Electrospun Polyethylene Terephthalate Nanofibers Loaded with Silver Nanoparticles: Novel Approach in Anti-Infective Therapy
Abstract
1. Introduction
2. Experimental Section
2.1. Materials
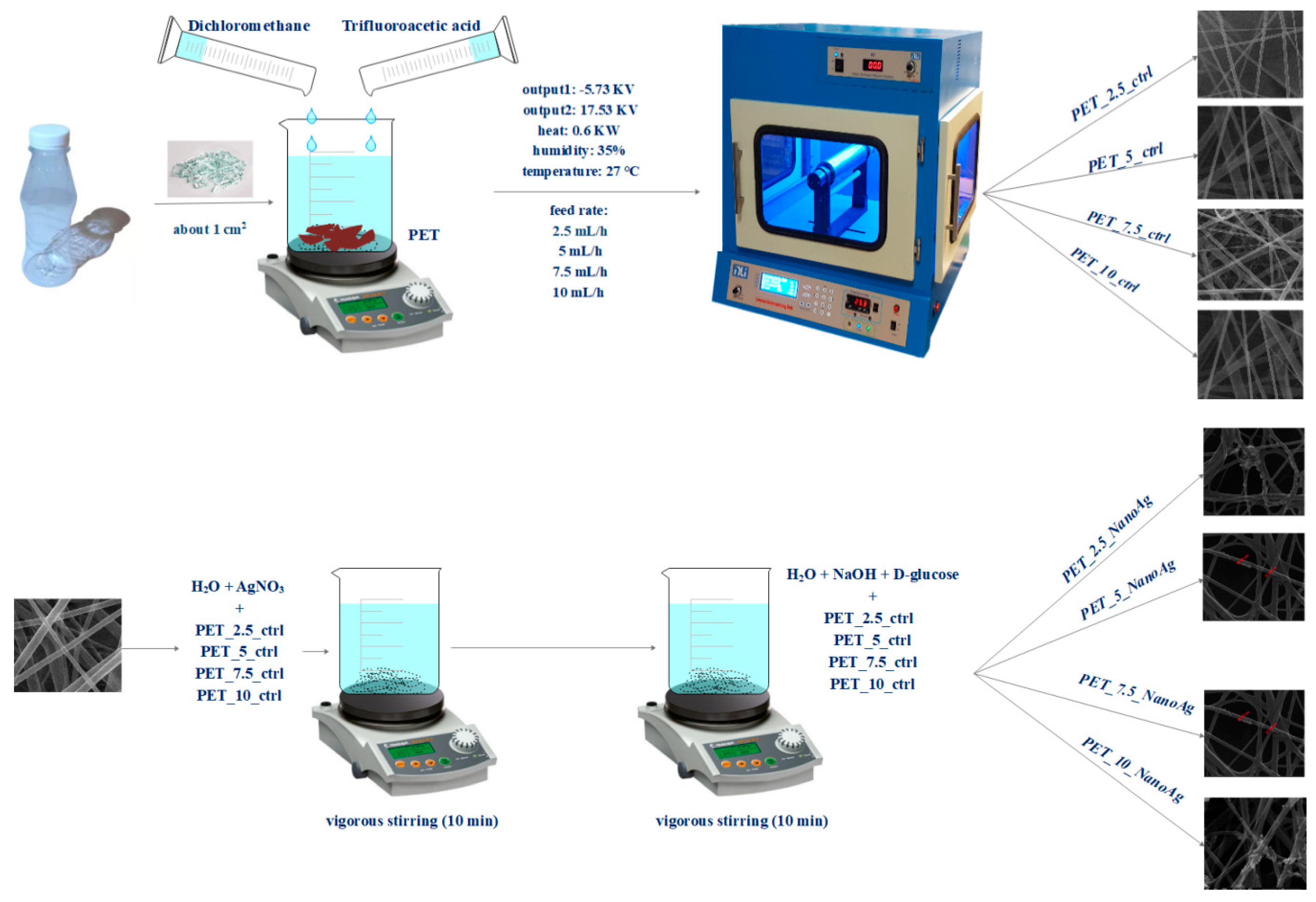
2.2. Electrospinning Deposition of PET Nanofibers
2.3. Silver Nanoparticle (NanoAg) Synthesis
2.4. Physico-Chemical Characterization
2.5. In Vitro Biocompatibility
2.5.1. Cell Line
2.5.2. MTT (3-(4,5-Dimethylthiazolyl-2)-2,5-diphenyltetrazolium bromide) Assay
2.6. In Vitro Antibacterial Tests
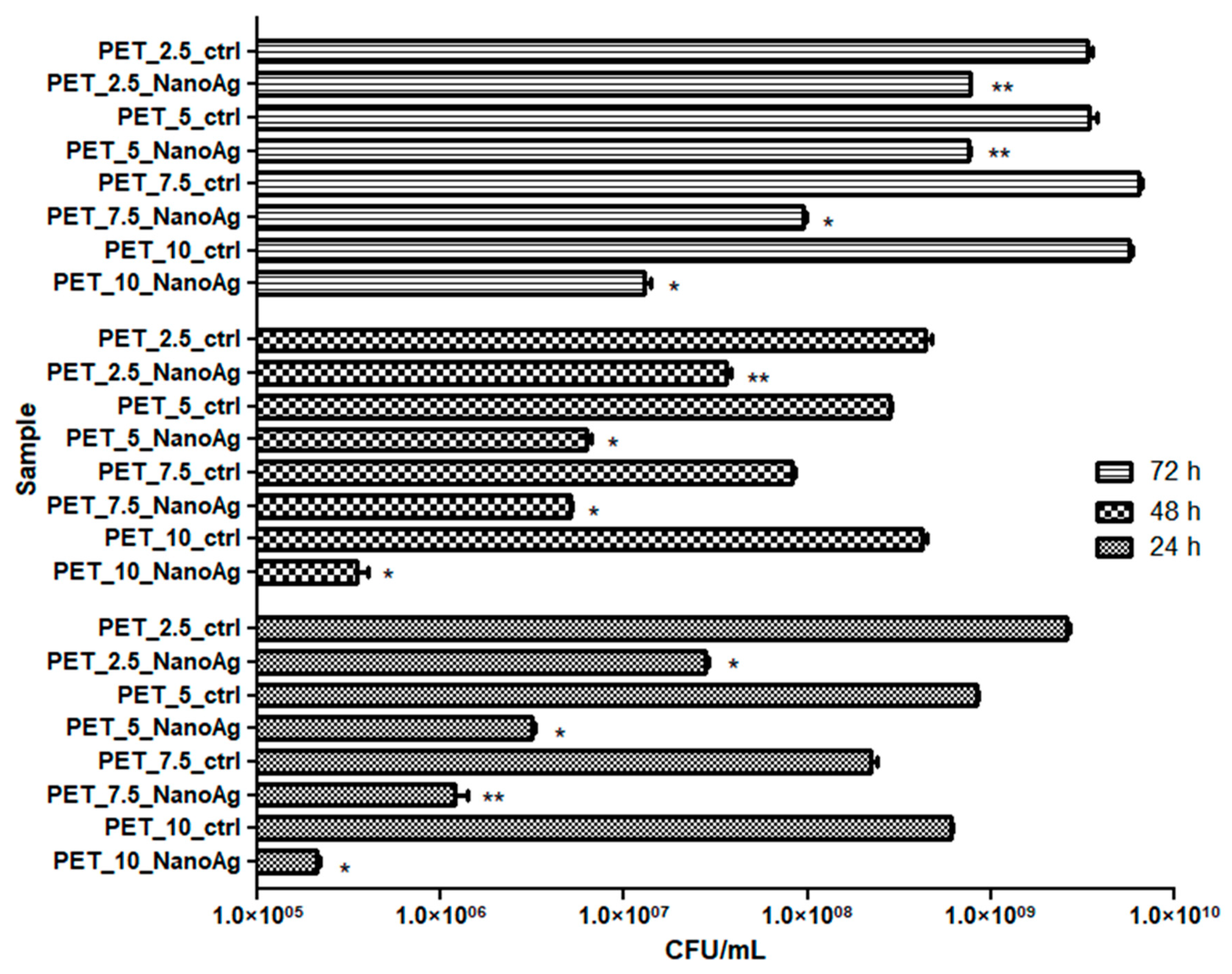
2.6.1. Growth of Planktonic (Floating) Microorganisms in the Presence of Material
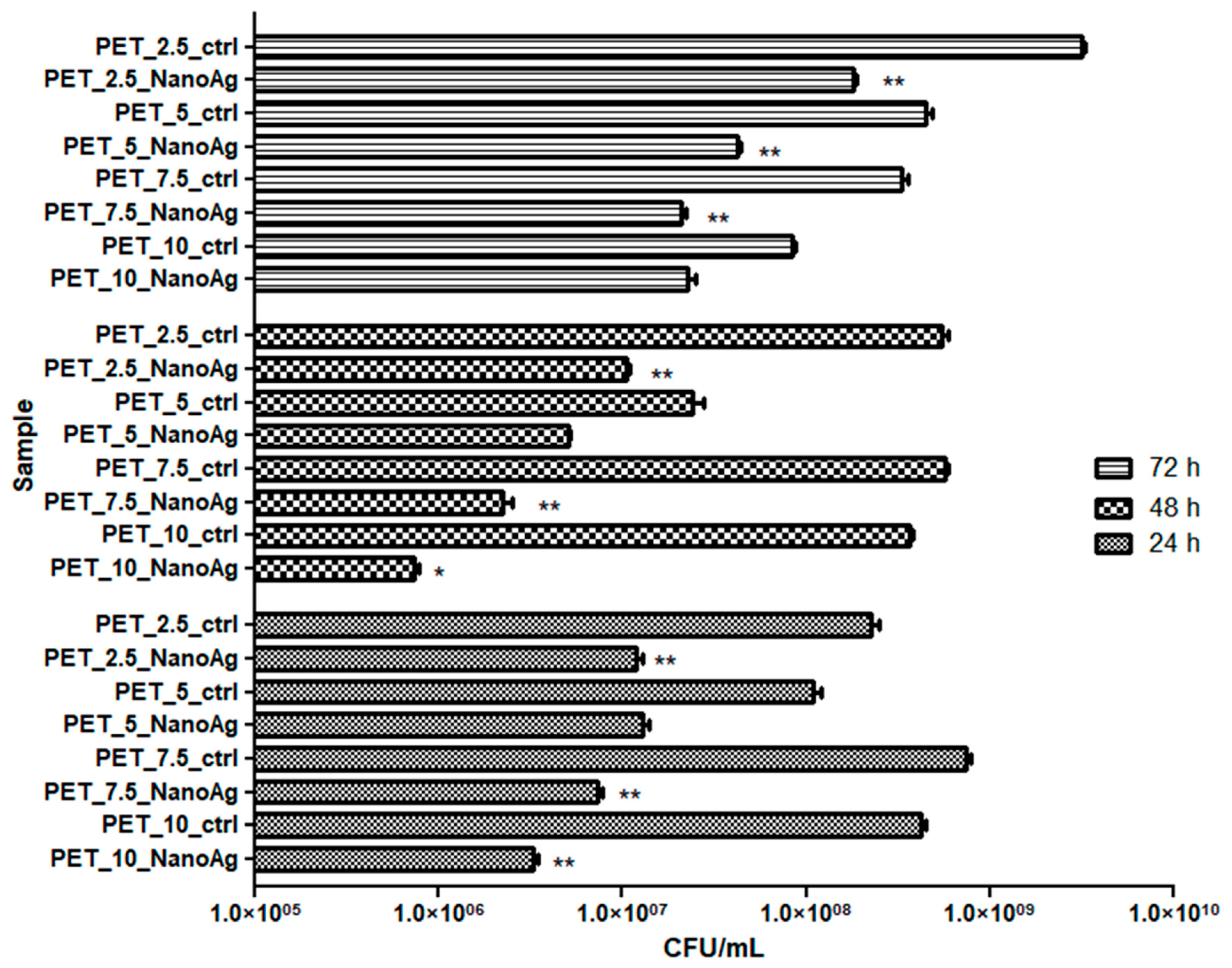
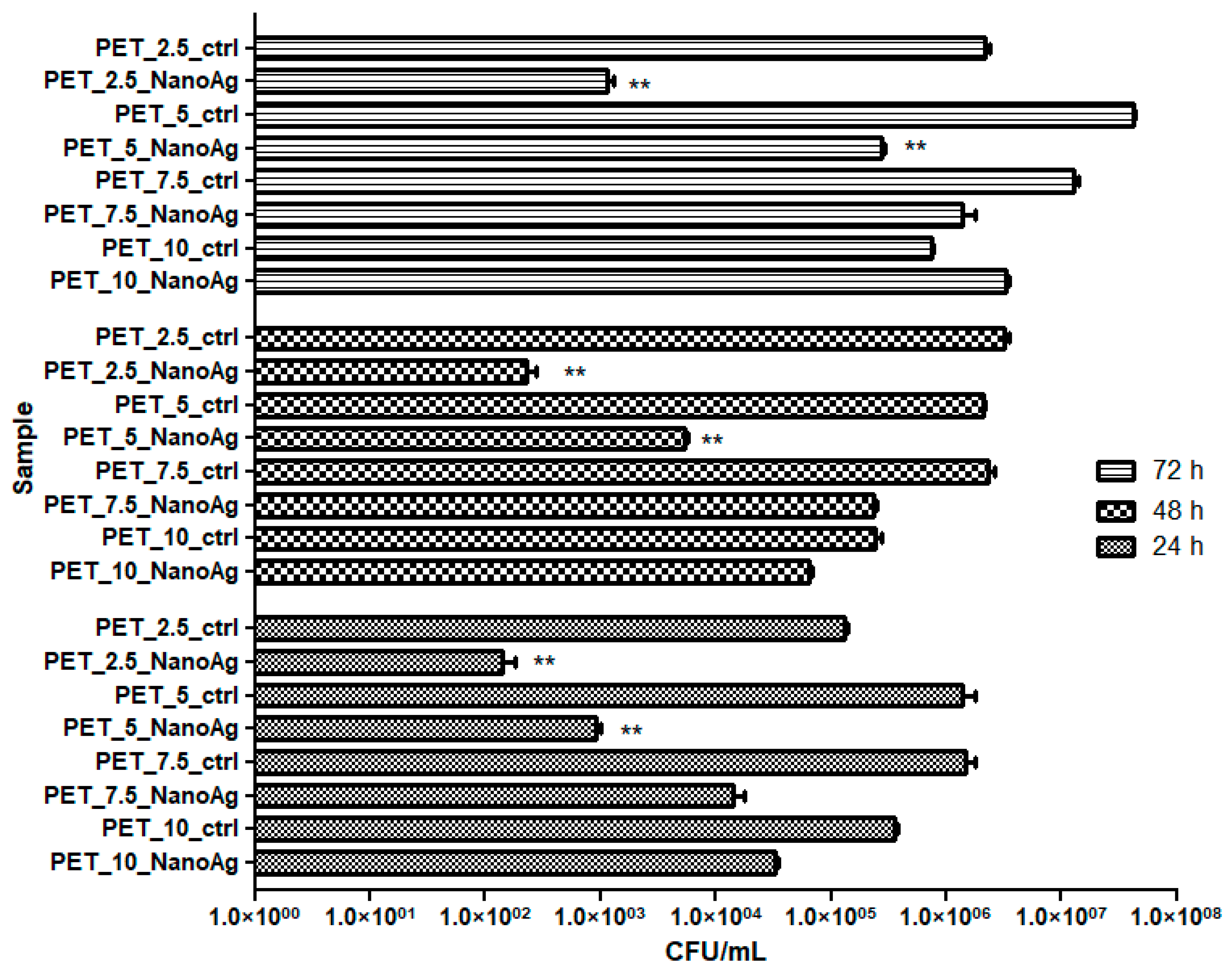
2.6.2. Evaluation of Adhesion and Biofilm Formation
2.7. In Vivo Biocompatibility Evaluation
2.7.1. Animals and Ethics
2.7.2. Experimental Design and Surgical Procedures
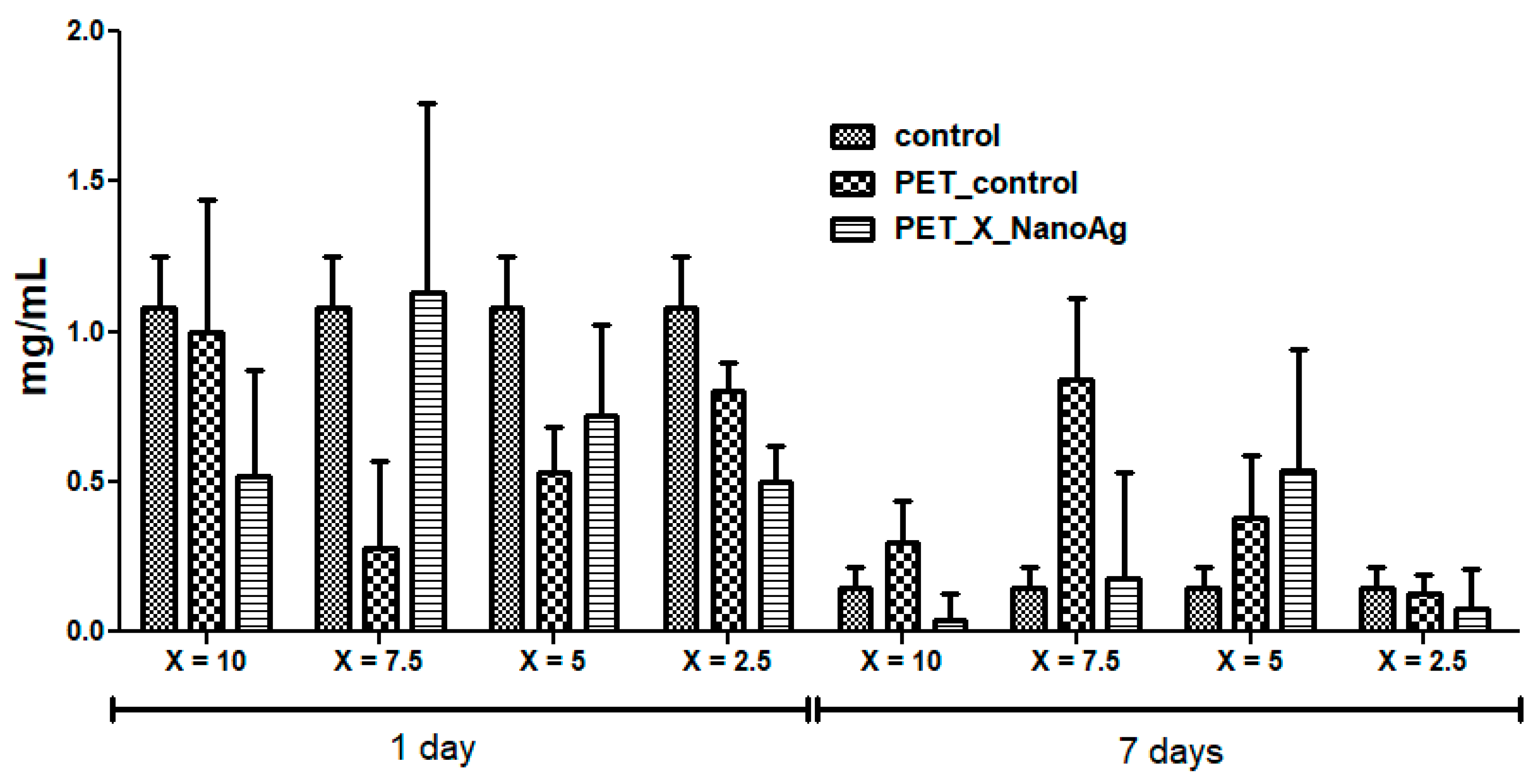
2.7.3. Biochemical Analysis
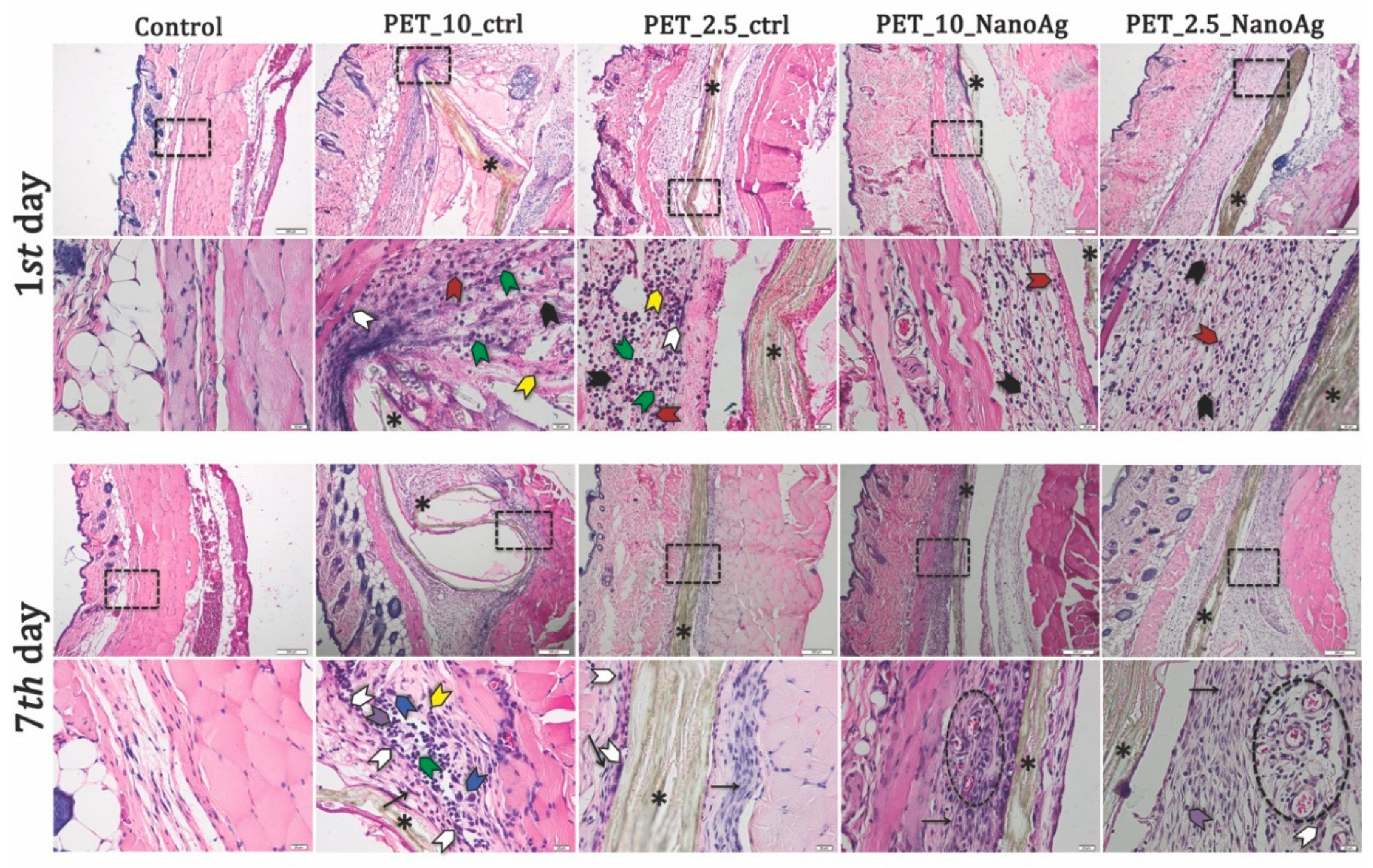
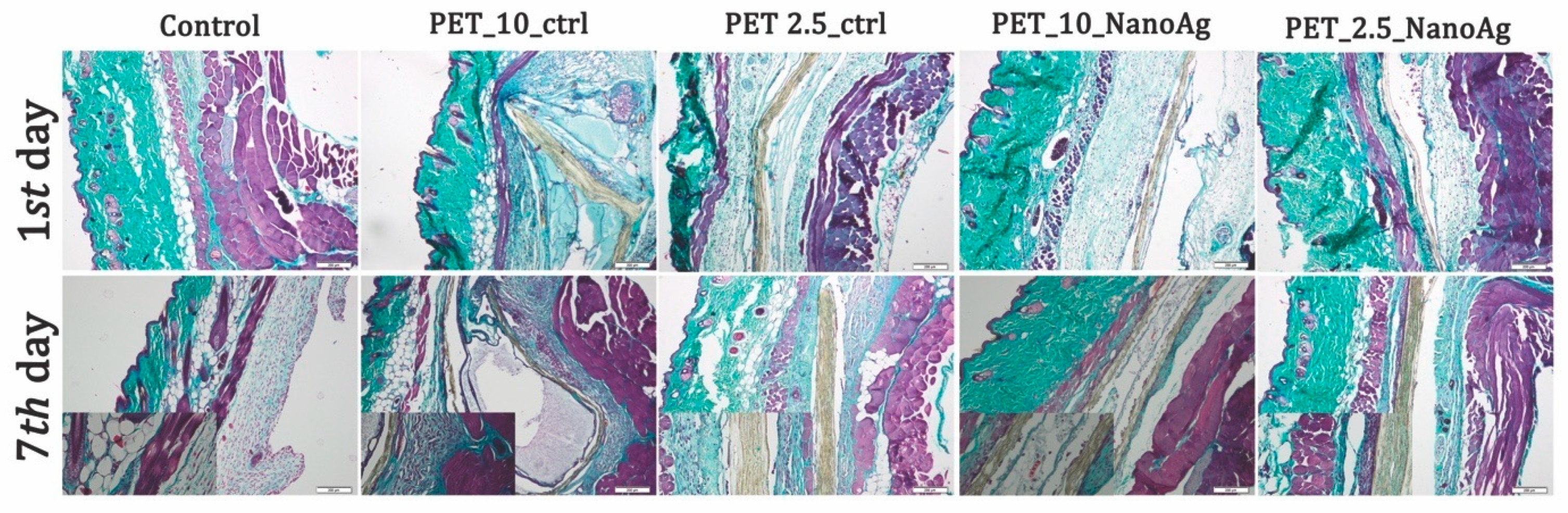
2.7.4. Histopathological Analysis
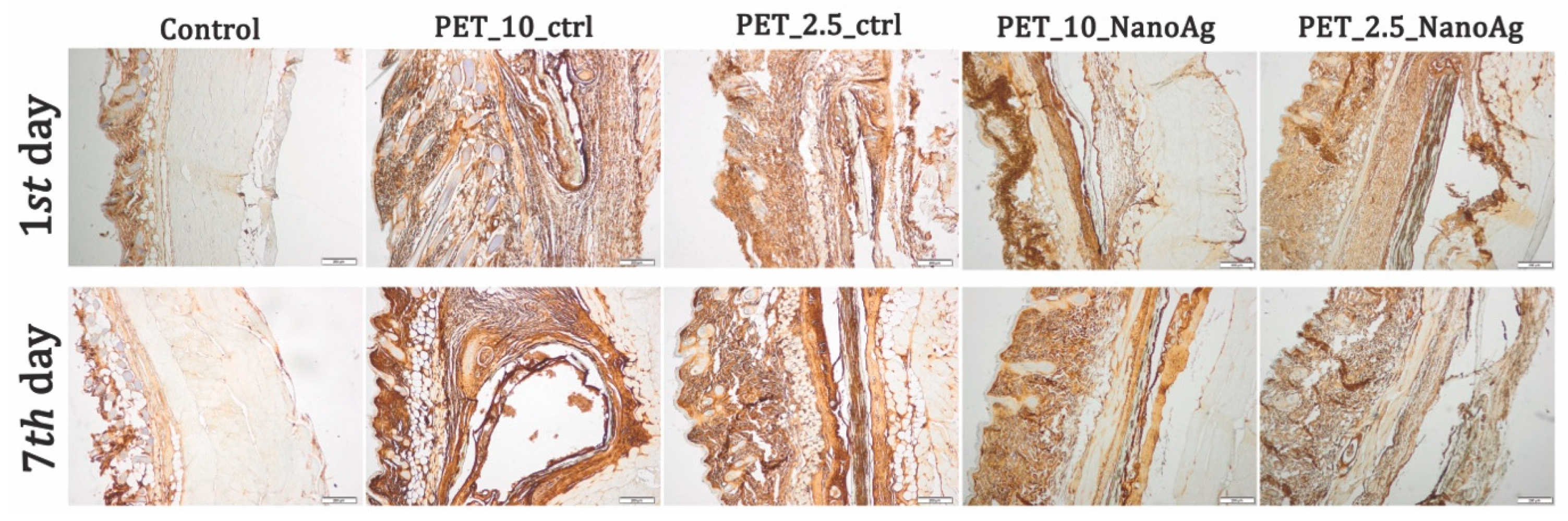
2.7.5. Immunohistochemistry
2.8. Statistical Analysis
3. Results
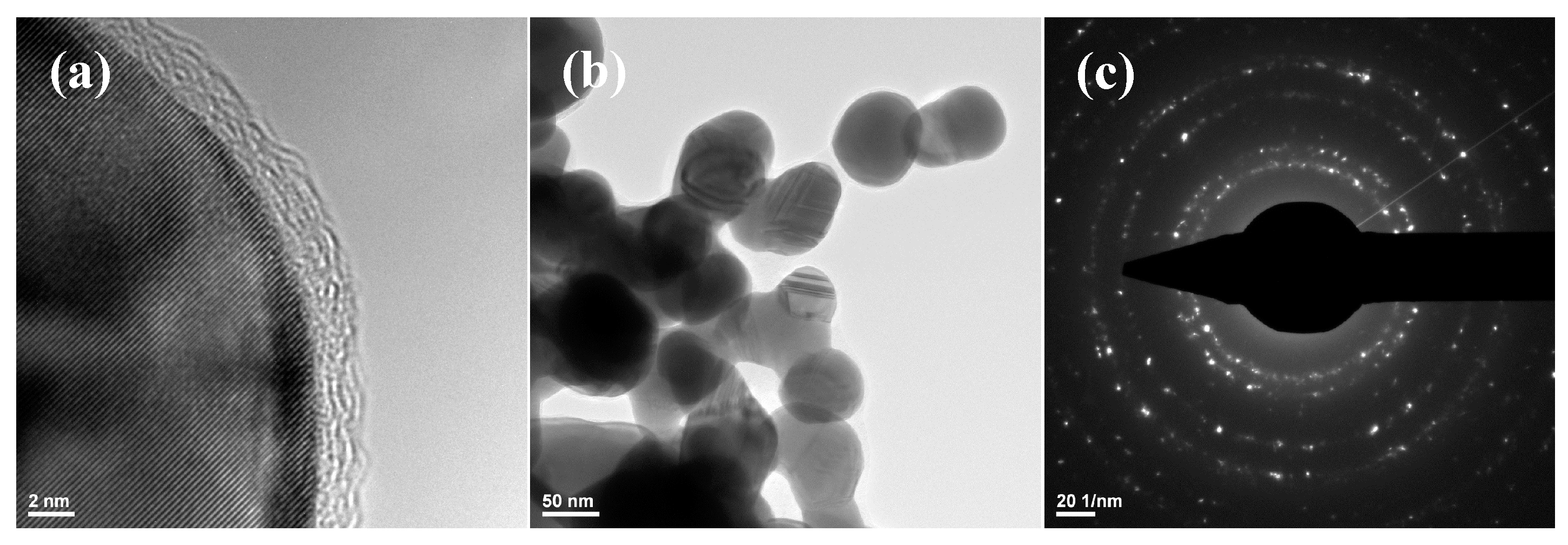
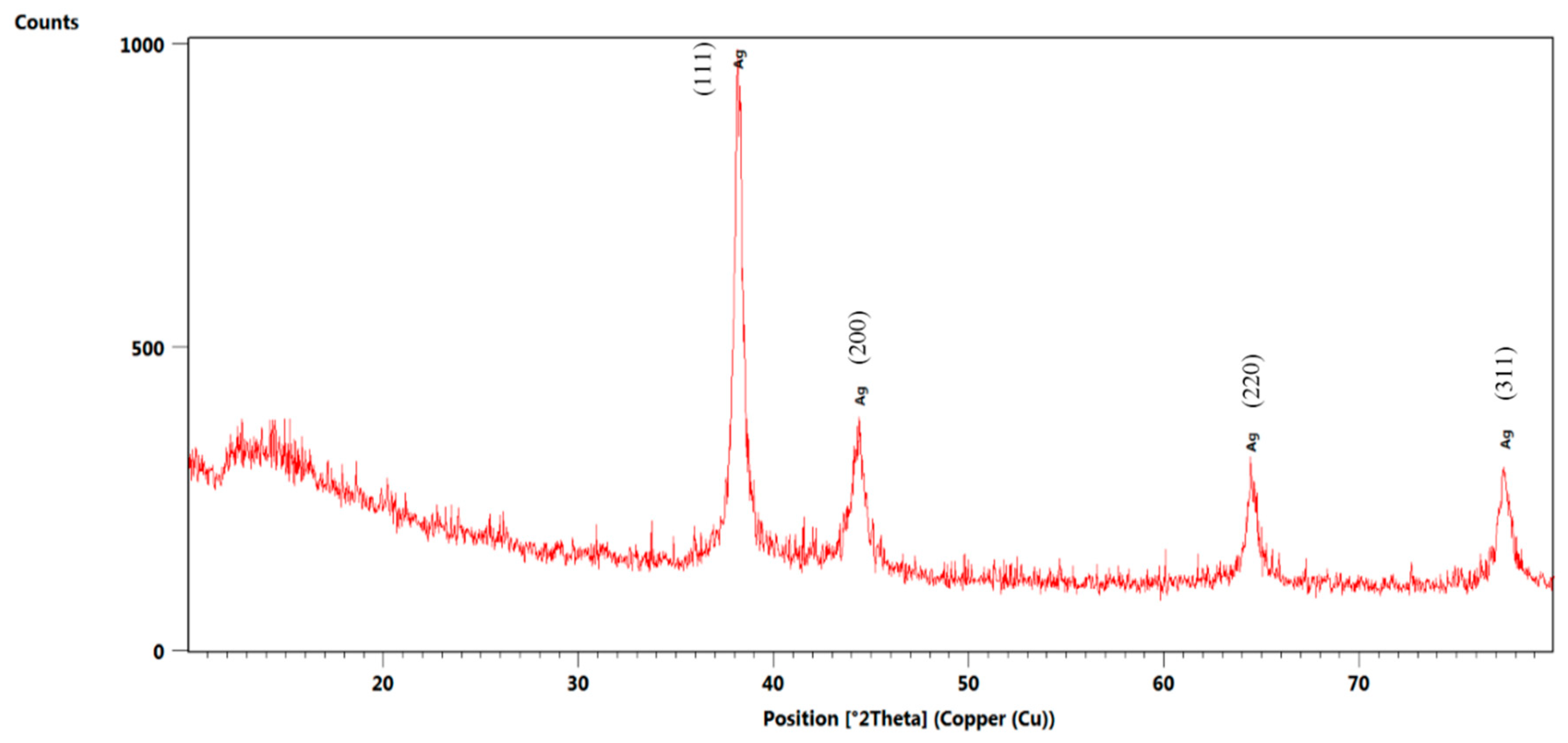
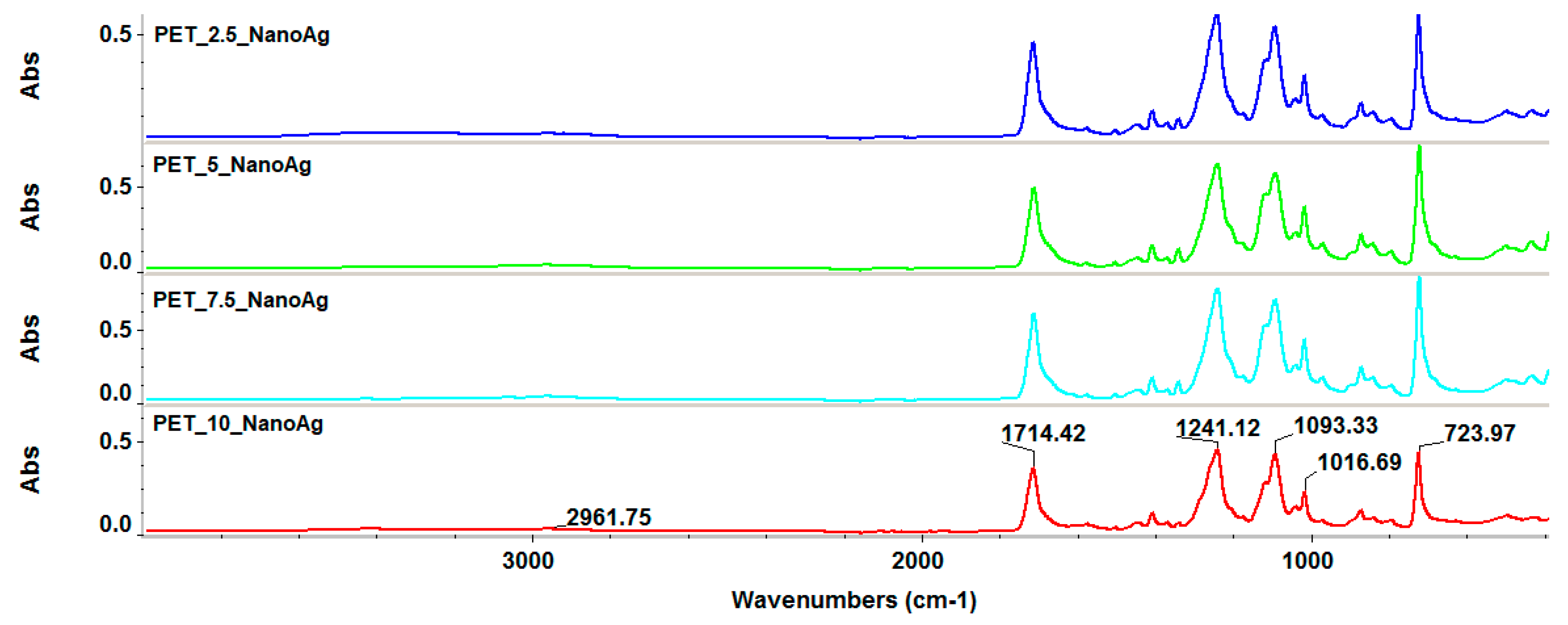
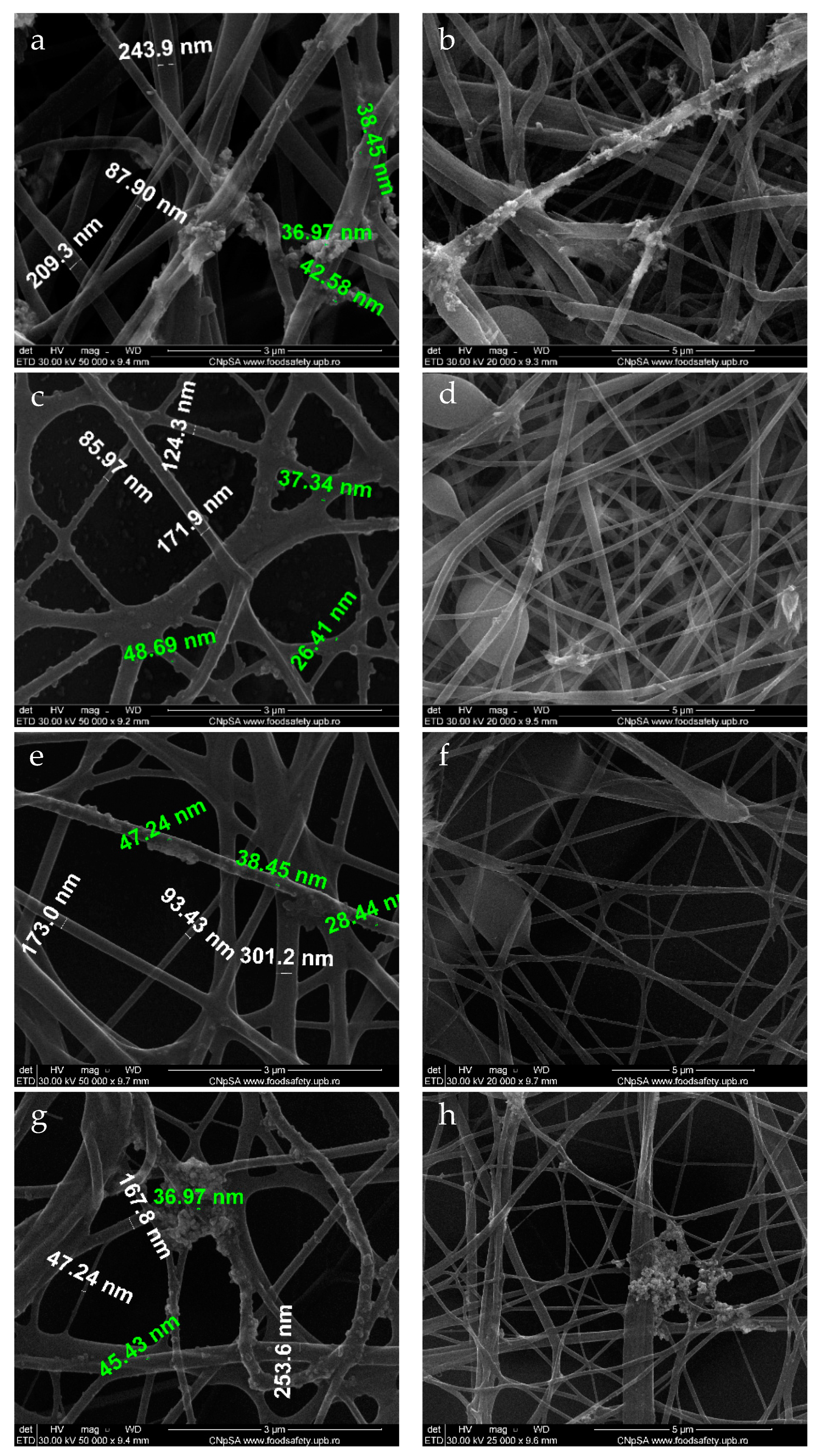
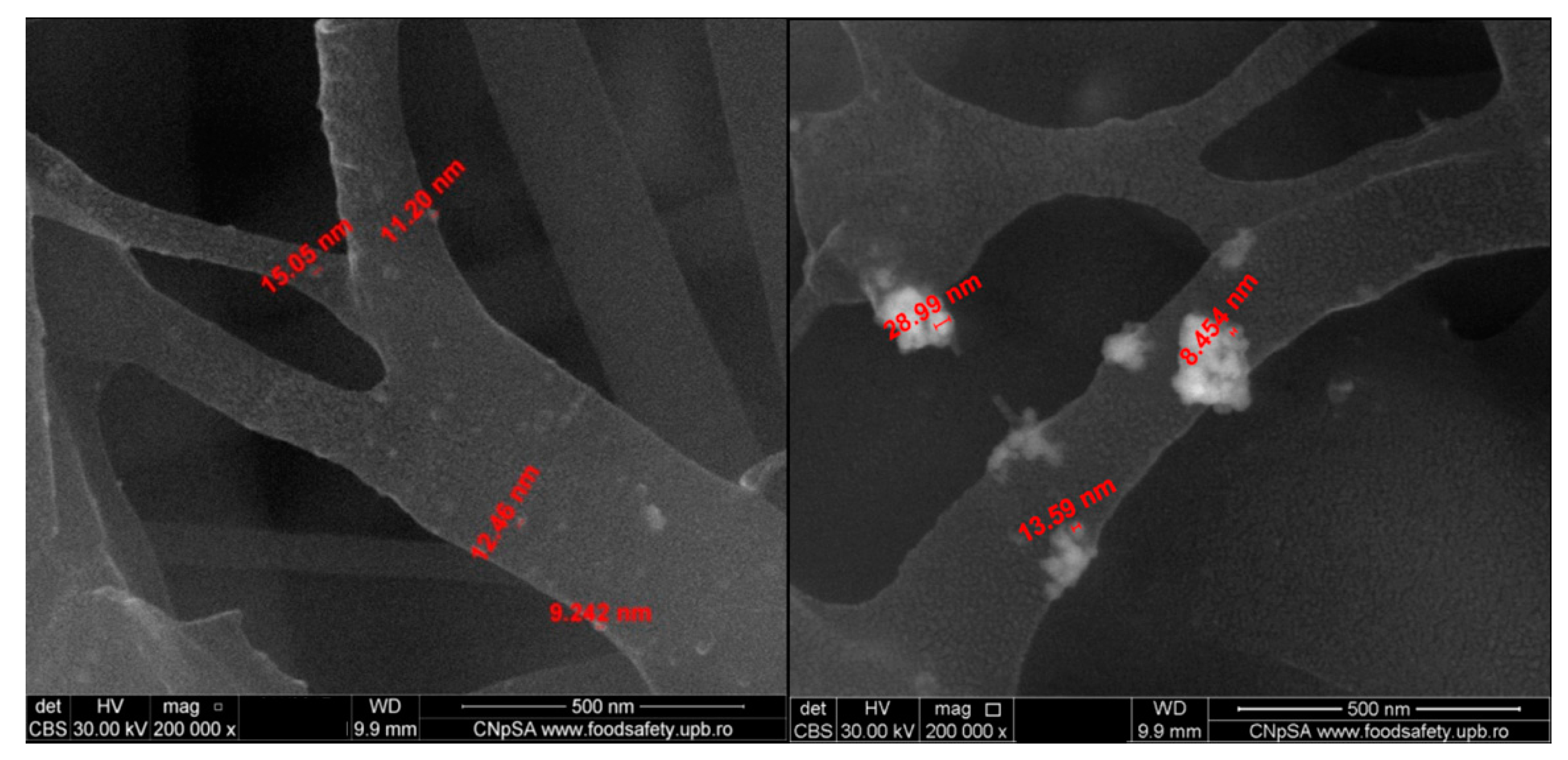
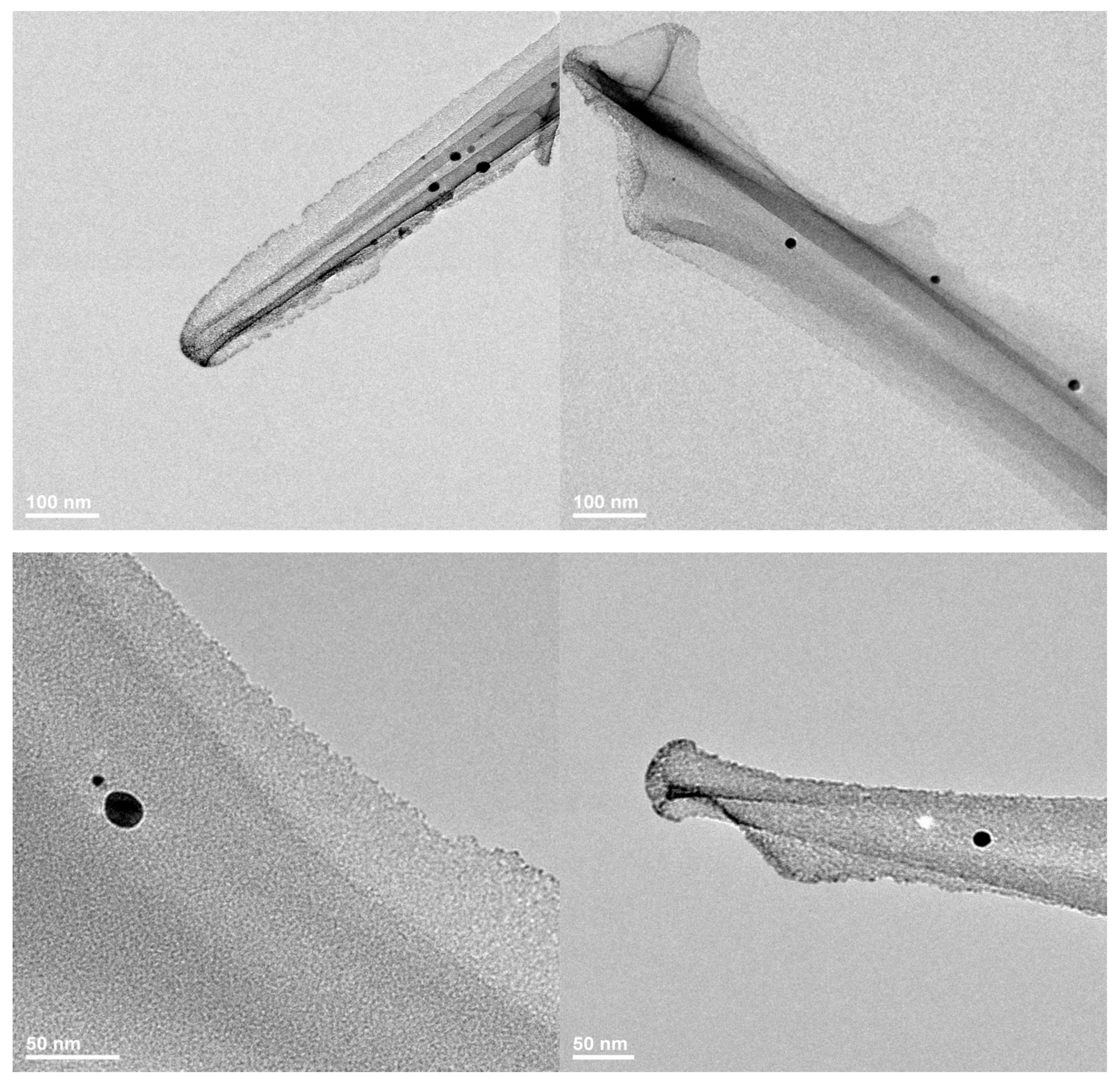
3.1. Characterization of the Obtained Materials
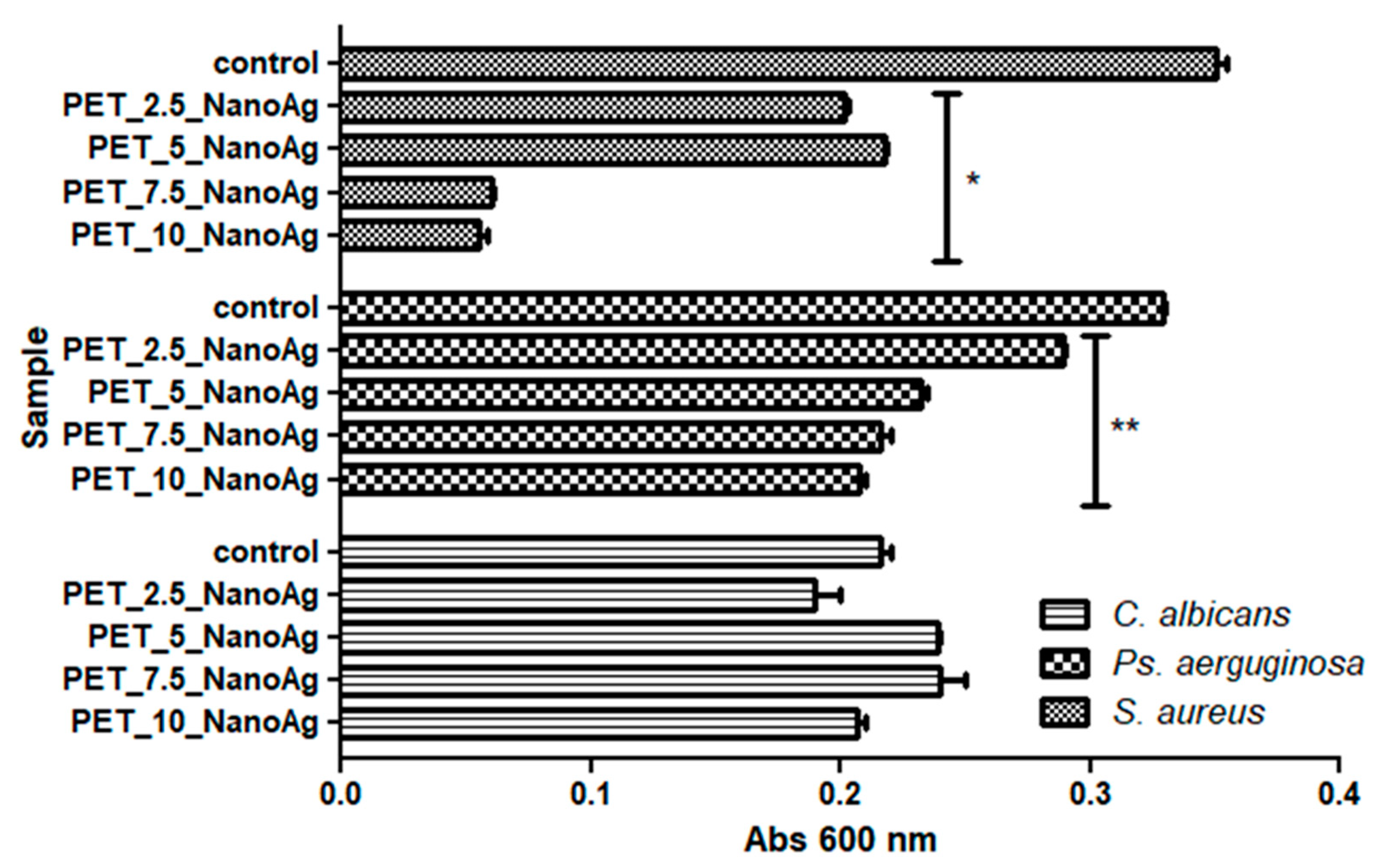
3.2. Antimicrobial Properties of the Prepared Samples
3.3. In Vitro and In Vivo Biological Response
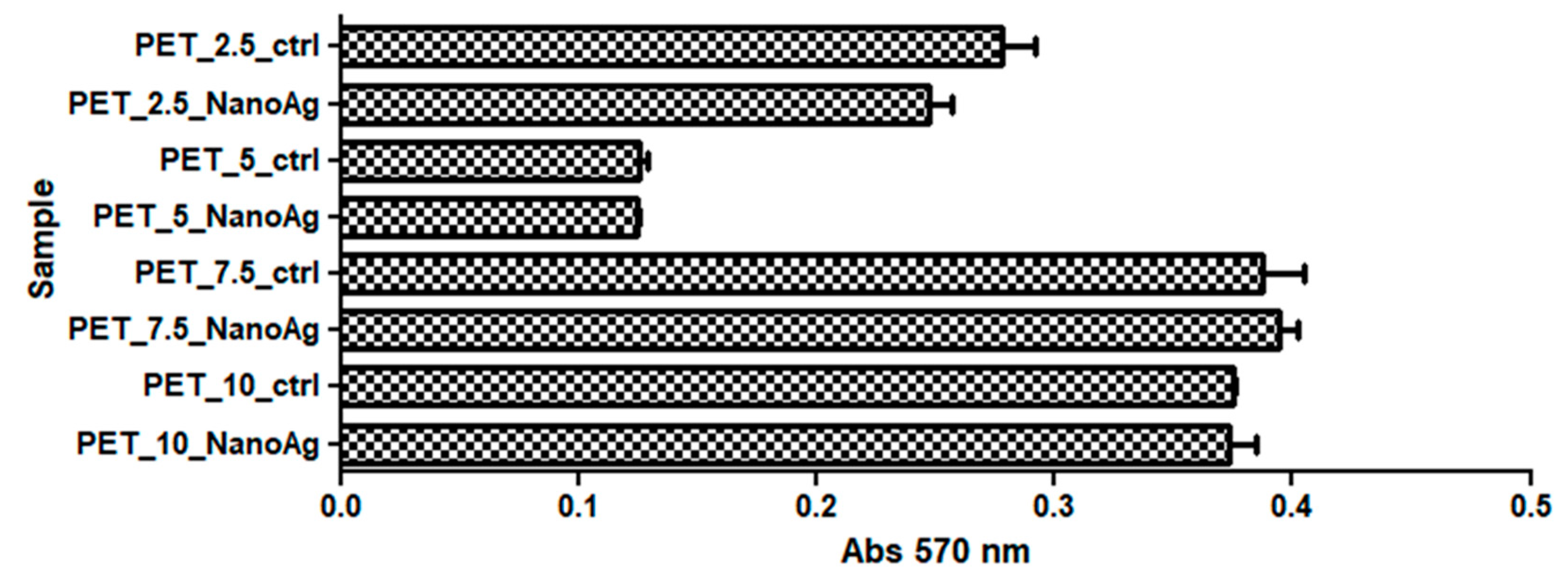
3.3.1. In Vitro Biocompatibility
3.3.2. In Vivo Biocompatibility and Inflammatory Response
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Lu, P.; Ding, B. Applications of electrospun fibers. Recent Pat. Nanotechnol. 2008, 2, 169–182. [Google Scholar] [CrossRef] [PubMed]
- Naghibzadeh, M.; Firoozi, S.; Nodoushan, F.S.; Adabi, M.; Khoradmehr, A.; Fesahat, F.; Esnaashari, S.S.; Khosravani, M.; Adabi, M.; Tavakol, S.; et al. Application of electrospun gelatin nanofibers in tissue engineering. Biointerface Res. Appl. Chem. 2018, 8, 3048–3052. [Google Scholar]
- Teleanu, R.I.; Gherasim, O.; Gherasim, T.G.; Grumezescu, V.; Grumezescu, A.M.; Teleanu, D.M. Nanomaterial-based approaches for neural regeneration. Pharmaceutics 2019, 11, 266. [Google Scholar] [CrossRef] [PubMed]
- Huang, Z.-M.; Zhang, Y.Z.; Kotaki, M.; Ramakrishna, S. A review on polymer nanofibers by electrospinning and their applications in nanocomposites. Compos. Sci. Technol. 2003, 63, 2223–2253. [Google Scholar] [CrossRef]
