Effective Transcutaneous Delivery of Hyaluronic Acid Using an Easy-to-Prepare Reverse Micelle Formulation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Synthesis of Fluorescein-Labeled HA (FCHA)
2.3. Preparation of the FCHA-Loaded Reverse Micelle Formulation
2.4. In Vitro Skin Permeation Study
2.5. In Vitro Skin Permeation Study
2.6. Statistical Analysis
3. Results & Discussion
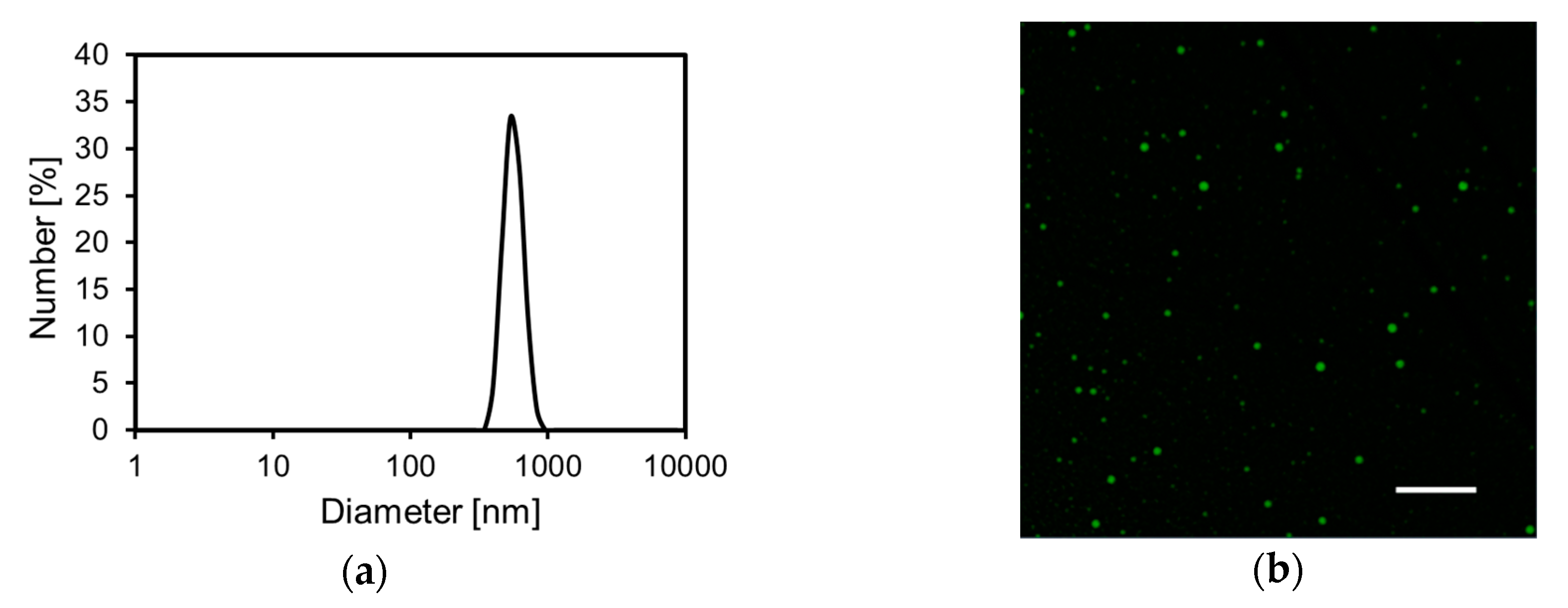
3.1. Preparation and Characterization of the Reverse Micelle Formulation
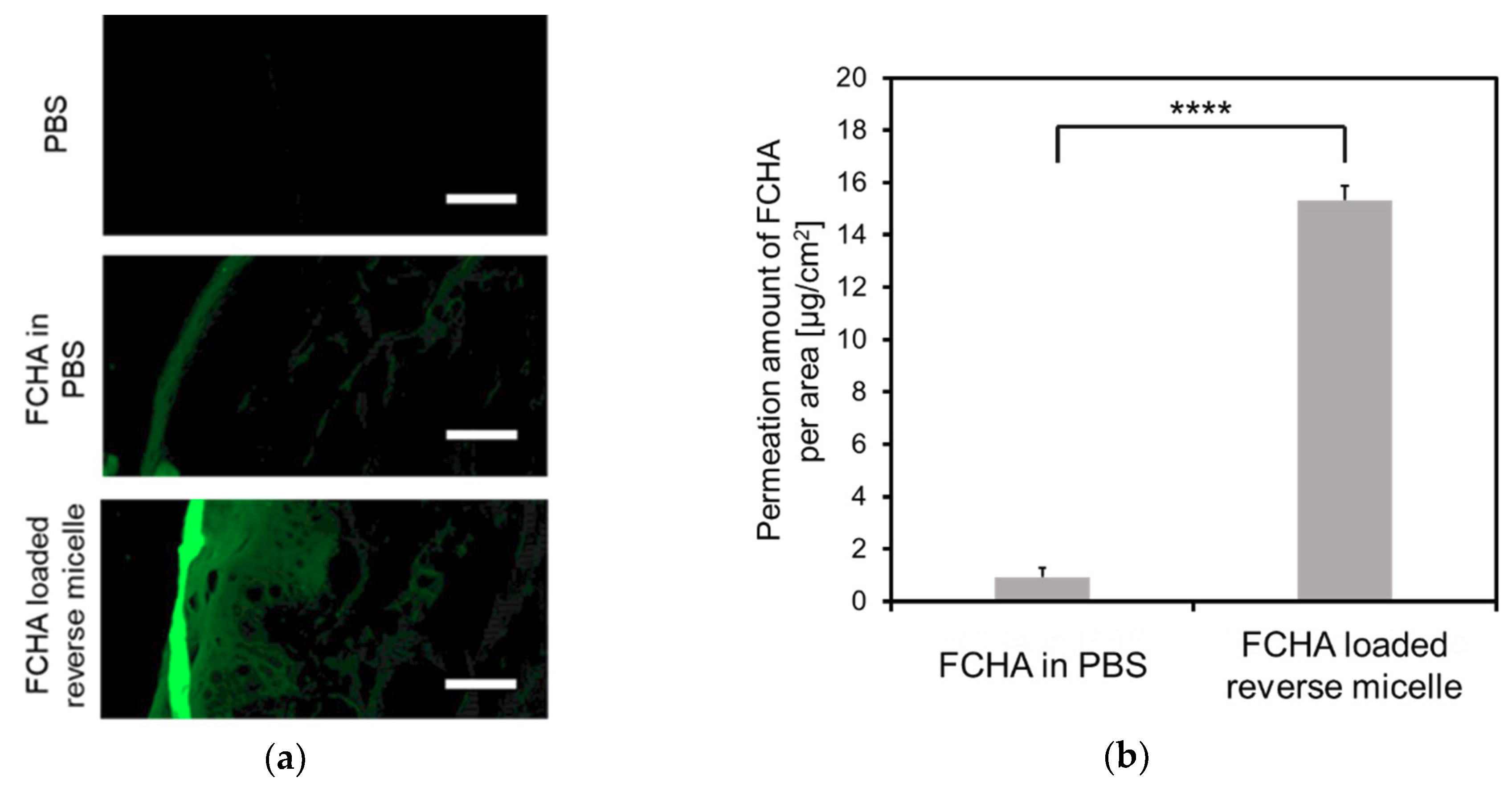
3.2. Permeation of FCHA into YMP Skin
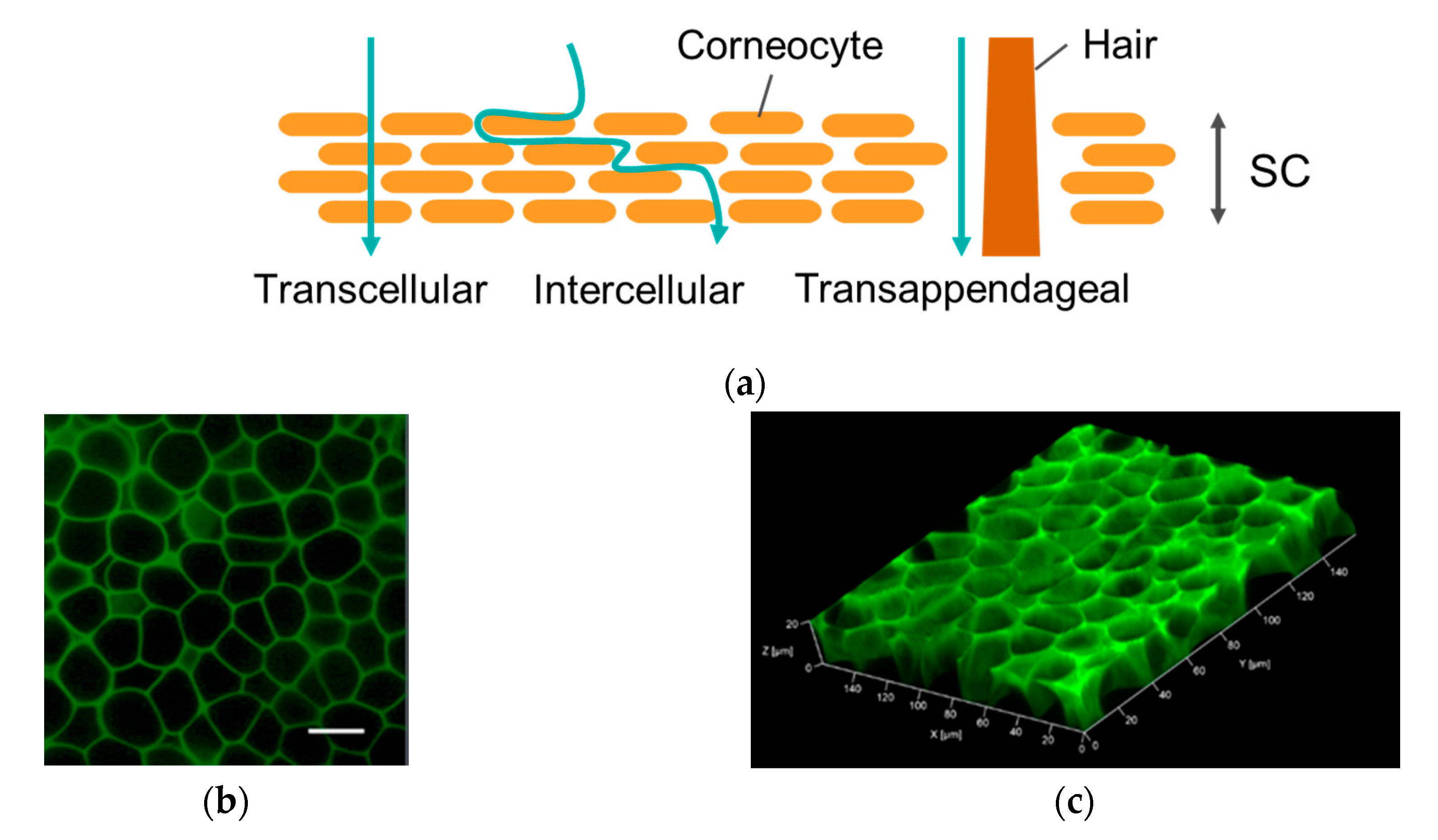
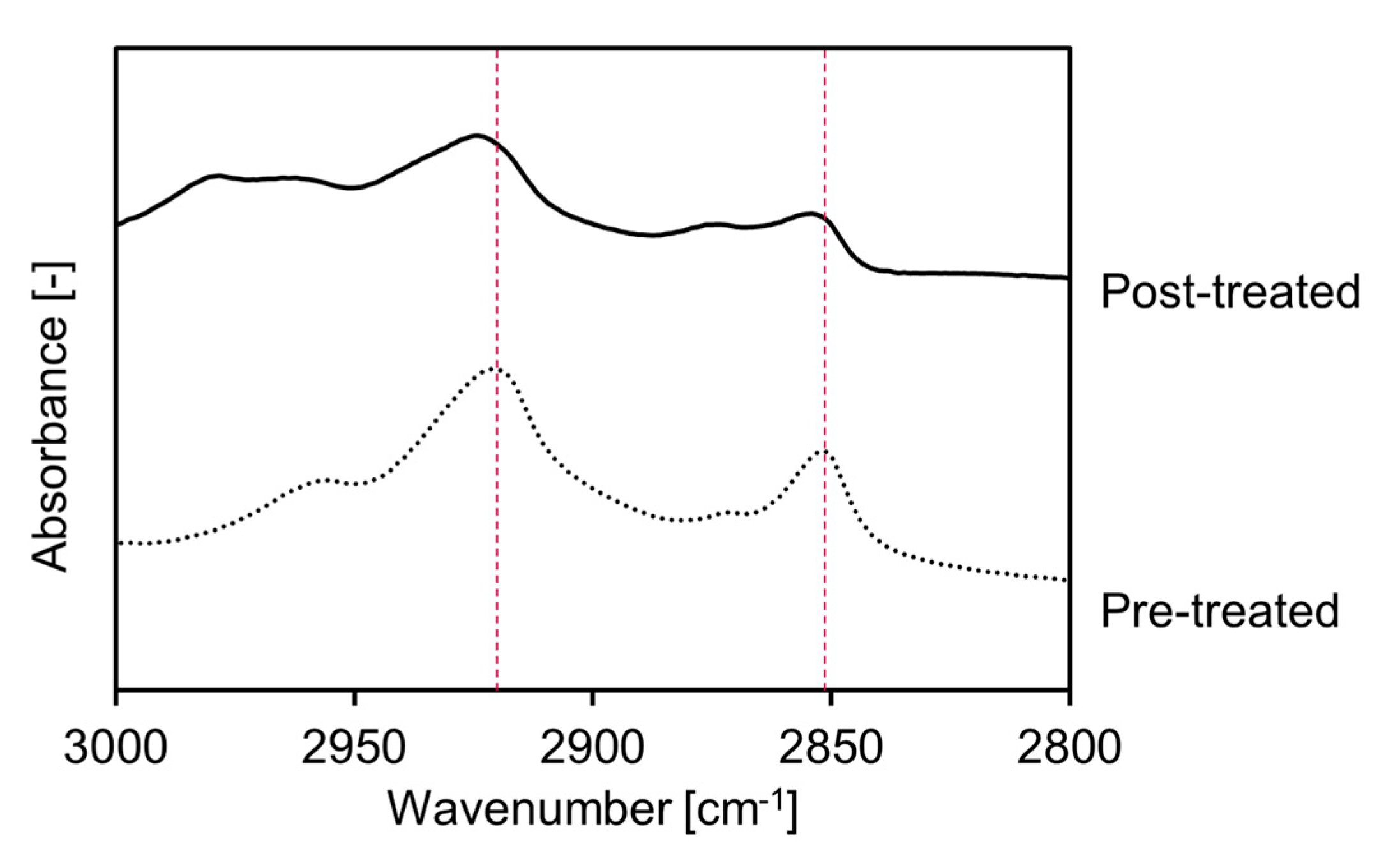
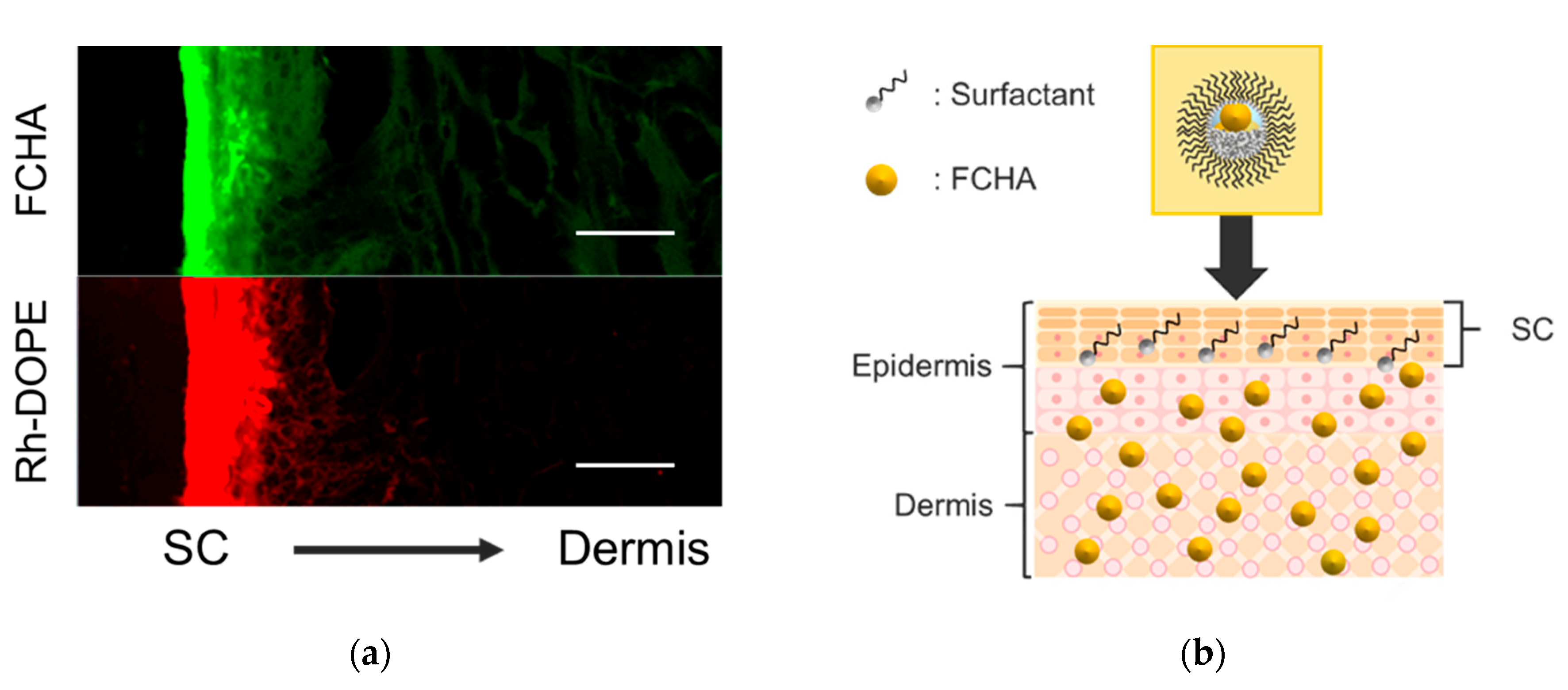
3.3. Permeation Mechanism of the FCHA-Loaded Reverse Micelle Formulation
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Meyer, L.J.; Sttern, R. Age-Dependent Changes of Hyaluronan in Human Skin. J. Invest. Dermatol. 1994, 102, 385–389. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takagi, Y.; Mori, K.; Taguchi, H.; Nishizaka, T.; Takema, Y. UVB sensitivity correlates with cutaneous barrier function in the skin of Japanese females. Photodermatol. Photoimmunol. Photomed. 2019, 35, 284–285. [Google Scholar] [CrossRef] [PubMed]
- Papakonstantinou, E.; Roth, M.; Karakiulakis, G. Hyaluronic acid: A key molecule in skin aging. Dermato-endocrinology 2012, 4, 253–258. [Google Scholar] [CrossRef] [Green Version]
