The Effect of Tailored Short Message Service (SMS) on Physical Activity: Results from a Three-Component Randomized Controlled Lifestyle Intervention in Women with PCOS
Abstract
1. Introduction
2. Materials and Methods
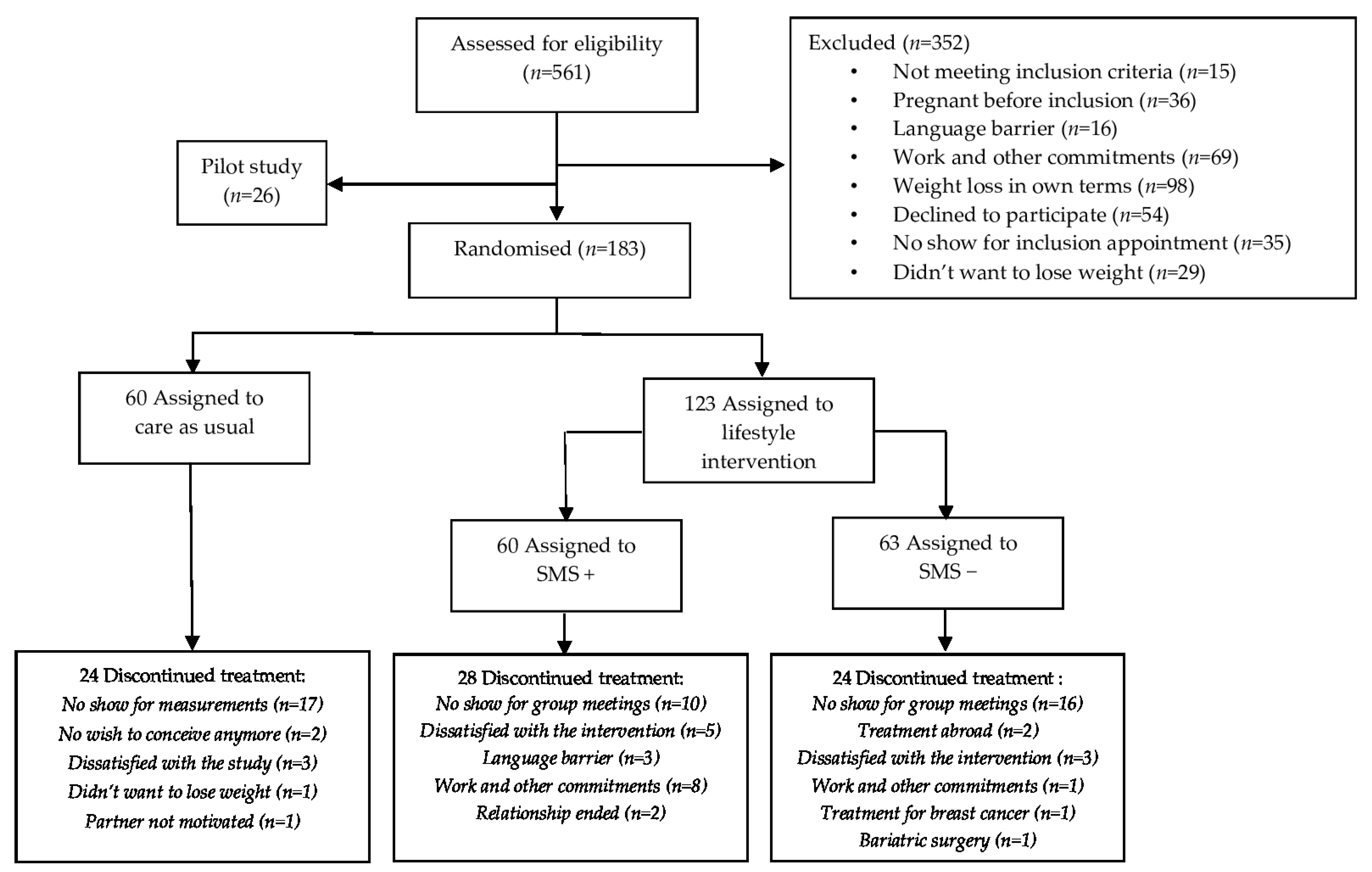
2.1. Trial Design
2.2. Participants
2.3. Three-Component Lifestyle Intervention (LSI) and Control Group (CAU)
2.4. Clinical and Endocrine Assessments
2.5. Outcome Measures
2.5.1. International Physical Activity Questionnaire (IPAQ)
- Low: no activity is reported or some activity is reported but not enough to meet categories ‘moderate or high’. These women reported activity equivalent to less than 600 METmin/week.
- Moderate: These women reported 3 or more days of vigorous activity of at least 20 min per day, 5 or more days of moderate-intensity activity and/or walking of at least 30 min per day, or 5 or more days of any combination of walking, moderate-intensity or vigorous-intensity activities equivalent to at least 600 METmin/week.