- Zhang, M.; Zhao, X.; Zhang, G.; Wei, G.; Su, Z. Electrospinning design of functional nanostructures for biosensor applications. J. Mater. Chem. B 2017, 5, 1699–1711. [Google Scholar] [CrossRef]
- Shi, X.; Zhou, W.; Ma, D.; Ma, Q.; Bridges, D.; Ma, Y.; Hu, A. Electrospinning of nanofibers and their applications for energy devices. J. Nanomater. 2015, 16, 122. [Google Scholar] [CrossRef]
- Ray, S.S.; Chen, S.-S.; Li, C.-W.; Nguyen, N.C.; Nguyen, H.T. A comprehensive review: Electrospinning technique for fabrication and surface modification of membranes for water treatment application. RSC Adv. 2016, 6, 85495–85514. [Google Scholar] [CrossRef]
- Özçam, A.E.; Roskov, K.E.; Spontak, R.J.; Genzer, J. Generation of functional pet microfibers through surface-initiated polymerization. J. Mater. Chem. 2012, 22, 5855–5864. [Google Scholar] [CrossRef]
- Mahendrasingam, A.; Martin, C.; Fuller, W.; Blundell, D.J.; Oldman, R.J.; MacKerron, D.H.; Harvie, J.L.; Riekel, C. Observation of a transient structure prior to strain-induced crystallization in poly(ethylene terephthalate). Polymer 2000, 41, 1217–1221. [Google Scholar] [CrossRef]
- Monier, M.; Abdel-Latif, D. Synthesis and characterization of ion-imprinted chelating fibers based on pet for selective removal of hg2+. Chem. Eng. J. 2013, 122, 452–460. [Google Scholar] [CrossRef]
- Ma, Z.; Kotaki, M.; Yong, T.; He, W.; Ramakrishna, S. Surface engineering of electrospun polyethylene terephthalate (pet) nanofibers towards development of a new material for blood vessel engineering. Biomaterials 2005, 26, 2527–2536. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Li, Y.; Ding, G.; Xie, X.; Jiang, M. Preparation and characterization of graphene oxide/poly(vinyl alcohol) composite nanofibers via electrospinning. J. Appl. Polym. Sci. 2013, 127, 3026–3032. [Google Scholar] [CrossRef]
- Huang, J.; Liu, Y.; You, T. Carbon nanofiber based electrochemical biosensors: A review. Anal. Methods 2010, 2, 202–211. [Google Scholar] [CrossRef]
- Klinge, U.; Park, J.-K.; Klosterhalfen, B. The ideal mesh. Pathobiology 2013, 80, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Longo, U.G.; Lamberti, A.; Maffulli, N.; Denaro, V. Tendon augmentation grafts: A systematic review. Br. Med. Bull. 2010, 94, 165–188. [Google Scholar] [CrossRef] [PubMed]
- Kannan, R.Y.; Salacinski, H.J.; Butler, P.E.; Hamilton, G.; Seifalian, A.M. Current status of prosthetic bypass grafts: A review. J. Biomed. Mater. Res. Part B Appl. Biomater. 2005, 74, 570–581. [Google Scholar] [CrossRef] [PubMed]
