Polyoxymethylene as Material for Removable Partial Dentures—A Literature Review and Illustrating Case Report
Abstract
1. Introduction
2. Literature Review
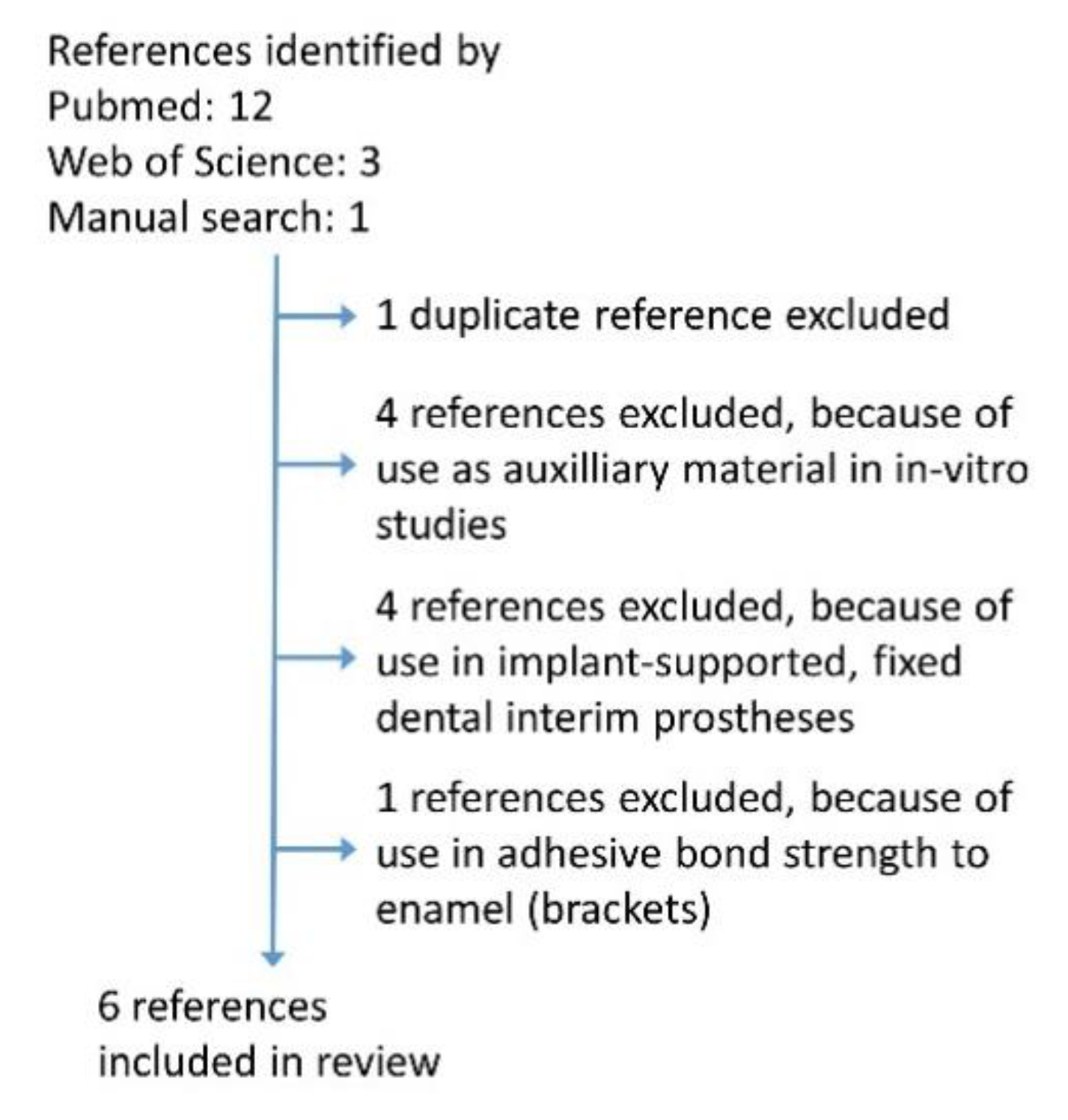
2.1. Search Strategy
2.2. Results of Literature Search
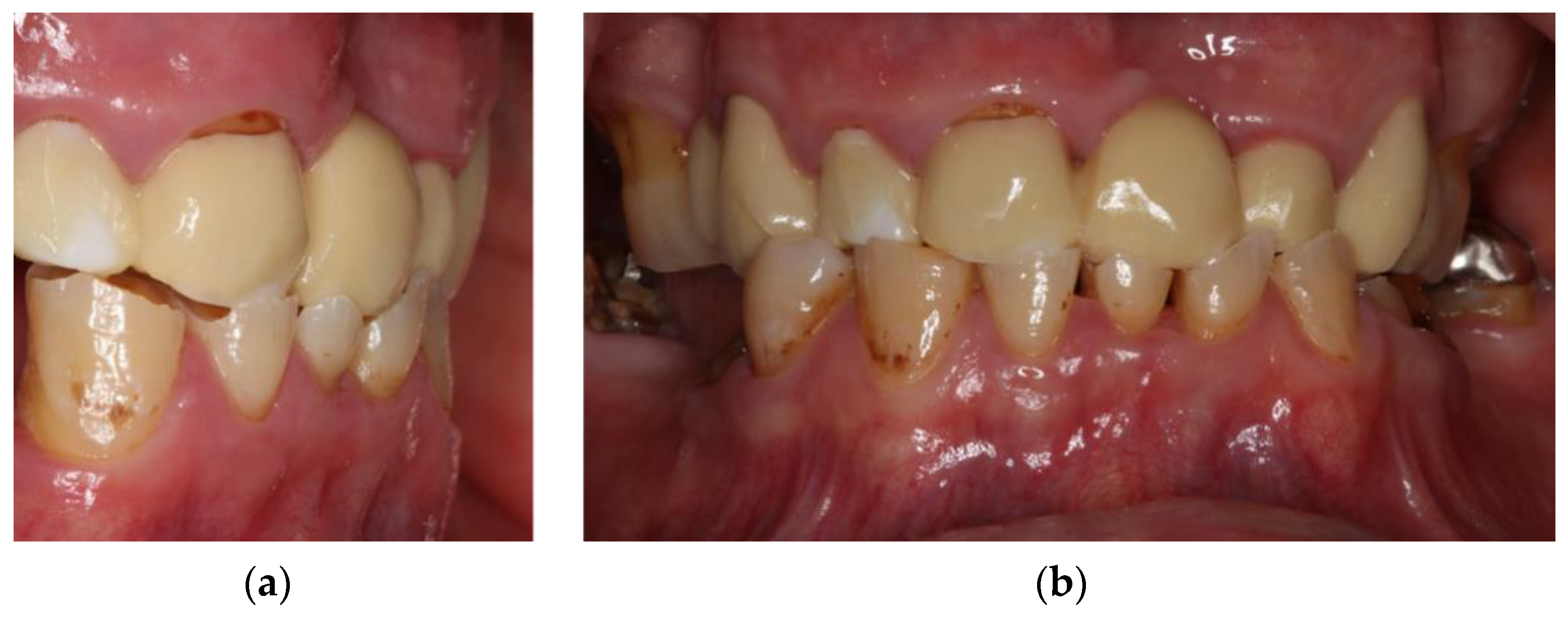
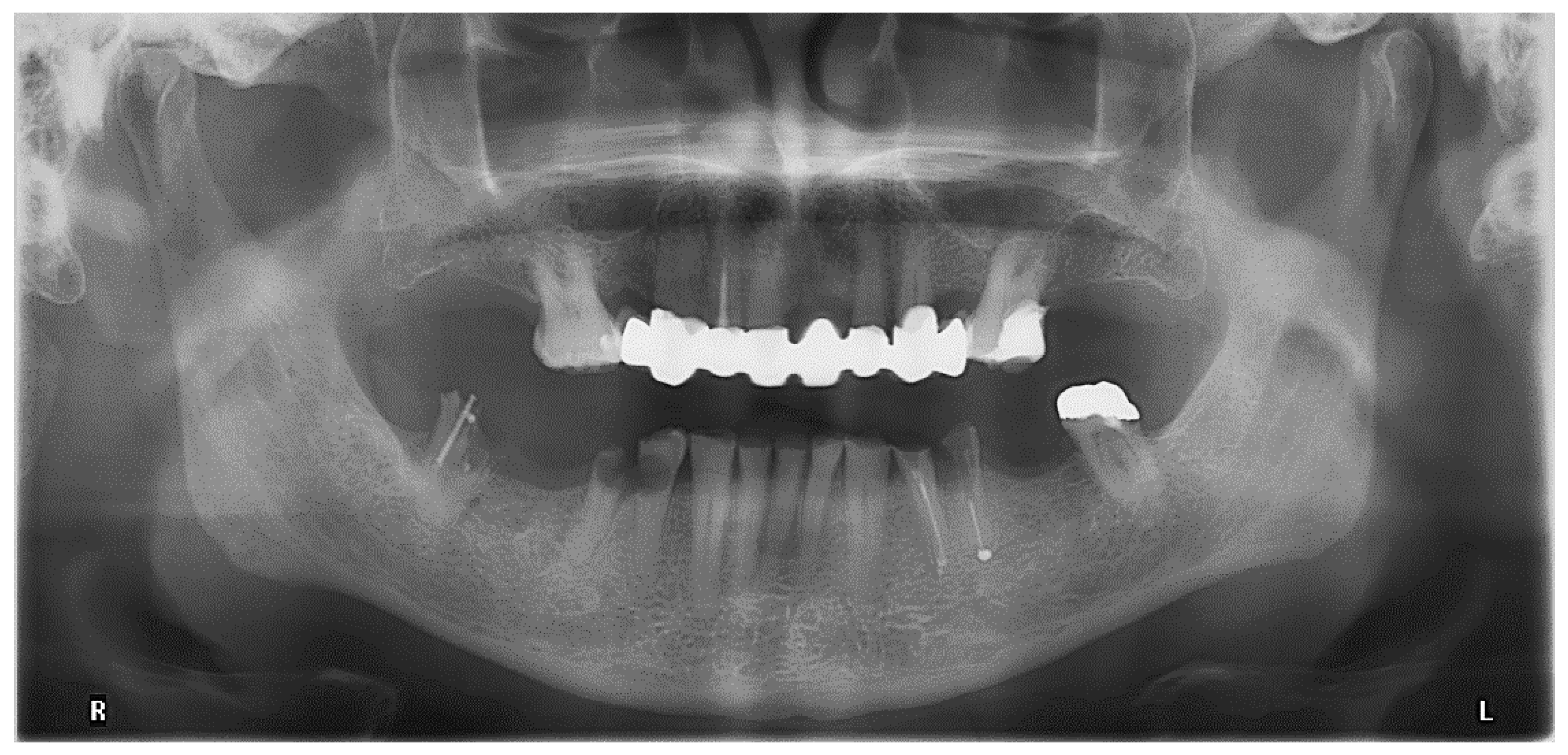
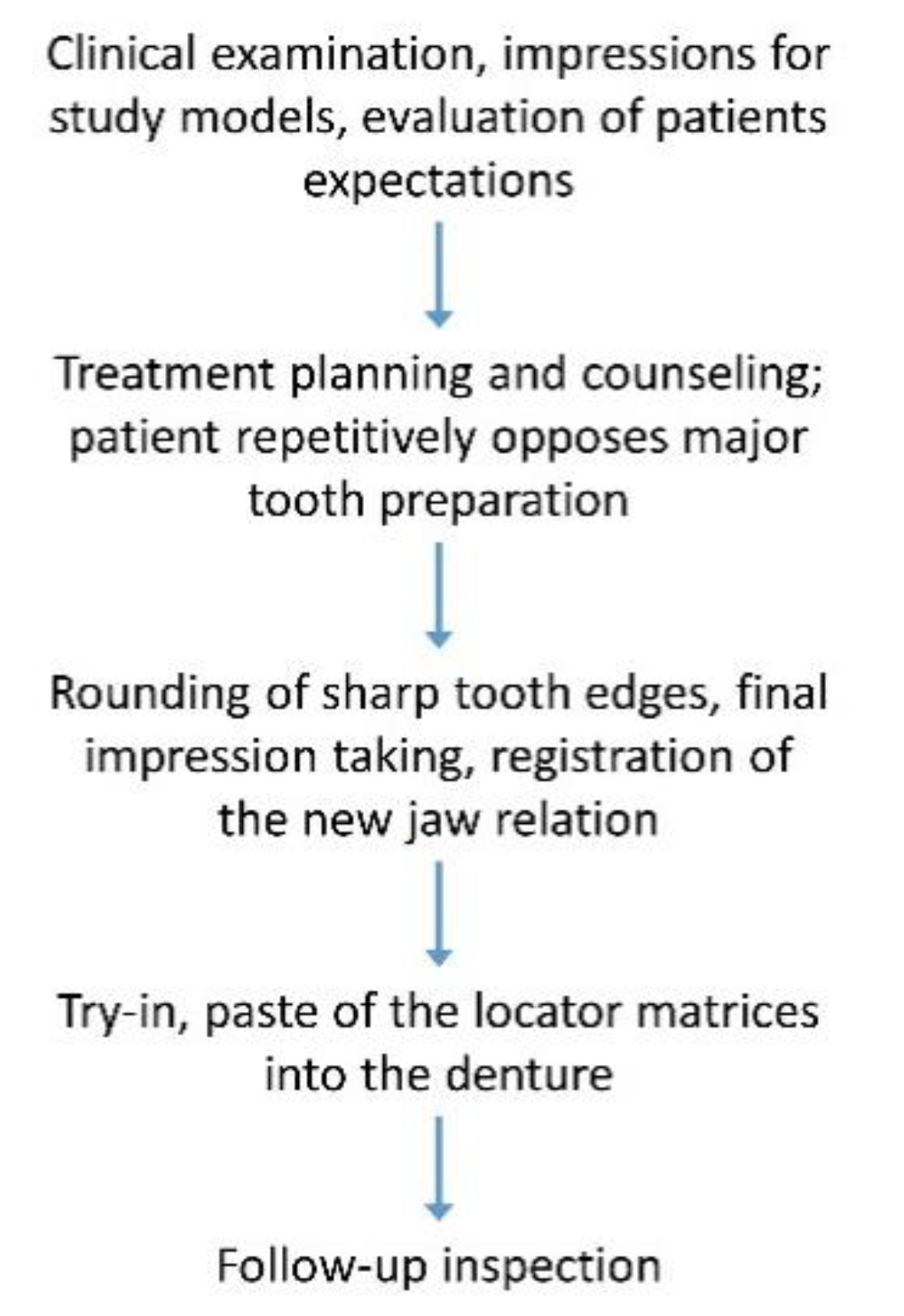
3. Case Report
- Removable multi-unit bridge including all remaining teeth and implants, fabricated from zirconium dioxide telescopic crowns and a veneered polyaryletherketone (PAEK) framework,
- Single-crown fixed dental prostheses for all teeth; Locator abutments on both implants and insertion of a clasp-retained RDP with PAEK framework,
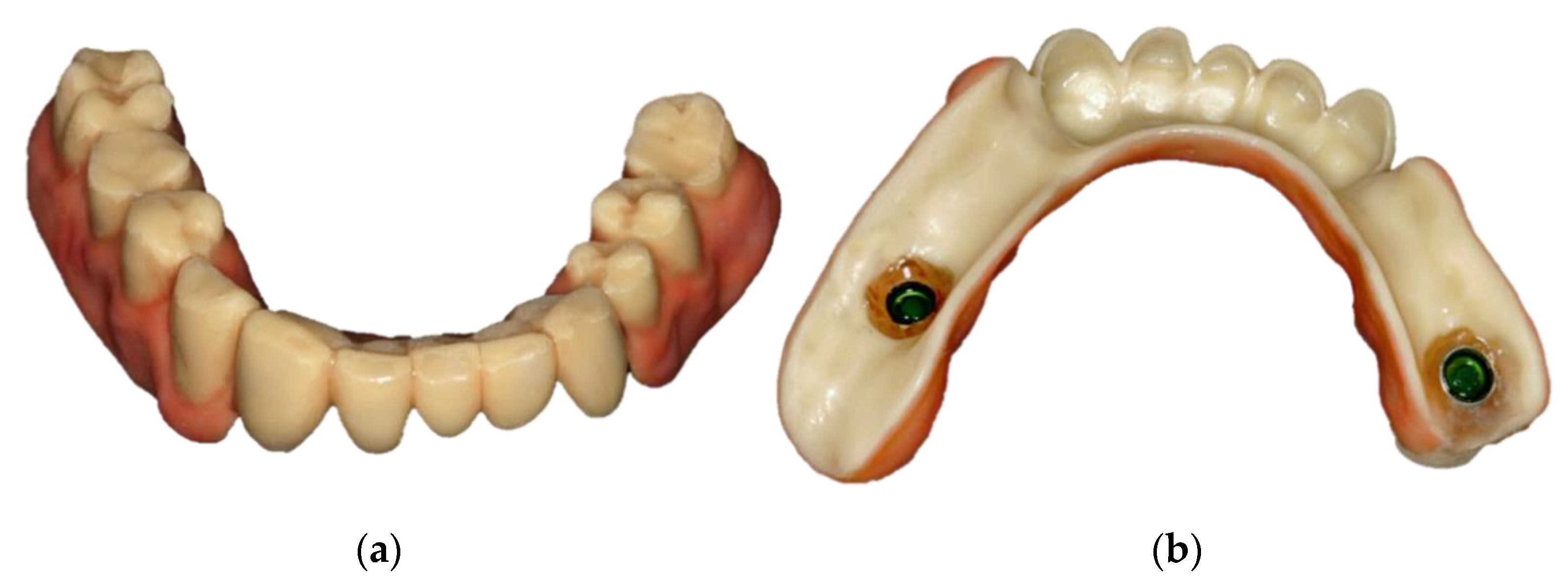
- Locator abutments on both implants, single-crown FDPs on the remaining lower molar teeth, insertion of a tooth-colored and tooth-shaped monolithic RDP fabricated from POM with minimally invasive preparation of the lower anterior teeth (experimental character in long-term endurance).