2.5.2. Maximal Cycle Ergometer Test
2.6. Statistical Methods
3. Results
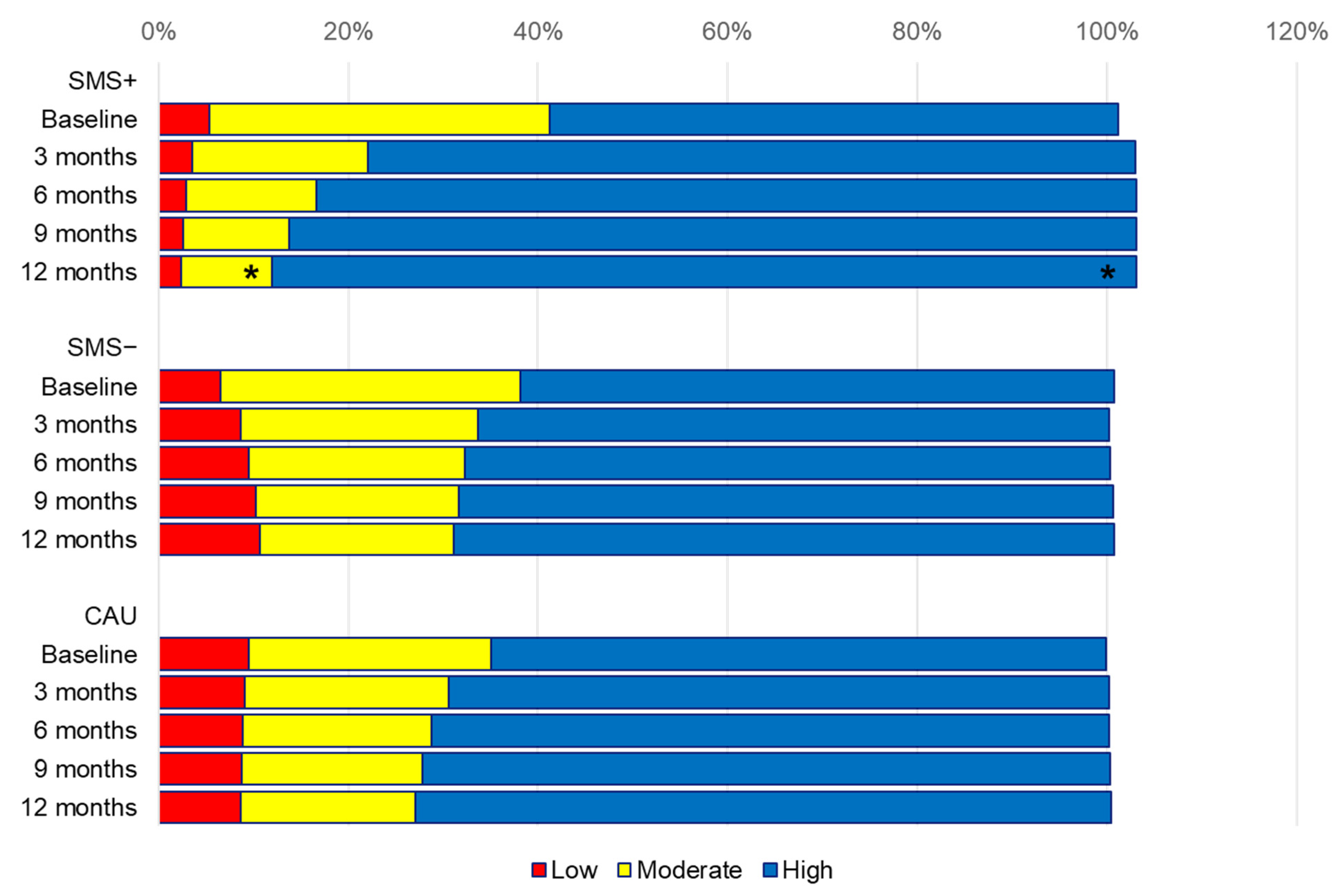
3.1. Changes in Low, Moderate and High Physical Activity Categories Estimates
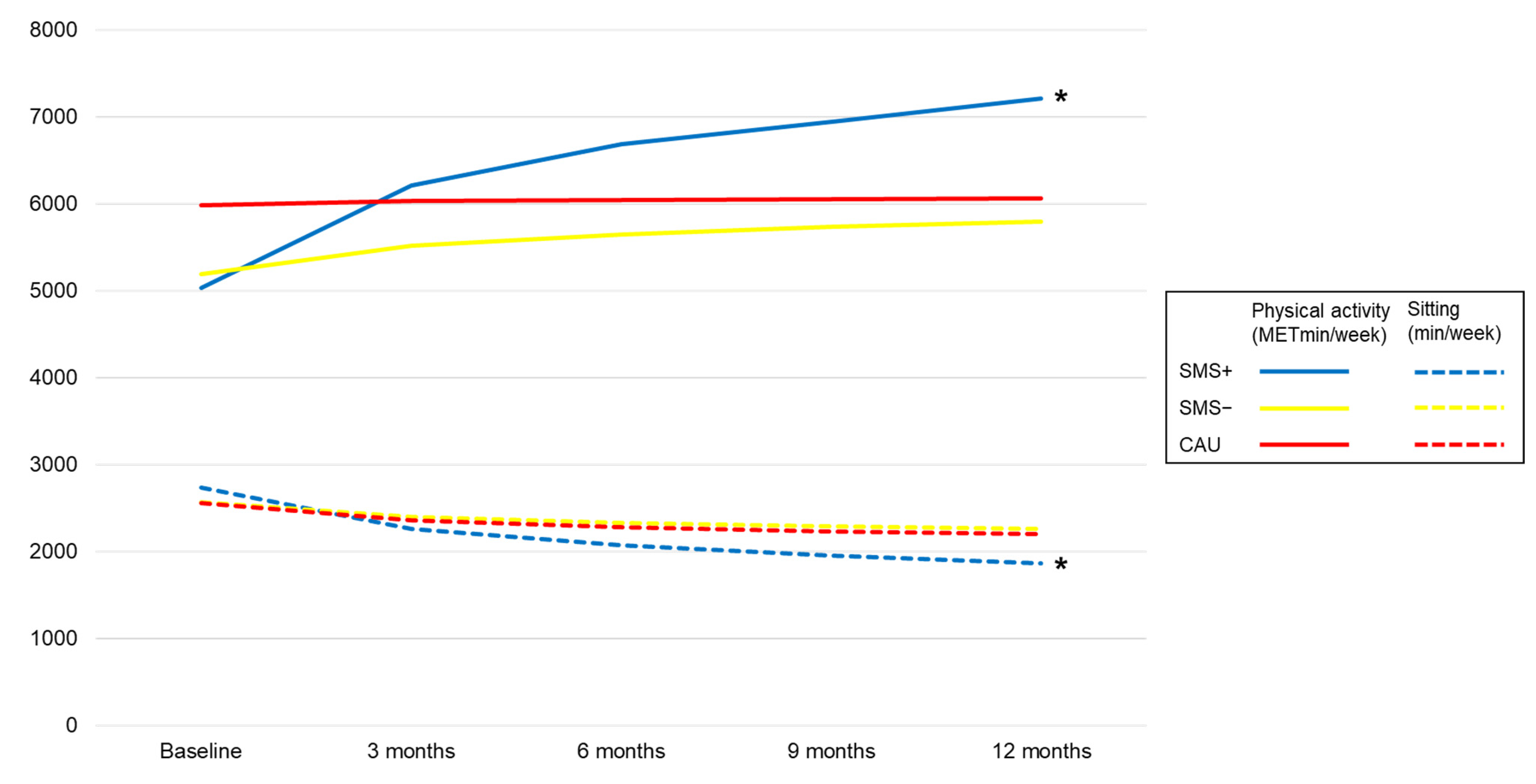
3.2. Physical Activity METminutes Estimates after 12 Months
3.3. Sedentary Behaviour Estimates after 12 Months
3.4. Aerobic Capacity Estimates after 12 Months within SMS+ and SMS−
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Teede, H.J.; Misso, M.L.; Costello, M.F.; Dokras, A.; Laven, J.; Moran, L.; Piltonen, T.; Norman, R.J.; on behalf of theInternational PCOS Network. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Fertil. Steril. 2018, 110, 364–379. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.; Davies, M.; Norman, R.; Moran, L. Overweight, obesity and central obesity in women with polycystic ovary syndrome: A systematic review and meta-analysis. Hum. Reprod. Update 2012, 18, 618–637. [Google Scholar] [CrossRef]
- Lim, S.S.; Norman, R.J.; Davies, M.J.; Moran, L.J. The effect of obesity on polycystic ovary syndrome: A systematic review and meta-analysis. Obes. Rev. 2013, 14, 95–109. [Google Scholar] [CrossRef] [PubMed]
- Glueck, C.J.; Goldenberg, N. Characteristics of obesity in polycystic ovary syndrome: Etiology, treatment, and genetics. Metabolism 2019, 92, 108–120. [Google Scholar] [CrossRef] [PubMed]
- Glueck, C.J.; Goldenberg, N. Fitness vs. Fatness on all-Cause Mortality: A Meta-Analysis. Prog. Cardiovasc. Dis. 2014, 56, 382–390. [Google Scholar]
- Koivula, R.W.; Tornberg, A.B.; Franks, P.W. Exercise and diabetes-related cardiovascular disease: Systematic review of published evidence from observational studies and clinical trials. Curr. Diab. Rep. 2013, 13, 372–380. [Google Scholar] [CrossRef]
- Nicolucci, A.; Balducci, S.; Cardelli, P.; Cavallo, S.; Fallucca, S.; Bazuro, A.; Simonelli, P.; Iacobini, C.; Zanuso, S.; Pugliese, G.; et al. Relationship of exercise volume to improvements of quality of life with supervised exercise training in patients with type 2 diabetes in a randomised controlled trial: The Italian Diabetes and Exercise Study (IDES). Diabetologia 2012, 55, 579–588. [Google Scholar] [CrossRef]
