Abstract
The transition from control modes to spontaneous modes is ubiquitous for mechanically ventilated patients yet there is little data describing the changes and patterns that occur to breathing during this transition for patients on ECMO. We identified high fidelity data among a diverse cohort of 419 mechanically ventilated patients on ECMO. We examined every ventilator change, describing the differences in >30,000 sets of original ventilator observations, focused around the time of transition from control modes to spontaneous modes. We performed multivariate regression with mixed effects, clustered by patient, to examine changes in ventilator characteristics within patients, including a subset among patients with low compliance (<30 milliliters (mL)/centimeters water (cmH2O)). We found that during the transition to spontaneous modes among patients with low compliance, patients exhibited greater tidal volumes (471 mL (364,585) vs. 425 mL (320,527); p < 0.0001), higher respiratory rate (23 breaths per minute (bpm) (18,28) vs. 18 bpm (14,23); p = 0.003), greater mechanical power (elastic component) (0.08 mL/(cmH2O × minute) (0.05,0.12) vs. 0.05 mL/(cmH2O × minute) (0.02,0.09); p < 0.0001) (range 0 to 1.4), and lower positive end expiratory pressure (PEEP) (6 cmH2O (5,8) vs. 10 cmH2O (8,11); p < 0.0001). For patients on control modes, the combination of increased tidal volume and increased respiratory rate was temporally associated with significantly low partial pressure of arterial oxygen (PaO2)/fraction of inspired oxygen (FiO2) ratio (p < 0.0001). These changes in ventilator parameters warrant prospective study, as they may be associated with worsened lung injury.
1. Introduction
The transition from control modes to spontaneous modes is ubiquitous during critical care, occurring among almost all mechanically ventilated patients. Spontaneous modes always differ from control modes in at least the absence of all of the following: (1) a fixed inspiratory duration, (2) a minimum respiratory rate, and (3) for volume regulated modes, a fixed tidal volume. For patients with improving respiratory function and stable metabolic demands, these differences may not be relevant and observed ventilatory parameters on spontaneous modes may remain unchanged. In contrast, for patients with lung injury, the loss of a fixed inspiratory duration and allowance of an unregulated tidal volume may lead to tachypnea, increased patient effort, and changes in tidal volume.
While there are studies to inform optimal liberation from mechanical ventilation [1,2], there are no studies we identified among patients managed on extracorporeal membrane oxygenation (ECMO). The significance of the concomitant use of ECMO during mechanical ventilation cannot be overstated, and relates primarily to the fact that patients on ECMO can have gas exchange independent of the ventilator. On ECMO, two of the primary drivers of respiratory effort—partial pressure of arterial carbon dioxide (PaCO2) and partial pressure of arterial oxygen (PaO2)—can be modified independently from the ventilator circuit. ECMO thus enables a greater range of ventilator settings—such as respiratory rate and tidal volume—than would be possible without ECMO. As both respiratory rate and tidal volume are important to the development of lung injury [3,4,5,6,7,8,9], we wished to understand ventilator parameters while on ECMO, specifically during the transition from control modes to spontaneous modes.
Our goals were to determine, using high fidelity data among a large cohort of patients on ECMO, (1) if there were differences between the ventilatory parameters during spontaneous modes compared to control modes, (2) if there was a pattern to these differences, (3) if these differences were associated with meaningful clinical changes at the level of the lung, such as changes in oxygenation, excessive tidal volume, or increases in respiratory rate.
2. Experimental Section
2.1. Data Source and Study Population
This secondary analysis was approved by the Institutional Review Board at the University of Utah under #00101562. Patients who received mechanical circulatory support or extracorporeal membrane oxygenation (ECMO) at the University of Utah from 1st January 2010 until 11th April 2019 were identified from the institutional mechanical circulatory support registry and included patients with both venoveno and venoarterial ECMO. Ventilatory data from these patients were then extracted from the University of Utah Electronic Data Warehouse (EDW) by a data scientist blinded to the goals of the analysis. The University of Utah EDW includes all electronic medical record (EMR) entries, including respiratory therapy and ventilator data; it has been previously validated as sufficiently accurate and complete for research [10,11]. Ventilator data is entered into the EMR by a clinical respiratory therapist, who record all changes to the ventilator, including date and time of change and who are in house 24/7. Patients were included in the analysis if they were ≥18 years of age and received ECMO and mechanical ventilation during their admission. We excluded patients who were not mechanically ventilated, who received only non-invasive positive pressure ventilation, who were missing at least one variable for analysis, and we excluded repeat ECMO runs. Supplemental Figure S1 details the patient flowchart.