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
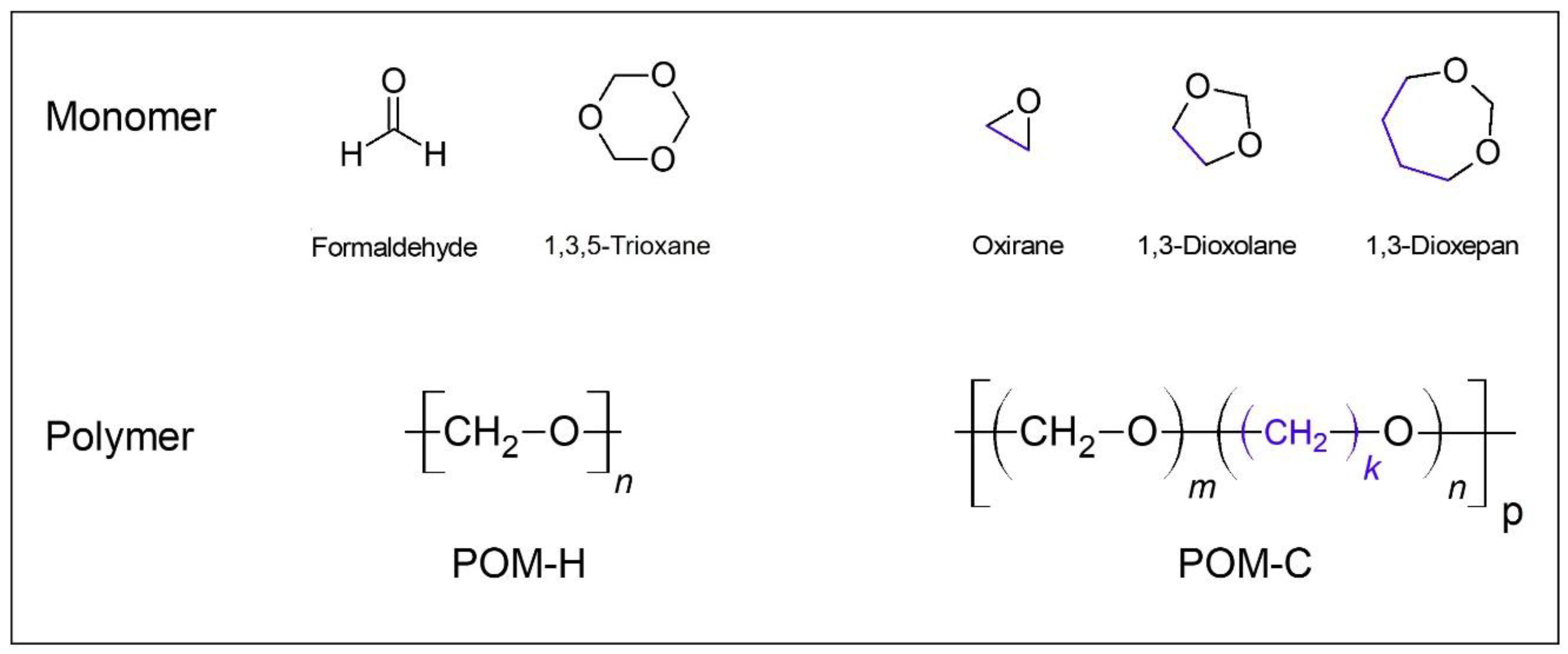
- Uchida, T.; Tadokoro, H. Structural studies of polyethers. IV. Structure analysis of the polyoxymethylene molecule by three-dimensional fourier syntheses. J. Polym. Sci. A-2 Polym. Phys. 1967, 5, 63–81. [Google Scholar] [CrossRef]
- Samyn, P.; van Driessche, I.; Schoukens, G. Thermal and spectroscopic analysis of worn polyoxymethylene surfaces and wear debris explaining degradation and polymerisation mechanisms. J. Polym. Res. 2007, 14, 411–422. [Google Scholar] [CrossRef]
- Eschbach, L. Nonresorbable polymers in bone surgery. Injury 2000, 31, D22–D27. [Google Scholar] [CrossRef]
- Klein, R.; Schüll, C.; Berger-Nicoletti, E.; Haubs, M.; Kurz, K.; Frey, H. ABA Triblock Copolymers Based on Linear Poly(oxymethylene) and Hyperbranched Poly(glycerol): Combining Polyacetals and Polyethers. Macromolecules 2013, 46, 8845–8852. [Google Scholar] [CrossRef]
