One-Year Clinical Aging of Low Stress Bulk-Fill Flowable Composite in Class II Restorations: A Case Report and Literature Review
Abstract
1. Introduction
2. Case Presentation
2.1. Materials and Methods
2.1.1. Tooth Restoration and Aging
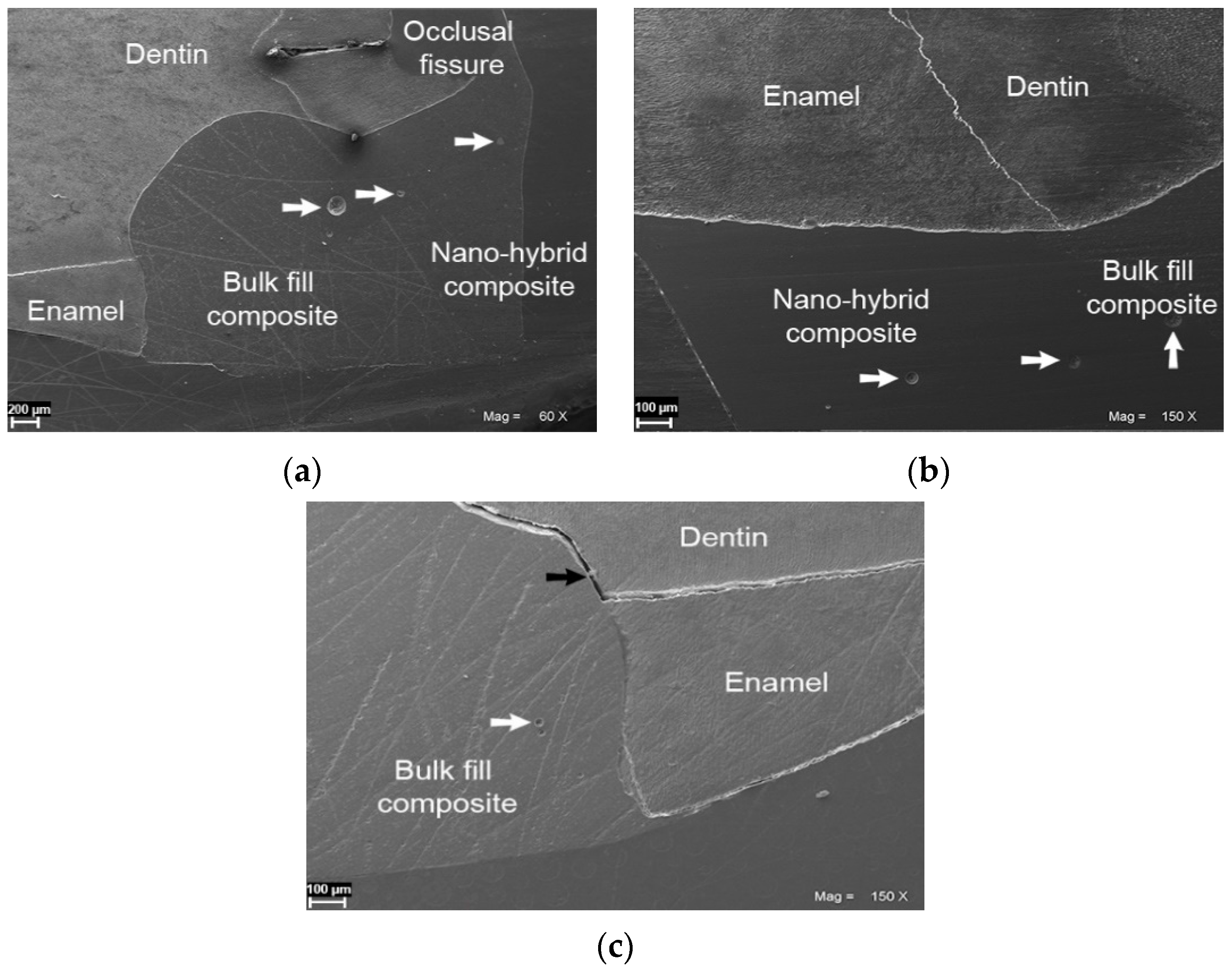
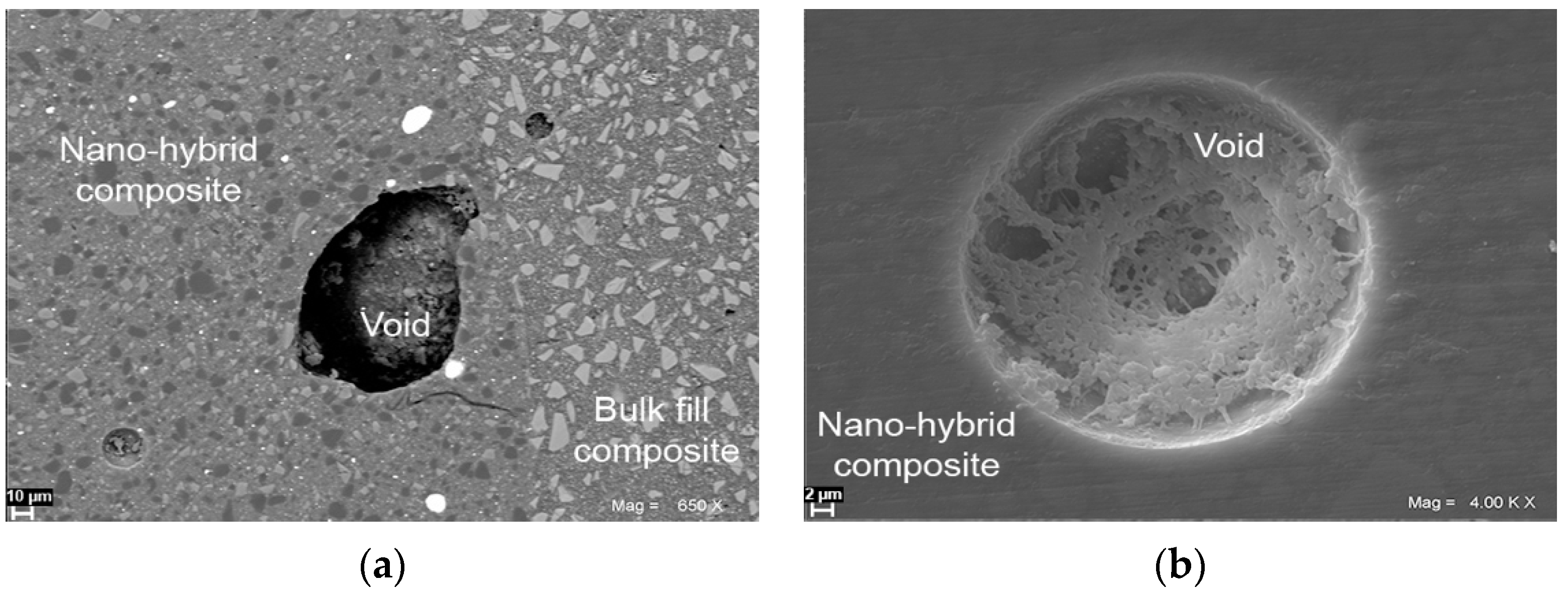
2.1.2. SEM Study
2.1.3. Results
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Miletic, V. Development of Dental Composites. In Dental Composite Materials for Direct Restorations; Springer: Cham, Switzerland, 2018; pp. 3–9. [Google Scholar]
- Zarow, M.; Vadini, M.; Chojnacka-Brozek, A.; Szczeklik, K.; Milewski, G.; Biferi, V.; D’Arcangelo, C.; De Angelis, F. Effect of fiber posts on stress distribution of endodontically treated upper premolars: Finite element analysis. Nanomaterials (Basel) 2020, 10, 1708. [Google Scholar] [CrossRef]
- Zarow, M.; Ramírez-Sebastià, A.; Paolone, G.; de Ribot Porta, J.; Mora, J.; Espona, J.; Durán-Sindreu, F.; Roig, M. A new classification system for the restoration of root filled teeth. Int. Endod. J. 2018, 51, 318–334. [Google Scholar] [CrossRef] [PubMed]
- Scotti, N.; Comba, A.; Gambino, A.; Paolino, D.S.; Alovisi, M.; Pasqualini, D.; Berutti, E. Microleakage at enamel and dentin margins with a bulk fills flowable resin. Eur. J. Dent. 2014, 8, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Hardan, L.S.; Amm, E.W.; Ghayad, A. Effect of different modes of light curing and resin composites on microleakage of class II restorations. Odontostomatol. Trop. 2008, 31, 27–34. [Google Scholar] [PubMed]
- Hardan, L.S.; Amm, E.W.; Ghayad, A.; Ghosn, C.; Khraisat, A. Effect of different modes of light curing and resin composites on microleakage of class II restorations—Part II. Odontostomatol. Trop. 2009, 32, 29–37. [Google Scholar] [PubMed]
- Bociong, K.; Szczesio, A.; Sokolowski, K.; Domarecka, M.; Sokolowski, J.; Krasowski, M.; Lukomska-Szymanska, M. the influence of water sorption of dental light-cured composites on shrinkage stress. Materials 2017, 10, 1142. [Google Scholar] [CrossRef] [PubMed]
- Sadeghi, M.; Lynch, C.D. The effect of flowable materials on the microleakage of class II composite restorations that extend apical to the cemento-enamel junction. Oper. Dent. 2009, 34, 306–311. [Google Scholar] [CrossRef] [PubMed]
- Roggendorf, M.J.; Krämer, N.; Appelt, A.; Naumann, M.; Frankenberger, R. Marginal quality of flowable 4-mm base vs. conventionally layered resin composite. J. Dent. 2011, 39, 643–647. [Google Scholar] [CrossRef]
- Frankenberger, R.; Krämer, N.; Lohbauer, U.; Nikolaenko, S.A.; Reich, S.M. Marginal integrity: Is the clinical performance of bonded restorations predictable in vitro? J. Adhes. Dent. 2007, 9, 107–116. [Google Scholar] [PubMed]
- Frankenberger, R.; Krämer, N.; Pelka, M.; Petschelt, A. Internal adaptation and overhang formation of direct class II resin composite restorations. Clin. Oral. Investig. 1999, 3, 208–215. [Google Scholar] [CrossRef]
