Application of Video Head Impulse Test in the Diagnosis and Follow-Up of Vestibular Schwannoma: Case Series, Narrative Literature Review and Clinical Practice Implications
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Consideration
2.2. Patient Clinical Characteristics and Study Protocol
2.3. Surgical Treatment
2.4. Video Head Impulse Test Protocol
3. Results
3.1. Patients’ Clinical Data and Video Head Impulse Test Results
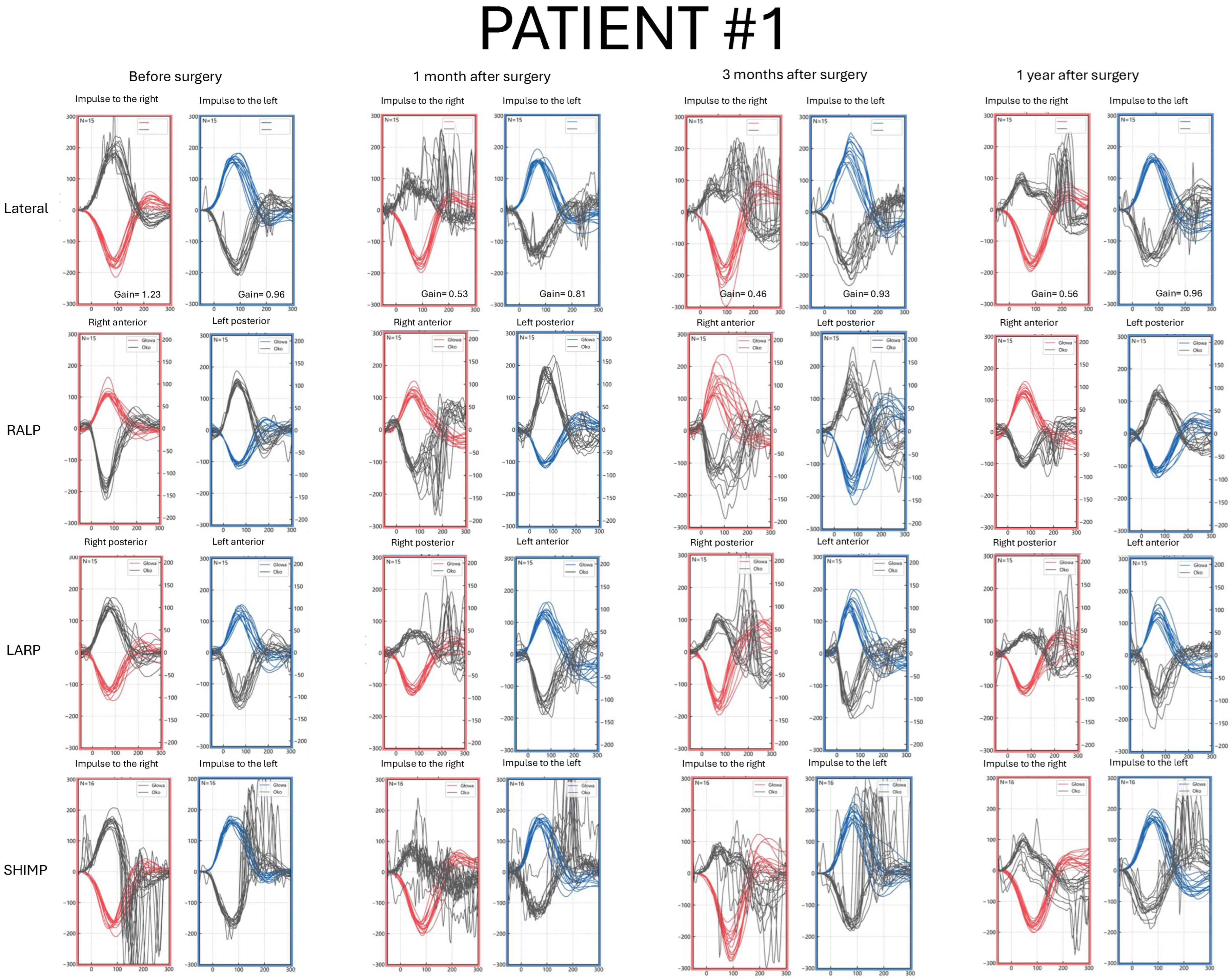
3.2. Patient #1—Clinical Characteristics and vHIT Results
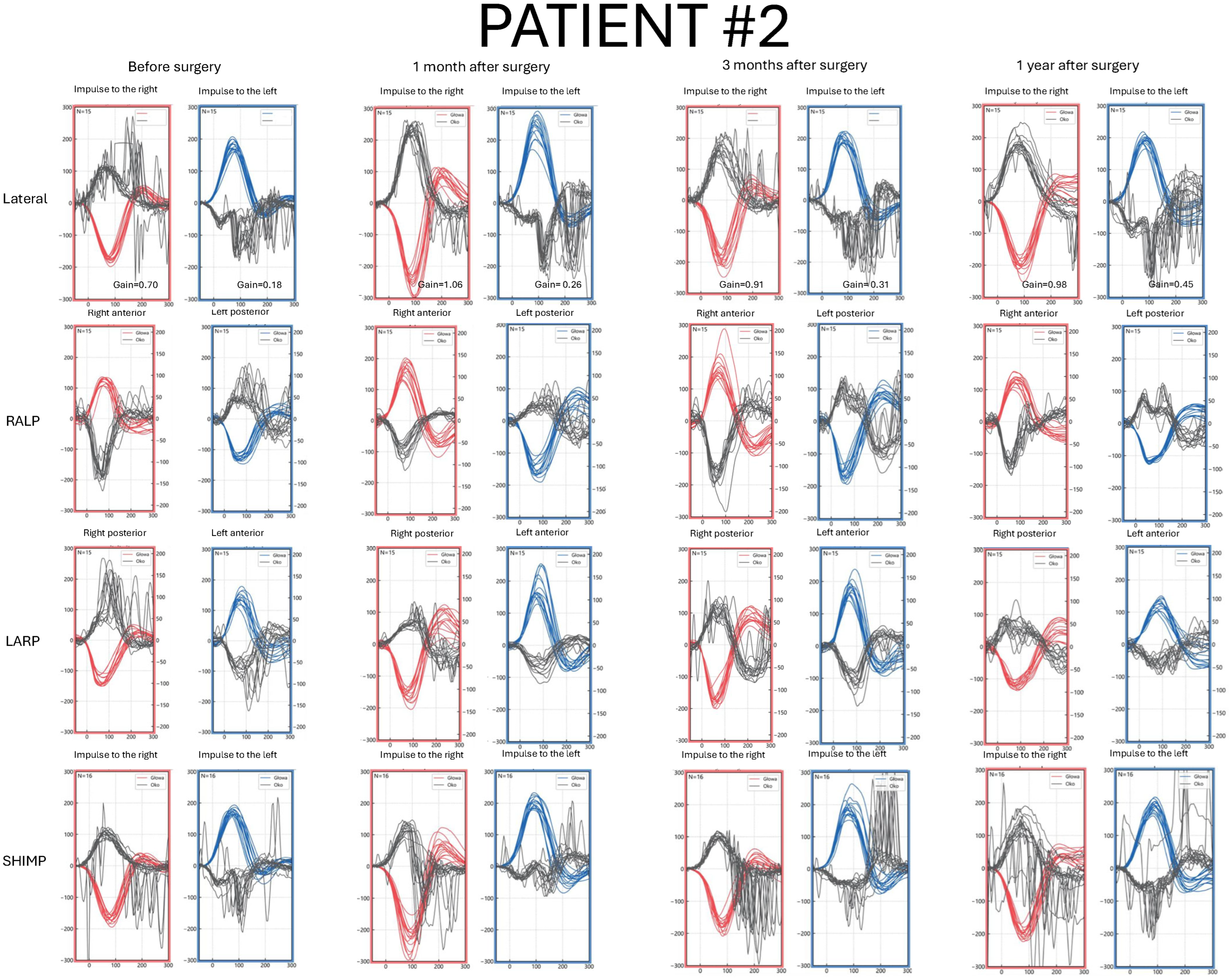
3.3. Patient #2—Clinical Characteristics and vHIT Results