2.2. Clinical Variables
Variables for analysis included both recorded and calculated variables. Recorded variables included mode (volume control, pressure control, spontaneous, and T-piece (for patients with a tracheostomy), respiratory rate in breaths per minute (BPM), tidal volume (VT) in milliliters (mL), PaO2, fraction of inspired oxygen (FiO2) (from 0.21 to 1), positive end expiratory pressure (PEEP) in centimeters of water (cmH2O), peak inspiratory pressure (PIP) in cmH2O, and respiratory system compliance (in mL/cmH2O). These variables included an associated date and time value. Given the complete capture of ventilatory changes inherent in the electronic data warehouse, variables describing ventilatory parameters such as PEEP or VT were assumed to be unchanged until a subsequent value was entered. For variables that remained unchanged for >24 h, we set all values after 24 h to missing. As patients had data recorded with every change or at least every 4 h if no change, this helped eliminate data errors, as data that had no changes at all for 24 h were felt to be erroneous. Further, as we limited our sensitivity analyses to the period of transition, data outside of 24 h after a transition was effectively eliminated. Derived values were then utilized for analysis of all models and tables, with counts of original observations of each variable reported in the results and below each table.
Calculated variables included (1) PaO2/FiO2 ratio; (2) control versus spontaneous mode categories: “control” included pressure control and volume control, spontaneous included spontaneous and T-piece; and (3) the elastic component of mechanical power. The elastic component of mechanical power has been previously suggested to be a reliable and accurate proxy for the energy applied to the lung during mechanical ventilation that is valid among both paralyzed and spontaneously breathing patients [12]. This is in contrast to the full mechanical power value, which is not valid in spontaneously breathing patients [13]. The elastic component of mechanical power was calculated as:
½ × lung elastance × (VT[in liters]2) × respiratory rate
The first value of any variable per patient was collected at the moment of the start of full support or spontaneous mode, as defined above, after intubation, and the last value collected as the final recorded value prior to extubation. We did not report clinical variables beyond ventilatory settings during the periods defined in each analysis.
2.3. Outcomes
We descriptively report ventilatory parameters over time centering around the transition from control modes to spontaneous modes. Outcomes included PaO2/FiO2 ratio, respiratory rate, VT, PEEP, respiratory system compliance, and elastic component of mechanical power. We examined the association between these variables, examining their change over the duration of time since the switch from control mode to spontaneous mode.
2.4. Statistical Analysis
We compared outcomes by ventilator mode (control versus spontaneous). Outcomes are descriptively reported as median and interquartile range (IQR), with differences assessed by univariate mixed effects panel regression, clustered by patient. Variables are graphically displayed by ventilator mode over time. For graphs showing duration of time at PEEP, VT and mechanical power (elastic component) as a function of ventilator mode, the duration of time at each value was calculated as median per patient and reported as median plus 95% confidence interval (95% CI) by mode. As our primary goal was to demonstrate the changes within patients based on mode, not between patients, we performed multivariate regression with mixed effects, clustered by patient. This is a type of multilevel regression that allows for analysis of data that is correlated within individual patients [14]. We intentionally did not adjust for or report covariates likely to influence differences between patients, such as age, comorbidities, or etiology of cardiopulmonary failure. We adjusted outcomes for potential confounders within patients, which we had determined a priori based on physiologic relevance and availability. Covariates for adjustment varied based on the outcome for each figure, but were selected from duration of time (in hours) since the switch to spontaneous mode, PEEP, compliance, respiratory rate, and VT. Full models are reported in the Supplement Tables S3–S18.
As we did not have data on patient sedation level, or other clinical status, we cannot attribute our findings only to the change in mode, but rather we want to highlight that the change in mode may have occurred, and likely did, in response to a change in patient clinical status. As such, the mode may have been a mediator in a causal pathway. Ventilatory changes may have also been associated with changes in clinical status or level of alertness.
2.5. Sensitivity Analyses
We performed two sensitivity analyses to assess the durability of our findings. First, as our focus was on the changes that occurred with the switch to spontaneous mode, we performed subset analyses to isolate our analysis on changes that were temporally proximate to the transition of mode; this included isolating from 2 h prior to the switch until 24 h after, or from 12 h prior until 24 h after. This accomplishes a few goals. This process ensured that the numbers of values per patient were balanced, effectively normalized for comparable durations of observation. This temporal restriction enables us to mitigate but not eliminate reverse causality, by focusing on ventilatory findings occurring temporally after the transition to spontaneous mode. As such, the transition occurred temporally first, and the ventilatory settings during spontaneous mode occurred temporally after. Variables were also labeled as occurring during spontaneous mode, additionally enabling identification during the period after the transition. Nevertheless, the findings are associations, and we cannot infer directionality beyond this temporal restriction. The temporal restriction also eliminated variance in duration of data collection per patient, normalizing the imbalance in numbers of observations between patients.
Secondly, as our cohort intentionally included patients across a range of cardiopulmonary failure etiologies requiring ECMO, we additionally performed sensitivity analyses to assess for differences when limited to patients with lung injury, such as acute respiratory distress syndrome. We defined this subset by limiting only to patients who had poor lung compliance (≤30 mL/cmH2O) (healthy range 100–400 mL/cmH2O) on first ventilatory assessment. From our previous work among patients with ARDS from three clinical trials [15], the median (IQR) lung compliance among patients was 29 mL/cmH2O (22,38). In other studies, ventilated patients primarily without ARDS (~10% ARDS) had a compliance of 37–111 (IQR) [16]. These studies together suggested to us that initial compliance of ≤30 mL/cmH2O was an appropriate cut-off to identify this subgroup.
