SEMAC + VAT for Suppression of Artifacts Induced by Dental-Implant-Supported Restorations in Magnetic Resonance Imaging
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Specimen Preparation
2.3. Magnetic Resonance Imaging
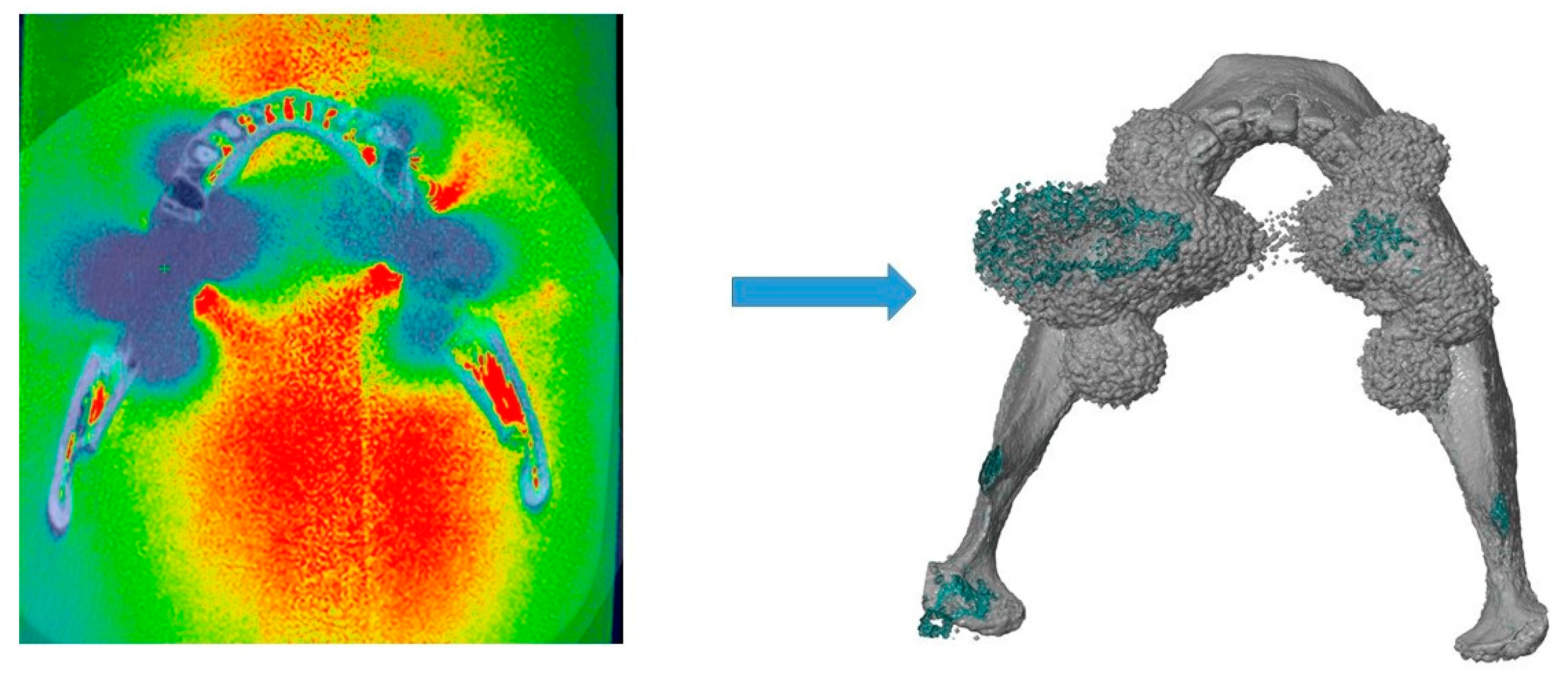
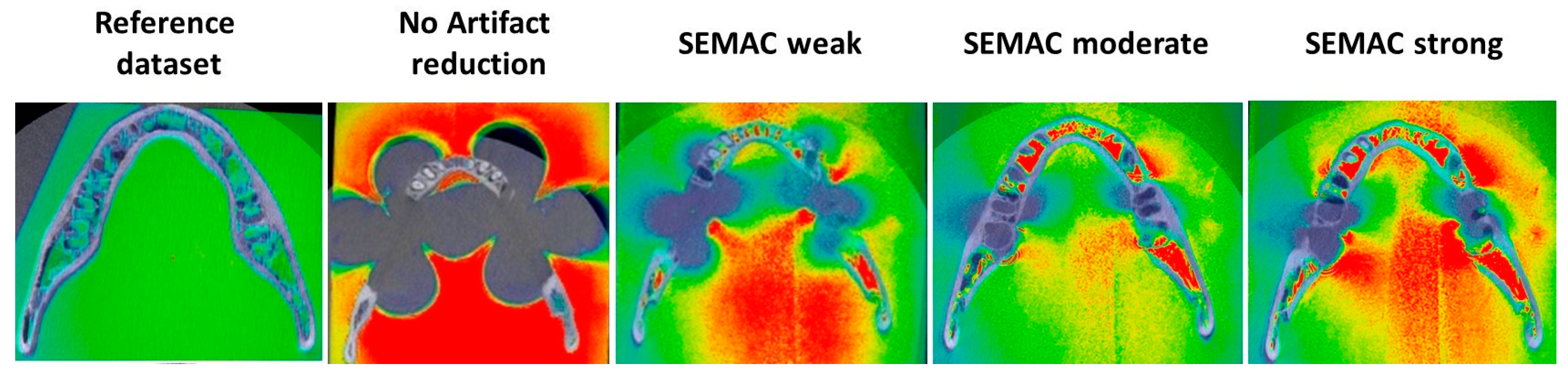
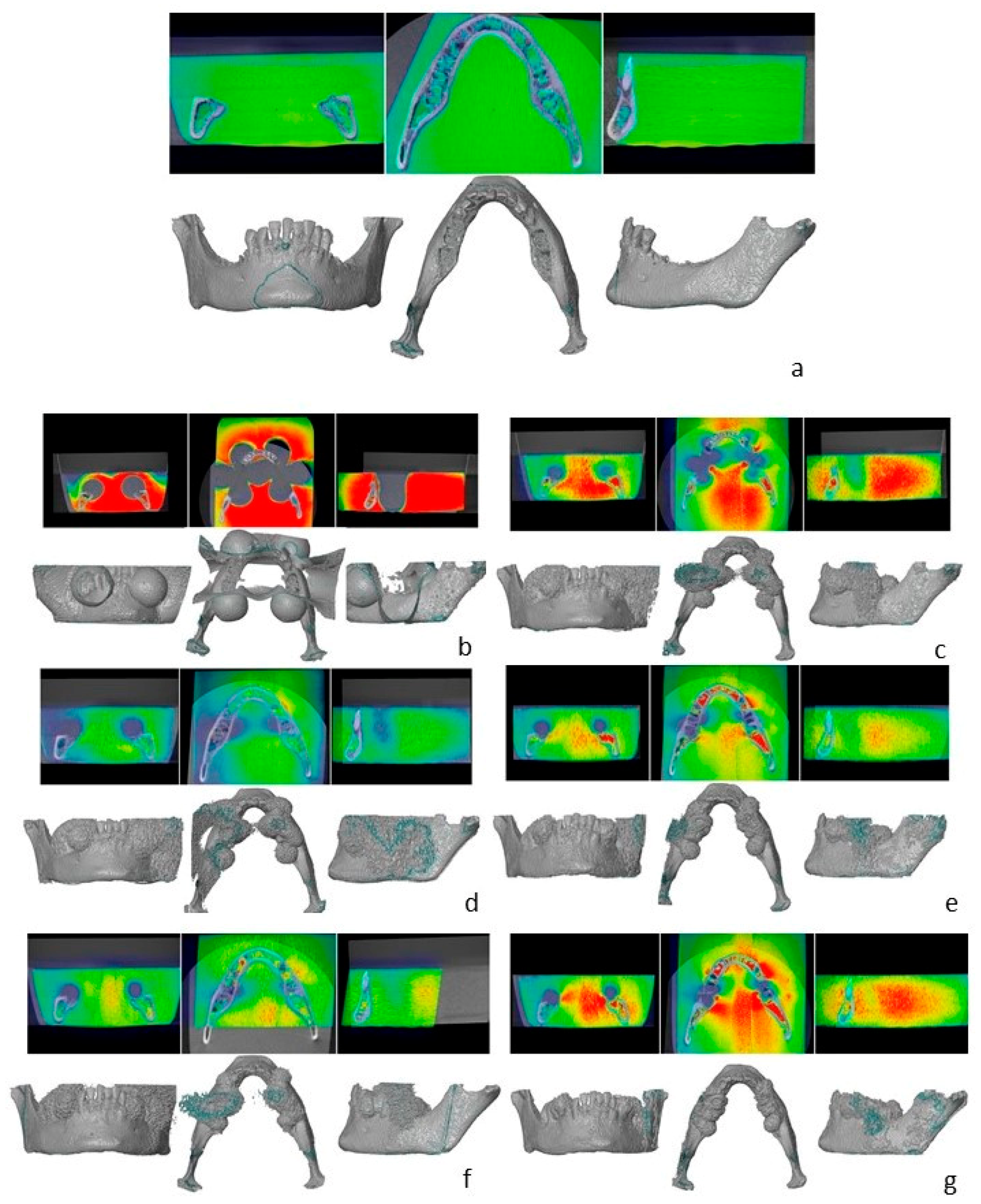
2.4. Artifact Assessment
2.5. Image Quality
2.6. Statistical Analysis
3. Results
3.1. Artifact Assessment
3.2. Image Quality
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mercado, F.; Mukaddam, K.; Filippi, A.; Bieri, O.P.; Lambrecht, T.J.; Kuhl, S. Fully Digitally Guided Implant Surgery Based on Magnetic Resonance Imaging. Int. J. Oral Maxillofac. Implant. 2019, 34, 529–534. [Google Scholar] [CrossRef] [PubMed]
- Zidan, M.; Schwindling, F.S.; Juerchott, A.; Mente, J.; Gehrig, H.; Nittka, M.; Hosseini, Z.; Jende, J.M.E.; Heiland, S.; Bendszus, M.; et al. Endodontic working length measurements of premolars and molars in high-resolution dental MRI: A clinical pilot study for assessment of reliability and accuracy. Clin. Oral Investig. 2022, 26, 6765–6772. [Google Scholar] [CrossRef] [PubMed]
- Wanner, L.; Ludwig, U.; Hovener, J.B.; Nelson, K.; Flugge, T. Magnetic resonance imaging-a diagnostic tool for postoperative evaluation of dental implants: A case report. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2018, 125, e103–e107. [Google Scholar] [CrossRef] [PubMed]
- Flugge, T.; Ludwig, U.; Hovener, J.B.; Kohal, R.; Wismeijer, D.; Nelson, K. Virtual implant planning and fully guided implant surgery using magnetic resonance imaging-Proof of principle. Clin. Oral Implant. Res. 2020, 31, 575–583. [Google Scholar] [CrossRef]
- Flugge, T.; Ludwig, U.; Winter, G.; Amrein, P.; Kernen, F.; Nelson, K. Fully guided implant surgery using Magnetic Resonance Imaging—An in vitro study on accuracy in human mandibles. Clin. Oral Implant. Res. 2020, 31, 737–746. [Google Scholar] [CrossRef]