3.4. Patient #3—Clinical Characteristics and vHIT Results

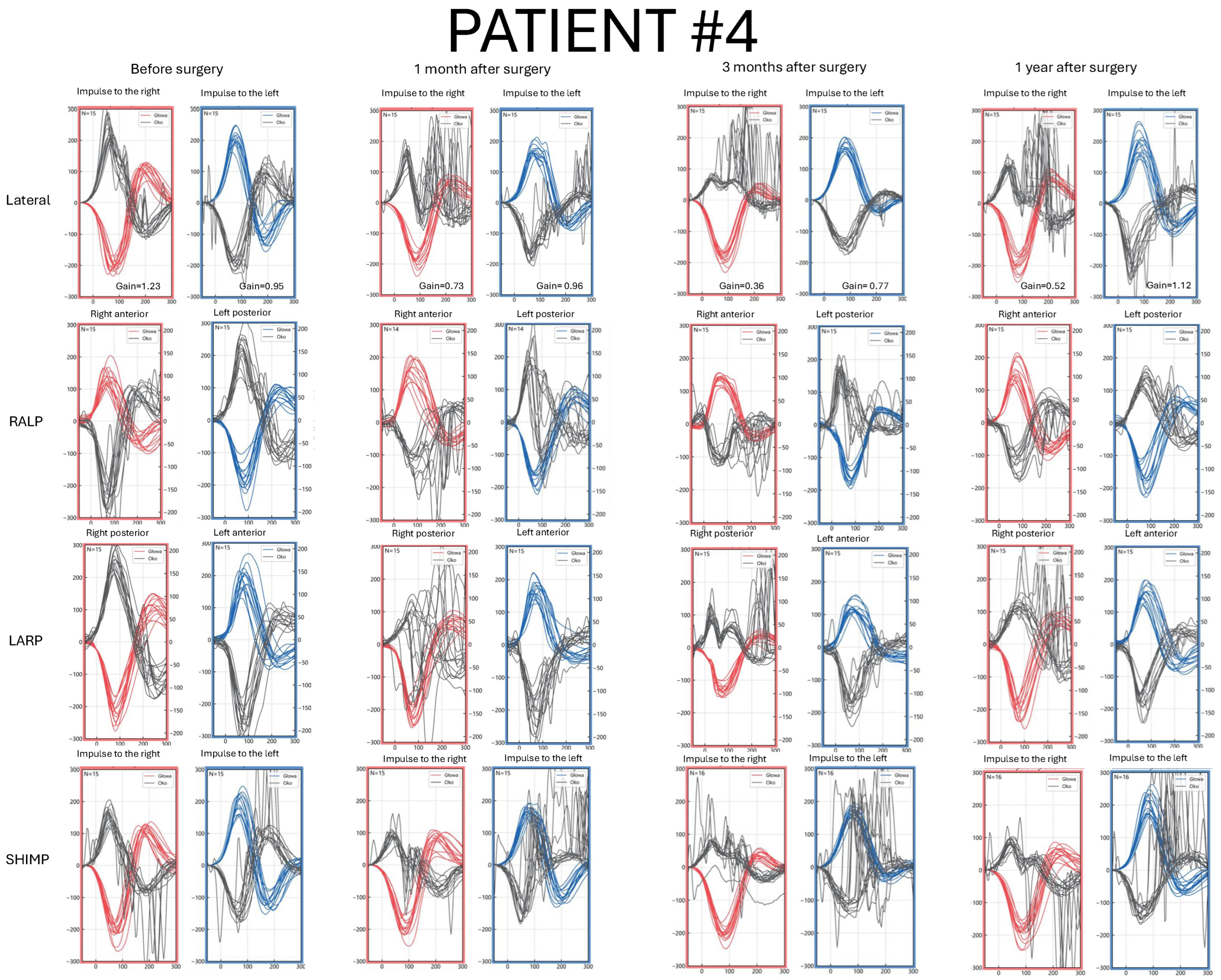
3.5. Patient #4—Clinical Characteristics and vHIT Results
- Case 1 is a Koos I intracanalicular vestibular schwannoma in the right internal acoustic meatus with CSF cap separating the tumor from the cochlea.