All statistical analyses were conducted in STATA v.15.1 (College Park, TX, USA). Given the size of the dataset to minimize type I error (false positive), statistical significance was set at the 0.001 level, and all tests were two-tailed.
3. Results
Among 483 patients initially, after filtering we had 419 patients for analysis. Among these patients, there were 33,940 original observations of VT; 36,882 original observations of respiratory rate; 33,655 original observations of PIP; 10,783 original observations of respiratory system compliance; 36,045 original observations of PEEP; 101,949 calculated observations of the elastic component of mechanical power. Table S1 describes variables across the entire cohort, differences in variables between spontaneous modes and control modes, and the statistical significance of the difference for each variable. Briefly, after adjusting for patient clustering, patients on spontaneous mode, versus (vs.) control modes, exhibited greater VT, improved compliance, and greater mechanical power (elastic component; range 0 to 1.4).
Results are presented among all patients during the period of transition (Section 3.1), among patients with low compliance (Section 3.2), among patients with low compliance during the period of transition (Section 3.3). Graphical results are reported in Section 3.4, with changes in variables as a function of time in Section 3.5.
3.1. Period of Transition
On average, patients underwent a transition from control modes to spontaneous modes 5 (2,8) times. Table 1 describes differences in variables during the transition from control to spontaneous modes (from 12 h prior until 24 h after). Briefly, after adjusting for patient clustering, during spontaneous mode breathing vs. control mode breathing, patients exhibited greater tidal volume (480 mL (375,570.5) vs. 520 mL (411.5,638); p < 0.0001), mechanical power (elastic component) (0.08 mL/(cmH2O × min) (0.05,0.12) vs. 0.06 mL/(cmH2O × min) (0.04,0.09); p < 0.0001) (range 0 to 1.4) and respiratory rate (18 (14,22) vs. 21 (16,27); p = 0.004). During this time, respiratory system compliance was greater and PEEP was statistically significantly lower, but with minimal clinical difference.

Table 1.
Ventilator parameters during the transition from control to support modes.
3.2. Subset Analysis, Patients with Lung Compliance <30 mL/cmH2O
Limited to patients with initial lung compliance <30 mL/cmH2O, Table S2 describes differences in variables by control vs. spontaneous modes. Again, during spontaneous mode breathing vs. control mode breathing, patients exhibited greater VT (469 mL (383,581) vs. 375 mL (260,480); p < 0.0001), and greater mechanical power (elastic component) (0.08 mL/(cmH2O × min) (0.05,0.12) vs. 0.05 mL/(cmH2O × min) (0.02,0.09); p < 0.0001) (range 0 to 1.4), and lower PEEP (6 cmH2O (5,8) vs. 10 cmH2O (8,11); p < 0.0001).
3.3. Subset Analysis, Patients with Lung Compliance <30 mL/cmH2O and during the Period of Transition
Limited to patients with initial lung compliance <30 mL/cmH2O, and only during the period of transition (12 h prior to 24 h after), Table 2 describes differences in variables by control vs. spontaneous modes. Again, during spontaneous mode breathing vs. control mode breathing, patients exhibited greater VT (471 mL (364,585) vs. 425 mL (320,527); p < 0.0001), higher respiratory rate (23 bpm (18,28) vs. 18 bpm (14,23); p = 0.003), and greater mechanical power (elastic component) (0.08 mL/(cmH2O × min) (0.05,0.12) vs. 0.06 mL/(cmH2O × min) (0.03,0.09); p < 0.0001) (range 0 to 1.4).

Table 2.
Subset analysis of ventilator parameters during the transition from control to support modes, among patients with lung compliance <30 cmH2O.
3.4. Graphical Analysis
Figure 1 shows the duration of time (median, 95% CI) per patient at each PEEP range. It can be seen that for patients on spontaneous modes, compared to control modes, significantly more time was spent at lower PEEP levels.
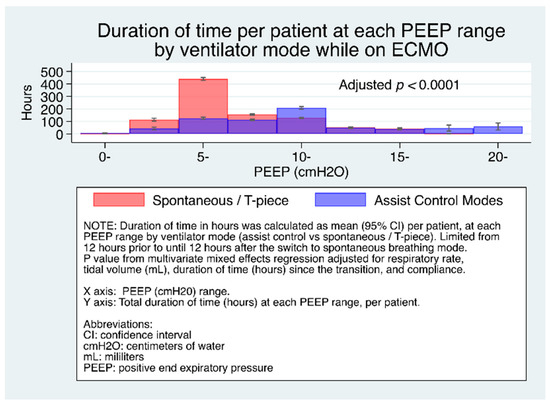
Figure 1.
Duration of time (median, 95% CI) per patient at each PEEP range by ventilator mode.
