Plasma Fibrinogen Independently Predicts Hypofibrinolysis in Severe COVID-19
Abstract
:1. Introduction
2. Results
2.1. Patients and Healthy Subjects
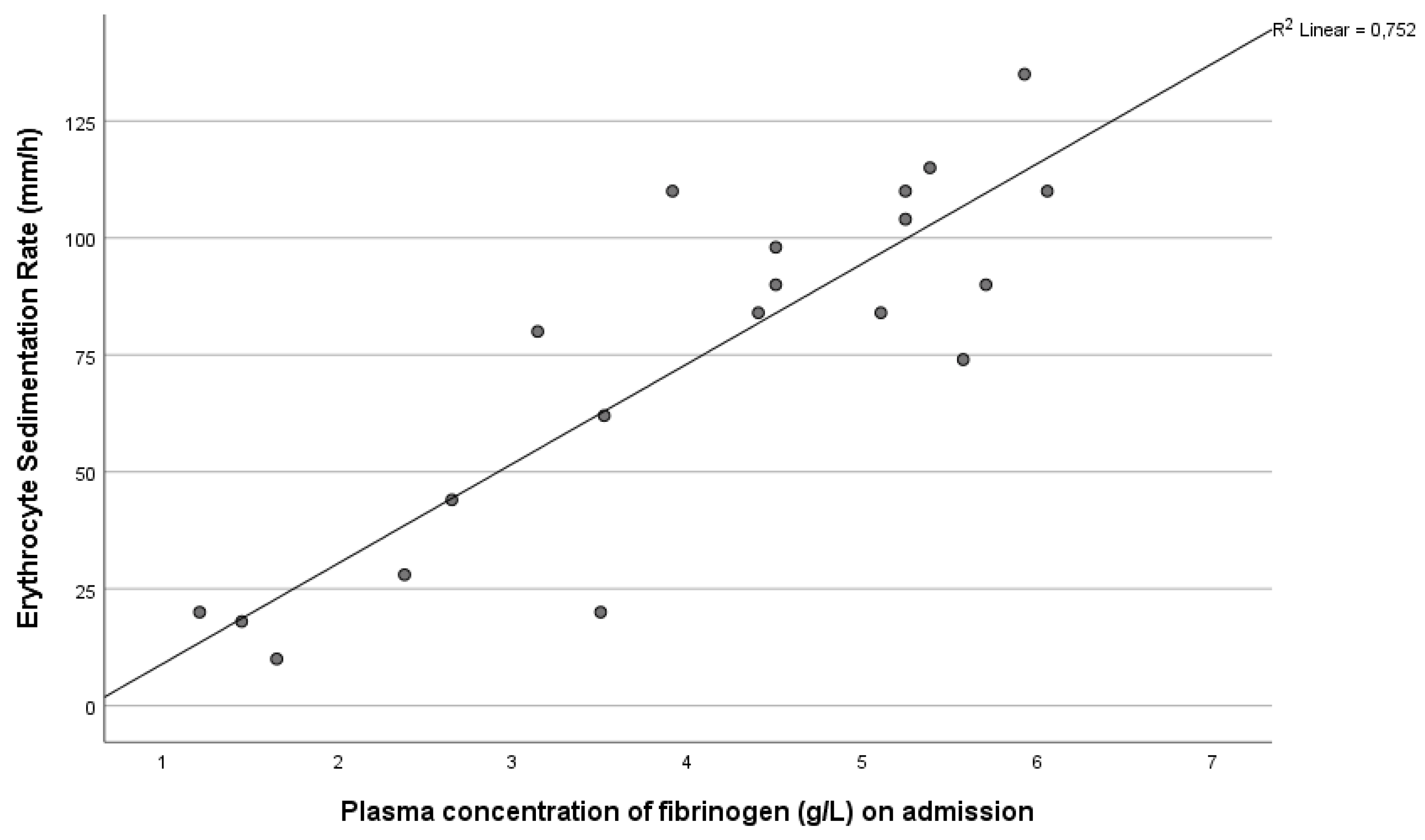
