Sociodemographic, Behavioural, and Health Factors Associated with Sedentary Behaviour in Community-Dwelling Older Adults: A Nationwide Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Sedentary Behaviour and Physical Activity
2.3. Variables
2.4. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Sociodemographic Factors Associated with Sedentary Behaviour
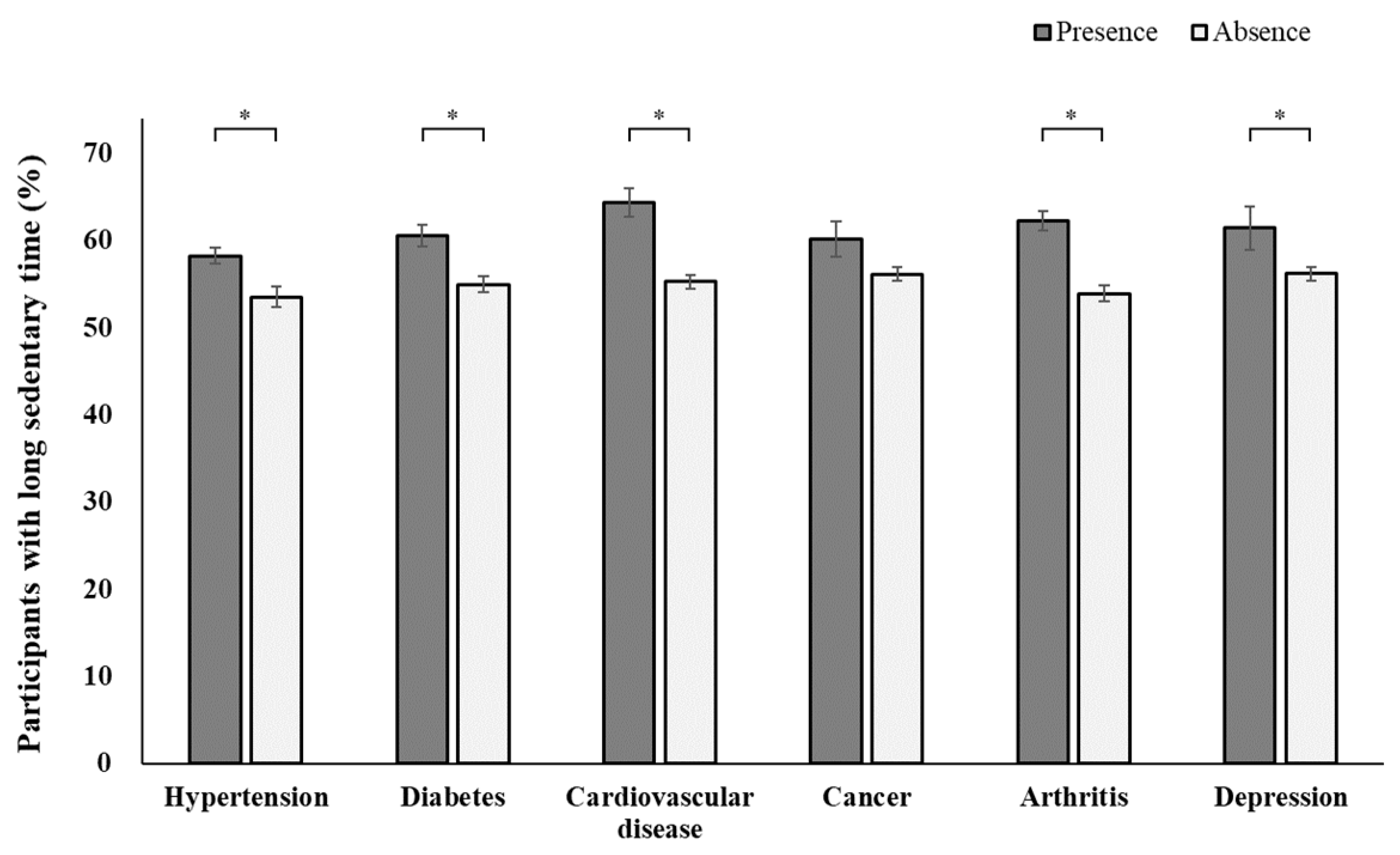
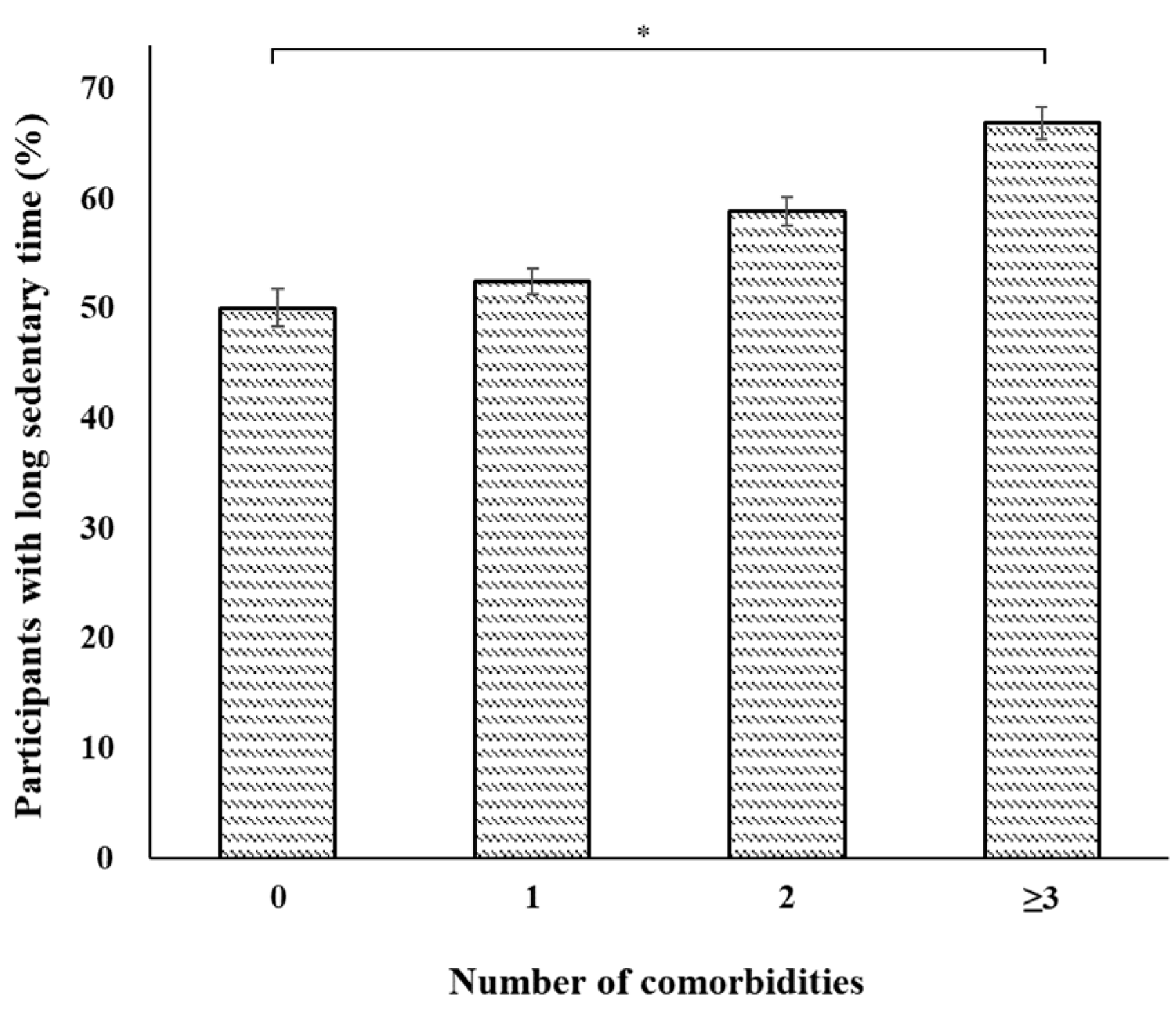
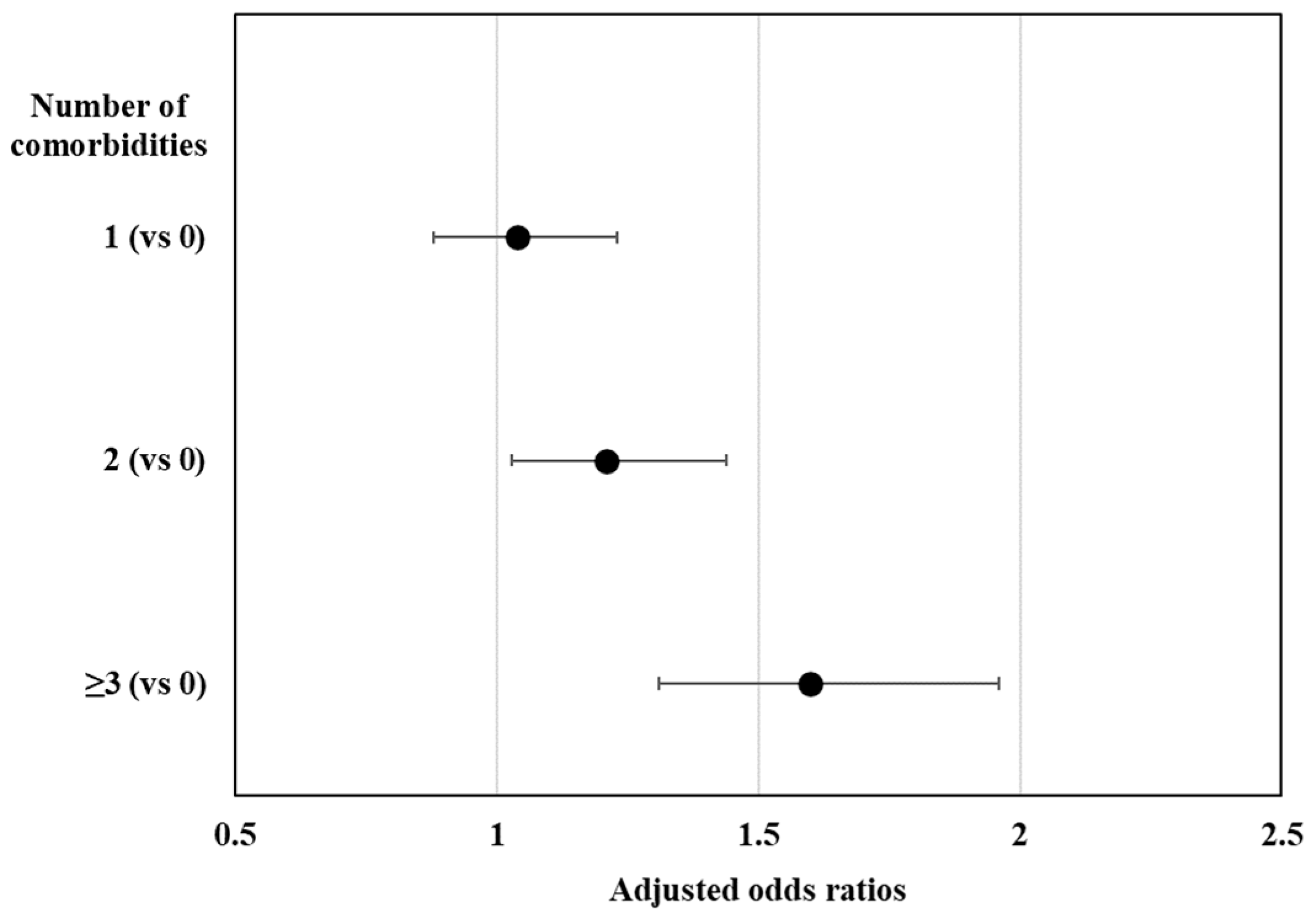
3.3. Behavioural and Health Factors Associated with Sedentary Behaviour
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tremblay, M.S.; Aubert, S.; Barnes, J.D.; Saunders, T.J.; Carson, V.; Latimer-Cheung, A.E.; Chastin, S.F.M.; Altenburg, T.M.; Chinapaw, M.J.M.; SBRN Terminology Consensus Project Participants. Sedentary Behavior Research Network (SBRN). Int J Behav. Nutr. Phys. Act. 2017, 14, 75. [Google Scholar] [CrossRef]
- Harvey, J.A.; Chastin, S.F.; Skelton, D.A. How sedentary are older people? A systematic review of the amount of sedentary behavior. J. Aging Phys. Act. 2015, 23, 471–487. [Google Scholar] [CrossRef]
- De Rezende, L.F.; Rey-López, J.P.; Matsudo, V.K.; do Carmo Luiz, O. Sedentary behavior and health outcomes among older adults: A systematic review. BMC Public Health 2014, 14, 333. [Google Scholar] [CrossRef]