- Van Meerbeek, B.; De Munck, J.; Yoshida, Y.; Inoue, S.; Vargas, M.; Vijay, P.; Van Landuyt, K.; Lambrechts, P.; Vanherle, G. Buonocore memorial lecture. Adhesion to enamel and dentin: Current status and future challenges. Oper. Dent. 2003, 28, 215–235. [Google Scholar]
- Stavridakis, M.M.; Dietschi, D.; Krejci, I. Polymerization shrinkage of flowable resin-based restorative materials. Oper. Dent. 2005, 30, 118–128. [Google Scholar]
- Colak, H.; Tokay, U.; Uzgur, R.; Hamidi, M.M.; Ercan, E. A prospective, randomized, double-blind clinical trial of one nano-hybrid and one high-viscosity bulk-fill composite restorative systems in class II cavities: 12 months results. Niger. J. Clin. Pract. 2017, 20, 822–831. [Google Scholar] [CrossRef]
- Leprince, J.G.; Palin, W.M.; Vanacker, J.; Sabbagh, J.; Devaux, J.; Leloup, G. Physico-mechanical characteristics of commercially available bulk-fill composites. J. Dent. 2014, 42, 993–1000. [Google Scholar] [CrossRef] [PubMed]
- Fronza, B.M.; Makishi, P.; Sadr, A.; Shimada, Y.; Sumi, Y.; Tagami, J.; Giannini, M. Evaluation of bulk-fill systems: Microtensile bond strength and non-destructive imaging of marginal adaptation. Braz. Oral. Res. 2018, 32, 80. [Google Scholar] [CrossRef]
- Domarecka, M.; Sokolowski, K.; Krasowski, M.; Lukomska-Szymanska, M.; Sokolowski, J. The shrinkage stress of modified flowable dental composites. Dent. Med. Prob. 2015, 52, 424–433. [Google Scholar] [CrossRef]
- Sokolowski, K.; Szczesio-Wlodarczyk, A.; Bociong, K.; Krasowski, M.; Fronczek-Wojciechowska, M.; Domarecka, M.; Sokolowski, J.; Lukomska-Szymanska, M. Contraction and hydroscopic expansion stress of dental ion-releasing polymeric materials. Polymers 2018, 10, 1093. [Google Scholar] [CrossRef] [PubMed]
- D’Amario, M.; De Angelis, F.; Vadini, M.; Marchili, N.; Mummolo, S.; D’Arcangelo, C. Influence of a repeated preheating procedure on mechanical properties of three resin composites. Oper. Dent. 2015, 40, 181–189. [Google Scholar] [CrossRef]
- D’Arcangelo, C.; Zarow, M.; De Angelis, F.; Vadini, M.; Paolantonio, M.; Giannoni, M.; D’Amario, M. Five-year retrospective clinical study of indirect composite restorations luted with a light-cured composite in posterior teeth. Clin. Oral. Investig. 2014, 18, 615–624. [Google Scholar] [CrossRef] [PubMed]
- Van Dijken, J.W.; Pallesen, U. Posterior bulk-filled resin composite restorations: A 5-year randomized controlled clinical study. J. Dent. 2016, 51, 29–35. [Google Scholar] [CrossRef]
- Heck, K.; Manhart, J.; Hickel, R.; Diegritz, C. Clinical evaluation of the bulk fill composite QuiXfil in molar class I and II cavities: 10-year results of a RCT. Dent. Mater. 2018, 34, 138–147. [Google Scholar] [CrossRef] [PubMed]
- Cidreira Boaro, L.C.; Pereira Lopes, D.; de Souza, A.; Lie Nakano, E.; Ayala Perez, M.D.; Pfeifer, C.S.; Gonçalves, F. Clinical performance and chemical-physical properties of bulk fill composites resin -a systematic review and meta-analysis. Dent. Mater. 2019, 35, 249–264. [Google Scholar] [CrossRef]