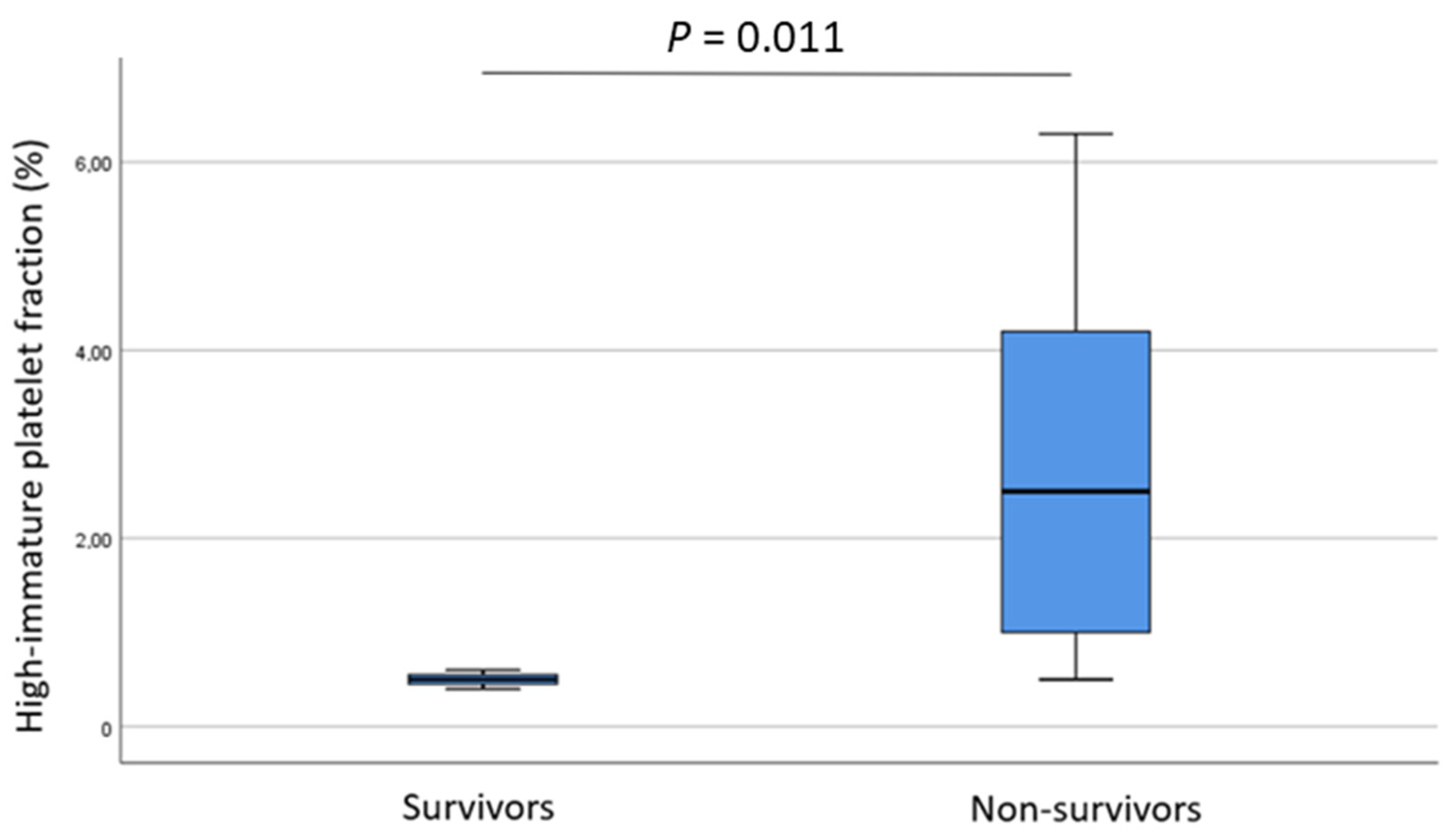
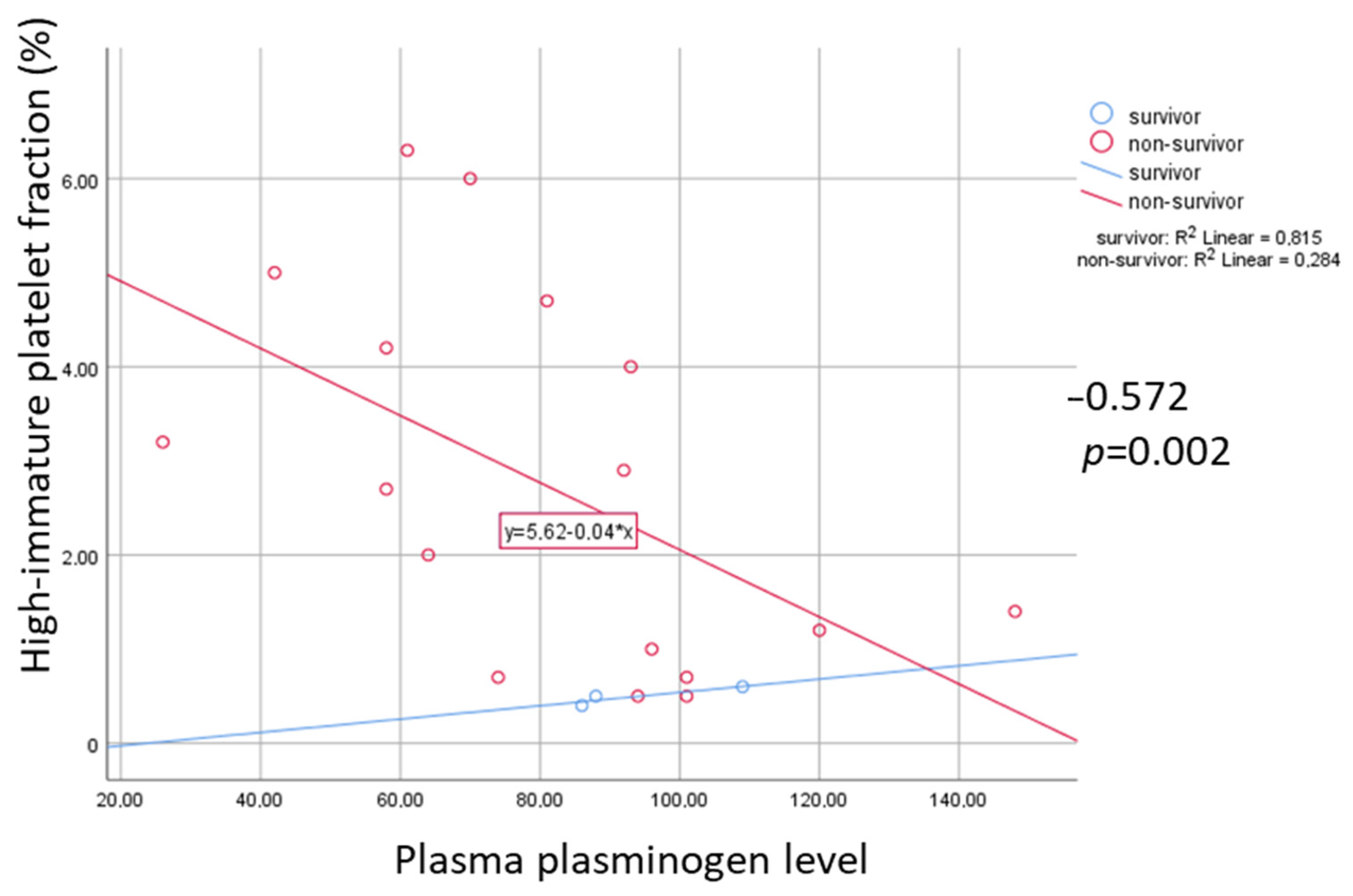
2.2. Non-Survivals vs. Survivals
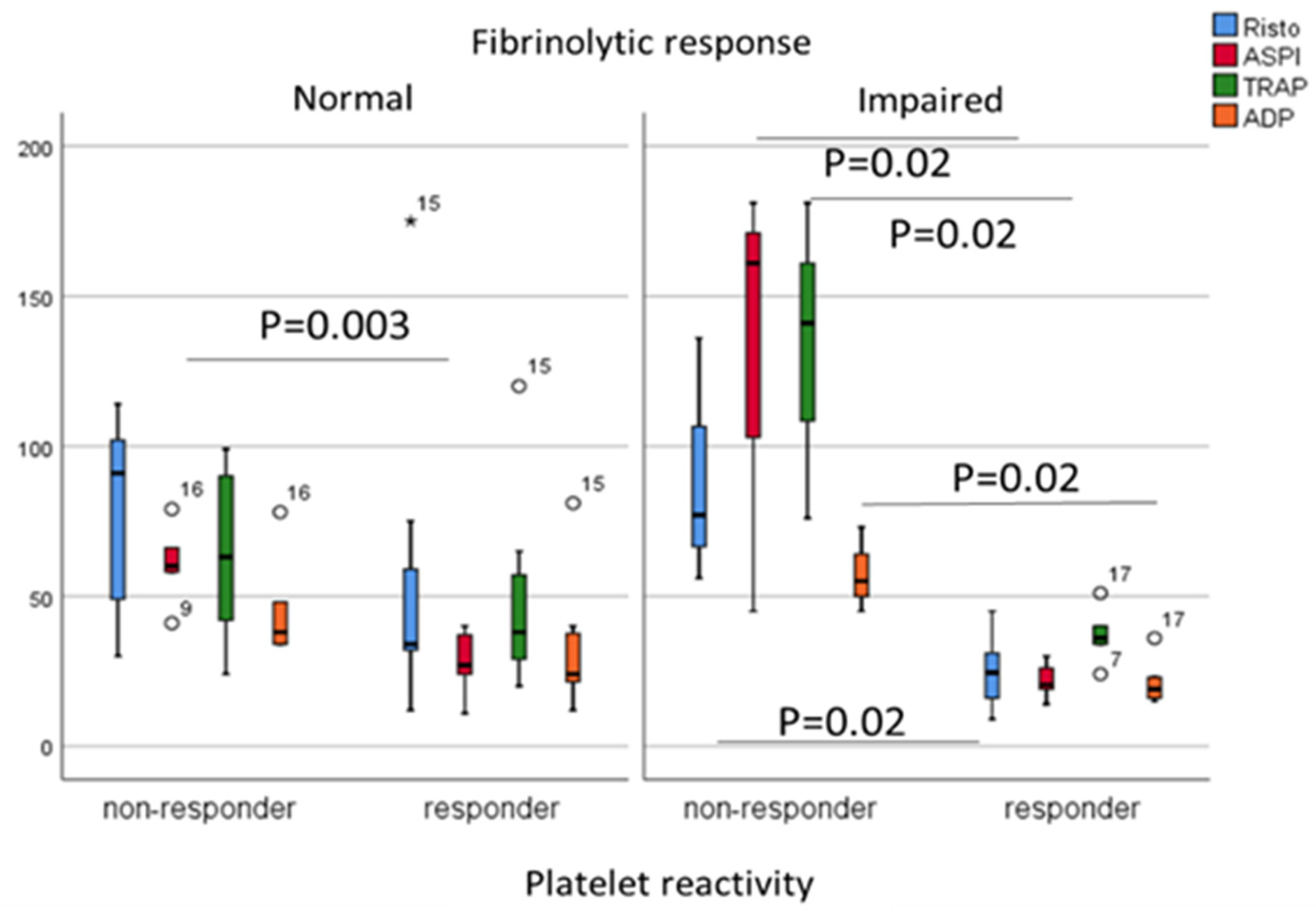