Figure 2 shows the duration of time (median, 95% CI) per patient at each tidal volume range during the transition to spontaneous breathing among all patients. Table S3 reports the full multivariate model among all patients, and Table S4 reports it among the subset of patients with low compliance. Patients on control modes spent greater time at higher tidal volumes (300–1000+) compared to control modes.
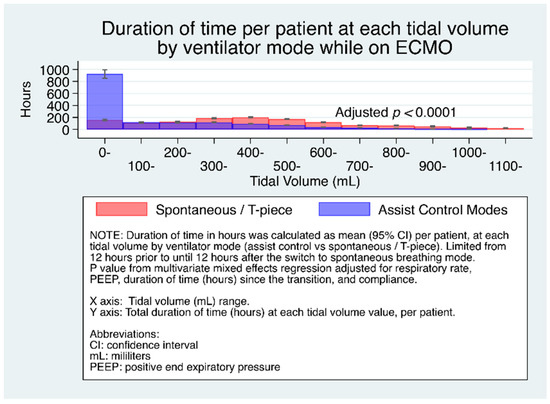
Figure 2.
Duration of time (median, 95% CI) per patient at each tidal volume range by ventilator mode.
Figure 3 shows the duration of time (median, 95% CI) per patient at each level of mechanical power (elastic component) range. The main figure shows the significantly greater time at the lowest mechanical power level for patients on control modes, and that above this level, the inset shows that patients on spontaneous mode had roughly double the duration of time at each higher mechanical power level.
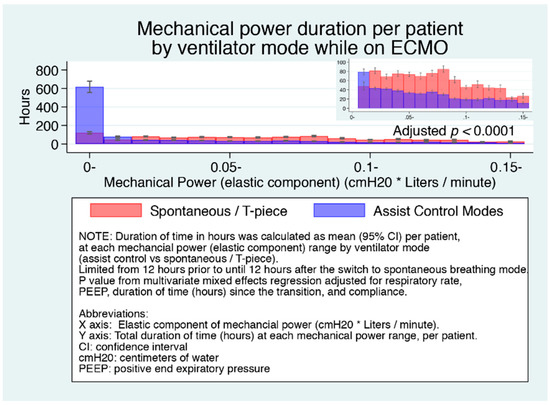
Figure 3.
Duration of time (median, 95% CI) per patient at each mechanical power (elastic component) range by ventilator mode.
3.5. Changes in Variables as a Function of Time
To examine the relationship between respiratory rate over time since the transition to spontaneous mode, we graphed the median (95% CI) respiratory rate of patients, after the switch to spontaneous modes. Figure 4 shows the adjusted increase in respiratory rate increases over time since the transition from control mode to spontaneous mode, among the subset of patients with low compliance. Figure S2 shows this same adjusted increase among all patients.
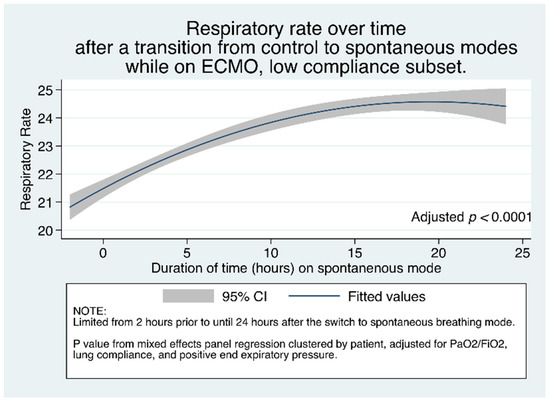
Figure 4.
Respiratory rate over time after a transition from control to spontaneous modes while on ECMO, among patients with low compliance (<30 mL/cmH2O). p value reflects multivariate mixed effect regression, clustered by patient.
To examine the change in PaO2/FiO2 over time after the change to spontaneous modes, we graphed the median (95% CI) across patients. Figure 5 shows that, among patients who are tachypneic (respiratory rate ≥ 30), as duration of time progresses after the transition from control modes to spontaneous modes, after multivariate adjustment with mixed effects clustered by patient, PaO2/FiO2 steadily decreases.
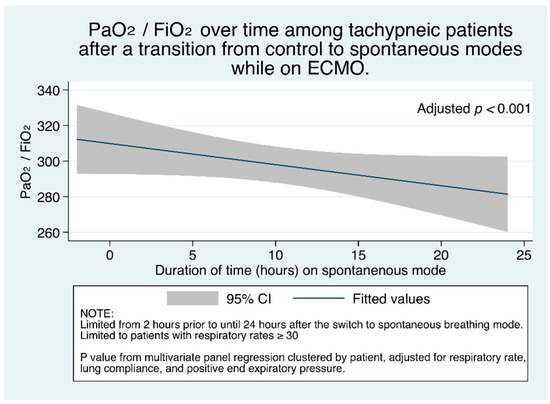
Figure 5.
PaO2/FiO2 ratio (95% CI) over time among tachypneic patients (respiratory rate ≥ 30).