- Mansour, S.H.; Ikladious, N.E. Depolymerization of poly(ethylene terephthalate) waste using 1,4-butanediol and triethylene glycol. J. Elastomers Plast. 2003, 35, 133–148. [Google Scholar] [CrossRef]
- Abbas, J.A.; Said, I.A.; Mohamed, M.A.; Yasin, S.A.; Ali, Z.A.; Ahmed, I.H. Electrospinning of polyethylene terephthalate (pet) nanofibers: Optimization study using taguchi design of experiment. IOP Conf. Ser. Mater. Sci. Eng. 2018, 454, 012130. [Google Scholar] [CrossRef]
- Esmaeili, E.; Deymeh, F.; Rounaghi, S.A. Synthesis and characterization of the electrospun fibers prepared from waste polymeric materials. Int. J. Nano Dimens. 2017, 8, 171–181. [Google Scholar]
- Zander, N.E.; Gillan, M.; Sweetser, D. Recycled pet nanofibers for water filtration applications. Materials 2016, 9, 247. [Google Scholar] [CrossRef]
- Sereshti, H.; Amini, F.; Najarzadekan, H. Electrospun polyethylene terephthalate (pet) nanofibers as a new adsorbent for micro-solid phase extraction of chromium(vi) in environmental water samples. RSC Adv. 2015, 5, 89195–89203. [Google Scholar] [CrossRef]
- Jhass, P.; Siaw-Sakyi, V.; Wild, T. Wound infection risk evaluation—A new prediction score—Wire. Wound Med. 2017, 16, 34–39. [Google Scholar] [CrossRef]
- Ditaranto, N.; Basoli, F.; Trombetta, M.; Cioffi, N.; Rainer, A. Electrospun nanomaterials implementing antibacterial inorganic nanophases. Appl. Sci. 2018, 8, 1643. [Google Scholar] [CrossRef]
- Armentano, I.; Arciola, C.R.; Fortunati, E.; Ferrari, D.; Mattioli, S.; Amoroso, C.F.; Rizzo, J.; Kenny, J.M.; Imbriani, M.; Visai, L. The interaction of bacteria with engineered nanostructured polymeric materials: A review. Sci. World J. 2014, 2014, 410423. [Google Scholar] [CrossRef] [PubMed]
- Bahrami, M.K.; Movafeghi, A.; Mahdavinia, G.R.; Hassanpouraghdam, M.B.; Gohari, G. Effects of bare and chitosan-coated Fe3O4 magnetic nanoparticles on seed germination and seedling growth of capsicum annuum L. Res. Appl. Chem. 2018, 8, 3552–3559. [Google Scholar]
- Narasaiah, B.P.; Mandal, B.K.; Chakravarthula, S.N. Mitigation of textile industries generated pollution by agro-waste cotton peels mediated synthesized silver nanoparticles. Biointerface Res. Appl. Chem. 2018, 8, 3602–3610. [Google Scholar]
- Sabry, N.M.; Tolba, S.; Abdel-Gawad, F.K.; Bassem, S.M.; Nassar, H.F.; El-Taweel, G.E.; Okasha, A.; Ibrahim, M. Interaction between nano silver and bacteria: Modeling approach. Biointerface Res. Appl. Chem. 2018, 8, 3570–3574. [Google Scholar]