- de Carvalho, E.S.F.J.M.; Wenzel, A.; Hansen, B.; Lund, T.E.; Spin-Neto, R. Magnetic Resonance Imaging for the Planning, Execution, and Follow-up of Implant-Based Oral Rehabilitation: Systematic Review. Int. J. Oral Maxillofac. Implant. 2021, 36, 432–441. [Google Scholar] [CrossRef]
- Juerchott, A.; Saleem, M.A.; Hilgenfeld, T.; Freudlsperger, C.; Zingler, S.; Lux, C.J.; Bendszus, M.; Heiland, S. 3D cephalometric analysis using Magnetic Resonance Imaging: Validation of accuracy and reproducibility. Sci. Rep. 2018, 8, 13029. [Google Scholar] [CrossRef]
- Hargreaves, B.A.; Worters, P.W.; Pauly, K.B.; Pauly, J.M.; Koch, K.M.; Gold, G.E. Metal-induced artifacts in MRI. AJR Am. J. Roentgenol. 2011, 197, 547–555. [Google Scholar] [CrossRef]
- Murakami, S.; Verdonschot, R.G.; Kataoka, M.; Kakimoto, N.; Shimamoto, H.; Kreiborg, S. A standardized evaluation of artefacts from metallic compounds during fast MR imaging. Dentomaxillofac. Radiol. 2016, 45, 20160094. [Google Scholar] [CrossRef]
- Bohner, L.; Hanisch, M.; Sesma, N.; Blanck-Lubarsch, M.; Kleinheinz, J. Artifacts in magnetic resonance imaging caused by dental materials: A systematic review. Dentomaxillofac. Radiol. 2022, 51, 20210450. [Google Scholar] [CrossRef]
- Germann, C.; Nanz, D.; Sutter, R. Magnetic Resonance Imaging Around Metal at 1.5 Tesla Techniques From Basic to Advanced and Clinical Impact. Investig. Radiol. 2021, 56, 734–748. [Google Scholar] [CrossRef] [PubMed]
- Ganapathi, M.; Joseph, G.; Savage, R.; Jones, A.R.; Timms, B.; Lyons, K. MRI susceptibility artefacts related to scaphoid screws: The effect of screw type, screw orientation and imaging parameters. J. Hand. Surg. Br. 2002, 27, 165–170. [Google Scholar] [CrossRef] [PubMed]
- Graham, M.S.; Drobnjak, I.; Jenkinson, M.; Zhang, H. Quantitative assessment of the susceptibility artefact and its interaction with motion in diffusion MRI. PLoS ONE 2017, 12, e0185647. [Google Scholar] [CrossRef] [PubMed]
- Ai, T.; Padua, A.; Goerner, F.; Nittka, M.; Gugala, Z.; Jadhav, S.; Trelles, M.; Johnson, R.F.; Lindsey, R.W.; Li, X.; et al. SEMAC-VAT and MSVAT-SPACE sequence strategies for metal artifact reduction in 1.5T magnetic resonance imaging. Invest. Radiol. 2012, 47, 267–276. [Google Scholar] [CrossRef] [PubMed]