- Caspersen, C.J.; Powell, K.E.; Christenson, G.M. Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Rep. 1985, 100, 126–131. [Google Scholar]
- Lum, D.; Barbosa, T.M. Brief Review: Effects of Isometric Strength Training on Strength and Dynamic Performance. Int. J. Sports Med. 2019, 40, 363–375. [Google Scholar] [CrossRef]
- Tremblay, M.S.; Aubert, S.; Barnes, J.D.; Saunders, T.J.; Carson, V.; Latimer-Cheung, A.E.; Chastin, S.F.M.; Altenburg, T.M.; Chinapaw, M.J.M. Sedentary Behavior Research Network (SBRN)–Terminology Consensus Project process and outcome. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 75. [Google Scholar] [CrossRef]
- Biddle, S.J.; Bennie, J.A.; Bauman, A.E.; Chau, J.Y.; Dunstan, D.; Owen, N.; Stamatakis, E.; van Uffelen, J.G.Z. Too much sitting and all-cause mortality: Is there a causal link? BMC Public Health 2016, 16, 635. [Google Scholar] [CrossRef]
- Ekelund, U.; Steene-Johannessen, J. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 2016, 388, 1302–1310. [Google Scholar] [CrossRef] [PubMed]
- Tay, C.T.; Moran, L.J.; Harrison, C.L.; Brown, E.J. Physical activity and sedentary behaviour in women with and without polycystic ovary syndrome: An Australian population-based cross-sectional study. Clin. Endocrinol. 2020, 93, 154–162. [Google Scholar] [CrossRef] [PubMed]
- Moran, L.J.; Ranasinha, S.; Zoungas, S.; McNaughton, S.; Brown, W.J.; Teede, H. The contribution of diet, physical activity and sedentary behaviour to body mass index in women with and without polycystic ovary syndrome. Hum. Reprod 2013, 28, 2276–2283. [Google Scholar] [CrossRef] [PubMed]
- Dona, S.; Bacchi, E.; Moghetti, P. Is Cardiorespiratory Fitness Impaired in PCOS Women? A Review of the Literature. J. Endocrinol. Investig. 2017, 40, 463–469. [Google Scholar] [CrossRef]
- Orio, F., Jr.; Giallauria, F.; Palomba, S.; Cascella, T.; Manguso, F.; Vuolo, L.; Russo, T.; Tolino, A.; Lombardi, G.; Colao, A.; et al. Cardiopulmonary Impairment in Young Women with Polycystic Ovary Syndrome. J. Clin. Endocrinol. Metab. 2006, 91, 2967–2971. [Google Scholar] [CrossRef]
- Wang, Z.; Groen, H.; Cantineau, A.E.P.; van Elten, T.M.; Karsten, M.D.A.; van Oers, A.M.; Mol, B.W.J.; Roseboom, T.J.; Hoek, A. Dietary Intake, Eating Behavior, Physical Activity, and Quality of Life in Infertile Women with PCOS and Obesity Compared with Non-PCOS Obese Controls. Nutrients 2021, 13, 3526. [Google Scholar] [CrossRef]