- Samoilova, N.A.; Krayukhina, M.A.; Popov, D.A.; Anuchina, N.M.; Piskarev, V.E. 3′-sialyllactose-decorated silver nanoparticles: Lectin binding and bactericidal properties. Biointerface Res. Appl. Chem. 2018, 8, 3095–3099. [Google Scholar]
- Teleanu, D.M.; Chircov, C.; Grumezescu, A.M.; Teleanu, R.I. Neurotoxicity of nanomaterials: An up-to-date overview. Nanomaterials 2019, 9, 96. [Google Scholar] [CrossRef]
- Teleanu, D.M.; Chircov, C.; Grumezescu, A.M.; Volceanov, A.; Teleanu, R.I. Impact of nanoparticles on brain health: An up to date overview. J. Clin. Med. 2018, 7, 490. [Google Scholar] [CrossRef]
- Wan, Y.Z.; Raman, S.; He, F.; Huang, Y. Surface modification of medical metals by ion implantation of silver and copper. Vacuum 2007, 81, 1114–1118. [Google Scholar] [CrossRef]
- You, C.; Han, C.; Wang, X.; Zheng, Y.; Li, Q.; Hu, X.; Sun, H. The progress of silver nanoparticles in the antibacterial mechanism, clinical application and cytotoxicity. Mol. Biol. Rep. 2012, 39, 9193–9201. [Google Scholar] [CrossRef]
- Sharma, N.; Phutela, K.; Goel, A.; Soni, S.; Batra, N. Exploring the bacterial based silver nanoparticle for their possible application as disinfectants. Biointerface Res. Appl. Chem. 2018, 8, 3100–3104. [Google Scholar]
- Choi, O.; Deng, K.K.; Kim, N.J.; Ross, L., Jr.; Surampalli, R.Y.; Hu, Z. The inhibitory effects of silver nanoparticles, silver ions, and silver chloride colloids on microbial growth. Water Res. 2008, 42, 3066–3074. [Google Scholar] [CrossRef] [PubMed]
- Song, K.; Wu, Q.; Qi, Y.; Kärki, T. 20-electrospun nanofibers with antimicrobial properties. In Electrospun Nanofibers; Afshari, M., Ed.; Woodhead Publishing: Sawston, UK, 2017; pp. 551–569. [Google Scholar]
- Zargham, S.; Bazgir, S.; Tavakoli, A.; Rashidi, A.S.; Damerchely, R. The effect of flow rate on morphology and deposition area of electrospun nylon 6 nanofiber. J. Eng. Fibers Fabr. 2012, 7. [Google Scholar] [CrossRef]
- Bakar, S.S.S.; Fong, K.C.; Eleyas, A.; Nazeri, M.F.M. Effect of voltage and flow rate electrospinning parameters on polyacrylonitrile electrospun fibers. IOP Conf. Ser. Mater. Sci. Eng. 2018, 318, 012076. [Google Scholar] [CrossRef]
- Khelissa, O.; Abdallah, M.; Jama, C.; Faille, C.; Chihib, N.-E. Bacterial contamination and biofilm formation on abiotic surfaces and strategies to overcome their persistence. J. Mater. Environ. Sci. 2017, 8, 3326–3346. [Google Scholar]
- Sadikot, R.T.; Blackwell, T.S.; Christman, J.W.; Prince, A.S. Pathogen-host interactions in pseudomonas aeruginosa pneumonia. Am. J. Respir. Crit. Care Med. 2005, 171, 1209–1223. [Google Scholar] [CrossRef]