- Tang, M.; Svirskis, D.; Leung, E.; Kanamala, M.; Wang, H. Can intracellular drug delivery using hyaluronic acid functionalised pH- sensitive liposomes overcome gemcitabine resistance in pancreatic cancer? J. Control. Release 2019, 305, 89–100. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Sugihara, K.; Gillilland, M.G.; Jon, S.; Kamada, N.; Moon, J.J. Hyaluronic acid–bilirubin nanomedicine for targeted modulation of dysregulated intestinal barrier, microbiome and immune responses in colitis. Nat. Mater. 2020, 19, 118–126. [Google Scholar] [CrossRef]
- Cadete, A.; Olivera, A.; Besev, M.; Dhal, P.K.; Gonçalves, L.; Almeida, A.J.; Bastiat, G.; Benoit, J.P.; Garcia-Fuentes, M. Self-assembled hyaluronan nanocapsules for the intracellular delivery of anticancer drugs. Sci. Rep. 2019, 9, 1–11. [Google Scholar] [CrossRef]
- He, M.-S.; Sheu, M.-M.; Huang, Z.-L.; Tsai, C.-H.; Tsai, R.-K. Sudden bilateral vision loss and brain infarction following cosmetic hyaluronic acid injection. JAMA Ophthalmol. 2013, 131, 1234–1235. [Google Scholar] [CrossRef]
- Carle, M.V.; Roe, R.; Novack, R.; Boyer, D.S. Cosmetic Facial Fillers and Severe Vision Loss. JAMA Ophthalmol. 2014, 132, 637–639. [Google Scholar] [CrossRef] [Green Version]
- Bos, J.D.; Meinardi, M.M.H.M. The 500 Dalton rule for the skin penetration of chemical compounds and drugs. Exp. Dermatol. 2000, 9, 165–169. [Google Scholar] [CrossRef]