- Lim, S.; Smith, C.A.; Costello, M.F.; MacMillan, F.; Moran, L.; Ee, C. Barriers and facilitators to weight management in overweight and obese women living in Australia with PCOS: A qualitative study. BMC Endocr. Disord 2019, 19, 106. [Google Scholar] [CrossRef]
- Lee, S.; Patel, P.; Myers, N.D.; Pfeiffer, K.A.; Smith, A.L. A Systematic Review of eHealth Interventions to Promote Physical Activity in Adults with Obesity or Overweight. Behav. Med. 2022, 1–18. [Google Scholar] [CrossRef]
- Fjeldsoe, B.S.; Marshall, A.L.; Miller, J.D. Behavior change interventions delivered by mobile telephone short-message service. Am. J. Prev. Med. 2009, 36, 165–173. [Google Scholar] [CrossRef]
- Dijkstra, A.; de Vries, H. The development of computer-generated tailored interventions. Patient. Educ. Couns. 1999, 36, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Ryan, P.; Lauver, D.R. The efficacy of tailored interventions. J. Nurs. Sch. 2002, 34, 331–337. [Google Scholar] [CrossRef]
- Jiskoot, G.; Benneheij, S.; Beerthuizen, A.; de Niet, J.; de Klerk, C.; Timman, R.; Busschbach, J.; Laven, J. A three-component cognitive behavioural lifestyle program for preconceptional weight-loss in women with polycystic ovary syndrome (PCOS): A protocol for a randomized controlled trial. Reprod Health 2017, 14, 34. [Google Scholar] [CrossRef] [PubMed]
- Jiskoot, G.; Timman, R.; Beerthuizen, A.; De Loos, A.D.; Busschbach, J.; Laven, J. Weight Reduction Through a Cognitive Behavioral Therapy Lifestyle Intervention in PCOS: The Primary Outcome of a Randomized Controlled Trial. Obesity 2020, 28, 2134–2141. [Google Scholar] [CrossRef] [PubMed]
- Rotterdam, E.A.; ASRM. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004, 81, 19–25. [Google Scholar]
- Brink, E.; van Rossum, C.; Postma-Smeets, A.; Stafleu, A.; Wolvers, D.; van Dooren, C.; Toxopeus, I.; Buurma-Rethans, E.; Geurts, M.; Ocké, M. Development of healthy and sustainable food-based dietary guidelines for the Netherlands. Public Health Nutr. 2019, 22, 2419–2435. [Google Scholar] [CrossRef]
- WHO. Global Recommendations on Physical Activity for Health; World Health Organization: Geneva, Switzerland, 2010.