- Balta, C.; Herman, H.; Rosu, M.; Cotoraci, C.; Ivan, A.; Folk, A.; Duka, R.; Dinescu, S.; Costache, M.; Alexandru, P.; et al. Homeostasis of blood parameters and inflammatory markers analysis during bone defect healing after scaffolds implantation in mice calvaria defects. Rom. Biotechnol. Lett. 2016, 22, 12018–12025. [Google Scholar]
- Romero-Gavilan, F.; Sanchez-Perez, A.M.; Araujo-Gomes, N.; Azkargorta, M.; Iloro, I.; Elortza, F.; Gurruchaga, M.; Goni, I.; Suay, J. Proteomic analysis of silica hybrid sol-gel coatings: A potential tool for predicting the biocompatibility of implants in vivo. Biofouling 2017, 33, 676–689. [Google Scholar] [CrossRef]
- Ratner, B.D. The Biocompatibility of Implant Materials; Elsevier: Amsterdam, The Netherlands, 2015; pp. 37–51. [Google Scholar]
- Anderson, J.M.; Rodriguez, A.; Chang, D.T. Foreign body reaction to biomaterials. Semin. Immunol. 2008, 20, 86–100. [Google Scholar] [CrossRef] [PubMed]
- Bos, G.W.; Hennink, W.E.; Brouwer, L.A.; den Otter, W.; Veldhuis, T.F.J.; van Nostrum, C.F.; van Luyn, M.J.A. Tissue reactions of in situ formed dextran hydrogels crosslinked by stereocomplex formation after subcutaneous implantation in rats. Biomaterials 2005, 26, 3901–3909. [Google Scholar] [CrossRef] [PubMed]
- Wilson, J.T.; Cui, W.; Sun, X.-L.; Tucker-Burden, C.; Weber, C.J.; Chaikof, E.L. In vivo biocompatibility and stability of a substrate-supported polymerizable membrane-mimetic film. Biomaterials 2007, 28, 609–617. [Google Scholar] [CrossRef] [PubMed]
- Jay, S.M.; Skokos, E.A.; Zeng, J.; Knox, K.; Kyriakides, T.R. Macrophage fusion leading to foreign body giant cell formation persists under phagocytic stimulation by microspheres in vitro and in vivo in mouse models. J. Biomed. Mater. Res. Part A 2010, 93, 189–199. [Google Scholar]
- Avula, M.N.; Rao, A.N.; McGill, L.D.; Grainger, D.W.; Solzbacher, F. Foreign body response to subcutaneous biomaterial implants in a mast cell-deficient kit(w-sh) murine model. Acta Biomater. 2014, 10, 1856–1863. [Google Scholar] [CrossRef] [PubMed]
- Hermenean, A.; Codreanu, A.; Herman, H.; Balta, C.; Rosu, M.; Mihali, C.-V.; Ivan, A.; Dinescu, S.; Ionita, M.; Costache, M. Chitosan-Graphene oxide 3d scaffolds as promising tools for bone regeneration in critical-size mouse calvarial defects. Sci. Rep. 2017, 7, 16641. [Google Scholar] [CrossRef] [PubMed]
- Chandorkar, Y.; Bhaskar, N.; Madras, G.; Basu, B. Long-term sustained release of salicylic acid from cross-linked biodegradable polyester induces a reduced foreign body response in mice. Biomacromolecules 2015, 16, 636–649. [Google Scholar] [CrossRef] [PubMed]