- Bergmann, W. Werkstofftechnik. Mit 4 Tabellen: Grundlagen, 7th ed.; Carl Hanser: Munich, Germany, 2013. [Google Scholar]
- Dechet, M.A.; Baumeister, I.; Schmidt, J. Development of Polyoxymethylene Particles via the Solution-Dissolution Process and Application to the Powder Bed Fusion of Polymers. Materials 2020, 13, 1535. [Google Scholar] [CrossRef] [PubMed]
- Wendel, B.; Rietzel, D.; Kühnlein, F.; Feulner, R.; Hülder, G.; Schmachtenberg, E. Additive Processing of Polymers. Macromol. Mater. Eng. 2008, 293, 799–809. [Google Scholar] [CrossRef]
- Domininghaus, H.; Elsner, P.; Eyerer, P.; Hirth, T. Kunststoffe. Eigenschaften und Anwendungen, 8th ed.; Springer: Berlin/Heidelberg, Germany, 2012; ISBN 9783642161728. [Google Scholar]
- Rubio, J.C.C.; Panzera, T.H.; Scarpa, F. Machining behaviour of three high-performance engineering plastics. Proc. Inst. Mech. Eng. Part B J. Eng. Manuf. 2015, 229, 28–37. [Google Scholar] [CrossRef]
- Kaiser, W. Kunststoffchemie für Ingenieure. Von der Synthese bis zur Anwendung, 5th ed.; Carl Hanser: Munich, Germany, 2021. [Google Scholar]
- Alqurashi, H.; Khurshid, Z.; Syed, A.U.Y.; Rashid Habib, S.; Rokaya, D.; Zafar, M.S. Polyetherketoneketone (PEKK): An emerging biomaterial for oral implants and dental prostheses. J. Adv. Res. 2021, 28, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Tannous, F.; Steiner, M.; Shahin, R.; Kern, M. Retentive forces and fatigue resistance of thermoplastic resin clasps. Dent. Mater. 2012, 28, 273–278. [Google Scholar] [CrossRef] [PubMed]
- Chuchulska, B.; Yankov, S.; Hristov, I.; Slavchev, D.; Grozev, L. A survey regarding the awareness of thermoplastic resins among bulgarian dentists and dental technicians. J. IMAB 2018, 24, 1863–1865. [Google Scholar] [CrossRef]