- Case 2 is a Koos IV vestibular schwannoma with a cystic component in the left cerebellopontine angle, causing brainstem displacement.
- Case 3 is a Koos II vestibular schwannoma occupying the fundus of the right internal acoustic meatus and protruding into the cerebellopontine angle.
- Case 4 is a Koos III vestibular schwannoma present in the right cerebellopontine angle cistern, occupying less than half of the internal acoustic meatus.

4. Discussion
Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kentala, E.; Pyykkö, I. Clinical picture of vestibular schwannoma. Auris Nasus Larynx 2001, 28, 15–22. [Google Scholar] [CrossRef]
- Ragab, A.; Emara, A.; Shouker, M.; Ebied, O. Prospective evaluation of the clinical profile and referral pattern differences of vestibular schwannomas and other cerebellopontine angle tumors. Otol. Neurotol. 2012, 33, 863–870. [Google Scholar] [CrossRef]
- Wiegand, D.A.; Ojemann, R.G.; Fickel, V. Surgical Treatment of Acoustic Neuroma (Vestibular Schwannoma) in the United States: Report from the Acoustic Neuroma Registry. Laryngoscope 1996, 106 Pt 1, 58–66. [Google Scholar] [CrossRef] [PubMed]
- Goldbrunner, R.; Weller, M.; Regis, J.; Lund-Johansen, M.; Stavrinou, P.; Reuss, D.; Evans, D.G.; Lefranc, F.; Sallabanda, K.; Falini, A.; et al. EANO guideline on the diagnosis and treatment of vestibular schwannoma. Neuro Oncol. 2020, 22, 31–45. [Google Scholar] [CrossRef]
- Żurek, M.; Wojciechowski, T.; Niemczyk, K. Nationwide clinico-epidemiological treatment analysis of adult patients with tumors of cerebellopontine angle and internal acoustic meatus in Poland during 2011–2020. BMC Public Health 2023, 23, 1735. [Google Scholar] [CrossRef] [PubMed]
- Batuecas-Caletrio, A.; Cruz-Ruiz, S.S.; Muñoz-Herrera, A.; Perez-Fernandez, N. The map of dizziness in vestibular schwannoma. Laryngoscope 2015, 125, 2784–2789. [Google Scholar] [CrossRef] [PubMed]
- Andersen, J.F.; Nilsen, K.S.; Vassbotn, F.S.; Møller, P.; Myrseth, E.; Lund-Johansen, M.; Goplen, F.K. Predictors of vertigo in patients with untreated vestibular schwannoma. Otol. Neurotol. 2015, 36, 647–652. [Google Scholar] [CrossRef]
- Torchalla, P.; Jasińska-Nowacka, A.; Lachowska, M.; Niemczyk, K. A Proposal for Comprehensive Audio-Vestibular Test Battery Protocol for Diagnosis and Follow-Up Monitoring in Patients with Vestibular Schwannoma Undergoing Surgical Tumor Removal. J. Clin. Med. 2024, 13, 5007. [Google Scholar] [CrossRef]
- Torchalla, P.; Jasińska-Nowacka, A.; Lachowska, M.; Niemczyk, K. Functional Outcome and Balance Compensation in Patients with Unilateral Vestibular Schwannoma After Surgical Treatment-Short- and Medium-Term Observation. J. Clin. Med. 2025, 14, 585. [Google Scholar] [CrossRef]
- MacDougall, H.G.; Weber, K.P.; McGarvie, L.A.; Halmagyi, G.M.; Curthoys, I.S. The video head impulse test: Diagnostic accuracy in peripheral vestibulopathy. Neurology 2009, 73, 1134–1141. [Google Scholar] [CrossRef]
- Alhabib, S.F.; Saliba, I. Video head impulse test: A review of the literature. Eur. Arch. Otorhinolaryngol. 2017, 274, 1215–1222. [Google Scholar] [CrossRef] [PubMed]