- Arbildo-Vega, H.I.; Lapinska, B.; Panda, S.; Lamas-Lara, C.; Khan, A.S.; Lukomska-Szymanska, M. Clinical effectiveness of bulk-fill and conventional resin composite restorations: Systematic Review and Meta-Analysis. Polymers 2020, 12, 1786. [Google Scholar] [CrossRef] [PubMed]
- Nazari, A.; Sadr, A.; Shimada, Y.; Tagami, J.; Sumi, Y. 3D assessment of void and gap formation in flowable resin composites using optical coherence tomography. J. Adhes. Dent. 2013, 15, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.J.; Kim, R.; Ferracane, J.L.; Lee, I.B. Influence of the compliance and layering method on the wall deflection of simulated cavities in bulk-fill composite restoration. Oper. Dent. 2016, 41, 183–194. [Google Scholar] [CrossRef] [PubMed]
- Ilie, N.; Hickel, R. Investigations on a methacrylate-based flowable composite based on the SDR™ technology. Dent. Mater. 2011, 27, 348–355. [Google Scholar] [CrossRef]
- Ilie, N.; Bucuta, S.; Draenert, M. Bulk-fill resin-based composites: An in vitro assessment of their mechanical performance. Oper. Dent. 2013, 38, 618–625. [Google Scholar] [CrossRef]
- Ilie, N.; Stark, K. Effect of different curing protocols on the mechanical properties of low-viscosity bulk-fill composites. Clin. Oral. Investig. 2015, 19, 271–279. [Google Scholar] [CrossRef]
- Garcia-Godoy, F.; Krämer, N.; Feilzer, A.J.; Frankenberger, R. Long-term degradation of enamel and dentin bonds: 6-year results in vitro vs. in vivo. Dent. Mater. 2010, 26, 1113–1118. [Google Scholar] [CrossRef]
- Khoroushi, M.; Rafizadeh, M.; Samimi, P. Bond strength of composite resin to enamel: Assessment of two ethanol wet-bonding techniques. J. Dent. 2014, 11, 150–160. [Google Scholar]
- Cadenaro, M.; Maravic, T.; Comba, A.; Mazzoni, A.; Fanfoni, L.; Hilton, T.; Ferracane, J.; Breschi, L. The role of polymerization in adhesive dentistry. Dent. Mater. 2019, 35, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Koshiro, K.; Inoue, S.; Sano, H.; De Munck, J.; Van Meerbeek, B. In vivo degradation of resin-dentin bonds produced by a self-etch and an etch-and-rinse adhesive. Eur. J. Oral. Sci. 2005, 113, 341–348. [Google Scholar] [CrossRef]
- Hardan, L.; Bourgi, R.; Kharouf, N.; Mancino, D.; Zarow, M.; Jakubowicz, N.; Haikel, Y.; Cuevas-Suárez, C.E. bond strength of universal adhesives to dentin: A systematic review and meta-analysis. Polymers 2021, 13, 814. [Google Scholar] [CrossRef] [PubMed]
- De Munck, J.; Van Meerbeek, B.; Yoshida, Y.; Inoue, S.; Vargas, M.; Suzuki, K.; Lambrechts, P.; Vanherle, G. Four-year water degradation of total-etch adhesives bonded to dentin. J. Dent. Res. 2003, 82, 136–140. [Google Scholar] [CrossRef] [PubMed]
- Nawrocka, A.; Łukomska-Szymańska, M. Extracted human teeth and their utility in dental research. Recommendations on proper preservation: A literature review. Dent. Med. Probl. 2019, 56, 185–190. [Google Scholar] [CrossRef]
- Lapinska, B.; Klimek, L.; Sokolowski, J.; Lukomska-Szymanska, M. Dentine surface morphology after chlorhexidine application-SEM study. Polymers 2018, 10, 905. [Google Scholar] [CrossRef]