- Felez-Nobrega, M.; Olaya, B.; Haro, J.M.; Stubbs, B.; Smith, L.; Koyanagi, A. Associations between sedentary behavior and happiness: An analysis of influential factors among middle-aged and older adults from six low- and middle-income countries. Maturitas 2021, 143, 157–164. [Google Scholar] [CrossRef]
- Ozaki, E.; Matsui, D.; Kuriyama, N.; Tomida, S.; Nukaya, Y.; Koyama, T. Association between sedentary time and falls among middle-aged women in Japan. Healthcare 2022, 10, 2354. [Google Scholar] [CrossRef] [PubMed]
- Gianoudis, J.; Bailey, C.A.; Daly, R.M. Associations between sedentary behaviour and body composition, muscle function and sarcopenia in community-dwelling older adults. Osteoporos. Int. 2015, 26, 571–579. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, V.D.; Tribess, S.; Meneguci, J.; Sasaki, J.E.; Garcia-Meneguci, C.A.; Carneiro, J.A.O.; Virtuoso, J.S. Association between frailty and the combination of physical activity level and sedentary behavior in older adults. BMC Public Health 2019, 19, 709. [Google Scholar] [CrossRef] [PubMed]
- Owen, N.; Sugiyama, T.; Eakin, E.E.; Gardiner, P.A.; Tremblay, M.S.; Sallis, J.F. Adults’ sedentary behavior determinants and interventions. Am. J. Prev. Med. 2011, 41, 189–196. [Google Scholar] [CrossRef]