- Zhu, J.; Tang, X.; Jia, Y.; Ho, C.; Huang, Q. Applications and delivery mechanisms of hyaluronic acid used for topical/transdermal delivery—A review. Int. J. Pharm. 2020, 578, 119127. [Google Scholar] [CrossRef]
- Witting, M.; Boreham, A.; Brodwolf, R.; Alexiev, U.; Friess, W.; Hedtrich, S. Interactions of Hyaluronic Acid with the Skin and Implications for the Dermal Delivery of Biomacromolecules. Mol. Pharm. 2015, 12, 1391–1401. [Google Scholar] [CrossRef] [PubMed]
- Vistoli, G.; Gennari, C.G.M.; Selmin, F.; Gardoni, F.; Franze, S.; Campisic, M.; Minghetti, P. The Role of the Conformational Profile of Polysaccharides on Skin Penetration: The Case of Hyaluronan and Its Sulfates. Chem. Biodivers. 2014, 11, 551–561. [Google Scholar]
- Bok, M.; Zhao, Z.; Jeon, S.; Jeong, J.; Lim, E. Ultrasonically and Iontophoretically Enhanced Drug-Delivery System Based on Dissolving Microneedle Patches. Sci. Rep. 2020, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Kasetvatin, C.; Rujivipat, S.; Tiyaboonchai, W. Combination of elastic liposomes and low frequency ultrasound for skin permeation enhancement of hyaluronic acid. Colloids Surfaces B Biointerfaces 2015, 135, 458–464. [Google Scholar] [CrossRef]
- Tokudome, Y.; Komi, T.; Omata, A.; Sekita, M. A new strategy for the passive skin delivery of nanoparticulate, high molecular weight hyaluronic acid prepared by a polyion complex method. Sci. Rep. 2018, 1–9. [Google Scholar] [CrossRef]