- Dressano, D.; Salvador, M.V.; Oliveira, M.T.; Marchi, G.M.; Fronza, B.M.; Hadis, M.; Palin, W.M.; Lima, A.F. Chemistry of novel and contemporary resin-based dental adhesives. J. Mech. Behav. Biomed. Mater. 2020, 110, 103875. [Google Scholar] [CrossRef]
- Cardoso, M.V.; de Almeida Neves, A.; Mine, A.; Coutinho, E.; Van Landuyt, K.; De Munck, J.; Van Meerbeek, B. Current aspects on bonding effectiveness and stability in adhesive dentistry. Aust. Dent. J. 2011, 56, 31–44. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, M.; Ohno, H.; Kaga, M.; Endo, K.; Sano, H.; Oguchi, H. In vivo degradation of resin-dentin bonds in humans over 1 to 3 years. J. Dent. Res. 2000, 79, 1385–1391. [Google Scholar] [CrossRef]
- Cuevas-Suárez, C.E.; da Rosa, W.L.O.; Lund, R.G.; da Silva, A.F.; Piva, E. Bonding performance of universal adhesives: An updated systematic review and meta-analysis. J. Adhes. Dent. 2019, 21, 7–26. [Google Scholar] [CrossRef]
- Guba, C.J.; Cochran, M.A.; Swartz, M.L. The effects of varied etching time and etching solution viscosity on bond strength and enamel morphology. Oper. Dent. 1994, 19, 146–153. [Google Scholar]
- Bernales Sender, F.R.; Castañeda Vía, J.A.; Tay, L.Y. Influence of different phosphoric acids before application of universal adhesive on the dental enamel. J. Esthet. Restor. Dent. 2020, 32, 797–805. [Google Scholar] [CrossRef]
- Barkmeier, W.W.; Erickson, R.L.; Latta, M.A. Fatigue limits of enamel bonds with moist and dry techniques. Dent. Mater. 2009, 25, 1527–1531. [Google Scholar] [CrossRef] [PubMed]
- Gamborgi, G.P.; Loguercio, A.D.; Reis, A. Influence of enamel border and regional variability on durability of resin-dentin bonds. J. Dent. 2007, 35, 371–376. [Google Scholar] [CrossRef] [PubMed]
- Soliman, S.; Preidl, R.; Karl, S.; Hofmann, N.; Krastl, G.; Klaiber, B. Influence of cavity margin design and restorative material on marginal quality and seal of extended class II resin composite restorations in vitro. J. Adhes. Dent. 2016, 18, 7–16. [Google Scholar] [CrossRef]
- Heintze, S.D.; Ruffieux, C.; Rousson, V. Clinical performance of cervical restorations—A meta-analysis. Dent. Mater. 2010, 26, 993–1000. [Google Scholar] [CrossRef] [PubMed]
- Ozer, F.; Blatz, M.B. Self-etch and etch-and-rinse adhesive systems in clinical dentistry. Compend. Contin. Educ. Dent. 2013, 34, 12–30. [Google Scholar] [PubMed]
- Manuja, N.; Nagpal, R.; Pandit, I.K. Dental adhesion: Mechanism, techniques and durability. J. Clin. Pediatr. Dent. 2012, 36, 223–234. [Google Scholar] [CrossRef] [PubMed]
- Boushell, L.W.; Heymann, H.O.; Ritter, A.V.; Sturdevant, J.R.; Swift, E.J., Jr.; Wilder, A.D., Jr.; Chung, Y.; Lambert, C.A.; Walter, R. Six-year clinical performance of etch-and-rinse and self-etch adhesives. Dent. Mater. 2016, 32, 1065–1072. [Google Scholar] [CrossRef] [PubMed]
- Bourgi, R.; Hardan, L.; Rivera-Gonzaga, A.; Cuevas-Suárez, C.E. Effect of warm-air stream for solvent evaporation on bond strength of adhesive systems: A systematic review and meta-analysis of in vitro studies. Int. J. Adhes. Adhes. 2021, 105, 102794. [Google Scholar] [CrossRef]