- Chastin, S.F.; De Craemer, M.; Lien, N.; Bernaards, C.; Buck, C.; Oppert, J.M.; Nazare, J.A.; Lakerveld, J.; O’Donoghue, G.; Holdsworth, M.; et al. The SOS-framework (Systems of Sedentary behaviours): An international transdisciplinary consensus framework for the study of determinants, research priorities and policy on sedentary behaviour across the life course: A DEDIPAC-study. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 83. [Google Scholar] [CrossRef]
- van der Berg, J.D.; Bosma, H.; Caserotti, P.; Eiriksdottir, G.; Arnardottir, N.Y.; Martin, K.R.; Brychta, R.J.; Chen, K.Y.; Sveinsson, T.; Johannsson, E.; et al. Midlife determinants associated with sedentary behavior in old age. Med. Sci. Sports Exerc. 2014, 46, 1359–1365. [Google Scholar] [CrossRef]
- Heseltine, R.; Skelton, D.A.; Kendrick, D.; Morris, R.W.; Griffin, M.; Haworth, D.; Masud, T.; Iliffe, S. ‘Keeping Moving’: Factors associated with sedentary behaviour among older people recruited to an exercise promotion trial in general practice. BMC Fam. Pract. 2015, 16, 67. [Google Scholar] [CrossRef]
- Chastin, S.F.; Buck, C.; Freiberger, E.; Murphy, M.; Brug, J.; Cardon, G.; O’Donoghue, G.; Pigeot, I.; Oppert, J.M. DEDIPAC consortium Systematic literature review of determinants of sedentary behaviour in older adults: A DEDIPAC study. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 127. [Google Scholar] [CrossRef] [PubMed]