- Batuecas-Caletrio, A.; Rey-Martinez, J.; Trinidad-Ruiz, G.; Matiño-Soler, E.; Cruz-Ruiz, S.S.; Muñoz-Herrera, A.; Perez-Fernandez, N. Vestibulo-Ocular Reflex Stabilization after Vestibular Schwannoma Surgery: A Story Told by Saccades. Front. Neurol. 2017, 8, 15. [Google Scholar] [CrossRef]
- Koos, W.T.; Day, J.D.; Matula, C.; Levy, D.I. Neurotopographic considerations in the microsurgical treatment of small acoustic neurinomas. J. Neurosurg. Mar. 1998, 88, 506–512. [Google Scholar] [CrossRef] [PubMed]
- Parietti-Winkler, C.; Gauchard, G.C.; Simon, C.; Perrin, P.P. Pre-operative vestibular pattern and balance compensation after vestibular schwannoma surgery. Neuroscience 2011, 172, 285–292. [Google Scholar] [CrossRef] [PubMed]
- Lin, K.L.; Chen, C.M.; Wang, S.J.; Young, Y.H. Correlating vestibular schwannoma size with vestibular-evoked myogenic potential results. Ear Hear. 2014, 35, 571–576. [Google Scholar] [CrossRef]
- Brown, C.S.; Peskoe, S.B.; Risoli, T., Jr.; Garrison, D.B.; Kaylie, D.M. Associations of Video Head Impulse Test and Caloric Testing among Patients with Vestibular Schwannoma. Otol. Neurotol. 2019, 161, 324–329. [Google Scholar] [CrossRef]
- West, N.; Sass, H.; Klokker, M.; Cayé-Thomasen, P. Video Head Impulse Test Results in Patients With a Vestibular Schwannoma-Sensitivity and Correlation With Other Vestibular System Function Tests, Hearing Acuity, and Tumor Size. Otol. Neurotol. 2020, 41, e623–e629. [Google Scholar] [CrossRef]
- Fujiwara, K.; Morita, S.; Fukuda, A.; Akamatsu, H.; Yanagi, H.; Hoshino, K.; Nakamaru, Y.; Kano, S.; Homma, A. Analysis of semicircular canal function as evaluated by video Head Impulse Test in patients with vestibular schwannoma. J. Vestib. Res. 2020, 30, 101–108. [Google Scholar] [CrossRef]
- Harun, A.; Agrawal, Y.; Tan, M.; Niparko, J.K.; Francis, H.W. Sex and age associations with vestibular schwannoma size and presenting symptoms. Otol. Neurotol. 2012, 33, 1604–1610. [Google Scholar] [CrossRef]
- Picciotti, P.M.; Rolesi, R.; Rossi, G.; Tizio, A.; Sergi, B.; Galli, J. Caloric Test, and Qualitative and Quantitative vHIT Analysis in Vestibular Schwannoma. Otol. Neurotol. 2025, 46, e215–e223. [Google Scholar] [CrossRef]
- Tranter-Entwistle, I.; Dawes, P.; Darlington, C.L.; Smith, P.F.; Cutfield, N. Video head impulse in comparison to caloric testing in unilateral vestibular schwannoma. Acta Otolaryngol. 2016, 136, 1110–1114. [Google Scholar] [CrossRef]
- Jensen, M.K.; Hougaard, D.D. Suppression head impulse testing is recommended for vestibular testing of patients with untreated unilateral vestibular schwannoma. Eur. Arch. Otorhinolaryngol. 2022, 279, 91–99. [Google Scholar] [CrossRef]
- Fujiwara, K.; Morita, S.; Motegi, H.; Yamaguchi, S.; Ishi, Y.; Hoshino, K.; Fukuda, A.; Kobayashi, M.; Nakamaru, Y.; Fujimura, M.; et al. Pre- and post-operative semicircular canal function evaluated by video head impulse test in patients with vestibular schwannoma. Auris Nasus Larynx 2024, 51, 542–547. [Google Scholar] [CrossRef]
