M.; Ernzen, M.; Pape, A.; Viyyuri, B.R. Pilot and Feasibility of Combining a Medication Adherence Intervention and Group Diabetes Education for Patients with Type-2 Diabetes. Pharmacy 2019, 7, 76. https://doi.org/10.3390/pharmacy7030076
Witry M, Ernzen M, Pape A, Viyyuri BR. Pilot and Feasibility of Combining a Medication Adherence Intervention and Group Diabetes Education for Patients with Type-2 Diabetes. Pharmacy. 2019; 7(3):76. https://doi.org/10.3390/pharmacy7030076
Chicago/Turabian StyleWitry, Matthew, Melissa Ernzen, Anthony Pape, and Brahmendra Reddy Viyyuri. 2019. "Pilot and Feasibility of Combining a Medication Adherence Intervention and Group Diabetes Education for Patients with Type-2 Diabetes" Pharmacy 7, no. 3: 76. https://doi.org/10.3390/pharmacy7030076
APA StyleWitry, M., Ernzen, M., Pape, A., & Viyyuri, B. R. (2019). Pilot and Feasibility of Combining a Medication Adherence Intervention and Group Diabetes Education for Patients with Type-2 Diabetes. Pharmacy, 7(3), 76. https://doi.org/10.3390/pharmacy7030076