- Bourgi, R.; Daood, U.; Bijle, M.N.; Fawzy, A.; Ghaleb, M.; Hardan, L. Reinforced universal adhesive by ribose crosslinker: A novel strategy in adhesive dentistry. Polymers 2021, 13, 704. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, R.M.; Pereira, J.C.; Yoshiyama, M.; Pashley, D.H. A review of polymerization contraction: The influence of stress development versus stress relief. Oper. Dent. 1996, 21, 17–24. [Google Scholar]
- Maske, T.T.; Hollanders, A.C.C.; Kuper, N.K.; Bronkhorst, E.M.; Cenci, M.S.; Huysmans, M.C.D.N.J.M. A threshold gap size for in situ secondary caries lesion development. J. Dent. 2019, 80, 36–40. [Google Scholar] [CrossRef]
- Maske, T.T.; Kuper, N.K.; Cenci, M.S.; Huysmans, M.D.N.J.M. Minimal gap size and dentin wall lesion development next to resin composite in a microcosm biofilm model. Caries. Res. 2017, 51, 475–481. [Google Scholar] [CrossRef]
- Demirci, M.; Tuncer, S.; Sancaklı, H.S.; Tekçe, N.; Baydemir, C. Clinical performance of different solvent-based dentin adhesives with nanofill or nanohybrid composites in class III restorations: Five year results. Oper. Dent. 2017, 42, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Blunck, U.; Knitter, K.; Jahn, K.R. Six-month clinical evaluation of XP BOND in noncarious cervical lesions. J. Adhes. Dent. 2007, 9, 265–268. [Google Scholar] [PubMed]
- Farias, D.C.; Lopes, G.C.; Baratieri, L.N. Two-year clinical performance of a two-step etch-and-rinse adhesive in non-carious cervical lesions: Influence of subject’s age and dentin etching time. Clin. Oral. Investig. 2015, 19, 1867–1874. [Google Scholar] [CrossRef] [PubMed]
- Bossardi, M.; Piva, E.; Isolan, C.; Münchow, E. One-year bonding performance of one-bottle etch-and-rinse adhesives to dentin at different moisture conditions. J. Adhes. Sci. Techn. 2019, 34, 686–694. [Google Scholar] [CrossRef]
- Toledano, M.; Osorio, R.; Albaladejo, A.; Aguilera, F.S.; Tay, F.R.; Ferrari, M. Effect of cyclic loading on the microtensile bond strengths of total-etch and self-etch adhesives. Oper. Dent. 2006, 31, 25–32. [Google Scholar] [CrossRef]
- Toledano, M.; Osorio, R.; Albaladejo, A.; Aguilera, F.S.; Osorio, E. Differential effect of in vitro degradation on resin-dentin bonds produced by self-etch versus total-etch adhesives. J. Biomed. Mater. Res. A. 2006, 77, 128–135. [Google Scholar] [CrossRef]
- Schwendicke, F.; Göstemeyer, G.; Blunck, U.; Paris, S.; Hsu, L.Y.; Tu, Y.K. Directly placed restorative materials: Review and network meta-analysis. J. Dent. Res. 2016, 95, 613–622. [Google Scholar] [CrossRef]
- Furness, A.; Tadros, M.Y.; Looney, S.W.; Rueggeberg, F.A. Effect of bulk/incremental fill on internal gap formation of bulk-fill composites. J. Dent. 2014, 42, 439–449. [Google Scholar] [CrossRef] [PubMed]
- Van Dijken, J.W.; Pallesen, U. A randomized controlled three year evaluation of “bulk-filled” posterior resin restorations based on stress decreasing resin technology. Dent. Mater. 2014, 30, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Shahidi, C. Évaluation In Vitro de L’adaptation Marginale de Restaurations de Classe II en Composite Réalisées Avec Différents Systèmes de Restauration à” Contraction de Polymérisation Réduite. Ph.D. Thesis, University of Geneva, Geneva, Switzerland, 2014. [Google Scholar]