This adjusted decrease in PaO2/FiO2 remained true in subset analysis among patients with low compliance (Figure S3). Decreasing PaO2/FiO2 with increasing duration of time was only true for patients with tachypnea though. Figure S4 shows that among patients without tachypnea, PaO2/FiO2 did not decrease with time in the overall cohort; among patients with low compliance, it significantly increased (Figure S5). This finding of decreasing PaO2/FiO2 only among tachypneic patients, and no change or improving PaO2/FiO2 among patients without tachypnea likely reflects worse lung function and injury in the tachypneic group.
Given our observations on increasing tidal volume and respiratory rate over time, we sought to examine whether the combination of large tidal volumes and increased respiratory rates would be associated with worsened oxygenation, due to development of alveolar injury and edema. Figure 6 shows the adjusted change in PaO2/FiO2 as a function of the combination of respiratory rate and tidal volume among patients on control modes. It can be seen that the combination of increased tidal volume with increased respiratory rate results in significantly decreased PaO2/FiO2. This observation is visually apparent at respiratory rates >25, and magnified with the combination with high tidal volume. The relationships between respiratory rate and PaO2/FiO2 and between tidal volume and PaO2/FiO2 remained qualitatively unchanged, and the variables were still statistically significantly different among the low compliance subset (Figure S6).
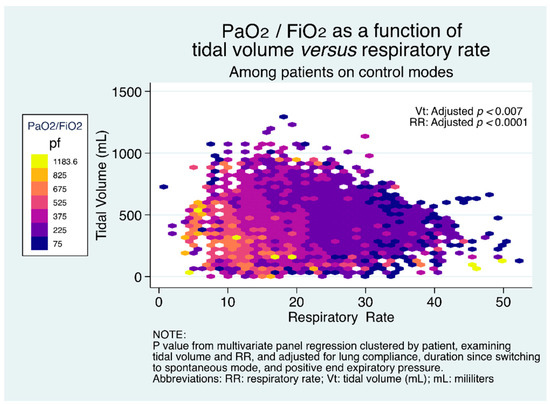
Figure 6.
PaO2/FiO2 as a function of the combination of respiratory rate and tidal volume among patients on control mode.
4. Discussion
We found that beginning with the transition from control mode to spontaneous modes during mechanical ventilation while on ECMO, patients demonstrated overall increased respiratory rates, increased tidal volumes, and increased elastic component of mechanical power. We further observed that increasing tidal volume and increasing respiratory rate were both temporally associated with decreased PaO2/FiO2 ratio, even after adjustment. Finally, we found that the combination of increased tidal volume and increased respiratory rate were additive, with a significantly decreased PaO2/FiO2 among patients with increases in both, especially above respiratory rates of 25.
These findings are the first, to our knowledge, to demonstrate the fixed effect (within patients) of changes in ventilatory parameters while transitioning from control modes to spontaneous modes on ECMO. This transition is ubiquitous among patients weaning from mechanical ventilation, and we found that within this cohort, patients underwent this transition a median of 5 times. The commonality of this transition among this cohort may reflect the ability for ECMO to provide adequate gas exchange despite lower ventilatory settings, and enabling patients to be more alert, both of which may be associated with a transition to spontaneous modes. Our findings are significant in that they suggest that this transition to spontaneous mode may be injurious for many patients, with observed decreases in PaO2/FiO2 ratio, and increases in tidal volume, respiratory rate, and the elastic component of mechanical power. We should note though that the ARMA study demonstrated worsening PaO2 in the group with improved mortality [5], reminding us that we cannot attribute the decreasing PaO2/FiO2 in this study to worsened lung function or harm based on this finding alone. Additionally, as we did not analyze data on dynamic changes in ECMO support, we cannot exclude the fact that the ECMO circuit may have influenced the change in PaO2/FiO2.
Previous studies have demonstrated that spontaneous breathing during mechanical ventilation for ARDS induces a pendelluft phenomenon within the lung [17], in which volumes of gas transition from one region to another without passing through the endotracheal tube, potentially resulting in occult regional over and under distension. Further, spontaneous breathing necessitates active muscle contraction, distorting the relationship between pressures measured at the endotracheal tube and those experienced by regional areas of the lung [18,19]. Thus, the ventilatory measurements, such as PEEP, may be inaccurate in spontaneous breathing patients. To address these limitations, we measured the elastic component of mechanical power, which has been suggested to be a superior method to quantify the energy applied to the lung in patients who are spontaneously breathing [12].
Our findings in this study thus build upon our previous work examining the association of mechanical power and outcomes among patients with ARDS [15]. It has been previously suggested that mechanical power, which encompasses additional ventilatory parameters such as rate, is able to capture repetitive force in a way that static measures are not [15,20,21]. In our previous work, we demonstrated that mechanical power added additional mortality prediction over other measures of force [15]. In this study, we showed that among spontaneously breathing patients, the elastic component of mechanical power was significantly higher among spontaneously breathing patients. If the elastic component of mechanical power is associated with lung injury or patient mortality, then this finding has significant implications. Our study also builds upon important previous knowledge that a period of cyclic overinflation can cause pulmonary edema and lung injury [22,23]. Our study shows that among patients with ECMO and mechanical ventilation, the combination of overinflation and rapid respiratory rate was temporally associated with significantly decreased PaO2/FiO2 ratio. Given our findings are retrospective and show associations only, prospective observational and clinical trials are needed to confirm or refute the validity of our findings.