- Clark, B.K.; Sugiyama, T.; Healy, G.N.; Salmon, J.; Dunstan, D.W.; Shaw, J.E.; Zimmet, P.Z.; Owen, N. Socio-demographic correlates of prolonged television viewing time in Australian men and women: The AusDiab study. J. Phys. Act. Health 2010, 7, 595–601. [Google Scholar] [CrossRef] [PubMed]
- King, A.C.; Goldberg, J.H.; Salmon, J.; Owen, N.; Dunstan, D.; Weber, D.; Doyle, C.; Robinson, T.N. Identifying subgroups of U.S. adults at risk for prolonged television viewing to inform program development. Am. J. Prev. Med. 2010, 38, 17–26. [Google Scholar] [CrossRef]
- Olanrewaju, O.; Stockwell, S.; Stubbs, B.; Smith, L. Sedentary behaviours, cognitive function, and possible mechanisms in older adults: A systematic review. Aging Clin. Exp. Res. 2020, 32, 969–984. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.A.; Lee, J.S.; Park, J.H.; Kim, Y.H. Patterns of physical activity and sedentary behavior and their associated factors among nondisabled stroke survivors. Maturitas 2022, 158, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, T.; Bull, F. Development of the World Health Organization global physical activity questionnaire (GPAQ). J. Public Health 2006, 14, 66–70. [Google Scholar] [CrossRef]
- World Health Organization Global Physical Activity Questionnaire (GPAQ) Analysis Guide. Available online: https://www.who.int/teams/noncommunicable-diseases/surveillance/systems-tools/physical-activity-surveillance (accessed on 2 December 2022).