- Meereis, C.T.W.; Münchow, E.A.; de Oliveira da Rosa, W.L.; da Silva, A.F.; Piva, E. Polymerization shrinkage stress of resin-based dental materials: A systematic review and meta-analyses of composition strategies. J. Mech. Behav. Biomed. Mater. 2018, 82, 268–281. [Google Scholar] [CrossRef] [PubMed]
- Soares, C.J.; Faria-E-Silva, A.L.; Rodrigues, M.P.; Fernandes Vilela, A.B.; Pfeifer, C.S.; Tantbirojn, D.; Versluis, A. Polymerization shrinkage stress of composite resins and resin cements—What do we need to know? Braz. Oral. Res. 2017, 31, 62. [Google Scholar] [CrossRef] [PubMed]
- Tomaszewska, I.M.; Kearns, J.O.; Ilie, N.; Fleming, G.J. Bulk fill restoratives: To cap or not to cap—that is the question? J. Dent. 2015, 43, 309–316. [Google Scholar] [CrossRef]
- Durán Ojeda, G.; Henríquez Gutiérrez, I.; Tisi, J.P.; Báez Rosales, A. A novel technique for bulk-fill resin-based restorations: Achieving function and esthetics in posterior teeth. Case. Rep. Dent. 2017, 2017, 9408591. [Google Scholar] [CrossRef] [PubMed]
- Ferraris, F.; Diamantopoulou, S.; Acunzo, R.; Alcidi, R. Influence of enamel composite thickness on value, chroma and translucency of a high and a nonhigh refractive index resin composite. Int. J. Esthet. Dent. 2014, 9, 382–401. [Google Scholar]
- Engelhardt, F.; Hahnel, S.; Preis, V.; Rosentritt, M. Comparison of flowable bulk-fill and flowable resin-based composites: An in vitro analysis. Clin. Oral. Investig. 2016, 20, 2123–2130. [Google Scholar] [CrossRef]
- Abou Rjeily, P.; Abou Chedid, J.C.; Hardan, L. A randomized clinical trial of “class II” composite restorations in second temporary molars: A comparison between bulk filling and incremental filling. Trop. Dent. J. 2017, 40, 37–47. [Google Scholar]
- Pardo Díaz, C.A.; Shimokawa, C.; Sampaio, C.S.; Freitas, A.Z.; Turbino, M.L. Characterization and comparative analysis of voids in class II composite resin restorations by optical coherence tomography. Oper. Dent. 2020, 45, 71–79. [Google Scholar] [CrossRef]
- Opdam, N.J.; Roeters, J.J.; Joosten, M.; Veeke, O. Porosities and voids in class I restorations placed by six operators using a packable or syringable composite. Dent. Mater. 2002, 18, 58–63. [Google Scholar] [CrossRef]
- Ogden, A.R. Porosity in composite resins-an Achilles’ heel? J. Dent. 1985, 13, 331–340. [Google Scholar] [CrossRef]
- Opdam, N.J.; Roeters, J.J.; Peters, T.C.; Burgersdijk, R.C.; Teunis, M. Cavity wall adaptation and voids in adhesive Class I resin composite restorations. Dent. Mater. 1996, 12, 230–235. [Google Scholar] [CrossRef]
- Ironside, J.G.; Makinson, O.F. Resin restorations: Causes of porosities. Quintessence. Int. 1993, 24, 867–873. [Google Scholar] [PubMed]
- Mulder, R.; Mohammed, N.; Du Plessis, A.; Le Roux, S.G. A pilot study investigating the presence of voids in bulk fill flowable composites. S. Afr. Dent. J. 2017, 72, 462–465. [Google Scholar] [CrossRef][Green Version]