- Sumayya, A.S.; Muraleedhara Kurup, G. Biocompatibility of subcutaneously implanted marine macromolecules cross-linked bio-composite scaffold for cartilage tissue engineering applications. J. Biomater. Sci. Polym. Ed. 2018, 29, 257–276. [Google Scholar] [CrossRef] [PubMed]
- De Faria, A.F.; Perreault, F.; Shaulsky, E.; Arias Chavez, L.H.; Elimelech, M. Antimicrobial electrospun biopolymer nanofiber mats functionalized with graphene oxide–silver nanocomposites. ACS Appl. Mater. Interfaces 2015, 7, 12751–12759. [Google Scholar] [CrossRef]
- Reznickova, A.; Novotna, Z.; Kolska, Z.; Svorcik, V. Immobilization of silver nanoparticles on polyethylene terephthalate. Nanoscale Res. Lett. 2014, 9, 305. [Google Scholar] [CrossRef] [PubMed]
- Liu, K.-G.; Abbasi, A.R.; Azadbakht, A.; Hu, M.-L.; Morsali, A. Deposition of silver nanoparticles on polyester fiber under ultrasound irradiations. Ultrason. Sonochemistry 2017, 34, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-W.; Bae, H.-S.; Xing, Z.; Kwon, O.H.; Huh, M.; Kang, I.-K. Preparation and properties of silver-containing nylon 6 nanofibers formed by electrospinning. J. Appl. Polym. Sci. 2009, 112, 2320–2326. [Google Scholar] [CrossRef]
- Perelshtein, I.; Applerot, G.; Perkas, N.; Guibert, G.; Mikhailov, S.; Gedanken, A. Sonochemical coating of silver nanoparticles on textile fabrics (nylon, polyester and cotton) and their antibacterial activity. Nanotechnology 2008, 19, 245705. [Google Scholar] [CrossRef] [PubMed]
- Shi, Q.; Vitchuli, N.; Nowak, J.; Caldwell, J.M.; Breidt, F.; Bourham, M.; Zhang, X.; McCord, M. Durable antibacterial ag/polyacrylonitrile (ag/pan) hybrid nanofibers prepared by atmospheric plasma treatment and electrospinning. Eur. Polym. J. 2011, 47, 1402–1409. [Google Scholar] [CrossRef]
- Wang, L.; Hu, C.; Shao, L. The antimicrobial activity of nanoparticles: Present situation and prospects for the future. Int. J. Nanomed. 2017, 12, 1227–1249. [Google Scholar] [CrossRef]
- Maiti, S.; Krishnan, D.; Barman, G.; Ghosh, S.K.; Laha, J.K. Antimicrobial activities of silver nanoparticles synthesized from lycopersicon esculentum extract. J. Anal. Sci. Technol. 2014, 5, 40. [Google Scholar] [CrossRef]
- Kubyshkin, A.; Chegodar, D.; Katsev, A.; Petrosyan, A.; Krivorutchenko, Y.; Postnikova, O. Antimicrobial effects of silver nanoparticles stabilized in solution by sodium alginate. Biochem. Mol. Biol. J. 2016, 2, 13. [Google Scholar] [CrossRef]