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sport. Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Committee, I.R. Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ)-Short and Long Forms. 2005. Available online: http://www.ipaq.ki.se/scoring.pdf (accessed on 1 February 2023).
- Thomas, S.; Reading, J.; Shephard, R.J. Revision of the Physical Activity Readiness Questionnaire (PAR-Q). Can J. Sport. Sci. 1992, 17, 338–345. [Google Scholar]
- Van der Steeg, G.E.; Takken, T. Reference values for maximum oxygen uptake relative to body mass in Dutch/Flemish subjects aged 6-65 years: The LowLands Fitness Registry. Eur. J. Appl. Physiol. 2021, 121, 1189–1196. [Google Scholar] [CrossRef]
- Tanaka, H.; Monahan, K.D.; Seals, D.R. Age-predicted maximal heart rate revisited. J. Am. Coll. Cardiol. 2001, 37, 153–156. [Google Scholar] [CrossRef]
- Borg, G.A. Psychophysical bases of perceived exertion. Med. Sci. Sport. Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef]
- Little, R.; Rubin, D. Statistical Analysis with Missing Data; John Wiley and Sons: New York, NY, USA, 1987. [Google Scholar]
- Webb, M.A.; Mani, H.; Robertson, S.J.; Waller, H.L.; Webb, D.R.; Edwardson, C.L.; Bodicoat, D.H.; Yates, T.; Khunti, K.; Davies, M. Moderate increases in daily step count are associated with reduced IL6 and CRP in women with PCOS. Endocr. Connect. 2018, 7, 1442–1447. [Google Scholar] [CrossRef] [PubMed]
- Nybacka, Å.; Carlström, K.; Ståhle, A.; Nyren, S.; Hellström, P.M.; Hirschberg, A.L. Randomized comparison of the influence of dietary management and/or physical exercise on ovarian function and metabolic parameters in overweight women with polycystic ovary syndrome. Fertil. Steril. 2011, 96, 1508–1513. [Google Scholar] [CrossRef] [PubMed]
- Benham, J.L.; Booth, J.E.; Corenblum, B.; Doucette, S.; Friedenreich, C.M. Exercise training and reproductive outcomes in women with polycystic ovary syndrome: A pilot randomized controlled trial. Clin. Endocrinol. 2021, 95, 332–343. [Google Scholar] [CrossRef]
- Roessler, K.K.; Birkebaek, C.; Ravn, P.; Andersen, M.S.; Glintborg, D. Effects of exercise and group counselling on body composition and VO2max in overweight women with polycystic ovary syndrome. Acta Obs. Gynecol. Scand. 2013, 92, 272–277. [Google Scholar] [CrossRef]
- Patten, R.K.; McIlvenna, L.C.; Levinger, I.; Garnham, A.P.; Shorakae, S.; Parker, A.G.; McAinch, A.J.; Rodgers, R.J.; Hiam, D.; Moreno-Asso, A.; et al. High-intensity training elicits greater improvements in cardio-metabolic and reproductive outcomes than moderate-intensity training in women with polycystic ovary syndrome: A randomized clinical trial. Hum. Reprod. 2022, 37, 1018–1029. [Google Scholar] [CrossRef] [PubMed]
- Patten, R.K.; Boyle, R.A.; Moholdt, T.; Kiel, I.; Hopkins, W.G.; Harrison, C.L.; Stepto, N.K. Exercise Interventions in Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis. Front. Physiol. 2020, 11, 606. [Google Scholar] [CrossRef]
- Awoke, M.A.; Earnest, A.; Joham, A.E.; Hodge, A.M.; Teede, H.J.; Brown, W.J.; Moran, L.J. Weight gain and lifestyle factors in women with and without polycystic ovary syndrome. Hum. Reprod. 2021, 37, 129–141. [Google Scholar] [CrossRef]
- Ashraf, S.; Aslam, R.; Bashir, I.; Majeed, I.; Jamshaid, M. Environmental determinants and PCOS symptoms severity: A cross-sectional study. Health Care Women Int. 2022, 43, 98–113. [Google Scholar] [CrossRef]