- Lee, J.; Lee, C.; Min, J.; Kang, D.W.; Kim, J.Y.; Yang, H.I.; Park, J.; Lee, M.K.; Lee, M.Y.; Park, I.; et al. Development of the Korean Global Physical Activity Questionnaire: Reliability and validity study. Glob. Health Promot. 2020, 27, 44–55. [Google Scholar] [CrossRef] [PubMed]
- Bull, F.C.; Maslin, T.S.; Armstrong, T. Global physical activity questionnaire (GPAQ): Nine country reliability and validity study. J. Phys. Act. Health 2009, 6, 790–804. [Google Scholar] [CrossRef]
- Ku, P.W.; Steptoe, A.; Liao, Y.; Hsueh, M.C.; Chen, L.J. A cut-off of daily sedentary time and all-cause mortality in adults: A meta-regression analysis involving more than 1 million participants. BMC Med. 2018, 16, 74. [Google Scholar] [CrossRef]
- World Health Organization. Global Recommendations on Physical Activity for Health; WHO: Geneva, Switzerland, 2010. [Google Scholar]
- Loprinzi, P.D. Sedentary behavior and medical multimorbidity. Physiol. Behav. 2015, 151, 395–397. [Google Scholar] [CrossRef]
- Kandola, A.; Stubbs, B.; Koyanagi, A. Physical multimorbidity and sedentary behavior in older adults: Findings from the Irish longitudinal study on ageing (TILDA). Maturitas 2020, 134, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Compernolle, S.; Cerin, E.; Barnett, A.; Zhang, C.J.P.; Van Cauwenberg, J.; Van Dyck, D. The role of socio-demographic factors and physical functioning in the intra- and interpersonal variability of older adults’ sedentary time: An observational two-country study. BMC Geriatr. 2022, 22, 495. [Google Scholar] [CrossRef] [PubMed]
- Dohrn, I.M.; Gardiner, P.A.; Winkler, E.; Welmer, A.K. Device-measured sedentary behavior and physical activity in older adults differ by demographic and health-related factors. Eur. Rev. Aging Phys. Act. 2020, 17, 8. [Google Scholar] [CrossRef] [PubMed]
- Müller, A.M.; Chen, B.; Wang, N.X.; Whitton, C.; Direito, A.; Petrunoff, N.; Müller-Riemenschneider, F. Correlates of sedentary behaviour in Asian adults: A systematic review. Obes. Rev. 2020, 21, e12976. [Google Scholar] [CrossRef]
- Zhou, W.; Webster, K.E.; Veliz, P.T.; Larson, J.L. Profiles of sedentary behaviors in the oldest old: Findings from the National Health and Aging Trends Study. Aging Clin. Exp. Res. 2022, 34, 2071–2079. [Google Scholar] [CrossRef]
- Singh, A.; Kim, Y. What has contributed to the large sex differentials in lifespan variation and life expectancy in South Korea? J. Biosoc. Sci. 2021, 53, 396–406. [Google Scholar] [CrossRef]
- Prince, S.A.; Reed, J.L.; McFetridge, C.; Tremblay, M.S.; Reid, R.D. Correlates of sedentary behaviour in adults: A systematic review. Obes. Rev. 2017, 18, 915–935. [Google Scholar] [CrossRef]
- Kikuchi, H.; Inoue, S.; Sugiyama, T.; Owen, N.; Oka, K.; Shimomitsu, T. Correlates of prolonged television viewing time in older Japanese men and women. BMC Public Health 2013, 13, 213. [Google Scholar] [CrossRef]
- Van Cauwenberg, J.; De Donder, L.; Clarys, P.; De Bourdeaudhuij, I.; Owen, N.; Dury, S.; De Witte, N.; Buffel, T.; Verté, D.; Deforche, B. Relationships of individual, social, and physical environmental factors with older adults’ television viewing time. J. Aging Phys. Act. 2014, 22, 508–517. [Google Scholar] [CrossRef]
- Shiroma, E.J.; Freedson, P.S.; Trost, S.G.; Lee, I.M. Patterns of accelerometer-assessed sedentary behavior in older women. JAMA 2013, 310, 2562–2563. [Google Scholar] [CrossRef] [PubMed]
- Zhu, W.; Cheng, Z.; Howard, V.J.; Judd, S.E.; Blair, S.N.; Sun, Y.; Hooker, S.P. Is adiposity associated with objectively measured physical activity and sedentary behaviors in older adults? BMC Geriatr. 2020, 20, 257. [Google Scholar] [CrossRef] [PubMed]