- Amin, N.; Pai, I.; Touska, P.; Connor, S.E.J. Utilization of SEMAC-VAT MRI for Improved Visualization of Posterior Fossa Structures in Patients With Cochlear Implants. Otol. Neurotol. 2021, 42, e451–e458. [Google Scholar] [CrossRef] [PubMed]
- Filli, L.; Jud, L.; Luechinger, R.; Nanz, D.; Andreisek, G.; Runge, V.M.; Kozerke, S.; Farshad-Amacker, N.A. Material-Dependent Implant Artifact Reduction Using SEMAC-VAT and MAVRIC: A Prospective MRI Phantom Study. Invest. Radiol. 2017, 52, 381–387. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.H.; Lim, D.; Kim, E.; Kim, S.; Song, H.T.; Suh, J.S. Usefulness of slice encoding for metal artifact correction (SEMAC) for reducing metallic artifacts in 3-T MRI. Magn. Reson. Imaging 2013, 31, 703–706. [Google Scholar] [CrossRef]
- Hilgenfeld, T.; Prager, M.; Schwindling, F.S.; Nittka, M.; Rammelsberg, P.; Bendszus, M.; Heiland, S.; Juerchott, A. MSVAT-SPACE-STIR and SEMAC-STIR for Reduction of Metallic Artifacts in 3T Head and Neck MRI. AJNR Am. J. Neuroradiol. 2018, 39, 1322–1329. [Google Scholar] [CrossRef]
- Reda, R.; Zanza, A.; Mazzoni, A.; Cicconetti, A.; Testarelli, L.; Di Nardo, D. An Update of the Possible Applications of Magnetic Resonance Imaging (MRI) in Dentistry: A Literature Review. J. Imaging 2021, 7, 75. [Google Scholar] [CrossRef]
- Graves, M.J.; Mitchell, D.G. Body MRI artifacts in clinical practice: A physicist’s and radiologist’s perspective. J. Magn. Reson. Imaging 2013, 38, 269–287. [Google Scholar] [CrossRef]
- Probst, M.; Richter, V.; Weitz, J.; Kirschke, J.S.; Ganter, C.; Troeltzsch, M.; Nittka, M.; Cornelius, C.P.; Zimmer, C.; Probst, F.A. Magnetic resonance imaging of the inferior alveolar nerve with special regard to metal artifact reduction. J. Craniomaxillofac. Surg. 2017, 45, 558–569. [Google Scholar] [CrossRef] [PubMed]