- Almeida, L.J.D.S., Jr.; Penha, K.J.S.; Souza, A.F.; Lula, E.C.O.; Magalhães, F.C.; Lima, D.M.; Firoozmand, L.M. Is there correlation between polymerization shrinkage, gap formation, and void in bulk fill composites? A μCT study. Braz. Oral. Res. 2017, 31, 100. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Reis, A.F.; Vestphal, M.; Amaral, R.C.D.; Rodrigues, J.A.; Roulet, J.F.; Roscoe, M.G. Efficiency of polymerization of bulk-fill composite resins: A systematic review. Braz. Oral. Res. 2017, 31, 59. [Google Scholar] [CrossRef]
- Oliveira, F.G.; Anchieta, R.B.; Rahal, V.; de Alexandre, R.S.; Machado, L.S.; Sundefeld, M.L.; Giannini, M.; Sundfeld, R.H. Correlation of the hybrid layer thickness and resin tags length with the bond strength of a self-etching adhesive system. Acta. Odontol. Latinoam. 2009, 22, 177–181. [Google Scholar]
- Rahal, V.; de Oliveira, F.G.; Briso, A.L.; dos Santos, P.H.; Sundefeld, M.L.; Sundfeld, R.H. Correlation between hybrid layer thickness, resin tag length and microtensile bond strength of a self-etching adhesive system. Acta. Odontol. Latinoam. 2012, 25, 231–237. [Google Scholar]
- Van Meerbeek, B.; Peumans, M.; Poitevin, A.; Mine, A.; Van Ende, A.; Neves, A.; De Munck, J. Relationship between bond-strength tests and clinical outcomes. Dent. Mater. 2010, 26, 100–121. [Google Scholar] [CrossRef]
- Çakır, N.N.; Demirbuga, S. The effect of five different universal adhesives on the clinical success of class I restorations: 24-month clinical follow-up. Clin. Oral. Investig. 2019, 23, 2767–2776. [Google Scholar] [CrossRef] [PubMed]
- Van Meerbeek, B.; Dhem, A.; Goret-Nicaise, M.; Braem, M.; Lambrechts, P.; VanHerle, G. Comparative SEM and TEM examination of the ultrastructure of the resin-dentin interdiffusion zone. J. Dent. Res. 1993, 72, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Rosales-Leal, J.I.; de la Torre-Moreno, F.J.; Bravo, M. Effect of pulp pressure on the micropermeability and sealing ability of etch & rinse and self-etching adhesives. Oper. Dent. 2007, 32, 242–250. [Google Scholar] [CrossRef]
- Zecin-Deren, A.; Sokolowski, J.; Szczesio-Wlodarczyk, A.; Piwonski, I.; Lukomska-Szymanska, M.; Lapinska, B. Multi-layer application of self-etch and universal adhesives and the effect on dentin bond strength. Molecules 2019, 24, 345. [Google Scholar] [CrossRef]
- Rodrigues, N.S.; de Souza, L.C.; Feitosa, V.P.; Loguercio, A.D.; D’Arcangelo, C.; Sauro, S.; Saboia, V.D.P.A. Effect of different conditioning/deproteinization protocols on the bond strength and degree of conversion of self-adhesive resin cements applied to dentin. Int. J. Adh. Adh. 2018, 81, 98–104. [Google Scholar] [CrossRef]
- Kharouf, N.; Ashi, T.; Eid, A.; Maguina, L.; Zghal, J.; Sekayan, N.; Bourgi, R.; Hardan, L.; Sauro, S.; Haikel, Y.; et al. Does adhesive layer thickness and tag length influence short/long-term bond strength of universal adhesive systems? An in-vitro study. Appl. Sci. 2021, 11, 2635. [Google Scholar] [CrossRef]