- Funatsu, A.; Tahara, Y.; Yamanaka, S.; Goto, M. Oil Gel Sheets Utilizing Solid–in–Oil Technique. MEMBRANE 2011, 36, 57–62. [Google Scholar] [CrossRef] [Green Version]
- Hoppel, M.; Juric, S.; Ettl, H.; Valenta, C. Effect of monoacyl phosphatidylcholine content on the formation of microemulsions and the dermal delivery of flufenamic acid. Int. J. Pharm. 2015, 479, 70–76. [Google Scholar] [CrossRef]
- Lehtinen, O.; Wahyu, R.; Nugroho, N.; Lehtimaa, T.; Vierros, S.; Hiekkataipale, P.; Ruokolainen, J.; Sammalkorpi, M.; Österberg, M. Effect of temperature, water content and free fatty acid on reverse micelle formation of phospholipids in vegetable oil. Colloids Surfaces B Biointerfaces 2017, 160, 355–363. [Google Scholar] [CrossRef] [Green Version]
- Kosakowska, K.A.; Casey, B.K.; Kurtz, S.L.; Lawson, L.B.; Grayson, S.M. Evaluation of Amphiphilic Star/Linear—Dendritic Polymer Reverse Micelles for Transdermal Drug Delivery: Directing Carrier Properties by Tailoring Core versus Peripheral Branching. Biomacromolecules 2018, 19, 3163–3176. [Google Scholar] [CrossRef]
- Szuma, P.; Jungnickel, C.; Koz, K.; Jacyna, B.; Cal, K. Transdermal transport of collagen and hyaluronic acid using water in oil microemulsion. Int. J. Pharm. 2019, 572. [Google Scholar] [CrossRef]