4.1. Limitations
Our study has a number important limitations. First, our study is largely descriptive of ventilatory observations, and should not suggest causality. Specifically, the factors driving changes in ventilatory parameters were not assessed in this study, and could include changes in metabolic demand (development of sepsis, hemorrhage), changes in sedation, or fluid administration, or worsening of lung injury. These changes may have contributed to the observed changes in ventilatory parameters. We attempted to adjust for relevant confounders for many of our observations, but we recognize that we did not examine all clinical drivers of changes in ventilation or pulmonary function. For instance, as partial pressure of carbon dioxide (PaCO2), a major driver of minute ventilation, was clinically modified though protocoled regular adjustments to sweep gas through the ECMO circuit, we did not adjust for degree of ventilatory failure/PaCO2, which remains an unmeasured covariate. Concomitantly, another important limitation is that as PaO2 could certainly be influenced by ECMO flow rates, we cannot attribute changes in blood oxygenation only to ventilatory changes, as it may have been influenced by ECMO flow or hemoglobin level, which was not available to us.
Secondly, we did not examine global outcomes such as length of stay, mortality or duration of mechanical ventilation. Further studies should examine whether the observed worsening of ventilatory parameters had an association with these important clinical outcomes. It is possible that these changes were not associated with worsened clinical outcome, and were simply reflective of pulmonary mechanical changes during weaning in the setting of acute lung injury.
Thirdly, we appreciate that in this single center analysis the ventilator parameters may be systematically influenced by institutional behavior. We cannot overcome this, but we tried to mitigate the effect by analyzing ~10 years of data, containing over 400 patients managed with ECMO for a variety of indications, in the hope that the temporal span and diversity would surmount patterned behavior in providers. We believe that the consistency and magnitude of our findings suggests some truth to the patterns beyond the institution, but our data requires external validation to confirm or refute our findings.
Finally, our analysis is among a heterogenous clinical group of patients with cardiopulmonary failure, including both ARDS, and patients with cardiogenic shock. The observation of significance within this heterogeneous clinical group suggest to us the durability of our findings, which we additionally confirmed by performing subset analysis among patients with low compliance, as would be found in patients with ARDS. Nevertheless, we recognize that this is imperfect method and further studies should prospectively collect data with consideration of these limitations.
4.2. Conclusions
In this analysis of 419 patients on mechanical ventilation and ECMO, we demonstrated that there were observable and statistically significant changes in ventilatory settings and blood gases during the transition from full support (control) modes to spontaneous modes. We further demonstrated time dependent changes in ventilator parameters around this period of transition. These changes in ventilator parameters warrant prospective study, as they may be associated with worsened lung injury.
Supplementary Materials
The following are available online at https://www.mdpi.com/2077-0383/10/5/1001/s1: Figure S1. Patient enrollment flowchart; Table S1: Ventilator parameters by support mode; Table S2. Subset analysis of ventilator parameters by support mode, among patients with lung compliance <30 cmH2O; Table S3. Multivariate analysis of the association between spontaneous mode and tidal volume during the period of transition. (For Figure 2); Table S4. Multivariate analysis of the association between spontaneous mode and tidal volume during the period of transition, among patients with lung compliance <30 cmH2O; Table S5. Multivariate analysis of the association between spontaneous mode and PEEP during the period of transition. (For Figure 1); Table S6. Multivariate analysis of the association between spontaneous mode and PEEP during the period of transition, among patients with lung compliance <30 cmH2O; Table S7. Multivariate analysis of the association between spontaneous mode and elastic component of mechanical power during the period of transition. (For Figure 3); Table S8. Multivariate analysis of the association between spontaneous mode and elastic component of mechanical power during the period of transition, among patients with lung compliance <30 cmH2O; Table S9. Multivariate analysis of the association between duration of time since transition to spontaneous mode and respiratory rate during the period of transition. (For Figure S2); Table S10. Multivariate analysis of the association between duration of time since transition to spontaneous mode and respiratory rate during the period of transition, among patients with lung compliance <30 cmH2O. (For Figure 4); Table S11. Multivariate analysis of the association between duration of time since transition to spontaneous mode and PaO2/FiO2 during the period of transition, among patients with tachypnea. (For Figure 5); Table S12. Multivariate analysis of the association between duration of time since transition to spontaneous mode and PaO2/FiO2 during the period of transition, among patients without tachypnea. (For Figure S4); Table S13. Multivariate analysis of the association between duration of time since transition to spontaneous mode and PaO2/FiO2 during the period of transition, among patients with tachypnea, low compliance subset. (For Figure S3); Table S14. Multivariate analysis of the association between duration of time since transition to spontaneous mode and PaO2/FiO2 during the period of transition, among patients without tachypnea, low compliance subset. (For Figure S5); Table S15. Multivariate analysis of the association between respiratory rate and PaO2/FiO2 during the period of transition, among patients on control modes. (For Figure 6); Table S16. Multivariate analysis of the association between tidal volume and PaO2/FiO2 during the period of transition, among patients on control modes. (For Figure 6); Table S17. Multivariate analysis of the association between respiratory rate and PaO2/FiO2 during the period of transition, among patients on control modes, low compliance subset. (For Figure S6); Table S18. Multivariate analysis of the association between tidal volume and PaO2/FiO2 during the period of transition, among patients on control modes, low compliance subset. (For Figure S6); Figure S2. Adjusted increase in respiratory rate increases over time since the transition from control mode to spontaneous mode, among patients; Figure S3. PaO2/FiO2 ratio (95% CI) over time among tachypneic patients (respiratory rate ≥ 30), low compliance subset; Figure S4. PaO2/FiO2 ratio (95% CI) over time among patients without tachypnea (respiratory rate < 30); Figure S5. PaO2/FiO2 ratio (95% CI) over time among patients without tachypnea (respiratory rate <3 0), low compliance subset; Figure S6. PaO2/FiO2 as a function of tidal volume and respiratory rate among patients with low compliance.