- Nasiri, M.; Monazzami, A.; Alavimilani, S.; Asemi, Z. The Effect of High Intensity Intermittent and Combined (Resistant and Endurance) Trainings on Some Anthropometric Indices and Aerobic Performance in Women with Polycystic Ovary Syndrome: A Randomized Controlled Clinical Trial Study. Int. J. Fertil. Steril. 2022, 16, 268–274. [Google Scholar]
- De Souza, S.A.F.; Faintuch, J.; Sant’Anna, A.F. Effect of weight loss on aerobic capacity in patients with severe obesity before and after bariatric surgery. Obes. Surg. 2010, 20, 871–875. [Google Scholar] [CrossRef] [PubMed]
- Paluch, A.E.; Bajpai, S.; Bassett, D.R.; Carnethon, M.R.; Ekelund, U.; Evenson, K.R.; Galuska, D.A.; Jefferis, B.J.; Kraus, W.E.; Lee, I.-M.; et al. Daily steps and all-cause mortality: A meta-analysis of 15 international cohorts. Lancet Public Health 2022, 7, e219–e228. [Google Scholar] [CrossRef] [PubMed]
- Ee, C.; Pirotta, S.; Mousa, A.; Moran, L.; Lim, S. Providing lifestyle advice to women with PCOS: An overview of practical issues affecting success. BMC Endocr. Disord. 2021, 21, 234. [Google Scholar] [CrossRef] [PubMed]
- Qiang, C.Z.; Yamamichi, M.; Hausman, V.; Altman, D.; Unit, I.S. Mobile Applications for the Health Sector; World Bank: Washington, DC, USA, 2011; Volume 2. [Google Scholar]
- Wang, L.; Guo, Y.; Wang, M.; Zhao, Y. A mobile health application to support self-management in patients with chronic obstructive pulmonary disease: A randomised controlled trial. Clin. Rehabil. 2021, 35, 90–101. [Google Scholar] [CrossRef]
- Wang, L.; Liu, Y.; Tan, H.; Huang, S. Transtheoretical model-based mobile health application for PCOS. Reprod. Health 2022, 19, 117. [Google Scholar] [CrossRef]
- Boyle, J.A.; Xu, R.; Gilbert, E.; Kuczynska-Burggraf, M.; Tan, B.; Teede, H.; Vincent, A.; Gibson-Helm, M.; Boyle, J.A. Ask PCOS: Identifying Need to Inform Evidence-Based App Development for Polycystic Ovary Syndrome. Semin. Reprod. Med. 2018, 36, 59–65. [Google Scholar]
- Xie, J.; Burstein, F.; Teede, H.J.; Boyle, J.A.; Garad, R. Personalized Mobile Tool AskPCOS Delivering Evidence-Based Quality Information about Polycystic Ovary Syndrome. Semin. Reprod. Med. 2018, 36, 66–72. [Google Scholar] [CrossRef]
- Althubaiti, A. Information bias in health research: Definition, pitfalls, and adjustment methods. J. Multidiscip. Healthc 2016, 9, 211–217. [Google Scholar] [CrossRef]
- Fletcher, G.F.; Ades, P.A.; Kligfield, P.; Arena, P. Exercise standards for testing and training: A scientific statement from the American Heart Association. Circulation 2013, 128, 873–934. [Google Scholar] [CrossRef]
- Kokkinos, P.; Kaminsky, L.A.; Arena, R.; Zhang, J.; Myers, J. A new generalized cycle ergometry equation for predicting maximal oxygen uptake: The Fitness Registry and the Importance of Exercise National Database (FRIEND). Eur. J. Prev. Cardiol. 2018, 25, 1077–1082. [Google Scholar] [CrossRef]
|
|
|
|
|
|
|
|
|
|
| Lifestyle Intervention | Care as Usual | |||||
|---|---|---|---|---|---|---|
| SMS+ n = 60 | Missing Values | SMS− n = 63 | Missing Values | n = 60 | Missing Values | |
| n (%) | n | n (%) | n | n (%) | n | |
| Nulliparous | 47 (79.7) | 1 | 47 (75.8) | 1 | 44 (75.9) | 2 |
| Caucasian | 30 (50.0) | - | 21 (35.0) | 3 | 25 (42.4) | 1 |
| Smoking | 13 (21.7) | - | 11 (17.7) | 1 | 14 (23.7) | 1 |
| Alcohol consumption | 12 (20.0) | - | 15 (24.2) | 1 | 19 (32.2) | 1 |
| Education | ||||||
| Low | 5 (8.3) | - | 5 (8.2) | 2 | 8 (14.3) | 4 |
| Intermediate | 33 (55.0) | - | 34 (55.7) | 2 | 35 (62.5) | 4 |
| High | 22 (36.7) | - | 22 (36.1) | 2 | 13 (23.2) | 4 |