- Himes, R.; Lee, S.; Mcmenigall, K.; Russell-jones, G. The influence of molecular adjuvants in the cutaneous response to antigen after topical vaccination. Vaccine 2011, 29, 5393–5398. [Google Scholar] [CrossRef] [PubMed]
- Kozaka, S.; Tahara, Y.; Wakabayashi, R.; Nakata, T.; Ueda, T.; Kamiya, N.; Goto, M. Transcutaneous Cancer Vaccine Using a Reverse Micellar Antigen Carrier. Mol. Pharm. 2020, 17, 645–655. [Google Scholar] [CrossRef] [PubMed]
- Zakrewsky, M.; Lovejoy, K.S.; Kern, T.L.; Miller, T.E.; Le, V.; Nagy, A.; Goumas, A.M.; Iyer, R.S.; Del Sesto, R.E.; Koppisch, A.T.; et al. Ionic liquids as a class of materials for transdermal delivery and pathogen neutralization. Proc. Natl. Acad. Sci. USA 2014, 111, 13313–13318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Banerjee, A.; Ibsen, K.; Iwao, Y.; Zakrewsky, M.; Mitragotri, S. Transdermal Protein Delivery Using Choline and Geranate ( CAGE ) Deep Eutectic Solvent. Adv. Healthc. Mater. 2017, 6, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kulkarni, C.V.; Wachter, W.; Iglesias-Salto, G.; Engelskirchen, S.; Ahualli, S. Monoolein: A magic lipid? Phys. Chem. Chem. Phys. 2011, 13, 3004–3021. [Google Scholar] [CrossRef]
- Karande, P.; Jain, A.; Ergun, K.; Kispersky, V.; Mitragotri, S. Design principles of chemical penetration enhancers for transdermal drug delivery. Proc. Natl. Acad. Sci. USA 2005, 102, 4688–4693. [Google Scholar] [CrossRef] [Green Version]