- Yaribeygi, H.; Atkin, S.L.; Simental-Mendía, L.E.; Sahebkar, A. Molecular mechanisms by which aerobic exercise induces insulin sensitivity. J. Cell. Physiol. 2019, 234, 12385–12392. [Google Scholar] [CrossRef] [PubMed]
- Antuna-Puente, B.; Feve, B.; Fellahi, S.; Bastard, J.P. Adipokines: The missing link between insulin resistance and obesity. Diabetes Metab. 2008, 34, 2–11. [Google Scholar] [CrossRef]
- Alibegovic, A.C.; Højbjerre, L.; Sonne, M.P.; van Hall, G.; Stallknecht, B.; Dela, F.; Vaag, A. Impact of 9 days of bed rest on hepatic and peripheral insulin action, insulin secretion, and whole-body lipolysis in healthy young male offspring of patients with type 2 diabetes. Diabetes 2009, 58, 2749–2756. [Google Scholar] [CrossRef]
- Le Roux, E.; De Jong, N.P.; Blanc, S.; Simon, C.; Bessesen, D.H.; Bergouignan, A. Physiology of physical inactivity, sedentary behaviours and non-exercise activity: Insights from the space bedrest model. J. Physiol. 2022, 600, 1037–1051. [Google Scholar] [CrossRef]
- Bergouignan, A.; Momken, I.; Schoeller, D.A.; Normand, S.; Zahariev, A.; Lescure, B.; Simon, C.; Blanc, S. Regulation of energy balance during long-term physical inactivity induced by bed rest with and without exercise training. J. Clin. Endocrinol. Metab. 2010, 95, 1045–1053. [Google Scholar] [CrossRef]
- Rudwill, F.; Bergouignan, A.; Gastebois, C.; Gauquelin-Koch, G.; Lefai, E.; Blanc, S.; Simon, C. Effect of enforced physical inactivity induced by 60-day of bed rest on hepatic markers of NAFLD in healthy normal-weight women. Liver Int. 2015, 35, 1700–1706. [Google Scholar] [CrossRef]
- Trappe, S.; Trappe, T.; Gallagher, P.; Harber, M.; Alkner, B.; Tesch, P. Human single muscle fibre function with 84 day bed-rest and resistance exercise. J. Physiol. 2004, 557, 501–513. [Google Scholar] [CrossRef]
- Fenton, S.A.M.; Veldhuijzen van Zanten, J.J.C.S.; Duda, J.L.; Metsios, G.S.; Kitas, G.D. Sedentary behaviour in rheumatoid arthritis: Definition, measurement and implications for health. Rheumatology 2018, 57, 213–226. [Google Scholar] [CrossRef]
- Lee, J.; Chang, R.W.; Ehrlich-Jones, L.; Kwoh, C.K.; Nevitt, M.; Semanik, P.A.; Sharma, L.; Sohn, M.W.; Song, J.; Dunlop, D.D. Sedentary behavior and physical function: Objective evidence from the osteoarthritis Initiative. Arthritis Care Res. 2015, 67, 366–373. [Google Scholar] [CrossRef] [PubMed]
- Deguchi, N.; Kojima, N.; Osuka, Y.; Sasai, H. Factors associated with passive sedentary behavior among community-dwelling older women with and without knee osteoarthritis: The Otassha study. Int. J. Environ. Res. Public Health 2022, 19, 13765. [Google Scholar] [CrossRef]
- Kanavaki, A.M.; Rushton, A.; Hale, E.; Klocke, R.; Abhishek, A.; Duda, J.L. Physical activity, sedentary behaviour and well-being: Experiences of people with knee and hip osteoarthritis. Psychol. Health, 2022; online ahead of print. [Google Scholar] [CrossRef]
- Vancampfort, D.; Stubbs, B.; Koyanagi, A. Physical chronic conditions, multimorbidity and sedentary behavior amongst middle-aged and older adults in six low- and middle-income countries. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 147. [Google Scholar] [CrossRef] [PubMed]
- Lai, T.F.; Liao, Y.; Hsueh, M.C.; Lin, K.P.; Chan, D.C.; Chen, Y.M.; Wen, C.J. Effect of isotemporal substitution of sedentary behavior with different intensities of physical activity on the muscle function of older adults in the context of a medical center. BMC Geriatr. 2023, 23, 130. [Google Scholar] [CrossRef] [PubMed]