| IPAQ physical activity category | n = 45 | n = 46 | n = 41 | |||
| Low | 2 (4.4) | 3 (6.5) | 5 (12.2) | |||
| Moderate | 16 (35.6) | 15 (32.6) | 10 (24.4) | |||
| High | 27 (61.4) | 28 (60.9) | 26 (63.4) | |||
| Median (IQR) | Missing values n | Median (IQR) | Missing values n | Median (IQR) | Missing values n | |
| Age (year) | 28 (26–32) | - | 30 (27–33) | 1 | 28 (26–32) | - |
| Weight (kg) | 95 (85–106) | - | 89 (80–104) | 1 | 84 (79–97) | - |
| BMI (kg/m²) | 33.5 (30.9–37.1) | - | 33.6 (30.4–36.0) | 1 | 30.6 (29.3–34.3) | - |
| Waist (cm) | 102 (94–110) | 4 | 100 (93–107) | 4 | 96 (89–109) | 1 |
| IPAQ | n = 46 | n = 47 | n = 43 | |||
| Walking (METmin/week) | 792 (330–2112) | 1148 (446–2153) | 1931 (512–4158) | |||
| Moderate (METmin/week) | 1935 (686–4447) | 2160 (1050–4187) | 1350 (720–3300) | |||
| Vigorous (METmin/week) | 960 (240–3840) | 1096 (380–3540) | 1440 (520–5280) | |||
| Total physical activity (METmin/week) | 3834 (2007–5567) | 3911 (2084–6555) | 3960 (1973–8573) | |||
| Sitting (min/week) | 2520 (1710–3630) | 2730 (1725–3240) | 2865 (1725–3360) | |||
| Maximum cycle ergometer test | n = 31 | n = 23 | ||||
| Peak load | 179 (148–210) | 166 (134–208) | - | |||
| Peak heart rate | 173 (170–181) | 168 (162–178) | - | |||
| mBorg | 7 (4–7) | 6 (5–8) | - | |||
| SMS+ vs. CAU Difference | p Value | SMS− vs. CAU Difference | p Value | SMS+ vs. SMS− Difference | p Value | |
|---|---|---|---|---|---|---|
| Category % | ||||||
| Low | −2.2 | 0.312 | 4.9 | 0.543 | −7.1 | 0.232 |
| Moderate | −18.9 | 0.182 | −4.0 | 0.823 | −14.9 | 0.220 |
| High | 22.6 | 0.079 | −1.5 | 0.922 | 24.0 | 0.060 |
| Domains METmin/week | ||||||
| Work | 1574 | 0.293 | 1615 | 0.318 | −42 | 0.981 |
| Transport | −7 | 0.952 | 259 | 0.635 | −266 | 0.479 |
| Domestic and garden | −776 | 0.145 | −264 | 0.665 | −512 | 0.330 |
| Leisure | 547 | 0.502 | −103 | 0.883 | 650 | 0.298 |
| Intensity METmin/week | ||||||
| Walking | 1106 | 0.047 | 403 | 0.421 | 703 | 0.134 |
| Moderate | −645 | 0.351 | −508 | 0.417 | −138 | 0.833 |
| Vigorous | 622 | 0.634 | 293 | 0.824 | 329 | 0.797 |
| Total physical activity | 2095 | 0.195 | 530 | 0.195 | 1565 | 0.243 |
| Sedentary behaviour min/week | ||||||
| Total sitting | −510 | 0.172 | 55 | 0.858 | −565 | 0.141 |
| IPAQ Responses | Group | Baseline | 3 Months | 6 Months | 9 Months | 12 Months | ||
|---|---|---|---|---|---|---|---|---|
| n | SMS+ | 46 | 21 | 10 | 8 | 5 | ||
| n | SMS− | 47 | 29 | 22 | 17 | 14 | ||
| n | CAU | 43 | 21 | 28 | 21 | 11 | ||
| Domains METmin/week | Group | Baseline | 3 months | 6 months | 9 months | 12 months | Change | p value within |
| Work | SMS+ | 3704 | 3845 | 3902 | 3938 | 3964 | 260 | 0.858 |
| SMS− | 3428 | 3591 | 3656 | 3698 | 3729 | 302 | 0.823 | |
| CAU | 5047 | 4337 | 4050 | 3867 | 3733 | −1313 | 0.200 | |
| Transport | SMS+ | 1203 | 1169 | 1155 | 1147 | 1140 | −63 | 0.826 |
| SMS− | 987 | 1097 | 1141 | 1169 | 1190 | 203 | 0.421 | |
| CAU | 1217 | 1187 | 1174 | 1167 | 1161 | −56 | 0.904 | |
| Domestic and garden | SMS+ | 1633 | 1392 | 1295 | 1233 | 1187 | −446 | 0.251 |
| SMS− | 1531 | 1567 | 1581 | 1590 | 1597 | 66 | 0.853 | |
| CAU | 1446 | 1624 | 1697 | 1743 | 1776 | 331 | 0.220 | |
| Leisure | SMS+ | 1348 | 1783 | 1959 | 2071 | 2153 | 805 | 0.132 |
| SMS− | 1393 | 1477 | 1510 | 1532 | 1548 | 155 | 0.639 | |
| CAU | 1481 | 1620 | 1677 | 1713 | 1739 | 258 | 0.661 | |
| Intensity METmin/week | Group | Baseline | 3 months | 6 months | 9 months | 12 months | Change | p value within |