- Taylor, R.L.; Kong, J.; Flanagan, S.; Pogson, J.; Croxson, G.; Pohl, D.; Welgampola, M.S. Prevalence of vestibular dysfunction in patients with vestibular schwannoma using video head-impulses and vestibular-evoked potentials. J. Neurol. 2015, 262, 1228–1237. [Google Scholar] [CrossRef]
- Fujiwara, K.; Yanagi, H.; Morita, S.; Hoshino, K.; Fukuda, A.; Nakamaru, Y.; Homma, A. Evaluation of Vertical Semicircular Canal Function in Patients with Vestibular Schwannoma. Ann. Otol. Rhinol. Laryngol. 2019, 128, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Pogson, J.M.; Taylor, R.L.; Bradshaw, A.P.; McGarvie, L.; D’Souza, M.; Flanagan, S.; Kong, J.; Biggs, N.; Shivalingam, B.; Greenberg, S.; et al. The human vestibulo-ocular reflex and compensatory saccades in schwannoma patients before and after vestibular nerve section. Clin. Neurophysiol. 2022, 138, 197–213. [Google Scholar] [CrossRef] [PubMed]
- Brooker, J.E.; Fletcher, J.M.; Dally, M.J.; Briggs, R.J.S.; Cousins, V.C.; Malham, G.M.; Kennedy, R.J.; Smee, R.I.; Burney, S. Factors associated with symptom-specific psychological and functional impact among acoustic neuroma patients. J. Laryngol. Otol. 2014, 128 (Suppl. S2), S16–S26. [Google Scholar] [CrossRef] [PubMed]
- Fuentealba-Bassaletti, C.; Neve, O.M.; van Esch, B.F.; Jansen, J.C.; Koot, R.W.; van Benthem, P.P.G.; Hensen, E.F. Vestibular Complaints Impact on the Long-Term Quality of Life of Vestibular Schwannoma Patients. Otol. Neurotol. 2023, 44, 161–167. [Google Scholar] [CrossRef]
- Batuecas-Caletrio, A.; Santacruz-Ruiz, S.; Muñoz-Herrera, A.; Perez-Fernandez, N. The vestibulo-ocular reflex and subjective balance after vestibular schwannoma surgery. Laryngoscope 2014, 124, 1431–1435. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jasińska-Nowacka, A.; Torchalla, P.; Wojciechowski, T.; Niemczyk, K. Application of Video Head Impulse Test in the Diagnosis and Follow-Up of Vestibular Schwannoma: Case Series, Narrative Literature Review and Clinical Practice Implications. J. Clin. Med. 2025, 14, 7222. https://doi.org/10.3390/jcm14207222
Jasińska-Nowacka A, Torchalla P, Wojciechowski T, Niemczyk K. Application of Video Head Impulse Test in the Diagnosis and Follow-Up of Vestibular Schwannoma: Case Series, Narrative Literature Review and Clinical Practice Implications. Journal of Clinical Medicine. 2025; 14(20):7222. https://doi.org/10.3390/jcm14207222
Chicago/Turabian StyleJasińska-Nowacka, Agnieszka, Patrycja Torchalla, Tomasz Wojciechowski, and Kazimierz Niemczyk. 2025. "Application of Video Head Impulse Test in the Diagnosis and Follow-Up of Vestibular Schwannoma: Case Series, Narrative Literature Review and Clinical Practice Implications" Journal of Clinical Medicine 14, no. 20: 7222. https://doi.org/10.3390/jcm14207222
APA StyleJasińska-Nowacka, A., Torchalla, P., Wojciechowski, T., & Niemczyk, K. (2025). Application of Video Head Impulse Test in the Diagnosis and Follow-Up of Vestibular Schwannoma: Case Series, Narrative Literature Review and Clinical Practice Implications. Journal of Clinical Medicine, 14(20), 7222. https://doi.org/10.3390/jcm14207222