- Gunzinger, J.M.; Delso, G.; Boss, A.; Porto, M.; Davison, H.; von Schulthess, G.K.; Huellner, M.; Stolzmann, P.; Veit-Haibach, P.; Burger, I.A. Metal artifact reduction in patients with dental implants using multispectral three-dimensional data acquisition for hybrid PET/MRI. EJNMMI Phys. 2014, 1, 102. [Google Scholar] [CrossRef] [PubMed]
- Zho, S.Y.; Kim, M.O.; Lee, K.W.; Kim, D.H. Artifact reduction from metallic dental materials in T1-weighted spin-echo imaging at 3.0 tesla. J. Magn. Reson. Imaging 2013, 37, 471–478. [Google Scholar] [CrossRef] [PubMed]
- Shafiei, F.; Honda, E.; Takahashi, H.; Sasaki, T. Artifacts from dental casting alloys in magnetic resonance imaging. J. Dent. Res. 2003, 82, 602–606. [Google Scholar] [CrossRef]
- Peschke, E.; Ulloa, P.; Jansen, O.; Hoevener, J.B. Metallic Implants in MRI—Hazards and Imaging Artifacts. Röntgenstr 2021, 193, 1285–1293. [Google Scholar] [CrossRef]
- Gaeta, M.; Cavallaro, M.; Vinci, S.L.; Mormina, E.; Blandino, A.; Marino, M.A.; Granata, F.; Tessitore, A.; Galletta, K.; D’Angelo, T.; et al. Magnetism of materials: Theory and practice in magnetic resonance imaging. Insights Imaging 2021, 12, 179. [Google Scholar] [CrossRef]

| Dental Implants | ||
|---|---|---|
| Specifications | Material/Alloy | Brand |
| sites 35, 45: 2 dental implants - diameter × length: 4.1 × 12 mm sites 37, 47: 2 dental implants - diameter × length: 4.1 × 8 mm | Titanium Grade 4 (Ti, O ≤ 0.4%, Fe 0.25–0.5%, N ≤ 0.05%, C ≤ 0.10%, H ≤ 0.012%) | Bone level Titanium SLA, Straumann |
| Restorations | ||
| Specifications | Material/Alloy | Brand |
| sites 35–37, sites 45–47: three-unit metallic restoration | Abutment | Variobase, Straumann |
| Bridge: 63% Co, 29% Cr, 6% Mo, < 1% Fe, Mn, Nb, Si | Bridge: Colado CAD CoCr4, Ivoclar | |
| Scan | Image Parameters | Scanning Time |
|---|---|---|
| Reference dataset 3D TSE factor 16, Sense 2,3, no CS, 100 slices, first level SAR | Image voxel size 0.15 × 0.15 × 0.5 mm, FOV 140 × 100 mm | 6 min |
| No SEMAC no VAT 3D TSE factor 16, no Sense, no CS, 200 slices, first level SAR | Image voxel size 0.15 × 0.15 × 0.25 mm | 8 min |