| Walking | SMS+ | 1404 | 1757 | 1899 | 1990 | 2057 | 652 | 0.063 |
| SMS− | 1483 | 1455 | 1444 | 1437 | 1432 | −51 | 0.879 | |
| CAU | 2131 | 1886 | 1787 | 1724 | 1677 | −453 | 0.245 | |
| Moderate | SMS+ | 2505 | 2563 | 2587 | 2602 | 2613 | 107 | 0.833 |
| SMS− | 2446 | 2579 | 2632 | 2666 | 2691 | 245 | 0.590 | |
| CAU | 2094 | 2500 | 2665 | 2769 | 2846 | 753 | 0.066 | |
| Vigorous | SMS+ | 2366 | 2415 | 2435 | 2448 | 2457 | 91 | 0.927 |
| SMS− | 2609 | 2481 | 2429 | 2396 | 2371 | −238 | 0.835 | |
| CAU | 3203 | 2916 | 2800 | 2726 | 2672 | −531 | 0.660 | |
| Total physical activity | SMS+ | 5031 | 6207 | 6681 | 6984 | 7206 | 2175 | 0.043 |
| SMS− | 5186 | 5516 | 5649 | 5734 | 5796 | 610 | 0.460 | |
| CAU | 5986 | 6029 | 6046 | 6057 | 6065 | 80 | 0.944 | |
| Sedentary min/week | Group | Baseline | 3 months | 6 months | 9 months | 12 months | Change | p value within |
| Total sitting | SMS+ | 2735 | 2265 | 2074 | 1953 | 1864 | −871 | 0.005 |
| SMS− | 2563 | 2397 | 2331 | 2288 | 2257 | −306 | 0.183 | |
| CAU | 2559 | 2364 | 2285 | 2235 | 2198 | −361 | 0.157 |
| Group | Baseline | 3 Months | 6 Months | 9 Months | 12 Months | Change | p Value within | p Value between | |
|---|---|---|---|---|---|---|---|---|---|
| Max performance n (total) | SMS+ | 31 (46) | 22 (25) | 13 (15) | 11 (12) | 9 (11) | - | - | - |
| SMS− | 23 (40) | 25 (29) | 19 (22) | 14 (18) | 16 (19) | - | - | - | |
| Peak load (watts) | SMS+ | 177 | 182 | 184 | 186 | 187 | 10 | 0.016 | 0.222 |
| SMS− | 168 | 169 | 170 | 170 | 170 | 3 | 0.516 | ||
| % of achieved maximum HR * | SMS+ | 93 | 93 | 93 | 93 | 93 | 0 | 0.557 | 0.195 |
| SMS− | 92 | 93 | 93 | 93 | 93 | 1 | 0.228 | ||
| Peak HR (BPM) | SMS+ | 175 | 174 | 173 | 173 | 173 | −2 | 0.226 | 0.173 |
| SMS− | 172 | 172 | 173 | 173 | 173 | 1 | 0.442 | ||
| mBorg | SMS+ | 6 | 6 | 6 | 6 | 6 | 0 | 0.688 | 0.552 |
| SMS− | 6 | 6 | 6 | 6 | 6 | 0 | 0.647 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dietz de Loos, A.; Jiskoot, G.; van den Berg-Emons, R.; Louwers, Y.; Beerthuizen, A.; van Busschbach, J.; Laven, J. The Effect of Tailored Short Message Service (SMS) on Physical Activity: Results from a Three-Component Randomized Controlled Lifestyle Intervention in Women with PCOS. J. Clin. Med. 2023, 12, 2466. https://doi.org/10.3390/jcm12072466
Dietz de Loos A, Jiskoot G, van den Berg-Emons R, Louwers Y, Beerthuizen A, van Busschbach J, Laven J. The Effect of Tailored Short Message Service (SMS) on Physical Activity: Results from a Three-Component Randomized Controlled Lifestyle Intervention in Women with PCOS. Journal of Clinical Medicine. 2023; 12(7):2466. https://doi.org/10.3390/jcm12072466
Chicago/Turabian StyleDietz de Loos, Alexandra, Geranne Jiskoot, Rita van den Berg-Emons, Yvonne Louwers, Annemerle Beerthuizen, Jan van Busschbach, and Joop Laven. 2023. "The Effect of Tailored Short Message Service (SMS) on Physical Activity: Results from a Three-Component Randomized Controlled Lifestyle Intervention in Women with PCOS" Journal of Clinical Medicine 12, no. 7: 2466. https://doi.org/10.3390/jcm12072466
APA StyleDietz de Loos, A., Jiskoot, G., van den Berg-Emons, R., Louwers, Y., Beerthuizen, A., van Busschbach, J., & Laven, J. (2023). The Effect of Tailored Short Message Service (SMS) on Physical Activity: Results from a Three-Component Randomized Controlled Lifestyle Intervention in Women with PCOS. Journal of Clinical Medicine, 12(7), 2466. https://doi.org/10.3390/jcm12072466