- Kinoshita, K.; Ozato, N.; Yamaguchi, T.; Sudo, M.; Yamashiro, Y.; Mori, K.; Ishida, M.; Katsuragi, Y.; Sasai, H.; Yasukawa, T.; et al. Association of sedentary behaviour and physical activity with cardiometabolic health in Japanese adults. Sci. Rep. 2022, 12, 2262. [Google Scholar] [CrossRef]
- Healy, G.N.; Clark, B.K.; Winkler, E.A.; Gardiner, P.A.; Brown, W.J.; Matthews, C.E. Measurement of adults’ sedentary time in population-based studies. Am. J. Prev. Med. 2011, 41, 216–227. [Google Scholar] [CrossRef] [PubMed]
| Variables | Total Participants | Short Sedentary Time | Long Sedentary Time | p Value |
|---|---|---|---|---|
| Unweighted number (n) | 8273 | 3663 | 4610 | |
| Weighted number (n) | 6,030,990 | 2,622,031 | 3,408,959 | |
| Sociodemographic factors | ||||
| Age groups | <0.001 | |||
| 65–69 | 34.32 (0.66) | 40.71 (0.96) | 29.40 (0.84) | |
| 70–74 | 26.13 (0.55) | 27.97 (0.83) | 24.72 (0.73) | |
| 75–79 | 23.67 (0.58) | 21.31 (0.86) | 25.49 (0.76) | |
| ≥80 | 15.88 (0.52) | 10.01 (0.62) | 20.39 (0.75) | |
| Sex | <0.001 | |||
| Men | 43.72 (0.56) | 47.39 (0.88) | 40.89 (0.77) | |
| Women | 56.28 (0.56) | 52.61 (0.88) | 59.11 (0.77) | |
| Education | 0.978 | |||
| ≤9 years | 72.14 (0.78) | 72.16 (1.02) | 72.13 (0.98) | |
| >9 years | 27.86 (0.78) | 27.84 (1.02) | 27.87 (0.98) | |
| Occupation | <0.001 | |||
| Employed | 32.83 (0.73) | 38.92 (1.08) | 28.16 (0.86) | |
| Unemployed | 67.17 (0.73) | 61.08 (1.08) | 71.84 (0.86) | |
| Marital status | 0.059 | |||
| Married | 99.28 (0.10) | 99.49 (0.11) | 99.13 (0.15) | |
| Unmarried | 0.72 (0.10) | 0.51 (0.11) | 0.87 (0.15) | |
| Household composition | <0.001 | |||
| Living with other | 80.21 (0.58) | 83.56 (0.68) | 77.62 (0.79) | |
| Living alone | 19.79 (0.58) | 16.44 (0.68) | 22.38 (0.79) | |
| Household income | <0.001 | |||
| Low | 45.88 (0.88) | 43.23 (1.13) | 47.91 (1.09) | |
| Lower-middle | 27.45 (0.69) | 29.40 (0.95) | 25.94 (0.86) | |
| Upper-middle | 16.03 (0.60) | 17.24 (0.83) | 15.10 (0.72) | |
| High | 10.65 (0.59) | 10.13 (0.68) | 11.05 (0.75) | |
| Residence | 0.005 | |||
| Rural | 24.03 (1.57) | 26.52 (1.89) | 22.11 (1.63) | |
| Urban | 75.97 (1.57) | 73.48 (1.89) | 77.89 (1.63) | |
| Behavioural factors | ||||
| Alcohol consumption | 0.956 | |||
| Non-excessive | 93.70 (0.32) | 93.72 (0.47) | 93.68 (0.42) | |
| Excessive | 6.30 (0.32) | 6.28 (0.47) | 6.32 (0.42) | |
| Smoking habits | 0.179 | |||
| Never | 61.86 (0.58) | 60.60 (0.93) | 62.83 (0.77) | |
| Past | 28.52 (0.54) | 29.37 (0.86) | 27.87 (0.71) | |
| Current | 9.62 (0.39) | 10.03 (0.56) | 9.30 (0.52) | |
| Aerobic exercise | <0.001 | |||
| Sufficient | 33.86 (0.69) | 42.27 (0.96) | 27.44 (0.86) | |
| Insufficient | 66.14 (0.69) | 57.73 (0.96) | 72.56 (0.86) | |
| Resistance exercise | 0.001 | |||
| Sufficient | 17.79 (0.53) | 19.87 (0.88) | 16.19 (0.65) | |
| Insufficient | 82.21 (0.53) | 80.13 (0.88) | 83.81 (0.65) | |
| Health factors | ||||
| Weight level | <0.001 | |||
| Underweight | 2.90 (0.22) | 2.68 (0.30) | 3.08 (0.30) | |
| Normal weight | 33.94 (0.64) | 36.44 (0.99) | 32.00 (0.80) | |
| Overweight | 26.23 (0.58) | 26.48 (0.88) | 26.04 (0.77) | |
| Obese | 36.92 (0.64) | 34.40 (0.96) | 38.88 (0.83) | |
| Hypertension | 62.99 (0.65) | 60.45 (0.98) | 64.95 (0.86) | <0.001 |
| Diabetes | 27.79 (0.58) | 25.24 (0.84) | 29.76 (0.77) | <0.001 |
| Cardiovascular disease | 13.50 (0.43) | 11.06 (0.58) | 15.37 (0.60) | <0.001 |
| Cancer | 10.13 (0.39) | 9.28 (0.56) | 10.78 (0.54) | 0.056 |
| Arthritis | 31.78 (0.59) | 27.61 (0.84) | 34.99 (0.83) | <0.001 |