- Fujii, M.; Yamanouchi, S.; Hori, N.; Iwanaga, N.; Nawaguchi, N.; Matsumoto, M. Evaluation of Yucatan Micropig Skin for Use as an in Vitro Model for Skin Permeation Study. Biol. Pharm. Bull. 1997, 20, 249–254. [Google Scholar] [CrossRef] [Green Version]
- Kotla, N.G.; Chandrasekar, B.; Rooney, P.; Sivaraman, G.; Larrañaga, A.; Krishna, K.V.; Pandit, A.; Rochev, Y. Biomimetic Lipid-Based Nanosystems for Enhanced Dermal Delivery of Drugs and Bioactive Agents. ACS Biomater. Sci. Eng. 2017, 3, 1262–1272. [Google Scholar] [CrossRef]
- Barry, B.W. Novel mechanisms and devices to enable successful transdermal drug delivery. Eur. J. Pharm. Sci. 2001, 14, 101–114. [Google Scholar] [CrossRef]
- Ruela, A.L.M.; Perissinato, A.G.; Lino, M.E.d.; Mudrik, P.S. Gislaine ribeiro pereira evaluation of skin absorption of drugs from topical and transdermal formulations. Braz. J. Pharm. Sci. 2014, 52, 527–544. [Google Scholar] [CrossRef] [Green Version]
- Mendelsohn, R.; Flach, C.R.; Moore, D.J. Determination of molecular conformation and permeation in skin via IR spectroscopy, microscopy, and imaging. Biochim. Biophys. Acta - Biomembr. 2006, 1758, 923–933. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pouliot, R.; Germain, L.; Auger, A.; Tremblay, N. Julianna Juhasz Physical characterization of the stratum corneum of an in vitro human skin equivalent produced by tissue engineering and its comparison with normal human skin by ATR-FTIR spectroscopy and thermal analysis (DSC). Biochim. Biophys. Acta 1999, 1439, 341–352. [Google Scholar] [CrossRef]