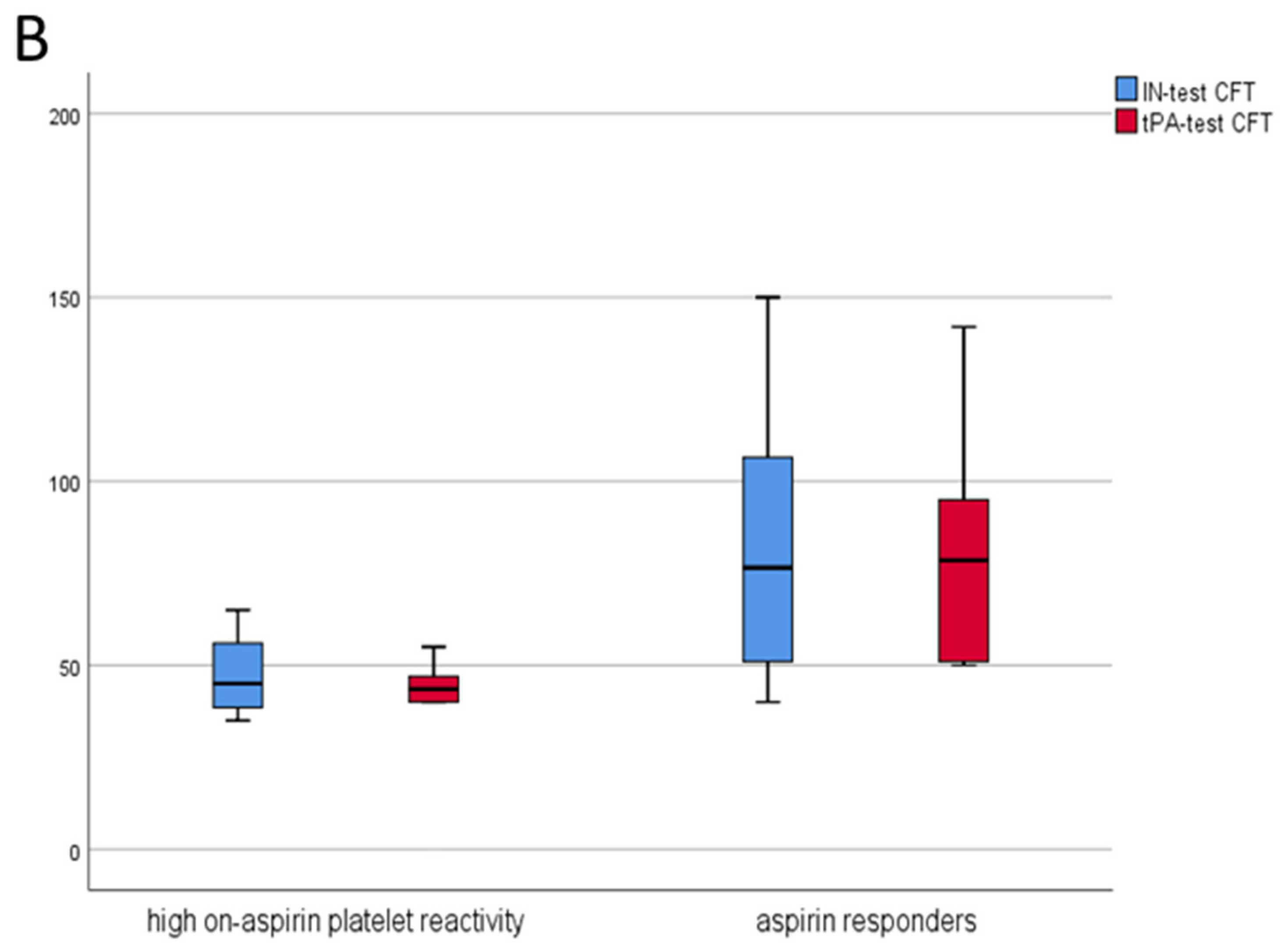
2.3. ‘Responders’ vs. ‘Non-Responders’
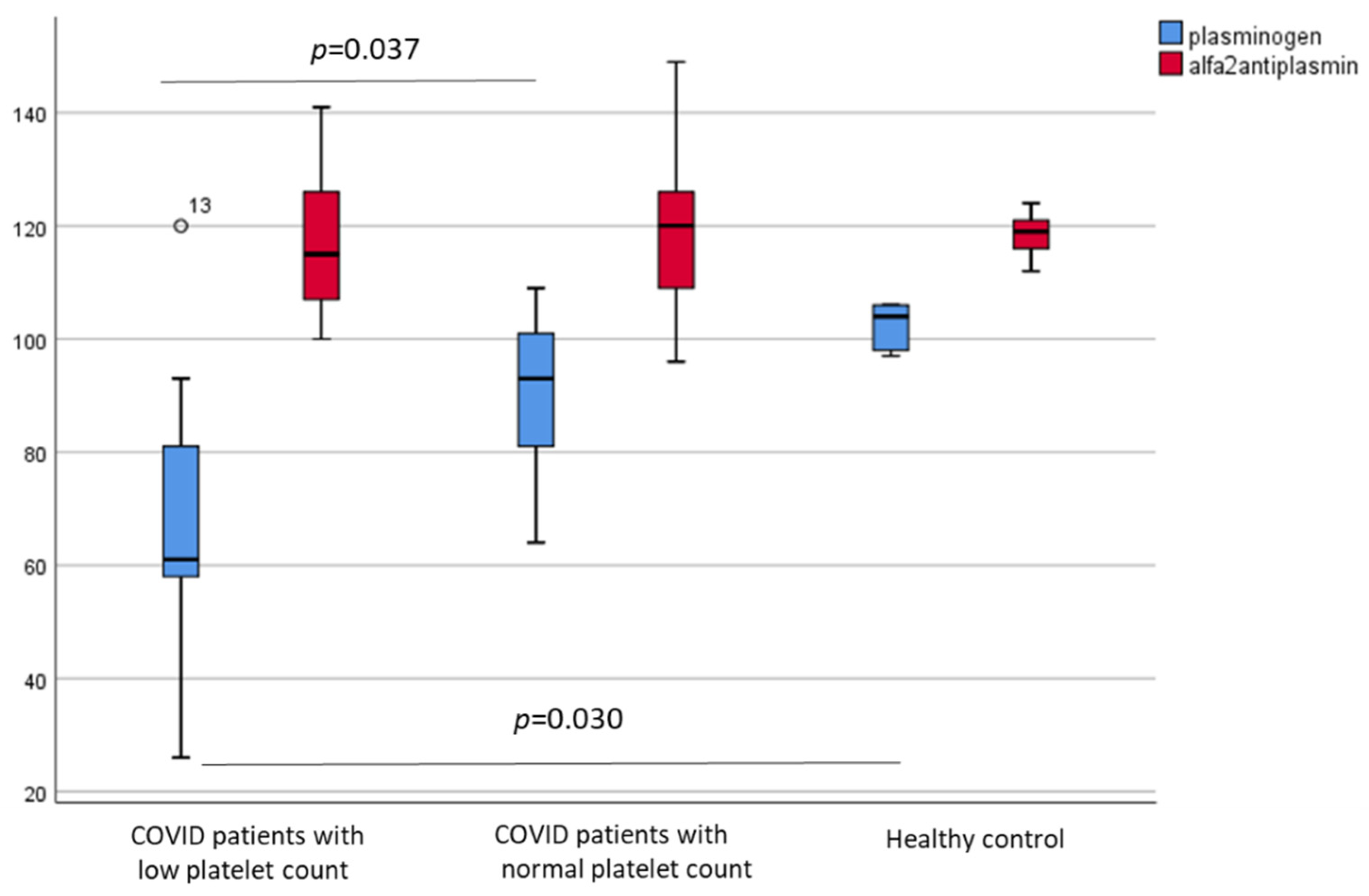
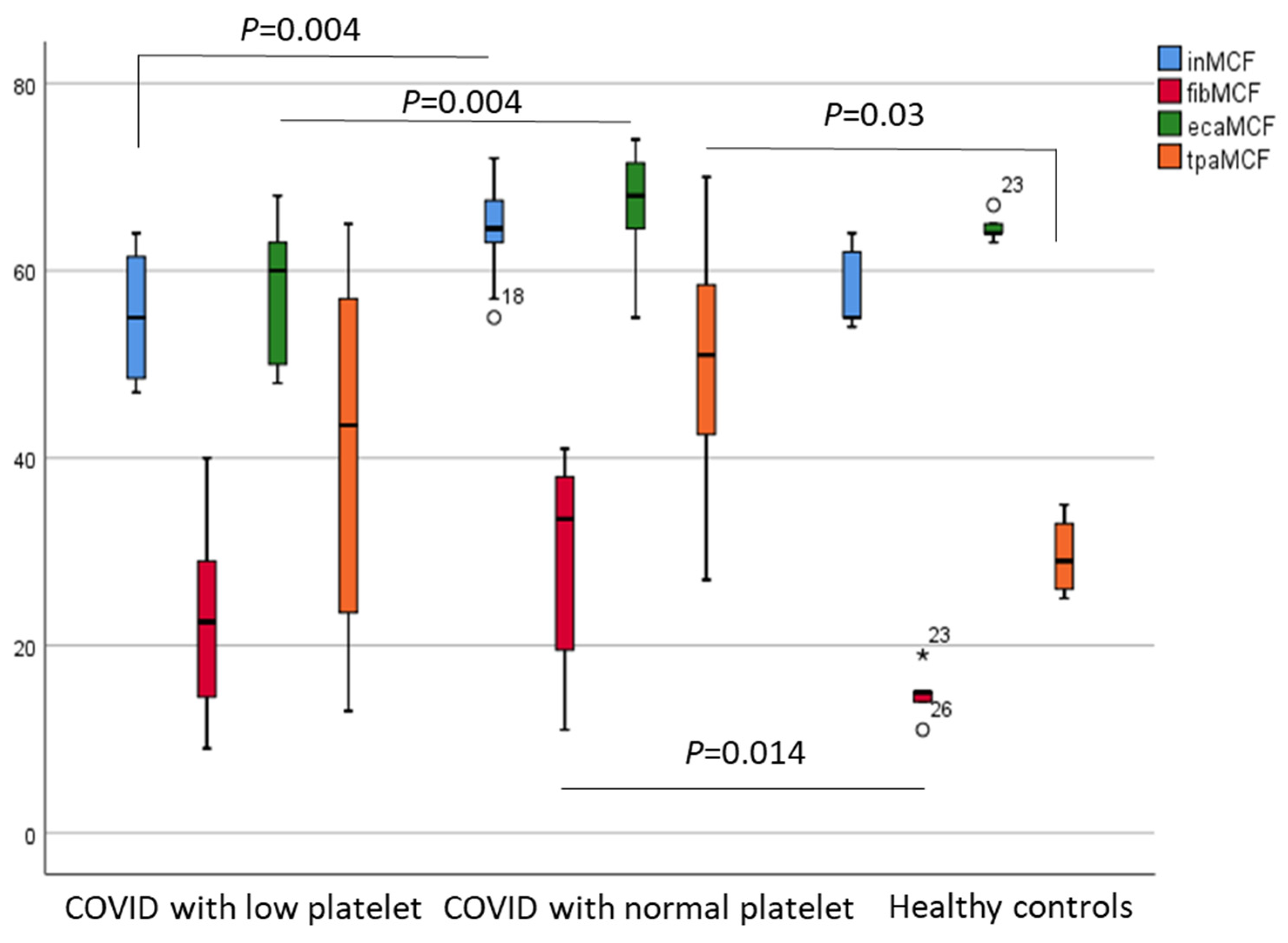
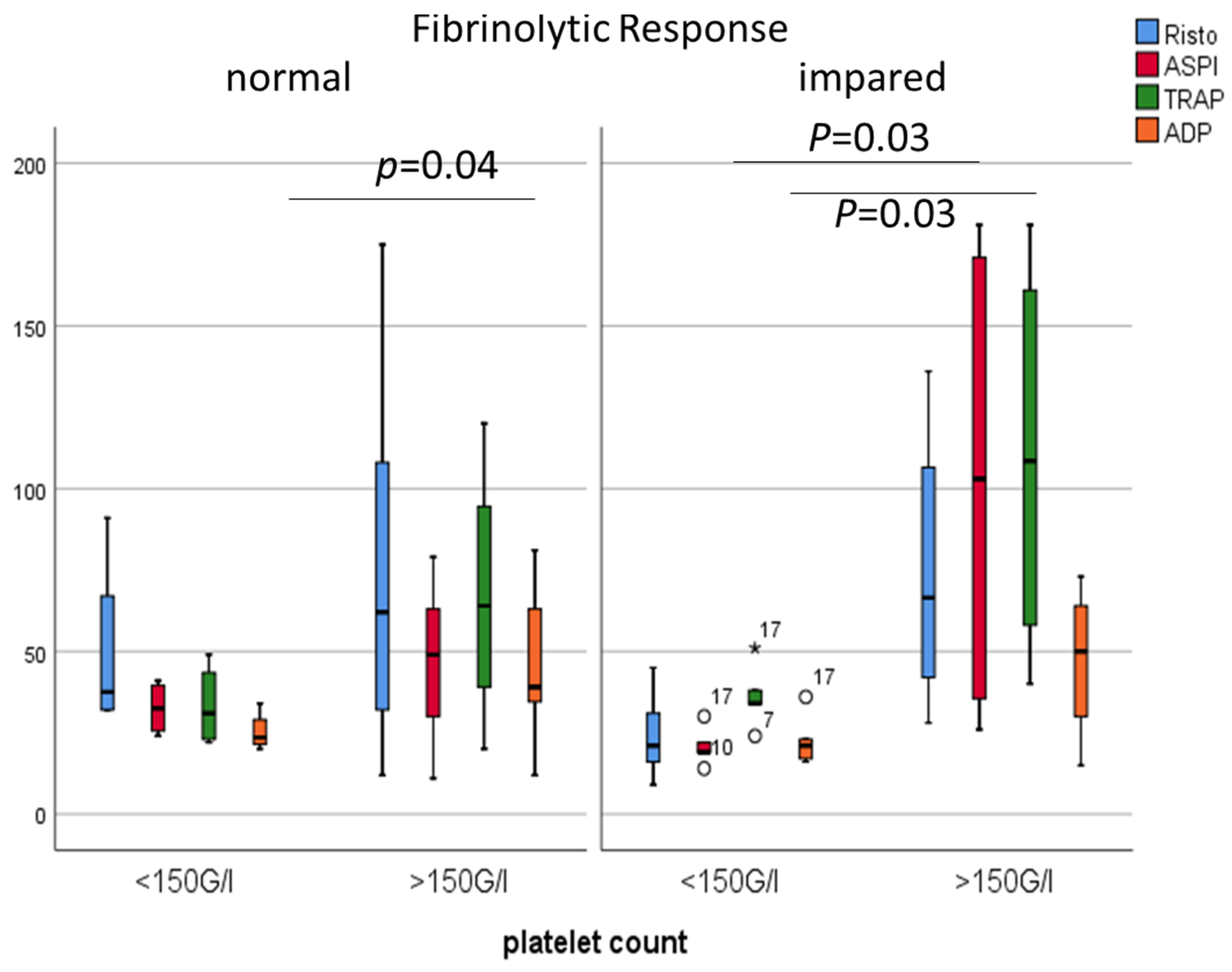
2.4. Admission Platelet Count in COVID-19 Patients
2.5. Independent Predictors of Ompaired Fibrinolytic Response
3. Discussion
4. Limitations
5. Methods
5.1. Blood Count, Platelet Count, High Immature Platelet Fraction (H-IPF) Measurement
5.2. The Erythrocyte Sedimentation Rate (ESR)
5.3. Hemostasis
5.4. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO Coronavirus (COVID-19). Dashboard|WHO Coronavirus (COVID-19) Dashboard with Vaccination Data. Available online: https://covid19.who.int/ (accessed on 20 July 2021).