- Scholz, K.J.; Hinderberger, M.; Widbiller, M.; Federlin, M.; Hiller, K.A.; Buchalla, W. Influence of selective caries excavation on marginal penetration of class II composite restorations in vitro. Eur. J. Oral. Sci. 2020, 128, 405–414. [Google Scholar] [CrossRef]
- Haak, R.; Siegner, J.; Ziebolz, D.; Blunck, U.; Fischer, S.; Hajtó, J.; Frankenberger, R.; Krause, F.; Schneider, H. OCT evaluation of the internal adaptation of ceramic veneers depending on preparation design and ceramic thickness. Dent. Mater. 2021, 37, 423–431. [Google Scholar] [CrossRef]
- Scholz, K.J.; Bittner, A.; Cieplik, F.; Hiller, K.A.; Schmalz, G.; Buchalla, W.; Federlin, M. Micromorphology of the adhesive interface of self-adhesive resin cements to enamel and dentin. Materials 2021, 14, 492. [Google Scholar] [CrossRef]

| Adhesive System | Type of Adhesive | Main Components (Lot No.) |
| Prime&Bond XP (Dentsply Caulk) | Two-step etch-and-rinse | PENTA, UDMA, HEMA, TEGDMA, TCB, tert-butanol, nanofiller, camphorquinone, stabilizer (1105001715) |
| Resin Composite | Type of Resin Composite | Main Components |
| Surefil SDR flow (Dentsply DeTrey GmbH) | Bulk-fill flowable | Barium-alumino-fluoro-boro-silicate glass, strontium alumino-fluoro-silicate glass, modified urethane dimethacrylate resin, EBPADMA, TEGDMA, CQ, BHT, UV stabilizer, titanium dioxide, and iron oxide pigments (1105121) |
| Ceram X Mono (Dentsply DeTrey GmbH) | Nano-hybrid composite | BisGMA, CQ, TEGDMA, UDMA, Ba–Al–borosilicate glass, methacrylate, functionalized silicon dioxide nanofiller, iron oxide pigments, titanium oxide pigments, aluminum sulfo silicate pigments (1106000932) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hardan, L.; Lukomska-Szymanska, M.; Zarow, M.; Cuevas-Suárez, C.E.; Bourgi, R.; Jakubowicz, N.; Sokolowski, K.; D’Arcangelo, C. One-Year Clinical Aging of Low Stress Bulk-Fill Flowable Composite in Class II Restorations: A Case Report and Literature Review. Coatings 2021, 11, 504. https://doi.org/10.3390/coatings11050504
Hardan L, Lukomska-Szymanska M, Zarow M, Cuevas-Suárez CE, Bourgi R, Jakubowicz N, Sokolowski K, D’Arcangelo C. One-Year Clinical Aging of Low Stress Bulk-Fill Flowable Composite in Class II Restorations: A Case Report and Literature Review. Coatings. 2021; 11(5):504. https://doi.org/10.3390/coatings11050504
Chicago/Turabian StyleHardan, Louis, Monika Lukomska-Szymanska, Maciej Zarow, Carlos Enrique Cuevas-Suárez, Rim Bourgi, Natalia Jakubowicz, Krzysztof Sokolowski, and Camillo D’Arcangelo. 2021. "One-Year Clinical Aging of Low Stress Bulk-Fill Flowable Composite in Class II Restorations: A Case Report and Literature Review" Coatings 11, no. 5: 504. https://doi.org/10.3390/coatings11050504
APA StyleHardan, L., Lukomska-Szymanska, M., Zarow, M., Cuevas-Suárez, C. E., Bourgi, R., Jakubowicz, N., Sokolowski, K., & D’Arcangelo, C. (2021). One-Year Clinical Aging of Low Stress Bulk-Fill Flowable Composite in Class II Restorations: A Case Report and Literature Review. Coatings, 11(5), 504. https://doi.org/10.3390/coatings11050504