- Akinshina, A.; Das, C.; Noro, M.G. Effect of monoglycerides and fatty acids on a ceramide bilayer. Phys. Chem. Chem. Phys. 2016, 18, 17446–17460. [Google Scholar] [CrossRef] [Green Version]
- Gupta, R.; Dwadasi, B.S.; Rai, B.; Mitragotri, S. Effect of Chemical Permeation Enhancers on Skin Permeability: In silico screening using Molecular Dynamics simulations. Sci. Rep. 2019, 9, 1456. [Google Scholar] [CrossRef] [Green Version]
- Botelho, M.A.; Guerreiro, S.J.; Queiroz, D.B.; Barros, G.; Cavalcante, M.; Souza, J.M.O.; Silva, A.M.; Lemos, T.L.G.; Quintans, L., Jr. Depth-scanning confocal Raman for rapid in vivo determination of testosterone concentration profiles in human skin. Medicalexpress 2014, 1, 31–35. [Google Scholar] [CrossRef] [Green Version]
- Tahara, Y.; Honda, S.; Kamiya, N.; Piao, H.; Hirata, A.; Hayakawa, E.; Fujii, T.; Goto, M. A solid-in-oil nanodispersion for transcutaneous protein delivery. J. Control. Release 2008, 131, 14–18. [Google Scholar] [CrossRef]

| IPM | IPA | MO | Water | W0 |
|---|---|---|---|---|
| (wt.%) | (wt.%) | (wt.%) | (wt.%) | (-) |
| 91.5 | 2.0 | 6.0 | 0.5 | 1.7 |
| 89.5 | 4.0 | |||
| 87.5 | 6.0 | |||
| 85.5 | 8.0 | |||
| 83.5 | 10.0 | |||
| 89.2 | 2.0 | 8.0 | 0.8 | 2.0 |