- Cohen, A.; Harari, E. Immature platelets in patients hospitalized with Covid-19. J. Thromb. Thrombolysis 2021, 51, 608–616. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.D.; Inchingolo, A.M. SARS-CoV-2 Disease Adjuvant Therapies and Supplements Breakthrough for the Infection Prevention. Microorganisms 2021, 9, 525. [Google Scholar] [CrossRef] [PubMed]
- Ulanowska, M.; Olas, B. Modulation of Hemostasis in COVID-19; Blood Platelets May Be Important Pieces in the COVID-19 Puzzle. Pathogens 2021, 10, 370. [Google Scholar] [CrossRef] [PubMed]
- Zhen, W.M.; van Wijk, X. Role of von Willebrand Factor in COVID-19 Associated Coagulopathy. J. Appl. Lab. Med. 2021, 6, 1305–1315. [Google Scholar] [CrossRef]
- Yusuf, S.; Hawken, S. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet 2004, 364, 937–952. [Google Scholar] [CrossRef]
- Arachchillage, D.; Laffan, M. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemost. 2020, 18, 1233–1234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tang, N.; Bai, H. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J. Thromb. Haemost. 2020, 18, 1094–1099. [Google Scholar] [CrossRef]
- Amgalan, A.; Othman, M. Hemostatic laboratory derangements in COVID-19 with a focus on platelet count. Platelets 2020, 31, 740–745. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Wang, K. Early decrease in blood platelet count is associated with poor prognosis in COVID-19 patients—Indications for predictive, preventive, and personalized medical approach. EPMA J. 2020, 11, 139. [Google Scholar] [CrossRef]
- Xu, P.; Zhou, Q. Mechanism of thrombocytopenia in COVID-19 patients. Ann. Hematol. 2020, 99, 1205–1208. [Google Scholar] [CrossRef] [Green Version]
- Tchachil, J. What do monitoring platelet counts in COVID-19 teach us? J. Thromb. Haemost. 2020, 18, 2071–2072. [Google Scholar] [CrossRef] [PubMed]
- Ouyang, S.M.; Zhu, H.Q. Temporal changes in laboratory markers of survivors and non-survivors of adult inpatients with COVID-19. BMC Infect. Dis. 2020, 20, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Abe, Y.; Wada, H. A simple technique to determine thrombopoiesis level using immature platelet fraction (IPF). Thromb Res. 2006, 118, 463–469. [Google Scholar] [CrossRef]
- Welder, D.; Jeon-Slaughter, H. Immature platelets as a biomarker for disease severity and mortality in COVID-19 patients. Br. J. Haematol. 2021, 194, 530–536. [Google Scholar] [CrossRef] [PubMed]
- Bachler, M.; Bosch, J. Impaired fibrinolysis in critically ill COVID-19 patients. Br. J. Anaesth. 2021, 126, 590–598. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.W.; Liu, W.W. Predictors of high on-aspirin platelet reactivity in elderly patients with coronary artery disease. Clin. Interv. Aging 2017, 12, 1271–1279. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bertolin, A.J.; Dalcoquio, T.F. Platelet Reactivity and Coagulation Markers in Patients with COVID-19. Adv. Ther. 2021, 38, 3911–3923. [Google Scholar] [CrossRef]
- Iacobucci, G. Covid-19: Aspirin does not improve survival for patients admitted to hospital, trial reports. BMJ 2021, 373. [Google Scholar] [CrossRef]
- RECOVERY Collaborative Group. Aspirin in patients admitted to hospital with COVID-19 (RECOVERY): A randomised, controlled, open-label, platform trial. Lancet 2021. [Google Scholar] [CrossRef]
- Kruse, J.M.; Magomedow, A. Thromboembolic complications in critically ill COVID-19 patients are associated with impaired fibrinolysis. Crit. Care 2020, 24, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Henry, B.M.; Santos de Oliveira, M.H. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): A meta-analysis. Clin. Chem. Lab. Med. 2020, 58, 1021–1028. [Google Scholar] [CrossRef] [Green Version]
- Ghahramani, S.; Tabrizi, R. Laboratory features of severe vs. non-severe COVID-19 patients in Asian populations: A systematic review and meta-analysis. Eur. J. Med. Res. 2020, 25, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Zeng, F.; Huang, Y. Association of inflammatory markers with the severity of COVID-19: A meta-analysis. Int. J. Infect. Dis. 2020, 96, 467–474. [Google Scholar] [CrossRef]
- Kermali, M.; Khalsa, R.K. The role of biomarkers in diagnosis of COVID-19—A systematic review. Life Sci. 2020, 254, 117788. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Li, L. Prognostic value of interleukin-6, C-reactive protein, and procalcitonin in patients with COVID-19. J. Clin. Virol. 2020, 127, 104370. [Google Scholar] [CrossRef] [PubMed]