Author Contributions
Conceptualization, N.M. and J.E.T.; methodology, K.S., N.M. and J.E.T.; software, N.M. and J.E.T.; formal analysis, K.S., N.M. and J.E.T.; investigation, K.S., N.M., S.O., and J.E.T.; data curation, K.S., N.M., and J.E.T.; writing—original draft preparation, J.E.T.; writing—review and editing, K.S., N.M., S.O., and J.E.T.; visualization, K.S., N.M., and J.E.T.; supervision, J.E.T.; funding acquisition: J.E.T. All authors have read and agreed to the published version of the manuscript.
Funding
J.E.T. is supported by a Career Development Award from the National Institutes of Health/National Heart, Lung, And Blood Institute (K23 HL141596).
Institutional Review Board Statement
This study was. Approved 11 July 2017 by the University of Utah Institutional Review Board (IRB) under 00101562.
Informed Consent Statement
Patient consent for this observational study was waived due to IRB determination.
Data Availability Statement
Data code is available from the corresponding author upon reason- able request.
Conflicts of Interest
J.E.T. received speaker fees and travel compensation from LivaNova and Philips Healthcare, unrelated to this work. None of the other authors declare conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Munshi, L.; Ferguson, N.D. Weaning from Mechanical Ventilation: What Should Be Done When a Patient’s Spontaneous Breathing Trial Fails? JAMA 2018, 320, 1865–1867. [Google Scholar] [CrossRef]
- McConville, J.F.; Kress, J.P. Weaning Patients from the Ventilator. N. Engl. J. Med. 2012, 367, 2233–2239. [Google Scholar] [CrossRef]
- Copland, I.B.; Martinez, F.; Kavanagh, B.P.; Engelberts, D.; McKerlie, C.; Belik, J.; Post, M. High tidal volume ventilation causes different inflammatory responses in newborn versus adult lung. Am. J. Respir. Crit. Care Med. 2004, 169, 739–748. [Google Scholar] [CrossRef]
- Hager, D.N.; Krishnan, J.A.; Hayden, D.L.; Brower, R.G. Tidal Volume Reduction in Patients with Acute Lung Injury When Plateau Pressures Are Not High. Am. J. Respir. Crit. Care Med. 2005, 172, 1241–1245. [Google Scholar] [CrossRef]
- Acute Respiratory Distress Syndrome, N.; Brower, R.G.; Matthay, M.A.; Morris, A.; Schoenfeld, D.; Thompson, B.T.; Wheeler, A. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N. Engl. J. Med. 2000, 342, 1301–1308. [Google Scholar] [CrossRef]
- Terragni, P.P.; Del Sorbo, L.; Mascia, L.; Urbino, R.; Martin, E.L.; Birocco, A.; Faggiano, C.; Quintel, M.; Gattinoni, L.; Ranieri, V.M. Tidal volume lower than 6 mL/kg enhances lung protection: Role of extracorporeal carbon dioxide removal. Anesthesiology 2009, 111, 826–835. [Google Scholar] [CrossRef] [PubMed]
- Frank, J.A.; Gutierrez, J.A.; Jones, K.D.; Allen, L.; Dobbs, L.; Matthay, M.A. Low tidal volume reduces epithelial and endothelial injury in acid-injured rat lungs. Am. J. Respir. Crit. Care Med. 2002, 165, 242–249. [Google Scholar] [CrossRef] [PubMed]
- Grasso, S.; Stripoli, T.; Mazzone, P.; Pezzuto, M.; Lacitignola, L.; Centonze, P.; Guarracino, A.; Esposito, C.; Herrmann, P.; Quintel, M.; et al. Low respiratory rate plus minimally invasive extracorporeal Co2 removal decreases systemic and pulmonary inflammatory mediators in experimental Acute Respiratory Distress Syndrome. Crit. Care Med. 2014, 42, e451–e460. [Google Scholar] [CrossRef]
- Araos, J.; Alegria, L.; Garcia, P.; Cruces, P.; Soto, D.; Erranz, B.; Amthauer, M.; Salomon, T.; Medina, T.; Rodriguez, F.; et al. Near-Apneic Ventilation Decreases Lung Injury and Fibroproliferation in an ARDS Model with ECMO. Am. J. Respir. Crit. Care Med. 2018. [Google Scholar] [CrossRef]