| 87.2 | 4.0 | |||
| 85.2 | 6.0 | |||
| 83.2 | 8.0 | |||
| 81.2 | 10.0 | |||
| 93.5 | 2.0 | 4.0 | 0.5 | 2.5 |
| 91.5 | 4.0 | |||
| 89.5 | 6.0 | |||
| 87.5 | 8.0 | |||
| 85.5 | 10.0 | |||
| 91.0 | 2.0 | 6.0 | 1.0 | 3.3 |
| 89.0 | 4.0 | |||
| 87.0 | 6.0 | |||
| 85.0 | 8.0 | |||
| 83.0 | 10.0 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kozaka, S.; Kashima, A.; Wakabayashi, R.; Nakata, T.; Ueda, T.; Goto, M. Effective Transcutaneous Delivery of Hyaluronic Acid Using an Easy-to-Prepare Reverse Micelle Formulation. Cosmetics 2020, 7, 52. https://doi.org/10.3390/cosmetics7030052
Kozaka S, Kashima A, Wakabayashi R, Nakata T, Ueda T, Goto M. Effective Transcutaneous Delivery of Hyaluronic Acid Using an Easy-to-Prepare Reverse Micelle Formulation. Cosmetics. 2020; 7(3):52. https://doi.org/10.3390/cosmetics7030052
Chicago/Turabian StyleKozaka, Shuto, Ayaka Kashima, Rie Wakabayashi, Takahiro Nakata, Taro Ueda, and Masahiro Goto. 2020. "Effective Transcutaneous Delivery of Hyaluronic Acid Using an Easy-to-Prepare Reverse Micelle Formulation" Cosmetics 7, no. 3: 52. https://doi.org/10.3390/cosmetics7030052
APA StyleKozaka, S., Kashima, A., Wakabayashi, R., Nakata, T., Ueda, T., & Goto, M. (2020). Effective Transcutaneous Delivery of Hyaluronic Acid Using an Easy-to-Prepare Reverse Micelle Formulation. Cosmetics, 7(3), 52. https://doi.org/10.3390/cosmetics7030052