- Hasan, K.M.F.; Pervez, M.N.; Talukder, M.E.; Sultana, M.Z.; Mahmud, S.; Meraz, M.M.; Bansal, V.; Genyang, C. A novel coloration of polyester fabric through green silver nanoparticles (g-agnps@pet). Nanomaterials 2019, 9, 569. [Google Scholar] [CrossRef]
- Behravan, M.; Hossein Panahi, A.; Naghizadeh, A.; Ziaee, M.; Mahdavi, R.; Mirzapour, A. Facile green synthesis of silver nanoparticles using berberis vulgaris leaf and root aqueous extract and its antibacterial activity. Int. J. Biol. Macromol. 2019, 124, 148–154. [Google Scholar] [CrossRef]
- Yasir, M.; Singh, J.; Tripathi, M.K.; Singh, P.; Shrivastava, R. Green synthesis of silver nanoparticles using leaf extract of common arrowhead houseplant and its anticandidal activity. Pharm. Mag. 2017, 13, S840–S844. [Google Scholar]
- Sanchez-Navarro, M.d.C.; Ruiz-Torres, C.A.; Nino-Martinez, N.; Sanchez-Sanchez, R.; Martinez-Castanon, G.A.; DeAlba-Montero, I.; Ruiz, F. Cytotoxic and bactericidal effect of silver nanoparticles obtained by green synthesis method using annona muricata aqueous extract and functionalized with 5-fluorouracil. Bioinorg. Chem. Appl. 2018, 2018, 6506381. [Google Scholar] [CrossRef] [PubMed]
- Rudakiya, D.M.; Pawar, K. Bactericidal potential of silver nanoparticles synthesized using cell-free extract of comamonas acidovorans: In vitro and in silico approaches. 3 Biotech 2017, 7, 92. [Google Scholar] [CrossRef] [PubMed]
- Liao, C.; Li, Y.; Tjong, S.C. Bactericidal and cytotoxic properties of silver nanoparticles. Int. J. Mol. Sci. 2019, 20, 449. [Google Scholar] [CrossRef] [PubMed]
- Lovric, V.; Goldberg, M.J.; Heuberer, P.R.; Oliver, R.A.; Stone, D.; Laky, B.; Page, R.S.; Walsh, W.R. Suture wear particles cause a significant inflammatory response in a murine synovial airpouch model. J. Orthop. Surg. Res. 2018, 13, 311. [Google Scholar] [CrossRef] [PubMed]
- Veleirinho, B.; Coelho, D.S.; Dias, P.F.; Maraschin, M.; Pinto, R.; Cargnin-Ferreira, E.; Peixoto, A.; Souza, J.A.; Ribeiro-do-Valle, R.M.; Lopes-da-Silva, J.A. Foreign body reaction associated with pet and pet/chitosan electrospun nanofibrous abdominal meshes. PLoS ONE 2014, 9, e95293. [Google Scholar] [CrossRef] [PubMed]
| Sample | Output 1 (kV) | Output 2 (kV) | Heat (KW) | Humidity (%) | Temperature (°C) | Feed Rate (mL/h) |
|---|---|---|---|---|---|---|
| PET_2.5_ctrl | −5.73 | 17.53 | 0.6 | 35 | 27 | 2.5 |
| PET_5_ctrl | 5 | |||||
| PET_7.5_ctrl | 7.5 | |||||
| PET_10_ctrl | 10 |
| Nanofibers | Explan Tation (days) | Edema | PMN | MONO LYM | MO | GC | PC | EOS | FC | NV |
|---|---|---|---|---|---|---|---|---|---|---|