| SEMAC + VAT weak | Image voxel size 0.25 × 0.25 × 1.0 mm | 5 min |
| SEMAC + VAT weak strong FID reduction and TSE 8 | Image voxel size 0.25 × 0.25 × 1.0 mm | 5 min |
| SEMAC + VAT medium 54 slices | Image voxel size 0.25 × 0.25 × 1.0 mm | 10 min |
| SEMAC + VAT medium Slice encoding in transverse direction, 80 slices | Image voxel size 0.25 × 0.25 × 1.0 mm, FOV 160 × 80 mm | 15 min |
| SEMAC + VAT strong | Image voxel size 0.25 × 0.25 × 1.0 mm | 23 min |
| Volume (cm3) | Volume Increase (%) | |
|---|---|---|
| Reference dataset | 3.654, 85 | - |
| No | 7.348, 17 | 60, 23 |
| SEMAC + VAT weak | 5.856, 21 | 31, 47 |
| SEMAC + VAT weak | 4.858, 25 | 32, 77 |
| SEMAC + VAT medium | 4.805, 39 | 19, 76 |
| SEMAC + VAT medium | 4.377, 16 | 19, 33 |
| SEMAC + VAT strong | 4.311, 21 | 17, 13 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bohner, L.; Hanisch, M.; Parize, H.; Sesma, N.; Kleinheinz, J.; Meier, N. SEMAC + VAT for Suppression of Artifacts Induced by Dental-Implant-Supported Restorations in Magnetic Resonance Imaging. J. Clin. Med. 2023, 12, 1117. https://doi.org/10.3390/jcm12031117
Bohner L, Hanisch M, Parize H, Sesma N, Kleinheinz J, Meier N. SEMAC + VAT for Suppression of Artifacts Induced by Dental-Implant-Supported Restorations in Magnetic Resonance Imaging. Journal of Clinical Medicine. 2023; 12(3):1117. https://doi.org/10.3390/jcm12031117
Chicago/Turabian StyleBohner, Lauren, Marcel Hanisch, Hian Parize, Newton Sesma, Johannes Kleinheinz, and Norbert Meier. 2023. "SEMAC + VAT for Suppression of Artifacts Induced by Dental-Implant-Supported Restorations in Magnetic Resonance Imaging" Journal of Clinical Medicine 12, no. 3: 1117. https://doi.org/10.3390/jcm12031117
APA StyleBohner, L., Hanisch, M., Parize, H., Sesma, N., Kleinheinz, J., & Meier, N. (2023). SEMAC + VAT for Suppression of Artifacts Induced by Dental-Implant-Supported Restorations in Magnetic Resonance Imaging. Journal of Clinical Medicine, 12(3), 1117. https://doi.org/10.3390/jcm12031117