- Lee, V.S.; Kawamoto, K.; Hess, R.; Park, C.; Young, J.; Hunter, C.; Johnson, S.; Gulbransen, S.; Pelt, C.E.; Horton, D.J.; et al. Implementation of a Value-Driven Outcomes Program to Identify High Variability in Clinical Costs and Outcomes and Association with Reduced Cost and Improved Quality. JAMA 2016, 316, 1061–1072. [Google Scholar] [CrossRef] [PubMed]
- Kawamoto, K.; Martin, C.J.; Williams, K.; Tu, M.C.; Park, C.G.; Hunter, C.; Staes, C.J.; Bray, B.E.; Deshmukh, V.G.; Holbrook, R.A.; et al. Value Driven Outcomes (VDO): A pragmatic, modular, and extensible software framework for understanding and improving health care costs and outcomes. J. Am. Med. Inform. Assoc. JAMIA 2015, 22, 223–235. [Google Scholar] [CrossRef] [PubMed]
- Huhle, R.; Serpa Neto, A.; Schultz, M.J.; Gama de Abreu, M. Is mechanical power the final word on ventilator-induced lung injury?-no. Ann. Transl. Med. 2018, 6, 394. [Google Scholar] [CrossRef]
- Chiumello, D.; Gotti, M.; Guanziroli, M.; Formenti, P.; Umbrello, M.; Pasticci, I.; Mistraletti, G.; Busana, M. Bedside calculation of mechanical power during volume- and pressure-controlled mechanical ventilation. Crit. Care 2020, 24, 417. [Google Scholar] [CrossRef]
- Kreft, I.; de Leeuw, J. Introducing Multilevel Modeling; Sage Publications, Inc.: New York, NY, USA, 1998. [Google Scholar] [CrossRef]
- Tonna, J.E.; Peltan, I.; Brown, S.M.; Herrick, J.S.; Keenan, H.T.; University of Utah Mechanical Power Study, G. Mechanical power and driving pressure as predictors of mortality among patients with ARDS. Intensive Care Med. 2020. [Google Scholar] [CrossRef]
- Serpa Neto, A.; Deliberato, R.O.; Johnson, A.E.W.; Bos, L.D.; Amorim, P.; Pereira, S.M.; Cazati, D.C.; Cordioli, R.L.; Correa, T.D.; Pollard, T.J.; et al. Mechanical power of ventilation is associated with mortality in critically ill patients: An analysis of patients in two observational cohorts. Intensive Care Med. 2018, 44, 1914–1922. [Google Scholar] [CrossRef]
- Yoshida, T.; Torsani, V.; Gomes, S.; De Santis, R.R.; Beraldo, M.A.; Costa, E.L.; Tucci, M.R.; Zin, W.A.; Kavanagh, B.P.; Amato, M.B. Spontaneous effort causes occult pendelluft during mechanical ventilation. Am. J. Respir. Crit. Care Med. 2013, 188, 1420–1427. [Google Scholar] [CrossRef]
- Gattinoni, L.; Tonetti, T.; Quintel, M. Regional physiology of ARDS. Crit. Care 2017, 21, 312. [Google Scholar] [CrossRef] [PubMed]
- Gama de Abreu, M.; Cuevas, M.; Spieth, P.M.; Carvalho, A.R.; Hietschold, V.; Stroszczynski, C.; Wiedemann, B.; Koch, T.; Pelosi, P.; Koch, E. Regional lung aeration and ventilation during pressure support and biphasic positive airway pressure ventilation in experimental lung injury. Crit. Care 2010, 14, R34. [Google Scholar] [CrossRef] [PubMed]
- Gattinoni, L.; Tonetti, T.; Cressoni, M.; Cadringher, P.; Herrmann, P.; Moerer, O.; Protti, A.; Gotti, M.; Chiurazzi, C.; Carlesso, E.; et al. Ventilator-related causes of lung injury: The mechanical power. Intensive Care Med. 2016, 42, 1567–1575. [Google Scholar] [CrossRef] [PubMed]
- Marini, J.J.; Rocco, P.R.M. Which component of mechanical power is most important in causing VILI? Crit. Care 2020, 24, 39. [Google Scholar] [CrossRef]
- Dreyfuss, D.; Soler, P.; Saumon, G. Spontaneous resolution of pulmonary edema caused by short periods of cyclic overinflation. J. Appl. Physiol. (1985) 1992, 72, 2081–2089. [Google Scholar] [CrossRef]
- Dreyfuss, D.; Saumon, G. Ventilator-induced lung injury: Lessons from experimental studies. Am. J. Respir. Crit. Care Med. 1998, 157, 294–323. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).