- Wang, L. C-reactive protein levels in the early stage of COVID-19. Médecine Mal. Infect. 2020, 50, 332–334. [Google Scholar] [CrossRef]
- Poudel, A.; Poudel, Y. D-dimer as a biomarker for assessment of COVID-19 prognosis: D-dimer levels on admission and its role in predicting disease outcome in hospitalized patients with COVID-19. PLoS ONE 2021, 16, e0256744. [Google Scholar] [CrossRef]
- Zhang, L.; Yan, X. D-dimer levels on admission to predict in-hospital mortality in patients with Covid-19. J. Thromb. Haemost. 2020, 18, 1324–1329. [Google Scholar] [CrossRef] [PubMed]
- Lodigiani, C.; Iapichino, G. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb. Res. 2020, 191, 9–14. [Google Scholar] [CrossRef]
- Klok, F.A.; Kruip, M.J.H.A. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb. Res. 2020, 191, 145–147. [Google Scholar] [CrossRef]
- Della-Morte, D.; Pacifici, F. Low level of plasminogen increases risk for mortality in COVID-19 patients. Cell Death Dis. 2021, 12, 1–8. [Google Scholar] [CrossRef]
- Wool, G.D.; Miller, J.L. The Impact of COVID-19 Disease on Platelets and Coagulation. Pathobiology 2021, 88, 15–27. [Google Scholar] [CrossRef] [PubMed]
- Ward, S.E.; Curley, G.F. Von Willebrand factor propeptide in severe coronavirus disease 2019 (COVID-19): Evidence of acute and sustained endothelial cell activation. Br. J. Haematol. 2021, 192, 714–719. [Google Scholar] [CrossRef] [PubMed]
- Incir, S.; Komesli, Z. Immature platelet fraction: Is a novel early predictive marker for disease severity in patients with Covid-19 pneumonia? Turkish J. Biochem. 2021. [Google Scholar] [CrossRef]
- Schrick, D.; Ezer, E. Novel predictors of future vascular events in post-stroke patients—A pilot study. Front. Neurol. 2021, 12, 971. [Google Scholar] [CrossRef] [PubMed]
- Ezer, E.; Schrick, D. A novel approach of platelet function test for prediction of attenuated response to clopidogrel. Clin Hemorheol Microcirc. 2019, 73, 359–369. [Google Scholar] [CrossRef] [Green Version]
- Roh, D.J.; Eiseman, K. Hypercoagulable viscoelastic blood clot characteristics in critically ill coronavirus disease 2019 patients and associations with thrombotic complications. J. Trauma Acute Care Surg. 2021, 90, 7–12. [Google Scholar] [CrossRef]

| Patients n = 21 | Controls n = 21 | p | |
|---|---|---|---|
| Age (y) | 69 (52–71) | 67 (63–69) | 0.222 |
| Male (n) | 12 (50%) | 11 (52%) | 0.757 |
| BMI | 27 (26–33) | 25 (24–26) | 0.189 |
| Hypertension | 16 (76) | ||
| Diabetes mellitus | 12 (57) | ||
| Thromboembolic event (stroke/TIA, DVT) | 5 (24) | ||
| Myocardial infarct | 4 (19) | ||
| Heart failure | 1 (5) | ||
| ESR (mm/h) | 84 (36–107) | 4 (4–10) | <0.001 |
| Platelet (g/L) | 214 (114–355) | 261 (248–265) | 0.950 |
| IPF (%) | 8.7 (6.1–12.5) | 7.6 (6.7–8.2) | 0.753 |
| H-IPF (%) | 2.2 (0.6–4.1) | 0.9 (0.8–1.0) | 0.308 |
| Fibrinogen (g/L) | 5.1 (3.5–5.4) | 3.2 (2.8–3.2) | 0.059 |
| D-dimer (µg FEU/L) | 2296 (1415–6260) | 495 (363–575) | <0.001 |
| APTT (s) | 12.9 (12.4–14.0) | 26.3 (24.9–27.8) | 0.002 |
| TT (s) | 34.0 (31.2–36.7) | 10.4 (10.2–10.8) | <0.001 |
| vWF:Ag (%) | 488 (412–605) | 109 (97–109) | <0.001 |
| vWF:RCo (%) | 399 (353–568) | 104 (97–109) | <0.001 |
| Plasminogen (%) | 86 (64–96) | 104 (98–106) | 0.028 |
| Alpha-2-antiplasmin (%) | 118 (107–126) | 119 (116–121) | 1.000 |
| hs-CRP(mg/L) | 90.5 (27.7–126.1) | 1.2 (0.9–1.5) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schrick, D.; Tőkés-Füzesi, M.; Réger, B.; Molnár, T. Plasma Fibrinogen Independently Predicts Hypofibrinolysis in Severe COVID-19. Metabolites 2021, 11, 826. https://doi.org/10.3390/metabo11120826
Schrick D, Tőkés-Füzesi M, Réger B, Molnár T. Plasma Fibrinogen Independently Predicts Hypofibrinolysis in Severe COVID-19. Metabolites. 2021; 11(12):826. https://doi.org/10.3390/metabo11120826
Chicago/Turabian StyleSchrick, Diana, Margit Tőkés-Füzesi, Barbara Réger, and Tihamér Molnár. 2021. "Plasma Fibrinogen Independently Predicts Hypofibrinolysis in Severe COVID-19" Metabolites 11, no. 12: 826. https://doi.org/10.3390/metabo11120826
APA StyleSchrick, D., Tőkés-Füzesi, M., Réger, B., & Molnár, T. (2021). Plasma Fibrinogen Independently Predicts Hypofibrinolysis in Severe COVID-19. Metabolites, 11(12), 826. https://doi.org/10.3390/metabo11120826