| Depression | 6.22 (0.31) | 5.52 (0.44) | 6.76 (0.42) | 0.039 |
| Sociodemographic Factors | Unadjusted OR (95% CI) | Adjusted OR * (95% CI) |
|---|---|---|
| Age groups | ||
| 65–69 | Reference | Reference |
| 70–74 | 1.22 (1.08–1.39) | 1.15 (1.01–1.31) |
| 75–79 | 1.66 (1.44–1.91) | 1.48 (1.26–1.73) |
| ≥80 | 2.82 (2.38–3.35) | 2.49 (2.05–3.01) |
| Sex | ||
| Men | Reference | Reference |
| Women | 1.30 (1.18–1.43) | 1.32 (1.11–1.57) |
| Education | ||
| ≤9 years | Reference | Reference |
| >9 years | 1.00 (0.89–1.13) | 1.22 (1.07–1.41) |
| Occupation | ||
| Employed | Reference | Reference |
| Unemployed | 1.63 (1.45–1.82) | 1.23 (1.09–1.38) |
| Marital status | ||
| Married | Reference | Reference |
| Unmarried | 1.71 (0.97–3.01) | 1.76 (0.95–3.28) |
| Household composition | ||
| Living with other(s) | Reference | Reference |
| Living alone | 1.47 (1.30–1.65) | 1.24 (1.08–1.43) |
| Household income | ||
| Low | Reference | Reference |
| Middle-low | 0.80 (0.70–0.90) | 1.00 (0.88–1.15) |
| Middle-high | 0.79 (0.68–0.92) | 0.96 (0.81–1.13) |
| High | 0.98 (0.82–1.18) | 1.24 (1.01–1.51) |
| Residence | ||
| Rural | Reference | Reference |
| Urban | 1.27 (1.08–1.50) | 1.35 (1.14–1.61) |
| Variables | Unadjusted OR (95% CI) | Adjusted OR * (95% CI) |
|---|---|---|
| Behavioural factors | ||
| Alcohol consumption | ||
| Non-excessive | Reference | Reference |
| Excessive | 1.01 (0.82–1.24) | 0.81 (0.65–1.02) |
| Smoking habits | ||
| Never | Reference | Reference |
| Past | 0.92 (0.82–1.02) | 1.23 (1.03–1.47) |
| Current | 0.89 (0.76–1.06) | 1.26 (1.02–1.57) |
| Aerobic exercise | ||
| Sufficient | Reference | Reference |
| Insufficient | 1.94 (1.74–2.16) | 1.80 (1.60–2.02) |
| Resistance exercise | ||
| Sufficient | Reference | Reference |
| Insufficient | 1.28 (1.11–1.48) | 1.01 (0.86–1.18) |
| Health factors | ||
| Weight level | ||
| Underweight | 1.31 (0.98–1.75) | 1.12 (0.83–1.52) |
| Normal weight | Reference | Reference |
| Overweight | 1.12 (0.98–1.28) | 1.17 (1.01–1.34) |
| Obese | 1.29 (1.14–1.46) | 1.27 (1.12–1.45) |
| Hypertension | 1.21 (1.09–1.35) | 1.01 (0.90–1.14) |
| Diabetes | 1.26 (1.12–1.40) | 1.17 (1.04–1.32) |
| Cardiovascular disease | 1.46 (1.26–1.69) | 1.30 (1.11–1.52) |
| Cancer | 1.18 (0.99–1.40) | 1.19 (0.99–1.43) |
| Arthritis | 1.41 (1.26–1.57) | 1.26 (1.11–1.43) |
| Depression | 1.24 (1.01–1.53) | 1.16 (0.94–1.44) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jang, D.K.; Park, M.; Kim, Y.H. Sociodemographic, Behavioural, and Health Factors Associated with Sedentary Behaviour in Community-Dwelling Older Adults: A Nationwide Cross-Sectional Study. J. Clin. Med. 2023, 12, 5005. https://doi.org/10.3390/jcm12155005
Jang DK, Park M, Kim YH. Sociodemographic, Behavioural, and Health Factors Associated with Sedentary Behaviour in Community-Dwelling Older Adults: A Nationwide Cross-Sectional Study. Journal of Clinical Medicine. 2023; 12(15):5005. https://doi.org/10.3390/jcm12155005
Chicago/Turabian StyleJang, Dong Kee, Mina Park, and Yeo Hyung Kim. 2023. "Sociodemographic, Behavioural, and Health Factors Associated with Sedentary Behaviour in Community-Dwelling Older Adults: A Nationwide Cross-Sectional Study" Journal of Clinical Medicine 12, no. 15: 5005. https://doi.org/10.3390/jcm12155005
APA StyleJang, D. K., Park, M., & Kim, Y. H. (2023). Sociodemographic, Behavioural, and Health Factors Associated with Sedentary Behaviour in Community-Dwelling Older Adults: A Nationwide Cross-Sectional Study. Journal of Clinical Medicine, 12(15), 5005. https://doi.org/10.3390/jcm12155005