| Control mice | 1 | − | + | − | − | − | − | − | − | − |
| 7 | − | − | + | + | − | − | − | − | − | |
| PET_10_ctrl | 1 | ++++ | ++++ | +++ | ++ | + | − | + | + | − |
| 7 | +++ | ++ | ++++ | ++++ | ++ | ++ | + | ++++ | − | |
| PET_7.5_ctrl | 1 | +++ | +++ | + | + | + | + | + | + | − |
| 7 | ++ | + | ++ | +++ | ++ | + | + | +++ | − | |
| PET_5_ctrl | 1 | + | +++ | sp | + | sp | − | + | + | − |
| 7 | ++ | + | ++ | +++ | + | + | + | ++ | − | |
| PET_2.5_ctrl | 1 | + | +++ | sp | + | sp | − | + | + | − |
| 7 | ++ | + | ++ | +++ | + | + | + | ++ | + | |
| PET_10_NanoAg | 1 | − | +++ | ++ | ++ | − | − | + | + | − |
| 7 | − | + | +++ | +++ | − | + | + | +++ | + | |
| PET_7.5_NanoAg | 1 | − | ++ | sp | sp | − | + | + | + | − |
| 7 | − | + | ++ | ++ | − | + | + | +++ | + | |
| PET_5_NanoAg | 1 | − | ++ | sp | + | − | − | + | + | − |
| 7 | − | + | + | +++ | − | + | + | ++ | + | |
| PET_2.5_NanoAg | 1 | − | ++ | sp | + | − | − | + | + | − |
| 7 | − | + | + | + | − | + | sp | + | ++ |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grumezescu, A.M.; Stoica, A.E.; Dima-Bălcescu, M.-Ș.; Chircov, C.; Gharbia, S.; Baltă, C.; Roșu, M.; Herman, H.; Holban, A.M.; Ficai, A.; et al. Electrospun Polyethylene Terephthalate Nanofibers Loaded with Silver Nanoparticles: Novel Approach in Anti-Infective Therapy. J. Clin. Med. 2019, 8, 1039. https://doi.org/10.3390/jcm8071039
Grumezescu AM, Stoica AE, Dima-Bălcescu M-Ș, Chircov C, Gharbia S, Baltă C, Roșu M, Herman H, Holban AM, Ficai A, et al. Electrospun Polyethylene Terephthalate Nanofibers Loaded with Silver Nanoparticles: Novel Approach in Anti-Infective Therapy. Journal of Clinical Medicine. 2019; 8(7):1039. https://doi.org/10.3390/jcm8071039
Chicago/Turabian StyleGrumezescu, Alexandru Mihai, Alexandra Elena Stoica, Mihnea-Ștefan Dima-Bălcescu, Cristina Chircov, Sami Gharbia, Cornel Baltă, Marcel Roșu, Hildegard Herman, Alina Maria Holban, Anton Ficai, and et al. 2019. "Electrospun Polyethylene Terephthalate Nanofibers Loaded with Silver Nanoparticles: Novel Approach in Anti-Infective Therapy" Journal of Clinical Medicine 8, no. 7: 1039. https://doi.org/10.3390/jcm8071039
APA StyleGrumezescu, A. M., Stoica, A. E., Dima-Bălcescu, M.-Ș., Chircov, C., Gharbia, S., Baltă, C., Roșu, M., Herman, H., Holban, A. M., Ficai, A., Vasile, B. S., Andronescu, E., Chifiriuc, M. C., & Hermenean, A. (2019). Electrospun Polyethylene Terephthalate Nanofibers Loaded with Silver Nanoparticles: Novel Approach in Anti-Infective Therapy. Journal of Clinical Medicine, 8(7), 1039. https://doi.org/10.3390/jcm8071039