- Ali, O.; Makou, M.; Papadopoulos, T.; Eliades, G. Laboratory evaluation of modern plastic brackets. Eur. J. Orthod. 2012, 34, 595–602. [Google Scholar] [CrossRef] [PubMed]
- Polychronakis, N.; Lagouvardos, P.; Polyzois, G.; Sykaras, N.; Zoidis, P. Color changes of polyetheretherketone (PEEK) and polyoxymethelene (POM) denture resins on single and combined staining/cleansing action by CIELab and CIEDE2000 formulas. J. Prosthodont. Res. 2020, 64, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Tribst, J.P.M.; Dal Piva, A.M.d.O.; Borges, A.L.S.; Araújo, R.M.; da Silva, J.M.F.; Bottino, M.A.; Kleverlaan, C.J.; de Jager, N. Effect of different materials and undercut on the removal force and stress distribution in circumferential clasps during direct retainer action in removable partial dentures. Dent. Mater. 2020, 36, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Rosca, B.; Ramalho, S.; Sampaio-Fernandes, J.C.; Portugal, J. Reparability of two different CAD/CAM polymer materials using a light-cured composite and universal adhesives. Rev. Port. Estomatol. Med. Dent. Cir. Maxilofac. 2016, 57, 189–196. [Google Scholar] [CrossRef]




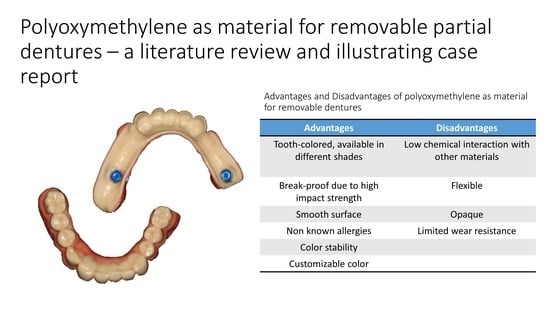
| Advantages | Disadvantages |
|---|---|
| Tooth-colored, available in different shades | Opaque |
| Break-proof due to high impact strength | Flexible |
| Smooth surface | Low chemical interaction with other materials |
| Non known allergies | Limited wear resistance |
| Color stability | |
| Customizable color |
| Material | Potential Allergens |
|---|---|
| Implant, Abutment, Housing | Ti6AI4V ELI, TiN |
| Matrix insert | Nylon |
| Light-curing coloring and glazing material | Methacrylate |
| Self-curing luting material | Hydroxymethacrylate, benzoylperoxide, butylhydroxytoluol |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schierz, O.; Schmohl, L.; Hahnel, S.; Rauch, A. Polyoxymethylene as Material for Removable Partial Dentures—A Literature Review and Illustrating Case Report. J. Clin. Med. 2021, 10, 1458. https://doi.org/10.3390/jcm10071458
Schierz O, Schmohl L, Hahnel S, Rauch A. Polyoxymethylene as Material for Removable Partial Dentures—A Literature Review and Illustrating Case Report. Journal of Clinical Medicine. 2021; 10(7):1458. https://doi.org/10.3390/jcm10071458
Chicago/Turabian StyleSchierz, Oliver, Leonie Schmohl, Sebastian Hahnel, and Angelika Rauch. 2021. "Polyoxymethylene as Material for Removable Partial Dentures—A Literature Review and Illustrating Case Report" Journal of Clinical Medicine 10, no. 7: 1458. https://doi.org/10.3390/jcm10071458
APA StyleSchierz, O., Schmohl, L., Hahnel, S., & Rauch, A. (2021). Polyoxymethylene as Material for Removable Partial Dentures—A Literature Review and Illustrating Case Report. Journal of Clinical Medicine, 10(7), 1458. https://doi.org/10.3390/jcm10071458